Children’s Mental Health Emergency Department …...2020/05/08 · One in five children in the...
Transcript of Children’s Mental Health Emergency Department …...2020/05/08 · One in five children in the...

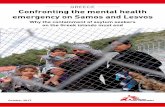
Children’s Mental Health EmergencyDepartment Visits: 2007–2016Charmaine B. Lo, PhD, MPH,a Jeffrey A. Bridge, PhD,b,c,d Junxin Shi, MD, PhD,e,f Lorah Ludwig, BS,g Rachel M. Stanley, MD, MHSAa,c
abstractBACKGROUND AND OBJECTIVES: Emergency department (ED) visits for children seeking mental healthcare have increased. Few studies have examined national patterns and characteristics of EDsthat these children present to. In data from the National Pediatric Readiness Project, it isreported that less than half of EDs are prepared to treat children. Our objective is to describethe trends in pediatric mental health visits to US EDs, with a focus on low-volume,nonmetropolitan EDs, which have been shown to be less prepared to provide pediatricemergency care.
METHODS: Using 2007 to 2016 Nationwide Emergency Department Sample databases, weassessed the number of ED visits made by children (5–17 years) with a mental health disorderusing descriptive statistics. ED characteristics included pediatric volume, children’s EDclassification, and location.
RESULTS: Pediatric ED visits have been stable; however, visits for deliberate self-harm increased329%, and visits for all mental health disorders rose 60%. Visits for children with a substanceuse disorder rose 159%, whereas alcohol-related disorders fell 39%. These increasedvisits occurred among EDs of all pediatric volumes, regardless of children’s ED classification.Visits to low-pediatric-volume and nonmetropolitan areas rose 53% and 41%, respectively.
CONCLUSIONS: Although the total number of pediatric ED visits has remained stable, visits amongchildren with mental health disorders have risen, particularly among youth presenting fordeliberate self-harm and substance abuse. The majority of these visits occur at nonchildren’sEDs in both metropolitan and nonurban settings, which have been shown to be less preparedto provide higher-level pediatric emergency care.
WHAT’S KNOWN ON THIS SUBJECT: Emergencydepartment visits for children with mental healthdisorders have risen, but little is known about thetypes of emergency departments and the rates ofmental health disorders that these children presentwith for emergency mental health care.
WHAT THIS STUDY ADDS: US children presenting withmental health disorders, particularly deliberate self-harm and substance use disorders, often seek care atfacilities that are likely less prepared to providehigher-level pediatric emergency care.
To cite: Lo CB, Bridge JA, Shi J, et al. Children’s Mental HealthEmergency Department Visits: 2007–2016. Pediatrics. 2020;145(6):e20191536
aDivision of Emergency Medicine, Nationwide Children’s Hospital, Columbus, Ohio; bCenters for Suicide Preventionand Research, ePediatric Trauma Research, and fInjury Research and Policy, The Research Institute at NationwideChildren’s Hospital, Columbus, Ohio; cDepartments of Pediatrics, dPsychiatry, and Behavioral Health, College ofMedicine, The Ohio State University, Columbus, Ohio; and gEmergency Medical Services for Children, Division ofChild, Adolescent, and Family Health, Maternal and Child Health Bureau, Health Resources and ServicesAdministration, Rockville, Maryland
Drs Lo and Stanley conceptualized and designed the study, conducted the literature review, draftedthe initial manuscript, and reviewed and revised the final manuscript; Dr Shi assisted with thestudy design, performed the data analysis, and critically reviewed and revised the final manuscript;Dr Bridge contributed to the study design, provided research methodology guidance, and criticallyreviewed and revised the final manuscript; Ms Ludwig assisted with the literature review andcritically reviewed and revised the final manuscript; and all authors have approved the finalmanuscript as submitted and agree to be accountable for all aspects of the work.
DOI: https://doi.org/10.1542/peds.2019-1536
Accepted for publication Mar 5, 2020
Address correspondence to Rachel M. Stanley, MD, MHSA, Nationwide Children’s Hospital,Department of Emergency Medicine, 700 Children’s Dr, Columbus, OH 43205. E-mail: [email protected]
PEDIATRICS Volume 145, number 6, June 2020:e20191536 ARTICLE by guest on August 31, 2020www.aappublications.org/newsDownloaded from

One in five children in the UnitedStates experiences a mental healthdisorder.1 Emergency departments(EDs) often serve as the safety netfor children seeking mental healthcare.2,3 There are more ED visitsfor children with mental healthdisorders, with hospitalizations forsuicide ideation and suicide attemptsmore than doubling over the last10 years.4,5
Children with mental health disordersmake up ∼2% to 5% of all pediatricED visits nationally, and this numberis increasing.6 These children areevaluated in all settings ranging fromchildren’s hospital EDs to EDs thatsee ,500 children per year.7,8 Mostchildren seeking emergency care areseen in nonchildren’s hospital EDs.9
Although the escalation of ED use forchildren with mental health disordershas been documented in theliterature, there have been fewstudies focused on characteristics ofthe EDs in which these children seekcare.10–14 The National PediatricReadiness Project (NPRP),a collaborative effort between theHealth Resources and ServicesAdministration’s (HRSA) EmergencyMedical Services for Childrenprogram, American Academy ofPediatrics, Emergency NursesAssociation, and American Collegeof Emergency Physicians, is a qualityimprovement initiative that aims toensure that all US EDs have theessential guidelines and resourcesin place to provide effectiveemergency care to children.11,12 Indata from the NPRP’s PediatricReadiness Survey, it was reportedthat less than half of hospital EDsare prepared with policies forchildren with mental healthdisorders, and in rural areas, thisdrops to one-third.8 Recently, theNPRP has shown that EDs that seesmall numbers of children are lesslikely to be prepared to treat childrenand have worse outcomes, includingmortality.9,15,16
We studied the 10-year trends inpediatric mental health visits in USEDs based on ED characteristicsdefined from the Pediatric ReadinessSurvey. Examining the characteristicsof EDs that children present to isimportant because pediatricreadiness has been linked to thepediatric volume and geographiclocation of EDs.
METHODS
We used data from the 2007 to 2016Nationwide Emergency DepartmentSample (NEDS), Healthcare Costand Utilization Project, and Agencyfor Healthcare Research andQuality.17 NEDS tracks informationabout ED visits across the countryand includes geographic, hospital,and patient information. NEDS is thelargest all-payer ED database publiclyavailable in the United States andcontains information for ∼20% ofUS EDs.18 NEDS is a stratifiedsample of US hospital-owned EDs,which is representative of all USEDs because the sampling frametakes into account importanthospital characteristics, such asgeographic region, trauma centerlevel, urban or rural location,teaching status, and hospital.17
We analyzed NEDS by lookingat patient demographics, mentalhealth conditions, and hospitalED characteristics.
Patient Demographics
Patient demographic information,such as sex, age, and ED disposition,was examined. We restricted thesample to children ages 5 to 17 yearsbecause age of onset for most mentalhealth conditions typically does notoccur before age 5.19 Age was thencategorized into tertiles: 5 to 9, 10 to14, and 15 to 17 years. We thengrouped children into 3 groups: (1)children with any mental healthdisorders, (2) children with substanceuse disorders, and (3) children whopresented for deliberate self-harm.
Mental Health Conditions CaseDefinition
We identified any diagnosis ofa mental and/or behavioral healthdisorder and aligned with theHealthcare Cost and UtilizationProject Clinical ClassificationSoftware (CCS) groupings for mentaland behavioral health disorders.20
CCS is a tool developed by theAgency for Healthcare Research andQuality that clusters InternationalClassification of Diseases, NinthRevision (ICD-9) and InternationalClassification of Diseases, 10thRevision (ICD-10) diagnosis andprocedure codes into a clinicallymeaningful categorization andstandard coding system.20–22 Thecategories of any mental healthdisorders included adjustmentdisorders (650); anxiety disorder(651); attention-deficit, conduct,and disruptive behavior disorders(652); impulse control disorders(656); mood disorders (657);schizophrenia and other psychoticdisorders (659); and a miscellaneousmental health disorder group thatwas inclusive of CCS categories653, 654, 655, and 670. Substanceuse disorders included alcohol-related disorders (660) andsubstance-related disorders (661).The final group of deliberate self-harm was composed of the CCScategory suicide and intentionalself-inflicted injury (662). The CCScategories and correspondingInternational Classification ofDiseases, Ninth Revision, ClinicalModification and InternationalClassification of Diseases, 10thRevision, Clinical Modificationcodes are provided in SupplementalTable 2.
Hospital ED Characteristics
We classified pediatric ED volume foreach site on the basis of the nationallyrepresentative Pediatric ReadinessSurvey categories,16 with theclassifications of low (,4000),medium (4000–9999), high
2 LO et al by guest on August 31, 2020www.aappublications.org/newsDownloaded from

(10 000–24 999), very high(25 000–49 999), and extremelyhigh ($50 000). Identification ofchildren’s hospital EDs wasdetermined by taking the median ageof all patients treated in a specific ED.A distinctive bimodal distributionwas detected in which children’shospital EDs had a median age of10 years or less, whereasnonchildren’s hospital EDs hada median age of .20. NEDS has ED
urban-rural location split into a4-category designation on the basisof the US Office of Managementand Budget metropolitan andmicropolitan statistical areastandards. These categories are asfollows: large metropolitan areaswith at least 1 million residents, smallmetropolitan areas with ,1 millionresidents, micropolitan areas, andnot metropolitan or micropolitan(the last is essentially a nonurban
residual). Metropolitan andmicropolitan statistical areas arestandards defined as having a corearea containing a substantialpopulation nucleus and closeeconomic and social ties to nearbycommunities.23
Statistical Analyses
Survey weighted data analyticmethods were used to calculatenational estimates for each year.
TABLE 1 Patient and Hospital Characteristics of ED Visits by Children With a Mental Health Disorder, 2007 vs 2016
Rate, per 1000 Population
2007 95% CI 2016 95% CI % Change P
Age, y5–9 6.9 6–7.8 10.3 9.1–11.5 49.0 ,.00110–14 14.5 13–15.9 23.7 21.4–26.1 63.8 ,.00115–17 31.2 28.9–33.5 52.4 48.8–56.0 67.9 ,.001
SexMale 16.9 15.4–18.5 24.5 22.4–26.6 44.9 ,.001Female 14.7 13.5–15.9 26.3 24.1–28.5 78.7 ,.001
All pediatric ED visits 273.5 249.6–297.5 305.5 272.1–338.8 11.7 .06Mental health disordersTotal 15.9 14.5–17.2 25.4 23.3–27.5 60.2 ,.001Any mental disorder 14.0 12.6–15.3 21.0 19.0–22.9 50.3 ,.001650: adjustment disorders 0.7 0.6–0.9 1.0 0.9–1.2 41.7 .002651: anxiety disorders 2.8 2.5–3 6.0 5.4–6.7 116.6 ,.001652: attention-deficit conduct and disruptive behavior disorders 5.8 5.1–6.5 8.1 7.2–9.0 40.1 ,.001656: impulse control disorders NEC 0.2 0.2–0.3 0.5 0.4–0.6 111.3 ,.001657: mood disorders 5.2 4.6–5.7 7.4 6.7–8.2 44.0 ,.001659: schizophrenia and other psychotic disorders 0.4 0.4–0.5 0.4 0.4–0.5 24.6 .27Miscellaneous mental health disordersb 2.6 2.3–2.9 4.9 4.3–5.5 90.9 ,.001
Substance use disorder 2.6 2.4–2.8 4.6 4.3–4.9 75.4 ,.001660: alcohol-related disorders 1.4 1.3–1.5 0.9 0.8–0.9 238.6 ,.001661: substance-related disorders 1.5 1.4–1.7 4.0 3.7–4.2 159.4 ,.001
662: deliberate self-harm 1.1 0.9–1.2 4.6 4.0–5.2 329.3 ,.001ED dispositionED visit in which the patient is treated and released 12.5 11.5–13.6 21.3 19.7–22.9 70.0 ,.001ED visit in which the patient is admitted to this same hospital 2.4 2.0–2.9 3.1 2.5–3.7 26.6 .05ED visit in which the patient is transferred to another short-term hospital 0.4 0.4–0.4 0.9 0.8–1.1 134.3 ,.001ED visit in which the patient died in the ED 0.0 0.0–0.0 0.0 0.0–0.0 54.7 .03Other 0.5 0.3–0.7 0.0 0.0–0.1 290.1 ,.001
ED volumeLow (,4000) 2.5 2.2–2.9 3.9 3.5–4.3 52.6 ,.001Medium (4000–9999) 6.3 5.4–7.2 6.8 5.9–7.6 7.4 .23High (10 000–24 999) 4.3 3.4–5.2 8.0 6.5–9.4 84.0 ,.001Very high (25 000–49 999) 1.6 0.8–2.4 3.5 2.0–5.0 117.4 .01Extremely high ($50 000) 1.1 0.2–2.0 3.3 1.5–5.1 206.0 .02
Children’s hospitalNonchildren’s hospital 14.6 13.5–15.8 22.7 21.0–24.4 55.1 ,.001Children’s hospital 1.2 0.3–2.1 2.7 0.9–4.5 120.6 .08
Hospital urban-rural locationLarge metropolitan area with at least 1 million residents 7.0 5.9–8.1 11.9 10.3–13.4 70.4 ,.001Small metropolitan areas with ,1 million residents 4.2 3.6–4.7 8.9 7.8–10.0 114.1 ,.001Micropolitan areas 1.7 1.5–1.9 2.0 1.6–2.3 15.3 .11Not metropolitan or micropolitan (nonurban residual) 0.7 0.6–0.8 1.0 0.8–1.2 41.4 .001
NEC, not elsewhere classifiable.a Inclusive of the following: CCS 653, delirium dementia and amnestic and other cognitive disorders; CCS 654, developmental disorders; CCS 655, disorders usually diagnosed in infancychildhood or adolescence; and CCS 670, miscellaneous mental health disorders.
PEDIATRICS Volume 145, number 6, June 2020 3 by guest on August 31, 2020www.aappublications.org/newsDownloaded from

We used US Census data to estimatethe population of correspondingage groups and then calculatedincidence rates per 1000 populationby demographics, diagnosis category,and hospital characteristics. Weused t tests to determine thestatistical significance of thedifference between the rates. Wecalculated the percentage of changesfrom 2007 to 2016 and confidenceintervals. All the analyses weredone by using SAS (Enterprise Guide,Version 7.11 HF3 [SAS Institute,Inc, Cary, NC]).
RESULTS
Over the 10-year study period,pediatric ED visits were stable;however, pediatric ED visits for allmental health disorders rose 60%(P , .001) (Table 1, Fig 1). Mentalhealth ED visits among all 3 agetertiles rose, most notably a 68%increase in visits among the 15- to17-year-old group (P , .001).
Significant rate increases were alsoobserved among both sexes andwas more pronounced among girls,with 74% (P , .001). Anxietydisorders (CCS 651) and impulsecontrol disorders (CCS 656)significantly increased by 117%(P , .001) and 111% (P , .001),respectively (Table 1). All substanceuse disorders rose by 75%(P , .001), with alcohol-relateddisorders decreasing by nearly 40%(P , .001), whereas substance usedisorders significantly increased by.150% (P , .001) (Table 1, Fig 1).ED visits for deliberate self-harmincreased 329% (P , .001) overthe 10-year study period (Table 1,Fig 1). The rates for treated andreleased and transferred toanother facility both rose 70% and134%, respectively (P , .001;Table 1).
Significant rate increases wereobserved among nearly all EDvolumes, except for medium-volume
facilities (P = .23), and was mostpronounced among facilities withhigher pediatric ED volumes(Table 1, Fig 2). Although these typesof visits rose 120% in children’shospital EDs (P = .08), the absoluterate change among nonchildren’shospital EDs was much greater,increasing from 14.6 per 1000to 22.7 per 1000, a difference of55% (P , .001) (Table 1).Similarly, pediatric mental healthED visits rose among all urban-rurallocations; although greatest amongthe large and small metropolitanareas (P , .001), a 41% increasewas observed among EDs classifiedas neither metropolitan normicropolitan (P = .001) (Table 1,Fig 3).
DISCUSSION
Over the 10-year study period,pediatric ED visits were stable;however, pediatric ED visits forall mental health disorders rose60%. Importantly, we observeda threefold increase in ED visitsfor deliberate self-harm, similarto trends reported by authorsof other studies, suggesting thatchildren are increasingly engagingin self-harm.9,10,24
Similarly, Torio et al4 foundincreasing visits by children formental health conditions between2006 and 2011, and Kalb et al’s10
National Hospital AmbulatoryMedical Care Survey studyfound similar trends, particularlyamong those presenting for asuicide-related visit. However,neither of these studies examinedhospital characteristics,specifically the number ofpediatric ED visits, and the dataused are older.
We found that all substance usedisorders rose 75%, largely driven bythe almost twofold increase in thesubstance use disorders subgroupand not the alcohol disorderssubgroup, which other studies have
FIGURE 1Percent change of pediatric ED visits among mental health subgroups. Line graph depicting yearlypercentage change from 2007 of ED visits made by US children and those with at least one of thefollowing mental health disorders: any mental health disorder, substance use disorder, and de-liberate self-harm diagnosis.
4 LO et al by guest on August 31, 2020www.aappublications.org/newsDownloaded from

shown.4,25 The rate increase insubstance use disorders, despitethe decline in alcohol use disorders,bears further investigation, especiallyas the opiate epidemic continues toescalate. EDs, regardless of pediatricspecialty, volume, and location, willneed to be prepared to handle thesecases.26,27
Although the increased rate ofpediatric mental health visits wasgreatest among high-pediatric-volume EDs, our results show that all
EDs, regardless of pediatric volume,experienced increased visits bychildren for mental health disorders.These visits increased by one-halfamong low-pediatric-volume EDs.28
The National Pediatric ReadinessAssessment, conducted in 2013,found that lower-pediatric-volumeEDs, with ,4000 pediatric visits peryear, and rural EDs are less preparedfor all pediatric emergencies, andonly one-third have pediatric mentalhealth policies or mental healthtransfer agreements.7,11,13,29–31 Our
findings of increased pediatric EDvisits for mental health at smaller-volume EDs in rural centers areconcerning given the potentialdecreased pediatric readiness forchildren with mental healthproblems. It will be important tofocus future mental healthpreparedness efforts and resourceson all hospital EDs, particularlysmaller-volume and rural EDs, andnot just on children’s hospital EDs.28
HRSA’s recently published CriticalCrossroads Care Pathway toolkit forEDs further highlights the rising ratesof pediatric behavioral healthconditions amid the gaps in hospitalpreparedness. This is a toolkitfor EDs that is focused on pediatricmental health visits and offersa customizable framework withresources that can be used in allsettings to improve the coordinationand continuity of care for childrenpresenting with mental healthdisorders.8 Toolkits and onlinetrainings addressing other importantcomponents of pediatric readiness,such as interfacility transferguidelines, are available and scalableto work within the resourcesavailable.32–34 They offer pragmatic,actionable recommendations to effectchange, especially in less-resourced,rural EDs.31
An opportunity to increase mentalhealth services in rural, lower-volumeEDs could include tele-mentalhealth services. Telemedicinecould also provide an avenue forincreasing access to behavioralhealth specialists who can screen,assist with acute interventions,and support connections to continuedcare within the community, therebyavoiding long-distance transfers,transportation costs, and delaysin care.35 Recent literature lookingat the use of telephone consultationprograms on the impact ofchildren’s mental health care usehave shown that the accessibilityof these programs has led to greater
FIGURE 2Comparison of percent change from 2007 of pediatric mental health ED visits by hospital pediatricED volume. Line graph depicting yearly percentage change from 2007 of ED visits made by USchildren by pediatric ED volume for each mental health subgroup. The subgroups depicted (A) allpediatric mental health ED visits, (B) any mental health disorder, (C) substance use disorder, and (D)deliberate self-harm diagnosis.
PEDIATRICS Volume 145, number 6, June 2020 5 by guest on August 31, 2020www.aappublications.org/newsDownloaded from

receipt of mental health treatmentof children.36
There is a nationwide shortage ofmental health care providers,especially in nonurban areas.37–39
This gap between the supply ofproviders and the demand for mentalhealth services has become especiallypronounced among those whospecialize in providing care tochildren.37,38,40,41 This shortage willhave a direct impact on theaccessibility and quality of mental
health care of children, particularlythose who live in rural areas, areyounger, and are uninsured.42–46
As the number of pediatric mentalhealth visits continues to rise inEDs, research is needed to identifyactionable solutions that will betterequip all EDs with the tools,personnel, and resources to bettermanage these cases. Solutions likescreening and assessment efforts forsuicidal ideation, a requirement of theJoint Commission for all patients
being evaluated for behavioralhealth conditions, may impact andimprove the quality and safety ofcare for children now and inyears to come.47 Further workexploring alternative care deliverymethods, such a telepsychiatryand establishing partnershipprograms with institutions thathave specialized pediatric mentalhealth resources, can better ensurecontinuity of care and help addressthe mental health crisis that USEDs are facing.
This study has some limitations.NEDS is a national database butdoes not have patient identifiersthat would allow for trackingof ED recidivism. Also, by design,NEDS does not have a primarydiagnosis code, so children maybe presenting for some reasonother than their mental healthcondition. However, ED care hasincreasingly become more patientcentered and mental healthsensitive so that providers canadjust their practice to delivermore mental health–informed care.There is also the potential thatcases were missed if the child didnot have a diagnosis for one of themental health conditions beforepresentation to the ED. However,because we limited our analysisto age 5 years and above, age ofonset for these conditions is morelikely to have occurred by then.Information on presence of inpatientpediatric psychiatric beds and ontransfers to appropriate facilities(eg, pediatric transfer guidelines,interfacility agreements, etc) isnot available in NEDS. The abilityof NEDS to identify children’shospitals is limited and as suchdoes not explicitly sample children’shospitals. We circumvented thisby categorizing each facility by themedian age of the patient; however,this may not have been foolproof,which may explain how the ratechange was not statisticallysignificant.
FIGURE 3Comparison of percent change from 2007 of pediatric mental health ED visits by metropolitan area.Line graph depicting yearly percentage change from 2007 of ED visits made by US children bymetropolitan area for each mental health subgroup. The subgroups depicted (A) all pediatric mentalhealth ED visits, (B) any mental health disorder, (C) substance use disorder, and (D) deliberate self-harm diagnosis.
6 LO et al by guest on August 31, 2020www.aappublications.org/newsDownloaded from

CONCLUSIONS
Although the total number ofpediatric ED visits has remainedstable, visits among children withmental health disorders havesteadily risen, with ED visits bychildren presenting with deliberateself-harm tripling over the 10-yearstudy period. The majority ofchildren presenting with mentalhealth disorders did not seek careat specialized pediatric EDs.We demonstrated significantlyincreased visits by childrenwith mental health disorders to
small-pediatric-volume, rural EDsthat may be least likely to beprepared to provide higher-levelpediatric care.
ACKNOWLEDGMENTS
The findings and conclusions inthis report are those of the authorsand do not necessarily reflect theofficial position of the HRSA. Theauthors would like to acknowledgeDoug MacDowell for his assistancewith the preparation of figures andtables.
ABBREVIATIONS
CCS: Clinical ClassificationSoftware
ED: emergency departmentHRSA: Health Resources and
Services AdministrationICD-9: International Classification
of Diseases, Ninth RevisionICD-10: International Classification
of Diseases, 10th RevisionNEDS: Nationwide Emergency
Department SampleNPRP: National Pediatric
Readiness Project
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright © 2020 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: No external funding.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2019-3542.
REFERENCES
1. Institute of Medicine. Emergency Carefor Children: Growing Pains.Washington, DC: The NationalAcademies Press; 2007
2. Mojtabai R. Trends in contacts withmental health professionals and costbarriers to mental health care amongadults with significant psychologicaldistress in the United States: 1997-2002.Am J Public Health. 2005;95(11):2009–2014
3. Sareen J, Jagdeo A, Cox BJ, et al.Perceived barriers to mental healthservice utilization in the United States,Ontario, and the Netherlands. PsychiatrServ. 2007;58(3):357–364
4. Torio CM, Encinosa W, Berdahl T,McCormick MC, Simpson LA. Annualreport on health care for children andyouth in the United States: nationalestimates of cost, utilization andexpenditures for children with mentalhealth conditions. Acad Pediatr. 2015;15(1):19–35
5. Plemmons G, Hall M, Doupnik S, et al.Hospitalization for suicide ideation or
attempt: 2008-2015. Pediatrics. 2018;141(6):e20172426
6. Abrams A, Badolato G, Goyal M. Racialdisparities in pediatric mental health-related emergency department visits:a five-year multi-institutional study. In:Proceedings from the AmericanAcademy of Pediatrics NationalConference & Exhibition; November 2,2018, 2018; Orlando, FL
7. Remick K, Gausche-Hill M, Joseph MM,Brown K, Snow SK, Wright JL; AMERICANACADEMY OF PEDIATRICS Committee onPediatric Emergency Medicine andSection on Surgery; American College ofEmergency Physicians PediatricEmergency Medicine Committee;Emergency Nurses Association PediatricCommittee. Pediatric readiness in theemergency department. Pediatrics. 2018;142(5):e20182459
8. US Department of Health and HumanServices, Health Resources andServices Administration, Maternal andChild Health Bureau. CriticalCrossroads Pediatric Mental Health
Care in the Emergency Department: ACare Pathway Resource Toolkit.Rockville, MD: U.S. Department of Healthand Human Services; 2019
9. Whitfill T, Auerbach M, Scherzer DJ, ShiJ, Xiang H, Stanley RM. Emergency carefor children in the United States:epidemiology and trends over time.J Emerg Med. 2018;55(3):423–434
10. Kalb LG, Stapp EK, Ballard ED, HolingueC, Keefer A, Riley A. Trends inpsychiatric emergency departmentvisits among youth and young adults inthe US. Pediatrics. 2019;143(4):e20182192
11. Grupp-Phelan J, Harman JS, Kelleher KJ.Trends in mental health and chroniccondition visits by children presentingfor care at U.S. emergencydepartments. Public Health Rep. 2007;122(1):55–61
12. Zima BT, Rodean J, Hall M, Bardach NS,Coker TR, Berry JG. Psychiatricdisorders and trends in resource use inpediatric hospitals. Pediatrics. 2016;138(5):e20160909
PEDIATRICS Volume 145, number 6, June 2020 7 by guest on August 31, 2020www.aappublications.org/newsDownloaded from

13. Santucci KA, Sather J, Baker MD.Emergency medicine trainingprograms’ educational requirements inthe management of psychiatricemergencies: current perspective.Pediatr Emerg Care. 2003;19(3):154–156
14. Sheridan DC, Spiro DM, Fu R, et al.Mental health utilization in a pediatricemergency department. Pediatr EmergCare. 2015;31(8):555–559
15. Ames SG, Davis BS, Marin JR, et al.Emergency department pediatricreadiness and mortality in critically illchildren. Pediatrics. 2019;144(3):e20190568
16. Gausche-Hill M, Ely M, Schmuhl P, et al.A national assessment of pediatricreadiness of emergency departments.JAMA Pediatr. 2015;169(6):527–534
17. Healthcare Cost and Utilization Project(HCUP). Overview of the NationwideEmergency Department Sample (NEDS).Available at: https://www.hcup-us.ahrq.gov/nedsoverview.jsp. AccessedDecember 13, 2017
18. Healthcare Cost and Utilization Project(HCUP). Databases. Available at: https://www.hcup-us.ahrq.gov/databases.jsp.Accessed December 13, 2017
19. Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustün TB. Ageof onset of mental disorders: a reviewof recent literature. Curr OpinPsychiatry. 2007;20(4):359–364
20. Healthcare Cost and Utilization Project(HCUP). Clinical ClassificationsSoftware (CCS) for ICD-9-CM. Availableat: https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. AccessedAugust 9, 2019
21. Healthcare Cost and Utilization Project(HCUP). Clinical ClassificationsSoftware (CCS) for ICD-9-CM Fact Sheet.Available at: https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccsfactsheet.jsp.Accessed August 9, 2019
22. Healthcare Cost and Utilization Project(HCUP). Beta Clinical ClassificationsSoftware (CCS) for ICD-10-PCS. Availableat: https://hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp.Accessed August 9, 2019
23. United States Census Bureau.Metropolitan and micropolitan.Available at: https://www.census.gov/
programs-surveys/metro-micro.html.Accessed August 9, 2019
24. Bridge JA, Olfson M, Fontanella CA,Marcus SC. Emergency departmentrecognition of mental disorders andshort-term risk of repeat self-harmamong young people enrolled inmedicaid. Suicide Life Threat Behav.2018;48(6):652–660
25. Miech RA, Johnston LD, O’Malley PM,Bachman JG, Schulenberg JE, PatrickME. Monitoring the Future NationalSurvey Results on Drug Use, 1975–2018.In: Secondary School Students, vol. Vol1. Ann Arbor, MI: Institute for SocialResearch, The University of Michigan;2019
26. Allareddy V, Rampa S, Allareddy V.Opioid abuse in children: an emergingpublic health crisis in the UnitedStates!. Pediatr Res. 2017;82(4):562–563
27. Mazer-Amirshahi M, Mullins PM,Rasooly IR, van den Anker J, Pines JM.Trends in prescription opioid use inpediatric emergency departmentpatients. Pediatr Emerg Care. 2014;30(4):230–235
28. Gausche-Hill M, Schmitz C, Lewis RJ.Pediatric preparedness of USemergency departments: a 2003 survey.Pediatrics. 2007;120(6):1229–1237
29. Doupnik SK, Esposito J, Lavelle J.Beyond mental health crisisstabilization in emergency departmentsand acute care hospitals. Pediatrics.2018;141(5):e20173059
30. Seidel JS, Hornbein M, Yoshiyama K,Kuznets D, Finklestein JZ, St Geme JWJr.. Emergency medical services andthe pediatric patient: are the needsbeing met? Pediatrics. 1984;73(6):769–772
31. Pilkey D, Edwards C, Richards R, OlsonLM, Ely M, Edgerton EA. Pediatricreadiness in critical access hospitalemergency departments. J RuralHealth. 2019;35(4):480–489
32. Emergency Medical Services forChildren. Interfacility transfer toolkit.Available at: https://emscimprovement.center/resources/publications/interfacility-transfer-tool-kit/. AccessedJanuary 10, 2018
33. Emergency Medical Services forChildren. Readiness toolkit. Available at:https://emscimprovement.center/
projects/pediatricreadiness/readiness-toolkit/. Accessed January 5, 2018
34. Emergency Medical Services forChildren. Ensuring pediatric readinessfor all emergency departments. 2017.Available at: https://emscimprovement.center/about/nprp-white-paper/.Accessed January 5, 2018
35. Spooner SA, Gotlieb EM; Committee onClinical Information Technology;Committee on Medical Liability.Telemedicine: pediatric applications.Pediatrics. 2004;113(6). Available at:www.pediatrics.org/cgi/content/full/113/6/e639
36. Stein BD, Kofner A, Vogt WB, Yu H. Anational examination of child psychiatrictelephone consultation programs’impact on children’s mental health careutilization. J Am Acad Child AdolescPsychiatry. 2019;58(10):1016–1019
37. Healthcare Cost and Utilization Project(HCUP). Shortage areas. Available at:https://data.hrsa.gov/topics/health-workforce/shortage-areas. AccessedDecember 13, 2017
38. Sills MR, Bland SD. Summary statisticsfor pediatric psychiatric visits to USemergency departments, 1993-1999.Pediatrics. 2002;110(4). Available at:www.pediatrics.org/cgi/content/full/110/4/e40
39. Healthcare Cost and Utilization Project(HCUP). National projections of supplyand demand for selected behavioralhealth practitioners, 2013-2025. 2016.Available at: https://bhw.hrsa.gov/sites/default/files/bhw/health-workforce-analysis/research/projections/behavioral-health2013-2025.pdf.Accessed August 9, 2019
40. Thomas CR, Holzer CE III. The continuingshortage of child and adolescentpsychiatrists. J Am Acad Child AdolescPsychiatry. 2006;45(9):1023–1031
41. Koppelman J. Children with mentaldisorders: making sense of their needsand the systems that help them. NHPFIssue Brief. 2004;(799):1–24
42. Kelleher KJ, Gardner W. Out of sight, outof mind - behavioral and developmentalcare for rural children. N Engl J Med.2017;376(14):1301–1303
43. Sturm R, Ringel JS, Andreyeva T.Geographic disparities in children’smental health care. Pediatrics. 2003;
8 LO et al by guest on August 31, 2020www.aappublications.org/newsDownloaded from

112(4). Available at: www.pediatrics.org/cgi/content/full/112/4/e308
44. Larkin GL, Claassen CA, Emond JA,Pelletier AJ, Camargo CA. Trends in U.S.emergency department visits formental health conditions, 1992 to 2001.Psychiatr Serv. 2005;56(6):671–677
45. Robinson LR, Holbrook JR, Bitsko RH,et al. Differences in health care, family,
and community factors associated withmental, behavioral, and developmentaldisorders among children aged2–8 years in rural and urban areas -United States, 2011–2012. MMWRSurveill Summ. 2017;66(8):1–11
46. Kataoka SH, Zhang L, Wells KB. Unmetneed for mental health care among USchildren: variation by ethnicity and
insurance status. Am J Psychiatry. 2002;159(9):1548–1555
47. The Joint Commission. R3 Report Issue18: National Patient Safety Goal forsuicide prevention. 2018. Available at:https://www.jointcommission.org/en/standards/r3-report/r3-report-issue-18-national-patient-safety-goal-for-suicide-prevention/. Accessed August 9, 2019
PEDIATRICS Volume 145, number 6, June 2020 9 by guest on August 31, 2020www.aappublications.org/newsDownloaded from

originally published online May 11, 2020; Pediatrics Stanley
Charmaine B. Lo, Jeffrey A. Bridge, Junxin Shi, Lorah Ludwig and Rachel M.2016−Children's Mental Health Emergency Department Visits: 2007
ServicesUpdated Information &
019-1536http://pediatrics.aappublications.org/content/early/2020/05/08/peds.2including high resolution figures, can be found at:
References
019-1536#BIBLhttp://pediatrics.aappublications.org/content/early/2020/05/08/peds.2This article cites 27 articles, 8 of which you can access for free at:
Subspecialty Collections
subhttp://www.aappublications.org/cgi/collection/emergency_medicine_Emergency Medicinefollowing collection(s): This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtmlin its entirety can be found online at: Information about reproducing this article in parts (figures, tables) or
Reprintshttp://www.aappublications.org/site/misc/reprints.xhtmlInformation about ordering reprints can be found online:
by guest on August 31, 2020www.aappublications.org/newsDownloaded from

originally published online May 11, 2020; Pediatrics Stanley
Charmaine B. Lo, Jeffrey A. Bridge, Junxin Shi, Lorah Ludwig and Rachel M.2016−Children's Mental Health Emergency Department Visits: 2007
http://pediatrics.aappublications.org/content/early/2020/05/08/peds.2019-1536located on the World Wide Web at:
The online version of this article, along with updated information and services, is
http://pediatrics.aappublications.org/content/suppl/2020/05/08/peds.2019-1536.DCSupplementalData Supplement at:
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397. the American Academy of Pediatrics, 345 Park Avenue, Itasca, Illinois, 60143. Copyright © 2020has been published continuously since 1948. Pediatrics is owned, published, and trademarked by Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
by guest on August 31, 2020www.aappublications.org/newsDownloaded from