Congestive Heart Failure 01
-
Upload
matrixtrinity -
Category
Documents
-
view
214 -
download
0
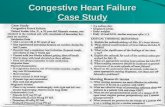
Transcript of Congestive Heart Failure 01
-
8/11/2019 Congestive Heart Failure 01
1/27
CONGESTIVE HEART
FAILURE
Minerva A. Cobus
-
8/11/2019 Congestive Heart Failure 01
2/27
CONGESTIVE HEART FAILURE
Is the inability of the heart to maintain an
adequate output of blood from one or
more ventricles resulting to an inadequatesupply of blood to the vital parts of the
body.
-
8/11/2019 Congestive Heart Failure 01
3/27
TYPES OF CHF
LEFT-SIDED CHFUSUALLY
PULMONARY BY NATURE
RIGHT SIDED CHFUSUALLY AFFECTS
THE PERIPHERY IN GENERAL
-
8/11/2019 Congestive Heart Failure 01
4/27
CAUSES
Coronary Artery Disease
Faulty Heart Valves
Cardiomyopathy
Congenital Heart Defects
Heart Arrhythmias
Kidney Failure
Hypertension (or related increase in BV)
-
8/11/2019 Congestive Heart Failure 01
5/27
CAUSES
Pulmonary Emboli
Rheumatic heart
disease Cor pulmonale
anemia
Arrhythmias
Rupture of papillary
muscle Bacterial endocarditis
-
8/11/2019 Congestive Heart Failure 01
6/27
PATHWAY OF BLOOD OXYGENATION
IN THE HEART
-
8/11/2019 Congestive Heart Failure 01
7/27
Pathology of Ventricular Failure
Systolic failure: causes ventricle not toempty properly (most common cause of
CHF) Heart muscle has decreased ability to
contract
Also caused by increased afterload
(hypertension), or mechanical abnormalities (like valvular heart disease)
Characterized by low forward blood flow
-
8/11/2019 Congestive Heart Failure 01
8/27
Pathology of Ventricular Failure
Diastolic failure: causes ventricle not to fillproperly
Disorder of heart relaxation and ventricularfilling
Usually the result of ventricular hypertrophy
Caused by chronic hypertension, aortic
stenosis, or cardiomyopathy Commonly seen in older adults
-
8/11/2019 Congestive Heart Failure 01
9/27
-
8/11/2019 Congestive Heart Failure 01
10/27
SIGNS AND SYMPTOMS
Fatigue and weakness
Shortness of breath (dyspnea) when you
exert yourself or when you lie down Persistent wheezing or cough with white
or pink blood-tinged phlegm
Pronounced neck veins Swelling (edema) in your legs, ankles and
feet
-
8/11/2019 Congestive Heart Failure 01
11/27
SIGNS AND SYMPTOMS
Swelling of your abdomen
Rapid weight gain from fluid retention
Lack of appetite and nausea Lightheadedness, dizzy spells or fainting
spells
Difficulty concentrating or decreasedalertness
Irregular or rapid heartbeat
-
8/11/2019 Congestive Heart Failure 01
12/27
Compensatory Mechanisms of the
heart in CHF
Increased
sympathetic nervous
system stimulation
Ventricular
hypertrophy
Hormonal response(Renal response)
-
8/11/2019 Congestive Heart Failure 01
13/27
Risk Factors for CHF
Coronary artery
disease
Hypertension
High cholesterol
levels
Advancing age
Cigarette smoking
Obesity
Proteinuria
Diabetes
Prolonged kidney
problems
-
8/11/2019 Congestive Heart Failure 01
14/27
Complications of Congestive Heart
Failure
Pleural effusion
Increased pressure in pleural capillaries
Leakage of fluid from capillaries into pleural space. Arrhythmias
Left ventricular thrombus
Hepatomegaly
Liver becomes congested with venous blood
Leads to impaired liver function
-
8/11/2019 Congestive Heart Failure 01
15/27
-
8/11/2019 Congestive Heart Failure 01
16/27
Nursing Care in Acute CHF
Decrease the intravascular volume With use of diuretics
Decrease the venous return Reduces congestion in heart and lungs
Sitting patient up facilitates breathing
Decreasing the afterload
Use of vasodilators (IV Nipride) Increasing myocardial contraction and CO
Reducing pulmonary congestion
-
8/11/2019 Congestive Heart Failure 01
17/27
Nursing Care of Acute CHF
Improve Gas Exchange and Oxygenation
Give IV morphine
Place on Oxygen Intubate and place on vent as needed
Improve cardiac function
Digitalis, or newer inotropic drugs (dobutamine)
increase cardiac contractility Hemodynamic monitoring
-
8/11/2019 Congestive Heart Failure 01
18/27
Nursing Care of Acute CHF
Reduce anxiety
Give Morphine
Approach patient calmly
Remember: Nursing care will focus on continual
physical assessment of the patient,
hemodynamic monitoring, and monitoring thepatients response to the treatment.
-
8/11/2019 Congestive Heart Failure 01
19/27
MANAGEMENTDigitalis Therapy
The major therapy for CHF
(+) inotropic, (-) chronotropic effects
Nsg. Implication: check for HR below 60and above 120
Monitor serum potassium (Normal3.5-5.5 mEq/L)
Examples: Lanoxin (Digoxin), Crystodigin(Digitoxin), Lanatoside (Cedilanid C),Deslanoside (Cedilanid D)
-
8/11/2019 Congestive Heart Failure 01
20/27
Beware of Digitalis Toxicity!!!
Bradycardia
G.I. Manifestations: Anorexia, N & V,
vomiting
Dysrythmias (most dangerous)
Yellow / green visions; halos around
the light among the elderly)
In males: gynecomastia, decreasedlibido and impotence
-
8/11/2019 Congestive Heart Failure 01
21/27
DIURETIC THERAPY
To decrease cardiac workload by reducingcirculating BV
Nsg. Implications:
a. Assess for s/sx of hypokalemia when givingthiazides and loop diuretics
b. Give potassium supplements
c. Best given early AM or early PM If thiazides are ineffective, a potassium sparing
diuretic may be given.
-
8/11/2019 Congestive Heart Failure 01
22/27
Examples of Diuretics:
1. ThiazidesChlorthiazide (Diuril),
Hyrochlorthiazide (Esixdrix, Hyrdodiuril)
2. Loop DiureticsFurosemide (Lasix),
Bumetamide (Burmex)
3. Potassim-sparingSpironolactone(Aldactone), Triamterene (Dyrenium)
-
8/11/2019 Congestive Heart Failure 01
23/27
VASODILATORS
Decreases resistance to ventricular emptying,thereby decreasing afterload.
Most commonly used as follows:
1. Nitroprusside (Nipride)
2. Hydralazine (Apresoline)
3. Nifedipine (a Calcium-channel blocker with
vasodilator effect)4. Captopril (an antihypertensive agent with
vasodilator effect)
-
8/11/2019 Congestive Heart Failure 01
24/27
Nursing Care of Chronic CHF
Angiotensin-converting enzyme (Ace) inhibitors:
Capoten, Vasotec, lisinopril (Prinivil, Zestril)
Reduces angiotension II and plasma aldosteronelevels
Increases cardiac output due to vasodilitation
Beta-adrenergic blocking agents:
Coreg (is the only beta-blocker used in mild tomoderate CHF)
-
8/11/2019 Congestive Heart Failure 01
25/27
Nursing Care of Chronic CHF
Nutritional Therapy
Sodium restriction with diet
Teach patient what foods are high in sodium and toavoid them
Severe CHF has the most sodium restrictive diet
instruct family in reading labels on food items
Fluids may be restricted in moderate to severe CHF
-
8/11/2019 Congestive Heart Failure 01
26/27
TREATMENT
Activity: Balanced program of activity and
rest
Oxygen therapy
Limit fats and cholesterol
Stop smoking
-
8/11/2019 Congestive Heart Failure 01
27/27
NURSING MANAGEMENT
Provide oxygenation
Promote rest and activity
Decrease anxiety Facilitate fluid balance
Provide skin care
Promote nutrition Promote elimination
Facilitate learning