Coronary Artery Disease and IHD
-
Upload
sudip-devadas -
Category
Documents
-
view
6 -
download
0
description
Transcript of Coronary Artery Disease and IHD
-
Coronary Artery Disease (Ref. Hari. 18 ed., pg -1998)
Angina Pectoris
Basic physiology
1. Coronary flow is maximum at early diastole.
2. 80% of the coronary filling occurs duringdiastole.
3. In aorta, blood flow drops maximum at the endof diastole.
Angina Pectoris is best diagnosed by history. (AIPG2010)
1. This is due to myocardial ischaemia andpresents as a central chest tightness orheaviness (Levine sign) which is brought onby exertion and relieved by rest.
2. It may radiate to one or both arms ,the neck,jaw or teeth. Atherosclerosis is the mostcommon cause of CAD.
3. ECG and Echo may be normal and cardiacenzyme are usually not raised in angina.
Unstable angina (Ref. Hari. 18 ed., Pg-2015)
Definition
1. Pts with new onset angina ( 4 - 6 weeks) that
$PSPOBSZ"SUFSZ%JTFBTF
th
th
-
is severe and/or frequency (>3 episodes/day)
2. Pts with accelerating anginaprolonged, morefrequent, severe or precipitated by lessexertion than previously
3. Pts with angina at rest or by minimalexertion usually lasting for >10 mints.
Important Points:
1. Variant (Prinzmetal's) angina: caused bycoronary artery spasm . Patient has painchest at rest & ECG show ST segmentelevation. Treatment Ca channel blocker andnitrates but beta blockers are Contraindicated.
2. Microvascular angina: In this case patient hassymptoms of angina i.e. he has pain chestwhich is precipitated by exertion. But he hasnormal coronary angiography. It occurs due toabnormal constriction or failure of relaxationof coronary resistance vessels. (Slow flowphenomena)
Important Points:
Tests
1. ECG: usually normal but may show STdepression; flat or inverted T waves'.
2. If resting ECG is normal, then do exercise ECG
Criteria of positive TMT
1. Appearance of horizontal or ST depression > 1mm lasting for > 0.08 Sec
2. Systolic fall of BP > 10mmHg
3. Development of VT
Q
Q
Q
Q
-
Extra Edge: An abnormal ST segment on a resting ECG,as seen in LBBB, LVH, or the use of digoxin by thepatient all reduce the accuracy of this test.Extra Edge: Those patients who can not run on the TMTmachine than drug induce stress test is done by usinginjection dobutamine
Angiography If TMT is positive than the nextinvestigation is angiography.TIMI Risk Score for Unstable Angina (UA) /Non STelevated MI (NSTEMI)
It estimates mortality for patients with unstable anginaand non-ST elevation MI.
The factors are:
1. Age 65 years
2. 3 Risk Factors for CAD
3. Known CAD (stenosis 50%)
4. Aspirin Use in Past 7d
5. Severe angina ( 2 episodes w/in 24 hrs)
6. ST changes 0.5mm
7. Elevated Cardiac Marker
Recent Advances: Pathology of Plaque.
1. Atherosclerotic plaques become progressivelycalcified over time, increases with age.
2. For this reason, methods for detectingcoronary calcium have been developed as ameasure of the presence of coronaryatherosclerosis.
3. Detection of calcium in atherosclerotic plaqueby electron beam CT scan (EBCT).
-
4. Coronary calcium detected by these imagingtechniques is quantified using the Agatstonscore most commonly, which is based on thearea and density of calcification.
Recent Advances:
1. LV dysfunction can be due to noncontractile orhypocontractile segments that are viable butare chronically ischemic (hibernatingmyocardium). (AIIMS May 2011)
2. As a consequence of chronic reduction inmyocardial blood flow these segments downregulate their contractile function.
3. These can be detected by using radionuclidescans of myocardial perfusion andmetabolism, PET or delayed scanning withthallium-201; or by improvement of regionalfunctional impairment, provoked by low-dosedobutamine.
4. In such patients, revascularization improvesmyocardial blood flow, can return function,and can improve survival.(Ref. Hari. 18 ed.,pg-2013)
Stress scintigraphy,
1. When used in combination with the stressECG, has yielded increased sensitivity (80%)and specificity (92%) over the standard stressECG alone.
2. Therefore, it is a particularly useful diagnostictool when the standard stress ECG is expectedto be of low yield (e.g., in patients with bundlebranch block) and in patients in whom aprevious stress ECG has produced equivocalresults.
th
-
3. Method. When the radioactive isotope thallium201 ( TI) or the technetium-based isonitrilesestamibi is injected into the peripheralvenous blood, the myocardial distribution ofthe substance is affected by blood flow andischemia, with areas of less blood flow andischemia taking up less TI or sestamibithan areas of normal blood flow. Withexercise, blood flow increases, but in patientswith coronary artery disease, those parts ofthe myocardium supplied by diseasedcoronary arteries and areas of MI take up less
TI or sestamibi than normal areas. Inpatients who are unable to exercise, infusionof dobutamine (to increase oxygen demand) ordipyridamole or adenosine (to cause coronaryvasodilation) are used to alter coronary flow.
Stress echocardiography. Echocardiography can detectregional ischemia by identifying areas of wall motionabnormalities that occur with stress and are notpresent at rest. This regional dysfunction indicates thatthe area involved is not receiving adequate blood flow.The sensitivity is similar to radionucleotide imaging.Cardiac catheterization with coronary arteriographyallows for direct visualization of the coronary arteriesby selective injection of radiographic contrast material.This procedure is the most sensitive and specific testcommonly used for coronary artery disease.
Recent Advances in Nuclear imaging
1. Thallium scan
2. Technetium 99 scan
3. PET using N-13 NH3 or rubidium 82.
201
201
201
-
Coronary angiography.
When assessed angiographically, flow in the culpritcoronary artery is described by a simple qualitativescale called the thrombolysis in myocardial infarction(TIMI) grading system:
Grade 0 indicates complete occlusion of the infarct-related artery;
Grade 1 indicates some penetration of the contrastmaterial beyond the point of obstruction but withoutperfusion of the distal coronary bed;
Grade 2 indicates perfusion of the entire infarct vesselinto the distal bed but with flow that is delayedcompared with that of a normal artery;
Grade 3 indicates full perfusion of the infarct vesselwith normal flow.
Management
1. Oral Antiplatelet (Ref. Hari. 18 ed., pg - 2019)
a. Aspirin reduces mortality by 34%.(AIIMS Nov 2010)
b. Prasugrel
c. Clopidogrel
2. Intravenous antiplatelet therapy
a. Abciximab
b. Eptifibatide
c. Tirofiban
3. Anticoagulant
a. Unfractionated heparin (UFH)
b. Enoxaparin
c. Fondaparinux
th
-
d. Bivalirudin
4. Beta blockers:
5. Nitrates:
6. Calcium antagonists: diltiazem (in Prinzmetalangina).
7. Statin if total cholesterol is high
8. K+ channel activator, eg Nicorandill
9. Ranolazine It is new anti anginal drug usefulfor refractory angina. (AIIMS May 2011)
Ranolazine, use for patients with chronicangina who continue to be symptomaticdespite a standard medical regimen. Themechanism it inhibits the late inwardsodium current (INa).
10. Revascularization.
Indication of revascularization & CABG (Ref. Hari. 18ed., pg - 2013)
a. Patients with an unacceptable level of anginadespite optimal medical management shouldbe considered for coronary revascularization.
b. Patients with single- or two-vessel diseasewith normal LV function and anatomicallysuitable lesions ordinarily are advised toundergo PCI.
c. Patients with three-vessel disease (or two-vessel disease that includes the proximal leftdescending coronary artery) and impairedglobal LV function (LV ejection fraction < 50%)or diabetes mellitus and those with left maincoronary artery disease or other lesionsunsuitable for catheter-based proceduresshould be considered for CABG as the initial
th
-
method of revascularization.
1. Percutaneous transluminal coronary angioplasty(PTCA)
a. Involves balloon dilatation of thestenotic vessel(s).
b. Stenting reduces restenosis rates.
c. Drug-coated stents reduce restenosis.Drug used are a. Sirolimus (also knownas Rapamycin) , b. Paclitaxel (MCQ)
d. Antiplatelet agents, eg clopidogrelreduce the risk of stent thrombosis.
e. IV platelet glycoprotein IIb/IIIa- inhibitorcan reduce procedure-related ischemicevents.
Example: eptifibatide , tirofiban,abciximab
2. Thrombolysis: Hemorrhage is the most frequentand potentially the most serious complication.
Recent Advances: Triflusal (New Drug)
Triflusal is a platelet aggregation inhibitor
Mechanism of action:
Triflusal is a platelet antiaggregant through;
1. Blocks cyclooxygenase inhibitingthromboxane A2, preventing aggregation.
2. 2, Preserves vascular prostacyclin, thuspromoting anti-aggregant effect
3. Blocks phosphodiesterase thereby increasingcAMP concentration, thereby promoting anti-aggregant effect due to inhibition of calciummobilization
Q
Q
-
Algorithm for risk stratification and treatment ofpatients with suspected CAD.
1. Low risk patient having UA/NSTEMI. Earlyconservative therapy = Aspirin clopidogrel,anticoagulant, anti-ischemic therapy.
2. High risk patient having UA/NSTEMI = Aspirin,anticoagulant, ADP inhibitor, (use IIb/IIIainhibitor if unstable angina is there) anti-ischemic therapy, early invasive therapy.
3. STEMI = Percutaneous coronary intervention(PCI), thrombolysis
Anticoagulant are LMWH, Fondaparinux
Anti-ischemic therapy = beta-blockers nitrate
ADP antagonist = Clopidogrel or prasugrel.
Recent Advances:
Black hole phenomena
1. Restenosis remains an important issue evenafter coronary brachytherapy despite itsefficacy in the treatment for in-stentrestenosis.
2. Vascular radiation was proposed as a therapyfor restenosis prevention.
3. Intracoronary radiation therapy and make it asafe, feasible, effective, and clinically usefultool to reduce restenosis.
4. The acute and chronic changes in vascularwall are unique following brachytherapy.
5. The restenotic tissue post coronarybrachytherapy is relatively acellular andappears echolucent in intravascularultrasound examination.
6. This is dubbed the black hole phenomenon.
-
Despite the similarity in the mode of action ofbrachytherapy and drug eluting stentimplantation, the black hole phenomenonseems to be uncommon after drug-elutingstent implantation except in those patientswho have had prior brachytherapy, bare-metalplacement and after treatment of saphenousvenous graft stenosis
Acute MI {Acute coronary syndrome (ACS)}(Ref. Hari.18 ed., Pg-2021)Definitions ACS includes unstable angina and evolvingMI, which share a common underlying pathology-plaquerupture, thrombosis, and inflammation.
ACS may rarely be due to emboli or coronary spasm innormal coronary arteries, or vasculitis.(Ref: Journal of the American College of Cardiology andAHA)
Table: Clinical classification of different types ofmyocardial infarction.
Type 1
Spontaneous myocardial infarction related to ischemiadue to a primary coronary events such as plaqueerosion and/or rupture, fissuring, or dissection.
Type 2
Myocardial infarction secondary to ischemia due toeither increased oxygen demand or decreased supply,e.g. coronary artery spasm, coronary embolism, anemia,arrhythmias, hypertension, or hypotension.
Type 3
th
-
Sudden unexpected cardiac death, including cardiacarrest, often with symptoms suggestive of myocardialischemia, accompanied by presumably new STelevation, or new LBBB, evidence of fresh thrombus in acoronary artery by angiography and/or at autopsy, butdeath occurring before blood samples could beobtained, or at a time before the appearance of cardiacbiomarkers in the blood.
Type 4a
Myocardial infarction associated with PCI
Type 4b
Myocardial infarction associated with stent thrombosisas documented by angiography or at autopsy
Type 5Myocardial infarction associated with CABGThe new ACC/ESC definition of myocardial infarction(MI)Definition of reinfarction
The definition of MI in patients undergo-ing CABG, TheCK-MB threshold should be 5times the upper limit ofnormal and the CK-MB threshold for PCI should be 3times the upper limit of normal.Diagnosis is based on the presence of at least 2 out of 3of (WHO criteria):
1. Typical history
2. ECG: changes
3. Cardiac enzyme rise.
Symptoms
1
-
1. Acute central chest pain, lasting >20min, oftenassociated with nausea sweating, dyspnea,palpitations. Ashen Grey Colour of the face isan important feature.
2. May present without chest pain ('silent'infarct) in elderly or diabetics . In suchpatients, presentations may include: profusesweating, syncope, pulmonary oedema,epigastric pain and vomiting, hypotension,oliguria, acute confusional state.
Signs:
1. Sweating, pulse increase or decrease, BPincrease or decrease.
2. Bradycardia is seen in Inferior wall MI.
3. There may be signs of heart failure raised JVP,3rd & 4 heart sound and basal crepitation
4. A pansystolic murmur (papillary muscledysfunction/rupture, or VSD).
5. A pericardial friction rub
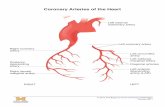
Arterial supply
1. Anteroseptal Left anterior descending (LAD)(Most common site)
2. Lateral wall Left circumflex
3. Inferior wall Right coronary artery (Second Most common site)
Important Points:LAD = Widows artery (LQ 2012)
1. Ant wall MI findings seen in leads - V V ,L1, AVL Artery involved left coronary artery
2. Inf wall MI - LII, LIII, AVF Artery involvedright coronary artery
Q
th Q
Q
Q
1 6
Q
Q
Q
-
3. Lat wall MI - LI, AVL, V , V Artery involvedcircumflex
4. Antero septal = V Most common site, Arteryinvolved LED.
Tests
1. ECG: Classically, hyperacute (tall) T waves (1sign of MI in ECG) (LQ 2012) occurs withinminutes of MI.
2. ST elevation (Pardees) or occur within 2 3hours.
3. T wave inversion occurs with in 8-12 hrs anddevelopment of pathological Q waves(transmural infarction) follow over 18-24 hoursto days.
4. In 10- 20% of cases of acute MI, the ECG maybe normal initially !!!.
5. Right coronary artery supply right ventricle,inferior wall of LV and posterior part of theinterventricular septum. ECG is not a good toolto diagnose ischemia of the posterior part ofinterventricular septum.
Serum cardiac markers
Enzyme Begin Peak Normal
CPK MB 4 8 hr 16 32 hr 2 3 days
LDH 12 24 hr 48 60 hr 7 10 weeks
Extra Edge
1. CPK MB / CPK- ratio of >2.5 is highlysuggestive of MI.
2. CPK MB also raised in
5 6 Q
1-3
st
Q
Q
Q
-
a. Myocarditis
b. Electrical cardioversion
c. Cardiac surgery
3. CPK MB has two isoforms
4. CPK MB /CPK MB >1.5 highly sensitive for MI
5. Cardiac specific Troponin T/Troponin I (LQ2012)are normally not detectable in the blood ofhealthy individuals but may increase after STEMIto levels >20 times higher than the upper level.So they are preferred biochemical markers for MI
(Ref. Hari. 18 ed., pg -2023)
6. Troponin T Test (TnT) Becomes +ve with in 2 4 hr and remain elevated for upto 10 14 days.Troponin T is the best test to diagnosis acute MI.Only in cases of reinfarction within 2 weeks, CPK-MB is more useful than troponin T.
Management of acute coronary syndrome (ACS)
1. Aspirin 300mg chewed
2. GTN sublingual.
3. Analgesia Morphine 2-3 mg IV or 10 15 mgIM
4. Thrombolysis, if no contraindication or primaryangioplasty
5. Beta-blocker
6. ACE-inhibitor. Consider starting ACE-I (eglisinopril 2.5mg) even in all normotensivepatients within 24h of acute MI, especially ifthere is clinical evidence of heart failure orecho evidence of LV dysfunction.
2 1 Q
Q th
Role of ACEI in acute MI
-
7. Low molecular weight heparin (eg enoxaparin).
8. GP IIb/ IIIa antagonist (eg tirofiban) used in High-risk patients (persistent or recurrent ischaemia,ST-depression, diabetes, raised troponin)
9. Clopidogrel, in addition to aspirin, should beconsidered for up to 12 months.
Important Points:
1. Warfarin is not used in treatment of Ac MI.
2. Triflusal reduces thromboxane synthesis soprevents platelet aggregation. It is analterative to aspirin in secondary prophylaxisof CVA and MI.
(This is new drug. It is not given in Harrison18 Edition !!!)
3. Trimetazidine is controls myocardial ischemiathrough intracellular metabolic changes. Itprotect the heart from the deleterious effectsof ischemia, and enhance LV contractility inpatients with stunned or hibernatingmyocardium. (AIIMS Nov 2012)
4. Ticagrelor has been approved for thereduction of thrombotic events in patientswith acute coronary syndrome.
Recent advances in the management of MI
1. Enhanced external counter pulsation (Ref.Hari. 18 ed., pg -2013)
a. Enhanced external counterpulsation
1. To control BP
2. To control LVF
3. To help in the remodeling of infarct tissue.
th
th
-
utilizes pneumatic cuffs on the lowerextremities to provide diastolicaugmentation and systolic unloadingof blood pressure in order to decreasecardiac work and oxygen consumptionwhile enhancing coronary blood flow.
b. Regular application improves angina,exercise capacity, and regionalmyocardial perfusion.
2. Trans myocardial LASER revascularization.
a. Transmyocardial laserrevascularization (to increaseintramyocardial channels of bloodflow), and the currentlyexperimental approaches of geneand stem cell therapies are understudy.(Ref. Hari. 18 ed., pg -1526)
Note: About Trans myocardial LASER revascularization,it is mentioned in 17 edition but it is not there in 18edition !!!)Newer Antianginal Drugs
1. Metabolic modulators, eg, trimetazidine,ranolazine
2. Direct bradycardic agents, eg, ivabradine
3. Potassium channel activators, eg, nicorandil
4. Rho-kinase inhibitors, eg, fasudil
5. Protein kinase G facilitators, eg, detanonoate
6. Sulfonylureas, eg, glibenclamide (This helps inmyocardial ischemic preconditioning)
Recent Advances: Ischemic preconditioning(IPC)
th
th th
-
1. In the heart, IPC is an intrinsic processwhereby repeated short episodes of ischaemiaprotect the myocardium against a subsequentischaemic insult.
2. If the blood supply to anorganor a tissue isimpaired for a short time (usually less thanfive minutes) then restored so that blood flowis resumed, and the process repeated two ormore times, the cells downstream of thetissue or organ are robustly protected from afinal ischemicinsult when the blood supply iscut off entirely and permanently.
3. The protective effect which is imparted by IPChas two windows of protection. The first, lastsbetween 46 hoursand has been namedclassical or early preconditioning. The secondwindow begins at 24 hours lasting up to 72hours post the ischaemia and reperfusionstimulus.
Trimetazidine
1. The metabolic modulators are known as pFOXinhibitors because they partially inhibit thefatty acid oxidation pathway in myocardium.
2. Because metabolism shifts to oxidation offatty acids in ischemic myocardium, theoxygen requirement per unit of ATP producedincreases.
3. Partial inhibition of the enzyme required forfatty acid oxidation (long-chain 3-ketoacylthiolase, LC-3KAT) appears to improve themetabolic status of ischemic tissue.
Ranolazine
1. The primary mechanism of therapeutic action
-
of ranolazine involves reduced contractility.
2. This action results from blockade of a latesodium current that facilitates calcium entryvia the sodium-calcium exchanger.
3. Ranolazine is approved for use in angina in theUSA.
Ivabradine,
1. It is called as bradycardic drugs, relativelyselective I sodium channel blockers, reducecardiac rate by inhibiting thehyperpolarization-activated sodium channel inthe sinoatrial node.
2. No other significant hemodynamic effectsoccurs.
3. Ivabradine appears to reduce anginal attackswith an efficacy similar to that of calciumchannel blockers and beta blockers.
4. The lack of effect on gastrointestinal andbronchial smooth muscle is an advantage ofivabradine.
5. Ivabradine acts by reducing the heart ratein amechanism different from beta blockersandcalcium channel blockers, two commonlyprescribed antianginaldrugs.
6. It is classified as a cardiotonic agent
Adverse effectsLuminous Phenomena(by patients described assensations of enhanced brightness in a fully maintainedvisual field).Fasudil Hydrochloride
It is a potentRho-kinaseinhibitor and vasodilator.
f
-
It is used for the treatment ofcerebral vasospasm,which is often due tosubarachnoid hemorrhage,as wellas to improve the cognitive decline seen instrokevictims. It is effective for the treatmentofpulmonary hypertension.It is used to enhancememoryand improve theprognosis ofAlzheimerspatientsNicorandil
1. It has vasodilating properties in normalcoronary arteries.
2. It reduces both preload and afterload.
3. It also provides some myocardial protectionvia preconditioning by activation of cardiacK channels.
4. It significant reduction in relative risk of fataland nonfatal coronary events in patientsreceiving the drug.
RV infarct
Features:
1. Usually associated with inferior wall MI
2. JVP is raised
3. Kussmaul sign is positive
a. Catheterization of the right side of theheart often reveals a distinctivehemodynamic pattern resemblingconstrictive pericarditis (steep rightatrial "y" descent and an early diastolicdip and plateau in RVwaveforms)(Ref. Hari. 18 ed., pg -2032)
b. Patient may or may not havehypotension
ATP
Q
Q
th
Q
-
c. Right ventricular failure(RVF)/infarction: Presents with lowcardiac out and JVP raised. Do aSwan-Ganz catheter to measure right -sided pressures a guide fluidreplacement
d. Give IV fluid for hypotension
Unstable angina: Manage along standard lines butthrombolysis is not done.Important Points:- CABG
Indications for CABG (to improve survival)
1. Left mainstem disease
2. Triple vessel disease involving proximal partof the left anterior descending.
To relieve symptoms
1. Angina unresponsive to drugs
2. Unstable angina (sometimes)
3. If angioplasty is unsuccessful
NB: When CABG and PTCA are both clinically validoptions, PTCA is preferred.
1. Artery used for by pass graft
a. Internal mammary artery
b. Radial artery
2. Vein used for by pass graft
a. Long saphenous vein
b. Mortality 50% of deaths occurwithin 24h of onset of symptom.(MCQ)
Q
Q
-
Complications of MI
1. Bradycardia or heart block:
a. Sinus bradycardia: treat with atropine 0.6 -1.2mg, or injection isoprenaline
Consider temporary cardiac pacing if noresponse, or poorly tolerated by thepatient.
b. 1 degree AV block: Observe closely asapproximately 40% develop higherdegrees of AV block.
c. 2 degree (II A block) Wenckebach(Mobitz type I) block: Does not requirepacing .
d. 2 degree (II B block) Mobitz type IIblock: Carries a high risk of developingcomplete AV block; should be paced .
e. Complete AV block: insert pacemaker
f. Bundle branch block: MI complicated bytrifascicular block or non-adjacentbifascicular disease should be paced.
2. Tachyarrhythmias:
a. K+, hypoxia and acidosis all predisposeto arrhythmias and should be corrected.
b. Regular broad complex tachycardia afterMI is almost always VT.
c. If hemodynamically stable, treat withantidysrhythmic.
d. Early VT: give lidocaine by infusion for12-24h or amiodarone.
e. Late VT (>24h) amiodarone and start oraltherapy (amiodarone or sotalol)
Q
st
nd
Q
nd
Q
Q
-
f. If hemodynamically compromised giveDC shock.
g. Af or flutter If hemodynamicallycompromised, DC cardioversionOtherwise control rate with digoxin orbeta -blocker.
h. In atrial flutter or intermittent Af, giveamiodarone or sotalol.
In MI, Bradycardia is most common in inferior wall MI.(LQ 2012) & Tachyarrhythmias are most common inanterior wall MI. (LQ 2012)Important Points:
Dofetilide: It is a pure K+ channel blocker, used formaintenance of sinus rhythm in symptomatic atrialflutter and fibrillation. It increase the refractory periodof both atria and ventricles.
3. Left ventricular failure (LVF)
Killips classification (for assessing theprognosis of a case of MI. It is based on degreeof LV dysfunction)
(Note: With the recent advancement in treatmentof MI, the above mentioned mortality percentageis much reduced now)
4. Cardiogenic shock By definition
a. Systolic arterial pressure < 90 mmHg
b. Cardiac index < 1.8 L/min/m
c. Pulm capillary wedge pressure >18 mm
2
-
Hg
Treatment
d. Vasopressor Dopamine, Dobutamine,Amrinone Milrinone
e. Intra aortic balloon pumping (IABP)
f. PTCA (It is the treatment of choice) MCQ(AIPG 12)
5. Right ventricular / infarction: Presents withlow cardiac out and JVP raised (LQ 2012). Doa Swan-Ganz catheter to measure right -sidedpressures a guide fluid replacement (LQ2012)
6. Pericarditis: Central chest pain, relieved bysitting forwards. ECG: saddle-shaped STelevation
7. DVT & PE: Patients are at risk of developingDVT & PE and should be prophylacticallyheparinized (enoxaparin) until fully mobile.
8. Systemic embolism: May arise from a LVmural thrombus. After large anterior MI,consider anticoagulation with warfarin for 3months.
9. Mitral regurgitation: Occurs due to papillarymuscle dysfunction
10. Ventricular septal defect: Presents withpansystolic murmur , JVP raised , cardiacfailure .
Diagnosis: Echo.
Treatment: Surgery.
Q
Q
Treatment-: NSAIDS. Echo to check foreffusion.
Q
Q
Q
Q Q
Q
-
Comment
11. Free wall rupture with in first week
a. Usually seen in first infarction, HT, noh/o angina and large wave infarct.
b. Presents with sudden loss of pulse,blood pressure & loss ofconsciousness. Electro mechanicaldissociation occurs . Electricalalternans is seen.
c. Cardiac tamponade result
12. Late malignant ventricular arrhythmias: Occur1-3wks post-MI. Avoid hypokaliemia the mosteasily avoidable cause. Consider 24h ECGmonitoring prior to discharge if large MI.
13. Dressler's syndrome: Recurrent pericarditis,pleural effusions, fever, pain chest , anaemiaand raised ESR 2-3 months post-MI.
Treatment: NSAIDS; steroids if severe.
14. Left ventricular aneurysm: This occurs late (4-6wks post-MI), and presents with LVF, angina.recurrent VT or systemic embolism.
ECG: Persistent ST segment elevation .
15. Shoulder hand syndrome = Pain In theshoulder joints occur after 2-3 months.
5IJTDPVSTFJTQPXFSFECZ
Q
Q
Q
Q
Q
Q
0Like Share
Previous Atherosclerosis< Next
Cardiomyopathy>
-
FullName
Email
Password
ContactNumber
"DDPVOU"MSFBEZ&YJTU F
-PHJO)FSFXFCMPHJO
'BDFCPPL$POOFDU
$SFBUF"DDPVOU
NBJMVTBUFFDPOUBDU!HSBEFTUBDLDPNNBJMUPDPOUBDU!HSBEFTUBDLDPN
"CPVU6TNBJOTJUFBCPVUVT
/FXTNBJOTJUFOFXT
#MPHCMPH
$POUBDU6TNBJOTJUFDPOUBDU
5FSNTBOE$POEJUJPOTNBJOTJUFQPMJDZ
%FWFMPQFSTNBJOTJUFEFWFMPQFS
1VCMJTIFSTNBJOTJUFQVCMJTIFS
1MFBTF 3FHJTUFS
G
PS