Consensus Statement on the Classification and Terminology of Neck Dissection.pdf
description
Transcript of Consensus Statement on the Classification and Terminology of Neck Dissection.pdf

ORIGINAL ARTICLE
Consensus Statement on the Classificationand Terminology of Neck DissectionK. Thomas Robbins, MD; Ashok R. Shaha, MD; Jesus E. Medina, MD; Joseph A. Califano, MD;Gregory T. Wolf, MD; Alfio Ferlito, MD; Peter M. Som, MD; Terry A. Day, MD;for the Committee for Neck Dissection Classification, American Head and Neck Society
Objective: To update the guidelines for neck dissec-tion terminology, as previously recommended by theAmerican Head and Neck Society.
Participants: Committee for Neck Dissection Classifi-cation, American Head and Neck Society; representa-tion from the Committee for Head and Neck Surgery andOncology, American Academy of Otolaryngology–Headand Neck Surgery (T.A.D.).
Evidence: Review of current literature on neck dissec-tion classification.
Consensus Process: Semiannual face-to-face meet-ings of the Committee for Neck Dissection Terminol-ogy and e-mail correspondence.
Conclusions: Standardization of terminology for neck dis-section is important for communication among cliniciansand researchers. New recommendations have been maderegarding the following: boundaries between levels I andII and between levels III/IV and VI; terminology of the su-perior mediastinal nodes; and the method of submittingsurgical specimens for pathologic analysis.
Arch Otolaryngol Head Neck Surg. 2008;134(5):536-538
T HE AMERICAN HEAD ANDNeck Society (AHNS), in co-operation with the Commit-tee for Head and Neck Sur-gery and Oncology of the
American Academy of Otolaryngology–Head and Neck Surgery, has made recom-mendations for neck dissection classifica-tion over the past 2 decades.1,2 The currentsystem has been accepted widely, thus al-lowing data to be reported without ambi-guity and promoting an ease of communi-cation among health care providers whotreat patients with head and neck cancer.
In the later publication,2 the recom-mendedmodificationswere intendedtoaddrefinements totheoriginalsystem.Includedwas the use of the hyoid bone and the cri-coidcartilageasmarkerstodefinethebound-arybetweenlevelsIIandIIIandlevelsIIIandIV, respectively, to allow radiologists to ac-curately localize nodal lesions within thedefined levels of the neck. Another modi-fication was to identify and define theboundaries of subzones in levels I, II, andV in response to the increasing awarenessof specific sublevels having lower or higherrisk for nodal metastases within a sublevelcomparedwiththeremainingregionwithinthe same zone. This change was intended
toheightenawarenessof thenuancesof thepatterns of lymph node metastases basedon the site of disease origin and to refinetreatment accordingly.
The third modification was intended toencourage a more uniform terminology forselective neck dissection, one that more ac-curately represents the specific levels of neckcontents removed. For example, in the caseof a patient with a T2N0 squamous cell car-cinoma located on the lateral border of theoral surface of the tongue who was under-going surgery to remove sublevels IB andIIA and levels III and IV, clinicians were en-couraged to define the neck dissection pro-cedure as selective neck dissection (sublevelsIB and IIA and levels III and IV). While thecommittee members recognized the term ex-tended supraomohyoid neck dissection as thetraditional name, there was agreement thatit was less precise than the definition by lev-els and sublevels. Similarly, in the case of apatient with a T1N0 squamous cell carci-noma of the supraglottic larynx who was un-dergoing an endoscopic resection and neckdissection to remove sublevel IIA and levelIII on each side, the recommended term forthis lymphadenectomy would be bilateralselective neck dissection (sublevel IIA and levelIII) rather than bilateral lateral neck dissec-tion. Practitioners were encouraged to usethe term selective neck dissection with spe-cific notation of the levels or sublevels re-moved and to rely less on historical termsthat were less precise.
CME available online atwww.jamaarchivescme.comand questions on page 469
Author Affiliations are listed atthe end of this article.Group Information:Drs Robbins, Shaha, Medina,Califano, Wolf, Ferlito, Som,and Day comprise theCommittee for Neck DissectionClassification, American Headand Neck Society.
(REPRINTED) ARCH OTOLARYNGOL HEAD NECK SURG/ VOL 134 (NO. 5), MAY 2008 WWW.ARCHOTO.COM536
©2008 American Medical Association. All rights reserved.Downloaded From: http://jamanetwork.net/ on 10/28/2013

The Neck Dissection Classification Committee of theAHNS has continued to review issues of terminology anddefinitions in several meetings over the past 3 years to ad-dress perceived shortcomings of the current system. Herein,we summarize some of the changes agreed on by generalconsensus among the members, and we encourage our col-leagues to adopt these additional modifications.
ALTERNATE NOMENCLATUREFOR THE RADICAL AND
MODIFIED RADICAL NECK DISSECTION
A recent proposal by the Japan Neck Dissection StudyGroup is to use the term total neck dissection when all 5levels are removed and the term selective neck dissectionwhen fewer than 5 levels are removed.3 The AHNS hasaccepted the terms radical neck dissection and modifiedradical neck dissection when all 5 levels are removed.However, we realize that the terms are more cumber-some than what the Japanese have proposed. Otherterms such as comprehensive neck dissection or even fullneck dissection are also less cumbersome. While we donot endorse any term, we strongly recommend that theintroduction of an alternate name for radical neck dis-section or modified radical neck dissection should pre-cisely describe the procedure to avoid any potential formisinterpretation. Also, the new term should include aclear denotation of nonlymphatic structures, as isimplied by the traditional terms radical neck dissectionand modified radical neck dissection.
REDEFINING THE BOUNDARYBETWEEN SUBLEVELS IB AND IIA
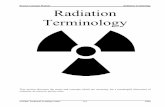
Currently, theboundarythatseparatessublevel IBfromsub-level IIA is defined as the border of the stylohyoid muscle.While this anatomic landmark can be recognized during aneck dissection procedure, it is not a very practical markerduring clinical examination, nor can it be identified by theradiologist on imaging studies.4 Therefore, based on con-sultationswithourradiologycolleagues,weproposeadopt-ingtheirrecommendationforanalternativeborderbetweenlevels I and II: the vertical plane defined by the posterioredge of the submandibular gland (Figure). For the radi-ologist, lymph nodes that lie anterior (or medial) to thisplane are defined as occupying level I, whereas those ly-ingposterior (or lateral) to it aredefinedasoccupying levelII. In the case of nodes that transgress this plane, the de-termination will be based on whether more than half ofthe node volume is located medial or lateral to the plane.While this system may occasionally result in the identi-fication of a postglandular node being categorized tosublevel IIA rather than sublevel IB, the frequency of thissituation is likely to be low and far outweighed by the ad-vantage of being compatible for radiological interpreta-tion. From the viewpoint of the surgeon removing levelII while preserving level I, the dissection plane typicallyused to separate the 2 levels is along the fascia overlyingthe posterior aspect of the submandibular gland.
INCORPORATING A RADIOLOGIC LANDMARKTO SEPARATE LEVELS III AND IV FROM LEVEL VI
Theanatomicboundary that separates themedialborderoflevels III and IV from the lateral border of level VI has tra-ditionallybeenthe lateralborderof thesternohyoidmuscle.However, this is not a landmark that radiologists can dis-cerneasily.Therefore,basedontherecommendationsofourconsultingradiologist (P.M.S.),weagree that themedial as-pectof thecommoncarotidartery is anacceptablealternatelandmark for separating these levelswhenviewing theneckin an axial plane, as is the case with computed tomographyandmagneticresonanceimagingevaluation.Intraoperatively,surgeons may still want to use the border of the sterno-hyoid muscle to define the medial extent of the neck dis-section when removing levels III and IV because the tar-geted nodes are usually more superficial to the carotidartery, which is often not exposed in the operative field.
DEFINING LYMPH NODE GROUPSLOCATED OUTSIDE THE TRADITIONALBOUNDARIES OF NECK DISSECTION,
WITH PARTICULAR REFERENCETO THE SUPERIOR MEDIASTINAL NODES
The traditional boundaries of the radical neck dissectionencompass levels I through V. However, the original de-scription of the level system by the surgeons at MemorialHospital in New York also included levels VI and VII.5 TheNeck Dissection Classification Committee of the AHNS pre-viously recommended the use of level VI to define the an-terior central compartment of the neck but did not recom-mend the use of level VII because it defined a region outside
IIB
III
IV
VII
VI
VB
VA
IIAIB
IA
Figure. Anatomic diagram of the neck depicting the boundaries of the 6 necklevels and 3 neck sublevels.
(REPRINTED) ARCH OTOLARYNGOL HEAD NECK SURG/ VOL 134 (NO. 5), MAY 2008 WWW.ARCHOTO.COM537
©2008 American Medical Association. All rights reserved.Downloaded From: http://jamanetwork.net/ on 10/28/2013

the typical boundaries of the neck. The committee be-lieved that lymph node groups located outside the bound-aries of the neck should be denoted by the anatomic nameused for the group. This policy was intended to discour-age the use of many new levels to define other lymph nodegroups and avoid a more complex number system. How-ever, the use of level VII in many publications continues tobe the preferred method for delineating nodes as the su-perior mediastinal group. In essence, most of these nodesrepresent an extension of the paratracheal lymph node chainextending inferiorly below the suprasternal notch along eachside of the cervical trachea to the level of the innominateartery. However, some superior mediastinal nodes ex-tend below the innominate artery to the level of the aor-tic arch. Removal of such nodes usually requires a trans-manubrial approach, whereas the typical case of superiormediastinal lymphadenopathy can be managed througha cervical approach only. Therefore, we recommend thatif the term level VII is to be used, it should refer to theextension of the chain of paratracheal nodes below thesuprasternal notch (the dividing line between levels VIand VII) to the level of the innominate artery only. Al-ternatively, these nodes might be defined as the superiormediastinal lymph nodes above the level of the innomi-nate artery.
SUBMITTING THE NECK DISSECTIONSPECIMEN FOR PATHOLOGIC ANALYSIS
The physician must be aware of the presence and extentof cancer involving the regional lymph nodes to deter-mine whether ancillary treatment is necessary. Therefore,the surgical specimen should be submitted to the patholo-gist in the manner most appropriate to determine the maxi-mum amount of information, including the total numberof lymph nodes in each level and sublevel, the number oflymph nodes with evidence of metastases, and whether thereis any evidence of extracapsular extension. Therefore, werecommend that the neck dissection specimen be dividedinto levels and sublevels by the surgeon while in the op-erating room immediately after the specimen is removedfrom the patient. This should be done on a separate backtable using instruments that will no longer be used in theoperative procedure. To minimize the risk of the patholo-gist and the processing team identifying the neck levels in-correctly, we strongly recommend that each neck level besubmitted to the laboratory in separate containers and care-fully labeled by the staff in the operating room under thedirect supervision of the surgeon. When possible, all ofthe sublevels that are removed should be submitted inseparate containers as well. In current surgical practice,most neck dissections are of the selective type, and speci-mens typically lack anatomic landmarks that histori-cally allowed pathologists to orient specimens; there-fore, we believe that this exercise of separating and labelingthe neck contents by each level and sublevel is of para-mount importance.
CONCLUSIONS
The Neck Dissection Committee of the AHNS will con-tinue to review and recommend modifications for neck dis-
section terminology and classification. The changes out-lined herein represent a consensus among a working groupthat has kept abreast of the emerging concepts and modi-fications being promoted worldwide. We believe that ourcommittee has responded to the changes in a manner thatacknowledges progress while maintaining consistency andrespect for the existing culture of communication. We be-lieve that our role in analyzing and responding to suchchanges will continue as new discoveries are made and al-ternative approaches developed.
Submitted for Publication: June 6, 2007; final revisionreceived August 21, 2007; accepted August 28, 2007.Author Affiliations: Division of Otolaryngology, South-ern Illinois University School of Medicine, Springfield (DrRobbins); Head and Neck Service, Memorial Sloan-Kettering Cancer Center, New York, New York (Dr Shaha);Department of Otolaryngology, University of OklahomaHealth Sciences Center, Oklahoma City (Dr Medina); De-partment of Otolaryngology–Head and Neck Surgery, JohnsHopkins University School of Medicine, Baltimore, Mary-land (Dr Califano); Department of Otolaryngology–Headand Neck Surgery, University of Michigan, Ann Arbor (DrWolf); Department of Surgical Sciences, Otorhinolaryn-gologic Clinic, University of Udine, Udine, Italy (Dr Fer-lito); Department of Radiology, Mount Sinai Medical Cen-ter, New York, New York (Dr Som); and Department ofOtolaryngology–Head and Neck Surgery, Medical Uni-versity of South Carolina, Charleston (Dr Day).Correspondence: K. Thomas Robbins, MD, SimmonsCoo-per Cancer Institute, Southern Illinois University Schoolof Medicine, PO Box 19677, Springfield, IL 62794-9677([email protected]).Author Contributions: Dr Robbins had full access to allthe data in the study and takes responsibility for the in-tegrity of the data and the accuracy of the data analysis.Study concept and design: Robbins, Medina, Califano, andDay. Analysis and interpretation of data: Shaha, Califano,Wolf, Ferlito, and Som. Drafting of the manuscript:Robbins, Califano, Som, and Day. Critical revision of themanuscript for important intellectual content: Shaha,Medina, Califano, Wolf, and Ferlito. Administrative, tech-nical, and material support: Robbins and Califano. Studysupervision: Robbins, Wolf, Ferlito, Som, and Day. De-velopment of Consensus: Shaha.Financial Disclosure: None reported.
REFERENCES
1. Robbins KT, Medina JE, Wolfe GT, Levine PA, Sessions RB, Pruet CW. Standard-izing neck dissection terminology: official report of the Academy’s Committee forHead and Neck Surgery and Oncology. Arch Otolaryngol Head Neck Surg. 1991;117(6):601-605.
2. Robbins KT, Clayman G, Levine PA, et al. Neck dissection classification update:revisions proposed by the American Head and Neck Society and the American Acad-emy of Otolaryngology–Head and Neck Surgery. Arch Otolaryngol Head Neck Surg.2002;128(7):751-758.
3. Hasegawa Y, Saikawa M, Hayasaki K, et al. A new classification and nomencla-ture system for neck dissections: a proposal by the Japan Neck Dissection StudyGroup. Jpn J Head Neck Cancer. 2005;31(1):71-78.
4. Som PM, Curtin HD, Mancuso AA. Imaging-based nodal classification for evalu-ation of neck metastatic adenopathy. AJR Am J Roentgenol. 2000;174(3):837-844.
5. Shah JP, Strong E, Spiro RH, Vikram B. Surgical grand rounds: neck dissection:current status and future possibilities. Clin Bull. 1981;11(1):25-33.
(REPRINTED) ARCH OTOLARYNGOL HEAD NECK SURG/ VOL 134 (NO. 5), MAY 2008 WWW.ARCHOTO.COM538
©2008 American Medical Association. All rights reserved.Downloaded From: http://jamanetwork.net/ on 10/28/2013