“Common” Pearls: Clinical Pharmacology - okpa.org · PDF fileReview common adverse...
Transcript of “Common” Pearls: Clinical Pharmacology - okpa.org · PDF fileReview common adverse...
“Common” Pearls:
Clinical Pharmacology
Chad Douglas, MD, PharmD
Medical Director-OUHSC Student/Employee Health Clinic
Clinical Assistant Professor Department of Family and Preventative Medicine
Objectives
1. Outline the most common empiric therapies for common
bacterial, viral and fungal infections
2. Discuss commonly overdosed mediations and their antidotes
3. Review common adverse reactions and side effects of
pharmacologic therapies
4. Answer general board preparation questions regarding clinical
pharmacology
1st Cephalexin(Keflex®)*, Cefadroxil (Duricef®) Cefazolin (Ancef®) IV
2nd Cefaclor (Ceclor®)*, Cefprozil (Cefzil®), Cefuroxime axetil (Ceftin®)*
3rd Cefixime (Suprax®)*, Ceftibuten (Cedax®), Cefdinir (Omnicef®)
Ceftriaxone(Rocephin®) IM
Cephalosporin Generations (po)
(<10% cross reactivity with PCN allergy and allergy to 1st generation
cephalosporin-cephalexin (Keflex®). <5% cross reactivity with 3rd generation
agents and higher)
Cephalosporin Generations
1st generation gram + (skin infections, Group A Strep Pharyngitis)
-Cephalexin(Keflex®)*, Cefadroxil (Duricef®) Cefazolin (Ancef®) IV
2nd generation gain some gram (–) (H. Influenza, M. catarrhalis)
Some S. pneumo (URI, OM, mild sinusitis, mild bronchitis)
- Cefaclor (Ceclor®)*, Cefprozil (Cefzil®), Cefuroxime axetil (Ceftin®)*
3rd generation gain more gram (-), gain better S. pneumo
coverage (URI, OM, Sinusitis, Bronchitis, CAP (not atypical)
-Cefixime (Suprax®), Cefdinir (Omnicef®), Ceftriaxone (Rocephin®) IM
Cephalosporin Generations Cont.
4rd generation- Cefepime (Maxipime®) (IV) broad spectrum but not
for anaerobes
5rd generation- Ceftaroline fosamil (Teflaro®) (IM, IV) – covers
MRSA, Only cephalosporin that covers MRSA. FDA Indications- CAP,
Skin Infections
Anaerobic coverage- 2nd gen- Cefoxitin and Cefotetan (IM/IV), Pseudomonas –
3rd gen Ceftazidime(IM/IV) 4th gen- Cefepime (IM/IV)
Bacterial Infection Treatment
MRSA
Trimethoprim/Sulfamethoxazole- TMP/SMX (Bactrim
DS, Septra DS®)
Doxycycline (Vibramycin®)
Clindamycin (Cleocin®) po
Linezolid (Zyvox®) mupirocin (Bactroban®)
Ceftriaxone (Rocephin®) IM -Will NOT cover MRSA!
(Beta lactams (dicloxacillin) work better for MSSA)
Streptococcal Skin Infections
Cephalexin (Keflex®)
Doxycycline (Vibramycin®)
Clindamycin (Cleocin®)
(Not TMP/SMX (Bactrim®)
Maxillary Sinusitis
Azithromycin (Zithromax®)
Augmentin, 2nd or 3rd gen ceph, Fluoroquinolone (not
Ciprofloxacin)
Streptococcal pharyngitis PCN VK, Amoxicillin, 2nd or 3rd gen ceph, clindamycin
(not azithromycin*) PCN G IM x 1 dose
Bacterial Infection Treatment
Otitis Media Amoxil®/Augmentin®, Azithromycin, 2nd or 3rd
gen cephalosporin, Ceftriaxone IM- peds
Otitis Externa (‘Swimmer’s Ear’)
Drops- Neomycin, Polymyxin B/HC,
Ciproflox/Dexamethasone (Ciprodex ®),
Ofloxacin (Floxin) Otic®
Pneumonia- Community acquired, strep pneumo
(Acute Bronchitis)
Levofloxacin (Levaquin®), Moxifloxacin
(Avelox®) (Not Cipro),
3rd gen or higher Cephalosporin, Doxycycline,
Azithromycin-peds
Pneumonia (atypical) Azithromycin, Doxycycline, Respiratory
Fluoroquinolones (Not Cipro),
Pseudomonas Ciprofloxacin (Cipro®)
Pertussis Azithromycin
Bacterial Infection Treatment
UTI (uncomplicated)
Nitrofurantoin* (CrCl >60), TMP/SMX*, Ciprofloxacin*,
Levofloxacin, (NOT Moxifloxacin -Avelox®),
Cephalosporin *Get Culture*
Acute Prostatitis
Ciprofloxacin (Cipro®)
Doxycycline + Ceftriaxone (Rocephin®) IM (any concerns
for STD’s)
TMP/SMX (Bactrim®)
Extended po course 21-30 days for all po abx
Rickettsial infections (RMSF, Ehrlichiosis,
Lyme*)
Doxycycline* ( >8 y/o) or Chloramphenicol ?
Giardiasis
Metronidazole (Flagyl®)
Clostridium Difficile (C. diff) Metronidazole, po Vancomycin
H. Pylori
- Amoxicillin + Clarithromycin(or Levaquin) +/-
Metronidazole+ PPI (Prevpac®)
- Bismulth + TCN+ Metronidazole+PPI (Pylera®)
Bacterial Infection Treatment
Bacterial Vaginosis Metronidazole (Flagyl®) or vaginal gel (¼)
Gonorrhea Ceftriaxone (Rocephin®)* IM, cefixime
(Suprax®), Doxycycline
Chlamydia Azithromycin*, Doxycycline
Trichomonas Metronidazole (Flagyl®)
Syphilis PCN G IM, Doxycycline in pen allergic
Pelvic Inflammatory Disease
Ceftriaxone (Rocephin®)IM, + Metronidazole +
Doxycycline at least 14 day treatment
Diverticulitis
Ciprofloxacin (Levoflox or Moxiflox) +
Metronidazole
Anaerobic infections above the diaphragm Clindamycin (gram + anaerobes)
Anaerobic infections below the diaphragm Metronidazole (gram – anaerobes)
Common Viruses and Antiviral Agents
Virus Treatment
Cytomegalovirus
Cidofovir (Vistide®)
Ganciclovir (Cytovene®) *
Foscarnet (Foscavir®)*
Fomivirsen (Vitravene®)
Hepatitis B virus
Adefovir dipivoxil
Interferon alfa-2b (Intron A)*
Lamivudine (Epivir HBV) *
Hepatitis C virus
Interferon alfa-2b/ribavirin*
Pegylated interferon
Sofosbuvir (Sovaldi®)
Simeprevir (Olysio®)
Virus Treatment
Herpes simplex virus (HSV I, HSV II)
Acyclovir (Zovirax®) * po, topical
Famciclovir (Famvir®)
Valacyclovir (Valtrex®) *
Influenza A virus Amantadine (Symmetrel)
Rimantadine (Flumadine)
Influenza A and B virus Oseltamivir (Tamiflu®)*
Zanamivir (Relenza®)
Respiratory syncytial virus (RSV)
Ribavirin
Varicella-zoster virus (Shingles)
Acyclovir (Zovirax®)
Valacyclovir (Valtrex®)
Human Papillomavirus (HPV)
Imiquimod (Aldara®)
Common Fungal infections and Antifungal
Agents
Tinea corporis/cruris/pedis- clotrimazole (Lotrimin®), terbinafine
(Lamisil®) po/topical. Onychomycosis – Get PAS stain, terbinafine po
or efinaconazole (Jublia®)
Tinea capitis- Griseofulvin po 4-6 weeks, Topical treatment not
effective for capitis
Tinea (pityriasis) versicolor (Malassezia furfur)- Ketoconazole topical
or po*, candidiasis-nystatin topical, azoles (fluconazole), Intravaginal
(Miconazole)
Nystatin does not cover Tinea (‘ring worm’), only candida, PO ‘Azoles’
cover both. Fungi (Dermatophytes) that cause human ring worm do
not come from animals
Medication Overdoses/Poison Exposures and Antidotes
Medication Antidotes
Acetaminophen N-Acetylcysteine (NAC)
Benzodiazepines Flumazenil* (Don’t Use!- causes seizures)
Digoxin Digoxin immune fab
Local Epinephrine Vasospasm Phentolamine
Heparin Protamine
Iron Deferoxamine
Methotrexate Leucovorin
Morphine (opiates) Naloxone (Narcan®)
Nitrogen mustard Sodium thiosulfate
Organophosphates Pralidoxime/2-PAM
Warfarin Phytonadione/vitamin K, FFP*
Crotalid Snakes (Rattlesnake, Water Moccasin
‘Cottonmouth’, Copperhead) Crotalidae polyvalent immune FAB (CroFab®)
Drugs That Can Cause Hepatic Failure/Hepatic toxicity
Acetaminophen*
Alcohol
Allopurinol
Carbamazepine*
Erythromycin (estolate salt)*
Flucytosine
Gancyclovir
Isoniazid
Ketoconazole*
Methotrexate
Niacin*
Oral contraceptives
Parenteral nutrition
Rifampin
Sulfonylureas
Valproate*
Drugs That Can Affect Renal Function/Nephrotoxity
Aminoglycosides*
Amphotericin B *
Cisplatin*
Contrast media * (CT iodinated contrast)
Cyclosporine
Foscarnet
Gold salts *
NSAIDs*
Pentamidine
Fluoroquinolones
Common Drugs ‘Safe’ in Pregnancy* Common Use
Beta Lactam abx (PCN’s, Cephalosporins) URI, OM, Sinusitis, Bronchitis, cellulitis (strep),
Methicillin Sensitive Staph Aureus (1/2)
1st generation antihistamines
Diphenhydramine (Benadryl®), Chlorpheniramine
(Chlor-Trimeton®)
Doxylamine* (some Uni-Som®, otc sleep aids)
Meclizine (Antivert®, OTC Dramamine II ®)
Promethazine (Phenergan®)**
2nd generation antihistamines (non sedating) Loratadine (Claritin®), Fexofenadine (Allegra®), Cetirizine (Zyrtec®) Pure antihistamine vs anticholinergic effects, allergies vs viral infections
Azithromycin URI, OM, Sinusitis, Pertussis, Chlamydia
Metronidazole (intravaginal for 1st trimester) po
ok 2nd and 3rd BV, Trichomonas, Diverticulitis
TMP/SMX (Bactrim DS®)* avoid use in 3rd
trimester Increases risk of kernicterus (brain damage from inc bilirubin- jaundice) MRSA, UTI’s
Nitrofurantoin (Macrobid®)* ok until 38 weeks
gestation UTI’s
Drugs That Can Cause Folic Acid Deficiency
Barbiturates
Methotrexate*
Oral contraceptives
Phenytoin
Primidone
Pyrimethamine*
Sulfasalazine
Trimethoprim (Hyperkalemia in high doses)
Drugs That Have Been Associated with
Immunologic (SLE – Like) Reaction
Ethosuximide (For absence seizures)
Hydralazine* (Rebound tachycardia if not on beta blocker, diltiazem or verapamil)
Isoniazid*
Methyldopa (Gold standard for HTN in pregnancy on boards)
Nitrofurantoin (rarely pulm fibrosis)
Penicillamine
Phenothiazines
Phenytoin
Procainamide
Quinidine
Sulfonamides
Tetracyclines
Drugs with notorious/common rxn Reaction
ACE Inhibitors- Lisinopril, enalapril,
ramipril, captopril Dry cough, angioedema*
Digoxin GI upset, halo w/ toxicity (around points of light)
PDE 5 inhibitors- sildenafil Blue tint to vision
Amlodipine (Norvasc®) Non pitting lower extremity edema
Diltiazem, Verapamil Slow conduction, HR. Verapamil- constipation
Anticholinergics Can’t see, can’t pee, can’t ____, can’t spit
Metoclopramide (Reglan®) Extrapyramidal sx (Can be permanent!)
Bupropion (Wellbutrin®) Seizures, avoid excessive ETOH
Tramadol (Ultram®), Linezolid
(Zyvox®) Serotonin syndrome combined with SSRIs, TCA’s- (theoretically)
Drugs with notorious/common rxn Reaction
Statins Myalgia
Metronidazole Disulfiram rxn c ETOH, metallic taste in mouth
Morphine Itching- Histamine release
Oxymetazoline (Afrin®)
Nasal phenylephrine (Neo-
Synephrine ®)
Rhinitis Medicamentosa (po toxicity in peds)
Phenazopyridine (Pyridium®) Orange/red urine, tears
Prednisone
- Inc WBC (Neutrophil demargination from endovascular lining, delayed migration into tissues, and inc bands released from bone marrow)
-Inc Blood glucose (mainly post prandial)
Medications That Should Not Be
Administered with Antacids/Ca++
Digoxin
Fluoroquinolones
Iron preparations*, sulfate, fumarate, gluconate
Isoniazid
Ketoconazole
Quinidine
Tetracyclines ie Doxycycline*
Drugs That Have Been Associated with
Hyperglycemia
Amiodarone
l-asparaginase
Epinephrine
Estrogens
Glucocorticoids* ie Prednisone
Lithium
Nicotinic acid
Oral contraceptives
Pentamidine
Phenytoin
Thyroid hormones
Drugs That Food Decreases Absorption
Ampicillin
Astemizole
Cefaclor
Didanosine
Digoxin (level 6˚after last dose)
Diltiazem
Etidronate
Furosemide
Indinavir
Isoniazid
Labetalol
Lansoprazole
Levodopa
Levothyroxine*
Lithium (level 12˚after PM dose)
Metoprolol
Penicillamine
Propranolol
Rifampin
Zafirlukast
Grapefruit Juice
Inhibition of CYP3A in small intestines
One whole grapefruit or 7oz juice (60ml Lime juice)
3 days for enzyme to recover
Only oral meds, Not Liver CYP3A
INCREASES drug levels
Amiodarone (50% inc AUC)
Colchicine (> 50% inc AUC)
CCB, Statins(ator, simva, lovastatin)
Oxycodone
3/4
Grapefruit,Orange, & Apple Juices
Inhibition of Organic Anion Transporting Poylpeptides (OATPs)
These transport some drugs into cells to increase absorption
Inhibition for 4 hours with only 1 fruit or 7oz juice
DECREASES drug levels
Levothyroxine (11% dec in absorption)
Ciprofloxacin (20% dec)
Fexofenadine (Allergra®) (40% dec)
Atenolol (40% dec)
Agents That Inhibit CYP-
450 Enzymes
Allopurinol
‘Azole’ antifungals*
Chloramphenicol
Cimetidine*
Disulfiram
Isoniazid
Metronidazole
Monoamine oxidase inhibitors
Oral antidiabetic agents
Warfarin
Agents That Induce CYP-450 Enzymes
Alcohol
Chloral hydrate
Chlordiazepoxide
Cortisone
Imipramine
Nicotine
Phenobarbital*
Phenytoin*
Prednisone
Rifampin*
Testosterone
Types of Drug-Drug, Drug-Food Interactions
Problems with absorption
Ca, Mg (divalent cations) with doxycycline, digoxin
Food inhibiting or increasing absorption
Levothyroxine-empty stomach Griseofulvin- with high fat meal
PPI’s decreasing acidic environment, decreased Ca, Fe, Mg absorption
Sucralfate (Carafate®) binding and barrier to absorption
CYP450 Liver Enzyme System
Azoles, cimetidine- broad inhibition
Phenobarbital, phenytoin, rifampin – broad inducers
Can inc or dec drug levels, keep pro drug from becoming active or increase production of active metabolite (codeine- CYP450 2D6)
CYP450 pharmacogenetic testing
Types of Drug-Drug, Drug-Food Interactions Cont
Protein Binding
Warfarin and SMX/TMP (Bactrim®)
Similar mechanism of action/therapeutic duplication
SSRI’s with TCAs and trazodone
Benzodiazepines with alcohol or any CNS depressing medication
Tramadol with SSRI’s (theoretically)
Amphetamine salts with bupropion and prednisone + pseudoephedrine
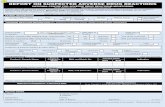
Drug Allergies
Drug Allergies – Ask rxn Allergy vs Adverse Drug
Reaction/Common Side Effect
True Allergy – Takes out whole drug (chemical) class
Adverse rxn – Just cannot use that specific drug
Document and categorize rxn and allergy vs adverse rxn in
EMR
PCN allergies
Low cross reactivity with cephalosporins <5%
Up to 70% of pts can loose their PCN allergy after 10 yrs*
Drug Allergies Continued
Sulfa Allergies
Sulfonylarylamines* (includes sulfa abx) 3% have true allergy
Avoid SMX/TMP, Sodium sulfacetamide, silver sulfadiazine
(Silvadene®), Sulfasalazine (Azulfidine®)
Nonsulfonylarylamines
Acetazolamide (Diamox®)*, Celecoxib (Celebrex®)*, Loop diuretics-
furosemide, torsemide, bumetamide, Thiazide diuretics- HCTZ*,
chlorthalidone*, Indapamide*, Sulfonylureas-glimepiride*, glyburide,
glipizide.
*Contraindication in U.S.package insert in one with true sulfonylarylamine
allergy
Metoprolol succinate (Toprol XL®) vs tartrate (Lopressor®) salt forms , q day vs bid
Doxycycline salt forms. Extended vs Immediate Release. DETAILS MATTER
Put indication in ‘sig’ (directions) field to be printed on label by the pharmacy. Also, can put
‘dose increase’ ‘dose decrease’, ‘replaces amlodipine’, etc. Avoids confusion from pharmacy
and pts. Can also put specialist/other prescribing/managing provider in sig field
Double check your MAs/Nurses entering medications in EMR. Have all new pt’s, established
complicated pts with multiple specialists, and transition of care pts bring in all medicine bottles
Most Medication errors occur with transitions of care!
Dr. Douglas’ Soap Box
Drugs To Avoid in Pregnancy
ACE Inhibitors/ARBs
Benzodiazepines
Ergotamine
Fluorouracil
Fluoroquinolones
Hormonal agents
Isotretinoin like agents,
Accutane
Methotrexate
Misoprostol
Paroxetine
Raloxifene
Statins
Tetracyclines - Doxycycline,
Minocycline
Thalidomide
Vitamin A palmitate
Warfarin
Common Drugs That Have Been Associated
with Photosensitivity Reactions
Amiodarone
Amitriptyline
Doxepine
Fluoxetine
Furosemide
Griseofulvin
Isotretinoin*
Ketoprofen
Naproxen
Oral contraceptives
Phenothiazines
(prochlorperazine, Compazine®)
Piroxicam
Sulfonamides*
TCN’s- Minocycline*,Doxycycline
Thiazides
Agents That Can Cause Pancreatitis
ETOH*
Azathioprine
Cimetidine
DPP-4 Inhibitors*
Dideoxyinosine (DDI)
Estrogens
Furosemide
Glucocorticoids
GLP-1 agonists
Mercaptopurine
Metronidazole
Parenteral nutrition
Ranitidine
Sulfonamides
Tetracyclines
Thiazides
Valproate