COPD ppt
-
Upload
monique-reyes -
Category
Documents
-
view
320 -
download
15
description
Transcript of COPD ppt

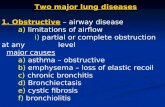
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
COPD is a lung disease characterized by chronic obstruction of lung airflow that interferes with normal breathing and is not fully reversible ndash WHO
it is one of most common diseases also known as chronic obstructive lung disease
Etiology and risk factors
Smoking is the primary risk factor for COPD The numerous irritants found in cigarette smoke stimulate excess mucus production and coughing destroy ciliary function and lead to inflammation and damage of bronchiolar and alveolar walls
Other Risk Factors
- air pollution
- second-hand smoke
- Hx Of childhood respiratory tract infection
- heredity
THERE ARE FOUR MAIN FORMS OF COPD
Asthma Bronchitis Emphysema Bronchiectasis
ASTHMA
Is a disorder of the bronchial airways characterizes by periods or reversible bronchospasm
Is often called reactive airway disease
Is a obstruction of the bronchioles characterized by attacks that occur suddenly and last from 30 to 60 minutes an attack that is difficult to control is referred to ldquo status asthmaticus ldquo
a disorder that causes the airways of the lungs to swell and narrow leading to wheezing shortness of breath chest tightness and coughing
Status Asthmaticus
is a severe life-threatening complication of asthma It is an acute episode of bronchospasm that leads to intensify With severe bronchospasm the workload of breathing increases 5 to 10 times which can lead to acute cor pulmonale ( right-sided heart failure resulting from lung disease)
STATUS ASTHMATICUS
bull pneumothorax commonly develops
If continues hypoxemia will be worsen acidosis begins if untreated not reversed respiratory or cardiac arrest ensues
ETIOLOGY AND RISK FACTORS
ASTHMA OCCURS IN FAMILIES WHICH SUGGESTS THAT IT IS AN INHERITED DISORDER
Environmental factors
ex viral infection allergens pollutants
Itching factors can excitatory states
ex stress laughing crying
Exercise Changes in temperature Strong odor
Asthma also is a component of triad disease
bull asthmabull nasal polypsbull allergy to aspirin
SUBSTANCES THAT TRIGGER ASTHMA
Type of Substance Examples
Air pollutants including dusts smoke mists amp fumes
Diesel exhaust tobacco smoke mineral rock coal amp wood dusts gases fumes amp vapors from aerosol agents chemicals cleaning materials solvents paints welding amp from heating amp cooling metals quickly
Pollens mites amp molds Trees flowers weeds hay plants
Animal dander Birds cats dogs
Medications Aspirin anti-inflammatory drugs
Foods Egg wheat nuts
SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

COPD is a lung disease characterized by chronic obstruction of lung airflow that interferes with normal breathing and is not fully reversible ndash WHO
it is one of most common diseases also known as chronic obstructive lung disease
Etiology and risk factors
Smoking is the primary risk factor for COPD The numerous irritants found in cigarette smoke stimulate excess mucus production and coughing destroy ciliary function and lead to inflammation and damage of bronchiolar and alveolar walls
Other Risk Factors
- air pollution
- second-hand smoke
- Hx Of childhood respiratory tract infection
- heredity
THERE ARE FOUR MAIN FORMS OF COPD
Asthma Bronchitis Emphysema Bronchiectasis
ASTHMA
Is a disorder of the bronchial airways characterizes by periods or reversible bronchospasm
Is often called reactive airway disease
Is a obstruction of the bronchioles characterized by attacks that occur suddenly and last from 30 to 60 minutes an attack that is difficult to control is referred to ldquo status asthmaticus ldquo
a disorder that causes the airways of the lungs to swell and narrow leading to wheezing shortness of breath chest tightness and coughing
Status Asthmaticus
is a severe life-threatening complication of asthma It is an acute episode of bronchospasm that leads to intensify With severe bronchospasm the workload of breathing increases 5 to 10 times which can lead to acute cor pulmonale ( right-sided heart failure resulting from lung disease)
STATUS ASTHMATICUS
bull pneumothorax commonly develops
If continues hypoxemia will be worsen acidosis begins if untreated not reversed respiratory or cardiac arrest ensues
ETIOLOGY AND RISK FACTORS
ASTHMA OCCURS IN FAMILIES WHICH SUGGESTS THAT IT IS AN INHERITED DISORDER
Environmental factors
ex viral infection allergens pollutants
Itching factors can excitatory states
ex stress laughing crying
Exercise Changes in temperature Strong odor
Asthma also is a component of triad disease
bull asthmabull nasal polypsbull allergy to aspirin
SUBSTANCES THAT TRIGGER ASTHMA
Type of Substance Examples
Air pollutants including dusts smoke mists amp fumes
Diesel exhaust tobacco smoke mineral rock coal amp wood dusts gases fumes amp vapors from aerosol agents chemicals cleaning materials solvents paints welding amp from heating amp cooling metals quickly
Pollens mites amp molds Trees flowers weeds hay plants
Animal dander Birds cats dogs
Medications Aspirin anti-inflammatory drugs
Foods Egg wheat nuts
SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

Etiology and risk factors
Smoking is the primary risk factor for COPD The numerous irritants found in cigarette smoke stimulate excess mucus production and coughing destroy ciliary function and lead to inflammation and damage of bronchiolar and alveolar walls
Other Risk Factors
- air pollution
- second-hand smoke
- Hx Of childhood respiratory tract infection
- heredity
THERE ARE FOUR MAIN FORMS OF COPD
Asthma Bronchitis Emphysema Bronchiectasis
ASTHMA
Is a disorder of the bronchial airways characterizes by periods or reversible bronchospasm
Is often called reactive airway disease
Is a obstruction of the bronchioles characterized by attacks that occur suddenly and last from 30 to 60 minutes an attack that is difficult to control is referred to ldquo status asthmaticus ldquo
a disorder that causes the airways of the lungs to swell and narrow leading to wheezing shortness of breath chest tightness and coughing
Status Asthmaticus
is a severe life-threatening complication of asthma It is an acute episode of bronchospasm that leads to intensify With severe bronchospasm the workload of breathing increases 5 to 10 times which can lead to acute cor pulmonale ( right-sided heart failure resulting from lung disease)
STATUS ASTHMATICUS
bull pneumothorax commonly develops
If continues hypoxemia will be worsen acidosis begins if untreated not reversed respiratory or cardiac arrest ensues
ETIOLOGY AND RISK FACTORS
ASTHMA OCCURS IN FAMILIES WHICH SUGGESTS THAT IT IS AN INHERITED DISORDER
Environmental factors
ex viral infection allergens pollutants
Itching factors can excitatory states
ex stress laughing crying
Exercise Changes in temperature Strong odor
Asthma also is a component of triad disease
bull asthmabull nasal polypsbull allergy to aspirin
SUBSTANCES THAT TRIGGER ASTHMA
Type of Substance Examples
Air pollutants including dusts smoke mists amp fumes
Diesel exhaust tobacco smoke mineral rock coal amp wood dusts gases fumes amp vapors from aerosol agents chemicals cleaning materials solvents paints welding amp from heating amp cooling metals quickly
Pollens mites amp molds Trees flowers weeds hay plants
Animal dander Birds cats dogs
Medications Aspirin anti-inflammatory drugs
Foods Egg wheat nuts
SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

Smoking is the primary risk factor for COPD The numerous irritants found in cigarette smoke stimulate excess mucus production and coughing destroy ciliary function and lead to inflammation and damage of bronchiolar and alveolar walls
Other Risk Factors
- air pollution
- second-hand smoke
- Hx Of childhood respiratory tract infection
- heredity
THERE ARE FOUR MAIN FORMS OF COPD
Asthma Bronchitis Emphysema Bronchiectasis
ASTHMA
Is a disorder of the bronchial airways characterizes by periods or reversible bronchospasm
Is often called reactive airway disease
Is a obstruction of the bronchioles characterized by attacks that occur suddenly and last from 30 to 60 minutes an attack that is difficult to control is referred to ldquo status asthmaticus ldquo
a disorder that causes the airways of the lungs to swell and narrow leading to wheezing shortness of breath chest tightness and coughing
Status Asthmaticus
is a severe life-threatening complication of asthma It is an acute episode of bronchospasm that leads to intensify With severe bronchospasm the workload of breathing increases 5 to 10 times which can lead to acute cor pulmonale ( right-sided heart failure resulting from lung disease)
STATUS ASTHMATICUS
bull pneumothorax commonly develops
If continues hypoxemia will be worsen acidosis begins if untreated not reversed respiratory or cardiac arrest ensues
ETIOLOGY AND RISK FACTORS
ASTHMA OCCURS IN FAMILIES WHICH SUGGESTS THAT IT IS AN INHERITED DISORDER
Environmental factors
ex viral infection allergens pollutants
Itching factors can excitatory states
ex stress laughing crying
Exercise Changes in temperature Strong odor
Asthma also is a component of triad disease
bull asthmabull nasal polypsbull allergy to aspirin
SUBSTANCES THAT TRIGGER ASTHMA
Type of Substance Examples
Air pollutants including dusts smoke mists amp fumes
Diesel exhaust tobacco smoke mineral rock coal amp wood dusts gases fumes amp vapors from aerosol agents chemicals cleaning materials solvents paints welding amp from heating amp cooling metals quickly
Pollens mites amp molds Trees flowers weeds hay plants
Animal dander Birds cats dogs
Medications Aspirin anti-inflammatory drugs
Foods Egg wheat nuts
SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

THERE ARE FOUR MAIN FORMS OF COPD
Asthma Bronchitis Emphysema Bronchiectasis
ASTHMA
Is a disorder of the bronchial airways characterizes by periods or reversible bronchospasm
Is often called reactive airway disease
Is a obstruction of the bronchioles characterized by attacks that occur suddenly and last from 30 to 60 minutes an attack that is difficult to control is referred to ldquo status asthmaticus ldquo
a disorder that causes the airways of the lungs to swell and narrow leading to wheezing shortness of breath chest tightness and coughing
Status Asthmaticus
is a severe life-threatening complication of asthma It is an acute episode of bronchospasm that leads to intensify With severe bronchospasm the workload of breathing increases 5 to 10 times which can lead to acute cor pulmonale ( right-sided heart failure resulting from lung disease)
STATUS ASTHMATICUS
bull pneumothorax commonly develops
If continues hypoxemia will be worsen acidosis begins if untreated not reversed respiratory or cardiac arrest ensues
ETIOLOGY AND RISK FACTORS
ASTHMA OCCURS IN FAMILIES WHICH SUGGESTS THAT IT IS AN INHERITED DISORDER
Environmental factors
ex viral infection allergens pollutants
Itching factors can excitatory states
ex stress laughing crying
Exercise Changes in temperature Strong odor
Asthma also is a component of triad disease
bull asthmabull nasal polypsbull allergy to aspirin
SUBSTANCES THAT TRIGGER ASTHMA
Type of Substance Examples
Air pollutants including dusts smoke mists amp fumes
Diesel exhaust tobacco smoke mineral rock coal amp wood dusts gases fumes amp vapors from aerosol agents chemicals cleaning materials solvents paints welding amp from heating amp cooling metals quickly
Pollens mites amp molds Trees flowers weeds hay plants
Animal dander Birds cats dogs
Medications Aspirin anti-inflammatory drugs
Foods Egg wheat nuts
SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

ASTHMA
Is a disorder of the bronchial airways characterizes by periods or reversible bronchospasm
Is often called reactive airway disease
Is a obstruction of the bronchioles characterized by attacks that occur suddenly and last from 30 to 60 minutes an attack that is difficult to control is referred to ldquo status asthmaticus ldquo
a disorder that causes the airways of the lungs to swell and narrow leading to wheezing shortness of breath chest tightness and coughing
Status Asthmaticus
is a severe life-threatening complication of asthma It is an acute episode of bronchospasm that leads to intensify With severe bronchospasm the workload of breathing increases 5 to 10 times which can lead to acute cor pulmonale ( right-sided heart failure resulting from lung disease)
STATUS ASTHMATICUS
bull pneumothorax commonly develops
If continues hypoxemia will be worsen acidosis begins if untreated not reversed respiratory or cardiac arrest ensues
ETIOLOGY AND RISK FACTORS
ASTHMA OCCURS IN FAMILIES WHICH SUGGESTS THAT IT IS AN INHERITED DISORDER
Environmental factors
ex viral infection allergens pollutants
Itching factors can excitatory states
ex stress laughing crying
Exercise Changes in temperature Strong odor
Asthma also is a component of triad disease
bull asthmabull nasal polypsbull allergy to aspirin
SUBSTANCES THAT TRIGGER ASTHMA
Type of Substance Examples
Air pollutants including dusts smoke mists amp fumes
Diesel exhaust tobacco smoke mineral rock coal amp wood dusts gases fumes amp vapors from aerosol agents chemicals cleaning materials solvents paints welding amp from heating amp cooling metals quickly
Pollens mites amp molds Trees flowers weeds hay plants
Animal dander Birds cats dogs
Medications Aspirin anti-inflammatory drugs
Foods Egg wheat nuts
SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

Status Asthmaticus
is a severe life-threatening complication of asthma It is an acute episode of bronchospasm that leads to intensify With severe bronchospasm the workload of breathing increases 5 to 10 times which can lead to acute cor pulmonale ( right-sided heart failure resulting from lung disease)
STATUS ASTHMATICUS
bull pneumothorax commonly develops
If continues hypoxemia will be worsen acidosis begins if untreated not reversed respiratory or cardiac arrest ensues
ETIOLOGY AND RISK FACTORS
ASTHMA OCCURS IN FAMILIES WHICH SUGGESTS THAT IT IS AN INHERITED DISORDER
Environmental factors
ex viral infection allergens pollutants
Itching factors can excitatory states
ex stress laughing crying
Exercise Changes in temperature Strong odor
Asthma also is a component of triad disease
bull asthmabull nasal polypsbull allergy to aspirin
SUBSTANCES THAT TRIGGER ASTHMA
Type of Substance Examples
Air pollutants including dusts smoke mists amp fumes
Diesel exhaust tobacco smoke mineral rock coal amp wood dusts gases fumes amp vapors from aerosol agents chemicals cleaning materials solvents paints welding amp from heating amp cooling metals quickly
Pollens mites amp molds Trees flowers weeds hay plants
Animal dander Birds cats dogs
Medications Aspirin anti-inflammatory drugs
Foods Egg wheat nuts
SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

STATUS ASTHMATICUS
bull pneumothorax commonly develops
If continues hypoxemia will be worsen acidosis begins if untreated not reversed respiratory or cardiac arrest ensues
ETIOLOGY AND RISK FACTORS
ASTHMA OCCURS IN FAMILIES WHICH SUGGESTS THAT IT IS AN INHERITED DISORDER
Environmental factors
ex viral infection allergens pollutants
Itching factors can excitatory states
ex stress laughing crying
Exercise Changes in temperature Strong odor
Asthma also is a component of triad disease
bull asthmabull nasal polypsbull allergy to aspirin
SUBSTANCES THAT TRIGGER ASTHMA
Type of Substance Examples
Air pollutants including dusts smoke mists amp fumes
Diesel exhaust tobacco smoke mineral rock coal amp wood dusts gases fumes amp vapors from aerosol agents chemicals cleaning materials solvents paints welding amp from heating amp cooling metals quickly
Pollens mites amp molds Trees flowers weeds hay plants
Animal dander Birds cats dogs
Medications Aspirin anti-inflammatory drugs
Foods Egg wheat nuts
SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

ETIOLOGY AND RISK FACTORS
ASTHMA OCCURS IN FAMILIES WHICH SUGGESTS THAT IT IS AN INHERITED DISORDER
Environmental factors
ex viral infection allergens pollutants
Itching factors can excitatory states
ex stress laughing crying
Exercise Changes in temperature Strong odor
Asthma also is a component of triad disease
bull asthmabull nasal polypsbull allergy to aspirin
SUBSTANCES THAT TRIGGER ASTHMA
Type of Substance Examples
Air pollutants including dusts smoke mists amp fumes
Diesel exhaust tobacco smoke mineral rock coal amp wood dusts gases fumes amp vapors from aerosol agents chemicals cleaning materials solvents paints welding amp from heating amp cooling metals quickly
Pollens mites amp molds Trees flowers weeds hay plants
Animal dander Birds cats dogs
Medications Aspirin anti-inflammatory drugs
Foods Egg wheat nuts
SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

ASTHMA OCCURS IN FAMILIES WHICH SUGGESTS THAT IT IS AN INHERITED DISORDER
Environmental factors
ex viral infection allergens pollutants
Itching factors can excitatory states
ex stress laughing crying
Exercise Changes in temperature Strong odor
Asthma also is a component of triad disease
bull asthmabull nasal polypsbull allergy to aspirin
SUBSTANCES THAT TRIGGER ASTHMA
Type of Substance Examples
Air pollutants including dusts smoke mists amp fumes
Diesel exhaust tobacco smoke mineral rock coal amp wood dusts gases fumes amp vapors from aerosol agents chemicals cleaning materials solvents paints welding amp from heating amp cooling metals quickly
Pollens mites amp molds Trees flowers weeds hay plants
Animal dander Birds cats dogs
Medications Aspirin anti-inflammatory drugs
Foods Egg wheat nuts
SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

SUBSTANCES THAT TRIGGER ASTHMA
Type of Substance Examples
Air pollutants including dusts smoke mists amp fumes
Diesel exhaust tobacco smoke mineral rock coal amp wood dusts gases fumes amp vapors from aerosol agents chemicals cleaning materials solvents paints welding amp from heating amp cooling metals quickly
Pollens mites amp molds Trees flowers weeds hay plants
Animal dander Birds cats dogs
Medications Aspirin anti-inflammatory drugs
Foods Egg wheat nuts
SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

SIGNS AND SYMPTOMS
coughing
wheezing a whistling sound
Shortness of breath
Chest tightness
sneezing and runny nose
Itchy and inflamed eyes
Substances that trigger asthma

Subjective
a Fatigueb Headache
Ojective
a Orthopnea expiratory wheezing stertorous breathing sounds cough
b cyanosis clubbing of the finger nailsc Distention of the neck veins
e Increased PCO2 and decreased PO2 of arterial blood gases
Poorly controlled asthma leads to
Increased visit to Doctor Urgent care clinic or ER
Hospitalization
Limitations in daily activities Lost of work days
Lower quality of life
DEATH
What you do if you have asthma identify and minimize contact with your asthma triggers
understand and take asthma medications as prescribed
recognize early signs that your asthma is getting worse
know what to do when your asthma is getting worse
PHYSICAL ASSESSMENT
MEDICAL HISTORY
What are your exact symptoms When do they occur and does anything specific seem to trigger them
Are you often exposed to tobacco smoke chemical fumes dust or other airborne irritants
Do you have hay fever or another allergic condition
Do you have any blood relatives with asthma hay fever or other allergies
What health problems do you have
What medications or herbal supplements do you take (Many medications can trigger asthma)
What is your occupation
Do you have pet birds or raise pigeons (In some people exposure to birds can cause asthma-like symptoms)
PHYSICAL EXAM
Your doctor may
bull Examine your nose throat and upper airways (upper respiratory tract)bull Use a stethoscope to listen to your breathing Wheezing mdash high-pitched whistling sounds when you breathe out mdash is one of the main signs of asthmabull Examine your skin for signs of allergic conditions such as eczema and hives
Your doctor will want to know whether you have common signs and symptoms of asthma such as
bull Recurrent wheezingbull Coughingbull Trouble breathingbull Chest tightnessbull Symptoms that occur or worsen at nightbull Symptoms that are triggered by cold air exercise or exposure to allergens
DIAGNOSTIC AND LABORATORY EXAMINATION
Spirometry
This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out
Peak flow
A peak flow meter is a simple device that measures how hard you can breathe out Lower than usual peak flow readings are a sign your lungs may not be working as well and that your asthma may be getting worse
Methacholine challenge
Methacholine is a known asthma trigger that when inhaled will cause mild constriction of your airways If you react to the methacholine you likely have asthma This test may be used even if your initial lung function test is normal
Imaging tests
A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems
Sputum Exam
This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing
Nursing Diagnosis
INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Poorly controlled asthma leads to
Increased visit to Doctor Urgent care clinic or ER
Hospitalization
Limitations in daily activities Lost of work days
Lower quality of life
DEATH
What you do if you have asthma identify and minimize contact with your asthma triggers
understand and take asthma medications as prescribed
recognize early signs that your asthma is getting worse
know what to do when your asthma is getting worse
PHYSICAL ASSESSMENT
MEDICAL HISTORY
What are your exact symptoms When do they occur and does anything specific seem to trigger them
Are you often exposed to tobacco smoke chemical fumes dust or other airborne irritants
Do you have hay fever or another allergic condition
Do you have any blood relatives with asthma hay fever or other allergies
What health problems do you have
What medications or herbal supplements do you take (Many medications can trigger asthma)
What is your occupation
Do you have pet birds or raise pigeons (In some people exposure to birds can cause asthma-like symptoms)
PHYSICAL EXAM
Your doctor may
bull Examine your nose throat and upper airways (upper respiratory tract)bull Use a stethoscope to listen to your breathing Wheezing mdash high-pitched whistling sounds when you breathe out mdash is one of the main signs of asthmabull Examine your skin for signs of allergic conditions such as eczema and hives
Your doctor will want to know whether you have common signs and symptoms of asthma such as
bull Recurrent wheezingbull Coughingbull Trouble breathingbull Chest tightnessbull Symptoms that occur or worsen at nightbull Symptoms that are triggered by cold air exercise or exposure to allergens
DIAGNOSTIC AND LABORATORY EXAMINATION
Spirometry
This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out
Peak flow
A peak flow meter is a simple device that measures how hard you can breathe out Lower than usual peak flow readings are a sign your lungs may not be working as well and that your asthma may be getting worse
Methacholine challenge
Methacholine is a known asthma trigger that when inhaled will cause mild constriction of your airways If you react to the methacholine you likely have asthma This test may be used even if your initial lung function test is normal
Imaging tests
A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems
Sputum Exam
This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing
Nursing Diagnosis
INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

What you do if you have asthma identify and minimize contact with your asthma triggers
understand and take asthma medications as prescribed
recognize early signs that your asthma is getting worse
know what to do when your asthma is getting worse
PHYSICAL ASSESSMENT
MEDICAL HISTORY
What are your exact symptoms When do they occur and does anything specific seem to trigger them
Are you often exposed to tobacco smoke chemical fumes dust or other airborne irritants
Do you have hay fever or another allergic condition
Do you have any blood relatives with asthma hay fever or other allergies
What health problems do you have
What medications or herbal supplements do you take (Many medications can trigger asthma)
What is your occupation
Do you have pet birds or raise pigeons (In some people exposure to birds can cause asthma-like symptoms)
PHYSICAL EXAM
Your doctor may
bull Examine your nose throat and upper airways (upper respiratory tract)bull Use a stethoscope to listen to your breathing Wheezing mdash high-pitched whistling sounds when you breathe out mdash is one of the main signs of asthmabull Examine your skin for signs of allergic conditions such as eczema and hives
Your doctor will want to know whether you have common signs and symptoms of asthma such as
bull Recurrent wheezingbull Coughingbull Trouble breathingbull Chest tightnessbull Symptoms that occur or worsen at nightbull Symptoms that are triggered by cold air exercise or exposure to allergens
DIAGNOSTIC AND LABORATORY EXAMINATION
Spirometry
This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out
Peak flow
A peak flow meter is a simple device that measures how hard you can breathe out Lower than usual peak flow readings are a sign your lungs may not be working as well and that your asthma may be getting worse
Methacholine challenge
Methacholine is a known asthma trigger that when inhaled will cause mild constriction of your airways If you react to the methacholine you likely have asthma This test may be used even if your initial lung function test is normal
Imaging tests
A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems
Sputum Exam
This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing
Nursing Diagnosis
INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PHYSICAL ASSESSMENT
MEDICAL HISTORY
What are your exact symptoms When do they occur and does anything specific seem to trigger them
Are you often exposed to tobacco smoke chemical fumes dust or other airborne irritants
Do you have hay fever or another allergic condition
Do you have any blood relatives with asthma hay fever or other allergies
What health problems do you have
What medications or herbal supplements do you take (Many medications can trigger asthma)
What is your occupation
Do you have pet birds or raise pigeons (In some people exposure to birds can cause asthma-like symptoms)
PHYSICAL EXAM
Your doctor may
bull Examine your nose throat and upper airways (upper respiratory tract)bull Use a stethoscope to listen to your breathing Wheezing mdash high-pitched whistling sounds when you breathe out mdash is one of the main signs of asthmabull Examine your skin for signs of allergic conditions such as eczema and hives
Your doctor will want to know whether you have common signs and symptoms of asthma such as
bull Recurrent wheezingbull Coughingbull Trouble breathingbull Chest tightnessbull Symptoms that occur or worsen at nightbull Symptoms that are triggered by cold air exercise or exposure to allergens
DIAGNOSTIC AND LABORATORY EXAMINATION
Spirometry
This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out
Peak flow
A peak flow meter is a simple device that measures how hard you can breathe out Lower than usual peak flow readings are a sign your lungs may not be working as well and that your asthma may be getting worse
Methacholine challenge
Methacholine is a known asthma trigger that when inhaled will cause mild constriction of your airways If you react to the methacholine you likely have asthma This test may be used even if your initial lung function test is normal
Imaging tests
A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems
Sputum Exam
This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing
Nursing Diagnosis
INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

MEDICAL HISTORY
What are your exact symptoms When do they occur and does anything specific seem to trigger them
Are you often exposed to tobacco smoke chemical fumes dust or other airborne irritants
Do you have hay fever or another allergic condition
Do you have any blood relatives with asthma hay fever or other allergies
What health problems do you have
What medications or herbal supplements do you take (Many medications can trigger asthma)
What is your occupation
Do you have pet birds or raise pigeons (In some people exposure to birds can cause asthma-like symptoms)
PHYSICAL EXAM
Your doctor may
bull Examine your nose throat and upper airways (upper respiratory tract)bull Use a stethoscope to listen to your breathing Wheezing mdash high-pitched whistling sounds when you breathe out mdash is one of the main signs of asthmabull Examine your skin for signs of allergic conditions such as eczema and hives
Your doctor will want to know whether you have common signs and symptoms of asthma such as
bull Recurrent wheezingbull Coughingbull Trouble breathingbull Chest tightnessbull Symptoms that occur or worsen at nightbull Symptoms that are triggered by cold air exercise or exposure to allergens
DIAGNOSTIC AND LABORATORY EXAMINATION
Spirometry
This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out
Peak flow
A peak flow meter is a simple device that measures how hard you can breathe out Lower than usual peak flow readings are a sign your lungs may not be working as well and that your asthma may be getting worse
Methacholine challenge
Methacholine is a known asthma trigger that when inhaled will cause mild constriction of your airways If you react to the methacholine you likely have asthma This test may be used even if your initial lung function test is normal
Imaging tests
A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems
Sputum Exam
This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing
Nursing Diagnosis
INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PHYSICAL EXAM
Your doctor may
bull Examine your nose throat and upper airways (upper respiratory tract)bull Use a stethoscope to listen to your breathing Wheezing mdash high-pitched whistling sounds when you breathe out mdash is one of the main signs of asthmabull Examine your skin for signs of allergic conditions such as eczema and hives
Your doctor will want to know whether you have common signs and symptoms of asthma such as
bull Recurrent wheezingbull Coughingbull Trouble breathingbull Chest tightnessbull Symptoms that occur or worsen at nightbull Symptoms that are triggered by cold air exercise or exposure to allergens
DIAGNOSTIC AND LABORATORY EXAMINATION
Spirometry
This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out
Peak flow
A peak flow meter is a simple device that measures how hard you can breathe out Lower than usual peak flow readings are a sign your lungs may not be working as well and that your asthma may be getting worse
Methacholine challenge
Methacholine is a known asthma trigger that when inhaled will cause mild constriction of your airways If you react to the methacholine you likely have asthma This test may be used even if your initial lung function test is normal
Imaging tests
A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems
Sputum Exam
This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing
Nursing Diagnosis
INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

DIAGNOSTIC AND LABORATORY EXAMINATION
Spirometry
This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out
Peak flow
A peak flow meter is a simple device that measures how hard you can breathe out Lower than usual peak flow readings are a sign your lungs may not be working as well and that your asthma may be getting worse
Methacholine challenge
Methacholine is a known asthma trigger that when inhaled will cause mild constriction of your airways If you react to the methacholine you likely have asthma This test may be used even if your initial lung function test is normal
Imaging tests
A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems
Sputum Exam
This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing
Nursing Diagnosis
INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Spirometry
This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out
Peak flow
A peak flow meter is a simple device that measures how hard you can breathe out Lower than usual peak flow readings are a sign your lungs may not be working as well and that your asthma may be getting worse
Methacholine challenge
Methacholine is a known asthma trigger that when inhaled will cause mild constriction of your airways If you react to the methacholine you likely have asthma This test may be used even if your initial lung function test is normal
Imaging tests
A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems
Sputum Exam
This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing
Nursing Diagnosis
INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Methacholine challenge
Methacholine is a known asthma trigger that when inhaled will cause mild constriction of your airways If you react to the methacholine you likely have asthma This test may be used even if your initial lung function test is normal
Imaging tests
A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems
Sputum Exam
This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing
Nursing Diagnosis
INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Imaging tests
A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems
Sputum Exam
This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing
Nursing Diagnosis
INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Nursing Diagnosis
INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

INEFFECTIVE BREATHING PATTERN
Related to Impaired exhalation and anxiety
Outcomes The client will have improved breathing patterns as evidence by
1A decreasing respiratory rate wn normal limits
2A decreased dyspnea less nasal flaring and reduced use of accessory muscle
3Decreased manifestations of anxiety
4A return of ABG levels wn normal limits
5O2 saturation greater than 95
6VC measurements wn normal limits or greater than 40
INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

INTERVENTIONS
aAssess the client frequently observing respiratory rate and depth
bAssess the breathing pattern for shortness of breath pursed-lip breathing nasal flaring strenal and intercostal retractioins or a prolonged expiratory phase
cPlace the client in a Fowlerrsquos Position and give O2 as ordered
dMonitor ABGs and O2 saturation levels to determine the effectiveness of tx
INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

INEFFECTIVE AIRWAY CLEARANCE
Related to Increased production of secretions and bronchospasmOutcomes The client will have effective airway clearance as evidence by
1Decreased inspiratory and expiratory wheezing
2Decreased rhonchi
3Decreased dry and non-productive cough
INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

INTERVENTIONS
aIf the clientrsquos airway is compromised the clientrsquos secretion may require suctioning
bMonitor the color and consistency of the sputum
cAssist the client to cough effectively
dEncourage oral fluids to thin the secretions and replace fluid lost through rapid respiration
eIf chest secretions are thick and difficult to expectorate client may benefit from postural drainage lung percussion and vibration expectorants and frequent position changes
f Give frequent oral care q 2 to 4 hrs to remove the taste of secretions and remoisten the oral mucous mm that have dried from mouth breathing
NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

NURSING MANAGEMENT
Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Ask the client to rate dyspnea on a scale of 0 to 10
Determine know medication allergies
Hx of cardiac disease
Assist the client to determine whether there is a pattern to the manifestation in order to help identify a trigger that precipitate the asthma
Ask the client about current medication that may induce bronchospasms (propranolol)
Ask the clientrsquos ability to manage asthma as well as the clientrsquos gen adaptation to the illness Denial of the illness can interfere w early tx
Determine whether the client is experiencing and increased no of stressors (can exacerbate asthma)
PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PHARMACOLOGICAL ACTIONS
Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Cromolyn sodium and nedocromil
are generally well tolerated with most side effects decreasing with continued use Make sure to tell your doctor if side effects do not resolve or become bothersome
Side effects include
bull Bad taste in mouthbull Coughbull Itching or Sore ThroatbullHeadachebullSneezing or stuffy nose
Make sure to notify your doctor promptly if you experience
Shortness of breathWheezing
ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

ALBUTEROL AND IPRATROPIUM INHALERBRAND NAME COMBIVENT COMBIVENT RESPIMAT
DRUG CLASS AND MECHANISM Albuterolipratropium is a combination product consisting of two bronchodilators albuterol (Proventil Ventolin) and ipratropium (Atrovent) that is used in the treatment of chronic obstructive pulmonary disease (bronchitis and emphysema) when there is evidence of spasm (narrowing) of the airways (bronchi) Bronchodilators dilate or enlarge the airways by relaxing the muscles surrounding the airways Albuterol and ipratropium work by different mechanisms but both cause the muscles of the airways to relax
PRESCRIBED FORis used in the treatment of bronchospasm or narrowing of the airways caused by emphysema or bronchitis in patients who require a second bronchodilator
SIDE EFFECTS Headache nausea nervousness trouble sleepingdizziness dry mouththroat coughing or runny nose may occur
ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

ALBUTEROL VENTOLIN PROVENTIL PROVENTIL-HFA ACCUNEB VOSPIRE PROAIR (SALBUTAMOL)
DRUG CLASS It dilates the airways of the lung and is used for
treating asthma and other conditions of the lung
PRESCRIBED FOR
Is used for relief and prevention of airway obstruction (bronchospasm) in patients with asthma or exercise induced asthma
Albuterol is also used for treating patients with emphysema or chronic bronchitis when their symptoms are related to reversible airway obstruction The inhaled form of albuterol starts working within 15 minutes and can last up to 6 hours
SIDE EFFECTS
nervousness tremor headache palpitation fast heart rate elevated blood pressure nausea dizziness and heartburn Throat irritation and nosebleed can also occur Allergic reactions may rarely occur and may manifest as rash hives swelling bronchospasm or anaphylaxis (shock) Worsening of diabetes and lowering of potassium have also been reported In rare patients inhaled albuterol can paradoxically precipitate life-threatening bronchospasm
Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Xolair
one of the immunomodulators is given as an injection As a result you may experience pain or swelling at the injection site
Other common side effects include
Viral illness
URTI
Sinusitis
Headache
Sore Throat
GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

GENERIC NAME ZAFIRLUKASTBRAND NAME ACCOLATE
DRUG CLASS AND MECHANISM
Zafirlukast is an oral leukotriene receptor antagonist used for treating asthma Leukotrienes are a group of chemicals manufactured in the body from arachidonic acid Release of leukotrienes within the body for example by allergic reactions promotes inflammation in many diseases such as asthma a disease in which inflammation occurs in the lungs
SIDE EFFECTSThe most common side effects of zafirlukast
are headache dizziness nausea diarrhea abdominal pain sore throat respiratory infections and rhinitis Liver failure has been associated with zafirlukast treatment
GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

GENERIC NAME terbutalineBRAND NAME Brethine
DRUG CLASS AND MECHANISMTerbutaline is a member of a class of drugs called beta adrenergic
receptor agonists (stimulators) that is used for treating asthma and other diseases of the airways
SIDE EFFECTSTerbutaline may cause side effects such as tremornausea
nervousness dizziness headache drowsiness heartburn heart palpitations fast heart rate and elevated blood pressure Vomiting anxiety restlessness lethargy excessive sweating chest pain and muscle cramping also may occur Low blood potassium (hypokalemia) and high blood glucose have been associated with terbutaline
Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Bronchitis
BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

BRONCHITIS
describes inflammation of the bronchial tubes (inflammation -itis) The inflammation causes swelling of the lining of these breathing tubes narrowing the tubes and promoting secretion of inflammatory fluid
The main symptom of bronchitis is a hacking cough It is likely that your cough will bring up thick yellow-grey mucus although this does not always happen
People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

People with bronchitis breathe less air and oxygen into their lungs they also have heavy mucus or phlegm forming in the airways Bronchitis may be acute or chronic (long-term)
Acute bronchitis is a shorter illness that commonly follows a cold or viral infection such as the flu It generally consists of a cough with green sputum chest discomfort or soreness fever and sometimes shortness of breath Acute bronchitis usually lasts a few days or weeks
Chronic bronchitis is characterized by a persistent mucus-producing cough on most days of the month three months of a year for two successive years in absence of a secondary cause of the cough People with chronic bronchitis have varying degrees of breathing difficulties and symptoms may get better and worsen during different parts of the year
Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Causes bronchitis
Bronchitis is caused by viruses bacteria and other particles that irritate the bronchial tubes
Acute bronchitis is usually caused by a viral infection in the bronchi - often the same viruses that causes cold and flu Bronchitis is actually part of the immune response to fighting against the infection since additional swelling occurs in the bronchial tubes as the immune systemlsquos actions generate mucus In addition to viruses bacteria exposure to tobacco smoke exposure to pollutants or solvents and gastroesophageal reflux disease (GERD) can also cause acute bronchitis
Chronic bronchitis is most commonly caused by cigarette smoking However it can also be the result of continuous attacks of acute bronchitis Air pollution dust toxic gases and other industrial fumes are known to be responsible for the condition
Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Risk factors and SignampSymptoms
FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

FACTORS THAT INCREASE YOUR RISK OF BRONCHITIS INCLUDE
Cigarette smoke People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis
Low resistance This may result from another acute illness such as a cold or from a chronic condition that compromises your immune system Older adults infants and young children have greater vulnerability to infection
Exposure to irritants on the job Risk of developing bronchitis is greater if you work around certain lung irritants such as grains or textiles or are exposed to chemical fumes
Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Signs and symptoms for both acute and chronic bronchitis include Inflammation or swelling of the bronchi
Coughing
Production of clear white yellow grey or green mucus (sputum)
Shortness of breath
Wheezing
Fatigue
Fever and chills
Chest pain or discomfort
Blocked or runny nose
PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PHARMACOLOGIC ACTION
GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

GENERIC NAME OFLOXACINBRAND NAME FLOXIN (DISCONTINUED BRAND)
DRUG CLASS AND MECHANISM Ofloxacin is an antibiotic
that is used to treat bacterial infections It belongs to the fluoroquinolone class of antibiotics which includes levofloxacin (Levaquin) ciprofloxacin (Cipro) gatifloxacin (Tequin) norfloxacin (Noroxin) moxifloxacin (Avelox) trovafloxacin (Trovan) and others Ofloxacin stops the multiplication of bacteria by inhibiting the reproduction and repair of their genetic material (DNA)
PRESCRIBED FOROfloxacin is used to
treat pneumonia and bronchitiscaused by Haemophilus influenzae and Streptococcus pneumoniae It also is used in treating skin infections caused by Staphylococcus aureus andStreptococcus pyogenes bacteria Ofloxacin is used to treat sexually transmitted diseases such as gonorrhea and chlamydia but is not effective against syphilis Ofloxacin is used often to treat urinary infections and prostate infections caused by E Coli
SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

SIDE EFFECTSThe most frequent side effects of ofloxacin include nauseavomiting diarrhea insomnia headache dizziness itching and vaginitis in women
DRUG INTERACTIONOfloxacin reduces the elimination of theophylline
elevating blood levels of theophylline (Theophylline is used to open airways in the treatment of asthma)
terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

terbutaline
fluticasone furoate and vilanterol inhalation powder
EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

EMPHYSEMA
Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Emphysema is a disorder in which the alveolar walls are destroyed This destruction leads to permanent over distention of the air spaces Emphysema occurs when the air sacs in your lungs are
gradually destroyed making you progressively more short of breath Emphysema is one of several diseases known collectively as chronic obstructive pulmonary disease (COPD) Smoking is the leading cause of emphysema
Characterized by distended inelastic or destroyed alveoli with bronchiolar obstruction and collapse these alterations greatly impair the diffusion of gases through the alveolar capillary membrane
which involves destruction of the lungs over time
Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Causes
The actual cause of emphysema is unknown Risk factors for the development of emphysema include cigarette smoking living or working in a highly polluted area and a family history of pulmonary disease Frequent childhood pulmonary infections have been identified as a cause of bronchiectasis
3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

3 Types of Emphysema
1Centriacinar or Centrilobular Emphysema
2Panacinar Emphysema
3Paraseptal Emphysema
CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

CENTRIACINAR OR CENTRILOBULAR EMPHYSEMA
Is the most common type produces destruction in the bronchioles usu in the upper lung regions
Inflammation begins in the bronchioles and spreads peripherally but usu The alveolar sac remains intact
This type of emphysema occurs most often in smokers
PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PANACINAR EMPHYSEMA
it destroys the entire alveolus and most commonly involves the lower portions of the lungs This form of the disease is generally observed in individuals with AAT deficiencies
focal panacinar emphysema can be seen at the lung bases in smokers
PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PARASEPTAL EMPHYSEMA
or distal acinar
It involves the distal airway structure alveolar ducts and alveolar sacs
The process is localized around the septa of the lungs and pleura resulting in isolated blebs along the lung periphery
Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Client who have primary emphysema have progressive dyspnea on exertion that eventually becomes dyspnea at rest
The anterioposterior diameter of the chest is enlarged and the chest has hyper resonant sounds to percussion
Chest films show overflation and flattened diaphragms
ABG values are usu Normal until later stage when compensated respiratory acidosis is often evident
Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Risk Factors
Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Factors that increase your risk of developing emphysema include
Smoking Emphysema is most likely to develop in cigarette smokers but cigar and pipe smokers also are susceptible The risk for all types of smokers increases with the number of years and amount of tobacco smoked Age Although the lung damage that occurs in emphysema develops gradually most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60
SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

SIGNS AND SYMPTOMS
Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Breathlessness
Other Emphysema Symptoms
o Wheezing This symptom of emphysema is shared with asthma Wheezing often improves with inhaled medicines called bronchodilators
o Cough A large proportion of people with emphysema experience a cough Often this is related to smoking However cough can persist as one of the symptoms of emphysema after quitting smoking
oChest tightness or pain These may be symptoms of emphysema or of coexisting heart disease Chest tightness occurs more often with exercise or during periods of breathlessness
People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

People with emphysema may also face some other less common emphysema symptoms
oLoss of appetite and weight lossoDepressionoPoor sleep qualityoDecreased sexual function
PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PHYSICAL ASSESSMENT
Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Anorexia fatigue weight loss
Feeling of breathlessnesscough sputum production flaring of the nostrils use of accessory muscles of respiration increased rate and depth of breathing dyspnea
Decreased respiratory excursionresonance to hyperresonance decreased breath sounds with prolonged expiration normal or decreased fremitus
LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

LABORATORY EXAM
Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Oximetry
Oximetry is a non-invasive test in which a sensor is taped or clipped onto a finger or earlobe to measure the percentage of red blood cells that have oxygen This value is usually greater than 92 Results less than 90 may signal the need for supplemental oxygen
Blood Tests
A complete blood cell count (CBC) may be performed to check for an increase in the number of red blood cells In response to lower blood oxygen concentrations the body manufactures more red blood cells to try to deliver as much oxygen as possible to cells
Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Alpha-1 antitrypsin levels may be measured to look for the genetic form of emphysema
The arterial blood gas can also give parameters to establish the diagnosis of chronic respiratory failure
Radiology
A plain chest X-ray may show lungs that have become too inflated and have lost normal lung markings consistent with destruction of alveoli and lung tissue
A CT scan can reveal more detail regarding the amount of lung destruction but is not a normal part of the evaluation of patients with emphysema
Pulmonary function tests or spirometry can measure the air flow into and out of the lungs and be used to predict the severity of emphysema
Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Some measurements include
FVC (forced vital capacity) the amount of air that can be forcibly exhaled after the largest breath possible
FEV1 (forced expiratory volume in 1 second) the amount of air that is forcibly exhaled in 1 second Even though total air exhalation may be less affected as the lung loses its elasticity it takes longer for the air to get out and FEV1 becomes a good marker for disease severity
FEV (forced expiratory volume) can be measured throughout the exhalation cycle often at 25 50 and 75 to help measure function of different sized bronchi and bronchioles
PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PEF (peak expiratory flow)
maximal speed of air during exhalation DLCO (diffusion capacity) measures how much carbon monoxide can be inhaled and absorbed into the bloodstream within a period of time A small amount of tracer carbon monoxide is inhaled and then quickly exhaled The amount of carbon monoxide in the exhaled air is measured and determines how well the lungs work in absorbing the gas This helps determine and measure lung function
Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Pathophysiology
Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Emphysema is a pathological diagnosis defined by permanent enlargement of airspaces distal to the terminal bronchioles This leads to a dramatic decline in the alveolar surface area available for gas exchange Furthermore loss of alveoli leads to airflow limitation by 2 mechanisms First loss of the alveolar walls results in a decrease in elastic recoil which leads to airflow limitation Second loss of the alveolar supporting structure leads to airway narrowing which further limits airflow
Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Emphysema commonly presents with chronic bronchitis Chronic bronchitis leads to obstruction by causing narrowing of both the large and small (lt 2 mm) airways In the large airways an increase in Goblet cells squamous metaplasia of ciliary epithelial cells and loss of serous acini can be seen In the small airways Goblet cell metaplasia smooth muscle hyperplasia and subepithelial fibrosis can be seen In healthy individuals small airways contribute little to airway resistance however in COPD patients these become the main site of airflow limitation
PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PRIMARY NURSING DIAGNOSIS
IMPAIRED GAS EXCHANGE RELATED TO DESTRUCTION OF ALVEOLAR WALLS
MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

MEDICAL MANAGEMENT
Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Treatment is directed at improving ventilation decreasing work of breathing and preventing infection
Smoking cessation
Physical therapy to conserve and increase pulmonary ventilation
Maintenance of proper environmental conditions to facilitate breathing
Psychological support
Ongoing program of patient education and rehabilitation
Bronchodilators and metered-dose inhalers (aerosol therapy dispensing particles in fine mist)
Treatment of infection (antimicrobial therapy at the first sign of respiratory infection)
Oxygenation in low concentrations for severe hypoxemia
MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

MEDICATIONS
Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Bronchodilators Anticholinergic agents such as atropine sulfate ipratropium bromide are used in reversal of bronchoconstriction
Bronchodilators Beta2-adrenergic agents such as( inhaled beta2-adrenergic agonists by metered-dose inhaler (MDI) such as albuterol metaproterenol or terbutaline )are used in reversal of bronchoconstriction
Systemic corticosteroids such as methylprednisolone IV prednisone PO is used to decrease inflammatory response and improve airflow in some patients for a few days during acute exacerbations
Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Other Drug Therapy
Bronchodilators which are used for prevention and maintenance therapy can be administered as aerosols or oral medications
Generally inhaled anticholinergic agents are the first-line therapy for emphysema with the addition of betaadrenergic agonists added in a stepwise fashion
Antibiotics are ordered if a secondary infection develops As a preventive measure influenza and pneumonia vaccines are administered
NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

NURSING INTERVENTIONS
Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Maintaining a patent airway is a priority Use a humidifier at night to help the patient mobilize secretions in the morning
Encourage the patient to use controlled coughing to clear secretions that might have collected in the lungs during sleep
Place patients who are experiencing dyspnea in a high Fowler position to improve lung expansion
Placing pillows on the overhead table and having the patient lean over in the orthopneic position may also be helpful
Teach the patient pursed-lip and diaphragmatic breathing To avoid infection screen visitors for contagious diseases and instruct the patient to avoid crowds
Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Conserve the patientrsquos energy in every possible way Plan activities to allow for rest periods eliminating nonessential procedures until the patient is stronger It may be necessary to assist with the activities of daily living and to anticipate the patientrsquos needs by having supplies within easy reach
Refer the patient to a pulmonary rehabilitation program if one is available in the community
Patient education is vital to long-term management Teach the patient about the disease and its implications for lifestyle changes such as avoidance of cigarette smoke and other irritants activity alterations and any necessary occupational changes Provide information to the patient and family about medications and equipment
DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

DISCHARGE PLANNING
Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Be sure the patient and family understand any medication prescribed including dosage route action and side effects
Instruct the patient to report any signs and symptoms of infection to the primary healthcare provider
Explain necessary dietary adjustments to the patient and family Recommend eating small frequent meals including high-protein high-density foods
Encourage the patient to plan rest periods around his or her activities conserving as much energy as possible
Arrange for return demonstrations of equipment used by the patient and family If the patient requires home oxygen therapy refer the patient to the appropriate rental service and explain the hazards of combustion and increasing the flow rate without consultation from the primary healthcare provider
BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

BRONCHIECTASIS
o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

o Bronchiectasis is an uncommon disease most often secondary to an infectious process that results in the abnormal and permanent distortion of one or more of the conducting bronchi or airways
oAn extreme form of obstructive bronchitis causes permanent abnormal dilation and distortion of bronchi and bronchioles It develop when bronchial walls are weakened by chronic inflammation conditions Any condition producing a narrowing of the lumen of the bronchioles however may result in bronchiectasis including tuberculosis adenoviral infections and pneumonia
3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

3 types of bronchiectasis1 Cylindrical bronchiectasis is the mildest form and reflects
the loss of the normal tapering of the airways The symptoms may be quite mild like a chronic cough and usually are discovered on CT scans of the chest
2 Saccular bronchiectasis is more severe with further distortion of the airway wall and symptomatically affected persons produce more sputum
3 Cystic bronchiectasis is the most severe form of bronchiectasis and fortunately it is the least common form This often occurred in the pre-antibiotic era when an infection would run its course and the patient would survive with residual lung damage These patients often would have a chronic productive cough bringing up a cup or more of discolored mucus each
Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Within the lungs air passages called bronchi form a tree-like structure through which air travels in and out The bronchi are lined with tiny hair-like projections called cilia which work to sweep mucus upwards within the lungs allowing it to be easily coughed out
Bronchiectasis is a condition in which some of the bronchi have become scarred and permanently enlarged During the disease process the cilia are damaged so that they are unable to effectively sweep away the mucus As a result mucus accumulates in parts of the lung that are affected and the risk of developing lung infections is increased Recurrent infections can then cause further scarring and bronchial enlargement thereby perpetuating the condition
Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Causes
Prior to the introduction of widespread immunizations programs bronchiectasis often occurred as the result of infection with measles or whooping cough
Currently bronchiectasis usually occurs as the result of an illness such as pneumonia (approximately 25 of all cases) Other causes include
Cystic fibrosisImmune deficiencyRecurrent aspiration of fluid into the lungs (as occurs with gastroesophageal reflux)Inhalation of a foreign object into the lungs (if left untreated)Inhalation of harmful chemicals eg ammoniaIn rare cases it may be congenital (present at birth
SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

SIGNS AND SYMPTOMS
The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

The main symptom of bronchiectasis is a mucus-producing cough The cough is usually worse in the mornings and is often brought on by changes in posture The mucus may be yellow-green in colour and foul smelling indicating the presence of infection
Other symptoms may include
Coughing up blood (more common in adults)Bad breathWheezing chest - a characteristic crackling sound may be heard when listening with a stethoscope Recurring lung infections A decline in general healthIn advanced bronchiectasis breathlessness can occur
DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

DIAGNOSIS
An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

An initial diagnosis of bronchiectasis is based on the patients symptoms their medical history and a physical examination Further diagnostic tests may include
Chest x-rayCT (computerized tomography) scan Blood testsTesting of the mucus to identify any bacteria presentChecking oxygen levels in the bloodLung function tests (spirometry)
TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

TREATMENT
Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Bronchiectasis is a chronic (long-term) condition that requires lifelong maintenance Good management of the condition is vital to prevent ongoing damage to the lungs and worsening of the conditionThe ultimate goal of treatment is to clear mucus from the chest and prevent further damage to the lungs The two main types of treatments used are
Medications
Physiotherapy and exerciseChest physiotherapy and postural drainage are used to
remove secretions from the lungs An individual program is usually developed where exercise and breathing techniques to clear the lungs of mucus are taught
Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Prevention
To help prevent bronchiectasis in children
Not smoking during pregnancy and having a smoke free home
Breastfeeding your children
Eating a healthy balanced diet
Early detection and treatment of chest infections
Making sure homes are warm and dry (making chest infections less likely)
Immunization for diseases like measles and whooping cough which can lead to bronchiectasis
CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

CAUSES OF COPD
ABOUT 90 OF PEOPLE WITH COPD ARE CURRENT OR FORMER SMOKERS -- AND THEIR DISEASE USUALLY APPEARS AFTER AGE 40 SECONDHAND SMOKE AND EXPOSURE TO ENVIRONMENTAL IRRITANTS AND POLLUTION ALSO CAN INCREASE YOUR RISK OF COPD IN RARE CASES THE DNA PASSED DOWN THROUGH A FAMILY CAN LEAD TO COPD EVEN IN NEVER SMOKERS ONE OF THESE GENETIC CONDITIONS IS CALLED ALPHA-1 ANTITRYPSIN (AAT) DEFICIENCY
RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

RISK FACTORS CAUSES Smoking is the leading cause of COPD The more a
person smokes the more likely that person will develop COPD
Exposure to certain gases or fumes in the workplace Exposure to heavy amounts of secondhand smoke and
pollution Frequent use of cooking fire without proper ventilation Rarely a genetic condition called
alpha-1 antitrypsin deficiency may play a role in causing COPD People who have this condition have low levels of alpha-1 antitrypsin (AAT)mdasha protein made in the liver
SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

SIGNS AND SYMPTOMS
INSIDE THE LUNGS COPD CAN CLOG THE AIRWAYS AND DAMAGE THE TINY BALLOON-LIKE SACS (ALVEOLI) THAT ABSORB OXYGEN THESE CHANGES CAN CAUSE THE FOLLOWING SYMPTOMS
Shortness of breath in everyday activitiesWheezingChest tightnessConstant coughingProducing a lot of mucus (sputum)Feeling tiredFrequent colds or flu
Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Severe COPD can make it difficult to walk cook clean house or even bathe Coughing up excess mucus and feeling short of breath may worsen Advanced illness can also cause
o Swollen legs or feet from fluid buildupo Weight losso Less muscle strength and enduranceo A headache in the morningo Blue or grey lips or fingernails (due to low oxygen levels)
PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PHYSICAL ASSESSMENT
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Nasal flaring
Cyanosis
Dyspnea
Decreased respiratory effort
Decreased LOC
Accessory muscle use
Decreased breath sounds
Decreased oxygen saturation
PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PHYSICALEXAM
FIRST YOUR DOCTOR WILL LISTEN TO YOUR CHEST AS YOU BREATHE THEN WILL ASK ABOUT YOUR SMOKING HISTORY AND WHETHER YOU HAVE A FAMILY HISTORY OF COPD THE AMOUNT OF OXYGEN IN YOUR BLOOD MAY BE MEASURED WITH A BLOOD TEST OR A PULSE OXIMETER A PAINLESS DEVICE THAT CLIPS TO A FINGER
MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

MEDICAL CHART REVIEW Allergies Chief Complaint or History of Present Illness Patient history and physical Past Medical and Surgical History Social and Family History Diagnosis Current orders (medicine diet activity etc) Physician Progress Note
EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

EXTREMITIES INSPECTION
Clubbing ndash loss of angle between nail and terminal phalanx - Look at the nail bed the skin is a little higher and the nail is a little lower - Have patient put their fingersrsquo nail bed to nail bedmdashyou should be able to see light thru a space bt the nail beds no clubbing- If you donrsquot see light between the 2 nail beds then therersquos clubbing Picture Angel bt nail bed and terminal phalanx is lostmdashyou would not see light coming through the nail bed
PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PULMONARY EXAM
bull INSPECTION (CHEST SHAPE AND SYMMETRY) bull PALPATION bull PERCUSSION bull AUSCULTATIONmdashIN GI EXAM YOU AUSCULTATE BEFORE YOU PALPATEmdashIF YOU PALPATE FIRST YOUrsquoLL CREATE BOWEL SOUNDS (THUS YOU WONrsquoT KNOW IF THEY WERE ABSENT TO BEGIN WITH)
SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

SPIROMETRY BREATH TEST
This involves blowing out as hard as possible into a small machine that tests lung capacity The results can be checked right away and the test does not involve exercising drawing blood or exposure to radiation
Using a stethoscope to listen to the lungs can also be helpful However sometimes the lungs sound normal even when COPD is present
Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Chest X-Ray
A chest X-ray isnt used to diagnose COPD but it may help rule out conditions that cause similar symptoms such as pneumonia In advanced COPD a chest X-ray might show lungs that appear much larger than normal
Sometimes patients need to have a blood test (called arterial blood gas) to measure the amounts of oxygen and carbon dioxide in the blood
PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PEAK FLOW TEST Is used to confirm you have COPD and not asthma your doctor might ask you to take regular measurements of your breathing using a peak flow meter at different times over several days The peak flow meter measures how fast you can breathe out
COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

COMPUTERIZED TOMOGRAPHY (CT) SCAN
Some people may need a CT scan This provides more information than an X-ray and can be useful in diagnosing other lung diseases or assessing changes to your lungs due to COPD
PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PATHOPHYSIOLOGY
PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

PATHOPHYSIO
NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

NURSING DIAGNOSIS
Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Ineffective airway clearance
related tobronchoconstriction
increased sputum production
ineffective cough
fatigue lack of energy
bronchopulmonary infection
Intervention
Give the patient 6 to 8 glasses of fluid day unless there is a cor pulmonale
Teach and give encouragement use of diaphragmatic breathing and coughing techniquesAssist in the provision of action nebulizer metered dose inhalersPerform postural drainage with percussion and vibration in the morning and evening according to the requiredInstruct patient to avoid irritants such as cigarette smoke aerosols temperature extremes and smokeTeach about the early signs of infection should
be reported to your doctor immediately increased sputum change in sputum color viscosity ofsputum increased shortness of breath chest tightness fatigueGive encouragement to patients to immunize against influenzae and Streptococcus pneumoniae
INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

INTERVENTIONS Activity intolerance
related toimbalance between oxygen supply with demand
Assess the individual response to the activity pulse blood pressure respiration
Measure vital signs immediately after the activity the client rest for 3 minutes then measuring the vital signs againSupport the patient in establishing a regular exercise using a treadmill and exercise walking or other exercise appropriate such as walking slowly
Assess the patients level of function of the last and develop training plans based on the status of basic functionsProvide oxygen as represented is required before and during the run of activity just in case
increase activity gradually clients currently or long bed rest started doing range of motion at least 2 times a dayIncrease tolerance to the activity by encouraging clients to do the activity more slowly or a shorter time with more rest or with a lot of help
ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

ANXIETY RELATED TO ACUTE BREATHING DIFFICULTIES AND FEAR OF SUFFOCATIONOUTCOME THE CLIENT WILL EXPRESS AN INCREASE IN PSYCHOLOGICAL COMFORT AND DEMONSTRATE THE USE OF EFFECTIVE COPING MECHANISM
Interventions Rationales
Remain with the client during acute episodes of breathing difficulty and provide care in a calm reassuring mannerProvide a quiet calm environmentDuring acute episodes open doors and curtains and limit of people and unnecessary equip in the room Provide a fan if the client perceives a benefit from the moving airEncourage the use of breathing retraining and relaxation techniquesGive sedatives and tranquilizers with extreme caution Nonpharmaceutical methods of anxiety reduction are more useful
Reassures the client that competent help is available if needed Anxiety can be contagious remain calmReduction or external stimuli helps promote relaxationEnvironmental changes may lessen the clientrsquos perceptions of suffocationA feeling of self-control and success in facilitating breathing helps reduce anxietyOversedation may cause respiratory depression
Evaluation Anxiety can usu Be controlled quickly but may recur with each episode of dyspnea and requires both short-term and long-term interventions
DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

DISTURBED SLEEP PATTERN RT DYSPNEA AND EXTERNAL STIMULIOUTCOME THE CLIENT WILL REPORT FEELING ADEQUATELY RESTED
Intervention Rationales
oPromote relaxation by providing a darkened quiet environment ensuring adequate room ventilation and following bedtime routinesoSchedule care activities to allow periods of uninterrupted sleepoAvoid the use of sleeping pillsoInstruct the client in measures to promote sleepa Avoid stimulants such as caffeineb Maintain a consistent bedtime and
a regular bedtime routine Etc
oThe hospital environment ca interfere with relaxation and sleep Using established bedtime rituals increases relaxationoFor most people completing four to five complete sleep cycles (60to90minutes) per night promote a feeling of being restedoMany forms of hypnotics sedatives and barbiturates impair sleep cyclesa Activity increases the need for
sleep and contributes to a feeling of tiredness
b Stimulants increase metabolism and inhibit relaxation
Evaluation During acute respiratory problems sleep may be difficult because of interruptions and dyspnea Short-term outcomes such as napping may be accomplishable Long-term plans for sleep may have to be deferred until dsypnea is controlled
Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Io Ineffective breathing pattern
related toshortness of breath
mucus
bronchoconstriction
airway irritants
Impaired gas exchange
related toventilation perfusion inequality
Imbalanced Nutrition less than body requirements
related toanorexia
Bathing Hygiene Self-care deficit
related tofatigue secondary to increased respiratory effort and ventilation and oxygenation insufficiency
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
Anxietyrelated tothreat to self-conceptthreat of deathpurposes that are not being met
Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Disturbed sleep pattern
related todiscomfortsleeping position Deficient Knowledge
related tolack of informationdo not know the source of information
Ineffective individual coping
related tolack of socializationanxietydepressionlow activity levels and an inability to work
NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

NURSING MANAGEMENT INTERVENTIONS
1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

1 Advice the elimination of smoking and other external irritants such as dust
2 Supervise the clientrsquos respiratory exercise such as pursed lips
3 Teach the proper use of a nebulizer and other special equipments
4 Carefully observe for symptoms of CO2 intoxication (CO2 narcosis) if O2 is being administer
5 Teach the client to adjust hisher activities to avoid over exertion
6 Teach the client to avoid people with respiratory infections
7 Teach the client to avoid the use sedatives of hypnotics which could compromise hisher respirations
8 Teach the client to maintain the highest resistance possible by getting adequate rest eating nutrious
9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

9 Provide nursing care for the client with chronic bronchitis or emphysema
- Administer prescribed medications which may include antibiotics broncodilators mucolytic agents and corticosteroids
-Antibiotics should be administered at the first sign of infection such as change in sputum Opioids sedatives and tranquilizers which can further depress respirations should be avoided
- Clear airways with postural drainage percussion or vibrating and suctioning as appropriate
- Promote infection control Encourage the client to obtain influenza and pneumonia vaccines at prescribed times
- Improve breathing patterns Demonstrate and encourage diaphragmatic and purse lip breathing Have the client take a deep breath and blow out against closed lips
- Administer oxygen A low arterial oxygen level is the clientrsquos primary drive for breathing Oxygen flow rate should be no more than 2 to 3 L per minute Higher levels will cause the client to quit breathing
-Discuss the importance of smoking cessation and avoiding second-hand smoke Discuss ways to quit smoking and make appropriate referrals Compromise is not acceptable the client must stop smoking
10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

10PROVIDE NURSING CARE FOR THE CLIENT WITH ASTHMA
- ADMINISTER PRESCRIBED MEDICATIONS WHICH MAY INCLUDE ADRENERGICS BRONCHODILATORS AND CORTICOSTEROIDS FOR ACUTE ATTACK ENCOURAGE USE OF A CROMOLYN INHALER AS PROPHYLACTIC TREATMENT
-PROVIDE TREATMENT DURING AN ACUTE ASTHMATIC ATTACK STAY WITH THE CLIENT AND KEEP HIM CALM AND IN AN UPRIGHT POSITION DO PURSE-LIP BREATHING WITH THE CLIENT ENCOURAGE RELAXATION TECHNIQUES
-IMPLEMENT MEASURES TO PREVENT ASTHMATIC ATTACKS TEACH THE CLIENT WITH THE FOLLOWING SKILLS (1) IDENTIFY AND ELIMINATE OR MINIMIZE EXPOSURE TO PULMONARY IRRITANTS (2) REMOVE RUGS AND CURTAINS FROM THE HOME CHANGE AIR FILTERS FREQUENTLY KEEP THE HOME AS DUST FREE AS POSSIBLE AND KEEP WINDOWS CLOSED DURING WINDY AND HIGH POLLEN DAYS
-USE AN INHALER AND TAKE MEDICATIONS AS PRESCRIBED AND NOTIFY THE HEALTH CARE PROVIDER WHEN NOT GAINING COMPLETE RELIEF
-NOTIFY THE HEALTH CARE PROVIDER WHEN A RESPIRATORY INFECTION OCCURS
-OBTAIN INFLUENZA AND PNEUMONIA VACCINES AT PRESCRIBED TIMES
TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

TREATMENT
BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

BRONCHODILATORS
Bronchodilators are medications that relax the muscles of the airways to help keep them open and make it easier to breathe Anticholinergics a type of bronchodilator are often used by people with COPD Short-acting bronchodilators last about four to six hours and are used on an as-needed basis Longer-acting bronchodilators can be used every day for people with more persistent symptoms People with COPD may use both types of bronchodilators
SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

SHORT-ACTING BRONCHODILATORS INCLUDE ALBUTEROL (PROAIR HFA VENTOLIN HFA OTHERS) LEVALBUTEROL (XOPENEX) AND IPRATROPIUM (ATROVENT)
THE LONG-ACTING BRONCHODILATORS INCLUDE TIOTROPIUM (SPIRIVA) SALMETEROL (SEREVENT) FORMOTEROL (FORADIL PERFOROMIST) ARFORMOTEROL (BROVANA) INDACATEROL (ARCAPTA) AND ACLIDINIUM (TUDORZA)
Depending on the severity of your disease you may need a short-acting bronchodilator before activities a long-acting bronchodilator that you use every day or both
CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

CORTICOSTEROIDS If bronchodilators dont provide enough relief people with COPD may take corticosteroids These are usually taken by inhaler They may reduce inflammation in the airways Steroids may also be given by pill or injection to treat flare-ups of COPD
INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

INHALED STEROIDS INHALED CORTICOSTEROID MEDICATIONS CAN REDUCE AIRWAY INFLAMMATION AND HELP PREVENT EXACERBATIONS
SIDE EFFECTS MAY INCLUDE BRUISING ORAL INFECTIONS AND HOARSENESS
THESE MEDICATIONS ARE USEFUL FOR PEOPLE WITH FREQUENT EXACERBATIONS OF COPD FLUTICASONE (FLOVENT) AND BUDESONIDE (PULMICORT) ARE EXAMPLES OF INHALED STEROIDS
COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

COMBINATION INHALERS
SOME MEDICATIONS COMBINE BRONCHODILATORS AND INHALED STEROIDS
SALMETEROL AND FLUTICASONE (ADVAIR) AND FORMOTEROL AND BUDESONIDE (SYMBICORT) ARE EXAMPLES OF COMBINATION INHALERS
ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

ORAL STEROIDS
FOR PEOPLE WHO HAVE A MODERATE OR SEVERE ACUTE EXACERBATION ORAL STEROIDS PREVENT FURTHER WORSENING OF COPD HOWEVER THESE MEDICATIONS CAN HAVE SERIOUS SIDE EFFECTS SUCH AS WEIGHT GAIN DIABETES OSTEOPOROSIS CATARACTS AND AN INCREASED RISK OF INFECTION
ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

ANTIBIOTICS
People with COPD are at greater risk for lung infections than healthy people If your cough and shortness of breath get worse or you develop fever talk to your doctor These are signs that a lung infection may be taking hold and your doctor may prescribe medications to help knock it out as quickly as possible You may also need adjustments to your COPD regimen
ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

ANTIBIOTICS RESPIRATORY INFECTIONS SUCH AS ACUTE BRONCHITIS PNEUMONIA AND INFLUENZA CAN AGGRAVATE COPD SYMPTOMS ANTIBIOTICS HELP FIGHT ACUTE EXACERBATIONS THE ANTIBIOTIC AZITHROMYCIN PREVENTS EXACERBATIONS BUT IT ISNT CLEAR WHETHER THIS IS DUE TO ITS ANTIBIOTIC EFFECT OR ITS ANTI-INFLAMMATORY PROPERTIES
SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

SURGERY
A small number of people with COPD may benefit from surgery Bullectomy and lung volume reduction surgery remove the diseased parts of the lung allowing the healthy tissue to perform better and making breathing easier
A lung transplant may help some people with the most severe COPD who have lung failure but it can have serious complications such as organ rejection and the need for lifelong immune-suppressing medications
EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

EXERCISE
Walking is one of the best things you can do if you have COPD Start with just five or 10 minutes at a time three to five days a week If you can walk without stopping to rest add another minute or two Even if you have severe COPD you may be able to reach 30 minutes of walking at a time Use your oxygen while exercising if you are on oxygen therapy Discuss your exercise plans with your doctor
HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

HOW QUITTING SMOKING HELPS
SMOKERS WITH COPD WILL LOSE LUNG FUNCTION MORE QUICKLY TOBACCO SMOKE DESTROYS THE TINY HAIR-LIKE CILIA THAT NORMALLY REPAIR AND CLEAN THE AIRWAYS -- AND HARMS THE LUNGS IN OTHER WAYS TOO QUITTING WILL SLOW OR STOP THE DAMAGE AND IS SIMPLY THE MOST IMPORTANT STEP YOU CAN TAKE FOR COPD YOULL ALSO GET THE OTHER BENEFITS OF QUITTING FOODS TASTE BETTER AND YOUR BLOOD PRESSURE AND HEART RATE LOWER TO HEALTHIER LEVELS
DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

DIET
A HEALTHY DIET IS IMPORTANT FOR PEOPLE WITH COPD BEING OVERWEIGHT CAN MAKE IT HARDER TO BREATHE AND BEING UNDERWEIGHT CAN MAKE YOU WEAK TALK TO YOUR DOCTOR ABOUT THE BEST EATING PLAN FOR YOU COMMON GUIDELINES INCLUDEDRINK 6-8 GLASSES OF WATER OR NON-CAFFEINATED BEVERAGES DAILYEAT HIGH-FIBER FOODS SUCH AS WHOLE GRAIN BREAD BRAN AND FRESH FRUIT
DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

DISCHARGE PLANNING
Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-

Spirometer should be measured in all patients before discharge
Patients should be re-established on their optimal maintenance bronchodilator therapy before discharge
Patients who have had an episode of respiratory failure should have satisfactory oximetry or arterial blood gas results before discharge
All aspects of the routine care that patients receive(including appropriateness and risk of side effects) should be assessed before discharge
Patients (or home carers) should be given appropriate information to enable them to fully understand the correct use of medications including oxygen before discharge
Arrangements for follow-up and home care (such as visiting nurse oxygen delivery referral for other support) should be made before discharge
Before the patient is discharged the patient family and physician should be confident that he or she can manage successfully When there is remaining doubt a formal activities of daily living assessment may be helpful
- CHRONIC OBSTRUCTIVE PULMONARY DISEASE
- Slide 2
- Etiology and risk factors
- Slide 4
- There are four main forms of copd
- Asthma
- Slide 7
- Status asthmaticus
- Etiology and risk factors (2)
- Asthma occurs in families which suggests that it is an inheri
- Substances that trigger asthma
- Signs and symptoms
- Slide 13
- Poorly controlled asthma leads to
- What you do if you have asthma
- Physical assessment
- Medical history
- Physical exam
- Diagnostic and laboratory examination
- Slide 20
- Slide 21
- Slide 22
- Nursing Diagnosis
- Ineffective breathing pattern
- interventions
- Ineffective airway clearance
- interventions (2)
- Nursing Management
- Slide 29
- Pharmacological actions
- Slide 31
- albuterol and ipratropium inhaler BRAND NAME Combivent Combi
- albuterol Ventolin Proventil Proventil-HFA AccuNeb Vospir
- Slide 34
- GENERIC NAME zafirlukast BRAND NAME Accolate
- Slide 36
- Slide 37
- Bronchitis
- BRONCHITIS
- Slide 40
- Slide 41
- Slide 42
- Risk factors and SignampSymptoms
- Slide 44
- Slide 45
- Pharmacologic action
- GENERIC NAME ofloxacin BRAND NAME Floxin (discontinued brand)
- Slide 48
- Slide 49
- emphysema
- Slide 51
- Slide 52
- 3 Types of Emphysema
- Centriacinar or Centrilobular Emphysema
- Panacinar Emphysema
- Paraseptal Emphysema
- Slide 57
- Risk Factors
- Slide 59
- Signs and Symptoms
- Slide 61
- Slide 62
- Physical assessment (2)
- Slide 64
- Laboratory exam
- Slide 66
- Slide 67
- Slide 68
- Slide 69
- Pathophysiology
- Slide 71
- Slide 72
- Primary Nursing Diagnosis Impaired gas exchange related to
- Medical Management
- Slide 75
- Medications
- Slide 77
- Slide 78
- Nursing Interventions
- Slide 80
- Slide 81
- Discharge Planning
- Slide 83
- Bronchiectasis
- Slide 85
- Slide 86
- Slide 87
- Slide 88
- Signs and Symptoms (2)
- Slide 90
- Diagnosis
- Slide 92
- Treatment
- Slide 94
- Slide 95
- Causes of COPD About 90 of people with COPD are current or
- Risk Factors Causes
- Signs and Symptoms Inside the lungs COPD can clog the airways
- Slide 99
- PHYSICAL ASSESSMENT
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal
- Slide 102
- PhysicalExam First your doctor will listen to your chest as
- Medical Chart Review
- Extremities Inspection
- Pulmonary Exam bull Inspection (chest shape and symmetry) bull Pal (2)
- Spirometry Breath Test
- Chest X-Ray
- Peak flow test
- Computerized Tomography (CT) scan
- PATHOPHYSIOLOGY
- PATHOPHYSIO
- NURSING DIAGNOSIS
- Slide 114
- Interventions
- anxiety related to acute breathing difficulties and fear of su
- disturbed sleep pattern rt dyspnea and external stimuli Outc
- I
- Slide 119
- NURSING MANAGEMENT INTERVENTIONS
- Slide 121
- Slide 122
- 10Provide nursing care for the client with asthma - Adminis
- TREATMENT
- Bronchodilators
- Short-acting bronchodilators include albuterol (ProAir HFA
- Corticosteroids
- Inhaled steroids Inhaled corticosteroid medications can reduc
- Combination inhalers Some medications combine bronchodilator
- Oral steroids For people who have a moderate or severe acute
- Antibiotics
- Antibiotics Respiratory infections such as acute bronchitis
- Surgery
- Exercise
- How Quitting Smoking Helps Smokers with COPD will lose lung fu
- Diet A healthy diet is important for people with COPD Being
- DISCHARGE PLANNING
- Slide 138
-