Clinical Neuropsychology Research Proposal - V. Westerberg
-
Upload
vm-westerberg -
Category
Healthcare
-
view
789 -
download
0
description
Transcript of Clinical Neuropsychology Research Proposal - V. Westerberg

MASSEY UNIVERSITY
175.722.- MASTER’S DEGREE RESEARCH PROPOSAL
CLINICAL NEUROPSYCHOLOGY RESEARCH PROPOSAL
Volatile Organic Solvent Neurotoxicity (VOSN) Assessment in New Zealand (NZ)
Supervisor: Prof Janet Leathem BA(Hons), MA, PhD Well., MNZCCPsych
Student: V. M. Westerberg MHlthSc (Psych)
Date: 10 September 2012
(Word count [excluding table of contents, references, & appendices]: 3,306)

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
2
TABLE OF CONTENTS
1.- Title Pg. 3
2.- Abstract 3
3.- Background 3
3.1.- Research objectives 3
3.2.- Research question 4
3.3.- Situation and Justification 4
3.4.- Literature Review 6
4.- Design, Methodology, and Methods 7
4.1.- Operational definition of VOSN 7
4.2.- Recruitment of Participants 8
4.2.1.- Sample 8
4.2.1.a.- Inclusion Criteria 8
4.2.1.b.- Exclusion Criteria 8
4.3.- Informed Consent 8
4.4.- Assessment 8
4.5.- Data analysis 9
4.6.- Potential Risks to Participants 10
4.7.- Potential Benefits to Participants and Others 10
5.- Limitations 11
6.- Location of Study 11
7.- Ethics 12
8.- Significance of Research 12
9.- Research Timeline 12
10.- Research Budget 12
11.- References 13
12.- Appendices
Appendix I: Informed Consent template
Appendix II: Swedish Questionnaire 16
Appendix III: Data Safety and Monitoring Plan template
Appendix IV: Low Risk Notification template
Appendix V: Research timeline
Appendix VI: Research budget template
16
16
24
25
28
31
32

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
3
CLINICAL NEUROPSYCHOLOGY RESEARCH PROPOSAL
1.- TITLE
Volatile Organic Solvent Neurotoxicity (VOSN) Evaluation in New Zealand (NZ).
2.- ABSTRACT
The current work aims to answer the question of whether, using NZ-normed tools, VOS
exposure impairs neuropsychological test results. It also highlights the need for the
development of diagnostic software to make VOSN assessment easier and faster for the benefit
of exposed workers, their families, and their employers. An evaluation of the current situation
and a literature review, support the justification for this work, as over the past 20 years, very
little research has been done about VOSN. The research design, methodology, and methods used
are all based on selected, robust research with a focus on recent developments. This proposal is
supplemented with additional useful information in the Appendices.
3.- BACKGROUND
3.1.- Research objectives
The purpose of this research project is threefold and can be divided into short, medium, and
long term goals:
Short term goal: To show whether Volatile Organic Solvents (VOS) impair neurological test
results in at-risk workers in New Zealand. Because of the word limit for this assignment, this
will be the sole scope of the current work.
Medium term goal: To suggest the development a tool for systematic, at-work, data collection of
volatile organic solvent neurotoxicity (VOSN) of employees at risk in the Wellington area
(initially)
Long term goal: Based on the hypothesis that early detection of cognitive and behavioural
symptoms of neurotoxicity may have positive health outcomes, the systematic screening of
VOSN will reduce the costs of disability on the workers, their families, insurance companies and
the government.

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
4
3.2.- Research question
Using NZ-normed tools, does exposure to Volatile Organic Solvents (VOS) result in impaired
neuropsychological test results?
3.3.- Situation and Justification
Organic solvents are compounds that share a chemical structure and physical properties of
volatility, lipophilicity, flammability, and low molecular weight. Although most organic solvents
are toxic, not all of them are. This research proposal focuses exclusively on the neurotoxic
volatile organic solvents most commonly used in NZ: chlorinated and aromatic hydrocarbons,
benzenes, toluenes, hexanes and ketones (DOL, 1998).
Volatile organic solvents (VOS) are extensively used in industry to manufacture glues, asphalt,
rubbers, paints, dyes, fuels, degreasing products, cosmetics (nail polish removers), agricultural
products (pesticides, fertilizers), plastics, cleaning products, inks, etc (Ogden, 1993). Short,
intense exposure to VOS is usually reversible, and easier to diagnose and treat successfully. But
it is long, insidious exposure to VOS which is much more likely to result in irreversible
neurotoxicity, evidenced as measurable cognitive and behavioural changes (Dobbs, 2009).
The reason for the neurotropism of VOS resides in their chemical structure: they are made of
lipophilic molecules which bind to other fat-containing molecules. Given that VOS easily
penetrate the skin and the mucosae (mainly the respiratory mucosa), the first highly lipophilic
molecules VOS will find, once they have been absorbed, are those of the central nervous system.
The amount of VOS retained is dependent on various factors, including sex (females are more
vulnerable), individual metabolic rate, physical activity, and substance use (medication, alcohol,
drugs) among others (Dobbs, 2009).
Following Ogden’s guidelines (1993) on the basis of United States data (NIOSH, 1987), it has
been estimated that around 100,000 NZ workers are currently potentially exposed to VOS
(Dryson & Ogden, 1998). Awareness of VOSN is high in the USA and in Scandinavian countries
where longitudinal research has been done since the 70’s. However, NZ only became aware of
VOSN in the 90’s when the Department of Health published the NZ Workplace Exposure
Standards, which was shortly followed by the Occupational and Health Service of the
Department of Labour (DOL, 2011b) booklet with the diagnostic criteria for chronic VOSN
(Dryson & Ogden, 1998; DOL, 2011b). The NZ DOL has recently developed two documents: the
Occupational Health Action Plan to 2013 and the Workplace Health and Safety Strategy for NZ
2015, which aim to reduce occupational health hazards, many of which are related to VOS

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
5
exposure (DOL, 2011a; DOL, 2009). Recent interest in VOSN has been shown by the Massey
University Centre for Public Health Research (CPHR), which has outlined what aims to be a
longitudinal study called Building Occupational Health Research in New Zealand (BROHNZ)
(Massey University, 2012).
Academic, governmental and industry bodies are constantly updating their knowledge and
awareness of the effects of VOS. Guidelines regarding protective clothing are, however, not
always observed by workers at risk as the clothing tends to interfere with their ability to do the
job effectively and in a timely manner, like gloves making it difficult to do fine work or the extra
clothing making workers uncomfortably hot (DOL, 1998). Self-employed workers are
particularly vulnerable, as they do not have the pressure and support to observe safety
standards. The added cost of protective clothing and its frequent replacement (e.g.: goggles,
gloves, masks) are further reasons for workers not to comply with industry and safety health
standards (DOL, 1998).
Based on the first NOHSAC report, VOSN causes occupational disease, which accounts for far
greater mortality per year (1,000) than occupational injuries (100) (Pearson et al., 2004).
Around 20,000 new cases of occupational disease are diagnosed every year in NZ, but there are
no clear estimates of how many are specifically due to VOS exposure or whether VOSN is more
related to dose than to time of exposure (DOL, 1998; Dobbs, 2009). The result of occupational
exposure to VOS can have a negative impact on the overall productivity and quality of life of the
at-risk working population. Ogden (1993), based on the work of Baker and Seppalainen about
the 1985 International Solvent Workshop, postulated what has become the internationally
accepted 3 types of Organic Solvent Neurotoxicity (OSN), known in this work as VOSN:
Type 1 VOSN: Acute exposure with reversible symptoms not detectable on neuropsychological
tests; corresponds to the WHO classification of organic affective syndrome.
Type 2 VOSN: Chronic exposure (≥ 10 years) with potentially irreversible symptoms.
Type 3 VOSN: Chronic exposure (≥ 10 years) with irreversible symptoms and dementia.
Additionally, Types 2 and 3 VOSN have been associated with systemic disorders like dermatitis,
ischaemic heart failure, cancers (lung cancer, lymphoma, leukemia, bladder cancer), decreased
fertility, repeated abortions in partners, and fetal abnormalities (DOL, 1998; Driscoll et al.,
2004; Dobbs, 2009).
Detection of VOSN is difficult because of the long latency period between the first exposure, the
first noticeable symptoms, and the first health-related consultation (Dobbs, 2009), and because
it is usually confounded and compounded with biological, marital, other occupational or other
stress-related problems. An increased awareness of VOSN would lead to earlier diagnoses and

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
6
to making better epidemiological estimates of its incidence and impact on health. Systematic, at-
work, data collection would greatly benefit workers and employers. A state-of-the-art software
called PSICOTOX has been developed by Cuban researcher P.J. Almirall (2000) to evaluate the
early negative functional effects of volatile neurotoxic substances in at-risk workers. Nothing
has been published in any other language but Spanish of this small, user-friendly programme.
The validity of its algorithm has been well established in South America (Almirall, 2000) and a
similar tool could be developed by researchers in NZ to allow VOS exposed workers to take the
online test and get to know the results and statistics immediately. This dynamic form of data
collection and analysis would increase both participants’ compliance and the amount of data
available for researchers. The assessment instruments mentioned in this work could be used,
copyright permitting, for the development of a VOSN detection software that the international
community could benefit from.
3.4.- Literature review
To complement the literature used in the Background section above, an extensive database
search was done using the key terms “solvent” and “neurotoxicity” on Massey University’s
Scopus, PsychINFO (EbscoHost), and Medline, for all years (1960-2012) and all electronic
document types (journal articles, reviews, conferences, editorials, surveys). Surprisingly, only
49, 6, and 42 documents could be found, respectively. Based on these results, it could be said
that interest in VOSN has decreased in the last decade compared with the amount of relevant
articles found that were written in the 70’s and 90’s. The reasons for this trend can only be
guessed, from a higher industry observation of safety guidelines to a reduced interest among
researchers in this issue.
The most recent articles found were written years ago by Masato Matsuoka (2007) and by
Finlay Dick (2006) and both are reviews of organic solvent toxicity studies. The articles show
that there is international agreement with regard to organic solvent (OS) toxicity levels (Type 1
acute, Type 2 moderate-chronic, and Type 3 severe-chronic) and their symptomatology. They
also demonstrate consensus in toluene having synergistic effects with all the other OS. However,
both articles fail to evaluate the assessment methods used in the studies reviewed.
Over 16 years of professional experience in research are condensed in a comprehensive 1997
article by White and Proctor with a very similar scope to that by Dryson and Ogden (1998)
mentioned below. The authors conclude that primary prevention and observation of official
health safety guidelines are essential to avoid irreversible neurotoxicity. Lees-Haley and
Williams (1997) claim that only long-term OS exposure causes neurotoxicity and take a
skeptical approach to the dozens of articles reviewed that intense, low-level exposure to VOS

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
7
may also cause neurotoxicity, and blame systematic internal consistency threats as responsible
for the results.
The most recent NZ article, and on which the NZ DOL is still basing its reports, is that by Dryson
and Ogden (1998), a metaanalysis of 4 years of published studies in which organic solvent
neurotoxicity classification types are confirmed, solvent types are classified by type and
industry, a demographic analysis is provided, and assessment methods are evaluated. The
neuropsychological battery suggested in this research proposal is a modified version of the one
recommended in this article of reference.
Renato Gilioli (1993) moves on to evaluate the economic impact of VOSN in the European Union
of the time. The author criticises the neuropsychological test batteries used by researchers as
producers of too many false positives and calls for the use of the well-validated, highly reliable
tool, the WHO NCTB.
Finally, among the database search, influential articles were found about the dose-related
neuroanatomical impact of OS exposure, assessed manly by CT scanning, showing diffuse
cortical atrophy (Triebig et al., 1992) in at-risk workers and severe neurologic damage in their
unborn progeny (Stoltenburg-Didinger, Altenkirch, & Wagner, 1990). Time-constraints made
further consideration of these interesting issues not feasible this time.
4.- DESIGN, METHODOLOGY, AND METHODS
This research project has been designed to collect symptoms data from neuropsychological test
results of workers exposed to VOS for a minimum period of 12 months and compare the results
with those of non-exposed individuals. To this end, a series of instruments will be administered,
at one year intervals, to create a database of which a longitudinal study can be derived in
keeping with goal number 3 of this proposal. However, the focus will be a non-experimental,
comparative, research design: A cross-sectional, between-groups, quantitative study that aims
to evaluate whether there is a relationship between the independent variable (occupational
exposure to VOS) and the dependent variable (VOSN).
4.1.- Operational definition of VOSN
Neurotoxicity due to VOS exposure will be operationally defined as solvent-related CAMFI
(Concentration, attention, memory [impairment], fatigue, insomnia). The A also stands for
anxiety, appetite loss, and alcohol intolerance; and the F, for frontal lobe functioning
abnormalities (DOL, 1998).

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
8
4.2.- Recruitment of Participants
4.2.1.- Sample
The sample will be integrated by male workers aged between 18 and 65, ideally roughly
representing NZ’s ethnicity mix: 67% Europeans, 14% Maori, 9% Asians, 7% Pacific islanders,
and 3% Indians (Statistics NZ, 2006). All participants will also meet the following criteria:
4.2.1.a.- Inclusion criteria:
Exposed group: Ten (10) or more volunteer individuals occupationally exposed to VOS for a
minimum of 12 months, recruited on site by the researcher.
Control group: At least ten (10) volunteer individuals not occupationally exposed to VOS,
preferably a convenience sample of undergraduate students of variable ages.
4.2.1.b.- Exclusion criteria:
History of psychiatric or neurologic disorder; having consumed alcohol or drugs in the 12 hours
prior to the evaluation; not being proficient in English.
The actual number of participants will depend on recruitment success and turnover rates.
For practical purposes, all participants will work in the Wellington city area. Potential
participants -professional independent workers developing their professional activity within a
radius of 10km from the Wellington Psychology Clinic- will be selected from the Yellow Pages:
From painters, pest-controllers, dry-cleaners, to professional house cleaners. They will be
approached in person by the student researcher. Participants who meet the recruitment criteria
will be contacted by phone and given further information about the assessment process.
4.3.- Informed Consent
Written informed consent (see template in Appendix I) will be obtained to participate in this
study from all participants, who with their signature, will allow the researchers to handle the
data and results obtained as per Massey University and the NZ Psychological Society Codes of
Ethics. In case of conflict, the higher standard of conduct will be observed.
4.4.- Assessment
In order to gather information for this study, the following assessment procedure, modified
from the guidelines by the NZ Department of Labour (DOL, 1998), will be used:

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
9
1. Clinical interview: A 1-hour interview with the worker and a relative or partner to gather
clinically relevant data (demographic, occupational, health, leisure, and toxic habits
information), and to assess for general functioning and neurological symptoms.
2. Screening questionnaire for VOS exposure: Swedish “Questionnaire 16” (5’) (see Appendix II).
3. Neuropsychological test battery: (alternating difficult and easy tests)
3.1. NZART (10’). The NZ-normed NART will be used to estimate pre-morbid intelligence
(Starkey & Halliday, 2011). Using this newly developed test will help improve its validity, with
the aim that more and more researchers feel encouraged to use this tool instead of the
commonly used US-validated ones.
3.2. Cancellation test (5’) to evaluate sustained attention (vigilance).
3.3. WAIS-V Picture Completion Test (5’) for simple visuospacial assessment.
3.4. WAIS-V Digit Symbol, a psychomotor speed test (5’).
3.5. WAIS-V Block Design (5’) for complex visuospacial speed assessment.
3.6. Digit Span (10’), immediate memory assessment.
3.7. Rey Complex Figure Test (10’) with 30’-delay recall, to assess short and long-term
visuospacial perception as well as motor coordination.
3.8. NZ-VLT, the NZ version of the California VLT based on findings by Barker-Collo, Clarkson,
Cribb, and Grogan (2002) to assess long-term verbal memory.
3.9. Similarities test (20’) from WAIS-V to evaluate frontal lobe functioning.
4. A second, feedback interview will be scheduled to communicate the results of the
neuropsychological evaluation and to discuss an intervention plan involving the individual and,
very possibly, his home, family, occupational, and social environments.
4.5.- Data analysis
The results of this between-group experimental research design will be analysed using Chi-
square for goodness of fit statistics, given that the data are nominal (categorical) and that the
aim is to determine the percentage of discrepancy between the observed and expected values of
the variables. The p value selected will be a standard p<0.05, with 3 degrees of freedom
(number of categories minus 1). The categories are: Exposed vs. Not exposed and With
neurological symptoms vs. Without neurological symptoms. This statistic will show whether the

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
10
null hypothesis is true or not if the critical value is greater than the calculated one (sum of
observed and expected frequencies).
Frequency distributions will be presented in the form of tables. With the aim to determine the
contribution of each factor to the diagnostic classification, a factor analysis will be done. The
results derived from the clinical history obtained during the initial interview will be excluded
from the factor analysis for both groups because from a statistical point of view its contribution
would be very hard to quantify.
4.6.- Potential Risks to Participants:
A template for a Data Safety and Monitoring Plan can be found in Appendix III. Appendix IV
contains Massey University’s Notification of Low Risk Research/Evaluation involving Human
Participants. Both forms are for the participants to sign. The following two identified potential
risks will be considered:
First, participants may find some questions uncomfortable to answer (toxic habits, sex life). This
foreseeable issue will be tackled by informing all participants of their right to withdraw from
the study at any time without consequences.
Second: There is a risk for the confidential information taken being accidentally released. This
contingency will be dealt with by de-identifying and codifying all data collected, which will be
kept in a locked file cabinet to which only the researchers will have access. With regard to
possible further confidentiality issues, the NZ Psychological Society Code of Ethics will be
observed at every moment (Evans, Rucklidge, & O’Driscoll, 2007).
4.7.- Potential Benefits to Participants and Others
Participants, specifically those in the exposed group, will benefit from being aware of their
symptoms so that action can be taken to prevent them from worsening. All participants will
benefit from knowing that their contribution may help others in their situation if regular
screening of VOSN is done at workplaces. If this research proposal is carried out and proven
successful, further funding may ensure that the programme keeps being implemented, updated,
expanded, and replicated. Knowledge diffusion through presentations in congresses and
lectures may capture the attention and interest of researchers, institutions and the media, so
that the industry progressively stops using the more toxic solvents and replace them with safer
ones.

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
11
5.- LIMITATIONS
Limitations of this study start by the potentially small sample gathered, meaning that
participant withdrawals can limit the validity of the results as well as the possibility for
generalisation. The aim is to recruit as many participants as possible to minimise these risks.
Another limitation is the choice of NZ-normed tests, which according to the developers, still
require further studies for further validation purposes. This is how science advances, taking
controlled risks, evaluating results and coming to conclusions. It is expected that the tests will
fare within the limits of acceptability described by the developers. It should not be expected that
every test used here will have the reliability and validity of highly researched tools like the
WAIS-V, although these will be within acceptable limits.
Under-reporting and under-diagnosing for reasons like professional and social desirability are
other potential limiting factors for getting a representative sample. Some individuals may
simply not want to know whether they have VOSN. The researcher has to be persuasive and
explain potential participants the wide range of advantages described in the Benefits section
above.
It has been shown that when p is set at 0.05 in multiple variables studies (>20), statistic
significance is not quite exact, a phenomenon called "multiple comparisons problem" (Coolican,
2009). This is usually solved using Bonferoni's procedure, provided that the tendencies found
are not in the direction of the differences. This issue should not be a problem in this case, as
only 9 tests are being applied.
The researcher is aware of the many unanswered questions regarding VOSN, like the possible
existence of a dose threshold level and interactions with commonly substances and medications.
No experiment can control for all the possible confounds, but every effort will be made to
identify and control possible confounds.
Finally, the provisional timeline provided in Appendix V does not take into account holiday
periods or semester breaks. This limitation would only delay the study some 2 to 3 weeks.
Consultation with the supervisor about holidays will fix this limitation.
6.- LOCATION OF STUDY
Should this research proposal be approved, the study will be conducted at Massey University
Psychology Clinic in Wellington.

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
12
7.- ETHICS
Communicating the results to participants will be done during the feedback interview. Because
the results may be used for further purposes like a presentation, a thesis, or a journal article, all
participants will have agreed to this possibility by signing the Informed Consent. The NZ
Psychological Society Code of Ethics (Evans, Rucklidge, & O’Driscoll, 2007) will be the reference
to follow throughout and beyond the duration of the experiment.
8.- SIGNIFICANCE OF RESEARCH
The relevance of this research proposal lies on the lack of recent studies about VOSN in New
Zealand. Of particular significance is the fact that this proposal aims to use NZ-normed tools
instead of the US-validated ones recommended by the NZ Department of Labour since 1992
(DOL, 1998). Validation of new, useful tools and studies rely on researchers taking controlled
risks and time to apply them, as in this case.
Additionally, this work proposes the novel idea of the need to develop an assessment and
diagnostic software for regular, early, fast detection of neurotoxicity due to occupational organic
solvent exposure that would lead to the production of large numbers of data to create a VOSN
longitudinal study in New Zealand.
9.- TIMELINE
A provisional timeline is described in Appendix V and implies full-time dedication for a
minimum of one year.
10.- BUDGET
Appendix VI contains the Research Proposal Budget Template to be filled out with the
assistance and input of the main supervisor, based on her experience.

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
13
11. – REFERENCES
Almirall Hernandez, P.J. (2000). Psicotox. Revista Cubana de Salud y Trabajo, 1(1), 2-13.
Barker-Collo, S., Clarkson, A., Cribb, A., & Grogan, M. (2002). The impact of American content on
California Verbal Learning Test performance: A New Zealand illustration. Clinical
Neuropsychologist, 16(3), 290-299. Retrieved from www.scopus.com
Coolican, H. (2009). Research methods and statistics in Psychology (5th ed.). London: Hodder
Education.
Department of Labour [DOL](1998). Chronic organic solvent neurotoxicity: Diagnostic criteria.
Wellington: Author. Retrieved from http://www.rikiott.com/pdf/a_solvent.pdf
Department of Labour [DOL](2009). Workplace Health and Safety Strategy for NZ 2015.
Wellington: Author. Retrieved from http://www.dol.govt.nz/whss/review/review-
report.asp
Department of Labour [DOL](2011a). Occupational Health Action Plan to 2013. Wellington:
Author. Retrieved from http://www.dol.govt.nz/whss/sector-plans/occupational-
health/03.asp#_edn15
Department of Labour [DOL](2011b). Workplace Exposure Standards and Biological Exposure
Indices. Wellington: Author. Retrieved from
http://www.osh.govt.nz/order/catalogue/329.shtml
Dick, F. D. (2006). Solvent neurotoxicity. Occupational and Environmental Medicine, 63(3), 221-
226. Retrieved from www.scopus.com
Dobbs, M.R. (2009). Clinical neurotoxicology: Syndromes, substances, environments. Philadelphia,
PA: Saunders-Elsevier.
Driscoll, T., Mannetje, A., Dryson, E., Feyer, A.M., Gander, P., McCracken, S., Pearce, N., &
Wagstaffe, M. (2004). The burden of occupational disease and injury in New Zealand:
Technical Report. National Occupational Health and Safety Advisory Committee
[NOHSAC]: Wellington.
Dryson, E. W., & Ogden, J. A. (1998). Chronic solvent neurotoxicity in new zealand: Notified cases
between 1993 and 1997. New Zealand Medical Journal, 111(1077), 425-427. Retrieved
from www.scopus.com

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
14
Evans, I.M., Rucklidge, J.J., & O’Driscoll, M.O. (Eds)(2007). Professional Practice of Psychology in
New Zealand. The New Zealand Psychological Society, Wellington: Author.
Gilioli, R. (1993). EURONEST: A concerted action of the European Community for the study of
organic solvents neurotoxicity. Environmental Research, 62(1), 89-98. Retrieved from
www.scopus.com
Lees-Haley, P. R., & Williams, C. W. (1997). Neurotoxicity of chronic low-dose exposure to
organic solvents: A skeptical review. Journal of Clinical Psychology, 53(7), 699-712.
Retrieved from www.scopus.com
Massey University Centre for Public Health Research [CPHR] (2012). Building Occupational
Health Research in New Zealand (BROHNZ). Wellington: Author. Retrieved from
http://publichealth.massey.ac.nz/Symposia/Sym2012/OCC/symposium%202012%20pr
esentations.htm
Matsuoka, M. (2007). Neurotoxicity of organic solvents - recent findings. Brain and Nerve, 59(6),
591-596. Retrieved from www.scopus.com
NIOSH [National Institute for Occupational Safety and Health] (1987). Organic Solvent
Neurotoxicity. US Department of Health and Human Services, Ohio: Author.
Ogden, J.A. (1993). The psychological and neuropsychological assessment of chronic organic
solvent neurotoxicity: A case series. New Zealand Journal of Psychology, 22, 82-93.
Retrieved from http://www.psychology.org.nz/cms_show_download.php?id=804
Pearce, N., Dryson, E., Feyer, A.M., Gander, P., McCracken, S., & Wagstaffe, M. (2004). The Burden
of Occupational Disease and Injury in New Zealand: Report to the Associate Minister of
Labour. National Occupational Health and Safety Advisory Committee [NOHSAC],
Wellington. Retrieved from www.scopus.com
Starkey, N.J., & Halliday, T. (2011). Development of the New Zealand Adult reading Test
[NZART]: Preliminary findings. New Zealand Journal of Psychology, 40 (3), 129-141.
Retrieved from www.scopus.com
Statistics NZ (2006). Quickstats about New Zealand’s Population and Dwellings: Ethnic groups.
Retrieved from
http://www.stats.govt.nz/Census/2006CensusHomePage/QuickStats/quickstats-about-
a-subject/nzs-population-and-dwellings/ethnic-groups.aspx

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
15
Stoltenburg-Didinger, G., Altenkirch, H., & Wagner, M. (1990). Neurotoxicity of organic solvent
mixtures: Embryotoxicity and fetotoxicity. Neurotoxicology and Teratology, 12(6), 585-
589. Retrieved from www.scopus.com
Triebig, G., Barocka, A., Erbguth, F., Holl, R., Lang, C., Lehrl, S., . . . Weltle, D. (1992). Neurotoxicity
of solvent mixtures in spray painters II: Neurologic, psychiatric, psychological, and
neuroradiologic findings. International Archives of Occupational and Environmental
Health, 64(5), 361-372. Retrieved from www.scopus.com
White, R. F., & Proctor, S. P. (1997). Solvents and neurotoxicity. Lancet, 349(9060), 1239-1243.
Retrieved from www.scopus.com

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
16
12.- APPENDICES
12.1.- Appendix I: Informed Consent Template
(available at http://www.who.int/rpc/research_ethics/informed_consent/en/)
[Name of Principle Investigator]
[Informed Consent form for ______________ _______] Name the group of individuals for whom this informed consent form is written. Because research for a single project is often carried out with a number of different groups of individuals - for example healthcare workers, patients, and parents of patients - it is important that you identify which group this particular consent is for. (Example: This Informed Consent Form is for men and women who attend clinic Z, and who we are inviting to participate in research on X. The title of our research project is "…………………………." ) You may provide the following information either as a running paragraph or under headings as shown below. [Name of Principal Investigator] [Name of Organization] [Name of Sponsor] [Name of Proposal and version] This Informed Consent Form has two parts:
Information Sheet (to share information about the research with you) Certificate of Consent (for signatures if you agree to take part)
You will be given a copy of the full Informed Consent Form PART I: Information Sheet Introduction Briefly state who you are and explain that you are inviting them to participate in the research you are doing. Inform them that they may talk to anyone they feel comfortable talking with about the research and that they can take time to reflect on whether they want to participate or not. Assure the participant that if they do not understand some of the words or concepts, that you will take time to explain them as you go along and that they can ask questions now or later. (Example: I am X, working for the Y Research Institute. We are doing research on Z disease, which is very common in this country. I am going to give you information and invite you to be part of this research. You do not have to decide today whether or not you will participate in the research. Before you decide, you can talk to anyone you feel comfortable with about the research. There may be some words that you do not understand. Please ask me to stop as we go through the information and I will take time to explain. If you have questions later, you can ask them of me, the study doctor or the staff.) Purpose of the research Explain in lay terms why you are doing the research. The language used should clarify rather than confuse. Use local and simplified terms for a disease, e.g. local name of disease instead of malaria, mosquito instead of anopheles, “mosquitoes help in spreading the disease” rather than “mosquitoes are
[YOUR INSTITUTIONAL LETTERHEAD HERE]
Please do not submit consent forms on the WHO letter head

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
17
the vectors”. Avoid using terms like pathogenesis, indicators, determinants, equitable etc. There are guides on the internet to help you find substitutes for words which are overly scientific or are professional jargon. (Example: Malaria is one of the most common and dangerous diseases in this region. The drugs that are currently used to help people with malaria are not as good as we would like them to be. In fact, only 40 out of every 100 people given the malaria drug XYZ are completely cured. There is a new drug which may work better. The reason we are doing this research is to find out if the new drug ABX is better than drug XYZ which is currently being used.) Type of Research Intervention Briefly state the type of intervention that will be undertaken. This will be expanded upon in the procedures section but it may be helpful and less confusing to the participant if they know from the very beginning whether, for example, the research involves a vaccine, an interview, a biopsy or a series of finger pricks. (Example: This research will involve a single injection in your arm as well as four follow-up visits to the clinic.) Participant selection State why this participant has been chosen for this research. People often wonder why they have been chosen to participate and may be fearful, confused or concerned. (Example: We are inviting all adults with malaria who attend clinic Z to participate in the research on the new malaria drug.)
Example of question to elucidate understanding: Do you know why we are asking you to take part in this study? Do you know what the study is about?
Voluntary Participation Indicate clearly that they can choose to participate or not. State, what the alternative - in terms of the treatment offered by the clinic - will be, if they decide not to participate. State, only if it is applicable, that they will still receive all the services they usually do whether they choose to participate or not. This can be repeated and expanded upon later in the form as well, but it is important to state clearly at the beginning of the form that participation is voluntary so that the other information can be heard in this context. (Example: Your participation in this research is entirely voluntary. It is your choice whether to participate or not. Whether you choose to participate or not, all the services you receive at this clinic will continue and nothing will change. If you choose not to participate in this research project, you will offered the treatment that is routinely offered in this clinic/hospital for disease Z, and we will tell you more about it later. You may change your mind later and stop participating even if you agreed earlier.)
Examples of question to elucidate understanding: If you decide not to take part in this research study, do you know what your options are? Do you know that you do not have to take part in this research study, if you do not wish to? Do you have any questions?
Include the following section only if the protocol is for a clinical trial: Information on the Trial Drug [Name of Drug] 1) give the phase of the trial and explain what that means. Explain to the participant why you are comparing or testing the drugs. 2) provide as much information as is appropriate and understandable about the drug such as its manufacturer or location of manufacture and the reason for its development. 3) explain the known experience with this drug 4) explain comprehensively all the known side-effects/toxicity of this drug, as well as the adverse effects of all the other medicines that are being used in the trial
(Example: The drug we are testing in this research is called ABX. It has been tested before with people who do not have malaria but who live in areas where malaria is common. We now want to test the drug on people who have malaria. This second research is called a "phase 2" trial.

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
18
The drug ABX is made by Company C. You should know that it has a few side effects. One of the side effects, or problems, is that you may feel tired for the first day after being given the drug. Also, 20% of the people who tried the drug in previous research experienced temporary swelling where the injection entered the skin. We know of no other problem or risks. Some participants in the research will not be given the drug which we are testing. Instead, they will be given the drug XYZ, the drug which is most commonly used in this region to treat malaria. There is no risk associated with that drug and no known problems. It does not, however, cure malaria as often as we would like.) Procedures and Protocol Describe or explain the exact procedures that will be followed on a step-by-step basis, the tests that will be done, and any drugs that will be given. Explain from the outset what some of the more unfamiliar procedures involve (placebo, randomization, biopsy, etc.) Indicate which procedure is routine and which is experimental or research.Participants should know what to expect and what is expected of them. Use active, rather than conditional, language. Write "we will ask you to…." instead of "we would like to ask you to….". In this template, this section has been divided into two: firstly, an explanation of unfamiliar procedures and, secondly, a description of process. A. Unfamiliar Procedures This section should be included if there may be procedures which are not familiar to the participant. If the protocol is for a clinical trial: 1) involving randomization or blinding, the participants should be told what that means and what chance they have of getting which drug (i.e. one in four chances of getting the test drug). (Example: Because we do not know if the new malaria drug is better than the currently available drug for treating malaria, we need to compare the two. To do this, we will put people taking part in this research into two groups. The groups are selected by chance, as if by tossing a coin. Participants in one group will be given the test drug while participants in the other group will be given the drug that is currently being used for malaria. It is important that neither you nor we know which of the two drugs you are given. This information will be in our files, but we will not look at these files until after the research is finished. This is the best way we have for testing without being influenced by what we think or hope might happen. We will then compare which of the two has the best results. The healthcare workers will be looking after you and the other participants very carefully during the study. If we are concerned about what the drug is doing, we will find out which drug you are getting and make changes. If there is anything you are concerned about or that is bothering you about the research please talk to me or one of the other researchers) 2) involving an inactive drug or placebo, it is important to ensure that the participants understand what is meant by a placebo or inactive drug. (Example: A placebo or inactive medicine looks like real medicine but it is not. It is a dummy or pretend medicine. It has no effect on a person because it has no real medicine in it. Sometimes when we want to know whether a new medicine is good, we give some people the new medicine and some people the pretend or dummy medicine. For the research to be good, it is important that you do not know whether you have been given the real medicine or the pretend or dummy medicine. This is one of the best ways we have for knowing what the medicine we are testing really does.) 3) which may necessitate a rescue medicine, then provide information about the rescue medicine or treatment such as what it is and the criterion for its use. For example, in pain trials, if the test drug does not control pain, then intravenous morphine may be used as a rescue medicine. (Example: If we find that the medicine that is being used does not have the desired effect, or not to the extent that we wish it to have, we will use what is called a “rescue medicine.” The medicine that we will use is called QRS and it has been proven to control pain. If you find that the drug we are testing does not stop your pain and it is very uncomfortable for you, we can use the rescue medicine to make you more comfortable.)

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
19
If the protocol is for clinical research: Firstly, explain that there are standards/guidelines that will be followed for the treatment of their condition. Secondly, if as part of the research a biopsy will be taken, then explain whether it will be under local anesthesia, sedation or general anesthesia, and what sort of symptoms and side effects the participant should expect under each category. (Example: You will receive the treatment of your condition according to national guidelines. This means that you will be (explain the treatment). To confirm the cause of your swelling, a small sample of your skin will be taken. The guidelines say that the sample must be taken using a local anesthesia which means that we will give you an injection close to the area where we will take the sample from. This will make the area numb so that you will not feel any pain when we take the sample.) For any clinical study (if relevant): If blood samples are to be taken explain how many times and how much in a language that the person understands. It may, for example, be inappropriate to tell a tribal villager that blood equal to a wine-glass full will be taken but it may be very appropriate to use pictures or other props to illustrate the procedure if it is unfamiliar. If the samples are to be used only for this research, then explicitly mention here that the biological samples obtained during this research procedure will be used only for this research, and will be destroyed after ____ years, when the research is completed. If the tissues/blood samples or any other human biological material will be stored for a duration longer than the research purpose, or is likely to be used for a purpose other than mentioned in the research proposal, then provide information about this and obtain consent specifically for such storage and use in addition to consent for participation in the study - (see last section) (Example: We will take blood from your arm using a syringe and needle. Each time we will take about this much blood (show a spoon, vial or other small container with a small amount of water in it. In total, we will take about ……..this much blood in x number of weeks/months. At the end of the research, in 1 year, any left over blood sample will be destroyed.)
B. Description of the Process Describe to the participant what will happen on a step-by-step basis. It may be helpful to the participant if you use drawings or props to better illustrate the procedures. A small vial or container with a little water in it is one way of showing how much blood will be withdrawn. (Example: During the research you make five visits to the clinic.
In the first visit, a small amount of blood, equal to about a teaspoon, will be taken from your arm with a syringe. This blood will be tested for the presence of substances that help your body to fight infections. We will also ask you a few questions about your general health and measure how tall you are and how much you weigh.
At the next visit, which will be two weeks later, you will again be asked some questions about your health and then you will be given either the test drug or the drug that is currently used for malaria. As explained before, neither you nor we will know whether you have received the test or the dummy/pretend drug.
After one week, you will come back to the clinic for a blood test. This will involve….) Duration Include a statement about the time commitments of the research for the participant including both the duration of the research and follow-up, if relevant. (Example: The research takes place over ___ (number of) days/ or ___ (number of) months in total. During that time, it will be necessary for you to come to the clinic/hospital/health facility _______(number of) days , for ____ (number of) hours each day. We would like to meet with you three months after your last clinic visit for a final check-up. In total, you will be asked to come 5 times to the clinic in 6 months. At the end of six months, the research will be finished.)

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
20
Examples of question to elucidate understanding: Can you tell me if you remember the number of times that we are asking you to come to the hospital to complete the treatment? The research project? How many injections will you be given? How many tablets? How much blood will be taken from your veins, using a syringe and needle? Over how many weeks? Etc. Do you have any other questions? Do you want me to go through the procedures again?
Side Effects Potential participants should be told if there are any known or anticipated side effects and what will happen in the event of a side effect or an unexpected event. (Example: As already mentioned, this drug can have some unwanted effects. It can make you tired and it can cause some temporary swelling around the place where the injection goes into your arm. It is possible that it may also cause some problems that we are not aware of. However, we will follow you closely and keep track of any unwanted effects or any problems. We may use some other medicines to decrease the symptoms of the side effects or reactions. Or we may stop the use of one or more drugs. If this is necessary we will discuss it together with you and you will always be consulted before we move to the next step.) Risks Explain and describe any possible or anticipated risks. Describe the level of care that will be available in the event that harm does occur, who will provide it, and who will pay for it. A risk can be thought of as being the possibility that harm may occur. Provide enough information about the risks that the participant can make an informed decision. (Example: By participating in this research it is possible that you will be at greater risk than you would otherwise be. There is, for example, a risk that your disease will not get better and that the new medicine doesn't work even as well as the old one. If, however, the medicine is not working and your fever does not go down in 48 hours we will give you quinine injections which will bring your fever down and make you more comfortable. While the possibility of this happening is very low, you should still be aware of the possibility. We will try to decrease the chances of this event occurring, but if something unexpected happens, we will provide you with______.)
Examples of question to elucidate understanding: Do you understand that, while the research study is on-going, no-one may know which medicine you re receiving? Do you know that the medicine that we are testing is a new medicine, and we do not know everything about it? Do you understand that you may have some unwanted side-effects from the medicines? Do you understand that these side-effects can happen whether or not you are in the research study? Etc. Do you have any other questions?
Benefits Mention only those activities that will be actual benefits and not those to which they are entitled regardless of participation. Benefits may be divided into benefits to the individual, benefits to the community in which the individual resides, and benefits to society as a whole as a result of finding an answer to the research question. (Example: If you participate in this research, you will have the following benefits: any interim illnesses will be treated at no charge to you. If your child falls sick during this period he/she will be treated free of charge. There may not be any benefit for you but your participation is likely to help us find the answer to the research question. There may not be any benefit to the society at this stage of the research, but future generations are likely to benefit.) Reimbursements State clearly what you will provide the participants with as a result of their participation. WHO does not encourage incentives. However, it recommends that reimbursements for expenses incurred as a result of participation in the research be provided. These may include, for example, travel costs and money for wages lost due to visits to health facilities. The amount should be determined within the host country context. (Example:. We will give you [amount of money] to pay for your travel to the clinic/parking and we will give you [amount] for lost work time. You will not be given any other money or gifts to take part in this research.)

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
21
Examples of question to elucidate understanding: Can you tell me if you have understood correctly the benefits that you will have if you take part in the study? Do you know if the study will pay for your travel costs and time lost, and do you know how much you will be re-imbursed? Do you have any other questions?
Confidentiality Explain how the research team will maintain the confidentiality of data, especially with respect to the information about the participant which would otherwise be known only to the physician but would now be available to the entire research team. Note that because something out of the ordinary is being done through research, any individual taking part in the research is likely to be more easily identified by members of the community and is therefore more likely to be stigmatized. (Example: With this research, something out of the ordinary is being done in your community. It is possible that if others in the community are aware that you are participating, they may ask you questions. We will not be sharing the identity of those participating in the research. The information that we collect from this research project will be kept confidential. Information about you that will be collected during the research will be put away and no-one but the researchers will be able to see it. Any information about you will have a number on it instead of your name. Only the researchers will know what your number is and we will lock that information up with a lock and key. It will not be shared with or given to anyone except [name who will have access to the information, such as research sponsors, DSMB board, your clinician, etc].)
Example of question to elucidate understanding: Did you understand the procedures that we will be using to make sure that any information that we as researchers collect about you will remain confidential? Do you have any questions about them?
Sharing the Results Where it is relevant, your plan for sharing the information with the participants should be provided. If you have a plan and a timeline for the sharing of information, include the details. You should also inform the participant that the research findings will be shared more broadly, for example, through publications and conferences. (Example: The knowledge that we get from doing this research will be shared with you through community meetings before it is made widely available to the public. Confidential information will not be shared. There will be small meetings in the community and these will be announced. After these meetings, we will publish the results in order that other interested people may learn from our research.) Right to Refuse or Withdraw This is a reconfirmation that participation is voluntary and includes the right to withdraw. Tailor this section to ensure that it fits for the group for whom you are seeking consent. The example used here is for a patient at a clinic. (Example: You do not have to take part in this research if you do not wish to do so and refusing to participate will not affect your treatment at this clinic in any way. You will still have all the benefits that you would otherwise have at this clinic. You may stop participating in the research at any time that you wish without losing any of your rights as a patient here. Your treatment at this clinic will not be affected in any way.) OR (Example: You do not have to take part in this research if you do not wish to do so. You may also stop participating in the research at any time you choose. It is your choice and all of your rights will still be respected.) Alternatives to Participating Include this section only if the study involves administration of investigational drugs or use of new therapeutic procedures. It is important to explain and describe the established standard treatment.
(Example: If you do not wish to take part in the research, you will be provided with the established standard treatment available at the centre/institute/hospital. People who have malaria are given….) Who to Contact Provide the name and contact information of someone who is involved, informed and accessible (a local person who can actually be contacted. State also that the proposal has been approved and how.

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
22
(Example: If you have any questions you may ask them now or later, even after the study has started. If you wish to ask questions later, you may contact any of the following: [name, address/telephone number/e-mail]) This proposal has been reviewed and approved by [name of the local IRB], which is a committee whose task it is to make sure that research participants are protected from harm. If you wish to find about more about the IRB, contact [name, address, telephone number.]). It has also been reviewed by the Ethics Review Committee of the World Health Organization (WHO), which is funding/sponsoring/supporting the study.
Example of question to elucidate understanding: Do you know that you do not have to take part in
this study if you do not wish to? You can say No if you wish to? Do you know that you can ask me questions later, if you wish to? Do you know that I have given the contact details of the person who can give you more information about the study? Etc.
You can ask me any more questions about any part of the research study, if you wish to. Do you have any questions? PART II: Certificate of Consent This section should be written in the first person and have a statement similar to the one in bold below. If the participant is illiterate but gives oral consent, a witness must sign. A researcher or the person going over the informed consent must sign each consent. The certificate of consent should avoid statements that have "I understand…." phrases. The understanding should perhaps be better tested through targeted questions during the reading of the information sheet (some examples of questions are given above), or through the questions being asked at the end of the reading of the information sheet, if the potential participant is reading the information sheet him/herself. I have read the foregoing information, or it has been read to me. I have had the opportunity to ask questions about it and any questions that I have asked have been answered to my satisfaction. I consent voluntarily to participate as a participant in this research. Print Name of Participant__________________
Signature of Participant ___________________
Date ___________________________ Day/month/year
If illiterate A literate witness must sign (if possible, this person should be selected by the participant and should have no connection to the research team). Participants who are illiterate should include their thumb-print as well. I have witnessed the accurate reading of the consent form to the potential participant, and the individual has had the opportunity to ask questions. I confirm that the individual has given consent freely.
Print name of witness_____________________ AND Thumb print of participant
Signature of witness ______________________
Date ________________________ Day/month/year

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
23
Statement by the researcher/person taking consent I have accurately read out the information sheet to the potential participant, and to the best of my ability made sure that the participant understands that the following will be done: 1. 2. 3. I confirm that the participant was given an opportunity to ask questions about the study, and all the questions asked by the participant have been answered correctly and to the best of my ability. I confirm that the individual has not been coerced into giving consent, and the consent has been given freely and voluntarily. A copy of this ICF has been provided to the participant.
Print Name of Researcher/person taking the consent________________________
Signature of Researcher /person taking the consent__________________________
Date ___________________________ Day/month/year

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
24
12.2.- Appendix II: Swedish “Questionnaire 16”
(available at http://www.rikiott.com/pdf/a_solvent.pdf)

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
25
12.3.- Appendix III: Data Safety and Monitoring Plan Template
(Modified from the downloadable University of Florida Addendum N, 2009. Available at http://tinyurl.com/bnfw9vx)
STUDY TITLE: SECTION 1: RISK RELATED TO STUDY DESIGN Risk and Complexity increase from left to right. Check appropriate answers. Research Design Observational Intervention, but
not intended to treat a disease
Treatment of a disease
Clinical Trial Design N/A Placebo Randomization Blinding Trial Phase N/A Phase I Phase II Phase III Number of sites Single site Multiple sites Possibility of major morbidity or mortality
No May be at risk for morbidity or mortality even if lesser outcomes such as relief of symptoms are addressed1
Yes
Investigational drug, device, or biologic
No Yes
Assessment of serious toxicity requiring comparison of rates
No Yes
Safety data available Yes Limited early data available
None
Potential for breach of confidentiality or invasion of privacy
Low
Moderate
High
Research experience of Primary Investigator
>2 years 1-2 years <1 year
SECTION 2: RISK RELATED TO STUDY POPULATION Risk increases left to right. Check all appropriate answers. Vulnerability of study subjects
Healthy Volunteer Person with disease; able to sign consent
Vulnerable Child; terminally ill; frail elderly, mentally impaired, persons too sick to give consent
Severity of pre-existing disease or condition
N/A Low Moderate High
SECTION 3: ADVERSE EVENTS Physical, social, psychological, or financial events that are anticipated due to subjects’ pre-existing disease. Expected AE due to Underlying Disease
Likelihood of event occurring
If event occurs, likely to be Serious?
Plan:

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
26
SECTION 4: RISK RELATED TO RESEARCH INTERVENTION Level Risk Study Procedures
1 No greater than minimal risk Standard psychological testing; epidemiological studies; blood draw, ECG, physical exam; use of otherwise discarded tissue obtained during a clinical procedure for clinical purposes only; behavioral study or nutritional assessment; surveys or questionnaires of a non-sensitive nature. Chart review. Use of already-developed database. Use of banked specimens.
2
Low Risk
Well-described, short-term treatments to relieve common symptoms with known safety data at a single site; trials with procedures such as indwelling catheter, endoscopy, lumbar puncture, bone marrow biopsy, oral glucose-tolerance test, induced sputum, skin biopsy, imaging studies, collection of sensitive information; therapeutic trials of an agent already approved for use in the population to be studied and for the indication already approved at a single site.
3
Moderate risk Vulnerable subjects if interventions are no greater than minimal or low risk. Subjects with disease exposed to placebo; therapeutic intervention trial involving procedure such as insulin clamp or organ biopsy. Studies involving subjects with illness being treated with procedures that may result in moderately severe adverse events.
4
Significant risk Clinical trials of diseases where the endpoints are major morbidity or mortality; assessment of serious toxicity requiring comparison of rates; implantation of a device with an IDE; use of a new chemical or drug for which there is limited or no available safety data in humans; gene transfer; multi-center trials involving risk to subjects; high-risk clinical procedure if performed solely for research purposes
SECTION 5: LIST YOUR SOURCES OF INFORMATION ABOUT RISK
Earlier studies (animal) Earlier trials (human) Investigator’s Brochure Package insert Other:
SECTION 6: DETERMINATION OF OVERALL RISK LEVEL Overall risk level is based on the factors described above in Sections 1 through 5 on study design, population being studied, and potential harms from participation in research. Considering all of these factors, the potential for harm to subjects in this study is
No more than minimal Low Moderate Significant SECTION 7: WHO WILL ASSESS SAFETY AND DATA INTEGRITY FOR YOUR STUDY?
Principal Investigator (required for all studies) Institutional Review Board (IRB – required for all studies) Independent Individual/Medical Monitor1 Internal Data and Safety Committee or Board with explicit guidelines2 Independent Data and Safety Monitoring Board (DSMB). NIH specifically requires the establishment
of Data and Safety Monitoring Boards (DSMBs) for multi-site clinical trials involving interventions that entail potential risk to the participants, and generally for Phase III clinical trails. Although Phase I and Phase II clinical trials may also use DSMBs, smaller clinical trials may not require this oversight format, and alternative monitoring plans may be appropriate.

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
27
SECTION 8: STUDY WIDE MONITORING FREQUENCY How often will the safety and data integrity of accumulating study-wide data across all subjects be monitored? Has a safety endpoint been established?
N/A No Yes – describe:
Has an efficacy endpoint been established? N/A No Yes – describe:
Have stopping rules been established? No Yes – describe:
SECTION 9: OTHER ASSESSMENTS a. WHAT will be assessed? b. Individual Subject Safety: List planned assessments and who will be responsible.
Safety Assessment
Special conditions/equipment Criteria leading to alteration or discontinuation of subject participation Personnel responsible for assessment
c. Data Quality and Confidentiality How will you check accuracy and quality of collected data? Were there any breaches of confidentiality? d. Regulatory Compliance If your study is sponsored, will the sponsor send a monitor?
Yes No Will you keep a Regulatory Binder?
Yes - No e. Evaluating and Reporting Adverse Events Who will evaluate adverse events for seriousness, expectedness, severity, and relationship to study intervention? What definitions will you use? What grading scales will you use to evaluate adverse event seriousness, severity, and relationship to study interventions? To which committees/agencies will adverse events be reported? (Check all that apply)
IRB (required) Others: Specify
Who will treat adverse events?

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
28
12.4.- Appendix IV: Massey University’s Notification of Low Risk Research/Evaluation
involving Human Participants
Te Kunenga ki Pürehuroa
NOTIFICATION OF LOW RISK RESEARCH/EVALUATION INVOLVING HUMAN PARTICIPANTS
(All notifications are to be typed)
(Do not modify the content or formatting of this document in any way)
SECTION A:
1. Project Title
Projected start date for data collection
Projected end date
(Low risk notifications will not be processed if recruitment and/or data collection has already begun.)
2. Applicant Details (Select the appropriate box and complete details)
ACADEMIC STAFF NOTIFICATION
Full Name of Staff Applicant/s
School/Department/Institute
Region (mark one only) Albany Palmerston North Wellington
Telephone Email Address
STUDENT NOTIFICATION
Full Name of Student Applicant
Postal Address
Telephone Email Address
Employer (if applicable)
Full Name of Supervisor(s)
School/Department/Institute
Region (mark one only) Albany Palmerston North Wellington
Telephone Email Address
GENERAL STAFF NOTIFICATION

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
29
Full Name of Applicant
Section
Region (mark one only) Albany Palmerston North Wellington
Telephone Email Address
Full Name of Line Manager
Section
3 Type of Project (provide detail as appropriate)
Staff Research/Evaluation:
Student Research: If other, please specify:
Academic Staff Name of Qualification
General Staff Credit Value of Research
Evaluation (e.g. 30, 60, 90, 120, 240, 360)
4. Describe the process that has been used to discuss and analyse the ethical issues present in this project. (Please refer to the Low Risk Guidelines on the Massey University Human Ethics Committee website)
During the project we will implement not only the “Code of Ethical Conduct for Research, Teaching and Evaluations Involving Human Participants” but also the New Zealand Psychological Society Code of Ethics (2007) and all other relevant University codes and policies, including the “Research Use of IT Infrastructure Policy”.
5. Summary of Project
Please outline the following (in no more than 200 words):
1. The purpose of the research, and 2. The methods you will use.
(Note: ALL the information provided in the notification is potentially available if a request is made under the Official Information Act. In the event that a request is made, the University, in the first instance, would endeavour to satisfy that request by providing this summary. Please ensure that the language used is comprehensible to all)
Please submit this Low Risk Notification (with the completed Screening Questionnaire) to:

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
30
The Ethics Administrator Research Ethics Office Old Main Building, PN221
Massey University Private Bag 11 222,
Palmerston North
SECTION B: DECLARATION (Complete appropriate box)
ACADEMIC STAFF RESEARCH Declaration for Academic Staff Applicant I have read the Code of Ethical Conduct for Research, Teaching and Evaluations involving Human Participants. I understand my obligations and the rights of the participants. I agree to undertake the research as set out in the Code of Ethical Conduct for Research, Teaching and Evaluations involving Human Participants. My Head of Department/School/Institute knows that I am undertaking this research. The information contained in this notification is to the very best of my knowledge accurate and not misleading.
Staff Applicant’s Signature Date:
STUDENT RESEARCH Declaration for Student Applicant I have read the Code of Ethical Conduct for Research, Teaching and Evaluations involving Human Participants and discussed the ethical analysis with my Supervisor. I understand my obligations and the rights of the participants. I agree to undertake the research as set out in the Code of Ethical Conduct for Research, Teaching and Evaluations involving Human Participants. The information contained in this notification is to the very best of my knowledge accurate and not misleading.
Student Applicant’s Signature Date:
Declaration for Supervisor I have assisted the student in the ethical analysis of this project. As supervisor of this research I will ensure that the research is carried out according to the Code of Ethical Conduct for Research, Teaching and Evaluations involving Human Participants.
Supervisor’s Signature Date:
Print Name
GENERAL STAFF RESEARCH/EVALUATIONS Declaration for General Staff Applicant I have read the Code of Ethical Conduct for Research, Teaching and Evaluations involving Human Participants and discussed the ethical analysis with my Supervisor. I understand my obligations and the rights of the participants. I agree to undertake the research as set out in the Code of Ethical Conduct for Research, Teaching and Evaluations involving Human Participants. The information contained in this notification is to the very best of my knowledge accurate and not misleading.
General Staff Applicant’s Signature Date:
Declaration for Line Manager I declare that to the best of my knowledge, this notification complies with the Code of Ethical Conduct for Research, Teaching and Evaluations involving Human Participants and that I have approved its content and agreed that it can be submitted.
Line Manager’s Signature & Name Date:

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
31
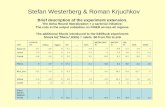
12.5.- Appendix V: Research Proposal Timeline
175.722.- Clinical Neuropsychology Research Proposal Timeline
Tasks Start date
Duration (days)
End date
Review proposal for feasibility with supervisor
18-Feb 8 26-Feb
Get phone numbers and addresses from Yellow Pages
20-Feb 5 25-Mar
Locate addresses on a map 19-Feb 1 20-Feb
Print-screen map with numbered dropped pins
20-Feb 1 21-Feb
Getting familiar with the surroundings by car
11-Mar 2 13-Mar
Program business locations in navigator
23-Feb 4 24-Feb
Visit potential participants 1 to 5 18-Feb 1 19-Feb
Evaluate response success 19-Feb 4 20-Feb
If response was low, select 5 more names and addresses.
24-Feb 4 25-Feb
Visit potential participants 6 to 10 19-Feb 18 10-Mar
Evaluate response success 10-Mar 2 12-Mar
If response was low, select 5 more names and addresses.
26-Feb 20 18-Mar
Allow time for further participant selection
28-Feb 20 28-Mar
Visit participants for informed consent and information about interview and testing
5-Mar 4 10-Mar
Ensure that all the tests are available 10-Mar 18 1-Apr
Book a room for all the interviews and testing processes.
12-Mar 16 12-Apr
Prepare and rehearse clinical interview 3-Mar 8 2-Apr
Read and rehearse test battery 5-Apr 8 20-Apr
Interview and test participants 1 to 10 21-Apr 3 30-May
Assess test results 1-Jun 28 30-Jun
Statistical analysis of test results 1-Jul 29 30-Jul
Write feedback and information reports 1-Aug 3 30-Aug
Book a room for all the feedback interviews.
1-Sep 3 20-Sep
Call to book a date and time for next year interviews
1-Dec 7 20-Dec

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
32
12.6.- Appendix VI: Research Proposal Budget Template
RESEARCH PROPOSAL BUDGET TEMPLATE
Research Project Title:
Duration of Project (months):
Nature of expenditure/ Item Quantity % of time NZ$
DIRECT COSTS
Personnel
Research Personnel
Principal Researcher/ Principal Investigator
Co-Researcher/Co- Investigator (if applicable)
Research Assistant ( part or full time/ Salary/month
Post Doctoral Associate
Graduate Students
Other Professionals:
Technician/ Programmer/ Assistants/Statistician, etc...
Project Assistant / Administrative Assistant
Clerical Assistance
Personnel Subtotal
Fringe Benefits
(25% on salaries of academic staff)
Fringe benefits Subtotal
Equipment
List of Equipment (include 40% on cost for freight charges)
Subtotal Equipment
Material and Supplies
List Materials and supplies
(include 40% on cost for freight charges for supplies from international sources)
Subtotal Material and Supplies
Travel
International Travel ( if Applicable to project )
Airfare and Destination from:…to: # of Trips
Traveller ( Amount / Trip ) # of Trips
Per diem ( $ / day ) # of Days
Local Transportation (if Applicable to Project )
Taxi Ride: from and to
Cost / Ride # of rides

175.722 – CLINICAL NEUROPSYCHOLOGY WESTERBERG, V. Master’s Degree Research Proposal
33
Car Rental per day # of Days
Gasoline Cost
Subtotal Travel
Publication/Reports
Editing & Proofreading
Translation cost/page # of pages
Book Cover Design
Layout, technical Production & Cost of Paper
Printing
Subtotal Publication
OTHER Direct Costs
Documentation (books & Software )
Consultant Services
Mail & Courrier
Communication / Internet/ Photocopying
Subtotal Other Direct Costs
WORKSHOP / CONFERENCE ( If applicable )
Workshop / conference Coordinator
Travel of Participants
Accomodation / Lodging / day # of nights
Perdiem / Guest ( $/Day* # of days* number of guests ) # of guests Invitation cards ( Design & Printing ) # of cards
Program ( Design & Printing ) # of Programs
Lunch ( Cost / Person ) # of People
Coffee Break - $----/person # of People
Social Event - $/guest # of guests
Photocopy
Press Officer
Materials & Supplies
Conference Equipment ( Overhead projector, flip chart, LCD etc )
Sound System $----/day # of days
Translation Booth $---/day # of days
Simultaneous Translation ( Translators ) $ / day # of days
Subtotal Workshop/Conference
Total Direct Costs
(Accounting Services, Auditor & Lawyers fees, Electricity, Maintenance, Depreciation of Equipment, use of office space, Insurance & renovation, and general project administration )
GRAND TOTAL (total direct costs + Indirect costs) ADDITIONAL COMMENTS: