Congestive cardiac Failure
-
Upload
anishkumar123 -
Category
Health & Medicine
-
view
2.170 -
download
4
Transcript of Congestive cardiac Failure

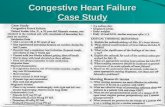
Congestive Heart Failure
Presented To : Dr. AbelPresented By : Anish Kumar. KRajiv Gandhi University Of Science and TechnologyClinical Rotation :Internal MedicineDate:2015/10/27

Results from any structural or functional abnormality that impairs the ability of the heart to eject blood (Systolic Heart Failure) or to fill with blood (Diastolic Heart Failure). Heart's pumping power is weaker than normal.
With heart failure , blood moves through the heart and body at a slower rate, and pressure in the heart increases. As a result, the heart cannot pump enough oxygen and nutrients to meet the body's needs.
Congestive Heart Failure (CHF)Congestive Cardiac Failure(CCF)Heart Failure (HF)

Congestive Heart FailureHeart Failure can divided: - Right Sided Heart Failure - Left Sided Heart Failure
Can be Either From,Diastolic Dysfunction(Inability to relax)Systolic Dysfunction (Inability to Contract)

Congestive Heart FailureEtiology
-Increase in Pulmonary pressure results fluid in alveoli (PULMONARY EDEMA) Increase in Systemic pressure results in fluid in tissues (PERIPHERAL EDEMA)
Health conditions that either damage the heart or make it work too hard- Coronary Artery Diseases (CAD)-Myocardial Infarction.-Heart muscle diseases (cardiomyopathy) -Heart inflammation (myocarditis)

Congestive Heart FailureRisk Factors
• Coronary artery Diseases• Myocardial Infarction• Hypertension• Diabetes• Heart Valve Disease( e.g.Aortic Stenosis)• Smoking• Obesity• Cardiomyopathy (Heart Muscle Diseases) 1)Dialated Cardiomyopathy (e.g. Alcohol,Viral Infections)
2)Hypertrophic Cardiomyopathy (Thickening of Heart Muscle ,septum between Rt and Lt Ventricle )
3)Restrictive Cardiomyopathy (Heart Muscles are rigid and unable to expand e.g Fibrosis)

Congestive Heart Failure

Congestive Heart FailurePathophysiology
In order to maintain normal cardiac output, severalcompensatory mechanisms play a role as under: Compensatory enlargement in the form of cardiac hypertrophy, cardiac dilatation, or both.
Tachycardia due to activation of neurohumoral system. e.g. release of norepinephrine and atrial natrouretic peptide, activation of renin-angiotensin aldosterone mechanism.

Congestive Heart Failure
STARLING’S LAWWithin limits, the force of ventricular contraction
is a function of the end-diastolic length of the cardiac muscle, which in turn is closely related to the ventricular end-diastolic volume.
This is achieved by increasing the length of sarcomeres in dilated heartIncreases the myocardial contractility and thereby attempts to maintain stroke volume.

Congestive Heart Failure
•Heart failure results in DEPRESSION of the ventricular function curve.
•COMPENSATION in the form of stretching of myocardial fibers results.
• Stretching leads to cardiac dilatation which occurs when the left ventricle fails to eject its normal end diastolic volume

Congestive Heart Failure
Sympathetic nervous system stimulation
Renin-angiotensin system activation
Myocardial hypertrophy
Altered cardiac Rhythm
Compensatory Mechanisms

Congestive Heart Failure

Congestive Heart Failure

Congestive Heart FailureVentricular remodeling
Altered cardiac rhythm

Congestive Heart Failure Types of Heart Failure
• Low-Output Heart Failure– Systolic Heart Failure:
– decreased cardiac output– Decreased Left ventricular ejection fraction
– Diastolic Heart Failure: – Elevated Left and Right ventricular end-diastolic pressures– May have normal LVEF
• High-Output Heart Failure– Seen with peripheral shunting, low-systemic vascular resistance,
hyperthryoidism, beri-beri, carcinoid, anemia– Often have normal cardiac output
• Right-Ventricular Failure– Seen with pulmonary hypertension, large RV infarctions.

Congestive Heart Failure
Clinical FeaturesLeft Sided Heart Failure:1) Pulmonary Edema a) Dyspnea (SOB) b)Orthopnea c)Paroxysmal Nocturnal Dyspnea
2)Decreased forward Perfusion Activated Renin Angiotensin Aldosterone System, which cause fluid retention and
worsenen CHF.

Congestive Heart FailureClinical Features
Right Sided Heart Failure: Most common cause of cause of Right Heart Failure is Left side Heart Failure. a) Dyspnea(SOB) b)Jugular Venous Distention c)Pitting Edema d)Ascitis e)Nutmeg Liver “Hepatomegaly”

Congestive Heart FailurePhysical Examination
• S3 gallop – Low sensitivity, but highly specific
• Cool, pale, cyanotic extremities– Have sinus tachycardia, diaphoresis and peripheral vasoconstriction
• Crackles or decreased breath sounds at bases (effusions) on lung exam• Elevated jugular venous pressure• Lower extremity edema• Ascites• Hepatomegaly• Splenomegaly• Displaced PMI
• Apical impulse that is laterally displaced past the midclavicular line is usually indicative of left ventricular enlargement>

Congestive Heart FailureDiagnosis
1)Echocardiogram -Distinguish systolic from Diastolic dysfunction by measuring Ejection Fraction -Determining Myocardial Ischemia is the precipitating cause. -Identify Valve Diseases.2)B Type Natriuretic Peptide (BNP)-Secreted by the Ventricles-Differentiate between causes of dyspnea due to heart Failure from the other cause
of dyspnea.3)Chest Xrays• -Determine any Cardiomegaly. Cephalization of the pulmonary vessels• Kerley B-lines• Pleural effusions4)EKG-To Identify arrhythmias,Ischemic Heart Diseases,Right and Left ventricular
Hypertrophy, and presence of conduction delays or abnormalities.

Congestive Heart Failure

Congestive Heart Failure Lab Investigations
• CBC– Since anemia can exacerbate heart failure
• Serum electrolytes and creatinine– before starting high dose diuretics
• Fasting Blood glucose– To evaluate for possible diabetes mellitus
• Thyroid function tests– Since thyrotoxicosis can result in A. Fib, and hypothyroidism can results in HF.
• Iron studies– To screen for hereditary hemochromatosis as cause of heart failure.
• ANA– To evaluate for possible lupus
• Viral studies – If viral mycocarditis suspected

Congestive Heart Failure• BNP
–With chronic heart failure, atrial mycotes secrete increase amounts of atrial natriuretic peptide (ANP) and brain natriuretic pepetide (BNP) in response to high atrial and ventricular filling pressures
–Usually is > 400 pg/mL in patients with dyspnea due to heart failure.

Congestive Heart Failure Cardiac Testing
• Exercise Testing– Should be part of initial evaluation of all patients with CHF.
• Coronary arteriography– Should be performed in patients presenting with heart failure who have
angina or significant ischemia– Reasonable in patients who have chest pain that may or may not be cardiac
in origin, in whom cardiac anatomy is not known, and in patients with known or suspected coronary artery disease who do not have angina.
– Measure cardiac output, degree of left ventricular dysfunction, and left ventricular end-diastolic pressure.
• Endomyocardial biopsy• Not frequently used• Really only useful in cases such as viral-induced cardiomyopathy

Congestive Heart FailureClassification of Heart Failure
• New York Heart Association (NYHA)– Class I – symptoms of HF only at levels that would limit normal
individuals.– Class II – symptoms of HF with ordinary exertion– Class III – symptoms of HF on less than ordinary exertion– Class IV – symptoms of HF at rest
• Guidelines– Stage A – High risk of HF, without structural heart disease or symptoms– Stage B – Heart disease with asymptomatic left ventricular dysfunction– Stage C – Prior or current symptoms of HF– Stage D – Advanced heart disease and severely symptomatic or refractory
HF

Congestive Heart FailureChronic Treatment of Systolic Heart Failure• Correction of systemic factors
– Thyroid dysfunction– Infections– Uncontrolled diabetes– Hypertension
• Lifestyle modification– Lower salt intake– Alcohol cessation– Medication compliance
• Maximize medications– Discontinue drugs that may contribute to heart failure
(NSAIDS, antiarrhythmics, calcium channel blockers)

Congestive Heart Failure
Pharmacological Therapy1. Loop diuretics.2. ACE inhibitor (or Angiotensin Receptor2 Blockers if
not tolerated).3. Beta blockers.4. Digoxin.5. Hydralazine, Nitrate.6. Potassium sparing diuretcs.

Congestive Heart Failure• Loop diuretics
• Furosemide, buteminide• For Fluid control, and to help relieve symptoms
• Potassium-sparing diuretics• Spironolactone, eplerenone• Help enhance diuresis• Maintain potassium• Shown to improve survival in CHF

Congestive Heart Failure
ACE Inhibitors• Improve survival in patients with all severities
of heart failure.• Begin therapy low and titrate up as possible:
• Enalapril –• Captopril • Lisinopril
• If cannot tolerate, may try ARB(Angiotensin II receptor blockers)

Congestive Heart FailureBeta Blockers
• Certain Beta blockers (carvedilol, metoprolol, bisoprolol) can improve overall and event free survival in NYHA class II to III HF, probably in class IV.
• Contraindicated:– Heart rate <60 bpm– Symptomatic bradycardia– Signs of peripheral hypoperfusion– COPD, asthma– PR interval > 0.24 sec, 2nd or 3rd degree block

Congestive Heart Failure
Hydralazine plus Nitrates• Dosing:– Hydralazine
– Started at 25 mg po TID, titrated up to 100 mg po TID
– Isosorbide dinitrate– Started at 40 mg po TID/QID
• Decreased mortality, lower rates of hospitalization, and improvement in quality of life.

Congestive Heart Failure
Digoxin• Given to patients with HF to control symptoms
such as fatigue, dyspnea, exercise intolerance• Shown to significantly reduce hospitalization
for heart failure, but no benefit in terms of overall mortality.

Congestive Heart FailureStatin Therapy
• Statin therapy is recommended in CHF for the secondary prevention of cardiovascular disease.
• Some studies have shown a possible benefit specifically in HF with statin therapy
• Improved LVEF• Reversal of ventricular remodeling• Reduction in inflammatory markers (CRP, IL-6, TNF-
alphaII)

Congestive Heart FailureTreating Congestive Heart failure
• Upright position• Nitrates• Lasix• Oxygen• ACE inhibitors• Digoxin
• Fluids(decrease)• After load (decrease)• Sodium retention• Test (Dig level, ABG’s, Potassium level)

Congestive Heart Failure
Medications to avoid In HF• NSAIDS
– Can cause worsening of preexisting HF
• Thiazolidinediones– Include rosiglitazone (Avandia), and pioglitazone (Actos)– Cause fluid retention that can exacerbate HF
• Metformin– People with HF who take it are at increased risk of potentially
lactic acidosis

Congestive Heart FailureImplantable Cardioverter-Defibrillators for HF
• Sustained ventricular tachycardia is associated with sudden cardiac death in HF.
• About one-third of mortality in HF is due to sudden cardiac death.
• Patients with ischemic or nonischemic cardiomyopathy, NYHA class II to III HF, and LVEF ≤ 35% have a significant survival benefit from an implantable cardioverter-defibrillator (ICD) for the primary prevention of SCD.

Congestive Heart Failure
Management of Refractory Heart Failure• Inotropic drugs:
– Dobutamine, dopamine, milrinone, nitroprusside, nitroglycerin• Mechanical circulatory support:
– Intraaortic balloon pump– Left ventricular assist device (LVAD)
• Cardiac Transplantation– A history of multiple hospitalizations for HF– Escalation in the intensity of medical therapy– A reproducable peak oxygen consumption with maximal
exercise (VO2max) of < 14 mL/kg per min. (normal is 20 mL/kg per min. or more) is relative indication, while a VO2max < 10 mL/kg per min is a stronger indication


Congestive Heart Failure