Circulatory Physiology AnS 536 Spring 2015. Development of the Circulatory System 1st functional...
-
Upload
ross-johnson -
Category
Documents
-
view
214 -
download
0
Transcript of Circulatory Physiology AnS 536 Spring 2015. Development of the Circulatory System 1st functional...
Development of the Development of the Circulatory SystemCirculatory System
1st functional organ system – heart is 1st functional organ system – heart is functional when embryo is 2 mm in sizefunctional when embryo is 2 mm in size
Heart rate peaks at 9 weeks, and slows Heart rate peaks at 9 weeks, and slows to ~145 beats at termto ~145 beats at term
Huge increase in cardiac output Huge increase in cardiac output postnatally but limited ability to postnatally but limited ability to increase further increase further – Increase in thyroid hormone prenatally Increase in thyroid hormone prenatally
matures myocardium in preparation for matures myocardium in preparation for increased postnatal requirementsincreased postnatal requirements
Development of the Development of the Circulatory SystemCirculatory System
The heart functions partly in parallel and The heart functions partly in parallel and dominated by right ventricular functiondominated by right ventricular function
Parallel function allows the shunts to be Parallel function allows the shunts to be more effective and the foramen ovale to more effective and the foramen ovale to not compromise cardiac outputnot compromise cardiac output
Heart functions in series postnatally with Heart functions in series postnatally with equal ventricular function equal ventricular function
Blood volume ~11% in fetus (7.5% in Blood volume ~11% in fetus (7.5% in adults) because of amount of placental adults) because of amount of placental bloodblood
VIDEO BREAKVIDEO BREAK
http://www.youtube.com/watch?http://www.youtube.com/watch?v=K4B5fFQ8OGw&feature=player_detv=K4B5fFQ8OGw&feature=player_detailpageailpage
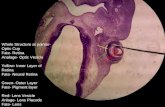
The Fetal Circulatory SystemThe Fetal Circulatory System
Pathways of the fetal heart and representative oxygen saturation values (in numbers). The via sinistra (red) directs well oxygenated blood from the umbilical vein (UV) through the ductus venosus (DV) (or left half of the liver) across the inferior vena cava (IVC), through the foramen ovale (FO), left atrium (LA) and ventricle (LV) and up the ascending aorta (AO) to join the via dextra (blue) in the descending AO. Deoxygenated blood from the superior vena cava (SVC) and IVC forms the via dextra through the right atrium (RA) and ventricle (RV), pulmonary trunk (PA) and ductus arteriosus (DA). The isthmus aortae (arrow) and the section of the left portal vein between the main stem (P) and the DV (striped area) represent watershed areas during hemodynamic compromise. CCA, common carotid arteries; FOV, foramen ovale valve; LHV, left hepatic vein; MHV, medial hepatic vein; PV, pulmonary vein; RHV, right hepatic vein
Fetal Circulatory ShuntsFetal Circulatory Shunts Foramen ovaleForamen ovale
– Shunts blood from the Shunts blood from the right atrium to the left right atrium to the left atriumatrium
Ductus arteriosusDuctus arteriosus– Shunts blood from the Shunts blood from the
pulmonary artery to the pulmonary artery to the ascending aortaascending aorta
– Bypasses pulmonary Bypasses pulmonary circulationcirculation
Ductus venosusDuctus venosus– Shunts blood from the Shunts blood from the
umbilical vein to the umbilical vein to the inferior vena cavainferior vena cava
– Separates the hepatoportal Separates the hepatoportal and systemic circulationand systemic circulation
PhysiologyPhysiology– Fetal blood passes from the Fetal blood passes from the
placenta placenta umbilical vein umbilical vein fetal heartfetal heart
– Left ventricle shunts blood to Left ventricle shunts blood to the craniumthe cranium
Advantages of shuntsAdvantages of shunts– Bypasses normal “flow Bypasses normal “flow
patterns” to allow most patterns” to allow most oxygenated blood (left oxygenated blood (left ventricle) to reach the fetal ventricle) to reach the fetal brainbrain
– Unsaturated blood (from the Unsaturated blood (from the right ventricle) is diverted to right ventricle) is diverted to the trunk and lower body of the trunk and lower body of the fetusthe fetus
Oxygen Tension LevelsOxygen Tension Levels
Blood coming from the placenta (umbilical veins) Blood coming from the placenta (umbilical veins) is 80% saturated with oxygenis 80% saturated with oxygen
Enters right atrium via inferior vena cavaEnters right atrium via inferior vena cava– Half of venous return bypasses portal circulation via Half of venous return bypasses portal circulation via
ductus venosusductus venosus– Because ductus venosus has small diameter, blood Because ductus venosus has small diameter, blood
accelerates and is more likely to push though foramen accelerates and is more likely to push though foramen ovale into left atrium and to “upper circulation”ovale into left atrium and to “upper circulation”
From right atrium to left atrium via foramen ovale From right atrium to left atrium via foramen ovale (now 65% saturated)(now 65% saturated)– Pumped to carotid artery and to brain (most oxygen Pumped to carotid artery and to brain (most oxygen
rich blood)rich blood)
Foramen OvaleForamen OvaleFlow distribution at the foramen Flow distribution at the foramen ovale. The edge of the atrial ovale. The edge of the atrial septum (crista dividens) divides the septum (crista dividens) divides the ascending flow in two arms, to the ascending flow in two arms, to the right and left atrium (RA and LA). right and left atrium (RA and LA). The horizontal diameter between The horizontal diameter between the foramen ovale valve and the the foramen ovale valve and the atrium (broken line) represents the atrium (broken line) represents the restricting area into the LA. restricting area into the LA. Position, direction and kinetic Position, direction and kinetic energy of the flow from the ductus energy of the flow from the ductus venosus makes it predominantly venosus makes it predominantly enter the left atrium (dark gray). enter the left atrium (dark gray). Conversely, blood from the inferior Conversely, blood from the inferior vena cava (IVC) enters the RA (light vena cava (IVC) enters the RA (light gray). Ao, aorta; PA, pulmonary gray). Ao, aorta; PA, pulmonary trunk; PV, stem of the portal vein trunk; PV, stem of the portal vein (From Kiserud and Rasmussen, (From Kiserud and Rasmussen, 2001)2001)
Oxygen Tension LevelsOxygen Tension Levels
Blood coming from the superior vena cava Blood coming from the superior vena cava is directed primarily through tricuspid is directed primarily through tricuspid valve into right ventricle (50% saturated valve into right ventricle (50% saturated with oxygen)with oxygen)
Enters aorta, provides lower levels of Enters aorta, provides lower levels of oxygen to caudal half of body and then oxygen to caudal half of body and then enters the umbilical arteries to be re-enters the umbilical arteries to be re-oxygenated in the placentaoxygenated in the placenta– Once oxygenated, returns to body as fully Once oxygenated, returns to body as fully
oxygenated blood via umbilical veins oxygenated blood via umbilical veins
Ductus ArteriosusDuctus Arteriosus Factors involved in closureFactors involved in closure
– PGEPGE2 2 helps maintain patency and nitic oxide helps maintain patency and nitic oxide will cause relaxation (indomethacin will will cause relaxation (indomethacin will induce closure anytime during latter half of induce closure anytime during latter half of third trimester through postnatal life)third trimester through postnatal life)
– Increased POIncreased PO22 of arterial blood postnatally of arterial blood postnatally causes spasms of the ductuscauses spasms of the ductus
– Fetus has low-resistance circulation from the Fetus has low-resistance circulation from the placenta during gestationplacenta during gestation Parturition, umbilical cord rupture, and initiation of Parturition, umbilical cord rupture, and initiation of
respiration increase resistancerespiration increase resistance
Ductus ArteriosusDuctus Arteriosus
Physiological changesPhysiological changes– Lungs become the organ of respirationLungs become the organ of respiration– Oxygen tension increasesOxygen tension increases– Right ventricular outflow passes into the Right ventricular outflow passes into the
lungs instead of the ductus lungs instead of the ductus – Ductus constriction begins shortly after Ductus constriction begins shortly after
birthbirth– Closure occurs 24-48 hours after birthClosure occurs 24-48 hours after birth
Ductus VenosusDuctus Venosus Factors involved in closureFactors involved in closure
– Liver pressure and resistanceLiver pressure and resistance– Gestational age Gestational age
and weight at birthand weight at birth Premature neonates will have Premature neonates will have
delayed closuredelayed closure
– DrugsDrugs Promote closurePromote closure
– Antenatal corticosteroidsAntenatal corticosteroids Delay closureDelay closure
– Prostaglandins and nitroxide Prostaglandins and nitroxide distend diameter of ductusdistend diameter of ductus
VIDEO BREAKVIDEO BREAK
http://www.youtube.com/watch?http://www.youtube.com/watch?v=SUP1K4gPw4s&feature=player_detav=SUP1K4gPw4s&feature=player_detailpageilpage
Ductus VenosusDuctus Venosus Physiologic changesPhysiologic changes
– Functional closure initially after Functional closure initially after birthbirth
– Umbilical vein constricts reducing Umbilical vein constricts reducing supply of shunted bloodsupply of shunted blood
Ductus venosus becomes Ductus venosus becomes ligamentum venosumligamentum venosum
Blood enters liver through Blood enters liver through hepatic sinuoidshepatic sinuoids
Foramen OvaleForamen Ovale Factors contributing to closureFactors contributing to closure
– Pulmonary and vascular Pulmonary and vascular resistance increaseresistance increase
Physiological changesPhysiological changes– Increased quantity of blood into the left Increased quantity of blood into the left
atriumatrium– Causes left atrial pressure to rise above that Causes left atrial pressure to rise above that
in the right atriumin the right atrium– Closes the flap of this one-way valve Closes the flap of this one-way valve
preventing blood flow across the septumpreventing blood flow across the septum Anatomical closure takes months or yearsAnatomical closure takes months or years
VIDEO BREAKVIDEO BREAK
http://www.youtube.com/watch?http://www.youtube.com/watch?v=wsDwQw1JjTU&feature=player_detav=wsDwQw1JjTU&feature=player_detailpageilpage
http://www.youtube.com/watch?http://www.youtube.com/watch?v=ZOtk_FSfHpw&feature=player_detaiv=ZOtk_FSfHpw&feature=player_detailpagelpage
Persistent (Patent) Persistent (Patent) Ductus ArteriosusDuctus Arteriosus
Failure of closure of the vessel that joins the Failure of closure of the vessel that joins the pulmonary artery to the aortapulmonary artery to the aorta
EffectsEffects– Depend on size of shunt and degree of Depend on size of shunt and degree of
pulmonary hypertensionpulmonary hypertension Small to moderate shuntsSmall to moderate shunts
– Easy to fatigue, dyspnea on exertion and exercise Easy to fatigue, dyspnea on exertion and exercise intolerance intolerance later in lifelater in life
Large shuntsLarge shunts– Poor growth and developmentPoor growth and development– Frequent episodes of pneumonitis and development of Frequent episodes of pneumonitis and development of
congestive heart failurecongestive heart failure– Life expectancy is markedly reduced – these individuals Life expectancy is markedly reduced – these individuals
often die in their second or third decadeoften die in their second or third decade
Persistent (Patent) Persistent (Patent) Ductus ArteriosusDuctus Arteriosus
Potential causesPotential causes– Hypoxia and acidosis will increase pulmonary vascular Hypoxia and acidosis will increase pulmonary vascular
resistance and increase right-to-left shuntingresistance and increase right-to-left shunting– Higher incidence when infants are born at high Higher incidence when infants are born at high
altitudes (>10,000 ft)altitudes (>10,000 ft)– Twice as common in females vs. malesTwice as common in females vs. males– Frequency increased in preterm infantsFrequency increased in preterm infants
Fail to close spontaneouslyFail to close spontaneously Closure induced with cyclooxygenase inhibiting drugs in Closure induced with cyclooxygenase inhibiting drugs in
premature babies ONLYpremature babies ONLY– COX-1 and COX-2 are enzymes in arachidonic acid metabolism COX-1 and COX-2 are enzymes in arachidonic acid metabolism
producing producing prostaglandins, prostacyclins and producing producing prostaglandins, prostacyclins and thromboxanesthromboxanes
– COX inhibitors are NSAIDCOX inhibitors are NSAIDSS (ibuprofen or indomethacin) (ibuprofen or indomethacin)
VIDEO BREAKVIDEO BREAK
http://www.youtube.com/watch?http://www.youtube.com/watch?v=g_zQEQBLv_g&feature=player_detaiv=g_zQEQBLv_g&feature=player_detailpagelpage
Persistent Pulmonary Persistent Pulmonary HypertensionHypertension
Occurs when pulmonary vascular Occurs when pulmonary vascular resistance fails to decreaseresistance fails to decrease
TreatmentsTreatments– Mechanical hyperventilationMechanical hyperventilation– Inhaled nitric oxideInhaled nitric oxide– VentilationVentilation– Extracorporeal membrane oxygenation Extracorporeal membrane oxygenation
(ECMO)(ECMO)– Free radical scavengers (SOD)Free radical scavengers (SOD)
Persistent Pulmonary Persistent Pulmonary HypertensionHypertension
Mechanical Mechanical hyperventilationhyperventilation– Results in alkalosisResults in alkalosis
Improves condition as Improves condition as systemic pH rises over systemic pH rises over 7.55 to 7.67.55 to 7.6
– Problems can occur if Problems can occur if too vigorous or too vigorous or sustained too long sustained too long
Inhaled nitric oxideInhaled nitric oxide– Mimics Mimics
endothelium-endothelium-derived relaxing derived relaxing factorfactor Promotes pulmonary Promotes pulmonary
vasodilatationvasodilatation Poorly sustained Poorly sustained
response in most response in most infantsinfants
Persistent Pulmonary Persistent Pulmonary HypertensionHypertension
VentilationVentilation– High oscillatory High oscillatory – Effective with severe Effective with severe
associated lung diseaseassociated lung disease
ECMOECMO– Infants placed on Infants placed on
blood bypass pumpblood bypass pump– Blood exits the right atrium Blood exits the right atrium
passes through a membrane passes through a membrane oxygenator and returns to oxygenator and returns to the aortic archthe aortic arch
– Lungs are essentially at restLungs are essentially at rest– When hypertension improves When hypertension improves
– infants are weaned off– infants are weaned off ProblemsProblems
– Used as a last resortUsed as a last resort– Neurodevelopmental Neurodevelopmental
disorders can occurdisorders can occur
Umbilical Vessel ConstrictionUmbilical Vessel Constriction
Factors involvedFactors involved– ChemicalChemical
BradykininsBradykinins EpinephrineEpinephrine SeratoninSeratonin
– MechanicalMechanical Increase in POIncrease in PO22
– HumoralHumoral ThromboxaneThromboxane HistamineHistamine
If constriction does If constriction does not occurnot occur– Persistent bleeding Persistent bleeding
leading to leading to hemorrhage and hemorrhage and severe blood losssevere blood loss
– Potential for Potential for infectioninfection
– Surgical Surgical intervention may be intervention may be neededneeded
Placental TransfusionPlacental Transfusion
Transfer of blood from Transfer of blood from the placenta to the the placenta to the fetus at birthfetus at birth
Dependent upon Dependent upon timing of umbilical timing of umbilical clamping clamping (1-5 minutes) after (1-5 minutes) after birthbirth
Late clampingLate clamping– Increases blood volume Increases blood volume
and RBC’s of neonate and RBC’s of neonate (20-50%)(20-50%)
– Can increase bilirubin Can increase bilirubin concentrationsconcentrations
Early clampingEarly clamping– Decreases blood volume Decreases blood volume
anemia anemia FoalsFoals
– Early clamping leads to Early clamping leads to barker syndrome, barker syndrome, temporary blindness, and temporary blindness, and dummy foal syndromedummy foal syndrome
– Increased frequency of Increased frequency of deathdeath