Chronic Renal Insufficiency Predicts Poor Outcome in Patients Undergoing Cardiac Resynchronization...
Transcript of Chronic Renal Insufficiency Predicts Poor Outcome in Patients Undergoing Cardiac Resynchronization...
outcomes of stress (burden), and physical and mental functioning in spousal care-givers of HF patients. Methods: A repeated measures design was used to examinepatterns at baseline, 1, 2, 3, & 5 months. Participants were randomly assigned to in-tervention or control groups. The Health Buddy, a simple, user-friendly, 6 by 9 inchtelecommunication device, was used to deliver the SS intervention. The interventiongroup accessed the Health Buddy daily for 10-15 minutes for information on HF,healthy lifestyle behaviors, emotional support, seeking SS, and conflict management.Coping, stress, physical and mental functioning were measured using valid, reliablequestionnaires. Sleep was measured with the Actiwatch L. Results: The 20 partici-pants were 80% Caucasian and 80% women with a mean age of 60 years. Findingsindicated the intervention group increased use of problem-focused coping and seek-ing SS, and were lower in blaming self, wishful thinking, and avoidance coping thanthe control group. For the control group, caregiver burden increased (demand up25%; difficulty up 10%; average burden up 16%). For the intervention group, care-giver burden decreased overall (demand down 5%; difficulty down 3%; average bur-den unchanged). Physical functioning was unchanged for the control group andimproved 8% in the intervention group. Mental functioning was unchanged for thecontrol group and decreased by 3% for the intervention group. Sleep latency rosein the control group from 18 to 20 minutes and decreased in the intervention groupfrom 28 to 15 minutes. Conclusion: Components of SS can be delivered via a tele-health communication device. Intervention participants improved coping skills,diminished burden, improved physical functioning and improved sleep latency.
310Patient Preferences for Survival and Quality of Life of Rural, Indigent HeartFailure Patients Are Similar to an Urban Heart Failure PopulationEldrin F. Lewis1, Dedric Clarke2, Kathy Hebert2, Lee Arcement2, Ronald Horswell3,Lynne W. Stevenson1; 1Cardiovascular Medicine, Brigham and Women’s Hospital,Boston, MA; 2Internal Medicine, Leonard J. Chabert Medical Center, Houma, LA;3Epidemiology, Louisiana State University School of Public Health, New Orleans,LA
Background: Increasing options for therapy in heart failure (HF) patients requirebetter understanding of patient preferences regarding quality of life (QOL) and sur-vival. Many rural, indigent patients are not enrolled in clinical heart failure trials inwhich these measures are assessed. Moreover, little is known about differences inpreferences of diverse HF populations. Methods: HF patients in a rural, indigentHF clinic in Louisiana (n 5 100) were compared to patients referred to an urban, ter-tiary care center (n 5 99). Patients completed the time trade-off (TTO) tool to assesswillingness to trade time for better health (higher score 5 less willingness to trade)and the Minnesota Living with Heart Failure questionnaire (LHF) to assess QOL(higher score 5 worse QOL). Results: Indigent HF patients were older (58 vs. 52,p ! 0.001), had more non-Whites (42% vs. 22%, p ! 0.001), higher ejection frac-tion (31% vs. 24%, p ! 0.001), and lower proportion with NYHA Class III-IV HF(41% vs. 74%, p ! 0.001). When stratified by NYHA Class, LHF and TTO prefer-ences increased equally between the two populations (NYHA I: LHF 25 vs. 27, TTO0.99 vs. 0.91), (NYHA II: LHF 47 vs. 45, TTO 0.90 vs. 0.86), (NYHA III: LHF 62 vs.59, TTO 0.66 vs. 0.69). In addition, patients’ willingness to trade time for betterhealth increased in a linear fashion as their QOL quartiles worsened in both popula-tions (Figure). Conclusions: There were no differences in QOL or preferences totrade time for better health between rural indigent and urban referral HF populations.Patients with worse QOL were more likely to trade time for better health in both HFpopulations, suggesting validity of preference assessment in both groups. The impactof therapies designed to improve QOL and honor patient preferences in one popula-tion may apply generally across diverse populations.
Figure. Increased Willingness to Trade Time for Perfect Health among Patients withWorse Quality of Life EQUALLY in Rural, Indigent and Urban Heart Failure Popu-lations.
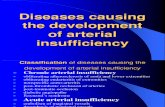
311Chronic Renal Insufficiency Predicts Poor Outcome in Patients UndergoingCardiac Resynchronization Therapy for Congestive Heart FailureGrace Lin1, Peter A. Brady1; 1Cardiology, Mayo Clinic, Rochester, MN
Background: Cardiac resynchronization therapy (CRT) improves outcomes in se-lected patients with congestive heart failure (CHF). Chronic renal insufficiency(CRI) is common in patients with CHF who are candidates for CRT. However, theimpact of CRI on outcome of patients undergoing CRT is unknown. Methods: Todetermine this, we assessed renal function in patients undergoing CRT between1999 and 2005 at Mayo Clinic, Rochester, MN. Creatinine clearance (CrCl) was es-timated using the Cockgroft-Gault equation and renal dysfunction was defined asmild (CrCl # 60 ml/min) or severe (CrCl # 30 ml/min). Potential differences in out-come according to the severity of CRI were compared by Kaplan Meier survivalcurves. Results: A total of 307 patients (243 male, 79%) who underwent CRT deviceimplantation during the study period were included. Underlying heart disease was is-chemic in 199 (65%) and non- ischemic in 108 (35%). Mean ejection fraction was22% 6 8% which was not significantly different in patients with mild versus severeCRI (p 5 0.15). Initial implant was successful in all except 10 patients; proceduretime was not different between the groups (p 5 0.05). Survival according to degreeof CRI is shown. Conclusions: The presence of CRI in patients undergoing CRT isassociated with worse outcomes with mortality increasing directly with degree of re-nal dysfunction. Based on these findings, the presence and severity of CRI should beaccounted for in determining potential benefit of CRT.
Survival by Degree of Renal Dysfunction
CrCl n 1 year 2 years p value
$61 ml/min 116 90% 81% !0.01#60 ml/min 158 79% 69% !0.01#30 ml/min 38 60% 37% !0.01
312Rapid De-Adoption of Nesiritide Following Adverse Publicity: Insights froma Large National Hospital DatabasePaul J. Hauptman1, Jason Swindle1, Mark A. Schnitzler1, Thomas E. Burroughs1;1Department of Medicine, Saint Louis University, St. Louis, MO; 2Premier Inc
Background: The adoption of new therapies for heart failure has been extensivelystudied in the clinical trials setting and clinical care. However, little is known aboutthe impact on practice of studies that suggest a possible safety concern. Following thepublication of data suggesting potential adverse effects with nesiritide (Nes)(MareApr 2005), we hypothesized that there would be a rapid decrease in Nesand an increase in dobutamine (D), milrinone (M) and nitroglycerin (NTG) use.Methods: We used the ‘‘Prospective Comparative Database’’, a large U.S. hospitalclinical and economic database developed by Premier Healthcare Informatics Inc(Charlotte NC) for quality and utilization benchmarking, to evaluate drug utilizationin a nationally representative sample of 378 acute care hospitals for select primaryICD-9 diagnoses of CHF (398.91, 402.xx, 404.xx and 428.xx) in two ‘‘eras’’: Dec2004-Apr 2005 (n 5 110,818) and MayeSept 2005 (n 5 88,676), while evaluatingyear over year trends. Results: Use of Nes dropped significantly (Figure) after a peakof 17.9% of HF admissions in Mar 05 (p ! 0.0001); there was no concomitant in-crease in M, D or NTG use. However, among patients who received Nes or inotropeor both, the percentage on M or D increased (Table); a similar pattern exists for Nes,NTG or both. Comparing patients on Nes during the two eras, there were minorchanges in age distribution but not gender. Length of stay decreased in both Nesand M/D groups likely representing seasonal variations. Conclusions: The use of ne-siritide declined rapidly in response to dissemination of adverse data in recent pub-lications. No concomitant increase was seen with inotrope use but among patientsselected for vasoactive therapy, a greater percentage received inotropic drugs andNTG versus Nes over time. Further research is required to determine the durationof the effect and the impact on patient outcomes.
Nesiritide and Inotrope Use among Patients on Vasoactive Therapy
May 04eSep 04 Dec 04eApr 05 May 05eSep 05
Nesiritide 43.0 46.4 34.3Inotrope 44.2 40.5 56.1Both 12.8 13.1 9.6
S96 Journal of Cardiac Failure Vol. 12 No. 6 Suppl. 2006