CLINICAL AND · 2013-07-23 · Biomechanics of Maxillary Overdenture, 33 References and Additional...
Transcript of CLINICAL AND · 2013-07-23 · Biomechanics of Maxillary Overdenture, 33 References and Additional...



CLINICAL AND
LABORATORY
MANUAL OF
IMPLANT
OVERDENTURES


CLINICAL AND
LABORATORY
MANUAL OF
IMPLANT
OVERDENTURES
Hamid R. Shafie

Dr. Hamid R. Shafie received certification in Ad-vanced Graduate Study of Prosthodontics from theGoldman School of Dental Medicine at Boston Uni-versity. He founded the Center for Oral Implantologyat Johns Hopkins University, where he trained manydentists in various aspects of implant dentistry. Dr.Shafie is president of the American Institute of Im-plant Dentistry, based inWashington, D.C. He is a fac-ulty member in the Department of Oral and Maxillo-facial Surgery at Washington Hospital Center, wherehe teaches postgraduate courses in oral implantology.He is an adjunct faculty member of the Boston Uni-versity Center for Implantology.
C© 2007 Hamid ShafieAll rights reserved
Editorial Offices:Blackwell Publishing Professional,2121 State Avenue, Ames, Iowa 50014-8300, USATel: +1 515 292 01409600 Garsington Road, Oxford OX4 2DQTel: 01865 776868
Blackwell Publishing Asia Pty Ltd,550 Swanston Street, Carlton South,
Victoria 3053, AustraliaTel: +61 (0)3 9347 0300Blackwell Wissenschafts Verlag, Kurfurstendamm 57,
10707 Berlin, GermanyTel: +49 (0)30 32 79 060
The right of the Author to be identified as the Authorof this Work has been asserted in accordance with theCopyright, Designs and Patents Act 1988.
All rights reserved. No part of this publication may bereproduced, stored in a retrieval system, or transmit-ted, in any form or by any means, electronic, mechan-ical, photocopying, recording or otherwise, except aspermitted by the UK Copyright, Designs and PatentsAct 1988, without the prior permission of the pub-lisher.
First published 2007 by Blackwell Munksgaard, aBlackwell Publishing Company
Library of Congress Cataloging-in-Publication Data
Clinical and laboratory manual of implantoverdentures/[edited by] Hamid R. Shafie.
p. ; cm.Includes bibliographical references and index.ISBN-13: 978-0-8138-0881-9 (alk. paper)ISBN-10: 0-8138-0881-2 (alk. paper)1. Implant-supported dentures. 2. Dental
implants. I. Shafie, Hamid R.[DNLM: 1. Denture, Complete. 2. Dental
Prosthesis, Implant-Supported. 3. Denture,Overlay. WU 530 C641 2006]
RK667.I45C55 2006617.6′93—dc22
2006036528
For further information on Blackwell Publishing, visitour website: www.blackwellpublishing.com

Dedication
I am dedicating this book to the memory of my beloved daughter Melody. I wrote most of this booksitting next to her hospital bed during her fight with neuroblastoma cancer. She was a symbol ofstrength and hope in life.
And . . .To my parents, Mehdi and Minoo, who gave me a love of life,To my wife Maryam, who gave me a life of love,To my daughter Ava, who gave joy and meaning to it all.
v

Acknowledgments
My enormous gratitude to the Blackwell Pub-lishing team for their willingness to go to batwith me: Antonia Seymour, Vice President, Pro-fessional Publishing; Dede Andersen, Manag-ing Editor; Don Kehoe, Marketing Manager;Judi Brown, Project Manager/Editor; MartinNielsen, Business Development Executive; andall of the other supporters at the Blackwell Pub-lishing. They stood by me during the toughestperiod of my life and they never gave up on me.
My special thanks to Natalie Baratpour,the medical illustrator from Globalgraphic. Shespent countless hours working with me tocreate all of the beautiful artwork for thisbook.
I would like to extend my special apprecia-tion to my invaluable business manager AmandaLudwa and my friend Christopher “Chris”Ludwa.
vi

Contents
CONTRIBUTORS, xiii
FOREWORD, xvDennis Tarnow
FOREWORD, xviZhimon Jacobson
INTRODUCTION, 1Hamid Shafie
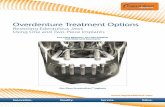
1 Patient Preferences andExpectations, 3Hamid Shafie
Implant Overdenture vs. ConventionalDenture, 3
Implant Overdenture vs. FixedImplant-Supported Prosthesis, 4
Indications for Implant Overdenture, 4Comparison of Treatment Strategies for
Implant Overdentures, 4The Breda Implant Overdenture Study, 5Overdenture Treatment Strategies, 6Common Mistakes in Constructing
Implant-Supported Overdentures, 6Successful Implant-Supported
Overdenture, 6References and Additional Reading, 6
2 Diagnosis and TreatmentPlanning, 11Hamid Shafie
Diagnostic Workup for ImplantOverdenture, 11
Benefits of Diagnostic Mounting, 11Radiographic Evaluation, 12
Panoramic Radiograph, 12Occlusal Radiograph, 13Computed Tomography
(CT Scan), 14Joint Treatment Planning, 15Anatomical Considerations During
Diagnosis and Treatment PlanningProcess, 15
Available Bone Quantity, 15Classification of Fully Edentulous
Ridges Based on BoneQuantity, 15
Classification of Edentulous RidgesBased on Bone Quality, 17
References and Additional Reading, 19
3 Surgical Guide and DiagnosticStent, 24Hamid Shafie, Wolfram Stein, andAmir Juzbasic
vii

viii CONTENTS
Classification of Surgical Guides, 26Gingiva Supported, 26Bone Supported, 26
Components and the Advantages of themed3D Technology, 27
Implant 3D Planning Software, 27Stationary Robot or Positioning
Device X1, 29Procedural Steps, 29References and Additional Reading, 29
4 Principles of AttachmentSelection, 31Hamid Shafie
Types of Attachments Basedon Resiliency, 32
Rigid Non-ResilientAttachments, 32
Restricted Vertical ResilientAttachments, 32
Hinge Resilient Attachments, 32Combination Resilient
Attachments, 32Rotary Resilient Attachments, 32Universal Resilient Attachments, 32
Attachment Selection Criteria, 32Different Attachment Assemblies, 33Factors Influencing the Design and
Resiliency Level of the AttachmentAssembly, 33
Biomechanical Considerations, 33Distal Extension to the Bar, 33Load Distribation of Stud vs. Bar
Attachments, 33Biomechanics of Maxillary
Overdenture, 33References and Additional Reading,
34
5 Stud Attachments, 37Hamid Shafie and James Ellison
Important Considerations Regarding theAlignment of Stud Attachments, 37
ERA Attachment, 37Chair-Side Utilization Procedure, 39Changing ERA Male Component, 43
VKS-OC rs Stud Attachment, 44Different Types of Matrices/Clips, 45
Clinical and Laboratory Proceduresfor VKS-OC rs AttachmentEmbedded in the AcrylicDenture Base, 45
Clinical and Laboratory Proceduresfor VKS-OC rs Attachment Castwithin the Chrome CobaltFramework, 49
Home Care, 52Straumann Retentive Anchor
Abutment, 52Contraindications for Using
Retentive Anchors, 53Design Specifications of the
Retentive Anchor and ItsCorresponding EllipticalMatrix, 53
Adjusting the Retention of theFemale Component, 54
Chair-Side Utilization of theRetentive Anchor Abutment andElliptical Matrix, 55
Clix® Attachment and the Astra Implant,57
Design Specification of the Clix®
Female Component, 57Design Specification of the Astra Ball
Abutment, 57Chair-Side Utilization Procedure, 58Replacing Clix® Inserts, 59
References and Additional Reading,60
6 Bar Attachments, 63Hamid Shafie and James Ellison
Bar Materials, 63Classification of Bar Attachments
Based on Cross-SectionalShapes, 63
Classification of Bars Based on theNature of Their Resiliency, 64
Factors that Influence the Flexibility ofthe Bar, 64
Fundamentals of Bar Arrangement,64
Vertical Relationship of the Bar to theAlveolar Ridge, 66
Sagittal Relationship of the Bar to theAlveolar Ridge, 66

CONTENTS ix
Sagittal Relationship of the Bar to theHinge Axis, 67
Anterior-Posterior DistanceRule, 68
Guidelines for Denture BaseExtension, 68
Hader Bar, 69Fabrication Procedures for a
Castable Hader Bar Attachmentwith Plastic Clips/Riders, 70
Fabrication Procedures for aCastable Hader Bar Attachmentwith Gold Alloy Clips/Riders, 71
Hader Clip Placement, 71Plastic Hader vs. Metal Clips, 72Mandibular Implant-Supported
Overdenture Utilizing HaderBar and Castable ERAAttachment, 72
Troubleshooting for Hader BarAttachment Assembly, 72
Dolder Bar, 72Indications, 72Contraindications, 73Dimensional Specifications, 73Fabrication Procedure for a Dolder Bar
Unit, 75Relining an Overdenture with a
Dolder Bar Unit AttachmentAssembly, 75
Fabrication Procedure for a Dolder BarJoint, 75
Relining an Overdenture with aDolder Bar Joint AttachmentAssembly, 76
Vario Soft Bar Pattern VSP, 76Advantages of Prefabricated
Titanium Bar, 77Advantages of Plastic Castable
Bar, 77Shapes of VSP Bar, 77Shapes of VSP Bar’s Clips, 77Fabrication Procedures of a Rigid
Fully Implant-BorneOverdenture Using a ParallelBar, 78
Fabrication Procedures of a HingeResilient Overdenture Using aBredent VSP Bar, 81
Verification of Passive Seat of theBar, 82
Incorporation of the Bar Assemblyinto the Denture, 82
References and AdditionalReading, 82
7 Spark Erosion, 85Hamid Shafie, Eduard Eisenmann,and Gunter Rubeling
Sheffield Test, 85Most Common Reasons for Ill Fit, 88Spark Erosion Process, 88
Clinical Steps, 89Laboratory Steps, 90Second Case, 96
References and Additional Reading, 102
8 Treatment Success with ImplantOverdenture, 104Hamid Shafie
Implant Survival, 104Prosthetic Success, 104Patient Related Factors, 105Biomechanical Risk Factors for Upper
Implant Overdenture, 105Biomechanical Risk Factors for Lower
Implant Overdenture, 106Shape of the Mandible and Its Effect on
the Loading of the SupportingImplants, 107
References and Additional Reading, 108
9 Occlusion and Implant-SupportedOverdenture, 112Hamid Shafie and Frank Luaciello
Different Occlusal Schemes Formed byDenture Teeth, 112
Set-Up Procedure for the BalancedOcclusion Utilizing Vita PhysiodensTeeth, 113
Setting Up the Premolars, 113Setting Up the Molars, 116
Important Points to Remember Duringthe Occlusal Adjustment, 120
Semi-Anatomic, 120Non-Anatomic, 120Lingualized, 122

x CONTENTS
History of Lingualized (Lingual Contact)Occlusion, 123
Set-Up Procedure for LingualizedOcclusion Utilizing IvoclarOrtholingual Teeth, 123
1: Position Mandibular Teeth, 1242: Position Maxillary Teeth, 1253: Eliminate Maxillary Buccal Cusp
Interferences, 1264: Eliminate Anterior Interferences,
1275: Eccentric Balance, 127
Equilibration after Processing, 1281: Re-Establish Centric Occlusion
Contacts, 1282: Eliminate Maxillary Buccal Cusp
and/or Anterior Interferences,129
3: Complete Equilibration byAdjusting Only the InclinePlanes of the MandibularPosterior Teeth, 129
Eccentric Jaw Movements, 129References and Additional Reading, 130
10 Surgical Considerations for ImplantOverdenture, 132Richard Green, George Obeid, RoyEskow, and Hamid Shafie
Presurgical Instructions, 132Treatment Room Preparation and
Utilization Protocol, 133Patient, 133Instruments, 133
Incisions and Flap Design, 133Incision and Flap Design
Objectives, 133Basic Flap Designs, 133
Mandibular Surgery, 1341: Crestal Incision, 1342: Extended Crestal Incision, 1343: Vestibular Incision, 135
Maxillary Surgery, 1361: Crestal Incision, 1362: Palatal Incision, 1363: Buccal Incision, 136Tissue Punch Technique, 136
Osteotomy and Implant Placement, 137Procedural Considerations during the
Surgery, 137
Suturing Techniques Used for ImplantOverdenture Surgeries, 138
1: Simple Interrupted, 1382: Continuous (Locking or
Non-Locking), 1383: Horizontal Mattress, 139Most Common Suturing Techniques
for Implant-SupportedOverdenture Cases, 139
Suture Material, 139Post-Surgical Care, 139
Post-Healing Criteria for SuccessfulIntegration of the Implant withSurrounding Tissues, 140
Procedural Considerations afterSurgery, 140
Site Preparation for Overdentures, 140Techniques for Site Development,
140Bone Grafting Materials, 140Available Resorbable Membranes,
142Split-Control System, 144
Bone-Spreading Sequence, 144Surgery-Related Problems, 146References and Additional Reading,
148
11 Straumann Implant System, 153Hamid Shafie
Two Sections of Straumann Implants,153
Rough Surface on the Implant Body,153
Polished Collar, 153Endosseous Diameters, 154Recommended Attachment Assemblies
for Straumann Implants, 155Surgical Steps for Standard Implants
Ø 4.1mm RN (Regular Neck), 1551: Preparation of the Implant Bed, 1552: Drilling Sequence for Standard
Implants Ø 4.1mm RN (RegularNeck), 156
3: Tapping the Implant Site, 1564: Implant Insertion, 156
Wound Closure, 159Healing Period for Straumann Implants
with SLA Surface, 160

CONTENTS xi
12 Endopore® Dental ImplantSystem, 161Hamid Shafie
Basic Facts, 161External Connection, 162Internal Connection, 162
Mechanical Rational for ShortEndopore® Dental Implants, 162
Advantages of the Endopore® DentalImplant System, 162
Surgical Steps, 163Postsurgical Instructions, 166Implant Uncovering Steps, 167Prosthetic Steps, 167
13 Overdenture Implants, 168Hamid Shafie
Classification of Overdenture ImplantsBased on Attachment DesignFeatures, 168
Two Basic Purposes for OverdentureImplants, 169
Providing Immediate Stabilizationfor an Overdenture, 169
Acting as Transitional ImplantsDuring Initial Healing Phase, 169
Maximus OS Overdenture Implant,169
Unique Features, 170Clinical Considerations, 170Surgical Steps, 171Prosthetic Steps, 178
ERA® Overdenture Implant, 179Design Specifications, 180Surgical Steps, 180Prosthetic Steps, 187Changing ERA Male
Component, 189References and Additional Reading,
191
14 Loading Approaches for MandibularImplant Overdentures, 192Dittmar May, George Romanos, andHamid Shafie
Healing Period before Loading, 192Three Concepts in Premature Loading,
192
Early Loading, 192Progressive Loading, 192Immediate Loading, 192
Critical Factors in Determining LoadingStrategies, 192
Important Indicating Factors forSuccess of Prematurely LoadedImplants, 193
Advantages of Immediate Loading inImplant-Supported OverdentureCases, 193
Important Requirements for TreatmentProtocol, 193
SynCone® Concept, 194Advantages of Telescopic Crown
Techniques, 194Patient Selection, 194Pre-Surgical Steps, 194Surgical Steps, 194Prosthetic Steps, 198Postoperative Instructions for
Patient, 201Delayed Loading Protocol with
SynCone® Concept, 202Troubleshooting, 202SynCone® Abutments and Framework-
Reinforced Overdenture, 203Procedural Sequences, 203References and Additional Reading, 204
15 Clinical Applications for theMeasurement of Implant StabilityUsing Osstell™ Mentor, 206Hamid Shafie and Neil Meredith
Clinical Stages When ISQ MeasurementCan Be Recorded, 208
Clinical Conditions Affecting theOutcome of ImmediatelyLoaded Implants, 208
16 Follow Up and Maintenance of theImplant Overdenture, 210Valerie Sternberg Smith andRoy Eskow
Characteristics of Ideal Peri-ImplantTissues, 210
Consequences for Failure to AchieveCleansable Attachment Design, 210

xii CONTENTS
Home Care Implements, 211Toothbrushes, 211Flossing Cords, 212Denture Brushes, 212Antimicrobials, 212
Recommended Routines at RecallVisits, 213
Radiographic Examination, 213Removal of Accretions, 213Cleaning the Prosthesis, 213Evaluation of the Attachment
Assembly Components, 213References and Additional Reading, 214
17 Core Principles of the SuccessfulImplant Practice, 216Sean Crabtree, Paul Homoly, AndressCharalabous, Peter Warkentin, andKornelius Warkentin
Vision, Team, Systems, Sales,Marketing, 216
Center Point VISION, 216Organizational Model/Systems, 217People, 218Sales, 220Marketing, 223
Why Making Implant Overdentures CanMake Your Restorative PracticeClick, 224
Attracting Older Patients, 224Case Acceptance for Complete
Dentistry, 225Branding of an Implant Practice, 226
Identity Ambassadors, 226External Marketing
Objectives, 227Marketing Research, 227Create a Brand Name for Your
Practice, 227Website, 227
Design Criteria for an ImplantPractice, 228
Reception Area, 229Waiting Room, 229Consultation Room, 230Surgical Operatory, 230Prosthetic Operatory, 230Hygiene and Recall Operatory, 231Sterilization Area, 231Staff Lounge, 231
INDEX, 233

Contributors
Andreas Charalambous, AIA, BArchCornell UniversityPrincipal, FORMA Design, Inc.
Sean M. Crabtree, BBAChairman/CEO Fortune Management
of TN, Inc.
Eduard Eisenmann, DMDAssistant Professor and Clinical LecturerCharite-University Medizin BerlinCampus Benjamin Franklin,Department of Restorative DentistryBerlin, GermanyPrivate Practice Limited to Implant
ProsthodoticsMannheim, Germany
James T. Ellison, CDT, BA, AASDirector of Education for the ERA Academy
Roy L. Eskow, DDSPractice Limited to Periodontics, Oral
Medicine, Implant, and RegenerativeSurgeries
Bethesda, Maryland
Robert N. Eskow, DMD, MScDClinical Professor,The Ashman Department of Implant Dentistry,New York University,College of DentistryPrivate Practice,Livingston, New Jersey
Richard J. Green, DDS, MScDStaff PeriodontistVA Hospital,Baltimore, MarylandPrivate Practice Limited to Periodontics,
Regenerative, and Implant DentistryBethesda, Maryland
Paul Homoly, DDS, CSPPresidentHomoly Communications Institute
Amir Juzbasic, MDTDirector of Laboratory ServicesAmerican Institute of Implant Dentistry
Frank Lauciello, DDSAssociate ProfessorState University of New York at Buffalo
xiii

xiv CONTRIBUTORS
Dittmar May, DMDOral and Maxillofacial SurgeonPractice Limited to Implant DentistryLunen, Germany
Neil Meredith, BDS., MSc., FDS, RCS,PhD (U.Lond.), PhD (U.Got.)Visiting ProfessorUniversity of Bristol,England
George Obeid, DDSChairman, Department of Oral and
Maxillofacial SurgeryWashington Hospital Center
George Romanos, DDS,Dr.med.dent., PhDClinical Professor of Implant DentistryNew York University,New York, USAAssociate Professor of Oral Surgery
and ImplantologyUniversity of Frankfurt, Germany
Gunter Rubeling, MDTHead of Department SAE DENTAL
VERTRIEB + Development, BremerhavenHead of Department Rubeling + KlarDental-Labor GmbH,Berlin, Germany
Wolfram Stein, MSc., PhDDepartment of Cranio-Maxillo-Facial Surgery,University of Heidelberg, GermanyResearch Group for Computer Assisted
Surgery
Valerie Sternberg Smith, RDH, BSClinical Instructor,The Ashman Department of Implant Dentistry,New York University,College of DentistryPrivate PracticeLivingston, New Jersay
Kornelius WarkentinArchetectual Solutions and Human FactorSpecialistIS2 Teaching CenterWashington, DC
Peter WarkentinDirector of Patient/Doctor Interactive InteriorDesign CoursesIS2 Teaching centerWashington, DC

Foreword
With all of the books available today onimplants, it is refreshing to see one that is sowell documented and thought out. It is a greathonor for me to write this Foreword forDr. Shafie’s Clinical and Laboratory Manualof Implant Overdentures. With more than20 million Americans being fully edentulous,there is no better time for this book to bewritten and utilized. Undergraduate programsacross the country are finally realizing that thetwo implant overdenture is, by far, therecommended treatment of choice over leavingsomeone fully edentulous. The amount of boneloss that we in dentistry have seen in fullyedentulous patients during past generations isfrightening to consider. We actually thoughtand were teaching that this aveolar boneatrophy was “normal”and continuous after extraction. What we nowknow is that two implants in the anteriormandible will stop this progressive bone lossand preserve the ridge instead of compressing itslowly as time passes.Dr. Shafie should be complimented for hisoutstanding and detailed work. He describeseach chapter with diagrams that are easy tofollow, along with clinical pictures to
document his thoughts. He also has coveredthe various abutment connections from manyof the commercial companies that are beingused today by clinicians all over the world. Thediscussion of occlusion and loading isparticularly important for the technician andthe clinician to understand. This manual is wellorganized and easy to follow with its step bystep breakdown of each topic and technique.Besides the different implants and abutmentsthat are available, the manual also goes intogreat detail on the construction of bars andhow to best utilize them for different clinicalsituations. There is even a practicemanagement chapter to help the clinicianincorporate this technology into a practice.This clinical laboratory manual should becomethe gold standard for technicians andclinicians when dealing with overdentures. Mydeepest congratulations for a job well done toDr. Shafie and his contributors.
Dennis Tarnow, Professor and ChairmanDepartment of Implant DentistryNew York University College of Dentistry
xv

Foreword
Given the increasing number of totallyedentulous patients around the world, havingthe knowledge to plan treatment and place andrestore implant-supported overdentures ismore important than ever. Totally edentulouspatients can become dentally-functionalthrough the placement of dental implants tosupport complete dentures. It is a great injusticeto allow patients, especially those who arefinancially restricted, to go through their liveswithout the renovating benefit of implants.The best venue for dentists to learn to treatpatients with implants is in dental school aspart of the regular curriculum. Dentaleducationaround the world has been lacking in trainingdental students about implantology, especiallywith regards to implant-supported completedentures. This inadequacy has forced manydentists to seek training in implantologythrough short courses sponsored by implantcompanies. With several hundred implantsystems available today, making sense ofdifferent options, surgically and prosthetically,is a monumental task. Dentists need accurateinformation regarding all aspects of
implantology, presented scientifically andwithout commercial bias, and this book hasfulfilled those requirements. Dr. Hamid Shafiehas authored a very comprehensive andcomplete book that addresses the mostcommon problems general dentists face inrestoring implant-supported dentures.Clinical and Laboratory Manual of ImplantOverdentures is invaluable as an educationaltool and will be effective as a resource for bothinexperienced and experienced dentists intreating edentulous patients. As aprosthodontic alumnus of Boston UniversityGoldman School of Dental Medicine, Dr. Shafiehas used his vast knowledge and experience toput together a very informative book on howto plan treatment and how to utilizeattachments in implant-supported removabledentures. I congratulate Dr. Shafie for his hardwork in compiling this information andpresenting it in such a logical manner.
Zhimon Jacobson, Professor/DirectorCenter for ImplantologyBoston University Goldman School of DentalMedicine
xvi

CLINICAL AND
LABORATORY
MANUAL OF
IMPLANT
OVERDENTURES


Introduction
Hamid Shafie
Total edentulism has been noted in 5 percentof adults who are 40 to 44 years old. This per-centage gradually increases to almost 42 percentin seniors. However, these percentages are de-ceptively low because the baby boomer gener-ation outnumbers the current population over65. We will see a significant increase in the num-ber of fully edentulous patients by the time babyboomers reach ages 65 and above.
The majority of general dentists still fabricateconventional complete, removable dentures fortheir fully edentulous patients. One of the maincomplaints of these patients is the instability ofthe lower denture. Since the conventional den-ture is fully tissue born and transfers all of themasticatory forces to the residual ridge, patientstend to experience significant and rapid loss ofthe alveolar ridge. Therefore, even an ideallyfabricated, lower, removable, complete denturewill be unstable after several months. This prob-lem has helped denture adhesive manufacturesbuild a multimillion-dollar market. Denture ad-hesive can be a quick solution for instability ofremovable prostheses but it does not eliminatethe etiology; that is, constant bone loss due to
direct transmission of masticatory forces to theresidual alveolar ridge.
Dental implants have changed the face ofprosthetic dentistry. They have shown a greatsuccess rate, as recorded in over 35 years of doc-umentation. Dental implants were introduced tothe United States in 1984 as an alternative treat-ment option for fully edentulous patients. Sincethen, however, most restorative dentists have fo-cused on utilizing them more in the treatment ofpartially edentulous patients and less in treat-ing fully edentulous patients. Probably one ofthe main reasons for devoting more attentionto fixed partial dentures supported by implantsis the significant demand by the sophisticatedbaby boomer generation. When this section ofpopulation reaches retirement age, we will see asignificant demand for implant-supported over-dentures.
The main benefit that the patient receivesfrom any kind of implant treatment is preven-tion of further bone loss in areas where tooth orteeth are missing. Implant-supported overden-tures not only provide required stability for thepatient but also eliminate the etiology of thisproblem by preventing further bone loss.
All of the money that patients are payingfor denture adhesive and fabrication of new
1

2 CLINICAL AND LABORATORY MANUAL OF IMPLANT OVERDENTURES
conventional, removable dentures in the courseof several years can be invested in more success-ful and predictable treatment options such asimplant-supported overdentures.
One of the main reasons why restorative den-tists may be reluctant to offer implant-supportedoverdentures to their patients is the complexityof attachment assemblies. About two hundreddifferent attachments are available, making itdifficult to choose the right attachment for a par-ticular patient.
This book encourages the use of implant over-dentures for fully edentulous patients and pro-vides the information required to simplify theprocedure:
� An easy way of classifying attachments re-gardless of brand name.
� Guidelines for the indications of each attach-ment assembly.
� Clinical steps fully illustrated with color pic-tures and schematic drawings.
� Treatment plan presentations for potentialcandidates of each type of treatment.
� Internal and external marketing methods re-lated to each treatment modality.
Implant-supported overdentures should bethe standard of care for all fully edentulouspatients. Conventional, removable, completedentures should be offered to a patient only ifthere is a medical or dental contraindication forimplant placement or if the patient is not in afinancial situation to afford an ideal treatmentplan.

1Patient Preferencesand Expectations
Hamid Shafie
Results from some studies show a weak as-sociation between a patient’s satisfaction withtheir prosthesis and the clinical qualities of theprosthesis as assessed by dentists. Some reportsalso show very little correlation between a pa-tient’s satisfaction and the clinical evaluation ofthe denture fit. On the other hand, a strong asso-ciation does exist between a patient’s perceivedmasticatory efficiency and their satisfaction withthe prosthesis.
IMPLANT OVERDENTUREVS. CONVENTIONALDENTURE
A major problem for edentulous patients hasbeen a lack of satisfaction with their completedentures. A survey of elderly patients showed
that 66 percent were dissatisfied with theircomplete dentures. The main reasons for thisdissatisfaction were discomfort, poor fit andretention, soreness, and pain, especially withmandibular dentures. Patients typically experi-ence significantly less chewing difficulties withimplant-supported overdentures than with con-ventional dentures. An evaluation of the mas-tication time and the magnitude of mastica-tory strokes show an almost equal efficiencyfor implant-supported overdentures and fixedimplant-supported prosthesis. The implant pro-cedure is relatively simple, and the treatmenttime is similar to that for complete dentures.
The data from several randomized studiesconfirm that implant-supported overdenturesprovide a better outcome than conventional den-tures. Benefits include psychological effects suchas satisfaction and oral health-related qualityof life, as well as functional benefits such aschewing ability. This improved function couldincrease the range of foods that an edentulouspatient can eat and, as a result, improve theirnutrition and general health.
3

4 CLINICAL AND LABORATORY MANUAL OF IMPLANT OVERDENTURES
IMPLANT OVERDENTUREVS. FIXED IMPLANT-SUPPORTED PROSTHESIS
Creating a natural aesthetic, enhancing facialappearance, and compensating for lost softand hard tissue is much easier with implantoverdentures than with fixed prosthesis. Mostpatients can afford one type of implant over-denture since they are less expensive comparedto fixed prosthesis. If one or more of the sup-porting implants fail, it is also easier to modifyan existing implant overdenture. A two-piece,precision fit implant overdenture is a good so-lution when the implants are placed in an unfa-vorable trajectory and cannot be utilized for afixed prosthesis. A milled substructure bar helpscreate an ideal path of insertion and an idealaesthetic outcome.
Overdenture treatment has less clinical in-volvement compared to the fixed prosthesis,which is especially important in elderly patientswith a medically compromised condition. In ad-dition, this treatment option can be used in pa-tients with compromised available bone. Im-plant survival rate is comparable to that for fixedimplant-supported prosthesis.
INDICATIONS FOR IMPLANTOVERDENTURE
� Compromised bone support for conventionaldenture
� Poor neuromuscular coordination� Low tolerance of mucosal tissues for a remov-
able acrylic base� Parafunctional habits leading to instability of
prosthesis� Active or hyperactive gag reflexes, stimulated
by upper removable denture� Psychological inability to wear a removable
prosthesis� Patient dissatisfaction with complete den-
tures and desire for more stability and com-fort
� Congenital or oral and maxillofacial defectsthat need oral rehabilitation
� High prosthodontic expectations
COMPARISON OFTREATMENT STRATEGIESFOR IMPLANTOVERDENTURES
The implant overdenture obtains support andretention from an attachment assembly affixedto the implant and to the denture base. Consid-ering the nature of masticatory force distribu-tion, three basic types of implant overdenturesare available:
� Mainly Tissue-Supported Implant Overden-ture: When two prefabricated individual at-tachments are utilized, the overdenture ismainly tissue-born. The attachments provideretention for the overdenture. With this treat-ment modality, the denture base should pro-vide maximum tissue coverage, similar to aconventional complete denture. During mas-tication, the residual ridge receives the ma-jority of the masticatory forces, which meansthat this type of prosthesis is mainly tissue-born rather than implant-born.
� Tissue-Implant-Supported Overdenture: Tis-sue-implant-supported overdenture is moreimplant-born compared to the previous typeof overdenture. To fabricate this type of over-denture, two implants and a resilient bar at-tachment assembly should be utilized. Thedenture base should still provide extendedtissue coverage. During mastication, the at-tachment assembly and supporting implantsreceive most of the masticatory forces. Theremainder of the chewing forces are trans-ferred to the posterior aspect of the overden-ture and ultimately absorbed by the support-ing tissue.
� Fully Implant-Supported Overdenture: Anattachment assembly that usually includesfour or more implants supports the fullyimplant-supported overdenture. During

PATIENT PREFERENCES AND EXPECTATIONS 5
mastication, the attachment assembly trans-fers all of the masticatory forces to thesupporting implants. With this type ofoverdenture, minimum flange and tissuecoverage is required since the prostheses arefully implant-born. A minimum of four im-plants is required. In a patient with an ovoidor pointed alveolar ridge, three implantscan be placed between the two mandibularforamens to form a tripod. In this case, theattachment assembly is not resilient, and theprosthesis is fully implantborn.
Successful fabrication of mainly tissue-supported implant overdentures and/or tissue-implant-supported overdentures still must ad-here to the basic principles for fabricating aconventional complete dentures:
� Accurate impression of underlying tissue� Maximum adaptation between the denture
base and the residual ridge� Proper vertical dimension of occlusion� Accurate centric relation� Appropriate denture teeth delection and set
up
Any clinical or laboratory error in fabricat-ing the implant overdenture may result in insta-bility of the prosthesis, soreness, and ultimatelypatient dissatisfaction.
The mainly tissue-supported implant over-denture requires two implants placed betweenthe mandibular foramen. The most commonposition is the canine area. However, placingthe implants in the lateral area (approximately14–15mm center to center) is another viableoption. This option provides the opportunityto place more implants posterior in case theprosthesis must be changed to tissue-implant-supported or fully implant-supported in thefuture.
Another advantage of placing the implantsin the lateral position is that it minimizes thehinge movement of the prosthesis around theaxis, which passes through the attachments. Ifthe implants were in the canine position, morehinge movement would occur when the patienttries to cut food with the lower incisors. Plac-
ing the implant in the lateral position reducesthe anterior-posterior distance from the incisaledges to the hinge axis between the implants.This reduces the lift and movement of the pos-terior section of the overdenture away fromthe residual ridge, which ultimately increasesstability.
THE BREDA IMPLANTOVERDENTURE STUDY
The Breda Implant Overdenture Study (BIOS)was set up as a randomized, controlled clinicaltrial to compare three different treatment op-tions for edentulous patients using the Strau-mann implant system. One hundred and tenedentulous patients with atrophic mandiblesand persistent conventional complete dentureproblems were selected. One-third of the pa-tients received a mainly tissue-supported over-denture supported by two implants and twoprefabricated ball attachments (2IBA), one-thirdreceived a tissue-implant-supported overdentureon two implants with a single bar (2ISB), andone-third received a fully implant-supportedoverdenture on four implants with a triple bar(4ITB).
For an overdenture with ball attachments,two Dolla Bona matrixes were used. For group2ISB, an egg-shaped Dolder Bar with a singlematrix was used. For group 4ITB, three egg-shaped Dolder Bars and three correspondingmatrixes were used. The investigators reportedthat treatment of the edentulous mandible withfour implants and three bar attachments is sig-nificantly more expensive than treatment withtwo individual attachments. However, multiplebar attachment assemblies require less long-termpost-care costs. During the 96-month period ofthis investigation, the two implants and singlebar attachment appeared to be the most ef-fective for edentulous patients when consider-ing patient satisfaction, clinical performance ofthe prostheses, and cost effectiveness. The studyalso found that patients who smoke are at a

6 CLINICAL AND LABORATORY MANUAL OF IMPLANT OVERDENTURES
higher risk of complications when treated withmandibular implant overdentures.
OVERDENTURETREATMENT STRATEGIES
The following factors affect the decision-makingprocess regarding overdenture treatment strate-gies:
� Soreness and discomfort associated with thedenture base and its flanges
� Bone quantity� Patient’s expectation for the treatment out-
come� Expected oral hygiene and patient compli-
ance� Jaw relationship� Distance between the upper and lower alve-
olar ridge� Expertise of the dentist and the lab technician� Patient’s finances
COMMON MISTAKES INCONSTRUCTINGIMPLANT-SUPPORTEDOVERDENTURES
� Poor treatment planning� Imprecise final impression� Inaccurate master model as well as working
model� Ill fitting framework� Poor choice of material and attachment.
SUCCESSFULIMPLANT-SUPPORTEDOVERDENTURE
Following are the basic requirements for a suc-cessful implant-supported overdenture:
� Stress-free fit of attachment assembly� Good oral hygiene� Biocompatibility of the chosen materials
� High biomechanical strength of chosen ma-terials
� Functional and equilibrated occlusion� Natural looking aesthetics� Absence of interferences with normal phonet-
ics
REFERENCES ANDADDITIONAL READING
Adell, R. (1983). Clinical results of osseointegratedimplants supporting fixed prosthesis in edentulousjaws. Journal of Prosthetic Dentistry, 50, 251–254.
Adell, R., Eriksson, B., Lekholm, U., Branemark, P. I.,& Jemt, T. (1990). A long-term follow-up studyof osseointegrated implants in the treatment oftotally edentulous jaws. International Journal ofOral & Maxillofacial Implants, 5, 347–359.
Adell, R., Lekholm, U., Rockler, B., & Branemark,P. I. (1981). A 15-year study of osseointegrated im-plants in the edentulous jaw. International Journalof Oral Surgery, 10, 387–416.
Albrektsson, T., Blomberg, S., Branemark, A., &Carlsson, G. E. (1987). Edentulousness—an oralhandicap. Patient reactions to treatment withjawbone-anchored protheses. Journal of Oral Re-habilitation, 14, 503–511.
Allen, P. F., & McMillan, A. S. (2002). Food selec-tion and perceptions of chewing ability followingprovision of implant and conventional prosthesesin complete denture wears. Clinical Oral ImplantResearch, 13, 320–326.
Anttila, S. S., Knuuttila, M. L., & Sakki, T. K. (2001).Relationship of depressive symptoms to edentu-lousness, dental health, and dental health behav-ior. Acta Odontologica Scandinavica, 59, 406–412.
Awad, M. A. & Feine, J. S. (1998). Measuring patientsatisfaction with mandibular prostheses. Commu-nity Dentistry and Oral Epidemiology, 26, 400–405.
Awad, M. A., Locker, D., Korner-Bitensky, N., &Feine J. S. (2000). Measuring the effect of intra-oral implant rehabilitation on the health-relatedquality of life in a randomized controlled clinicaltrial. Journal of Dental Research, 79, 1659–1663.
Awad, M. A., Lund, J. P., Dufresne, E., & Feine,J. S. (2003). Comparing the efficacy of mandibularimplant-retained overdentures and conventional

PATIENT PREFERENCES AND EXPECTATIONS 7
dentures among middle-aged edentulous patients:Satisfaction and functional assessment. Interna-tional Journal of Prosthodontics, 16, 117–122.
Awad, M. A., Lund, L. P., Shapiro, S. H., et al.(2003). Oral health status and treatment satisfac-tion with mandibular implant overdentures andconventional dentures. A randomized clinical trialin a senior population. International Journal ofProsthodontics, 4, 390–396.
Axelsson, G. & Helgadottir, S. (1995). Edentulous-ness in Iceland in 1990. A national questionnairesurvey. Acta Odontologica Scandinavica, 53, 279–282.
Axelsson, P., Paulander, J., & Lindhe, J. (1998). Re-lationship between smoking and dental status in35-, 50-, 65-, and 75-year-old individuals. Journalof Clinical Periodontology, 25, 297–305.
Batenburg, R. H. K., van Oort, R. P., Reintsema, H.,Brouwer, T. T., Raghoebar, G. M., & Boering, G.(1998). Mandibular overdentures supported bytwo Branemark, IMZ, or ITI implants. A prospec-tive comparative preliminary study: One-year re-sults. Clinical Oral Implants Research, 9, 374–383.
Berg E. (1984) The influence of some anamnestic, de-mographic, and clinical variables on patient accep-tance of new complete dentures. Acta Odontolog-ica Scandinavica, 42, 119–127.
Bergendal, T., & Engquist, B. (1998). Implant-supported overdentures: A longitudinal prospec-tive study. International Journal of Oral & Max-illofacial Implants, 13, 253–262.
Bergman, B. & Carlsson, G. E. (1972). Review of54 complete denture wearers. Patient’s opinions1 year after treatment. Acta Odontologica Scandi-navica, 30, 399–414.
Boerrigter, E. M., Geertman, M. E., Van Oort, R. P.,et al. (1995). Patient satisfaction with implant-retained mandibular overdentures. A compari-son with new complete dentures not retained byimplants—a multicentre randomized clinical trial.British Journal of Oral & Maxillofacial Surgery,33, 282–288.
Boerrigter, E. M., Stegenga, B., Raghoebar, G. M.,& Boering, G. (1995). Patient satisfaction andchewing ability with implant-retained mandibularoverdentures: A comparison with new completedentures with or without preprosthetic surgery.Journal of Oral and Maxillofacial Surgery, 53,1167–1173.
Bosker, H. & van Dijk, L. (1989) The transmandibu-lar implant: a 12-year follow-up study. Journal ofOral and Maxillofacial Surgery, 47, 442–450.
Bouma, J., Boerrigter, L. M., Van Oort, R. P., vanSonderen, E., & Boering, G. (1997). Psychosocialeffects of implant-retained overdentures. Interna-tional Journal of Oral & Maxillofacial Implants,12, 515–522.
Bouma, J., Uitenbroek, D., Westert, G., Schaub,R. M., & van de Poel, F. (1987). Pathways to fullmouth extraction. Community Dentistry and OralEpidemiology, 15, 301–305.
Bouma, J., van de Poel, F., Schaub, R. M., & Uiten-broek, D. (1986). Differences in total tooth ex-traction between an urban and a rural area in theNetherlands. Community Dentistry and Oral Epi-demiology, 14, 181–183.
Brodeur, J. M., Benigeri, M., Naccache, H., OlivierM., & Payette, M. (1996). Trends in the level ofedentulism in Quebec between 1980 and 1993 [inFrench]. Journal of the Canadian Dental Associa-tion 62, 159–160, 162–166.
Budtz-Jorgensen, E. “Epidemiology: Dental and Pros-thetic Status of Older Adults.” Chapter 1 inProsthodontics for the Elderly: Diagnosis andTreatment. Chicago: Quintessence Publishing,1999.
Burns, D. R., Unger, J. W., Elswick, R. K. Jr.,& Giglio, J. A. (1995). Prospective clinicalevaluation of mandibular implant overdentures:Part I: Retention, stability and tissue response.The Journal of Prosthetic Dentistry, 73, 354–363.
Carlsson, G. E., Otterland, A., & Wennstrom, A.(1967). Patient factors in appreciation of completedentures. Journal of Prosthetic Dentistry, 17, 322–328.
Centers for Disease Control and Prevention. (1999).Total tooth loss among persons aged > or =65 years–Selected states, 1995–1997. MMWRMorbidity and Mortality Weekly Report, 48, 206–210.
Cune, M. S. “Overdentures on Dental Implants.”(thesis, Utrecht, the Netherlands University ofUtrecht, 1993).
Davis, D. M., Rogers, J. O., & Packer, M. E. (1996).The extent of maintenance required by implant-retained mandibular overdentures: A 3-year re-port. International Journal of Oral & Maxillofa-cial Implants, 11, 767–774.
Dolan, T. A., Gilbert, G. H., Duncan, R. P., & Roer-ster, U. (2001) Risk indicators of edentulism, par-tial tooth loss and prosthetic status among blackand white middle-aged and older adults. Commu-nity Dentistry and Oral Epidemiology, 29, 329–340.