Corel Ventura - KORCEK · thickness of the mucosa thin to avoid rectal wall injury. The incision...
Transcript of Corel Ventura - KORCEK · thickness of the mucosa thin to avoid rectal wall injury. The incision...

Authors operated on their Surgical departement67 years old women with incomplete evacuation,and digital support during defecation, giant recto-cele and massive vaginal vault prolaps. Authorsrealized cinedefecography and detected giant rec-tocele, depth was 8 cm, anorectal angle was 120degrees. They stated Resting pressure 40 cm H2O,
and Maximum squeeze pressure 50cm H2O by anorec-tal manometry. Authors verified external anal sphinc-ters defect by endoanal ultrasound and determinedPudendal nerve terminal motor latency (PN TML)and recorded pathologic values of n.pudendal latency (left branch 2,7 msec., right branch 4,3 msec). In con-cerning massive vaginal vault prolaps, huge rerecto-cele and clinical incompletely evacuation with self digi-tal support during defecation with present defect odexternal anal sphincters and pathologic values of PNTML, authors indicated and made combined trans-vaginal, endorectal and perineal reconstructive opera-tive performance.In the present time two years after the surgery radi-ologic mean depth of the rectocele was significantly re-duced (preoperatively 8cm; postoperatively 1 cm).Anorectal angle is 100 degrees. Values of the PN TMLis normaly (left branch of n. pudendalis 1,7 msec andright branch of n. pudendalis 1,9 msec). Authors re-corded Resting pressure 60 cm H2O and Maximumsqueeze pressure 110 cm H2O by anorectal mano-metry. They didnt visualized any external anal sphinc-ters defect by anal ultrasound. Postoperatively difficult evacuation completely disap-peared and digital support was no longer necessaryduring evacuation.
Key words: rectocela, parasacral, vaginal, endorectal
INTRODUCTION
Rectocele is defined as an abnormal bulging of the an-terior rectal wall into the vagina, which is occasion-
ally diagnosed in middle-aged or elderly females whocomplain of chronic constipation2,9,28. It is sometimes
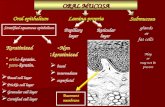
encountered incidentally at the time of vaginal or rectalexaminations. Rectocele treatment is designed to reducespecific symptoms, such as difficult evacuation, incom-plete evacuation, and digital support during defecation. Alumpy vaginal protrusion, vaginal bulging, and pelvicheaviness also are important symptoms that indicate theneed for treatment29. Conservative management, includingbiofeedback training, can be helpful for patients with mildsymptoms20 . If conservative management fails to relievethe symptoms, surgical treatment is advocated.What con-stitutes the optimal procedure has been discussed foryears among colorectal surgeons and urogynecologists.Alarge variety of surgical techniques are available for thetreatment of rectocele, including transvaginal, transper-ineal, endorectal, transabdominal, and combined appro-aches1,5,24. In addition to the surgical technique itself, innumerous studies the question of using synthetic materialfor the repair of pelvic organ prolapses is addressed3,14.Endorectal rectocele repair has been performed by col-orectal surgeons. However, the results of endorectal repairhave been reported with varying success. In addition,some authors have suggested that the endorectal approachmight deteriorate anal sphincter function8,17,23.Transvagi-nal rectocele repair has been used mainly by gynecolo-gists as a posterior colporrhaphy. This consists of theplication of the levator muscles or the plication of the rec-tovaginal fascia. Although clinical results after transvagi-nal rectocele repair have been widely reported, thephysiologic influences after transvaginal rectocele repairhave not been fully investigated10,18, 19, 20.
. ........................................
Combined parasacral, vaginal and endorectalapproach in surgical treatment of giant rectocele
J. Korcek1, E. Bakos1, A.Farkas2
1Surgical Clinic, Section of Colorectal Surgery FacultyHospital Nitra Slovak republic 2EMG laboratory, Medical center Nitra, Slovak republic
/PRIKAZ SLU^AJA 6161.351-007.43-089.844
rezi
me

CASE REPORT
On our Surgical clinic we examined 67 years oldwomen with incomplete evacuation, and digital supportduring defecation, giant rectocele and massive vaginalvault prolaps. We are realized cinedefecography and de-tected giant rectocele depth 8 cm, anorectal angle was120 degrees. Dynamic magnetic resonance imaging defe-cography we have not ability carry out. We are statedResting pressure 40 cm H2O, and Maximum squeezepressure 50cm H2O by anorectal manometry. We verifiedexternal anal sphincter defect by endoanal ultrasound anddetermined Pudendal nerve terminal motor latency (PNTML) and recorded pathologic values of n.pudendal la-tency (left branch 2,7 msec., right branch 4,3 msec). In
concerning massive vaginal vault prolaps, huge rerecto-cele and clinical incompletely evacuation with self digitalsupport during defecation with present defect of externalanal sphincters and pathologic values of PN TML, we in-dicated and made combined transvaginal, endorectal andperineal reconstructive operative performance.
OPERATIVE TECHNIQUE
One day before surgery was administred ortograde lav-age with A.B. Taylor solution.In the morning on the dayof surgery enema was administered. A systemic antibioticwas given immediately before the operation commenced.The operation was performed in two position. At he firstin the dorsal lithotomy position under spinal anesthesia.
PICTURE 1: PATIENT IN THE DORSAL LITHOTOMY POSITIONUNDER SPINAL ANESTHESIA. BOTH SIDES OF THELABIA MAIORA WERE SUTURED LATERALLY FORBETTER EXPOSURE
PICTURE 2: THE VAGINAL MUCOSA WAS THEN FREED FROMTHE UNDERLYING RECTAL WALL WITH A SHARPDISSECTION BY USING SCISSORS
PICTURE 3:A ADEQUATE AMOUNT OF THE MUCOSA WAS EX-CISED IF THE MUCOSA SEEMED EXCESSIVE FORTHE RECONSTRUCTION OF THE POSTERIOR WALLOF THE VAGINA
PICTURE 4 : THE MOST PROXIMAL LEVEL OF THE SUTURE WASDETERMINED BY CHECKING THE SIZE OF THE IN-TROITUS, USUALLY AT LEAST TWO FINGERS WIDE
44 J. Korcek et al ACI Vol. LIII

Both sides of the labia maior were sutured laterally forbetter exposure (pct. 1). The posterior vaginal mucosawas infiltrated with an epinephrine solution to minimizebleeding during dissection. A U-shaped incision wasmade in the posterior wall of the vagina along the lowerone-half of the vaginal introitus. The vaginal mucosa wasthen freed from the underlying rectal wall with a sharpdissection by using scissors (pct. 2).
During dissection, care was constantly taken to keep thethickness of the mucosa thin to avoid rectal wall injury.
The incision was extended upward to the level of theproximal border of the rectocele. Then, dissection wasperformed laterally to create the lateral space of the rec-tum until the puborectalis portions of the levator ani werereached. After the entire area of the rectocele was freedfrom the posterior vaginal mucosa, both sides of the mus-culofascial component (puborectalis portions) were gras-ped with Allis clamps, and approximated with intermittentnonabsorbable sutures (00-Prolene, Ethicon Inc.). Themost proximal level of the suture was determined by che-cking the size of the introitus, usually at least two fingerswide (pct. 4).
A adequate amount of the mucosa was sometimes ex-cised if the mucosa seemed excessive for the reconstruc-tion of the posterior wall of the vagina (pct. 3).
PICTURE 5: THE MIDLINE OF THE VAGINAL MUCOSA WAS AP-PROXIMATED WITH INTERMITTENT DELAYED AB-SORBABLE SUTURES AND BOTH SIDES OF THELATERAL BORDER WERE SUTURED WITH INTER-MITTENT DELAYED ABSORBABLE SUTURES
PICTURE 6: LEVATOR PLASTY ANTERIOR CAN BE EASILY PER-FORMED USING THE SPECIAL PERINEAL PERATIVEAPPROACH OPERATIVE FIELD AFTER THE LEVA-TOR PLASTY ANTERIOR
PICTURE 7 : PATIENT IN JACK-KNIFE POSITION. LEFT PARASAC-RAL APPROACH – SKIN INCISION
PICTURE 8 : RELEASING POSTERIOR – AIMED TO ACHIEVEA CORRECTION OF THE ANORECTAL ANGLE
Br. 2 Combined parasacral, vaginal and endorectal approach in 45surgical treatment of giant rectocele

In that case, care was taken not to remove too much mu-cosa to avoid postoperative constriction. The midline ofthe vaginal mucosa was approximated with intermittentdelayed absorbable sutures (0-Coated Vicryl, EthiconInc.) and both sides of the lateral border were sutured withintermittent delayed absorbable sutures (000-Coated Vi-cryl, Ethicon Inc.) (pct. 5). No drain was placed inside andone piece of gauze was packed. After that we lead socalled "smile incision", semicircular cut along the rear pe-rimeter of the perineum followed by the proximal inter-sphincteric preparation, and made Levator plasty anteriorcan be easily performed using this special perineal opera-tive approach (pct. 6).
We changed position of the patient in Jack-knife posi-tion and made endorectal repair of rectocele (pct. 10).Anal mucosa is incised transversely 1 cm above the den-tate line and disected from the internal anal sphincter and
the rectal circular muscle to a height of 10 cm (pct. 11).We sutured rectal mucosal layer is concertinaed together(3-0 Vicryl Ethicon Inc.) (pct. 12). In addition we lead leftparasacral skin incision (pct. 7) and made "releasing pos-terior" (pct. 8), reefing of the m. puborectalis (pct. 9) andoverlap plasty "scar over scar". We inserted one silikonedrain under the suture (pct. 13,14). In order to preventtromboembolic complications, the patient was given lowmolecular Heparin. The patient was given intravenous so-lutions without amino acids and fats until the fourth dayand then fed orally.
RESULT
PICTURE 9 : OPERATIVE FIELD AFTER THE PLICATION OF THEMUSCLE PUBORECTALIS. OPERATIVE FIELD BE-FORE THE OVERLAP PLASTY
PICTURE 10 : GIANT RECTOCELE
PICTURE 11ANAL MUCOSA IS INCISED TRANSVERSELY L CMABOVE THE DENTATE LINE AND DISECTED FROMTHE INTERNAL ANAL SPHINCTER AND THE REC-TAL CIRCULAR MUSCLE TO A HEIGHT OF 10 CM
PICTURE 12SUTURED RECTAL MUCOSAL LAYER IS CONCERTI-NAED TOGETHER WITH INTERMITTENT DELAYEDABSORBABLE SUTURES
46 J. Korcek et al ACI Vol. LIII

There was no intraoperative rectal wall injury. No earlypostoperative complications, such as bleeding, hematoma,or wound infections were observed. The patient under-went a clinical examination, anal manometry, cinedefe-cography, PN TML and anal ultrasound at 3 and 6 monthsand 1 and 2 years after surgery. In the present time twoyears after the surgery Continence grading scale score is 4points. Radiologic mean depth of the rectocele was sig-nificantly reduced (preoperatively 8cm, postoperatively 1cm). Anorectal angle is 100 degrees. Values of the PNTML is normaly (left branch of n. pudendalis 1,7 msecand right branch of n. pudendalis 1,9 msec). We recordedResting pressure 60 cm H2O and Maximum squeezepressure 110 cm H2O by anorectal manometry.We didntvisualized any external anal sphincters defect by anal ul-trasound. Postoperatively difficult evacuation completelydisappeared and digital support was no longer necessaryduring evacuation.
DISCUSION
Rectocele refers to displacement of the anterior rectalwall and the posterior vaginal wall into the vagina. Thepathogenesis of rectocele is not well known. It seems tobe considered that defects or tissue weakness in the rec-tovaginal septum are initially caused by vaginal delivery,and then aggravated by repetitive increase of intrarectalpressure. Neurodegenerative disorders and connective tis-sue diseases also might be of importance for the etiologicfactors, which might be the cause of rectocele in nulli-parous women. Rectocele often coexists with other pelvicorgan prolapses, such as cystocele, vaginal vault prolapse,and enterocele2,9,10,11,25. Generally, 3 cm is defined as ab-normal bulging and considered to be an indication for sur-gical repair if it is symptomatic. Some authors advocatethat barium trapping on defecographic findings also is agood indicator1,20,22. The clinical implication of a coexis-tent finding of rectal intussusception or enterocele is notclear. Another aspect of coexistent problems concerningrectocele repair is paradoxic sphincter reaction or anismusThe role of this finding is debatable but one should bear inmind that some authors report that paradoxic sphincter re-action or anismus might be a cause of poor functional out-come13,19.
What constitutes the optimal surgical approach has beendebated for years. Endorectal rectocele repair was first re-ported by Sullivan et al. in 1968, and other surgeons fol-lowed or modified his procedure. However, endorectalrectocele repair has not always been successful. Trans-vaginal repair, known as posterior colporrhaphy, is rein-forcement of the rectovaginal septum by the approxima-tion of levator muscles (levatorplasty). This procedure hastraditionally been performed by gynecologists. However,the possibility of dyspareunia is a well-known drawbackof transvaginal repair. Incidences of dyspareunia havebeen variously reported at approximately 20 percent. Al-though many authors do not recommend this procedurefor patients of childbearing age or sexually active women,they believe that transvaginal repair should not be avoidedsimply because it causes dyspareunia. The physiologic in-fluence after rectocele repair is not well understood. Moststudies do not investigate with anorectal physiologic tests.The endorectal approach usually needs an anal dilator foradequate rectal exposure during an operation, which couldcause sphincter damage. Regarding rectal threshold andmaximum tolerable volume, endorectal repair is morelikely to decrease postoperatively. No significant changeshave been reported in rectal compliance after endorectalor transvaginal repair10,18,21,24,26,29. The transvaginal ap-proach should be considered if the patient’s anal sphincterfunction is previously weakened. Recent publications de-scribing new techniques using collagen mesh or a staplingdevice have received great attention from colorectal sur-geons. I believe that the transvaginal repair bio implantsseems to have more long-term effectiveness comparedwith biomaterial implants3,4. Stapled transanal rectal re-section (S.T.A.R.R.) became one of the recommendedprocedures for obstructed defecation syndrome over thelast few years. The procedure, introduced by Longo, is
PICTURE 13OPERATIVE FIELD AFTER SUTURE OF THE OPERA-TIONAL APPROACHES
PICTURE 14OPERATIVE FIELD 3 WEEKS AFTER SURGERY
Br. 2 Combined parasacral, vaginal and endorectal approach in 47surgical treatment of giant rectocele

characterized by endorectal performed full-thickness rec-tal wall resection. The S.T.A.R.R. procedure is based onthe idea that removal of defunct parts of the rectal wallwill improve obstructed defecation. The technique pro-vides the opportunity to perform endorectal rectocele re-moval without the risks of transabdominal procedures.This novel technique seems to be safe and effective in thetreatment of outlet obstruction caused by the combinationof intussusception and rectocele5,6,7,14. Randomized trialsare required to confirm these findings.
CONCLUSION
In the case if old multiparous women have massivevaginal vault prolaps, huge rerectocele and clinical incom-pletely evacuation with self digital support during defeca-tion and present defect of external anal sphincters andpathologic values of PN TML, combined one stage trans-vaginal, endorectal and perineal reconstructive operativeperformance is reasonable surgical modality with excelentresult.
SUMMARY
KOMBINOVNI PARASAKRALNI, VAGINALNI IENDOREKTALNI PRISTUP U HIRUR[KOMZBRINJAVANJU TRETMANU GIGANTSKEREKTOKELE
Autori su na hirur{kom odeljenju operisali ‘enu staru 67godina sa tegobama u vidu nekompletne evakuacije i digi-talnim pomaganjem u toku defekacije, sa verifikovanomgigantskom rektocelom i masivnim prolapsom vagine.Sprovedena je defekografija i otkrivena gigantska rekto-cela dubine 8 cm, sa anorektalnim uglom od 120 stepeni.Analnom manometrijom konstatovan pritisak u miru od40 cm vodenog stuba a pri voljno kontrakciji od 50 cmvodenog stuba. Endorektalnim ulrazvukom verifikovandefekt kontinuiteta analnih sfinktera, i latencu puden-danog motornog nerva (PN TML) i zabele‘ene su pa-tolo{ke vrednosti (leva grana 2,7 msec, desna grana 4,3msec). Uzimaju}i u obzir navedeno, indikovana je kombi-novana transvaginalna, endorektalna, transperinealna pro-cedura.
Na kontrolnom pregledu, dve godine posle operacije,rektocela je redukovana sa sada{njom dubinom od 1 cm,anorektalnim uglom od 100 stepeni. Vrednosti PN TML(leva grana 1,7 msec, desna grana 1,9 msec). Manometri-jski, pritisak u miru 60 cm vodenog stuba, a pri voljnojkontrakciji 110 cm. Na endorektalnom ultrazvuku nijevidjen prekid kontinuiteta sfinktera, sa rezolucijomnavedenih tegoba.
Klju~ne re~i: rektocela, parasakralno, vagina,endorektalno
REFERENCES
1. Abramov, Y, Gandhi, S, Goldberg, RP, Botros, SM,Kwon, C, Sand, PK (2005): Site-specific rectocele repaircompared with standard posterior colporrhaphy ObstetGynecol 105: 314-318
2. Aigner F, Zbar A, Ludwikowski B (2004): The recto-genital septum. Dis Colon Rectum 47:131–140
3. Altman, D, Mellgren, A, Blomgren, B et al (2004):Clinical and histological safety assessment of rectocele re-pair using collagen mesh Acta Obstet Gynecol Scand 83:995- 1000
4. Altman, D, Zetterstrom, J, Lopez, A et al. (2005):Functional and anatomic outcome after transvaginal recto-cele repair using collagen mesh: a prospective study DisColon Rectum 48: 1233-41
5. Altomare, DF, Rinaldi, M, Veglia, A, Petrolino, M,Fazio, M, Sallustio,P. (2002): Combined perineal and en-dorectal repair of rectocele by circular stapler: a novelsurgical technique Dis Colon Rectum 45: 1549-1552
6. Boccasanta, P, Venturi, M, Salamina, G et al.(2004): New trends in the surgical treatment of outlet ob-struction: clinical and functional results of two novel tran-sanal stapled techniques from a randomised controlledtrial Int J Colorectal Dis 19: 359-369
7. Boccasanta, P, Venturi, M, Stuto, A et al. (2004):Stapled transanal rectal resection for outlet obstruction: aprospective, multicenter trial" Dis Colon Rectum 47:1285-1296
8. Capps, WF, Jr (1975): Rectoplasty and perineoplastyfor the symptomatic rectocele: a report of fifty cases DisColon Rectum 18: 237-243
9. D’Hoore, A, Penninckx, F (2003) :Obstructed defeca-tion Colorectal Dis 5: 280-287
10. Cundiff, GW, Fenner, D (2004): Evaluation andtreatment of women with rectocele: focus on associateddefecatory and sexual dysfunction Obstet Gynecol104:1403-21
11. Dam, JH, Huisman, WM, Hop, WC, Schouten, WR(2000): Fecal continence after rectocele repair: a prospec-tive study Int J Colorectal Dis 15: 54-57
12. Fritsch H, Lienemann A, Brenner E, NudwikowskiB (2004): Clinical anatomy of the pelvic floor Adv AnatEmbryol Cell Biology 175
13. Heriot, AG, Skull, A, Kumar, D (2004): Functionaland physiological outcome following transanal repair ofrectocele Br J Surg 91: 1340-1344
14. Hyman H (2004) Whats new in colon and rectal sur-gery J Am Coll Surg 199: 917–922
15. Kenton, K, Shott, S, Brubaker, L (1999): Theanatomic and functional variability of rectoceles inwomen Int Urogynecol J Pelvic Floor Dysfunct 10: 96-99
16. Longo A: Obstructed defecation because of rectalpathologies. Novel surgical treatment: stapled transanalrectal resection (STARR). In Acts of 14th InternationalColorectal Disease Symposium, Fort Lauderdale, FL,2003
17. Lopez, A, Anzen, B, Bremmer, S et al. (2001): Du-rability of success after rectocele repair Int Urogynecol JPelvic Floor Dysfunct 12: 97-103
18. Maeda, K, Maruta, M, Hanai, T et al. (2003):Transvaginal anterior levatorplasty with posterior colpor-rhaphy for symptomatic rectocele Tech Coloproctol 7:181-185
48 J. Korcek et al ACI Vol. LIII

19. Maglinte D, Kelvin M, Fitzgerald K (1999): Asso-ciation of compartment defect in pelvic floor dysfunctionAm J Rad 172: 439–444
20. Maher C, Baessler K, Glazener CM, Adams EJ,Hagen S.: Surgical management of pelvic organ prolapsein women. Cochrane Database Syst Rev 2004;CD004014.
21. Maher, CF, Qatawneh, AM, Baessler, K, Schluter,PJ:Midline rectovaginal fascial plication for repair of rec-tocele and obstructed defecation Obstet Gynecol2004;104: 685-689
22. Mellgren, A, Bremmer, S, Johansson, C et al.: De-fecography. Results of investigations in 2,816 patients DisColon Rectum 1994;37:1133-1141
23. Miklos, JR, Kohli, N, Lucente, V, Saye,WB: Site-specific fascial defects in the diagnosis and surgical man-agement of enterocele Am J Obstet Gynecol 1998; 179:1418-1422
24. Nieminen, K, Hiltunen, KM, Laitinen, J, Oksala, J,Heinonen, PK: Transanal or vaginal approach to rectocelerepair: a prospective, randomized pilot study Dis ColonRectum 2004;47: 1636-1642
25. Rentsch, M, Paetzel, C, Lenhart, M et al.: Dynamicmagnetic resonance imaging defecography: a diagnosticalternative in the assessment of pelvic floor disorders inproctology Dis Colon Rectum 2001;44: 999-1007
26. Sullivan, ES, Leaverton, GH, Hardwick, CE:Transrectal perineal repair: an adjunct to improved func-tion afteranorectal surgery Dis Colon Rectum 1968;11:106-114
27. Von Hayek H: Das Bindegewebe und die glatteMuskulatur des Beckenbodens In: Dix A, Wildbolz G(eds) Handbuch der Urologie. Springer,Berlin Heidelberg,S 1969;289–313
28.Yoshioka, K, Matsui, Y, Yamada, O et al.: Physi-ologic and anatomic assessment of patients with rectoceleDis Colon Rectum 1991;34:704-708
29. Zbar, AP, Lienemann, A, Fritsch, H, Beer-Gabel,M, Pescatori, M: Rectocele: pathogenesis and surgicalmanagement Int J Colorectal Dis 2003;18: 369-384
Br. 2 Combined parasacral, vaginal and endorectal approach in 49surgical treatment of giant rectocele