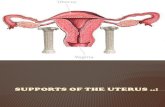
Congenital abnormaleties of the uterus
-
Upload
ian-donald-inter-school-followship-of-ultrasound -
Category
Health & Medicine
-
view
509 -
download
1
Transcript of Congenital abnormaleties of the uterus

CONGENITAL ANOMALIES OF THE UTEUUS
PRESENTED BY
OUSMANE BECHIR HASSABALLAH
IAN DONALD INTER SCHOOL FOLLOWSHIP OF ULTRASOUND
Batch 6
101012015
Introduction
Uterine malformations result from partial or
complete failure of one of three mechanisms
either separately or combined - agenesis
fusion and resorption Agenesis results in
either a complete absence of the uterus or a
unicornuate uterus a failure to fusion gives
rise to uterine didelphys or a bicornuate uterus
and a septated uterus is due to a failure of
resorption
incidence The incidence of muellerian anomalies has
historically varied widely due to the different
populations studied small sample sizes
prospective versus retrospective study designs
different classification systems and the type of
test used to make the diagnosis The need for a
standard classification of muellerian anomalies
was self-evident
In the general population the incidence of uterine
anomalies are estimated to be 3-4 (Sorensen 1988)
This increases to 73 in infertile patients ( Saravelos
2008)
Why is this important
Majority have no problem conceiving but
have higher rates of
ndash 1 Spontaneous Abortion
ndash 2 Premature Delivery
ndash 3 Infertility
ndash 4 Abnormal Fetal Lie
ndash 5 Dystocia at delivery
ndash 6 Dysmenorrhea endometriosis
ndash 7 Cervical incompetence
Uterine Anomalies
Absence of Uterus Fusion anomalies
Muumlllerian duct anomaly classification
The American Fertility Society (AFS)
classified muellerian anomalies according to
the major uterine anatomic types The AFS
classes of muellerian anomalies are
Hypoplasiaagenesis
Unicornuate
Didelphys
Bicornuate
Septate
Arcuate
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
The Muumlllerian duct anomaly classification is a
seven point system that can be used to describe a
number of embryonic Muumlllerian duct anomalies
class I uterine agenesisuterine hypoplasia
ndash a vaginal (uterus normal variety of
abnormal forms)
ndash b cervical
ndash c fundal
ndash d tubal
ndash e combined
class II unicornuate uterusunicornis
unicollis ~6-25
ndash a communicating contralateral rudimentary
horn contains endometrium
ndash b non-communicating contralateral
rudimentary horn contains endometrium
ndash c contralateral horn has no endometrial
cavity
ndash d no horn
ndash class III uterus didelphys ~5-11
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
class IV bicornuate uterus next commonest
type ~10-39
ndash a complete division all the way down to
internal the os
ndash b partial division not extending to the os
class V septate uterus commonest anomaly
~34-55
ndash a complete division all the way down to the
internal os
ndash b incomplete division
class VI arcuate uterus ~7
class VII in utero Diethylstilbestrol (DES)
exposure T shaped uterus
Classification into 4 groups
1 Agenesis of uterusvagina Rokitansky-
Kuster-Hauser Syndrome
2-Unilateral development Unicornate
uterus
3 Lateral Fusion defects (obstructive or
non-obstructive)
4-Defects in Vertical Fusion (obstructive or
non-obstructive)
Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Introduction
Uterine malformations result from partial or
complete failure of one of three mechanisms
either separately or combined - agenesis
fusion and resorption Agenesis results in
either a complete absence of the uterus or a
unicornuate uterus a failure to fusion gives
rise to uterine didelphys or a bicornuate uterus
and a septated uterus is due to a failure of
resorption
incidence The incidence of muellerian anomalies has
historically varied widely due to the different
populations studied small sample sizes
prospective versus retrospective study designs
different classification systems and the type of
test used to make the diagnosis The need for a
standard classification of muellerian anomalies
was self-evident
In the general population the incidence of uterine
anomalies are estimated to be 3-4 (Sorensen 1988)
This increases to 73 in infertile patients ( Saravelos
2008)
Why is this important
Majority have no problem conceiving but
have higher rates of
ndash 1 Spontaneous Abortion
ndash 2 Premature Delivery
ndash 3 Infertility
ndash 4 Abnormal Fetal Lie
ndash 5 Dystocia at delivery
ndash 6 Dysmenorrhea endometriosis
ndash 7 Cervical incompetence
Uterine Anomalies
Absence of Uterus Fusion anomalies
Muumlllerian duct anomaly classification
The American Fertility Society (AFS)
classified muellerian anomalies according to
the major uterine anatomic types The AFS
classes of muellerian anomalies are
Hypoplasiaagenesis
Unicornuate
Didelphys
Bicornuate
Septate
Arcuate
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
The Muumlllerian duct anomaly classification is a
seven point system that can be used to describe a
number of embryonic Muumlllerian duct anomalies
class I uterine agenesisuterine hypoplasia
ndash a vaginal (uterus normal variety of
abnormal forms)
ndash b cervical
ndash c fundal
ndash d tubal
ndash e combined
class II unicornuate uterusunicornis
unicollis ~6-25
ndash a communicating contralateral rudimentary
horn contains endometrium
ndash b non-communicating contralateral
rudimentary horn contains endometrium
ndash c contralateral horn has no endometrial
cavity
ndash d no horn
ndash class III uterus didelphys ~5-11
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
class IV bicornuate uterus next commonest
type ~10-39
ndash a complete division all the way down to
internal the os
ndash b partial division not extending to the os
class V septate uterus commonest anomaly
~34-55
ndash a complete division all the way down to the
internal os
ndash b incomplete division
class VI arcuate uterus ~7
class VII in utero Diethylstilbestrol (DES)
exposure T shaped uterus
Classification into 4 groups
1 Agenesis of uterusvagina Rokitansky-
Kuster-Hauser Syndrome
2-Unilateral development Unicornate
uterus
3 Lateral Fusion defects (obstructive or
non-obstructive)
4-Defects in Vertical Fusion (obstructive or
non-obstructive)
Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

incidence The incidence of muellerian anomalies has
historically varied widely due to the different
populations studied small sample sizes
prospective versus retrospective study designs
different classification systems and the type of
test used to make the diagnosis The need for a
standard classification of muellerian anomalies
was self-evident
In the general population the incidence of uterine
anomalies are estimated to be 3-4 (Sorensen 1988)
This increases to 73 in infertile patients ( Saravelos
2008)
Why is this important
Majority have no problem conceiving but
have higher rates of
ndash 1 Spontaneous Abortion
ndash 2 Premature Delivery
ndash 3 Infertility
ndash 4 Abnormal Fetal Lie
ndash 5 Dystocia at delivery
ndash 6 Dysmenorrhea endometriosis
ndash 7 Cervical incompetence
Uterine Anomalies
Absence of Uterus Fusion anomalies
Muumlllerian duct anomaly classification
The American Fertility Society (AFS)
classified muellerian anomalies according to
the major uterine anatomic types The AFS
classes of muellerian anomalies are
Hypoplasiaagenesis
Unicornuate
Didelphys
Bicornuate
Septate
Arcuate
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
The Muumlllerian duct anomaly classification is a
seven point system that can be used to describe a
number of embryonic Muumlllerian duct anomalies
class I uterine agenesisuterine hypoplasia
ndash a vaginal (uterus normal variety of
abnormal forms)
ndash b cervical
ndash c fundal
ndash d tubal
ndash e combined
class II unicornuate uterusunicornis
unicollis ~6-25
ndash a communicating contralateral rudimentary
horn contains endometrium
ndash b non-communicating contralateral
rudimentary horn contains endometrium
ndash c contralateral horn has no endometrial
cavity
ndash d no horn
ndash class III uterus didelphys ~5-11
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
class IV bicornuate uterus next commonest
type ~10-39
ndash a complete division all the way down to
internal the os
ndash b partial division not extending to the os
class V septate uterus commonest anomaly
~34-55
ndash a complete division all the way down to the
internal os
ndash b incomplete division
class VI arcuate uterus ~7
class VII in utero Diethylstilbestrol (DES)
exposure T shaped uterus
Classification into 4 groups
1 Agenesis of uterusvagina Rokitansky-
Kuster-Hauser Syndrome
2-Unilateral development Unicornate
uterus
3 Lateral Fusion defects (obstructive or
non-obstructive)
4-Defects in Vertical Fusion (obstructive or
non-obstructive)
Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Why is this important
Majority have no problem conceiving but
have higher rates of
ndash 1 Spontaneous Abortion
ndash 2 Premature Delivery
ndash 3 Infertility
ndash 4 Abnormal Fetal Lie
ndash 5 Dystocia at delivery
ndash 6 Dysmenorrhea endometriosis
ndash 7 Cervical incompetence
Uterine Anomalies
Absence of Uterus Fusion anomalies
Muumlllerian duct anomaly classification
The American Fertility Society (AFS)
classified muellerian anomalies according to
the major uterine anatomic types The AFS
classes of muellerian anomalies are
Hypoplasiaagenesis
Unicornuate
Didelphys
Bicornuate
Septate
Arcuate
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
The Muumlllerian duct anomaly classification is a
seven point system that can be used to describe a
number of embryonic Muumlllerian duct anomalies
class I uterine agenesisuterine hypoplasia
ndash a vaginal (uterus normal variety of
abnormal forms)
ndash b cervical
ndash c fundal
ndash d tubal
ndash e combined
class II unicornuate uterusunicornis
unicollis ~6-25
ndash a communicating contralateral rudimentary
horn contains endometrium
ndash b non-communicating contralateral
rudimentary horn contains endometrium
ndash c contralateral horn has no endometrial
cavity
ndash d no horn
ndash class III uterus didelphys ~5-11
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
class IV bicornuate uterus next commonest
type ~10-39
ndash a complete division all the way down to
internal the os
ndash b partial division not extending to the os
class V septate uterus commonest anomaly
~34-55
ndash a complete division all the way down to the
internal os
ndash b incomplete division
class VI arcuate uterus ~7
class VII in utero Diethylstilbestrol (DES)
exposure T shaped uterus
Classification into 4 groups
1 Agenesis of uterusvagina Rokitansky-
Kuster-Hauser Syndrome
2-Unilateral development Unicornate
uterus
3 Lateral Fusion defects (obstructive or
non-obstructive)
4-Defects in Vertical Fusion (obstructive or
non-obstructive)
Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Uterine Anomalies
Absence of Uterus Fusion anomalies
Muumlllerian duct anomaly classification
The American Fertility Society (AFS)
classified muellerian anomalies according to
the major uterine anatomic types The AFS
classes of muellerian anomalies are
Hypoplasiaagenesis
Unicornuate
Didelphys
Bicornuate
Septate
Arcuate
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
The Muumlllerian duct anomaly classification is a
seven point system that can be used to describe a
number of embryonic Muumlllerian duct anomalies
class I uterine agenesisuterine hypoplasia
ndash a vaginal (uterus normal variety of
abnormal forms)
ndash b cervical
ndash c fundal
ndash d tubal
ndash e combined
class II unicornuate uterusunicornis
unicollis ~6-25
ndash a communicating contralateral rudimentary
horn contains endometrium
ndash b non-communicating contralateral
rudimentary horn contains endometrium
ndash c contralateral horn has no endometrial
cavity
ndash d no horn
ndash class III uterus didelphys ~5-11
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
class IV bicornuate uterus next commonest
type ~10-39
ndash a complete division all the way down to
internal the os
ndash b partial division not extending to the os
class V septate uterus commonest anomaly
~34-55
ndash a complete division all the way down to the
internal os
ndash b incomplete division
class VI arcuate uterus ~7
class VII in utero Diethylstilbestrol (DES)
exposure T shaped uterus
Classification into 4 groups
1 Agenesis of uterusvagina Rokitansky-
Kuster-Hauser Syndrome
2-Unilateral development Unicornate
uterus
3 Lateral Fusion defects (obstructive or
non-obstructive)
4-Defects in Vertical Fusion (obstructive or
non-obstructive)
Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Muumlllerian duct anomaly classification
The American Fertility Society (AFS)
classified muellerian anomalies according to
the major uterine anatomic types The AFS
classes of muellerian anomalies are
Hypoplasiaagenesis
Unicornuate
Didelphys
Bicornuate
Septate
Arcuate
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
The Muumlllerian duct anomaly classification is a
seven point system that can be used to describe a
number of embryonic Muumlllerian duct anomalies
class I uterine agenesisuterine hypoplasia
ndash a vaginal (uterus normal variety of
abnormal forms)
ndash b cervical
ndash c fundal
ndash d tubal
ndash e combined
class II unicornuate uterusunicornis
unicollis ~6-25
ndash a communicating contralateral rudimentary
horn contains endometrium
ndash b non-communicating contralateral
rudimentary horn contains endometrium
ndash c contralateral horn has no endometrial
cavity
ndash d no horn
ndash class III uterus didelphys ~5-11
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
class IV bicornuate uterus next commonest
type ~10-39
ndash a complete division all the way down to
internal the os
ndash b partial division not extending to the os
class V septate uterus commonest anomaly
~34-55
ndash a complete division all the way down to the
internal os
ndash b incomplete division
class VI arcuate uterus ~7
class VII in utero Diethylstilbestrol (DES)
exposure T shaped uterus
Classification into 4 groups
1 Agenesis of uterusvagina Rokitansky-
Kuster-Hauser Syndrome
2-Unilateral development Unicornate
uterus
3 Lateral Fusion defects (obstructive or
non-obstructive)
4-Defects in Vertical Fusion (obstructive or
non-obstructive)
Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
The Muumlllerian duct anomaly classification is a
seven point system that can be used to describe a
number of embryonic Muumlllerian duct anomalies
class I uterine agenesisuterine hypoplasia
ndash a vaginal (uterus normal variety of
abnormal forms)
ndash b cervical
ndash c fundal
ndash d tubal
ndash e combined
class II unicornuate uterusunicornis
unicollis ~6-25
ndash a communicating contralateral rudimentary
horn contains endometrium
ndash b non-communicating contralateral
rudimentary horn contains endometrium
ndash c contralateral horn has no endometrial
cavity
ndash d no horn
ndash class III uterus didelphys ~5-11
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
class IV bicornuate uterus next commonest
type ~10-39
ndash a complete division all the way down to
internal the os
ndash b partial division not extending to the os
class V septate uterus commonest anomaly
~34-55
ndash a complete division all the way down to the
internal os
ndash b incomplete division
class VI arcuate uterus ~7
class VII in utero Diethylstilbestrol (DES)
exposure T shaped uterus
Classification into 4 groups
1 Agenesis of uterusvagina Rokitansky-
Kuster-Hauser Syndrome
2-Unilateral development Unicornate
uterus
3 Lateral Fusion defects (obstructive or
non-obstructive)
4-Defects in Vertical Fusion (obstructive or
non-obstructive)
Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

class II unicornuate uterusunicornis
unicollis ~6-25
ndash a communicating contralateral rudimentary
horn contains endometrium
ndash b non-communicating contralateral
rudimentary horn contains endometrium
ndash c contralateral horn has no endometrial
cavity
ndash d no horn
ndash class III uterus didelphys ~5-11
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
class IV bicornuate uterus next commonest
type ~10-39
ndash a complete division all the way down to
internal the os
ndash b partial division not extending to the os
class V septate uterus commonest anomaly
~34-55
ndash a complete division all the way down to the
internal os
ndash b incomplete division
class VI arcuate uterus ~7
class VII in utero Diethylstilbestrol (DES)
exposure T shaped uterus
Classification into 4 groups
1 Agenesis of uterusvagina Rokitansky-
Kuster-Hauser Syndrome
2-Unilateral development Unicornate
uterus
3 Lateral Fusion defects (obstructive or
non-obstructive)
4-Defects in Vertical Fusion (obstructive or
non-obstructive)
Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Muumlllerian duct anomaly classificationDr Ayush Goel and Dr Frank Gaillard et al
class IV bicornuate uterus next commonest
type ~10-39
ndash a complete division all the way down to
internal the os
ndash b partial division not extending to the os
class V septate uterus commonest anomaly
~34-55
ndash a complete division all the way down to the
internal os
ndash b incomplete division
class VI arcuate uterus ~7
class VII in utero Diethylstilbestrol (DES)
exposure T shaped uterus
Classification into 4 groups
1 Agenesis of uterusvagina Rokitansky-
Kuster-Hauser Syndrome
2-Unilateral development Unicornate
uterus
3 Lateral Fusion defects (obstructive or
non-obstructive)
4-Defects in Vertical Fusion (obstructive or
non-obstructive)
Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

class VI arcuate uterus ~7
class VII in utero Diethylstilbestrol (DES)
exposure T shaped uterus
Classification into 4 groups
1 Agenesis of uterusvagina Rokitansky-
Kuster-Hauser Syndrome
2-Unilateral development Unicornate
uterus
3 Lateral Fusion defects (obstructive or
non-obstructive)
4-Defects in Vertical Fusion (obstructive or
non-obstructive)
Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Classification into 4 groups
1 Agenesis of uterusvagina Rokitansky-
Kuster-Hauser Syndrome
2-Unilateral development Unicornate
uterus
3 Lateral Fusion defects (obstructive or
non-obstructive)
4-Defects in Vertical Fusion (obstructive or
non-obstructive)
Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Uterine agenesis
is the extreme of Mullerian duct anomalies
(Class I) where there is complete absence of
uterine tissue above the vagina
Epidemiology
The uterine agenesis-hypoplasia spectrum
accounts for ~10-15 of all Muumlllerian duct
anomalies
Clinical presentation
Clinical presentation is characterised by primary
amenorrhoea with normal hormonal levels
guaranteed by fully functional gonads
Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Pathology
Complete absence of the Mullerian ducts is
termed Mayer-Rokitansky-Kuster-Hauser
(MRKH) syndrome which includes absence
of the vagina as well
Associations
renal tract anomalies including renal
agenesis
skeletal vertebral anomalies
The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

The uterus is small measuring just 38 x 12 cm hypoplasia
Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Figure 2 Pelvic ultrasound longitudinal showing the urinary bladder and
absent uterus
Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Figure 3 Pelvic ultrasound showing an ectopic pelvic kidney indenting
on the urinary bladder superiorly
Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Figure 4 Intravenous urography showing pevicaeal system of the ectopic
kidney
Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Figure 5 Enhanced axial CT of the pelvis showing contrast in the urinary
bladder (and rectal contrast) but no uterus
Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Sagittal and transverse ultrasound images show a markedly hypoplastic
uterus measuring less than 48 x 16 x 27 cm in a middle-aged female
patient with primary infertility
Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Unicornuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
A unicornuate uterus or unicornis unicollis is a
type of Mullerian duct anomaly (class II) This
type can account for ~10 (range 6-13) of
uterine anomalies and infertility is seen in
~125 (range 5-20) of cases
Pathology
There is failure of one muumlllerian duct to elongate
while the other develops normally The
embryologic predominance of the unicornuate
uterus to be on the right has not been explained It
may or may not have rudimentary horn
Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Sub-classification
It can be classified into to the following types
according to the
type a with rudimentary horn the American
Fertility Society 3
ndash a1 horn contains endometrium
a1a communicating contralateral
rudimentary horn contains endometrium
(10)
a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

a1b non-communicating contralateral
rudimentary horn contains
endometrium (22)
ndash a2 contralateral horn has no endometrial
cavity (33)
type b no horn (35)
Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Associations
renal abnormalities
ndash renal anomalies are more commonly
associated with a unicornuate uterus than
with other muumlllerian duct anomalies and are
present in 40 of cases eg renal agenesis
ndash the renal anomaly is always ipsilateral to the
rudimentary horn
cryptomenorrhea within endometrium
containing rudimentary horn that does not
communicate with the endometrial cavity
primary infertility 4
Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Ultrasound
Can be diffcult to detect on 2D ultrasound
The uterus may be seen tapering to one side
Hysterosalpingogram (HSG)
MRI
Radiographic features
Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Complications
Of the Mullerian duct anomalies a
unicornuate uterus is considered to have the
second worse obstetric outcome (worst with
a septate uterus)
Spontaneous abortion rates are reported to
range from 41-62 Reported premature
birth rates range from 10-20 Fetal
survival rate is ~40 (range 38-57)
Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Reconstructed 3-dimensional sonogram of a left unicornuate uterus in the
coronal plane showing the characteristic fusiform banana-shaped uterus
with a single left horn and a single endometrial cavity
Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Unicornuate uterus after saline infusion
this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

this ultrasound image (3D) is a coronal plane showing a unicornuate uterus
The cavity (at C) only goes to one fallopian tube (goes up to her right tube)
3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

3 dimensional coronal image of a unicornuate uterus
Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Unicornuate uterus A multiplanar display of the left unicornuate uterus is
shown This diagnosis is difficult to establish with 2DUS because the uterus
may appear grossly normal or slightly laterally deviated With 3DUS the
diagnosis is confidently made because the coronal plane (C) shows clearly that
there is only a single cornual angle (arrow) The cervical canal has a normal
appearance A Axial view B sagittal view C coronal view
Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Unicornuate Uterus Ultrasound Pregnant uterus ndash fetus
Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Uterus didelphysDr Jeremy Jones and Dr Frank Gaillard et al
is a type of Muumlllerian duct anomaly (class III)
where there is complete duplication of uterine horns
as well as duplication of the cervix with no
communication between them
Epidemiology
Didelphic uteri account for approximately ~8
(range 5-11) of Muumlllerian duct anomalies
Clinical presentation
Many patients are asymptomatic although some
may occasionally experience dyspareunia as a result
of the vaginal septum
Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Pathology
It results from failed ductal fusion that occurs
between the 12th and 16th week of pregnancy and
is characterized by two symmetric widely
divergent uterine horns and two cervices The
uterine volume in each duplicated segment is
reduced As with most uterine anatomical
anomalies there is an increased incidence of
fertility issues and Muumlllerian abnormalities in
general are over represented in infertile women
The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

The chance of seeing a pregnancy to term is
significantly reduced down to only 20
with a third of pregnancies ending in
abortion and over half in premature
deliveries Only 40 of pregnancies
resulted in living children 2
Along with unicornuate uterus uterus
didelphys has the greatest impact on
reproductive performance reference required
Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Associations
renal agenesis
vaginal septum which can include transverse
vaginal septum
ndash there is a vaginal septum in 75 of cases and
obstruction to one horn is possible from occasional
transverse septae
Radiographic features
Classically shows two widely spaced uterine corpora
each with a single Fallopian tube Separate divergent
uterine horns with large fundal cleft (as distinct from
a septate uterus)
Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Hysterosalpingogram (HSG)
Pelvic ultrasound
Separate divergent uterine horns are
identified with a large fundal cleft
Endometrial cavities are uniformly separate
with no evidence of communication Two
separate cervices need to be documented
MRI
2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

2-dimensional image of a didelphic uterus with a
gestational sac (arrow) in the left horn
Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Ultrasound image showing duplication of uterus corpus characterizes this
Mullerian Duct Anomaly Didelphys uterus (Type III) or Complete
bicornuate (Type IVa) Ultrasound scan
Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Complications
infertility
unilateral hydrocolpos haematocolpos (if a
vaginal septum is present)
endometriosis
Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Bicornuate uterusDr Frank Gaillard et al
A bicornuate uterus is a type of uterine
duplication anomaly It can be classified as
a class IV Mullerian duct anomaly
Epidemiology
Overall congenital uterine anomalies occur in
~15 of females (range 01-3) Bicornuate
uteri are thought to represent ~25 (range 10-
39) of Mullerian duct anomalies
Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Clinical presentation
In most cases a bicornuate uterus is
incidentally discovered when the pelvis is
imaged The most common symptomatic
presentation is with early pregnancy loss
and cervical incompetence 6
Pathology
A bicornuate uterus results from an
abnormal development of the
paramesonephric ducts There is a partial
failure of fusion of the ducts resulting in a
uterus divided into two horns
Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Associations
associated longitudinal vaginal septum may be
present in ~25 of cases
as with other Mullerian duct anomalies
abnormalities of the renal tract may also be
present
Subtypes
Bicornuate uterus is divided according to the
involvement of the cervical canal
bicornuate bicollis - two cervical canals central
myometrium extends to external cervical os
bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

bicornuate unicollis - one cervical canal
central myometrium extends to internal
cervical os
Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Radiographic features
General
The preferred methods of imaging uterine
anomalies are ultrasound
hysterosalpingogram or MRI The external
uterine contour is concave or heart-shaped
and the uterine horns are widely divergent
The fundal cleft is typically more than 1cm
deep and the intercornual distance is
widened
The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

The uterus is seen as comprising of caudally
fused symmetric uterine cavities with some
degree of communication between the two
cavities (usually at the uterine isthmus) Although
not a specific finding the angle between the
horns of the bicornuate uterus is usually more
than 105deg
Fluoroscopy - hysterosalpinogram (HSG)
A divided uterus can be seen but it is difficult to
differentiate between septate and bicornuate
anomalies since the uterine fundal contour is not
visible
MRI
Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Treatment and prognosis
Surgical intervention is usually not indicated in
absence of reproductive difficulties
In women with a history of recurrent pregnancy
loss and in whom no other infertility issues have
been identified a Strassman metroplasty can be
considered
In patients with cervical incompetence
placement of a cervical cerclage may increase
fetal survival rates 9 Indeed the association
between cervical incompetence and bicornuate
uterus is so high that prophylactic cerclage may
be appropriate in some instances
Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Practical points
Septate uterus increases the risk of early
pregnancy loss and hysteroscopic
intervention to resect the septum is
sometimes pursued In this situation
differentiation between a septate uterus or a
bicornuate uterus is critical outcome
Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Bicornuate uterus (with pregnancy in one horn)
Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Surface rendering of a bicornuate uterus The serosal indentation
(arrow) is evident
Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Bicornuate uterus with unilateral pregnancy
Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Septate uterusDr Matt A Morgan and Dr Natalie Yang et al
A septate uterus is a common type of congenital
uterine anomaly and it may lead to an increased rate
of pregnancy loss The main imaging differential
diagnoses are arcuate uterus and bicornuate uterus
Epidemiology
It is considered the commonest uterine anomaly
(accounts for ~55 of such anomalies) It is classified
as a class V Mullerian duct anomaly Septate uterus
is the most common anomaly associated with
reproductive failure (67)
Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Pathology
Septate uterus is considered a type of uterine
duplication anomaly It results from partial or
complete failure of resorption of the uterovaginal
septum after fusion of the para-mesonephric
ducts The septum is usually fibrous but can also
have varying muscular components
Subtypes
a partial septum (sub-septate uterus) involves the
endometrial canal but not the cervix
a septum is considered complete if it extends to
either the internal or external cervical os 10
septum extends into the vagina septate uterus and
vagina
Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Associations
As with other uterine anomalies concurrent
renal anomalies may be associated
Radiographic features
General
the external uterine fundal contour may be
convex flat or mildly (lt 1 cm) concave
acute angle lt75 degrees between uterine
cavities
endometrial canals are completely separated by
tissue iso-echoic to myometrium with
extension into endocervical canal
Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Ultrasound
The echogenic endometrial stripe is separated at the
fundus by the intermediate echogenicity septum
The septum extends to the cervix in a complete
septate uterus The external uterine contour must
demonstrate a convex flat or mildly concave
(ideally lt1cm) configuration and may best be
appreciated on coronal images of the uterus
Colour Doppler
May show vascularity in the septum in 70 of
cases and if present may be associated with a higher
rate of obstetric complications
Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Fluoroscopy - Hysterosalpingogram
Accuracy of hysterosalpingogram alone is
only 55 for differentiation of septate uterus
from bicornuate uterus
Pelvic MRI
MRI is considered the current imaging
modality of choice
Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Complications
90 miscarriage rate
ndash a patient with a septate uterus does not
usually not have difficulty conceiving but
a septate uterus is associated with the
highest rate of pregnancy loss of the
Muumlllerian duct anomalies
Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Treatment and prognosis
The distinction between septate uterus and bicornuate
uterus has important management implications In
septate uterus but not in bicornuate uterus the
septum can be shaved off during hysteroscopy
(metroplasty) to form a single uterine cavity without
perforating the uterus 4
Reproductive outcome has been shown to improve
after resection of the septum with reported decreases
in the spontaneous abortion rate from 88 to 59
after hysteroscopic metroplasty
Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Differential diagnosis
Considerations a hysterosalpingogram include
bicornuate uterus the shape of the external
uterine contour is crucial to differentiate a
septate uterus from a bicornuate uterus because
widely different clinical and interventional
approaches are assigned to each anomaly
On ultrasound or MRI images also consider
arcuate uterus small myometrial indentation in
the fundus with normal fundal contour
thick intra-uterine adhesion band
Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Septate Uterus
Most COMMON anomaly 55
May be complete incomplete
bull25 early abortions
bull5 - 7 late abortions amp Premature labors
3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

3-dimensional coronal view of a septated uterus (a) distance
between ostia (+ +) (b) length of septum (x x)
(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

(12 weeks) Longitudinal section of the fetus showing its location belong the
uterine septum within the amniotic cavity that had spread to the both uterine
horns
The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

The fetal head situated in the right uterine horn
Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Transverse plane through the uterus The uterine septum is hypoechoic and
hypovascular At this level the placenta (PL) begins to spread on the posterior
wall (retroverted uterus)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Donald School Journal of Ultrasound in Obstetrics and Gynecology July-September
20115(3)243-256
Figs A to C Septate uterus seen on 3D VCI-C (A) septal vessels on 3D
power Doppler (B) and 3D SIS with coronal plane (C)
Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Arcuate uterusDr Yuranga Weerakkody and Dr Natalie Yang et al
An arcuate uterus is a mildly variant shape of
the uterus It is technically one of the Muumlllerian
duct anomalies but is often classified as a
normal variant It is the uterine anomaly that is
least commonly associated with reproductive
failure Arcuate uterus can be characterized with
ultrasound or MRI
Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Pathology
An arcuate uterus is
characterized by a mild
indentation of the
endometrium at the
uterine fundus It occurs
due to a failure of
complete resorption of
the uterovaginal septum
It is the most common
Mullarian duct anomaly
affecting 39 of the
general population
Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Radiographic features
General features include
normal fundal contour
no division of uterine horns
smooth indentation of fundal endometrial
canal - the depth of indentation is usually
considered to be lt1 cm
increased transverse diameter of uterine
cavity
Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Pelvic ultrasound
A normal external uterine
contour is noted with a
broad smooth indentation
on the fundal segment of
the endometrium No
division of the uterine
horns
Hysterosalpingogram
MRI
Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Differential diagnosis
septate uterus
ndash arcuate uterus and septate uterus exist on a
spectrum from least to most resorption of
the uterovaginal septum respectively
bicornuate uterus
ndash arcuate uterus can be distinguished from
a bicornuate uterus on the basis of its complete
fundal unification (ie the arcuate uterus has a
normal or slightly indented external fundal contour
whereas the bicornuate has a more marked fundal
indentation no more than 5 mm above the level of
the uterine horns)
Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Figs A to E Arcuate uterus seen on 2D scan (A) SIS (B) 3D reconstructed
coronal plane during SIS (C) 3D VCI-C rendering (D) and 3D inversion mode
(E)
Donald School Journal of Ultrasound in Obstetrics and Gynecology July-
September 20115(3)243-256
RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

RKH Syndrome Diagnosis
Expected Menarche
Difficult to differentiate from imperforate
hymen
No uterus on exam US MRI
Laparoscopy IVP
Confused with Androgen Resistance
Syndrome with shallow pouch and no
uterus
Determine karyotype
Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Abnormalities of the
ovaries
1) agenesis or complete absence
2) Gonadal dysgenesis streak
gonads as in Turner syndrome
3) Failure of descent into the pelvis
4) Ovotestis ldquotrue hermaphroditerdquo
In which combined ovarian and
testicular tissues seen
conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

conclusion
All uterine anomalies negatively affect the live
birth rate and result in a higher frequency of
obstetrical complications Depending upon
the type of muellerian anomaly cervical
incompetence spontaneous miscarriage
preterm delivery breech presentation
abnormal fetal lie and intrauterine growth
restriction are all increased to a variable
degree 167
3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

3DUS enables the measurement of the length
of a uterine septum amp depth of fundal cleft
In addition 3D ultrasound in diagnosing
uterine congenital malformations has been
found to be a reproducible method(Salim 2003)
While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

While transvaginal sonography is an excellent
screening examination for uterine anomalies it is
not as effective as 3D ultrasound in distinguishing
specific malformations For example Jurkovic et al
20 reported a 100 sensitivity and specificity for
the three-dimensional ultrasound detection of
uterine anomalies in contrast to 100 sensitivity
and 95 specificity for two-dimensional
ultrasound However the positive predictive value
of three-dimensional and two-dimensional
ultrasound for muellerian anomalies was 100 and
50 respectively
MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

MRI has been the gold standard for categorizing
uterine anomalies because of its 98 - 100 accuracy
While ultrasound will remain the primary modality
utilized to evaluate muellerian anomalies MRI can
offer additional diagnostic information in patients with
equivocal ultrasound findings As a result laparoscopy
or open surgery are no longer required to make a
definitive diagnosis of a uterine anomaly
Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Thank you
At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

At 6TH week gestation
Paramesonephric
or Mullerian Duct
develops lateral to
the Mesonephric
rdquowolffian ldquo Duct
The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

The middle and caudal parts of
the Mullerian ducts undergoes
medial migration and fusion
The cranial 13 rarr tubes
The middle 13 rarr uterus and
cervix
Caudal 13 rarr upper 34 of
vagina
Development of the vagina

Development of the vagina