Congenital heart disease - prime.edu.pk heart disease.pdf · Learning objectives By the end of this...
Transcript of Congenital heart disease - prime.edu.pk heart disease.pdf · Learning objectives By the end of this...
Learning objectives
By the end of this lecture, final year student should be able to • Classify different types congenital heart disease. • Discuss the pathophysiology of congenital heart
disease. • Interpret the CXR and ECG of acynotic heart
disease. • Manage a child with acyanotic heart disease and
refer appropriately whenever needed.
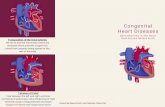
Fetal circulation
• Three cardiovascular structures unique to the fetus are important for maintaining this parallel circulation:
• the ductus venosus, • foramen ovale, and • ductus arteriosus.
prevalence
v Congenital heart disease occurs in 0.5–0.8% of live births.
v When two 1st-degree relatives have congenital heart disease, the risk for a subsequent child may reach 20–30%.
classification
CHD is divided into • Acyanotic heart disease (L-R shunt lesion)
• cyanotic heart disease (R-L shunt lesion)
Acyanotic heart disease L-R shunt lesions: • Atrial Septal Defect • ventricular Septal Defect • Patent ductus arteriosus
Obstructive Lesions • Pulmonary stenosis • Aortic stenosis • Coarctation of aorta
Regurgitant Lesions • Pulmonary regurgitation • Aortic regurgitation • Mitral valve prolapse
Ventricular Septal Defect • Is the most common congenital heart disease.
VSD may be • supracristal • perimembranous or • muscular •
CLINICAL MANIFESTATIONS
Clinical finding depends upon ü Size of the defect
ü pulmonary blood flow and pressure
CLINICAL MANIFESTATIONS
• dyspnoea, • feeding difficulties, • poor growth, • profuse perspiration, • recurrent pulmonary infections, and • cardiac failure in early infancy
Precordium exam
ü palpable parasternal lift, ü a laterally displaced apical impulse , ü a systolic thrill. ü The holosystolic murmur of grade 4 or above ü increased intensity of pulmonic component of
the 2nd heart sound ü mid-diastolic, low-pitched rumble at the apex
TREATMENT
• WHICH TYPE OF VSD IS MOST LIKELY TO CLOSE?
• FOR HOW LONG SHOULD WE WAIT FOR VSD TO CLOSE SPONTANOUSLY?
TREATMENT OF SMALL VSD
• an isolated, small, hemodynamically
insignificant VSD is not an indication for surgery
• Prophylactic antibiotics,
TREATMENT OF large VSD
Medical management has two aims: • to control heart failure and
• to prevent the development of pulmonary vascular disease
Indications for surgery • patients at any age with large defects in whom clinical
symptoms and failure to thrive cannot be controlled medically;
• infants between 6 and 12 mo of age with large defects associated with pulmonary hypertension, even if the symptoms are controlled by medication;
• patients older than 24 mo with a Qp : Qs ratio greater than 2 : 1.
• Patients with supracristal VSD of any size
ASD
• sinus venosus defect: high in septum • Ostium secundum defect: midseptum • Ostium primum defect: low in septum
CLINICAL MANIFESTATIONS
• dyspnea, • easy fatigability, • palpitations, • sustained atrial arrhythmia • heart failure.
CLINICAL MANIFESTATIONS
• A right ventricular systolic lift • A loud 1st heart. • Wide fixed splitting of the 2nd heart sound • A short, rumbling mid-diastolic murmur
produced by the increased volume of blood flow across the tricuspid valve
• Ejection systolic murmur at the upper left sternal border
complications
• pulmonary hypertension, • atrial dysrhythmias, • tricuspid or mitral insufficiency, and • heart failure • infective endocarditis
treatment
• ASDs detected in term infants may close spontaneously
• Surgical or transcatheter device closure is advised for all symptomatic patients and also for asymptomatic patients with a Qp : Qs ratio of at least 2 : 1.
• The timing for elective closure is after the 1st yr and before entry into school
Patent ductus arterious
• Functional closure of the ductus normally occurs soon after birth, but if the ductus remains patent , aortic blood is shunted into the pulmonary artery.
• PDA persisting beyond the 1st few weeks of life in a term infant rarely closes spontaneously
PATHOPHYSIOLOGY
• As a result of the higher aortic pressure, blood shunts left to right through the ductus, from the aorta to the pulmonary artery
• In extreme case, 70% of the left ventricular output may be shunted through the ductus to the pulmonary circulation
• Displaced and heaving apex beat • Machinery or rolling thunder murmur at left
upper sternal border.