CIBASPAIN All corrections.doc
Transcript of CIBASPAIN All corrections.doc

Anales de psicologia (1999 in press).
With permission of editor, this paper is an updated reprint of an article that appeared in
Contemporary Hypnosis, 1998, 15, 22-33.
La naturaleza de la analgesia hipnótica: bases y evidencias neurofisiológicas
Helen J. Crawford, Ph.D.
Department of Psychology
Virginia Polytechnic Institute and State University
Blacksburg, Virginia 24061-0436
e-mail: hjc @ vt.edu phone: 504 231-6520
Timothy Knebel, Ph.D.
Department of Psychology
Virginia Polytechnic Institute and State University
Blacksburg, Virginia 24061-0436
Jennifer M. C. Vendemia
Department of Psychology
Virginia Polytechnic Institute and State University
Blacksburg, Virginia 24061-0436
James E. Horton
Department of Psychology
University of Virginia’s College at Wise
Wise, Virginia 24293-0016
Virginia Polytechnic Institute and State University
Blacksburg, Virginia 24061-0436
Key Words: Hypnosis, Hypnotic Analgesia, Pain, Somatosensory Evoked Potentials,
Electroencephalogram, Cerebral Blood Flow

Abstract
This paper reviews neurophysiological research (EEG, event-related potential,
cerebral blood flow, functional Magnetic Resonance Imaging, and neurochemical) that
supports the proposal that hypnotic analgesia is an active inhibitory process involving
several brain systems mediating attentional and nociceptive processes. Even though the
processes of hypnotic analgesia may be dissociated from conscious awareness and appear
to be beyond volitional control, it is proposed that hypnotic analgesia depends on the
activation of a supervisory, attention control system -- involving the anterior frontal
cortex -- which then participates with other cortical and subcortical systems in the
allocation of thalamocortical activities. Hypnotic analgesia affects the active allocation
of attention and disattention associated with the anterior frontal region, as well as spatio-
temporal aspects pain perception associated with the posterior cortical systems.

The Nature of Hypnotic Analgesia:
Neurophysiological Foundation and Evidence
Hypnosis is one of the best documented behavioral interventions for controlling
acute and chronic pain in adults and children (for reviews, see Barber, 1996; Barber &
Adrian, 1982; Chaves, 1989, 1994; Crawford, 1994a,b; 1995, in press; Evans, 1988;
Gibson, 1994; E. R. Hilgard & J. R. Hilgard, 1994; J. R. Hilgard & LeBaron, 1984;
Holroyd, 1996; Olness & Gardner, 1988). Hypnotically suggested analgesia involves
techniques of distraction, redefinition and dissociation to reduce or eliminate the
perception of pain. The positive correlation between standardized hypnotic susceptibility
test scores and degree of reduced pain obtained following hypnotically suggested
analgesia is significant, usually around 0.5. Low hypnotizable persons (“lows”) can
reduce the distress of accompanying pain due probably to the relaxation component of
hypnosis. Whereas, moderately to highly (“highs”) hypnotizable persons are more likely
to reduce -- and even eliminate -- both the distress and the sensory dimensions of pain
due to relaxation and attentional/disattentional (inhibitory) processes (Crawford, 1994a,b;
Hilgard & Hilgard, 1994). Further acceptance of hypnotic analgesia as an early
intervention, in conjunction with other medical interventions, for the treatment of acute
as well as chronic pain may occur by an understanding of its neurophysiological
underpinnings.
The purpose of the present paper is to review what we now know about the
neurophysiological bases of hypnotic analgesia as moderated by hypnotic susceptibility
level. It is placed within an evolving model that proposes (a) hypnotic analgesia depends
upon the activation of a supervisory, attention control system that suppresses incoming

painful stimuli at cortical and subcortical levels and thereby prevents them from reaching
conscious awareness, and (b) highly hypnotizable persons can better control pain because
of their more effective frontal attentional system that permits them to either attend to or
disattend incoming stimuli (for reviews, see Crawford, 1994a,b; in press; Crawford &
Gruzelier, 1992, Gruzelier, 1998). This paper may be considered a midstream report,
much like Crawford and Gruzelier’s (1992) general review on the
neuropsychophysiology of hypnosis.
Neurophysiology of Pain
Pain is a dynamic, multifaceted experience involving sensory-discriminative,
motivational-affective, cognitive and motoric dimensions (e.g., Melzack,, 1992; Melzack
& Casey, 1968; Melzack & Wall, 1965; Price, 1988). Neuroimaging studies support the
view that any sensory event engages an extensive network of brain systems working both
sequentially and in parallel (Posner & Raichle, 1994). Pain is no exception. The
physical significance, intensity, duration, somatic involvement, location, and overall
unpleasantness of pain is profoundly influenced by a complex array of environmental,
social, emotional and situational variables synthesized through neural activation of
cortical and subcortical systems (Chandler & Dong, 1995).
During the administration of experimental pain, activation of various regions of the
brain reflect processing of different aspects of pain (for review, see Treede, Kenshalo,
Gracely, & Jones, 1999). These may include primary (S1) and secondary (S2)
somatosensory cortex (e.g., Downs, et al., 1998; Howland, Wakai, Mjaanes, Balog, &
Cleeland, 1995), thalamus (e.g., Craig, 1998; Craig, Bushnell, Shang, & Blomqvist,
1994), insula (e.g., Downs et al., 1998), anterior cingulate cortex (e.g., Davis, Wood,

Crawley, & Mikulis, 1995; Devinsky, Morrell, & Vogt, 1995; Downs, et al., 1998;
Hutchison, Davis, Lozano, Tasker, & Dostrovsky, 1999; Jones, Brown, Friston, Qi, &
Frackowiak, 1991; Sweet, 1995; Talbot, Marrett, Evans, Meyer, Bushnell, & Duncan,
1991), basal ganglia (Chundler & Dong, 1995), and anterior frontal cortex (e.g., Bromm
& Chen, 1995; Derbyshire, Chen, & Jones, 1996; Derbyshire et al., 1994; Downs, et al.,
1998). These many discrete brain regions have been identified as subserving four main
functions: “sensation-perception (primary somatosensory cortex, thalamus and insula);
attention (anterior cingulate cortex); descending pain control (periaqueductal grey); and
an extensive network related to sensory-motor integration (supplementary motor cortex,
bilateral putamen and insula, anterior lobe and vermis of the cerebellum and superior
colliculus)” (Iadarola et al., 1998, p. 931 ). Recently, Ploghaus et al. (1999) showed that
the expectation of pain activates sites that are “distinct from, but close to, locations
mediating pain experience itself” (p. 1979).
There are several descending inhibitory systems that modulate sensory input,
including higher centers (e.g., anterior frontal cortex), the midbrain (e.g., hypothalamus),
the periaqueductal gray area (Depaulis & Bandler, 1991; Franzén & Ahlquist, 1996), and
the spinal cord (for review, see Markenson, 1996). Phylogenetically speaking, regions of
the anterior frontal cortex are relatively recent, and in humans these regions have been
widely associated with programming and regulating behavior including attention and
inhibitory processes (e.g., Luria, 1966; Norman & Shallice, 1986; Pribram, 1991; Stuss,
Shallice, T., Alexander, M. P., & Picton, 1995). Since hypnotic analgesia is attention-
based, we would anticipate the interactive involvement of attentional systems, inhibitory
processes, and multiple pain systems of the brain

Neurophysiology of Hypnotic Analgesia
The search for neurophysiological markers or changes during hypnotic analgesia has
occurred for the past 30-40 years. The 1990’s “Decade of the Brain” has brought new,
sophisticated techniques and theories that are now being applied to the study of pain
processing and the manipulation of attentional and pain processes through hypnotic
analgesia. New technologies available to researchers include electroencephalographic
(EEG) frequency analysis, EEG topographic brain mapping, somatosensory event-related
potential (SERP) topographic brain mapping, positron emission tomography (PET),
regional cerebral blood flow (rCBF), single photon emission computed tomography
(SPECT), and functional Magnetic Resonance Imaging (fMRI).
As this research becomes more interdisciplinary in nature, researchers must continue
to be vigilant to ensure that they incorporate adequate research designs developed within
the field of hypnosis (Barabasz & Barabasz, 1992; Crawford & Gruzelier, 1992; Hilgard,
1965). It is imperative to use participants who have been well-screened and categorized
using standardized hypnotic susceptibility scales, and adequate comparisons of attention
to the pain (“attend”) and hypnotic analgesia conditions that are counterbalanced or
placed within an A-B-A design. The studying of Aptitude (trait) X Treatment
interactions, through a combination of experimental and correlational methods (Crawford
& Allen, 1983; Cronbach; 1975; Tellegen, 1981) is crucial in hypnosis research.
Hypnotic susceptibility level is important to evaluate since it appears that highly
hypnotizable persons can better control pain because of their more effective frontal
attentional system that permits them to either attend to or disattend incoming stimuli
(e.g., Crawford, Brown, & Moon, 1993; Crawford, Knebel et al., 1998; Spiegel, Bierre &

Rootenberg, 1989; Zachriae & Bjerring, 1994; for reviews, see Crawford, 1994a,b; in
press; Crawford & Gruzelier, 1992; Crawford, Horton, McClain-Furmanski, &
Vendemia, 1998). Comparisons between low and highly hypnotizable persons is crucial
to sort out the effects of hypnotic analgesia per se from more general relaxation and other
effects. The highly hypnotizable person should be screened for inclusion based upon
previously demonstrated abilities to greatly reduce or eliminate the perception of distress
and sensory pain.
Anterior frontal (prefrontal) cortex activation may occur during painful stimulation
(Crawford, Horton et al., 1998; Crawford, Horton, McClain-Furmanski et al., Downs et
al., 1998; Iadorola et al., 1998) and/or the anticipation of pain (Ploghaus et al., 1999).
Thus, we propose it is also involved, in cooperation with subcortical regions including
the thalamus, in the gating or inhibiting of somatosensory input when hypnotic analgesia
is employed. The anterior frontal cortex is activated during directed attention and
inhibition (e.g., Posner & Petersen, 1990). It also operates at early stages of sensory
processing on cortical and subcortical structures, from “the periphery through dorsal
column nuclei and thalamus to the sensory cortex” (Yamaguchi & Knight, 1990, p. 281).
Surprisingly, on-going chronic pain may actually disrupt anterior frontal activation
(Derbyshire et al., 1994, 1996). If that is the case, then hypnotic analgesia techniques
may activate inhibitory processing of the anterior frontal cortex and thereby result in the
downward inhibition of incoming pain and pain memories.
Recent studies of cerebral blood flow and brain wave electrical activity (EEG and
somatosensory event-related potentials at surface and subcortical region recording sites)
support the proposal that the anterior frontal attention system is, through interaction with

other cortical and subcortical regions, actively involved in suppressing incoming
information about noxious stimuli during hypnotic analgesia. These studies will now be
reviewed.
Neuroimaging Research
Changes in rCBF metabolism, as measured by the 133-xenon method, accompanying
rest, ischemic pain without suggested analgesia, and ischemic pain with suggested
analgesia conditions in sessions with and without hypnosis were investigated by
Crawford, Gur, Skolnick, Gur and Benson (1993). Participants were healthy young men:
six were very low in hypnotizability (as measured by three standardized scales of
hypnotic susceptibility) and five were very high in hypnotizability. Training in applying
techniques of hypnotic analgesia to both cold pressor pain and ischemic pain preceded
the rCBF study. Highs who participated consistently eliminated all pain perception in
these training sessions. No rCBF differences were observed during waking, but
following a hypnotic induction only the highs showed a dramatic increase in rCBF,
ranging from 13% to 28% during rest, that may reflect increased cognitive effort or
arousal during hypnosis. It should be noted that other rCBF, PET and SPECT studies
have reported increases and decreases in cerebral blood flow in various cortical and
subcortical regions during hypnotic rest or hallucinatory suggestions (De Benedittis &
Longostreui, 1988; De Benedittis & Carli, 1990; Grond, Pawlik, Walter, Lesch, & Heiss,
1995; Halama, 1989; Maquet et al., 1999; Meyer, Diehl, Ulrich, & Meinig, 1989;
Rainville et al., 1999; Szechtman, Woody, Bowers, & Nahmias, 1998; Walter et al.,
1990). Germaine to our prior research, Rainville et al. (1999) reported bilateral PET
activation in anterior frontal cortex with predominant activity in the left hemisphere and

corresponding right hemisphere activation of the anterior cingulate associated with the
hypnotic state in highs (no lows were assessed). These studies provide strong evidence
for neurophysiological changes during hypnosis
During hypnotic analgesia, our rCBF study (Crawford et al., 1993) found that only
highly hypnotizable persons showed increased bilateral rCBFactivation in the anterior
frontal cortex as well as the somatosensory cortex. Similar frontal cortex increases have
been observed during hypnotic suggestions for pain modulation in subsequent PET
(Rainville, 1998; Rainville et al., 1999; Wik, Fischer, Bragée, Finer & Fredrickson,
1999) and SPECT (Heinrichs, Klemm, Scholz, & Biersack, 1997) research. We
interpreted such increased anterior frontal rCBF to reflect greater inhibitory processing
and supervisory planning occurring in these regions during hypnotic analgesia. This
research supports the view that hypnotic analgesia involves the supervisory attentional
control system (Hilgard, 1986) of the anterior frontal cortex in a topographically specific
inhibitory feedback circuit that cooperates in the regulation of thalamocortical activities
(e.g., Birbaumer, Elbert, Canavan, and Rockstroh, 1990) (Crawford, in press).
The increased blood flow in the somatosensory region observed during hypnotic
analgesia (Crawford et al., 1993) is difficult to interpret in light of recent conflicting
findings. Our fMRI research (Crawford, Horton, et al., 1998) found inconsistent bilateral
and unilateral primary and secondary somatosensory activation reductions and/or
increases during successful hypnotic analgesia. Rainville et al. (1999) reported suggested
pain reduction was accompanied by PET changes in somatosensory cortex. While the
somatosensory cortex is assumed to be involved in pain processing, neuroimaging studies
have reported increased blood flow (e.g., Casey et al., 1994; Coghill et al., 1994;

Heinrichs et al., 1997), no changes (Derbyshire et al., 1994, Jones et al., 1991; Rainville,
Duncan, Price, Carrier, & Bushnell, 1997), or decreased activity (Apkarian et al., 1992).
Only when we better understand the complex interplay between thalamic nuclei (and
other brain regions) and the somatosensory cortex during attention or disattention to pain
will we be able to interpret these findings.
In a SPECT study using thermal stimulation during hyperanalgesia and
hypoanalgesia, Heinrichs et al. (1997) reported continuing activation of the frontal lobe
during hypnotic suggestions. Interestingly, suggestions of increased pain was associated
with a distinct activity in the postcentral gyrus of the somatosensory system. This latter
finding was also observed by Hofbauer, Rainville, Duncan and Bushnell (1998; see also
Rainville et al., 1999).
A PET study of hypnotically responsive women with fibromyalgia (Wik et al., 1999)
underpins and extends our prior findings. During hypnotic analgesia, in comparison to
rest, patients reported substantial decreases in their chronic pain. Reduced pain
perception was accompanied by increased activation in the bilateral orbitofrontal cortex
(BA 11) in accordance with Crawford et al. (1993). Increases were also observed in
bilateral subcollosal cingulate (BA 24), right thalamus, and left inferior parietal (BA
40/39) areas. Decreases were observed in bilateral anterior (BA 24/33) and posterior
(BA 23/31) cingulate. Wik et al. noted that all areas, but the inferior parietal, are related
to limbic system structures that are engaged during pain defense or emotional processing.
Reduced cingulate activation suggests less attention was given to the encoding of the
associative significance of pain. They suggest that “the left inferior parietal activation

may then reflect psychological mechanisms serving to prevent awareness of pain, once
signaling has reached higher centres” (p. 11).
Reduced anterior cingulate involvement during hypnotic analgesia has previously
been observed in somatosensory event-related potentials (Kropotov, Crawford, &
Polyakov, 1997; see discussion in next section) and fMRI (Crawford, Horton et al., 1998)
research using noxious electrical stimulation, and PET research using painfully hot water
(Rainville, 1998; Rainville et al., 1997, 1999). In fMRI research, Crawford, Horton et al.
(1998) observed hemispheric shifts in activation and deactivation in various cingulate
regions in highs who eliminated all conscious awareness of sensory and distress pain. In
PET research, Rainville et al. (1997) observed decreased anterior cingulate activation
(BA 24) correlated with reduced distress perception. Furthermore, Crawford, Horton et
al. (1998) reported continued frontal activation with shifts in activation in the insula,
thalamus, sensorimotor cortex, and parietal regions during hypnotic analgesia.
These neuroimaging studies provide strong evidence that hypnotic analgesia impacts
neural pathways that modulate sensory-discriminative, emotional processing, attention,
and sensory-motor integration networks associated with pain (e.g., Iadarola et al., 1998).
Somatosensory Event-Related Potentials
Scalp-recorded somatosensory event-related potentials (SERPs) show significant
changes in mid to late components in response to unpleasant cutaneous stimulation
during hypnotic analgesia (e.g., Arendt-Nielsen, Zachariae, & Bjerring, 1990; Crawford,
1994a; Crawford, Knebel, et al., 1998; Danziger et al., 1998; De Pascalis, Crawford, &
Marucci, 1992; Horton, McClain-Furmanski, Mészáros, & Crawford, 1998; Mészáros &
Bányai, 1978; Mészáros, Bányai, & Greguss, 1978; McClain-Furmanski, Horton, &

Crawford, 1999; Sharev & Tal, 1989; Spiegel, Bierre, & Rootenberg, 1989; Zachariae &
Bjerring, 1994; for reviews, see Crawford, 1994a,b, in press; Crawford & Gruzelier,
1992, De Pascalis, 1998; Spiegel, 1996) in mid frontal, central, parietal, and/or occipital
regions. Few of these studies evaluated SERP changes in the anterior frontal region
during hypnotic analgesia, yet recent neurophysiological models of attention and pain
point to the importance of evaluating anterior frontal activity during hypnotic analgesia
processes.
Our research has been expanded to include anterior frontal cerebral dynamics as well
as more posterior regions by evaluating SERP activity in (1) scalp-recorded temporal
anterior frontal, mid-frontal, central and parietal regions in participants drawn from two
populations: healthy young adults (Crawford et al, 1997, 1999; Horton et al., 1998,
McClain-Furmanski, 1998) and adults with chronic low back pain (Crawford, Knebel et
al., 1998); and (2) temporarily implanted intracranial electrodes in the anterior cingulate
and anterior temporal cortex, as well as other areas (Kropotov et al., 1997).
In this review, an emphasis is placed upon findings from our recent study (Crawford,
Knebel et al., 1998) of 17 men and women, aged 19 to 43 years, with chronic low back
pain. On the Stanford Hypnotic Susceptibility Scale Form C (SHSS:C; Weitzenhoffer &
Hilgard, 1962) the participants were found to be all moderately to highly hypnotizable
except for one low hypnotizable man.
Three experimental sessions occurred approximately one week apart. The first
session involved the assessment of hypnotic susceptibility and pain control training, the
second involved SERP assessment to noxious electrical stimuli during attention and
hypnotic analgesia conditions, and the third involved EEG assessment to cold pressor

pain during attention and hypnotic analgesia conditions. At the first session, following
the SHSS:C, participants were taught hypnotic analgesia techniques to control pain
experimentally produced pain. Participants dipped their left hand into water and ice for
60 second immersions (‘cold pressor test”). By the third hypnotic analgesia dip, 60%
had completely eliminated all pain perception and 80% had completely eliminated all
distress perception. In comparison to unselected college students, these results are of a
surprising magnitude and raise important research questions whether adults with chronic
pain are more hypnotizable than the general population. If they are hypnotizable, then
hypnotic analgesia techniques should be quite suitable for assisting in the control of their
own pain (Crawford, Knebel et al., 1998).
The development of self-efficacy was documented across the sessions through the
successful transfer of newly learned skills from the reduction of experimental pain to the
reduction of their own chronic pain. Overall the participants reported significant chronic
pain reduction (McGill Pain Questionnaire), increased psychological well-being (Beck
Depression Inventory; SCL-90-R) and increased sleep quality (fewer minutes to fall
asleep).
In the second experimental session, the participants had their SERPs recorded at the
scalp while 30 noxious electrical stimuli were administered to the left middle finger
during conditions of waking and hypnosis. Reported below are the results of the within-
subjects, A-B-A design following a hypnotic induction in which blocks of stimuli were
presented in conditions of attend, hypnotic analgesia, and attend. The two attend
conditions were averaged and compared to the hypnotic analgesia condition.

For the adults with chronic low back pain, during hypnotic analgesia, hypothesized
inhibitory processing was implicated by an enhanced N140 in the anterior frontal (Fp1,
Fp2) region. This component is thought to reflect the “complex reciprocal interactions
between posterior and prefrontal [anterior frontal] cortex and subcortical structures” that
play “a key role in governing sequential attention processes” (Desmedt & Tomberg,
1989, p. 343). Additionally, during hypnotic analgesia, a greater N250 negativity was
observed in the fronto-central region. These findings suggest an “active disattention
during hypnotic analgesia, rather than the normally increasing spotlighted attention
towards relevant incoming sensory signals” (Crawford, Knebel et al., 1998, p 111).
Reductions of perceived intensity of pain during hypnotic analgesia were
accompanied by reduced P200 amplitudes in the mid-frontal, central and left parietal
regions, and reduced P300 amplitudes in the right midfrontal and central regions. These
findings may be interpreted as suggesting the reduced involvement of the parietal cortex.
One of the functions of the parietal cortex is to determine positions of body parts by
organizing sensory inputs received from the somatosensory and anterior frontal cortex
(Desmedt & Tomberg, 1989).
Our laboratory is the first to examine hypnotically related changes in the contingent
variations, which are related to arousal and attention (Tecce, 1972; Tecce & Cattanach,
1982) in the pre-stimulus SERP period prior to the regularly occurring electrical stimulus
that occurred every three seconds for 30 trials. Much work has centered around the CNV
(contingent negative variation), hypothesized to reveal enhanced cortical excitability
enabling a preparatory state. Additionally, there is a positive-moving contingent
variation (CPV) that may result from inhibitory processing and “a ‘disfacilitation’ in

cortical neuronal networks” (Rockstroh, Müller, Wagner, Cohen, & Elbert, 1993, p. 236;
for review, see Birbaumer et al., 1990). If hypnotic analgesia involves inhibitory
processing, then such a positive-moving contingent variation may be present.
Among the adults with chronic low back pain, we observed additional evidence for
the occurrence of inhibitory processing during hypnotic analgesia: a positive-going slope
of the prestimulus contingent cortical potential only in the left anterior frontal region.
This may reflect a lowering of cortical activity (Birbaumer et al., 1990; Rockstroh et al.,
1993) and increased inhibitory processing (Tecce, 1972; Tecce & Cattanach, 1972). The
asymmetry is strong evidence against eye movement artifact. Gruzelier (Gruzelier, 1988;
Crawford & Gruzelier, 1992) suggests a decreased involvement of the left anterior region
during hypnotic induction and certain hypnotic phenomena. In a recent study of healthy
young adults (Crawford et al., 1999) we found the CPV to be present at all evaluated
scalp sites.
Kropotov et al. (1997) was the first to demonstrate the potential involvement of the
anterior cingulate and the anterior temporal cortex in hypnotically suggested analgesia.
They recorded intracranial SERPs to 30 painful cutaneous stimuli in conditions of attend,
hypnotic analgesia, and attend in two female patients with obsessive-compulsive disorder
bearing multiple temporarily implanted intracranial electrodes. These electrodes were
located in the anterior cingulate cortex, amygdala, temporal cortex, and parietal cortex.
Hypnotically suggested analgesia led to a successful reduction of self-reported pain
perception and accompanying SERP intracranial changes in the hypnotically responsive
patient, but not in the non-hypnotically responsive patient. As shown in Figure 1,
reduced pain perception to noxious electrical stimuli to the right middle finger was

accompanied by (a) a significant reduction of the positive SERP component within the
range of 140-160 msec poststimulus recorded in the left anterior cingulate cortex, and (b)
a significant enhancement of the negative SERP component 200-260 msec poststimulus
recorded in the left anterior temporal cortex. No significant changes were observed in
other cortical regions or at the scalp-recorded mid-frontal Fz.
____________________
Insert Figure 1 about here
____________________
These findings are consistent with recent research (e.g., Bromm & Chen, 1995;
Derbyshire et al., 1996; Talbot et al., 1991) which implicates the anterior cingulate
cortex’s involvement in pain processing and the organization of responses to emotional
and noxious stimuli (Devinsky et al., 1995). We also interpret these findings to be
“indicative of increased active and controlled inhibitory processing of the incoming
painful stimuli . . . [and] further evidence that hypnotic analgesia is analogous to a No-
Go condition of response inhibition” (Kropotov et al., 1997, p. 6).
In summary, somatosensory event-related research strongly demonstrates that active
inhibitory processes in the brain are involved in hypnotic analgesia. Future work will
include evaluating earlier SERP components as well as localizing their sources in cortical
and subcortical structures.
EEG Activity
Further evidence of inhibitory processes occurring during hypnotic analgesia may be
gleaned from studies of EEG activity. Most hypnosis studies have evaluated EEG

activity during the administration of ongoing tonic pain, usually cold pressor pain.
Stimulus-bound EEG activity following phasic painful stimuli has yet to be addressed.
In a patient undergoing dental surgery with hypnosis as the sole anesthetic, total
EEG power decreased with a greater diminution in the left hemisphere in alpha and theta
EEG bands (Chen, Dworkin, & Bloomquist, 1981). Karlin, Morgan, and Goldstein
(1980) reported hemispheric shifts in total EEG power during hypnotic analgesia to cold
pressor pain that were interpreted as greater overall right-hemisphere involvement at the
bipolar parieto-occipital derivation.
Crawford (1990) evaluated the accompanying EEG during 60-sec immersions of the
left hand into ice cold water during conditions of attend and hypnotic analgesia. Of
particular interest were interactions between condition and hypnotic level in the high
theta (5.5 - 7.5 Hz frequency band). First, as has been shown often in the literature (e.g.,
Sabourin, Cutcomb, Crawford, & Pribram, 1990; for a review, see Crawford &
Gruzelier, 1992), highs generated significantly more high theta than did lows at mid
frontal (F3, F4), temporal (T3, T4), parietal (P3, P4) and occipital (O1, O2) sites. This
theta activity is thought to possibly originate in the hippocampal region and be associated
with focused attention, and thus reflective of the more effective attention system
observed in highly hypnotizable persons (for review, see Crawford & Gruzelier, 1992).
The low hypnotizables showed no significant hemispheric asymmetries, while the high
hypnotizables did. In the temporal region (T3, T4), when concentrating on the pain the
highs were significantly more left hemisphere dominant in high theta. By contrast,
during hypnotic analgesia the highs showed a significant shift to less left hemispheric
theta power and greater right hemisphere theta power.

Using phasic pain consisting of electric shocks to the left wrist, De Pascalis and
Perrone (1996) assessed ongoing bilateral EEG activity recorded from mid frontal,
central and posterior regions during waking, hypnosis with no analgesia, and hypnosis
with analgesia in low and high hypnotizables. They did not evaluate the stimulus-bound
EEG following each painful stimuli, although the SERPs were evaluated in a separate
publication (De Pascalis et al., 1992). During hypnotic analgesia, highs showed
reductions of total power, delta (0.5 - 3.75 Hz) and beta 1 (13-15.75 Hz) in the right
hemisphere, which was accompanied by a decrease in sympathetic activity level as
evidenced by heart period variability. De Pascalis and Perrone found no differences in
high theta (6-7.5 Hz) at recorded sites, but it should be noted that they did not record
from the temporal region where Crawford (1990) observed high theta hemispheric shifts.
In both attend and analgesia conditions during hypnosis, highs evidenced a reduction of
low theta (4-5.75 Hz) with similar levels of activity in both hemispheres, whereas in
waking there was greater low theta present in the left hemisphere. The reduction of low
theta during hypnosis suggests greater cortical arousal or attention during hypnosis. This
provides further support to Crawford et al.’s (1993) previously discussed proposal that
hypnosis requires cognitive effort.
Other Neurophysiological Changes during Hypnotic Analgesia
Hypnotic analgesia can have an inhibitory effect on peripheral spinal reflex activity
that suggests it has an impact upon descending thalamo-spinal pathways for pain control
(for review, see Price, 1996). The Hoffman reflex amplitude decreased significantly
during hypnosis in high but not low hypnotizables, yet suggested analgesia had no effect
(Santarcangelo, Busse, & Carli, 1989). Reductions in brief latency (Hagbarth & Finer,

1963) and R-III amplitude (Danziger et al., 1998; Kiernan, Dane, Phillips, & Price,
1995) of spinal reflexes were observed during hypnotic analgesia. Danziger et al. (1998)
evaluated both the RIII reflex and SERPs to noxious stimuli during attend and hypnotic
analgesia conditions in highly hypnotizable participants (no lows). While all participants
displayed reduced late SERPs and increased pain tolerance during hypnotic analgesia,
there were two subgroups with distinct patters of RIII reflex modulation. One subgroup
showed a strong inhibition of the reflex, whereas the other subgroup showed a strong
facilitation of the reflex. While all shifted their attention away from the pain, some were
more reactive and others less reactive motorically. These are intriguing findings that
need further exploration.
Since some inhibitory processes operate via endogenous opioid peptides, several
studies assessed the potential effect of hypnotic analgesia on the opiate descending
control mechanism. Unlike opiate analgesia, hypnotic analgesia has generally not been
reversed by the opiate antagonist naloxone hydrochloride (Barber & Mayer, 1977;
Goldstein & Hilgard, 1988; Spiegel & Albert, 1983; but see Stevenson, 1978) except
under circumstances of stress (Frid & Singer, 1978). Preliminary studies (e.g.,
Domangue, Margolis, Lieberman, & Kaji, 1985; Sternbach, 1982) suggest other
neurochemical processes may be involved in hypnotic analgesia. The mean plasma level
of beta-endorphin-immunoreactivity was enhanced after hypnotic analgesia in arthritic
patients, while no changes in plasma levels of epinephrine, dopamine or serotonin
occurred (Domangue et al., 1985). The surprising paucity of research in this area leaves
it open to exciting explorations.
General Summary

The research reviewed here supports the view that hypnotic analgesia is an active
inhibitory process that involves attentional, inhibitory and multiple pain systems in the
brain. Even though the processes may be dissociated from conscious awareness and
appear to be beyond volitional control, we propose that hypnotic analgesia depends upon
the activation of a supervisory, attention control system -- involving the anterior frontal
cortex -- which then participates with other cortical and subcortical processes in the
allocation of thalamocortical activities. Hypnotic analgesia is the result of changes that
affect the active allocation of attention and disattention associated with the anterior
frontal region, as well as spatio-temporal aspects of the perception of pain associated
with the posterior cortical systems.

Footnotes
With the kind permission of the editor of Contemporary Hypnosis, this paper is an
updated and expanded reprint of an article by Crawford, Knebel, and Vendemia that
appeared in Contemporary Hypnosis, 1998, 15, 22-33.

Acknowledgments
Portions of the research from our laboratory were supported by grants to Crawford
from the National Institutes of Health (R21 RR09598), The Spencer Foundation, a
National Institutes of Health Biomedical Research Support Grant, and a Virginia Tech
Aspires Grant. We gratefully acknowledge our collaborators (J. H. Downs, III, L.
Kaplan, J. Kropotov, Y Polyakov, K.H. Pribram, M. Xie) who participated in some of
the studies discussed herein.

References
Apkarian, V. A., Stea, R. A., Manglos, S. H., Szevernyi, N. M., King, R. B., & Thomas,
F. D. (1992). Persistent pain inhibits contralateral somatosensory cortical activity in
humans. Neuroscience Letters, 140, 141-147.
Arendt-Nielsen, N. L., Zacharie, R., & Bjerring, P. (1990). Quantitative evaluation of
hypnotically suggested hyperaesthesia and analgesia by painful laser stimulation.
Pain, 42, 243-251.
Barabasz, A. F., & Barabasz, M. (1992). Research designs and considerations. In E.
Fromm & M. R. Nash (Eds.), Contemporary hypnosis research (pp. 173-200). NY:
Guilford Press.
Barber, J. (Ed.) (1996). Hypnosis and suggestion in the treatment of pain: A clinical
guide. New York: W. W. Norton & Co.
Barber, J., & Adrian, C. (Eds.) (1982). Psychological approaches to the management of
pain. New York: Brunner/Mazel.
Barber, J., & Meyer, D. (1977). Evaluation of the efficacy and neural mechanism of a
hypnotic analgesia procedure in experimental and clinical dental pain. Pain, 4, 4-48.
Birbaumer, N., Elbert, T., Canavan, A.G.M., & Rockstroh, B. (1990). Slow potentials of
the cerebral cortex and behavior. Physiological Review, 70, 1-41.
Bromm, B., & Chen, A. C. (1995). Brain electrical source analysis of laser evoked
potentials in response to painful trigeminal nerve stimulation.
Electroencephalography and Clinical Neurophysiology, 95, 14-26.
Casey, K. I., Minoshima, S., Berger, K. L., Koeppe, R. A., Morrow, T. J., Frey, K. A.
(1994). Positron Emission Tomographic analysis of cerebral structures activated

specifically by repetitive noxious heat stimuli. Journal of Neurophysiology, 71, 802-
807.
Chaves, J. F. (1989). Hypnotic control of clinical pain. In N. P. Spanos & J. F. Chaves
(Eds.), Hypnosis: The cognitive-behavioral perspective (pp. 242-272). Buffalo, NY:
Prometheus Books.
Chaves, J. F. (1994). Recent advances in the application of hypnosis to pain
management. American Journal of Clinical Hypnosis, 37, 117-129.
Chen, A. C. N., Dworkin, S. F., & Bloomquist, D. S. (1981). Cortical power spectrum
analysis of hypnotic pain control in surgery. International Journal of Neuroscience,
13, 127-136.
Chundler, E. H., & Dong, W. K. (1995). The role of the basal ganglia in nociception and
pain. Pain, 60, 3-38.
Coghill, R. C., Talbot, J. D., Evans, A. C., Meyer, E., Gjedde, A., Bushnell, M. C., &
Duncan, G. H. (1994). Distributed processing of pain and vibration by the human
brain. Journal of Neuroscience, 14, 4095-4108.
Craig, A. D. (1998). A new version of the thalamic disinhibition hypothesis of central
pain. Pain Forum, 7, 1-14.
Craig, A. D., Bushnell, M. C., Zhang, E. T., & Bloomqvist, A. (1994). A thalamic
nucleus specific for pain and temperature sensation. Nature, 372, 770-773.
Crawford, H. J. (1990). Cognitive and psychophysiological correlates of hypnotic
responsiveness and hypnosis. In M. L. Fass & D. Brown (Eds.), Creative mastery in
hypnosis and hypnoanalysis: A festschrift for Erika Fromm (pp. 155-168). Hillsdale,
New Jersey: Erlbaum.

Crawford, H. J. (1994a). Brain systems involved in attention and disattention (hypnotic
analgesia) to pain. In K. Pribram (Ed.), Origins: Brain and self organization (pp. 661-
679). Hillsdale, NJ: Lawrence Erlbaum Associates, Inc.
Crawford, H. J. (1994b). Brain dynamics and hypnosis: Attentional and disattentional
processes. International Journal of Clinical and Experimental Hypnosis, 42, 4204-
232.
Crawford, H. J. (1995 October). Use of hypnotic techniques in the control of pain:
Neuropsychophysiological foundation and evidence. Invited presentation at
Technology Assessment Conference on Integration of Behavioral and Relaxation
Approaches into the Treatment of Chronic Pain and Insomnia. National Institutes of
Health, Bethesda, MD.
Crawford, H. J. (in press). Neuropsychophysiology of hypnosis: Towards an
understanding of how hypnotic interventions work. In G. D. Burrows, R. O. Stanley,
& P. B. Bloom (Eds.), Advances in Clinical Hypnosis. New York: Wiley.
Crawford, H. J., & Allen, S. N. (1983). Enhanced visual memory during hypnosis as
mediated by hypnotic responsiveness and cognitive strategies. Journal of
Experimental Psychology: General, 112, 662-685.
Crawford, H. J., Brown, A., & Moon, C. (1993). Sustained attentional and disattentional
abilities: Differences between low and highly hypnotizable persons. Journal of
Abnormal Psychology, 102, 534-543.
Crawford, H. J., & Gruzelier, J. H. (1992). A midstream view of the
neuropsychophysiology of hypnosis: Recent research and future directions. In E.

Fromm & M. R. Nash (Eds.), Contemporary hypnosis research (pp. 227-266). NY:
Guilford Press.
Crawford, H. J., Gur, R. C., Skolnick, B., Gur, R. E., & Benson, D. (1993). Effects of
hypnosis on regional cerebral blood flow during ischemic pain with and without
suggested hypnotic analgesia. International Journal of Psychophysiology, 15, 181-
195.
Crawford, H. J., Horton, J. E., Harrington, G. C., Vendemia, J. M. C., Plantec, M. B.,
Jung, S., Shamro, C. & Downs, III, J. H. (1998). Hypnotic analgesia (disattending
pain) impacts neuronal network activation: An fMRI study of noxious
somatosensory TENS stimuli. Neuroimage, 7, S436.
Crawford, H.J., Horton, J.E., McClain-Furmanski, D., & Vendemia, J. (1998). Brain
dynamic shifts during the elimination of perceived pain and distress: Neuroimaging
studies of hypnotic analgesia. INABIS98, 0611.
http://www.mcmaster.ca/inabis98/woody/crawford0611/index.html
Crawford, H. J., Knebel, T., Kaplan, L., Vendemia, J. M. C., Xie, M., Jamison, S., &
Pribram, K. H. (1998). Hypnotic Analgesia: I. Somatosensory Event-Related
Potential Changes to Noxious Stimuli and II. Transfer Learning to Reduce Chronic
Low Back Pain. International Journal of Clinical and Experimental Hypnosis, 46,
92-132.
Crawford, H. J., Knebel, T., Xie, M., Horton, J. E., & Pribram, K. H . (1999).
Attentional Vs. Inhibitory (Hypnotic Analgesia) Processing of Noxious Stimuli:
Somatosensory Event-Related Potential Amplitude and Latency Differences
Between Low and Highly Hypnotizable Persons. Unpublished manuscript.

Crawford, H. J., Knebel, T., Vendemia, J. M. C. (1998). The nature of hypnotic
analgesia: Neurophysiological foundation and evidence. Contemporary Hypnosis,
1998, 15, 22-33.Crawford, H. J., Knebel, T., Vendemia, J., Kaplan, L., Xie, M.,
L’Hommedieu, C., & Pribram, K. (1997). Somatosensory event-related potentials
and allocation of attention to pain: Effects of hypnotic analgesia as moderated by
hypnotizability level. International Journal of Psychophysiology, 25, 72-73.
Cronbach, L. J. (1975). Beyond the two disciplines of scientific psychology. American
Psychologist, 30, 116-127.
Danziger, N., Flurnier, E., Bouhassira, D., Michaud, D., De Broucker, T., Santarcangelo,
E., Carli, g., Chertock, L., & Willer, J. C. (1998). Different strategies of modulation
can be operative during hypnotic analgesia: A neurophysiological study. Pain,
75(1), 85-92.
Davis, K.D., Wood, M. L., Crawley, A. P., & Mikulis, D. J. (1995). fMRI of human
somatosensory and cingulate cortex during painful electrical nerve stimulation.
Neuroreport, 7, 321-325.
De Benedittis, G., & Carli, G. (1990). Psineurobiologia dell’ipnosi. In M. Tiengo (Ed.),
Seminari sul dolore (pp. 59-116). Milan: Centro Studi sull’Analgesia, Università
degli Studi di Milano.
De Benedittis, G., & Longostreui, G. P. (1988, July). Cerebral blood flow changes in
hypnosis: A single photon emission computerized tomography (SPECT) study.
Paper presented at the 4th World Congress of Psychophysiology, Prague,
Czechoslovakia.

De Pascalis, V.; (1998). Brain mechanisms and attentional processes in hypnosis.
Presented at INABIS '98 - 5th Internet World Congress on Biomedical Sciences at
McMaster University, Canada, Dec 7-16th. Invited Symposium. Available at URL
http://www.mcmaster.ca/inabis98/woody/de_pascalis0311/index.html
De Pascalis, V., Crawford, H. J., & Marucci, F. S. (1992). Analgesia ipnotica nella
modulazione del dolore: Effeti sui potenziali somatosensoriali. [The modulation of
pain by hypnotic analgesia: Effect on somatosensory evoked potentials.]
Comunicazioni Scientifiche di Psicologie Generale, 71-89.
De Pascalis, V., & Perrone, M. (1996). EEG asymmetry and heart rate during
experience of hypnotic analgesia in high and low hypnotizables. International
Journal of Psychophysiology, 21, 163-175.
Depaulis, A., & Bandler, R. (Eds.) (1991). The midbrain periaqueductal gray matter:
Functional, anatomical and neurochemical organization. New York: Plenum.
Derbyshire, S. W. G., Chen, A. C. N., & Jones, A. K. P. (1996). Somatosensory and
frontal cortical processing during pain experience. In O. Franzén, R. Johansson, &
L. Terenius (Eds.), Somesthesis and the neurobiology of the somatosensory cortex
(pp. 385-394). Basel, Switzerland: Birkhäuser Verlag.
Derbyshire, S. W. G., Jones, A. K. P., Devani, P., Friston, K. J., Feinmann, C., Harris,
M., Pearce, S., Watson, J. D. G., & Frackowiak, R. S. J. (1994). Cerebral responses
to pain in patients with atypical facial pain measured by Positron Emission
Tomography. Journal of Neurology, Neurosurgery and Psychiatry, 57, 1166-1173.
Desmedt, J. E., & Tomberg, C. (1989). Mapping early somatosensory evoked potentials
in selective attention: critical evaluation of control conditions using for titrating by

difference the cognitive P30, P40, P100 and N140. Electroencephalography and
Clinical Neurophysiology, 74, 321-346.
Devinsky, O., Morrell, M. J., & Vogt, B. A. (1995). Contributions of anterior cingulate
cortex to behaviour. Brain, 118, 279-306.
Domangue, B. B., Margolis, C. G., Lieberman, D., & Kaji, H. (1985). Biochemical
correlates of hypnoanalgesia in arthritic pain patients. Journal of Clinical
Psychiatry, 46, 235-238.
Downs III, J. H., Crawford, H. J., Plantec, M. B., Horton, J. E., Vendemia, J. M. C.,
Harrington, G. C., Yung, S., & Shamro, C. (1998). Attention to painful
somatosensory TENS stimuli: An fMRI study. Neuroimage, 7, S432.
Evans, F. J. (1988). Hypnosis and pain control. Advances, Institute for the
Advancement of Health, 5, 31-39.
Franzén, O., & Ahlquist, M. (1996 June). Cerebral representation and coding of sharp
dental pain in man. Paper presented at the 8th World Congress of
Psychophysiology, Tampere, Finland.
Frid, M., & Singer, G. (1980). The effects of naloxone on human pain reactions during
stress. In C. Peck & M. Wallace (Eds.), Problems in pain: Proceedings of the first
Australian New Zealand conference on pain (pp. 78-86). Sydney: Pergamon Press.
Gibson, H. B. (Ed.) (1994) Psychology, pain and anaesthesia. London: Chapman &
Hall.
Goldstein, A., & Hilgard, E. R. (1975). Failure of opiate antagonist naloxone to modify
hypnotic analgesia. Proceedings of the National Academy of Sciences, 72, 2041-
2043.

Grond, M., Pawlik, G., Walter, H., Lesch, O. M., Heiss, W. D. (1995). Hypnotic
catalepsy-induced changes of regional cerebral glucose metabolism. Psychiatry
Research, 61, 173-179.
Gruzelier, J. H. (1988). The neuropsychology of hypnosis. In M. Heap (Ed.), Hypnosis:
Current clinical, experimental and forensic practices (pp. 68-76). London: Croom
Helm.
Gruzelier, J; (1998). A working model of the neurophysiology of hypnotic telaxation.
Presented at INABIS '98 - 5th Internet World Congress on Biomedical Sciences at
McMaster University, Canada, Dec 7-16th. Invited Symposium. Available at URL
http://www.mcmaster.ca/inabis98/woody/gruzelier0814/index.html
Hagbarth, K. E., & Finer, B. L. (1963). The plasticity of human withdrawal reflexes to
noxious skin stimuli in lower limbs. Progress in Brain Research, 1, 65-78.
Head, H. (1920). Studies in neurology (2 vols). London: Oxford University Press.
Heinrichs, M., Klemm, E., Scholz, O. B., Biersack, H. J. (1997). Wenn Nociception
nicht mehr schmerzhaft ist . . . Welche Aenderungen der Hirndurchblutung
korrelieren mit hypnotisch modifizierter Schmerzempfindung? / When nociception
does not hurt anymore: Do changes in regional cerebral blood flow correlate with
hypnotically modified perception of pain? Experimentelle und Klinische Hypnose,
13(2), 111-124.
Hilgard, E. R. (1965). Hypnotic susceptibility. New York: Harcourt, Brace & World.
Hilgard, E. R. (1986). Divided consciousness: Multiple controls in human thought and
action. New York: Wiley.

Hilgard, E. R., & Hilgard, J. R. (1994). Hypnosis in the relief of pain (rev. ed.). New
York: Brunner/Mazel, Inc.
Hilgard, J. R., & LeBaron, S. W. (1984). Hypnotherapy of pain in children with cancer.
Los Altos, Ca.: William Kaufman.
Hoffauer, R. K., Rainville, P., Duncan, G. H., & Bushnell, M. C. (1998). Modulation of
pain sensation alters activity in human cerebral cortex. Society for Neuroscience
Abstract, 24: Abstract # 447.5.
Holroyd, J. (1996). Hypnosis treatment of clinical pain: Understanding why hypnosis is
useful. International Journal of Clinical and Experimental Hypnosis, 44, 33-51.
Horton, J. E., McClain-Furmanski, D. Mészáros, I., & Crawford, H. J. (1998). To inhibit
pain is to actively shift conscious awareness: Somatosensory event-related potential
evidence during hypnotic analgesia. International Journal of Psychophysiology, 30,
234-235.
Howland, E. W., Wakai, R. T., Mjaanes, B. A., Balog, J. P., & Cleeland, C. S. (1995).
Whole head mapping of magnetic fields following painful electric finger shock.
Cognitive Brain Research, 2, 165-172.
Hutchison, W. D., Davis, K. D., Lozano, A. M., Tasker, R. R., & Dostrovsky, J. O.
(1999). Pain-related neurons in the human cingulate cortex. Nature Neuroscience, 2,
403-405.
Iadarola, M. J., Berman, K. R., Seffiro, T. A., Byas-Smith, M. G., Gracely, R. H., Max,
M. B., & Bennett, G. J. (1998). Neural activation during acute capsaicin-evoked pain
and allodynia assessed with PET. Brain, 121, 931-947.

Jones, A. K. P., Brown, W. D., Friston, K. J., Qi, L. Y., & Frackowiak, S. J. (1991).
Cortical and subcortical localization of response in pain in man using positron
emission tomography. Proceedings of the Royal Society London, Series B.,
Biological Sciences, 244, 39-44.
Karlin, R., Morgan, D., & Goldstein, L. (1980). Hypnotic analgesia: A preliminary
investigation of quantitated hemispheric electroencephalographic and attentional
correlates. Journal of Abnormal Psychology, 89, 591-594.
Kiernan, B. D., Dane, J. R., Phillips, L. H., & Price, D. D. (1995). Hypnoanalgesia
reduces R-III nocioceptive reflex: Further evidence concerning the multifactorial
nature of hypnotic analgesia. Pain, 60, 39-47.
Kropotov, J. D., Crawford, H. J., & Polyakov, Y. I. (1997). Somatosensory event-related
potential changes to painful stimuli during hypnotic analgesia: Anterior cingulate
cortex and anterior temporal cortex intracranial recordings. International Journal of
Psychophysiology, 27, 1-8.
Luria, A.R. (1966). the higher cortical functions in man. New York: Basic.
Maquet, P., Faymonville, M. E., Degueldre, C., Delfiore, G., Franck, G., Luxen, A.,
Lamy, M. (1999). Functional neuroanatomy of hypnotic state. Biological Psychiatry,
45, 327-33.
Markenson, J. A. (1996). Mechanisms of chronic pain. The American Journal of
Medicine, 101 (suppl 1A), 6-28.
McClain-Furmanski, D., Horton, J. E., & Crawford, H. J. (1999). Inhibition of pain:

Effects on somatosensory event-related potentials during hypnotic analgesia in high
but not low hypnotizable persons. A Supplement of the Journal of Cognitive
Neuroscience: Cognitive Neuroscience Society Annual Meeting Program, 85.
Melzack, R. (1992). Recent concepts of pain. Journal of Medicine, 13, 147-160.
Melzack, R., & Casey, K. L. (1968). Sensory, motivational, and central control
determinants of pain. A new conceptual model. In D. R. Kenshalo (Ed.), The Skin
Senses (pp. 423-439). Springfield, IL: C.C. Thomas.
Melzack, R., & Wall, P. D. (1965). Pain mechanisms: a new theory. Science, 150, 971-
979.
Mészáros, I., & Bányai, É. I. (1978). Electrophysiological characteristics of hypnosis.
In K. Lissak (Ed.), Neural and neurohumoral organization of motivated behavior (pp.
173-187). Akademii Kiado, Budapest.
Mészáros, I., Bányai, É. I., & Greguss, A. C. (1978). Alteration of activity level: The
essence of hypnosis or a byproduct of the type of induction? In G. Adám, I.
Mészáros, & É. I. Bányai (Eds.), Advanced Physiological Science, Brain and
Behaviour, 17, 457-465.
Norman, D. A., & Shallice, T. (1986). Attention to action: Willed and automatic control
of behavior. In R. J. Davidson, G. E. Schwartz, and D. E. Shapiro (Eds),
Consciousness and self-regulation (vol. 4), New York: Plenum Press.
Olness, K., & Gardner, G. G. (1988). Hypnosis and hypnotherapy with children (2nd
ed.). Philadelphia, MA: Grune & Stratton.

Ploghaus, A., Tracey, I., Gati, J. S., Clare, S., Menon, R. S., Matthews, P. M., &
Rawlins, J. N. P. (1999). Dissociating pain from its anticipation in the human brain.
Science, 284, 1979-1981.
Posner, M. I., & Petersen, S. E. (1990). The attentional system of the human brain.
Annual Review of Neuroscience, 13, 25-42.
Posner, M. I., & Raichle, M. E. (1994). Images of mind. New York: Scientific
American Library.
Pribram, K. H. (1991). Brain and perception: Holonomy and structure in figural
processing. Hillsdale, NJ: Lawrence Erlbaum.
Price, D. D. (1988). Psychological and neural mechanisms of pain. New York: Raven.
Price, D. D. (1996). Hypnotic analgesia: Psychological and neural mechanisms. In J.
Barber (Ed.), Hypnosis and suggestion in the treatment of pain: A clinical guide (pp.
67-84). New York: W. W. Norton & Co.
Rainville, P.; (1998). Brain Imaging Studies of the Hypnotic Modulation of Pain
Sensation and Pain Affect. Presented at INABIS '98 - 5th Internet World Congress
on Biomedical Sciences at McMaster University, Canada, Dec 7-16th. Invited
Symposium. Available at URL
http://www.mcmaster.ca/inabis98/woody/rainville0419/index.html
Rainville, P., Duncan, G. H., Price, D. D., Carrier, B. & Bushnell, M. C. (1997). Pain
affect encoded in human anterior cingulate but not somatosensory cortex. Science,
277(5328), 968-971.

Rainville, P., Hofbauer, R. K., Paus, T., Duncan, G. H., Bushnell, M. C., & Price, D.
(1999). Cerebral mechanisms of hypnotic induction and suggestion. Journal of
Cognitive Neuroscience, 11(1), 110-125.
Rockstroh, B., Müller, M., Wagner, M., Cohen, R., & Elbert, T. (1993). “Probing” the
nature of the CNV. Electroencephalography and clinical Neurophysiology, 87, 235-
241.
Sabourin, M. E., Cutcomb, S. D., Crawford, H. J., & Pribram, K. H. (1990). EEG
correlates of hypnotic susceptibility and hypnotic trance: Spectral analysis and
coherence. International Journal of Psychophysiology, 10, 125-142.
Santarcangelo, E. L., Busse, K., & Carli, G. (1989). Changes in electromyographically
recorded human monosynaptic reflex in relation to hypnotic susceptibility and
hypnosis. Neuroscience Letters, 104, 157-160.
Szechtman, H., Woody, E., Bowers, K. S., & Nahmias, C. (1998). Where the imaginal
appears real: a positron emission tomography study of auditory hallucinations.
Proceedings of the National Academy of Sciences, 95, 1956-60.
Sharav, V., & Tal, M. (1989). Masseter inhibitory periods and sensations evoked by
electrical tooth-pulp stimulation in subjects under hypnotic anesthesia. Brain
Research, 479, 247-254.
Spiegel, D. (1991). Neurophysiological correlates of hypnosis and dissociation. Journal
of Neuropsychiatry and Clinical Neurosciences, 3, 440-445.
Spiegel, D., & Albert, L. H. (1983). Naloxone fails to reverse hypnotic alleviation of
chronic pain. Psychopharmacology, 81, 140-143.

Spiegel, D., Bierre, P., & Rootenberg, J. (1989). Hypnotic alteration of somatosensory
perception. American Journal of Psychiatry, 146, 749-754.
Sternbach, R. A. (1982). On strategies for identifying neurochemical correlates of
hypnotic analgesia: A brief communication. International Journal of Clinical and
Experimental Hypnosis, 30, 251-256.
Stevenson, J. B. (1978). Reversal of hypnosis-induced analgesia by naloxone. Lancet, 2,
991-992.
Stuss, D. T., Shallice, T., Alexander, M. P., & Picton, T. W. (1995). A multidisciplinary
approach to anterior attentional functions. In J. Grafman, K. Hollyoak, and F. Boller
(Eds.), Structure and functions of the human prefrontal cortex, Annals of the New
York Academy of Sciences, 279, 191-211.
Sweet, W.H., Pain: Old and new methods of study and treatment. Acta Neurochir
Suppl., 64, 83-87.
Talbot, J. D., Marrett, S., Evans, A. C., Meyer, E., Bushnell, M. C., & Duncan, G. H.
(1991). Multiple representations of pain in human cerebral cortex. Science, 251,
1355-1358.
Tecce, J. J. (1972). Contingent negative variation (CNV) and psychological processes in
man. Psychological Bulletin, 77, 73-108.
Tecce, J. J., & Cattanach, L. (1982). Contingent negative variation. In E. Niedermeyer
& F. Lopes da Silva (Eds.), Electroencephalography: Basic principles, clinical
applications and related fields (pp. 543-562). Baltimore: Urban and Schwarzenberg.
Tellegen, A (1981). Practicing the two disciplines for relaxation and enlightenment:
Comment on “Role of the biofeedback signal in electromyograph biofeedback: The

relevance of attention: by Qualls and Sheehan. Journal of Experimental Psychology:
General, 110, 217-226.
Treede, R-D, Kenshalo, D. R., Gracely, R. H., & Jones, A. K. P. (1999). The cortical
representation of pain. Pain, 79, 105-111.
Walter, H., Podreka, I., Steiner, M., Suess, E., Benda, N., Hajji, M., Lesch, O. M.,
Musalek, M., & Passweg, V. (1990). A contribution to classification of
hallucinations. Psychopathology, 23, 97-105.
Wik, G., Fischer, H., Bragée, B., Finer, B., & Fredrikson, M. (1999). Functional
anatomy of hypnotic analgesia: a PET study of patients with fibromyalgia. European
Journal of Pain, 3, 7-12.
Weitzenhoffer, A. M., & Hilgard, E. R. (1962). Stanford Hypnotic Susceptibility Scale,
Form C. Palo Alto, CA: Consulting Psychologists Press.
Yamaguchi, S., & Knight, R. T. (1990). Gating of somatosensory input by human
prefrontal cortex. Brain Research, 521, 281-288.
Zachariae, R., & Bjerring, P. (1994). Laser-induced pain-related brain potentials and
sensory pain ratings in high and low hypnotizable subjects during hypnotic
suggestions of relaxation, dissociated imagery, focused analgesia, and placebo.
International Journal of Clinical and Experimental Hypnosis, 42, 56-80.


Figures
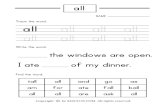
Figure 1. In a hypnotizable patient, somatosensory event-related potentials at two
intracranial sites, averaged across 30 trials during conditions of attend, hypnotically
suggested analgesia and attend. Note the reduction in the positive component at 140-160
msec in the left anterior cingulate (upper) and the increase in the negative component at
200-260 msec in the left anterior temporal cortex (lower). With permission, reprinted
from Kropotov et al. (1997, p. 5).