Children's View Summer 2012
-
Upload
the-childrens-hospital-of-philadelphia -
Category
Documents
-
view
218 -
download
1
description
Transcript of Children's View Summer 2012

anniversary50thof theNICU
Sum
mer
201
2
A Lifesaving Journey for Twin Brothers
also inside
Children’s

Founded in 1855, The Children’s Hospital of Philadelphia is the birthplace of pediatric medicine in America. Throughout its history, a passionate spirit of innovation has driven this renowned institution to pursue scientific discovery, establish the highest standards of patient care, train future leaders in pediatrics and advocate for children’s health. A haven of hope for children and families worldwide, CHOP is a nonprofit charitable organization that relies on the generous support of its donors to continue to set the global standard for pediatric care.
ExEcutivE vP & chiEf DEvEloPmEnt officEr
Stuart Sullivan
AssistAnt vP, communicAtions & Donor rElAtions
Mark Turbiville
EDitor
Julie Sloane
WritErs
Sara Barton Louis Bell, M.D. Zan HaleMark Jolly-Van Bodegraven Eugene MyersAbny Santicola Jessa Stephens Tyler Weaver
PhotogrAPhy
Ed Cunicelli Kevin Monko Andy Todes
DEsign
SwivelStudios, Inc.
ProDuction
Kimberly Caulfield Nicole Keane
Birthdays are some of the happiest moments in childhood. This year, we at CHOP are celebrating a birthday of our own as the Harriet and Ronald Lassin Newborn/Infant Intensive Care Unit turns 50.
Today, we take for granted that hospitals have a special unit
dedicated to critically ill infants, but in the 1960s, N/IICUs
were a cutting-edge idea. CHOP was a pioneer in the field, and
through the decades our research has helped clinicians worldwide
learn how to better care for neonates. We are proud that our
Division of Neonatology is ranked among the best in the nation,
and hope you enjoy learning more about the N/IICU and its
patients in this issue.
As you flip through the pages, you might notice an updated
look for Children’s View. Please email [email protected],
and let us know what you think. As always, the magazine will
continue to bring you inspiring and touching stories of CHOP
patients like Xavier Ross (Page 16), Kyle and Andrew Malmstrom
(Page 18) and Steven Huang (Page 20).
Your contributions to Children’s Hospital keep us at the
forefront of pediatric medicine, allowing us to dive into new
research and start new clinical programs — as we did with the
N/IICU in 1962 — that help countless children.
Thank you for helping our patients celebrate many more
happy birthdays.
officErs
Mortimer J. BuckleyChairman
Mark Fishman Vice Chairman
Tristram C. Colket, Jr., R. Anderson Pew Honorary Vice Chairmen
Steven M. Altschuler, M.D. Chief Executive Officer
Aminta Hawkins Breaux, Ph.D. Secretary
Anthony A. Latini Treasurer
Thomas J. Todorow Assistant Treasurer
Jeffrey D. Kahn, Esq. General Counsel & Assistant Secretary
Margaret M. Jones Assistant Secretary
BoArD of trustEEs
N. Scott Adzick, M.D., M.M.M. • Steven M. Altschuler, M.D. • Clark Hooper Baruch • A. Lorris Betz, M.D., Ph.D. • Fred N. Biesecker •
Aminta Hawkins Breaux, Ph.D. • Mortimer J. Buckley • Stephen B. Burke • Dominic J. Caruso • Alan R. Cohen, M.D. • Tristram C. Colket, Jr. • Arthur Dantchik • Mark Denneen • Mark Fishman • Lynne L. Garbose, Esq. • Anthony A. Latini • James L. McCabe • John Milligan, C.P.A. • Asuka Nakahara • Jeffrey E. Perelman • R. Anderson Pew •
Gerald D. Quill • Daniel T. Roble • David B. Rubenstein • Anne Faulkner Schoemaker • Salem D. Shuchman • Binney Wietlisbach • Nancy Wolfson • Dirk E. Ziff
Ex-officio
Tami Benton, M.D. • David Cohen, M.D. • Jeffrey A. Fine, Psy.D. •
Kathleen Chavanu Gorman, M.S.N., R.N. • William J. Greeley, M.D., M.B.A. • Diego Jaramillo, M.D., M.P.H.
EmEritus
Leonard Abramson • Willard Boothby • Ruth M. Colket • Armin C. Frank • Peter C. Morse • George Reath Jr. • Stuart T. Saunders Jr., Esq. • Richard D. Wood Jr.
Steven M. Altschuler, M.D. Chief Executive Officer
© 2012 The Children’s Hospital of Philadelphia, All Rights Reserved.
the view from here
Children’s View is produced by The Children’s Hospital of Philadelphia Foundation.
commEnts AnD inquiriEs shoulD BE ADDrEssED to:
The Children’s Hospital of Philadelphia Foundation34th Street and Civic Center Boulevard Philadelphia, PA 19104-4399 [email protected]
For information about making a contribution to support CHOP, call 267-426-6500 or visit GiftofChildhood.org.
PrintED By
Children’s8
LLC

The rooftop Sea Garden opens at Children’s Seashore House.
2Today@CHOP CHOP’s travel TV show, teen driver safety advice and more
18Blood BrothersA twin-to-twin bone marrow transplant for aplastic anemia
20From China to CHOPA healthy start in America for a boy with Gaucher disease
22Volunteers in PhilanthropyA season of fabulous fundraising events
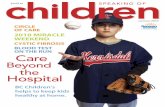
ON THE COVER: Anna, 2 months, in the N/IICU
Baby Steps, Big MilestonesThe Harriet and Ronald Lassin Newborn/Infant Intensive Care Unit celebrates its 50th anniversary.
First-time parents find hope for their baby’s heart at CHOP.
An artist-in-residence gives cancer patients a creative outlet.
Children’s
cover story

today@CHOP
Every Tuesday and Thursday, volunteer Justin Gelzhiser takes Children’s Hospital patients on a world tour. They’ve been to Japan, China, Brazil, Egypt, England, India, Namibia, Australia and Guatemala — without ever getting out of bed. Patients watch him on Galaxy 51, CHOP’s in-house TV channel, as he broadcasts from THE VOICE studio in the Colket Atrium.
“I love seeing the world come alive through a patient’s eyes,” says Gelzhiser, a graduate student at the University of Pennsylvania who has taught in elementary schools in Japan, South Africa and Costa Rica. “The places we ‘visit’ go from being abstract points on a map to tangible places they can experience.”
Gelzhiser often brings in international guests from each show’s featured country. They initially keep the country a secret — giving clues like showing the flag, teaching a few words in the native language or talking about the climate — and encourage patients to call in from their rooms with a guess. Once the mystery is solved, they share more information about that country’s music, customs, historical figures, sports and food and show any mementos they brought to the studio. Green screen technology, recently purchased thanks to a gift from Jacob and Kristina Brodie, will allow Gelzhiser and guests to superimpose themselves over images and video from around the globe.
“It’s fun,” says Gelzhiser, a high-energy 28-year-old who is a thesis away from a master’s degree in intercultural communication. “For me, it’s the best way to combine volunteering at CHOP, my previous international experiences and my studies at Penn into one platform.”
In one particularly ambitious show, Gelzhiser used Skype to beam the show live from China, where he was visiting. He walked the streets of rural Yunnan province in southern China with his laptop camera beaming the scenes back to Philadelphia as children called in questions from their beds at CHOP. “I want kids to feel like they leave their rooms and travel the world with me,” he says. —ZAN HALE
Around THE World IN 60 Minutes
Justin Gelzhiser (top, and above on-camera with Aungelee, 9, and Sean, 7) brings flags, international clothing and props like a lion-dog figurine from Okinawa, Japan (above right), and foreign currency (below). His show’s mascot, a Chinese plush turtle named Kame-chan (left), appears regularly.
2 | Children’s vIew | Summer 2012

today@CHOP
When Peter Barkman, full-time businessman and part-time drummer for the rock band Jung Wombats, looked out over the sea of teens and tweens in CHOP’s Main Café, he saw kids rocking out and having a good time.
At the Battle of the Bands, held the evening of March 29, patients could be just like any other kids — hanging out with friends, dancing to live music, cheering for their favorite bands. “It’s an opportunity for them to put whatever is ailing them on the shelf for a while and escape,” says Barkman, whose daughter Lauren was successfully treated at CHOP for acute
lymphoblastic leukemia. “Our goal is to take them on a musical journey.”
Jung Wombats was one of four bands and a solo act that competed that night. It’s Always Sunny in Sedation, a group of musical nurses, physicians and other staff, largely from the Sedation Unit, got together especially for this year’s Battle of the Bands. But it was Gypsy Wisdom, a Philadelphia cover band, that earned a trophy as the winning band. Then all the kids crowded onto the stage for the encore and joined in singing Adele’s “Set Fire to the Rain.” —ZAn HALe Above: Battle of the Bands’ patient-crafted trophies
my CHOP hero
“The first time we visited the endocrinology department at CHOP, my daughter’s growth was not even close to the ‘normal’ range and my husband and I were
very nervous. After a few minutes in the exam room, Dr. Alter walked in with a wide smile on his face and a Mickey Mouse tie around his neck.
He held out his hand and greeted my daughter. Instantly, all of our apprehension disappeared.
now, after many years of follow-up visits, we have gotten to know him and respect him even more. His methodical approach to my daughter’s treatment is what we admire the most. We know that his decisions are always made after careful thought, research and discussion. Although my daughter’s main concern is still wondering what tie Dr. Alter will be wearing that day!”
— S T e P H A n I e , M O T H e R O F M A D D y, 1 2
To honor a CHOP employee who has gone above and beyond for your family, go to giftofchildhood.org/myhero.
Craig Alter, M.D. PEDiAtric EnDocrinologist on choP fAculty sincE 1999
CHOP Teens Rock Out
Summer 2012 | Children’s vIew | 3

today@CHOP
Jessie Boyko’s cart is stocked with acrylics, tempera, watercolor, oils, crayons, pencils and metallic paper. On Mondays, she pushes it from room to room
in the oncology units at The Children’s Hospital of Philadelphia as its artist-in-residence.
She sits with patients from 3-year-olds to young adults. The kids talk about dragons, the beach, pets, hobbies, fishing, home. Boyko talks about textures, shapes, colors, printmaking, the great
artists. Nobody talks about cancer. Boyko, who has a master’s degree in fine
arts and teaches at Moore College of Art & Design, will spend up to two hours with each child. The time passes quickly as the kids escape into their imaginations and creativity. They laugh. They learn.
The Artist-in-Residence program is funded by LIVESTRONG, the Lance Armstrong Foundation, and a private donor. Since it began last year, it has brought joy to hundreds of cancer patients.
“The need and the want and the desire to create are there,” Boyko says. “Those hours of talking and working, those are moments where they’re able to be kids.” —SARA BARTON
4 | Children’s vIew | Summer 2012

kids in the hall
“What do you want to be when you grow up?”WE WAlkED thE hAlls of choP AnD AskED PAtiEnts thE sAmE quEstion:
To get to CHOP, the Gurungs traveled farther than most families — more than 7,000 miles. After 20 years in a Nepalese refugee camp, hoping to return to their home in
Bhutan, Shankar and Mani Kumari Gurung volunteered to resettle in the United States so that their three children, who were all born in the camp, could have better schooling and healthcare.
The Gurungs are three of the 70 children whom CHOP’s Refugee Health Program cared for in its first year. Seventy-five percent were Bhutanese, while others hailed from Burma, Iraq and Sudan.
The clinic screens the children and begins treatment for problems ranging from tuberculosis to parasitic infections to vitamin deficiencies.
“For many kids, this is their first real comprehensive physical,” says Mary Fabio, M.D., who is co-director of the program with Khoi Dang, M.D. “They have no concept of a primary care visit.”
Six months after arriving in the U.S., Shankar has a job and his older son and daughter are enjoying their new school and making friends. For medical care, they have been transitioned to CHOP’s Primary Care Center in South Philadelphia.
When the Gurung family is asked about their new life, an interpreter translates: “Whatever they have dreamed about Philadelphia, they have found that it is much better.” —EUGENE MYERS
Helping Refugees Start new Lives
Shankar and Mani Kumari Gurung (seated) with son Ajay, 14, daughter Deoki, 16, and son Seesom, 3
Summer 2012 | Children’s vIew | 5

What percentage of its waste does CHOP currently recycle?
A. 10%B. 29%C. 38%D. 55%
The total weight of CHOP’s 2011 recycling would equal how many 14-ton recycling trucks?
A. 25B. 52C. 73D. 113
How many pounds of card-board and paper are recy-cled at CHOP each month?
A. 79,000B. 92,000C. 116,000D. 137,000
Which of the following items are not recycled at CHOP?
A. DiapersB. Kitchen greaseC. Printer cartridgesD. Batteries
Each month, CHOP’s main cafeteria collects how many tons of food garbage for compost?
A. 1B. 2.5C. 3.5D. 4.5
—TYLER WEAVER
quiz
Ans
wer
s: 1
) D, 2
) D, 3
) C, 4
) A, 5
) D
142
53
Clean&GreenYou know CHOP is the best pediatric hospital — but did you know it’s also one of the greenest? Through its EcoCHOP sustainability program, the Hospital recycles items from 28 categories, everything from light bulbs to laptops. Before you recycle this magazine, see if you can answer the following questions:
When the sun is shining and the weather is warm, it’s no fun for kids to be stuck inside a hospital. So CHOP has brought the fun of playing outside to its patients with the new Sea Garden on the third-floor deck of Children’s Seashore House.
The Sea Garden is both fun and functional. It is a play space, a venue for physical and occupational therapy sessions and a place to rest and connect with nature, all designed with different ages and abilities in mind. A variety of programming will engage patients: Art therapists on the Child life team will
use the garden as inspiration. Various staff and volunteers will teach children about flowers, plants, nutrition and the environment. In the future, the garden may even provide food for children to sample.
Landscape designers at Groundswell Design Group in Hopewell, N.J., donated their services to create the Sea Garden, whose motto is “Hope Blooms Here,” and the Pennsylvania Horticultural Society will help maintain the garden. Many of the plants that fill the garden were also donated by local nurseries. – MARK JOLLY-VAN BODEGRAVEN
Hope Blooms
Here
For more information on the Sea Garden, please visit giftofchildhood.org/garden.
Pennsylvania Horticultural
Society project manager
Julie Snell helps Eoin, 4,
plant beans and lettuce.
6 | Children’s vIew | Summer 2012

To learn more about teen driving from the Center for Injury Research and Prevention, please visit teendriversource.org.
Louis Bell, M.D., chief of the Division of General Pediatrics at CHOP, explains the latest in medical thinking on an important topic: teen driver safety.
demonstrate that teens who say their parents monitor their driving have half the crash risk of teens with permissive parents who are less involved.
As an experienced adult driver, you must continue practicing with your teen in a variety of situations, even after he or she has a license. Gradually advance teen drivers from low-risk situations, such as familiar one-lane roads in the daytime, to higher-risk conditions like highways and night driving. As the teen demonstrates maturity and develops good judgment, allow him or her more driving privileges. CIRP also advises that teen drivers avoid riding with anyone other than experienced adults in their first six months behind the wheel, when they’re at their greatest risk of a crash. In my experience as a father of seven, the highest risk with brand-new drivers is driving with friends in unfamiliar areas.
Safe driving behavior is one of the most important health behaviors a teen can adopt. Teens don’t have to be in an accident to learn how to avoid one — they simply need to be prepared, in body and mind, to drive well.
With vacations upon us, many new teen drivers will be taking to the road, heading to summer jobs or hanging out with friends. Parents are right to be nervous: The highest lifetime risk of an accident happens when new drivers are behind the wheel without adult supervision. The good news is that there are many things a parent can do to keep teen drivers on course.
Cellphones, texting and distraction from passengers are rightly seen as risk factors for an accident, no matter what your age, but studies from my colleagues at CHOP’s Center for Injury Research and Prevention (CIRP) show that for teen drivers, something simpler is at the root of many accidents: inexperience.
Driving is complicated and requires higher order skills, which new drivers have to develop, such as scanning around the vehicle for hazards. Teens need a lot of supervised driving time with an adult, even after passing a driving test. And once they are driving on their own, it’s vital to set driving ground rules as a family — making clear these are for safety, not out of a desire to control the teen — and get buy-in from teens to follow them.
Passing the driving test doesn’t mean the teen is an experienced driver, says Flaura Winston, M.D., founder and scientific co-director of CIRP and an expert in teen driving safety. Her team found that teens have the lowest lifetime risk of being in a crash while driving with their parents and that families are not practicing for long enough and in enough situations to give teens a firm driving foundation. Families are important: Studies at CIRP, funded in large part by State Farm,
Protecting Teen Drivers
B Y L O U I S B E L L , M . D .
ask Dr. Bell
Passing the driving test doesn’t mean the teen is an experienced driver.
Summer 2012 | Children’s vIew | 7

Baby Steps,
Big Milestones
Celebrating 50 years of caring for our smallest patients
8 | Children’s vIew | Summer 2012

aring for a critically ill newborn
is a delicate balancing act. The
ventilators that deliver lifesaving
oxygen can damage fragile lungs.
The food necessary for growth can
harm a preemie’s digestive system.
The life-sustaining nutrients and
medication lines that feed into
an infant’s arms and legs create a
risk for infection. It’s a fine line
between “too much” and “not
enough” of anything in a tiny baby.
C. Everett Koop, M.D., and a nurse care for one of the first N/IICU babies in the 1960s.
Anna, 2 months, was the only survivor among premature triplets.
Many babies in the Harriet and Ronald Lassin Newborn/Infant Intensive
Care Unit were born too soon — some as early as 22 weeks, the very minimum
threshold for survival — while others have rare disorders or congenital
anomalies. As the N/IICU staff works to give them the best chance at a normal
life, the infants’ parents endure weeks and months of waiting, worrying, hoping.
This year marks the 50th anniversary of the N/IICU, and it has come a long
way since CHOP Surgeon-in-Chief C. Everett Koop, M.D., opened the one-
room, 12-bed unit in 1962. Today it can house as many as 83 infants at a time
— around 1,200 a year — with a range of lifesaving technologies unimaginable
in the 1960s.
CHOP’s Division of Neonatology is ranked among the best in the nation
and, accordingly, its N/IICU draws the very sickest babies from around the
region. Aside from the 15 percent who were diagnosed with birth defects
prenatally and born in CHOP’s Garbose Family Special Delivery Unit, the
babies are all transported from other hospitals. To the credit of the 35 attending
physicians, 307 nurses and 63 other staff, the vast majority of them survive.
“Many nurseries can take care of a preterm baby just fine, but when there
criti
is a delicate ba
ventilators
B Y J U L I E S L O A N E
cover story
Summer 2012 | Children’s vIew | 9

A group of surgeons, doctors and nurses hovered around Katelyn Farrell, a day-old newborn who was
barely clinging to life, working quickly to
hook her up to the contraption they hoped
would save her. As the girl’s condition
worsened, the lead surgeon made the final
connections and switched on the machine.
A great cheer went up as Katelyn’s skin
went from sickly purple to healthy pink.
Katelyn was out of immediate danger
and the ECMO program at CHOP had
officially begun.
On May 8, 1990, Katelyn became
the first baby at Children’s Hospital to
benefit from Extracorporeal Membrane
Oxygenation (ECMO), a machine that
essentially does the work of the heart and
lungs when the baby’s own are failing. It is
one of the key technologies that has helped
improve the care of gravely ill newborns
over the last 20 years.
“What is that? What are they doing?”
Michele Rupert wondered when she
first saw her little girl amid a frightening
network of tubes and wires, surrounded
by doctors and machinery. But Michele
trusted that her baby was in good hands.
At the time, ECMO was a relatively
new therapy; it had only been approved at
CHOP a month before Katelyn’s arrival.
Today, nearly 1,000 children have received
ECMO at CHOP — about 50 each
year — making it one of the most active
programs in the country.
For many babies like Katelyn, who was
rushed to CHOP within hours of birth
for surgery to correct a congenital defect,
ECMO is the last hope for survival. It isn’t
a cure but a temporary measure to bypass
the heart and lungs, allowing them to rest,
recover and strengthen.
It worked for Katelyn. Within a couple
of days, she had stabilized enough to be
taken off ECMO, and she went home
within a month. Michele remembers it as
the most stressful time of her life, but today
her daughter shrugs it off.
Though Katelyn remembers nothing
of her ordeal, she has embarked on a career
helping children too, working in day care
while she earns a teaching degree. “She’s
amazing now, a typical 21-year-old,”
says her mom. —EUGENE MYERS
are complications, they send the babies
to CHOP,” says Phyllis Dennery, M.D.,
division chief of Neonatology. “We have
all the pediatric subspecialties and
specialized technologies that allow us
to take care to the next level.”
Bill Fox, M.D., was hired in 1973 as
one of the first neonatologists at CHOP
and is still with the N/IICU today. The
care is constantly improving, he says,
because the staff is encouraged to debate
and discuss each patient’s case.
“Many of our babies have such
complicated problems that there’s no rule
book for how to treat them,” he says.
A Pioneering Neonate Turns 21
40-year N/IICU veteran Bill Fox, M.D.
Liam, 6 months (top); Cailin Connelly, R.N., herself once a CHOP N/IICU patient, helps Jaden, 3 months, and his mother (bottom).
Katelyn as an infant with her mother and uncle (left and center), and today (right).
10 | Children’s vIew | Summer 2012

cover story
CHOP’s Smallest PatientLittle Myla weighs less than 3 pounds. As she lies sleeping
in her incubator in CHOP’s N/IICU, a respirator and cardiac
monitor whir and light up her otherwise dark, cocoon-like room.
Stickers on her chest and wrists monitor her heart rate, breathing
rate and oxygen, and there is an IV to feed her. When her
mother strokes her tiny hand and murmurs, “My miracle baby,”
Myla stirs, acknowledging her familiar sound and touch. It’s an
emotional moment for a family that has been through so much.
In February, Myla and her twin brother, Jules, were born at
Pennsylvania Hospital after 23 weeks of gestation, little more
than halfway through a typical pregnancy. Each about the size
of an adult hand, they weighed less than 2 pounds combined.
Their skin was thinner than tissue paper and their inner organs
even more fragile.
“The likelihood of survival of babies born at such a degree
of prematurity is less than 20 percent,” says Kelly Wade, M.D.,
Ph.D., CHOP attending neonatologist.
Wade and the other CHOP physicians who operate
Pennsylvania Hospital’s Newborn Care immediately placed them
on life support and tried every possible medical intervention.
But only six days after birth, Jules passed away. A day later, Myla
took a turn for the worse. An infection
in her delicate intestine swelled her
stomach like a balloon. The neonatal
surgical team at CHOP was her only
hope for survival.
When Myla was transported to
CHOP, she was the smallest baby in the
N/IICU. Five days later she underwent
surgery. A second surgery is now needed,
but surgeons feel the risks are too high at her small size. So the
N/IICU and surgical team — and her family — wait and hope
for her to grow stronger.
The neonatal team has supported the family every step of the
way. The team put together a scrapbook dedicated to Jules, and
they’ve encouraged the family to be equal partners in Myla’s care.
Her mother, Stacey, a registered nurse, has been able to stay in
one of the N/IICU’s overnight sleep rooms every night, and she
assists the care team in whatever way she can.
A month after Myla was born, Stacey was finally able to hold
her for the first time.
“Now I get to kiss her head,” she says. “I like that part. It’s the
best thing in life.” —ABNY SANTICOLA
“Having a whole team of experienced neonatologists weighing
in on every patient makes the care that much better.”
The nurse-to-patient ratio in the N/IICU is 1-to-2 or
even 1-to-1, ensuring that there is always a watchful eye on
the infants’ precarious health. It also gives nurses a special
bond with many families.
“Many of our babies have such complicated problems that there’s
no rule book for how to treat them.”
CONTINUED ON PAGE 14
Mom Stacey Julien keeps watch over Myla, 2 months.
Summer 2012 | Children’s vIew | 11

In her red-and-white polka-dot dress, 3-year-old Isabella Schneeman elicits more than
one “awww” from strangers as she smiles for the
camera outside the N/IICU. A flesh-colored
bandage covers a small opening in her throat,
the only visible reminder of all that Isabella went
through in her time behind its doors.
Born at 25 weeks near their home in
Clayton, N.J., Isabella and her twin sister,
Brooke, struggled to breathe, their airways not
yet fully developed. When the babies’ health
worsened, their parents, Libby and David,
knew exactly where to take them — Libby has
been an ultrasound technician at CHOP for
nine years.
Sadly, as CHOP transport came to get
the twins in August 2008, Brooke passed
away. Doctors in CHOP’s Neonatal Airway
Program worried about Isabella’s airway; she
relied completely on a ventilator to stay alive.
There are plenty of chairs at VMS Movement Specialists, a Newtown, Pa., gym their parents own, but identical twins Savion and Savaughn, 11, would rather squeeze side-by-side in the same chair than sit separately. As they sit and
read, you can only tell them apart because Savaughn
is about three inches shorter and has a four-inch scar
across his stomach — a reminder of the miracle that
they are both here, together, and healthy today.
In 2000, their father, Vaughn Hebron, retired from
the NFL. He’d been a fan favorite on the Philadelphia
Eagles and earned two Super Bowl rings in Denver,
where he was the Broncos’ all-time leading kick-
returner. He was about to start work as an analyst on
Comcast’s “Postgame Live” show when he and his
wife, Kim, learned they would be having twins.
At five months, when most parents discover their
baby’s sex, the Hebrons were instead dealt a blow. Tests
revealed the babies had a life-threatening condition
called twin-twin transfusion syndrome (TTTS), in
which one twin gets too much blood, oxygen and
nutrients, while the other twin doesn’t get enough.
“They told us there was a 70 percent chance one or
both wouldn’t make it,” says Vaughn.
At 32 weeks, one twin’s heart rate became
erratic, and doctors at their local hospital ordered
an emergency c-section. Savion weighed 3 pounds,
7 ounces, and Savaughn, just 2 pounds, 9 ounces.
By evening, Savaughn’s skin had turned ashen and
his stomach was distended. Unsure of the problem,
doctors advised the couple to send him to CHOP.
“They gave me a Polaroid of Savaughn and said
I should say goodbye,” remembers Kim with tears
in her eyes.
Saving Savaughn
and LaughingRunning
“They gave me a Polaroid of Savaughn and said I should say goodbye.”
Isabella, 3
12 | Children’s vIew | Summer 2012

cover story
Her parents hoped to avoid a tracheostomy, an incision in the throat to make a new airway, which requires years of constant monitoring and suctioning to keep the airway clear and prevents the child from speaking.
The following December, Isabella managed to dislodge her own breathing tube. Doctors kept her alive with chest compressions as they worked to replace it. They succeeded, but only with great difficulty. Isabella’s airway was critical: underdeveloped, scarred and collapsing. A tracheostomy was now her only option.
Ian Jacobs, M.D., surgical director of the Neonatal Airway Program, and neonatologist Janet Lioy, M.D., planned the procedure before Jacobs operated.
Isabella went home for the first time in March 2009, with a ventilator to force air through her tracheostomy into her lungs to
Watching her run and laugh, you would never know how desperately she once struggled for air.
ensure that she would get enough oxygen.“I never thought about it as something
unusual,” Libby says. “She was our firstborn and she came with all this equipment, just something we loaded up in the car to take her to Target or to the zoo.”
CHOP’s Home Ventilation Program made monthly visits to the Schneemans’ home to check on Isabella’s breathing equipment and provided support around the clock. Her doctors closely monitored her tracheostomy and growing airway.
Jacobs surgically reconstructed Isabella’s throat last June, and her tracheostomy tube was removed in September. She is eating, growing and singing like any other little girl. Watching her run and laugh, you would never know how desperately she once struggled for air.
“She’s running out of the N/IICU,” says Libby, smiling. “That’s awfully appropriate.” —eUGene MyeRS
and Laughing
At CHOP, Savaughn was diagnosed with necrotizing enterocolitis, a condition not uncommon in premature infants where portions of bowel tissue decay. CHOP surgeons immediately removed three inches of his intestine. The procedure was a success.
Vaughn was at Savaughn’s side in the N/IICU every day for the next three months of recovery. “I’d go from CHOP to the studio, tape ‘Postgame Live,’ then go back to CHOP,” he says. “You’re going through this time of trauma, and they made it so comfortable, so easy. I’d come in, and it felt like I was coming into the locker room. It was like a second home.”
“The nurses in the N/IICU were amazing,” says Kim. “They dotted every i and crossed every t, leaving nothing to question. They were so good to us, and for Savaughn to come home healthy, all I can feel is blessed.”
Finished reading now, the boys run around the gym. Savion pretends to box; Savaughn does a pullup. They breakdance to a song only they seem to hear.
“They’re quite the characters,” says Kim, “but they love to be together. It’s amazing to watch.” —MARk TURBIvILLe
“They gave me a Polaroid of Savaughn and said I should say goodbye.”
OPPOSITe: The twins at 7 months
(top) and vaughn and newborn
Savaughn in the n/IICU (bottom)
THIS PAGe: vaughn and kim
Hebron with identical twins
Savaughn (left) and Savion, 11
Isabella at 12 months and as a newborn (below)
Summer 2012 | Children’s vIew | 13

cover story
“When the babies come to the N/IICU, we always tell
the parents their course is going to be like a roller coaster,”
says Peggy Nelson, R.N.C., who has been caring for CHOP’s
infant patients for 33 years. “We encourage them to take it
one day at a time.”
To help these families, a psychosocial program supported
by the Neubauer Family Foundation helps parents bond with
their children and keep spirits up through months of stressful
uncertainty.
Many of the N/IICU’s physicians, including Dennery and
Fox, are also researchers, studying areas such as the long-term
consequences of being born premature, less-damaging ways
CONTINUED FROM PAGE 11
The original N/IICU in the early 1970s
Division Chief Phyllis Dennery, M.D., examines Keith, 7 months.
Encouraging Family BondingThinking back on her daughter Charlotte’s three-month stay in the N/IICU, Lindsay Groff recalls how powerless she felt. “You feel
like the doctors and nurses are helping to heal her, but
you’re just sitting there, helplessly looking at your sick
baby,” she remembers.
A routine ultrasound before birth diagnosed
Charlotte with giant omphalocele, a life-threatening
condition in which her abdominal organs were
outside of her body. The team at CHOP’s Center
for Fetal Diagnosis and Treatment prepared Lindsay
for what the diagnosis meant: Immediately after
birth, Charlotte would quickly be whisked away to
undergo the first of many surgeries, and she would
be in the N/IICU for weeks, until all of her surgical
wounds healed.
The news was devastating. But the team gave her
hope and worked to involve her in Charlotte’s care.
From the start, the nurses, doctors and lactation
consultants encouraged Lindsay to breastfeed as a
way to help Charlotte grow stronger.
“Breast milk is optimal nutrition for the baby,
especially babies with gastrointestinal problems,”
says Rosario Wessner, R.N.C., N/IICU nurse and
Breastfeeding Committee chair, who leads a breast
pumping support group at CHOP. “We use breast
milk as a kind of medical intervention, and at the
same time it allows families to contribute to their
to deliver oxygen and the effect of light on neonates.
In fact, CHOP has long been at the forefront of
neonatology; the modern incubator, the Isolette, was
invented at CHOP in 1938 and stood for 50 years as
the industry standard.
CHOP’s neonatologists are also great collaborators.
Many of the division’s programs, such as the Newborn
and Infant Chronic Lung Disease Program and
Neonatal Airway Program, incorporate staff from
Pulmonary Medicine, Otolaryngology, Rehabilitation
and Surgery. Over the decades, the division’s expert
neonatologists also have branched out to other local
14 | Children’s vIew | Summer 2012

After three weeks in the N/IICU, when Charlotte
was finally stable enough to be held, the N/IICU team taught Lindsay
“kangaroo care,” which promotes mother-child bonding through skin-to-skin contact.
Luna, 2 weeks
baby’s care and recovery.”
Immediately after Charlotte was delivered
in CHOP’s Garbose Family Special Delivery
Unit, Lindsay began pumping her breast milk
as instructed. Over the next few weeks, as
Charlotte underwent a total of seven surgeries
to repair her birth defect, the N/IICU team
encouraged Lindsay to clean Charlotte’s mouth
with a cotton swab dipped in breast milk, which
carries antibodies that would absorb through
the baby’s oral cavity and make her stronger.
After three weeks in the N/IICU, when
Charlotte was finally stable enough to be held,
the N/IICU team taught Lindsay “kangaroo
care,” which promotes mother-child bonding
through skin-to-skin contact. When Charlotte
finally breastfed for the first time, N/IICU
team members cheered and high-fived to
celebrate such an important milestone.
“They were genuinely as excited about
Charlotte’s eating as our family was,” Lindsay
says, holding back tears. “I’ll never forget that.”
Now almost 2, Charlotte is a healthy
toddler, and Lindsay credits the neonatal team
that supported her with her incredible recovery.
“Most people don’t realize that she was
ever sick,” says her mom. “The support of the
N/IICU staff during the process was so critical,
and I know that it helped her thrive. We are
forever grateful to CHOP.” —ABNY SANTICOLA
hospitals. Today, CHOP Newborn Care runs the
intensive care nurseries at 12 local hospitals, including
the Hospital of the University of Pennsylvania.
The patients never remember their neonatologists,
but the staff loves when they return years later.
“You can’t believe it’s the same person,” says
Dennery. “They were a vulnerable little baby, and then
they come back as a grown person who can talk and
who’s really vibrant. It’s such a wonderful feeling.”
To support the N/IICU and its lifesaving work, please visit giftofchildhood.org/supportNICU.
Charlotte, 1 month, and Lindsay practice kangaroo care (above left). Mother and daughter today (right).
Summer 2012 | Children’s vIew | 15

B Y J E S S A S T E P H E N S
First-time parents
find hope for their
baby’s heart at CHOP
16 | Children’s vIew | Summer 2012

jackie Ross was 20 weeks pregnant with her first child when she and her husband, Nate, received the devastating news: The baby they already loved so dearly would be born with half a heart.
“I saw it as a death sentence,” Jackie says. “We went through
all the stages of mourning.”
But as she and Nate learned more about their son’s condition,
hypoplastic left heart syndrome (HLHS), they found that they
had options — good ones. And when they watched a video about
CHOP’s Fetal Heart Program, which cares for babies with heart
defects while they are still in the womb, Jackie says, “We finally
realized that this might all be OK.”
Though the couple had the option of going to a top hospital in
New York City, they chose CHOP’s Cardiac Center because of its
team’s expertise in treating babies with HLHS, a serious heart defect
in which the left side of the heart is underdeveloped. And they were
thrilled to learn that Jackie could deliver in the Hospital’s Garbose
Family Special Delivery Unit (SDU), so she would be just down
the hall from her son as he awaited his first open-heart surgery.
“As soon as we walked into the SDU,” Jackie remembers,
“I said, ‘This is exactly where we’re supposed to be.’”
Xavier Thomas Ross was born in the SDU on May 28, 2011.
“It was amazing,” Jackie says. “My biggest fear was that it wasn’t
going to be like ‘real’ labor because of his heart. But they did
everything they could to make it as normal as possible.” Jackie and
Nate spent hours cuddling and rocking Xavier. Their families visited.
Four days later, Xavier was wheeled to the operating room where
J. William Gaynor, M.D., performed the Norwood procedure, the
first of the three incredibly complex surgeries required to reconstruct
Xavier’s tiny heart. When the surgeries are completed, the right side
of Xavier’s heart will be able to pump oxygenated blood to his body
— a job normally done by the left side. He will face many challenges,
but he is expected to live a full and happy life.
Thirty years ago, his future wouldn’t have been nearly as bright. At
that time, many children with heart defects like Xavier’s died within
days of birth. “We were basically trying to get the kids to survive —
period,” says Gil Wernovsky, M.D., Xavier’s cardiologist at CHOP.
“Now, care has advanced to the point that the vast majority of these
patients survive, and we’re focused
on making sure they have a good
quality of life as they grow up.”
Xavier’s surgery went well,
and after a month at CHOP, he
went home. It was a joyous but
nerve-racking time for Jackie and
Nate. Xavier needed constant
care: changing his feeding tube,
monitoring his oxygen levels,
weighing him every other day,
tracking every milliliter he ate. It
was exhausting. And it was very
serious work, because babies with
HLHS are at especially high risk
for complications during the time
between their first and second
surgeries. It helped that a nurse
practitioner from the Cardiac Center called Jackie and Nate every
week to track Xavier’s progress and was always available to answer
their questions. They had also taken several classes at CHOP to
learn how to care for their fragile baby. “I really think that was
why he did so well at home,” Jackie says. “I was so prepared.”
Honoring Xavier’s “heart journey” is now a huge part of his
parents’ lives. To raise awareness about congenital heart disease, Jackie
wears a pendant in the shape of a bandaged, broken heart, and Nate
appeared on the TV show “NY Ink” to get a tattoo in honor of his
son. As for Xavier, he had his second open-heart surgery at CHOP
in October, and he’ll have his third sometime in the next few years.
For now, though, this always-smiling survivor is focused on the
things he loves most in life: eating, playing with toys, taking baths
and going for rides in the car. And during a recent trip to Florida,
he experienced many new things. He went to the beach. He went
to the zoo. And, for the very first time, he started waving hello.
Honoring Xavier’s “heart journey” is now a huge part of his parents’ lives.
OPPOSITE: Xavier is all smiles at 10 months.
LEFT: Nate’s tattoo honors his son’s journey
(top); Jackie holds Xavier, whose onesie
shows a sense of humor (bottom).
To learn what you can do to help kids like Xavier, please visit giftofchildhood.org/supportcardiac.
Summer 2012 | Children’s vIew | 17

Kyle and Andrew Malmstrom are as close as two brothers can be. The twin 12-year-old boys do everything together. They have the same blond hair and impish smiles, but genetic testing to see if they truly were identical never seemed important — until Kyle noticed purple dots on his skin last September.
Kyle’s pediatrician told his parents, Kim and Mike, to take him to CHOP immediately, so they drove an hour from their home in Spring City, Pa., to the Emergency Department. “The triage nurses took one look at Kyle and put us immediately into isolation,” Kim says. “Within the hour, hematologists were getting blood work done.”
That blood work revealed that Kyle’s platelet count was only 4,000; the normal range is 150,000 to 450,000. After two bone marrow biopsies, Kyle’s doctors diagnosed him with a severe form of aplastic anemia, a condition so rare it affects only two out of every million people. It meant that Kyle’s bone marrow was no longer making new red and white blood cells and platelets.
“It’s as if the workers have left and you have an empty factory,” explains Nancy Bunin, M.D., director of the Bone Marrow Transplant Program at CHOP. “Red blood cells typically last for two months. Platelets last six days, and white blood cells last only one day. Without a constant supply of them, you’re at risk for infection, bleeding and developing potentially life-threatening heart problems.”
AndrewBrothersBlood B y
e U G e n e
M y e R S
A bone marrow transplant from one twin saves his brother’s life
18 | Children’s vIew | Summer 2012

Kyle
Kyle’s best option was a bone marrow transplant from a sibling
donor. The odds of an exact sibling match are only 25 percent, but
Kyle was very lucky. He had two: his older sister, Amanda, and
Andrew. Doctors ultimately chose Andrew and confirmed that
the two boys are genetically identical. “I always knew we were!”
insisted Kyle.
As an identical twin, Andrew’s fully compatible bone marrow
significantly increased the likelihood to better than 95 percent
that a transplant would cure Kyle. Andrew was nervous about the
procedure but willing to do whatever it took to get Kyle back
to normal.
The transplant, performed in October, was CHOP’s first between
twins for aplastic anemia, though twin transplants have been done
at CHOP in the past to treat leukemia. In a 90-minute surgical
procedure, Andrew was placed under general anesthesia while
doctors used a special needle to remove a small amount of liquid
marrow from his hip bone. For his sacrifice, Andrew suffered nausea
from medication and endured two weeks of soreness — a small price
to pay for saving his brother’s life.
OPPOSITE: Kyle prepares to receive the infusion of Andrew’s bone marrow
(top). The brothers cheer on the Flyers during Kyle’s hospital stay (middle).
Healthy post-transplant, the twins with their mother, Kim (bottom).
To Kyle, the transplant seemed no different than the weekly
platelet infusions he had been getting: After receiving chemotherapy
to prepare his body for the transplant, an IV in his arm delivered
Andrew’s donated marrow to his blood.
The healthy marrow migrated into Kyle’s bones, which soon
began producing healthy blood cells again. He returned to school
in April, ending more than seven months of near total isolation
from the public — a difficult time for twin brothers who are usually
inseparable. But Kyle made the most of it: He became a master bingo
player and learned to play guitar through the Music Therapy Program
during his month at CHOP.
And now that Kyle’s doing well, he and his family have been
focusing their energy on making “quillows,” quilts that fold into
pillows, to donate to other bone marrow transplant patients at
CHOP. Kyle wants the kids there to have the same comforts of
home that he had at the Hospital, and to give them the hope of
getting better like him.
“We sew strength, courage and hope into each stitch, from
one survivor to another,” Kyle says.
Kyle’s doctors diagnosed him with a severe form of aplastic anemia,
a condition so rare it affects only two out of every million people.
For more about the Malmstrom brothers, please visit childrensview.org.
Summer 2012 | Children’s vIew | 19

ChinaCHOP
AFTER A DIAGNOSIS OF GAUCHER DISEASE,
STEVEN HUANG STARTS A HEALTHY NEW LIFE
B Y J U L I E S L O A N E
from
to
20 | Children’s vIew | Summer 2012

During Steven’s two- to three-hour infusions, they read books and color. Steven declares his favorite color to be “red blue purple turquoise hot pink.”
OPPOSITE:
Diana and Steven Huang
(center); genetic counselor
Sara Chadwick, M.S., M.P.H.
(left), and Paige Kaplan,
M.B.B.Ch. (inset)
THIS PAGE:
Steven receives
his infusion in CHOP’s
Day Medicine clinic.To read the story of Amber Mickley, another child living with Gaucher disease, visit childrensview.org.
The local doctor in his native Fuzhou, China, couldn’t make
a diagnosis but wanted to remove Steven’s spleen. From her
home in Phoenixville, Pa., Steven’s aunt, Diana Huang,
shook her head. This was not right. She flew to China and
took Steven to a hospital in Hong Kong, where she first
heard the words: Gaucher disease.
Gaucher (pronounced “go-SHAY”) is a rare genetic
disease that affects the lysosomes, the cells’ garbage
recyclers. Gaucher causes an enzyme deficiency that
blocks the lysosomes from working properly, leading
to symptoms like painful and brittle bones, enlarged
liver and spleen, extreme fatigue and easy bleeding.
Since 1991, the disease has been treatable with regular
enzyme replacement therapy — which can prevent
nearly all symptoms if taken before permanent bone
damage sets in — but the medication is not readily
available in much of Asia.
Steven’s family didn’t need any more bad news.
Steven’s mother and grandmother both had been
recently diagnosed with cancer, and his grandfather
had passed away. With nobody healthy to care for
Steven, Diana had already begun the process to adopt
her nephew, whom she had met only twice. Now, this
diagnosis brought added urgency. In America, Steven
could get medical treatment.
Diana spent eight months running Steven all over
Asia — to Taiwan, to South Korea … wherever she
could locate the enzyme, which cost the family $10,000
a month.
It was a relief when Diana learned that 45 minutes
from her home, the Lysosomal Disease Center at The
Children’s Hospital of Philadelphia offers one of the
nation’s strongest programs to treat Gaucher disease.
(In fact, as the only program in the region, it treats
both children and adults.) By email, Diana began working
with Center Director Paige Kaplan, M.B.B.Ch., on Steven’s
treatment plan.
After 22 months, the adoption became official, and on July
27, 2011, Steven and his aunt arrived in the U.S. Five days
later, he had his first appointment at CHOP. Until he could
be covered by Diana’s health insurance, Genzyme donated
his medication. Genzyme has also been a great supporter of
the Lysosomal Disease Center and Kaplan’s team, physicians
Jaya Ganesh, M.B.B.S., M.D., and Can Ficicioglu, M.D.,
Ph.D., and genetic counselors Kristi Fitzgerald, M.S., C.G.C.,
Sara Chadwick, M.S., M.P.H., and Colleen Clarke, M.S. The
company has given more than $2 million to date to support
education, research and fellowships on metabolic disease at CHOP.
Over the next five months, Steven had more than 40
appointments at CHOP and received enzyme infusions every
two weeks. He has responded beautifully. Steven’s spleen has
reduced in size by half, his nose rarely bleeds and he can walk
without falling. He has grown several inches and his bone
density is improving.
Unfortunately, Steven has type 3 Gaucher disease, a less
common, more severe form that could damage his brain.
It is a devastating problem that could show up at any age —
or never. So far, he shows no neurologic problems and has
wowed Kaplan with his intellect. After three months in the
U.S., Steven completely switched to speaking English; within
eight months — at the age of 4 — he began to read.
Kaplan hopes that a new medication with molecules small
enough to reach the brain, currently in trials at Genzyme, will
become available before Steven shows neurologic problems. The
doctor smiles warmly as she looks over at Diana and her nephew
playing. “She’s so good with him. His progress is really amazing.”
During Steven’s two- to three-hour infusions, they read
books and color. Steven declares his favorite color crayon to
be “red blue purple turquoise hot pink.”
On a recent call to his mother in China, Steven even
offered advice. “He picked up the phone and shouted,
‘Fight cancer!’” Diana says, laughing. “My sister knows her
son is in good care now, and it lets her focus on her health.
I’m so glad CHOP is taking care of him now. He is doing
so well and growing up so fast.”
At the age of 2, Steven Huang’s belly started growing bigger and bigger. His nose bled constantly. When not exhausted, he would stumble around and fall as if drunk.
Summer 2012 | Children’s vIew | 21

SIGNATURE EVENTSvolunteers in philanthropy
On March 31, more than 140 volunteers, Trustees and CHOP leaders gathered for the second annual Volunteer Leadership Summit. The daylong event featured inspiring stories from patients and volunteers and provided attendees with the opportunity to meet, exchange ideas and celebrate everything they do to support the Hospital. Trustee Anne Faulkner Schoemaker presented the 2012 HOPE Award for Distinguished Volunteer Service to Darlene Logan and Judith Royal for their dedication and tireless support of the Sickle Cell Center and the annual Blue Tag Gala.
On April 22, the Philadelphia Eagles and CHOP teamed up to host the third annual Huddle Up for Autism Family Fun and Awareness Day at Lincoln Financial Field. The day drew 5,000 participants and raised $75,000 for the Center for Autism Research.
The fifth annual Childhood Friends Wine Tasting, hosted by Philadelphia magazine with support from PA Wine & Spirits Stores and the Lubert Family Foundation, was held on April 19 at Tendenza in Philadelphia and raised more than $32,000 for programs at CHOP.
On May 3, the Daisy Day Luncheon and Fashion Show, the largest annual fundraising event for CHOP, was held at the Hyatt at the Bellevue in Philadelphia. Honorary co-chairs of the event were Helaine and Joseph Banner and Nancy and James Minnick, and the Annenberg Foundation was a presenting sponsor. The event featured keynote speeches from neurosurgeon Phillip Storm, M.D., and neurosurgery patients Jennifer Minnick and Jason Banner. Keren Craig, co-founder of Marchesa, presented the Marchesa Fall 2012 collection, sponsored by Saks Fifth Avenue. This year's event raised more than $1.5 million to benefit the Division of Neurosurgery at CHOP.
VOLUNTEER LEADERSHIP
SUMMIT56TH ANNUAL DAISY DAY LUNCHEON & FASHION SHOW
AYY
HUDDLE UP for AUTISM
CHILDHOOD FRIE NDS WINE TASTING & RECE PTION
22 | Children’s vIew | Summer 2012

COMMUNITY EVENTS WINTER 2011-2012volunteers in philanthropy
MC
MA
STE
RS
PH
OTO
GR
AP
HY
1 FRIENDS OF CELI Jan. 27 Knowlton Mansion, Philadelphia The third annual dinner raised $24,000 for the Center for Autism Research.
2 EAISE FAMILY FOUNDATION RALLY FOR RESEARCH
Feb. 3 Adelphia Grand Ballroom, Deptford, N.J. The buffet dinner and basket auction raised $35,000 for brain tumor research.
3 TWEETHEART SOCIAL
Feb. 11 NEST, Philadelphia The family fun day raised nearly $3,000 to support programs at CHOP and featured pizza making by Chef Marc Vetri.
4 HEART WEEK
Feb. 13–17 Richard L. Rice Elementary School, Marlton, N.J. The weeklong school fundraiser collected more than $1,000 to support the Heart Transplantation Program.
5 SUNOCO BALLOON CAMPAIGN
March 1–31 Participating Sunoco locations
Sunoco and its customers raised more than $25,000 to benefit Children’s Miracle Network at CHOP.
6 ENTERPRISE HOLDINGS FOUNDATION CHECK PRESENTATION March 5 Springfield Country Club, Springfield, Pa. At the Credit Unions for Kids chapter meeting, the Enterprise Holdings Foundation presented a check for $5,000 to Children’s Miracle Network at CHOP.
7 ANJALI POWER YOGA KARMA CLASS
March 17 Anjali Power Yoga, Westmont, N.J. Clancey Carle and Cheryl Cucinotta hosted
a karma yoga class to collect art supplies and donations for the Child Life, Education and Creative Arts Therapy department.
8 SEVENTH ANNUAL MIRIAM QUIGLEY DANCE-A-THON March 17 St. Katharine of Siena Gym, Wayne, Pa. The Miriam’s Kids Research Foundation brought 650 people together to raise $35,000 for pediatric brain tumor research.
9 SKATE OFF FOR BRENDAN DIXON
March 23 The Skatium, Havertown, Pa.
The ice-skating event raised more than $14,000 to benefit the Center for Pediatric Eosinophilic Disorders at CHOP.
10 FRANKFORD CANDY’S SPARE SOME TIME FOR CHARITY
March 28 North Bowl, Philadelphia
The bowling event raised $11,000 for CHOP.
1
2 3
4
7
5
8
6
9 10
Summer 2012 | Children’s vIew | 23

UPCOMING EVENTSvolunteers in philanthropy
For details on upcoming events, go toRegister your event with The Children’s Hospital of Philadelphia Foundation at GiftofChildhood.org or contact the Community Fundraising team at [email protected] or 267-426-6496. We can help you get started and make sure your event is listed on our website.
Planning a CHOP Fundraiser?
Hope to see
you there!
Sunday, Oct. 7, 2012 10 a.m. Villanova University Stadium www.giftofchildhood.org/buddywalk
Come out and join the fun with Honorary Chairs Cliff and Kristen Lee! Sunday, Sept. 30, 2012
Fabulous prizes Fantastic post-race buffet Fun activities for the kids Race begins at 8:30 a.m.
www.parkwayrun.org
24 | Children’s vIew | Summer 2012

Gift of Childhood.org/plannedgiving
Many of the most important and enduring gifts to CHOP have been legacy gifts.
Including Children’s Hospital in your will, or as a beneficiary of a retirement plan, is one of the easiest ways to invest in the health and well-being of future generations of children. These gifts won’t affect your current cash flow and may even help reduce taxes for loved ones.
If you have already made a planned gift to CHOP, thank you, and please let us know. We can help you designate your gift to a specific Hospital program, and we’ll invite you to join the Lewis Society, a select group of supporters who have included Children’s Hospital in their plans.
Visit us at giftofchildhood.org/plannedgiving to learn more, or contact Tom Yates, director of planned giving, at 267-426-6472 or [email protected].
Let Your Legacy Be the Gift of Childhood
Our care, our research, our teaching. They all rely on gifts from Children’s Hospital supporters, now and in the future.
EdieAge 2 | Oncology
sunday, oct. 7, 2012 • 10 a.m. • villanova university stadium • www.giftofchildhood.org/buddywalk

NameAge ? | Oncology
BreannaAge 9 | Oncology
Please recycle. Children’s View is printed on 55 percent recycled paper and 30 percent post-consumer waste paper.
Because our doctors successfully treat the worst childhood diseases.
Because our scientists make discoveries that save kids’ lives.
Because someone like you took a moment to give.
Hope lives here.
GiftofChildhood.org