COMMON SKIN CANCERS Recognition and Management 2014/Storch-Escott.pdf · COMMON SKIN CANCERS...
Transcript of COMMON SKIN CANCERS Recognition and Management 2014/Storch-Escott.pdf · COMMON SKIN CANCERS...

2/3/2014
1
COMMON SKIN CANCERS Recognition and Management
Marlyn J. Storch-Escott
RN, BSN, MSN, ANP
Objectives
• List the most common types of skin cancers.
• Identify 2-3 clinical manifestations of each common skin cancer.
• Explain the difference between shave biopsy, punch biopsy, and excisional biopsy.
• Describe the treatment modalities for the common types of skin cancer.
Structure of the Skin

2/3/2014
2
Epidermis
• Outermost layer of the skin
• Composition
– Stratum basalis (separates dermis from epidermis)
– Stratum spinosum (spiny cell layer)
– Stratum granulosum (granular cell layer)
– Stratum corneum (cornified layer)
Dermis
• Two layers
• Adventitial layer
– Reticular
• Functions
– Temperature control
– Mechanical
– Cutaneous sensation
Subcutaneous
• Composition
– Distinct flat lobules
– Blood vessels, nerves, and lymphatics
• Functions
– Heat insulator
– Shock absorber

2/3/2014
3
Ancillary Skin Structures
• Glands
– Sebaceous (sebum: antifungal properties)
– Eccrine (sweat)
– Apocrine (produce scent in axilla and perineum)
• Hair
• Nails
General Functions of the Skin
• Sensation
• Protection
»Thermoregulation
• Secretion
• Flexibility
Sunlight and the Skin
Photobiology

2/3/2014
4
• Photobiologic skin reactions and diseases
• Caused by ultraviolet light
From the sun in the form of
Solar radiation
Solar Radiation
• Continuous spectrum of wave lengths of electromagnetic energy over 290 nm (nm = unit for measuring the wavelength of light = nanometer)
Ultraviolet light
• Divided into:
– UVA (320 -400 nm)
• Constant throughout the day
• Penetrates window glass
• Interacts with topical and systemic chemicals and medications
• Produces immediate and delayed tanning – Results in Photoaging
• Can reach dermis and subcutaneous fat (longer wavelenths)

2/3/2014
5
– UVB (290 -320 nm)
• Most intense between 10 AM and 4 PM
• Absorbed by window glass
• Prior exposure to UVA enhances sunburn reaction of UVB
• Primarily responsible for sunburn, suntan, and skin cancers
• Delivers high amount of energy to stratum corneum and superficial layers of the epidermis
– UVC (100 – 290 nm)
• Absorbed by the ozone layer
• Only transmitted artificially in germicidal lamps and mercury arc lamps
Effects of Sun Damaged Skin
• Photoaging – Solar elastosis
– Course, deep wrinkling
– Skin thickens
– Persistent pigmentation
– Telangiectasia
– Maturation of keratinocytes
• Sun tan and sun burn
• Skin cancers

2/3/2014
6

2/3/2014
7
Tolerance to Sunlight
• Dependent on individual’s skin type
– Estimated on response to first 30 minutes of exposure to summer sun
Skin Types
• Type 1: always burns easily; never tans, very sensitive
• Type 2: usually burns easily; tans minimally, very sensitive
• Type 3: Burns moderately; tans gradually and uniformly, sensitive
• Type 4: burns minimally; always tans well, moderately sensitive
• Type 5: Rarely burns; tans profusely, minimally sensitive
• Type 6: Never burns: deeply pigmented, insensitive
Types of skin lesions due to
Solar radiation and/or tanning beds

2/3/2014
8
Actinic Keratosis (AK)
• Appears as a poorly circumscribed, pink, red or tan papule that feels or looks scaly, crusty, or crumbly, generally rough and dry
– May itch or present with burning or pricking sensation
– Can bleed, but rarely
– May present as cutaneous horn
– Actinic cheilitis on lips

2/3/2014
9
• Located on sun-exposed areas of the skin
– Face, head, neck, arms, hands, and legs
• Mainly on skin types 1 -3
– Possibility on 4 and 5
• May be visualized but mainly located by feel
AKs considered pre-malignant lesions
• Regarded as precursor to SCC or BCC
– Mainly progress to SCC
– Estimates of transformation range from 0.025% to 20% per year
• 44% - 97% SCCs
• 36% BCCs
– Dictates need to treat these lesions

2/3/2014
10
AKs
• Seen more frequently in males
• Increase in numbers with age
• Skin types 1 – 3 mainly
• History of excessive sun exposure without protection
– Produce atypical squamous cells in the epidermis
• Penetration of the epidermis/dermis junction indicates development of SCC
Diagnosis of AKs
• History of extreme frequent sun exposure
• Clinical picture
– Felt and/or visualized
• Biopsy (shave biopsy)
– Only if indurated lesion
• Would indicate SCC

2/3/2014
11
Differential Diagnoses
• Seborrheic keratosis
• Bowen’s disease
• BCC
• SCC

2/3/2014
12
Treatment of AKs
Cryotherapy
• Use of liquid nitrogen to freeze the lesions – Boiling point of liquid nitrogen is – 196 C
– Freezes lesions to about -50 C
• Administered by direct spray or contact swab – 10 to 15 second exposure
• Margin beyond lesion of 1 -3 mm
• Allow slow thawing 20 -40 seconds
• Pain is moderate to severe during freezing
• May produce dyspigmentation
Cryotherapy after effects
• Erythema
• Edema (localized)
• Blister formation (7 -10 days for formation)
• May experience fluid drainage
• Dry crust forms
• 99% cure rate fro treated lesions

2/3/2014
13
Electrodesication and Curettage (ED&C)
• Requires local anesthesia (Lidocaine with epinephrine) • Equipment required:
– Electricator, Hyfrecator, Bantam Bovie, Ritter coagulator – Sharp dermal curets (1 7 mm)
• Using a small size curet, held like a pencil, skin around the lesion is held taut with fingers of free hand
• Use smooth, firm strokes with curet until firm tissue base is acquired and resistance occurs
• Then dessication is achieved by inserting needle of electrosurgical unit into the tissue – Char produced result in hemostasis
Care of ED&C site
• Heals by secondary intention
• Wound should be cleansed daily with soap and water
• Antibiotic ointment may be applied
• Light dressing in place until dry
• Follow-up visit in 7 -10 days
• Patient should be instructed in signs of infection

2/3/2014
14
Photodynamic Therapy (PDT)
• Light therapy for treatment of lesions
• Requires
– Photosensitizing drug and light source – 20% 5-aminolevulinic acid (hydrochloride salt) and a vehicle
– Light of proper wave length and power
» Blue light (BLU-U)
• Provides uniform blue light distribution for 1000 sec
• Power density fixed at 10mW/cm2
– Tissue oxygen
PDT
• Functions by light activating the drug in the tissue which creates a singlet oxygen which is highly cytotoxic, results in tissue destruction
• Safety precautions
– Protective eye goggles for both patient and provider

2/3/2014
15
Patient discomfort with PDT
• Stinging and burning occurs most severely in the initial stages; plateaus at approximately 6 minutes
• Symptoms diminish at completion of treatment
• Within 24 hours discomfort should abate entirely
PDT Discomfort Relief Measures
• NSAIDs prior to or after procedure
– May also use acetaminophen, diazepam, dipherhydramine HCl, hydrocodone
• Use of topical lidocaine 4% or ELA-Max
• Ice packs
• Cold compresses
• Post treatment topical steroid cream
Common local responses to PDT
• Crusting
• Pruritus
• Scaling
• Rarely, vesicle or blister formation

2/3/2014
16
TOPICAL MEDICATIONS for
Actinic Keratosis
5-FU 5%, 1%, 0.5% cream
• Applied QD or BID for 3 -5 weeks
• Inhibits thymidylate synthetase thus preventing cell proliferation and causing selective cell death
• Produces inflammation, erythema, and edema initially
• Continued until erosion, necrosis, and ulceration of lesions occurs
• Complete healing in 1 -2 months after cessation of medication
• Adverse reactions are local: burning, crusting, and allergic contact dermatitis
• May use weekly pulse dosing
– Apply BID two consecutive days a week
– F/U in 3 – 4 weeks

2/3/2014
17

2/3/2014
18
IMIQUIMOD Cream 5%
• Applied 3x / week at HS for 4 – 6 weeks
• Left on 8 hours and then washed off
• Produces interferon which destroys precancerous and cancer cells, is an immune response modifier
• More readily accepted by patient – Lesser number of applications
– Skin response less intense than 5-FU
– Similar results to 5-FU
Diclofenac Sodium Gel 3%
• Applied BID for 60 – 90 days
• Inhibits cyclooxygenase and acts through induction of apoptosis, inhibition of angiogenesis and up-regulation of arachidonic acid pathway
• Adverse reactions: contact dermatitis, dry skin, edema, exfoliation, pain, paresthesia, pruritis, rash

2/3/2014
19
CHEMICAL PEEL for
Actinic Keratosis
• Alpha hydroxy acids topically cause epidermolysis and elimination or keratosis
• Includes – 30 – 70% Glycolic acid
– Trichloroacetic acid 35 %
– Jessner’s solution
• 5-FU often used for 5 – 7 days prior to peel to “light up” the lesions
• Acid is applied to the lesions with cotton swab and left on for 5 – 10 minutes
• Then removed with alcohol – Produces a controlled, partial thickness exfoliation of
epidermis and outer dermis
Local complications of chemical peel
• Pigmentation changes
• Scarring
• Milia
• Ectropion
• Infection
• Activation of herpes simplex
• Toxic shock syndrome

2/3/2014
20
Chemical facial exfoliation can be:
• DEEP
– Phenol in Baker’s formula is used
– Burn extends 2 – 3 mm
– May cause cardiac arrhythmias
– Full epithelialization occurs in 6 – 7 days
– Provides substantial improvement in rhytidosis and actinic damage
• MEDIUM – DEPTH
– Trichloroacetic acid 35% - 50%
– Lightens pigmentation and improves rhytides
– Minimal systemic toxicity
– Local complications: scarring and pigmentation problems.
• SUPERFICIAL
– Trichloroacetic acid 10% - 25% or
– Glycolic acid 50% - 70%
– Depth of penetration titrated by timed duration of acid placement
• Left on 3 – 7 minutes
• Repeated 3 - 4 times
– Removes AKs, fine wrinkles, lentigines, melasma, and seborrheic keratoses

2/3/2014
21
BASAL CELL CARCINOMA (BCC)
• Most common form of skin cancer
• Locally invasive, aggressive, and destructive
– Extremely rare metastasis
• Persistently bleeding and scabbing, non-healing papule is most common presentation

2/3/2014
22
Risk Factors for BCC
• Fair skin (mainly types 1 -3)
• Degree of sun exposure
• Men have higher incidence than women
• Tanning beds ( emit both UVA and UVB radiation)
• Over 40 years of age
Location of BCCs
• Head and neck: most commonly
– 25 – 30% on the nose
• Shoulders
• Back
• Upper chest
• Arms and legs

2/3/2014
23
Pathophysiology of BCC
• Arises from basal keratinocytes of the epidermis and adnexal structures (hair follicles and eccrine sweat ducts)
Histologic Types
• Nodular (21%)
• Superficial (17%)
• Micronodular (15%)
• Infiltrative (7%)
• Morpheaform (1%)
– Mixed pattern can be present in 38.5% if the lesions of BCC

2/3/2014
24
Morphology of BCC
• Papule or nodule with rolled border
• Translucent or “pearly” with possible crust
• Round or ovoid with depressed center
• Erythematous (red to pink)
• Telangiectasia present
• May be pigmented brown, black, or blue
• Generally firm or hard

2/3/2014
25
Diagnosis of BCC
• Visual exam – Good lighting, hand magnifier, palpation
• Biopsy – Shave biopsy
• Removal of small piece of suspect lesion
– Excisional biopsy • Removal of entire suspect lesion
– Punch biopsy • Removal of entire suspect lesion down to subcutaneous
level
• All biopsies require local anesthesia – Generally Lidocaine with epinephrine
• A scalpel blade or a punch instrument if punch biopsy being performed
• Medication for hemostasis – 25% - 30% aluminum chloride
– Silver nitrate sticks
• Sutures if punch biopsy or excisional biopsy performed

2/3/2014
26

2/3/2014
27
Differential diagnoses for BCCs
• Sebaceous hyperplasia
• Seborrheic keratosis
• Bowen’s disease
• Granuloma annulare
• Actinic keratosis
• Nevus
• Melanoma

2/3/2014
28
Treatment Modalities for BCC
• Excisional surgery
• Moh’s Micrographic surgery
• ED&C (can be combined with cryotherapy or topical medications)
• Cryotherapy (can be combined with topical medications)
• Photodynamic Therapy (PDT)
• Topical medications (5-FU or Imiquimod)
• Rarely radiation or laser surgery
Variant of BCC Gorlin’s syndrome
• Basal cell nevoid syndrome – Rare inherited disease
– Autosomal dominant • Gene located on chromosome 9q22.3q31
• Characterized by – Multiple nevoid BCCs
– Pits in palms of hands and soles of feet
– Multiple jaw cysts
– Facial structure changes
– Skeletal abnormalities

2/3/2014
29

2/3/2014
30
SQUAMOUS CELL CARCINOMA (scc)
• Second most common form of skin cancer
• Lesion is metastatic – 5 year survival rate 14 – 39%
– Matastasizes to regional lymph nodes
– Then to liver, lungs, bone, and brain
• Most common in sun-exposed areas – Scalp, dorsal hands, and pinna

2/3/2014
31
Risk Factors of SCC
• Sun exposure, especially UVB radiation
• Immunosuppression
• Other lesions: AKs, Bowen’s disease, keratoacanthomas, lichen sclerosis et atrophicus (vulva), leukoplakia
• Chemical exposure: arsenic and therapeutic tar
• Sites of chronic infections: sinus tracks and bone

2/3/2014
32
Location of SCC
• Most commonly: rim of ear and lips
• Face and neck
• Bald scalp
• Shoulders, arms, hands
• Back

2/3/2014
33
Pathophysiology of SCC
• Originates in epidermis from keratinocytes
• Proliferates indefinitely
• Penetrated the epidermal basement membrane
• Proliferates into the dermis
Histologic Types of SCC
• Highly differentiated SCC
– Firm or hard on palpation
• Poorly differentiated SCC
– Fleshy, granulomatous, and soft on palpation
Morphology of SCC
• Indurated papule, plaque, or nodule
• May have thick keratotic scale or hyperkeratosis
• Firm, hard, often freely moveable or soft and, fleshy
• Erythematous base, yellowish skin color
• Polygonal, oval, round or umbilicated
• Telangiectasia
• Freckling
• Dry, scaly atrophic skin
• Regional lymphadenopathy

2/3/2014
34
Diagnosis of SCC
• Visual examination
• Palpate lymph nodes
• Biopsy
– Shave
– Excisional
– Punch
Differential Diagnosis of SCC
• Keratoacanthoma
• Wart
• Seborrheic keratosis
• Nummular eczema
• Psoriasis
• Paget’s disease

2/3/2014
35

2/3/2014
36
Treatment Modalities for SCC
• Excisional surgery
• Mohs micrographic surgery
• Radiation
• ED&C
• Photodynamic therapy (PDT)
• Topical medication: 5-FU or Imiquimod
• Laser surgery

2/3/2014
37
Variables for Recurrence and Metastasis of SCC
• Size: <2cm or >2cm • Depth: <4mm/Clark level I to II or >4mm/Clark level of
IV or V • Differentiation: well differentiated or poorly
differentiated (greater risk with poorly) • Site: Ear (greater for recurrence) or lip (greater for
metastasis) • Scar carcinoma (metastasis) • Previous treatment • Perineural involvement • Immunosuppression (metastasis)
Variants of SCC
• Bowen’s disease (SC in situ)
• Erythroplasia (Queyrat)
• Marjolin’s ulcer

2/3/2014
38
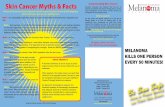
MALIGNANT MELANOMA

2/3/2014
39
• One of the most dangerous tumors
• Ability to metastasize to any organ
• Can present anywhere on the body
• May arise from a newly developed lesion or a pre-existing lesion
• Only common cancer in the US whose incidence is increasing
• Most common cancer in adults aged 25 – 29 and second most common in ages 15 - 29
Risk Factors for Melanoma
• High levels of sun exposure • TANNING BEDS • Experiencing sunburns (more than 3 in lifetime) • Having numerous nevi (moles) • White race • History of melanoma in first degree relative • Immunosuppression • Previous cutaneous melanoma • Sun sensitivity

2/3/2014
40
Location of melanoma
• ANYWHERE on the body
– Be especially vigilant with feet, between toes, perineal area, gluteal fold, and mouth

2/3/2014
41
Pathophysiology of Melanoma
• Originates in melanocytes
– Primarily found in basal layer of skin
– Also located in GI tract, eyes, ears, and oral and genital mucosa
• Melanocyte degenerates and becomes neoplastic
– Then can move into any area

2/3/2014
42
Histologic Types
• Type I: Superficial spreading (70%)
– Most common in middle age
– Occurs anywhere on the body
• Upper back, both sexes
• Women’s legs
– Bizarre lesion shapes, especially over time
– Multiple colors, including dull red
• Type II: Lentigo maligna (10%)
– Most common in 60 or 70 year olds
– Mainly on the facial area
– Mainly radial growth
– Mainly brown or black in color

2/3/2014
43
• Type III: Acral lentiginous melanoma (2 -8%)
– Seen in 29% to 72% in black and Asian patients
– Found on palms, soles, terminal phalanges, and mucous membranes
– Sudden appearance of Hutchinson’s sign
• Pigmented band in proximal nail fold

2/3/2014
44
• Type IV: Nodular melanoma (10 – 15%)
– Multiple colors: Blue-black, purple, red-brown, flesh-colored
– Raised above the skin
– May be ulcerated, crusty, and frequently bleeds
– More frequent in males
– Dome-shaped, polyploidy, pedunculated

2/3/2014
45
Morphology of Melanoma
• ABCDs of melanoma – A: asymmetry – B: border – C: color – D: diameter – E: elevation and enlargement
• Changes in surface characteristics • Development of symptoms
– Itching (pruritus), tenderness, pain
•

2/3/2014
46

2/3/2014
47
Diagnosis of Melanoma
• Visual examination – Using ABCDs of melanoma
• Use of dermatoscopy – Apply fluid to skin – Position dermatoscope over lesion – Three point checklist (novice)
• Asymmetry of color and structure • Atypical network of cells • Blue-white structure
– Pattern analysis
• Biopsy – Total excisional biopsy with narrow margins – Punch biopsy
Differential Diagnosis of Melanoma
• Congenital nevus
• Common acquired nevus
• Superficial spreading nevus
• Clark’s nevus
• Blue nevus
• Spitz nevus
• Pigmented BCC
• Pyogenic granuloma

2/3/2014
48

2/3/2014
49

2/3/2014
50
Treatment Modalities for Melanoma
• Depends upon staging of melanoma
– Looks at thickness, depth, and spread
• Diagnostic Indicators
– Clark’s level
• I: confined to the epidermis
• II: invasion of papillary dermis (upper)
• III: filling of the papillary dermis (lower)
• IV: extending into the reticular dermis
• V: invasion of the subcutaneous tissue
– Breslow Thickness
• Better melanoma stage diagnostic indicator
• Measure (in millimeters) of the vertical depth of tumor measured from the granular cell (very top) layer downward
• Breslow thickness and Survival rate – < 1mm: 5 year survival is 95 -100%
– 1 – 2mm: 5 year survival is 80 – 96%
– 2.1 – 4mm: 5 year survival is 60 – 75%
– > 4mm: 5 year survival is 37 – 50%
Staging of Tumor
• Process used to describe the extent of the disease
• Consider thickness, depth, and spread • Guides providers to appropriate treatment plan
and determines prognosis • Goes from 0 to 4 • Key information indicators
– T = tumor (thickness, number assigned, appearance of tumor [letter assigned]
– N = lymph nodes ( 0 – 3) – M = metastasis (spread of tumor)

2/3/2014
51
Types of Therapy for Melanoma
• Surgical excision – Simple excision – Mohs surgery – Wide local excision – Excision with sentinel lymph node biopsy
• Immunotherapy – Treats the whole body – Use of biologic agents that stimulated the immune system
• Include interferons and interleukins – Interferon alpha 2-b: Stage II and III – Interleukin – 2: Stage IV
» Requires hospitalization » Two cycles of high dose IV therapy drug » Must be closely monitored
• Chemotherapy – Decarbazine (DTIC)
– Taxanes (docetaxel and paclitaxes)
– Platinum agents • May be administered by isolated limb perfusion (ILP)
• Radiation therapy – Gamma knife
– Cyber knife
• Regional perfusion (ILP) – Melphalen: drug gold standard for ILP
• Clinical trials
Side Effects of Melanoma Treatment
• Pain
• Scarring
• Infection
• Lymphedema
• Fatigue
• GI discomfort
– Nausea, vomiting, diarrhea, constipation

2/3/2014
52
On-going Melanoma Monitoring
• Total body skin exams by dermatologist – Q 3 months – first year – Q 6 months – 2 – 5 years – Yearly – 6 years and on
• Lab Studies – CBC, electrolytes, renal function, liver function and
LDH levels
• Annual chest x-rays • Radiologic imaging
– Bone scan, CT scans, MRIs, PET scans
General Skin Cancer Prevention
• Avoid sun exposure during peak sun hours • Wear sun protectant clothes • Always wear wide-brimmed hat • Utilize sunscreen daily
– SPF (Sun protection factor) • Ratio of time required to produce erythema through a
sunscreen product to the time required to produce the same degree of erythema without the sunscreen
• SPF ranges from 15 – 65 or 70 • SPF 15 provides 50% protection • SPF 34 provided 97% protection
Agents for Protection Against Solar Radiation
• UVB protective agents – Para-aminobenzoic acid (PA
– PABA esters
– Cinnamates
– Salicylates
– Phenylbenzimidazole sulfonic acid
• UVA protectant agent – Benzophenes
– Dibenzolmethanes
– Avobenzones

2/3/2014
53
• Physical Blockers
– Zinc oxide
– Titanium dioxide
– Iron oxide
– Kaolin
– Veterinary petrolatum
Thank You for Your Attention
ANY QUESTIONS?