Coding Behavioral Health Services - StarkMHAR · • Exam of gait & station Psychiatric •...
Transcript of Coding Behavioral Health Services - StarkMHAR · • Exam of gait & station Psychiatric •...
CPT Changes for 2017
Significant revision in 2013
2017
Individual vs. family psychotherapy
Family member changed to informant
Direction on reporting time spent providing
psychotherapy services
Direction on how to report both individual & family
psychotherapy on the same date of service
Direction of reporting E/M level and time based
psychotherapy code on the same date of service
1995 vs. 1997 Guidelines
Biggest difference is in Examination Documentation
1995- multi-system exam
1997- specialty specific exam
Medicare only requires that one set is followed
Documentation
Components to selecting E/M levels
History
Examination
Medical decision making
Counseling
Coordination of care
Nature of presenting problem
Time
Key Components
Documentation of History
The CPT Manual’s levels are based on 4 types of history
documentation
Problem Focused
Focused Expanded Problem
Detailed
Comprehensive
Documentation of History (cont.)
Chief Complaint is required for all levels of the history
CC, ROS, PFSH- listed separate vs. included in HPI
Using previous ROS and/or PFSH documentation
Document any changes and date of earlier ROS/PFSH
Ancillary staff or patient forms may provide ROS & PFSH
Must be noted info recorded by someone else
Notation that physician reviewed documentation
History of Present Illness
Description of the development of the patient’s present illness.
Elements
Location
Quality
Severity
Duration
Timing
Context
Modifying factors
Associated signs and symptoms
Status of at least 3 chronic or inactive conditions
Review of Systems
Identifies signs/symptoms by organ system that the patient is
experiencing or has experience
• Constitutional
symptoms
• Eyes
• Ears/Nose/Mouth/Thro
at
• Cardiovascular
• Respiratory
• Gastrointestinal
• Genitourinary
• Musculoskeletal
• Integumentary
• Neurological
• Psychiatric
• Endocrine
• Hematologic/Lymphatic
• Allergic/Immunologic
Past Medical, Family, Social
History
Past history- illnesses, operations, injuries
Family history- illness of pt’s family; may be hereditary or place
the pt at risk
Social- smoking, drinking, living situation, marital status
Documentation of
Examination
Levels are based on 4 types of exam documentation
Problem focused
Expanded Problem
Detailed
Comprehensive
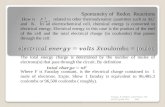
1997 Guidelines-
General Multi-system Exam vs.
Single Organ System Examination
General Multi System
Exam
Level Single Organ System
1-5 elements identified by · in one or more organ
system(s) or body area(s)
Problem
Focused
1-5 elements identified by ·
6 or more elements
identified by · in one or
more organ system(s) or
body area(s)
Expanded
Problem
Focused
6 or more elements identified
by ·
2+ elements identified by · from any 6 areas/systems or
12+ elements identified by ·from 2+ organ systems or
body areas
Detailed
9+ elements identified by a · using the psych exam template
2+ elements identified by ·from 9 organ systems or body
areasCompreh
ensive
Document all elements
in bolded outline system
boxes and 1+ element in
unbolded system boxes
Documentation of
Examination (cont.)
Specific abnormal and relevant negative findings of the
examination must be documented
A brief statement or notation indicating "negative" or
"normal" is sufficient to document normal findings
related to unaffected area(s) or asymptomatic organ
system(s)
General Multi-System Exam
Organ Systems/Body Areas
Constitutional
Eyes
ENT/Mouth
Neck
Respiratory
Cardiovascular
Chest/Breasts
Gastrointestinal/Abdom
en
GU
Lymphatic
Musculoskeletal
Skin
Neurologic
Psychiatric
Psychiatric Specialty Exam
Organ Systems/Body AreasOrgan System/Body
Area
Elements of Examination
Constitutional • Measurement of any three of the following seven vital signs: 1)
sitting or standing blood pressure, 2) supine blood pressure, 3)
pulse rate and regularity, 4) respiration, 5) temperature, 6)
height, 7) weight
• General appearance of patient
Musculoskeletal • Assessment of muscle strength and with notation of any atrophy
and abnormal movements
• Exam of gait & station
Psychiatric • Description of speech including: rate, volume, articulation,
coherence, and spontaneity with notation of abnormalities
• Description of thought processes including: rate of thoughts,
content of thoughts, abstract reasoning, and computation
• Description of associations
• Description of abnormal psychotic thoughts including:
hallucinations, delusions, preoccupation with violence, homicidal
or suicidal ideation, and obsessions
• Description of the patient's judgement and insight
• Complete mental status exam- orientation to time/place/person,
recent & remote memories, attention span/concentration,
language, fund of knowledge, mood & affect
Medical Decision Making Based on 4 types complexity of MDM
Straightforward
Low Complexity
Moderate Complexity
High Complexity
Complexities are based off of
three forms of MDM
Number of possible diagnoses and/or number of
management options considered
Amount and/or complexity of medical records,
diagnostic tests, and/or other info that must be
obtained, reviewed and analyzed
Risk of significant complications, morbidity, and/or
mortality, comorbidities associated w/ pt’s presenting
problems, diagnostic procedures and/or possible
management options
Number of Diagnoses or Management
Options Number of possible dx and/or management options
An assessment, clinical impression, or diagnosis should be
documented
Further treatment should be documented
Referrals/consultations should be documented
Minimal Limited Multiple Extensive
Diagnoses 1
establishe
d
1 established
& 1 rule out
2 rule out or
differential
2+ rule out or
differential
Problems Improved Stable
Resolving
Unstable
Unchanging
Worsening
Marked Change
Management
Options
1-2 2-3 3 changes in
treatment plan
4+ changes in
treatment plan
Amount and/or Complexity of
Data to be Reviewed Any ordered diagnostic services should be documented
Review of diagnostic services
Old records & other sources of information
Discussions w/ others that interpreted diagnostic services
Independent visualization/interpretation
Minimal Limited Moderate Extensive
Medical Data 1 source 2 sources 3 sources Multiple sources
Diagnostic
Tests
2 3 4 More than 4
Review of
Results
Confirmato
ry review`
Confirmation
of results w/
another
physician
Results
discussed w/
physician
performing
test
Unexpected
results,
contradictory
reviews, requires
additional reviews
Risk of Significant Complications,
Morbidity, and/or Mortality
Based on the risks associated with the presenting
problems, diagnostic procedures, and possible
management options
Comorbidities/underlying diseases
Invasive Diagnostic Procedure
Ordered, scheduled, or performed
Urgent invasive diagnostic procedure
Ordered or referred, stated or implied
Modified Table of Risk TablePresenting Problems Diagnostic
Procedures Ordered
Management Options Selected
Minimal One self limited problem Lab tests-
venipuncture or
urinalysis
Reassurance
Low 2 or more self-limited or
minor problems with one
stable, chronic illness or
acute uncomplicated illness
-Psychological
testing
-Skull Film
-Psychotherapy
-Environmental intervention
-Referral for consultation
Moderate -One or more chronic illness
with mild exacerbation,
progression, or side effects
of treatment or
-2 or more stable chronic
illnesses or undiagnosed
new problem with uncertain
prognosis
Electroencephalogra
m
-Neuropsychological
testing
-Prescription drug management
-Open-door seclusion
-Electroconvulsive therapy-
inpatient, outpatient, routine;
no comorbid medical conditions
High -1 or more chronic illnesses
with severe exacerbation,
progression, or side effect
of treatment or
-Acute illness with threat to
life
-Lumbar puncture
-Suicide risk
assessment
-Drug therapy requiring intensive
monitoring
-Closed-door seclusion
-Suicide observation
Electroconvulsion therapy- with
comorbid medical condition
-Rapid intramuscular neuroleptic
administration
-Pharmacological restraint
Medical Decision Making Once each section of the MDM is configured, the following
table is used to determine the overall MDM of the visit.
Straightforwar
d
Low
Complexity
Moderate
Complexity
High
Complexity
Number of
diagnoses or
management
options
Minimal Limited Multiple Extensive
Amount and/or
complexity of
data reviewed
Minimal/None Limited Moderate Extensive
Risk of
complications
and/or morbidity
or mortality
Minimal Low Moderate High
Time Based E/M Levels
Counseling and/or coordination of care dominates 50%+
of physicians time
Total record of time must be documented
Counseling and coordination of care should be described
in depth
Inpatient Discharge Codes
Psychotherapy Codes
Time Based
“Unit of time is attained when the mid-point is passed.” CPT Time Guidelines
90832 & 90833- 16 – 37 minutes
90834 & 90836- 38 – 52 minutes
90837 & 90838- 53 or more minutes
Prolonged Service Codes
For psychotherapy sessions that are 90 minutes or longer face to face with the patient
Add on codes
E/M Levels & Psychotherapy
Codes
Different codes based on reporting with or
without an E/M level
Used when medical management is provided in
addition to
E/M based on components of history, exam, MDM
Time used to meet E/M level requirements is not
included in reported psychotherapy time
Separate diagnosis is not required
E/M level should be listed first followed by
psychotherapy code
Interactive Complexity
Specific communication factors that complicate the delivery of a psychiatric procedure- psychotherapy, evaluation, etc.
Must meet one of the following in order to report:
Need to manage maladaptive communication (related to e.g. high anxiety, high reactivity, repeated questions, or disagreement) among participants that complicates delivery of care
Caregiver emotions or behavior that interferes with caregiver’s understanding & ability to assist in the implementation of treatment plan
Evidence or disclosure of a sentinel event and mandated report to 3rd part (abuse or neglect with report to state agency) with imitation of discussion of the sentinel event and/or report with patient and other visit participants.
Interactive Complexity (cont.)
Must meet one of the following in order
to report: (cont.)
The time providing interactive complexity
should be included in the psychotherapy
codes
Not considered a factor for Evaluation &
Management coding
Psychotherapy for Crisis
Presenting problem is typically life threatening or
complex and requires immediate attention
Accumulative time for date of service
Does not have to continuous
Can be with patient and/or family
If less than 30 minutes- refer to 90832 or 90833
Implementation & Provider
Resources
Date of service July 1, 2017
www.bh.medicaid.ohio.gov
Resources
American Medical Association (2017), Current
Procedural Terminology (CPT), Professional Edition
American Medical Association ,CPT Assistant
The Ohio Behavioral Health Redesign. Retrieved from
http://bh.medicaid.ohio.gov/
Centers for Medicare & Medicaid Services. (1997) 1997
Documentation Guidelines for Evaluation & Management
Services Retrieved from
https://www.cms.gov/Outreach-and-
Education/Medicare-Learning-Network-
MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf
Disclaimers
The information provided in this presentation is intended for educational and informational purposes to describe current coding practices. However, KT Coding & Transcription, Inc. assumes no responsibility or liability for the results or consequences that may arise from information obtained from this presentation. The information contained in the presentation is provided for information purposes only and represents no statement, promise or guarantee concerning levels of reimbursement, payment or charge. Although prepared for use by professionals, the presentation information should not be utilized as a substitute for professional services in specific situations. If legal advice is required, the services of a professional should be sought.
CPT Disclaimer -- American Medical Association (AMA) Notice CPT codes, descriptions and other data only are copyright 2017 American Medical Association. All rights reserved.