Congenital Cytomegalovirus Infection
description
Transcript of Congenital Cytomegalovirus Infection
-
Congenital cytomegalovirus infection 1
Congenital cytomegalovirus infection
Congenital cytomegalovirus infectionClassification and external resources
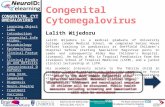
Micrograph of a cytomegalovirus (CMV) infection of the placenta (CMV placentitis). The characteristic large nucleus of a CMV infected cell isseen off-centre at the bottom-right of the image. H&E stain.
ICD-10 P35.1 [1]
ICD-9 771.1 [2]
MedlinePlus 001343 [3]
eMedicine article/963090 [4]
Congenital cytomegalovirus infection refers to a condition where cytomegalovirus is transmitted in the perinatalperiod.HCMV is one of the TORCH infections that lead to congenital abnormalities. (These are: toxoplasmosis, rubella,cytomegalovirus, and herpes simplex. )
EpidemiologyCongenital HCMV infection occurs when the mother suffers a primary infection (or reactivation) during pregnancy.Due to the lower seroprevalence of HCMV in industrialized countries and higher socioeconomic groups, congenitalinfections are actually less common in poorer communities, where more women of child-bearing age are alreadyseropositive. In industrialized countries up to 8% of HCMV seronegative mothers contract primary HCMV infectionduring pregnancy, of which roughly 50% will transmit to the fetus. Between 22-38% of infected fetuses are thenborn with symptoms, which may include pneumonia, gastrointestinal, retinal and neurological disease. HCMVinfection occurs in roughly 1% of all neonates with those who are not congenitally infected contracting the infectionpossibly through breast milk. Other sources of neonatal infection are bodily fluids which are known to contain hightitres in shedding individuals: saliva (
-
Congenital cytomegalovirus infection 2
Alcohol Syndrome, Spina Bifida, and Pediatric HIV/AIDS.[5]
PresentationFor infants who are infected by their mothers before birth, two potential adverse scenarios exist: Generalized infection may occur in the infant, and can cause complications such as low birth weight,
microcephaly, seizures, petechial rash similar to the "blueberry muffin" rash of congenital rubella syndrome, andmoderate hepatosplenomegaly (with jaundice). Though severe cases can be fatal, with supportive treatment mostinfants with CMV disease will survive. However, from 80% to 90% will have complications within the first fewyears of life that may include hearing loss, vision impairment, and varying degrees of mental retardation.
Another 5% to 10% of infants who are infected but without symptoms at birth will subsequently have varyingdegrees of hearing and mental or coordination problems.
These risks appear to be almost exclusively associated with women who previously have not been infected withCMV and who are having their first infection with the virus during pregnancy. There appears to be little risk ofCMV-related complications for women who have been infected at least 6 months prior to conception. For this group,which makes up 50% to 80% of the women of child-bearing age, the rate of newborn CMV infection is 1%, andthese infants appear to have no significant illness or abnormalities.The virus can also be transmitted to the infant at delivery from contact with genital secretions or later in infancythrough breast milk. However, these infections usually result in little or no clinical illness in the infant.To summarise, during a pregnancy when a woman who has never had CMV infection becomes infected with CMV,there is a risk that after birth the infant may have CMV-related complications, the most common of which areassociated with hearing loss, visual impairment, or diminished mental and motor capabilities. On the other hand,infants and children who acquire CMV after birth have few, if any, symptoms or complications.
PreventionRecommendations for pregnant women with regard to CMV infection: Throughout the pregnancy, practice good personal hygiene, especially handwashing with soap and water, after
contact with diapers or oral secretions (particularly with a child who is in day care). Women who develop a mononucleosis-like illness during pregnancy should be evaluated for CMV infection and
counseled about the possible risks to the unborn child. Laboratory testing for antibody to CMV can be performed to determine if a woman has already had CMV
infection. Recovery of CMV from the cervix or urine of women at or before the time of delivery does not warrant a
cesarean section. The demonstrated benefits of breast-feeding outweigh the minimal risk of acquiring CMV from the breast-feeding
mother. There is no need to either screen for CMV or exclude CMV-excreting children from schools or institutions
because the virus is frequently found in many healthy children and adults.
ChildcareMost healthy people working with infants and children face no special risk from CMV infection. However, forwomen of child-bearing age who previously have not been infected with CMV, there is a potential risk to thedeveloping unborn child (the risk is described above in the Pregnancy section). Contact with children who are in daycare, where CMV infection is commonly transmitted among young children (particularly toddlers), may be a sourceof exposure to CMV. Since CMV is transmitted through contact with infected body fluids, including urine andsaliva, child care providers (meaning day care workers, special education teachers, as well as mothers) should be
-
Congenital cytomegalovirus infection 3
educated about the risks of CMV infection and the precautions they can take. Day care workers appear to be at agreater risk than hospital and other health care providers, and this may be due in part to the increased emphasis onpersonal hygiene in the health care setting.Recommendations for individuals providing care for infants and children: Employees should be educated concerning CMV, its transmission, and hygienic practices, such as handwashing,
which minimize the risk of infection. Susceptible nonpregnant women working with infants and children should not routinely be transferred to other
work situations. Pregnant women working with infants and children should be informed of the risk of acquiring CMV infection
and the possible effects on the unborn child. Routine laboratory testing for CMV antibody in female workers is not specifically recommended due to its high
occurrence, but can be performed to determine their immune status.
CMV Testing and DiagnosisPeople infected with CMV develop antibodies to it, initially IgM later IgG indicating current infection and immunityrespectively. If the virus is detected in the blood, saliva, urine or other body tissues, it means that the person has anactive infection.When infected with CMV, most women have no symptoms, but some may have symptoms resemblingmononucleosis. Women who develop a mononucleosis-like illness during pregnancy should consult their medicalprovider.The Centers for Disease Control and Prevention (CDC) does not recommend routine maternal screening for CMVinfection during pregnancy because there is no test that can definitively rule out primary CMV infection duringpregnancy. Women who are concerned about CMV infection during pregnancy should practice CMV preventionmeasures.Considering that the CMV virus is present in saliva, urine, tears, blood, mucus, and other bodily fluids,frequent hand washing with soap and water is important after contact with diapers or oral secretions, especially witha child who is in daycare or interacting with other young children on a regular basis.A diagnosis of congenital CMV infection can be made if the virus is found in an infant's urine, saliva, blood, or otherbody tissues during the first week after birth. Antibody tests cannot be used to diagnose congenital CMV; a diagnosiscan only be made if the virus is detected during the first week of life. Congenital CMV cannot be diagnosed if theinfant is tested more than one week after birth.Visually healthy infants are not routinely tested for CMV infection although only 10-20% will show signs ofinfection at birth[citation needed] though up to 80% may go onto show signs of prenatal infection in later life. If apregnant woman finds out that she has become infected with CMV for the first time during her pregnancy, sheshould have her infant tested for CMV as soon as possible after birth.
-
Congenital cytomegalovirus infection 4
References[1] http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ P35. 1[2] http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=771. 1[3] http:/ / www. nlm. nih. gov/ medlineplus/ ency/ article/ 001343. htm[4] http:/ / emedicine. medscape. com/ article/ 963090-overview[5][5] ()
External links Cytomegalovirus (CMV) (http:/ / www. nhs. uk/ conditions/ Cytomegalovirus/ ) - NHS Choices CMV: Congenital CMV Infection (http:/ / www. cdc. gov/ cmv/ congenital-infection. html) - CDC
-
Article Sources and Contributors 5
Article Sources and ContributorsCongenital cytomegalovirus infection Source: http://en.wikipedia.org/w/index.php?oldid=593844694 Contributors: Arcadian, ArcadianOnUnsecuredLoc, Bearcat, Diptanshu.D, Download,John of Reading, Klgillis, Lepidoptera, Ruslik0, Wolfmankurd, Xezbeth, 2 anonymous edits
Image Sources, Licenses and ContributorsFile:CMV placentitis1 mini.jpg Source: http://en.wikipedia.org/w/index.php?title=File:CMV_placentitis1_mini.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors:Nephron
LicenseCreative Commons Attribution-Share Alike 3.0//creativecommons.org/licenses/by-sa/3.0/
Congenital cytomegalovirus infectionEpidemiologyPresentationPreventionChildcareCMV Testing and Diagnosis
ReferencesExternal links
License