Classification adjustments (For funding models)
description
Transcript of Classification adjustments (For funding models)

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Ric Marshall
Thursday, 8th December 2011
10.00-10.45am
Classification adjustments (For funding models)

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
DRG classifications around the world

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
• for resource homogeneity and clinical meaningfulness
• To compensate for “classification failure”– The classification may not be able to measure
the selection by one hospital of particular types of cases
• Alternatively use additional flag for a price adjustment – eg use of ventilation, Dx – OR peer hospital flag.
Refinement of classes

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Adjusting for classification limitations

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
• outliers and exceptional cases.• Many systems use outliers or exceptional case
adjustments • Well documented example is Victoria.• Critics call it “tinkering” or interfering with the
signals from the payment mechanism.• Others say that it adds precisions and fairness
to the payment system.• WHO IS RIGHT?
Extra categories in Funding model

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
• Substitution and different models of care
• When does the care type change?
• What is the optimum?
• What is the norm?
Outpatient and sub-acute caseload and DRGs

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
• IMPORTANT FOR CONSISTENT DATA
• ‘APPLES WITH APPLES’
Admission and discharge policies

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
• Particularly important where substitution with inpatient services can occur eg– Work up for a surgical admission– The rehabilitation phase of a joint
replacement– Or even complete episodes
• Payment neutral incentives
• Guidelines and clear definitions of payment rules
Outpatient activity management tools

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
• MODELLING, MODELLING, MODELLING
Simulation of adjustments for funding precision

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
• The need to keep classes to manageable numbers
• Approaches to specifying outliers.
Outlier policies or classification changes

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Clear Description of Costs
• Different health systems fund different activities eg – private providers usually include capital costs
through depreciation, while public providers often have a separate funding mechanism
– some systems exclude (or “unbundle”) some highly variable/high cost components of care, like intensive care or prostheses
• The contracted prices should match the appropriate costs– This might not happen if you adopt other countries
’ costs (eg no blood costs in Australian data).

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Specifying Contract Prices
Usually:
• Relative Value Score (Cost Weight) × Unit Price• Cost weights are derived empirically from
hospital Data• The unit price is negotiated
- ideally all hospitals would have same unit price.- the unit price can be modified to reflect:-
- differences in cost between groups of hospitals- efficiencies of scale (eg Victoria)
- transition arrangements ie “blend” the desired unit price with the hospital’s average cost (as in the Irish
Model and the private sector in Australia).

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Other Hospital Products
• DRGs are only designed to describe acute admitted hospital episodes
• Different classifications are needed for other hospital services:– Outpatients– Long stay care– Health promotion activities– etc

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
How good are DRGs
• Typically DRGs explain about 25%-40% of the variation in the costs of treating patients.
• Hospitals don’t get a random sample of patients. Referral patterns and role delineation means that some hospitals treat sicker patients.
• Most systems have rules that provide extra payments so hospitals aren’t disadvantaged (ie share financial risk).
• With appropriate risk mitigation, funding models can explain over 80% of the variation in cost.

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Rules to moderate financial risk
• Financial risk moderation for individual patients through outlier policy
• Same day policy
• Severity co-payments for specific subgroups within DRGs
• Grants
• High cost patient “adjustment funding pools”

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
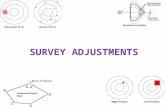
Outlier Policy
Frequency
Length of stay (days)
Average LOS
Low Boundary
High Boundary
Paid below the standard rate
Paid the standard rate
Paid above the standard rate
High Outliers
Low Outliers
Adjustments are made to the “average” rate for patients that stay in hospital for fewer days than or more days than the pre-defined times for each DRG

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
General Casemix Model
Funds (red)
Days in Hospital
Low Inlier Boundary
Total $ Cost (green)
High Inlier Boundary

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Same Day Policy
– Differences between the costs of DRGs in different hospitals can be due to differences in the proportions of same day cases. This can be due to:-
• Different types of cases in the DRG (COMPLEXITY)• Differences in admission/discharge policy (eg admitting rather than
treating on an outpatient basis.• Hospital clinical practice• Efficiency
– Setting separate same day payment rate within a DRG can be used to prevent hospitals with mostly overnight patients being inappropriately disadvantaged.
– Same day payment rates are not always a good idea because they can discourage hospitals from moving to same day care where appropriate – CLINICAL JUDGEMENT IS REQUIRED.

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Co-payments for specific subgroups within DRGs
• Sometimes it is possible to identify subgroups within a DRG that cost more than the average. In these cases additional payments can be made.
• Co-payments are best used where groups of patients have higher than average cost in many DRGs. eg in Victoria– Mechanical ventilated patients– Native Australians
• Using too many copayments reverts back to input based funding.

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Grants or ‘Block funding’
• Higher costs for some hospitals can be:– difficult to quantify (eg teaching hospital costs) or – not directly related to activity (eg running an
emergency department; the department must be kept open regardless of the level of activity)
• In such cases cash grants are often paid to hospitals in addition to activity based funding.
• Such grants are often easier to use in a public system than in a private system.

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Adjustment Funding Pools• A set budget is put aside for allocating additional
funding for specific patients based upon applications from hospitals
• Example 1: New Technology in Victoria– AU$3million is set aside and hospitals apply for funding specific
technologies in small numbers of patients
• Example 2: High Cost Patient Pool in Western Australia– Approximately 20% of total hospital costs are required to treat
the most expensive 5% of patients. These patients are difficult to fund under the casemix “averaging” approach. In WA hospitals are able to apply for additional funding for individual patients, but patients’ records are independently clinically reviewed and payment approved by an industry committee.

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Risk Moderation While in Transition
• When new activity based funding models are introduced not all hospitals are equally affected- some win and others lose.
• It is important to protect hospitals from extreme budgetary changes until they have time to adjust to the new funding model (ie find efficiencies).
• This is usually done by introducing “transition” grants or differential unit prices in the first few years.

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Types of Casemix Models• Casemix was initially developed as a prospective payment
mechanism (ie this year’s activity determines this year’s funding). – This approach is still widely used (eg USA Medicare, Victoria
public hospitals and within the Private sector).
• Prospective payment increases the incentives to achieve technical efficiency but reduces budgetary certainty for hospitals.
• Casemix can also be used as a retrospective payment mechanism (ie last year’s activity determines this year’s funding). – This form of model is used in Ireland and New South Wales.
• Typically, in retrospective casemix models this year’s budget is set based upon last year’s budget plus growth.

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Limiting the total amount of activity
• Experience suggests that health expenditure is extremely elastic and the potential to spend money on health care almost certainly exceeds any system’s capacity to pay for that care.
• Most systems attempt to limit the amount of activity funded by:– setting activity caps (ie only funding activity to a
certain level) or– excluding funding for some health care
intervention (eg cosmetic surgery) or– introducing patient contributions

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Variations around activity Targets
• Hospitals cannot exactly identify how many people will be admitted
• Funding models can be designed to accommodate this uncertainty by funding activity above target activity at a marginal rate and reducing funding at a marginal rate for hospitals failing to achieve target.

Serbia Health Project – Additional Financing Training for Trainers on AR-DRG, 05-09.12.2011
Република СрбијаМИНИСТАРСТВО ЗДРАВЉА
Other Components of a successful casemix policy
• In the previous slides we have described the technical issues in developing a successful casemix policy.
• Non-technical issues are equally important:-– Openness and transparency– Fairness– Stakeholders involved– Formal channels of review– Willingness to listen and change