Characterization of an animal model of Bladder painful ... · Characterization of an animal model...
Transcript of Characterization of an animal model of Bladder painful ... · Characterization of an animal model...
Characterization of an animal model of Bladder Painful Syndrome/ Interstitial Cystitis
Rita Daniela Santos Matos
Mestrado em Biologia Celular e Molecular Departamento de Biologia Faculdade de Ciências da Universidade do Porto 2014
Orientador Ana Cristina Estrela de Oliveira Charrua Cordeiro, PhD Faculdade de Medicina da Universidade do Porto
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 3
Todas as correções determinadas pelo júri, e só essas, foram efetuadas. O Presidente do Júri,
Porto, ______/______/_________
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 5
Dissertação para a candidatura ao grau de
Mestre em Biologia Celular e Molecular
submetida à Faculdade de Ciências da
Universidade do Porto.
A presente dissertação foi orientada pela
Doutora Ana Cristina Estrela de Oliveira Charrua
Cordeiro e foi realizada no Centro de
Investigação Médica da Faculdade de Medicina
da Universidade do Porto.
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 7
Acknowledgments
First, I would like to thank to Dr. Ana Charrua not only for supervising this
thesis, but also for all comprehension, sympathy, care, support, interest, knowledge
and time dispensed with me. Thank you so much.
I also would like to thank Prof. Francisco Cruz to accept me in this great group
and allow me the contact with this amazing research area.
I would like to thank Prof. Célia Cruz and Prof. António Avelino for their
availability since the first time.
I must not forget to thanks to “lunch friends” Dr. Bárbara Frias, Dr. Ana Coelho,
Raquel Oliveira, Isabel Regadas, Lígia Almeida, Diana Nascimento, Gisela Borges,
José Pedro Castro and César Monteiro, for their constant good mood, sympathy and
for the excellent way that welcomed me.
I also would like to thank to Anabela Silvestre and Elisa Nova for their technical
support.
At last, but not the least, I would like to thank to my family. To my parents and
my brother that while away, always supported me. To my father, thank you for your
words of advice, care and support. To my mother and my brother, thank you for your
happiness and to make me laugh every day, even when I want to cry.
To my grandmother, for her love and care.
I would like to thank to Daniel for his care, love, friendship, support and for all
the hours that we spent in front of computer working. Thank you to being present in my
life whenever I need.
Thank you!
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 9
Resumo
O Síndrome Doloroso Vesical/Cistite Intersticial (BPS/IC, do inglês bladder pain
syndrome/ interstitial cystitis) é um síndrome crónico e doloroso, cuja etiologia
permanece desconhecida. Doentes com esta patologia apresentam uma
hiperatividade do sistema nervoso simpático, caracterizada pelo aumento da
expressão de tirosina hidroxilase na bexiga, pelo aumento dos níveis de noradrenalina
na urina e pelo aumento da pressão sanguínea e ritmo cardíaco durante a distensão
da bexiga. Estes doentes também apresentam um aumento da expressão do TRPV1
na bexiga. A hiperatividade simpática pode também ser observada em várias
patologias dolorosas em humanos e em modelos animals de dor.
Estudos anteriores demonstraram que a estimulação crónica adrenérgica com
fenilefrina em ratos induz um comportamento de dor, aumenta a frequência urinária e
disfunção do urotélio, o que simula o BPS/IC. A dor e o aumento da frequência urinária
são dependentes dos aferentes primários sensíveis à capsaicina, um agonista do
TRPV1. A desensibilização destes aferentes primários por doses elevadas de
capsaicina reverte os efeitos induzidos pela fenilefrina, sugerindo uma possível relação
entre a atividade adrenérgica e a atividade nociceptiva (como o próprio TRPV1 ou com
outros recetores como os recetores canabinóides, por exemplo).
Este trabalho teve três objetivos principais. O primeiro objetivo foi demonstrar o
envolvimento dos adrenocetores no aparecimento dos sintomas de BPS/IC,
caracterizando qual o subtipo de adrenorecetor que está envolvido no aparecimento
da dor e nas alterações histológicas observadas em animais submetidos a estimulação
crónica adrenérgica com fenilefrina. O segundo objetivo foi avaliar a relação entre os
adrenocetores e o TRPV1 durante a estimulação crónica adrenérgica com fenilefrina.
O terceiro objetivo foi verificar como é que os endocanabinóides modulam a dor
vesical e a hiperatividade durante a cistite.
Para avaliar qual o subtipo de adrenocetor que está envolvido no aparecimento
da dor, aos ratos Wistar fêmeas injetados diariamente com 2.5 mg/Kg de fenilefrina
(subcutânea durante 14 dias) foi-lhes administrado oralmente os seguintes
antagonistas dos α1 – adrenocetores: Silodosina, Naftopidil ou Prazosina. Ao dia 15,
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 10
os animais foram anestesiados com uretano (1.2 g/Kg) e as cistometrias foram
realizadas durante 2h. Depois deste período, os animais foram perfundidos com
paraformaldeído e a bexiga e o segmento L6 da medula espinhal foram colhidos. A
bexiga dos animais foi cortada e corada com Hematoxilina-Eosina para analisar a
morfologia do urotélio e com Azul de Toluidina para estudar os mastócitos. Os cortes
de bexigas foram também sujeitos a uma reação de imunofluorescência contra a
caspase 3, para analisar a apoptose do urotélio. Os segmentos da região L6 da
medula espinal foram sujeitos a reação de imunohistoquímica contra a proteína Fos.
Para estudar a relação entre os adrenocetores e as vias nociceptivas, um
grupo de ratinhos mutantes para o TRPV1 foram injetados diariamente com fenilefrina,
durante 14 dias. O comportamento doloroso foi avaliado nestes animais. Mais ainda,
um grupo de ratos Wistar fêmeas e respetivos controlos foram injetados diariamente
com fenilefrina durante 14 dias. No fim do tratamento os animais foram submetidos a
cistometria com capsaicina.
Para avaliar se os endocanabinóides modulam a dor vesical e a hiperatividade
durante a cistite, um grupo de ratos Wistar fêmeas foram instilados com
lipopolisacarídeo (LPS) e com URB (inibidor da FAAH, do inglês fatty acid amide
hydrolase), e foi avaliado o comportamento doloroso, bem como o funcionamento da
bexiga através da cistometria. Estas experiências foram repetidas em animais tratados
com LPS, URB e antagonistas do recetor canabinóide 1 (CB1), recetor canabinóide 2
(CB2) e TRPV1 (MJ15, SR144528 e SB366791, respetivamente). Os segmentos L6 da
medula espinal foram sujeitos a uma reação de imunohistoquímica contra a proteína
Fos.
Este trabalho confirmou que a estimulação crónica adrenérgica com fenilefrina
induz um comportamento de dor, infiltração de mastócitos, apoptose de células
uroteliais e ativação das vias nociceptivas. A Silodosina (antagonista dos α1A-
adrenorecetores) reduz os efeitos induzidos pela fenilefrina. Para além disso, o TRPV1
e o CB1 parecem estar envolvidos na hiperatividade da bexiga.
Assim sendo, podemos afirmar que BPS/IC resulta da interação entre várias
vias, nomeadamente dos α1A-adrenoreceptores, do TRPV1 e do CB1.
Palavras-chave: Síndrome doloroso vesical/ cistite intersticial; alfa-adrenorecetores;
TRPV1; CB1; vias nociceptivas
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 11
Abstract
Bladder painful syndrome/ interstitial cystitis (BPS/IC) is a chronic debilitating
condition with unknown etiology. Patients with BPS/IC present an increased
sympathetic activity, characterized by an increase in tyrosine hydroxylase expression in
the bladder, increased noradrenaline levels in urine and elevated mean blood pressure
and heart rate during bladder hydrodistention. These patients also present an increase
in expression of TRPV1 in the bladder. Sympathetic overactivity also can be observed
in several human painful diseases and in rat pain models.
Previous studies showed that chronic adrenergic stimulation with phenylephrine
(PHE) in rats induced pain behavior, increased voiding frequency and urothelial
dysfunction, which mimic BPS/IC. Pain and increased frequency where dependent of
capsaicin sensitive primary afferents activation since desensitization of these fibers
with high levels of capsaicin reverse the phenylephrine mediated effect, demonstrating
a possible relation between adrenergic activity and nociceptive activity (like TRPV1 or
other receptors like cannabinoid receptors, for example).
Hence, this work had three main goals. The first goal was to demonstrate the
involvement of adrenoceptors in the appearance of BPS/IC symptoms, characterizing
which subtypes are involved in the appearance of pain and histological changes
observed in animals submitted to chronic adrenergic stimulation with phenylephrine.
The second aim was to evaluate the cross-talk between adrenoceptors and TRPV1
during chronic adrenergic stimulation with phenylephrine. The third aim was to verify
how endocannabinoids modulate the bladder pain and hyperactivity during cystitis.
To assess which adrenoceptor subtypes are involved in the appearance of pain,
to female Wistar rats injected with 2.5 mg/Kg/day of phenylephrine (PHE;
subcutaneously for 14 days) was administrated orally the follow antagonists of
adrenoceptors: Silodosin, Naftopidil or Prazosin. The visceral pain behavior and
voiding pattern were analyzed before and 14 days after PHE treatment. At day 15,
animals were anaesthetized with urethane (1.2 g/Kg) and cystometries were performed
for 2h. Animals were then perfused with paraformaldehyde and the bladder and L6
spinal cord segments were harvested. Bladder sections from these animals were
stained with Hematoxylin-eosin to analyze urothelium morphology, with Toluidine Blue
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 12
to study mast cells, and immunoreacted (IR) against caspase 3, to investigate
urothelial apoptosis. L6 spinal cord segments were IR against Fos.
Furthermore, to study the cross-talk between adrenoceptors and nociceptive
pathways, a group of TRPV1 knockout mice were injected with PHE daily for 14 days.
Visceral pain behavior and cystometry were performed in these animals. Further, a
group of female Wistar rats was daily injected with phenylephrine for 14 days. At the
end of treatment, animals were submitted to cystometry with capsaicin.
To assess if endocannabinoids modulate bladder pain and hyperactivity during
cystitis, a group of female Wistar rats were instilled with lipopolysaccharide (LPS) and
URB (inhibitor of FAAH, fatty acid amide hydrolase). Visceral pain behavior and
cystometry were performed. These experiments were repeated in rats co-treated with
LPS, URB and antagonists of CB1, CB2 and TRPV1 (MJ15, SR144528 and
SB366791, respectively). L6 spinal cord segments were IR against Fos.
The results confirm that chronic adrenergic stimulation with PHE induce visceral
pain, mast cells infiltration, apoptosis of urothelial cells and activation of nociceptive
pathways. Silodosin (antagonist of α1A-adrenoceptor subtype) seem to be more
effective than naftopidil or prazosin (α1D and α1-adrenoceptor antagonists, respectively)
to reduce the effects induced by PHE. This work also shows that TRPV1 and CB1 are
involved in bladder hyperactivity.
Thus, it can be affirmed that BPS/IC result the interaction between several
pathways, namely those involving α1A-adrenoceptors, TRPV1 and CB1.
Keywords: Bladder painful syndrome/ interstitial cystitis; alpha-adrenoceptors; TRPV1;
CB1; nociceptive pathways
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 13
Table of Contents
Table list ......................................................................................................................... 15
Figure list ........................................................................................................................ 16
Abbreviations ................................................................................................................. 18
I. Introduction ............................................................................................................. 21
1. Bladder painful syndrome/ Interstitial cystitis (BPS/IC) ..................................... 22
1.1 Definition of BPS/IC .................................................................................... 22
1.2 Etiology of BPS/IC ...................................................................................... 24
1.3 Diagnosis of BPS/IC .................................................................................... 24
1.4 Epidemiology of BPS/IC .............................................................................. 25
1.5 Treatment of BPS/IC .................................................................................... 25
2. Sympathetic nervous system dysfunction in BPS/IC .......................................... 26
2.1. Nociceptive pathway modulation by adrenoceptors ........................................ 27
II. Aims ........................................................................................................................ 32
III. Material and Methods .......................................................................................... 34
1. Experimental Animals ......................................................................................... 36
2. Chronic adrenergic stimulation ........................................................................... 36
2.1. Blockade of alpha1-adrenoceptors ............................................................... 36
2.1.1. Pain behavior test ..................................................................................... 37
2.1.2. Organ motility test .................................................................................... 38
2.1.3. Cystometry ............................................................................................... 38
2.1.4. Tissue harvesting and processing ............................................................. 39
2.1.5. Immunohistochemistry ............................................................................. 39
2.1.6. Bladder Histological Evaluation ............................................................... 40
2.2 Cross-talk between adrenoceptors and TRPV1 ............................................ 40
3. Cannabinoid system and TRPV1 cross-talk during cystitis ................................ 40
3.1 LPS-induced cystitis ..................................................................................... 40
3.2 Pain behavior test ......................................................................................... 41
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 14
3.3 Cystometries ................................................................................................. 41
4. Data presentation ................................................................................................. 41
IV. Results ................................................................................................................. 43
1. Blockade of alpha1-adrenoceptors ...................................................................... 45
1.1 Pain behavior test .............................................................................................. 45
1.2 Organ motility test ........................................................................................ 46
1.3 Cystometry ........................................................................................................ 46
1.4 Immunohistochemistry ................................................................................. 47
1.5 Bladder histological evaluation ......................................................................... 49
2. Cross-talk between adrenoceptors and TRPV1 ................................................... 50
2.1 Pain behavior test .............................................................................................. 50
2.2 Cystometry ................................................................................................... 51
3. Cannabinoid system and TRPV1 cross-talk during cystitis ................................ 52
3.1 Cystometries ................................................................................................. 52
3.2 Pain behavior test ......................................................................................... 55
3.3 Immunohistochemistry ................................................................................. 56
V. Discussion ............................................................................................................... 59
VI. Conclusion ........................................................................................................... 67
VII. Future work ......................................................................................................... 71
VIII. References ........................................................................................................... 76
IX. Attachments ......................................................................................................... 86
1. Phenylephrine and antagonist solutions .............................................................. 88
2. Cystometry, tissue harvesting and processing solutions ..................................... 88
3. Immunoreaction against Fos in spinal cord segments ......................................... 89
4. Immunoreaction against caspase 3 in bladder sections ....................................... 90
5. Preparation of solutions for immunoreaction ...................................................... 91
6. Hematoxylin-Eosin staining in bladder sections ................................................. 92
7. Toluidine Blue staining in bladder sections ........................................................ 92
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 15
Table list
Table 1. Experimental group of Wistar rats submitted to chronic adrenergic stimulation
and alpha-adrenoceptors antagonists……………………………………………..…….38
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 16
Figure list
Figure 1. Hunner’s lesion in bladder from patients with BPS/IC, adapted from
ESSIC……………………………………………………………………………….….24
Figure 2. Animals placed in individual chambers to perform visceral pain behavior test
(figure 2a), in lower abdominal region using a series of Von Frey monofilaments (figure
2b)…………………………………………………………………………………..…..38
Figure 3. Animals placed into boxes with filter paper to analyze alterations on bladder
motility……………………………………………………………………………...…..39
Figure 4. Animals under cystometry, over a heating pad and with a 20-gauge needle
inserted in the bladder dome to infuse saline solution……………………………...…..40
Figure 5. Graph bar showing lower abdominal mechanical pain threshold using Von
Frey filaments in control animals, PHE group, PHE +Silodosin group, PHE +Naftopidil
group and PHE +Prazosin group………………………….…………………...……….46
Figure 6. Graph bar showing the voiding frequency (urinary spots/ h) of control
animals, animals submitted to chronic adrenergic stimulation with PHE and animals
submitted to chronic adrenergic stimulation with PHE and α-adrenoceptors
antagonists……………………………………………………………………………...47
Figure 7. Graph bar showing the bladder reflex activity (bladder contractions/ minute)
of control animals and animals submitted to chronic adrenergic stimulation with PHE
and α-adrenoceptors antagonists………………………………………………………..48
Figure 8. Graph bar showing the spinal Fos expression (number of Fos immunopositive
cells/ section) in control animals and animals submitted to chronic adrenergic
stimulation with PHE and α-adrenoceptors
antagonists.......................................................................................................................49
Figure 9. Bladder sections immunoreacted against caspase 3 in control animals and
animals submitted to chronic adrenergic stimulation with PHE and α-adrenoceptors
antagonists……………………………………………………………………………...49
Figure 10. Graph bar showing urothelium integrity (percentage of low urothelium) of
bladder sections stained with Hematoxylin-Eosin………...............................................50
Figure 11. Graph bar showing the mast cells in bladder sections stained with Toluidine
Blue……………………………………………………………………………………..51
Figure 12 Graph bar showing lower abdominal mechanical pain threshold using Von
Frey filaments in WT saline animals and WT and KO TRPV1 animals under chronic
adrenergic stimulation……………………………………………...…………………..52
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 17
Figure 13. Graph bar of bladder reflex activity evaluated during cystometry with saline
and capsaicin in control Wistar rats and in Wistar rats submitted to chronic adrenergic
stimulation with PHE…………………………………………………………………...52
Figure 14. Line graph of bladder reflex activity of control animals and LPS-treated
animals submitted to different concentrations of URB937..…………………………...53
Figure 15. Graph bar of bladder reflex activity of control animals and LPS-treated
animals submitted to URB937 and SR144528…………….…………………………...54
Figure 16. Graph bar of bladder reflex activity of control animals and LPS-treated
animals submitted to URB937 and MJ15………………….…………………………...55
Figure 17. Graph bar of bladder reflex activity of control animals and LPS-treated
animals submitted to URB937 and SB366791……………..……..……………………56
Figure 18. Graph bar showing lower abdominal mechanical pain threshold using Von
Frey filaments in control animals, LPS-inflamed animals and animals administrated
with URB937………………………………...…………………………………………57
Figure 19. Graph bar of expression of Fos protein in control animals, LPS-inflamed and
in LPS and URB937..…………………………………………………………………..58
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 18
Abbreviations
ACh – Acetylcholine
APF – Antiproliferative factor
ATP – Adenosine triphosphate
BDNF – Brain derived neurotrophic factor
AEA - Anandamide
BPS - Bladder painful syndrome
BPS/IC – Bladder painful syndrome/ Interstitial cystitis
CAP - Capsaicin
CaMKII – Calmodulin-dependent Kinase II
CB1 – Cannabinoid receptor 1
CB2 – Cannabinoid receptor 2
EEC – European Economic Community
ESSIC – European Society for the Study of Interstitial Cystitis
FAAH – Fatty acid amide hydrolase
GAG-layer – Glycosaminoglycan-layer
IC – Interstitial Cystitis
ICS – International Continence Society
KO – Knockout
LPS – Lipopolysaccharide
L6 – Lumbar 6
NGF – Nerve growth factor
P2X3 – P2X purine receptor
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 19
PBS – Painful bladder syndrome
PHE – Phenylephrine
PIP2 – Phosphothylinositol (4,5)-biphosphate
PKA – Protein kinase A
PKC – Protein kinase C
PLA2 – Phopholipase A2
PLC – Phospholipase C
PLD – Phospholipase D
TH – Tyrosine hydroxylase
TRPV1 – Transient receptor potential vanilloid 1
SP – Substance P
WT – Wild type
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 21
I. Introduction
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 22
I. Introduction
1. Bladder painful syndrome/ Interstitial cystitis (BPS/IC)
1.1 Definition of BPS/IC
Bladder Painful Syndrome/Interstitial cystitis (BPS/IC) is a chronic pathology
characterized by supra-pubic pain related to bladder filling, frequently accompanied by
other lower urinary tract symptoms such as increased daytime and night-time
frequency, in the absence of proven urinary infection or other obvious pathology [1]. It
is a chronic debilitating and multifactorial syndrome with no long-term effective therapy
[1, 2]. The principal symptom of this syndrome is suprapubic pain [3], which might be
felt in other regions rather than the bladder [1, 2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15].
BPS/IC is more predominant in women [1]. BPS/IC has a great impact in the
psychological, social, economic, professional and personal life of patients with this
disease, so much that sometimes small and easy actions like travelling, recreation
activities with family and sleeping become very hard [1, 2].
This syndrome can be divided into two different subtypes: the classic subtype
and the nonclassic/ nonulcerative subtype [7, 11, 12, 16]. They differ in various
aspects, like histopathological characteristics, age distribution (patients with non-
ulcerative form being younger than patients with classic form), complications pattern
and response to treatment [12, 13]. Patients with classic BPS/IC exhibit pelvic pain, an
increase in urinary frequency and urgency and blood in urine [14]. Five to fifty patients
develop Hunner´s lesion (figure 1), which is a “circumscript, reddened mucosal area
with small vessels radiating towards a central scar, with a fibrin deposit or coagulum
attached to this area. With an increase in bladder distension this site can rupture and
lead to an edema” [14, 17]. These lesions can be confirmed by cystoscopy with
hydrodistension under general, epidural or local anesthesia by experienced urologists
and in some cases it may be necessary to make a biopsy to confirm Hunner´s lesion
and exclude a carcinoma [14]. Hunner’s lesion may also be confoundable with
glomerulations. However, the latter are areas of bleeding in the bladder wall and do not
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 23
lead automatically to a diagnosis of BPS/IC [14]. Presently it is still unclear if the non-
ulcer and classic subtypes represent different stages of a single disease or if they are
different diseases entities [14].
Figure 1. Hunner´s lesion in bladder from patients with BPS/IC, adapted from ESSIC (European Society for the study of BPS/IC) in
http://www.essic.eu/video_028images.html.
The designation of this syndrome has changed over the years. Initially, the
syndrome was called Interstitial Cystitis (IC) due to the presence of “typical cystoscopic
and histological features” on the bladder wall, which include inflammation in the deeper
layers of the bladder wall [1, 14, 18]. However, not all patients presented bladder
inflammation signs. Hence, the term IC was progressively changed to Painful Bladder
Syndrome (PBS) evidencing bladder pain instead of inflammation. The International
Continence Society (ICS) define PBS as “the complaint of suprapubic pain related to
bladder filling, accompanied by other symptoms such as increased daytime and night-
time frequency, in the absence of proven urinary infection or other obvious pathology”
[19]. However, this definition excluded 34% of the patients having bladder pain and
being classified by experts to have IC. So, the ESSIC group propose to give it the
name of bladder painful syndrome (BPS). ESSIC defines that “Bladder painful
syndrome would be diagnosed on the basis of chronic pelvic pain, pressure or
discomfort perceived to be related to the urinary bladder accompanied by at least one
other urinary symptom like persistent urge to void or urinary frequency, of more than
six weeks duration, in the absence of infection or other identifiable causes. Confusable
diseases as the cause of symptoms must be excluded. Further documentation and
classification of BPS might be performed according to findings at cystoscopy with
hydrosdistention and morphological findings in bladder biopsies” [14, 20]. However,
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 24
omitting the name “Interstitial cystitis” might cause serious problems in different health
systems, so it was decided that the name of Bladder Painful Syndrome/Interstitial
Cystitis could be used during the transition time [14].
Therefore, in this thesis, the term BPS/IC will be used now on, even when
referring to research where the anterior nomenclature was used.
1.2 Etiology of BPS/IC
The etiology of BPS/IC remains unknown, although several hypotheses have
been proposed, mostly linked to a dysfunction in the urothelium: Infection [1, 10, 11,
21, 22], Inflammation [1, 10, 13, 21, 22], Mast cell activation [1, 2, 11, 12, 21, 22, 23,
24], Urothelial dysfunction/ glycosaminoglycan (GAG)-layer defect [1, 2, 10],
Autoimmune mechanisms [1, 10, 13, 21, 22], Toxic agents [1, 22], among others.
1.3 Diagnosis of BPS/IC
The absence of a consensus definition for BPS/IC and the fact that the
symptoms are not specific (symptoms are very similar to other conditions, called
confoundable diseases) difficult the diagnosis of these patients. So, the diagnosis of
BPS/IC is a diagnosis of exclusion and the patients can remain undiagnosed for years
[24]. The diagnosis of BPS/IC, due to the lack of specific markers, is based on
symptoms described by the patients, such as pain, discomfort or pressure, and
exclusion of any identifiable infection [2, 7, 10, 22]. BPS/IC diagnosis also includes
cystoscopy with or without hydrodistention and may include biopsy to analyze mast cell
infiltration [7]. However, a negative result in all of these parameters does not exclude
BPS/IC. Occasionally, some patients do not exhibit abnormalities in the bladder, but
they have other BPS/IC symptoms. So, it is important to exclude all other confoundable
diseases, that could be the causes of the symptoms [5, 7, 22].
Furthermore, not all initial symptoms appear simultaneously but rather gradually
[24]. In the early stage of the disease, symptoms may be mild and intermittent, but they
tend to become constant and severe while the disease progresses [24]. Nocturia, for
example, tends to appear later in the progress of the disease and, commonly, women
report exacerbation of the symptoms during the premenstrual week [24]. Although the
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 25
median age of diagnosis of patients is 42-46 years old [24], the non-ulcer subtype of
BPS/IC is usually associated with younger age at diagnosis [22].
1.4 Epidemiology of BPS/IC
The prevalence of BPS/IC is difficult to estimate because of diagnosis
demands. Hence, the available information about BPS/IC prevalence is based on
different criteria. It is widely accepted that BPS/IC is more frequent in women than in
men, with a female/male ratio that ranges from 5:1 to 10:1 [12, 25]. Also, some studies
show that BPS/IC seems to be more frequent in Caucasians [7, 8, 10, 12, 24, 26].
However, one should not exclude that the cultural difference may reflect the different
frequency observed in those studies. Ito et al. say that BPS/IC is rare in Asian
countries with an incidence of 2 per 100000 urological patients [7, 27]. On the other
hand, the prevalence of BPS/IC in United States is 3-fold greater than the prevalence
in Europe [28]. Looking at the overall population, Moutzouris et al. estimate a
prevalence of 52 to 197 per 100000 women and 40 to 70 per 100000 men, diagnosed
by a physician [24].
1.5 Treatment of BPS/IC
Treatment of BPS/IC is not effective; it aims to reduce the symptoms and
improve the patient´s quality of life, focusing in pain and urological symptoms
(frequency and urgency). Presently, the most used treatments can be divided into four
groups: conservative therapy, oral medication, intravesical therapy and interventional
treatment and surgery [1, 2, 7, 11, 13, 18, 22, 26]. The conservative therapy includes
alterations in the quotidian of patients diagnosed with BPS/IC to improve their life´s
quality [1, 2, 7, 10, 22]. The oral medication includes a large variety of oral therapies,
aiming at reducing symptoms. However, this type of treatments present reduced
efficacy. Intravesical therapy consists on the application of a local anesthetic, alone or
with other drugs, directly into the bladder. Interventional treatment for patients with
BPS/IC include bladder distension, electromotive drug administration, transurethral
resection, botulinum toxin A and hyperbaric oxygen. Surgery is only used as a last
option [1, 2, 7, 10, 12, 14, 22].
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 26
2. Sympathetic nervous system dysfunction in BPS/IC
The relation between BPS/IC and the sympathetic nervous system was never
evaluated. However, it is known that patients with BPS/IC present high levels of urinary
catecholamines [29]. In 1999, Stein et al., showed that patients with BPS/IC have high
levels of urinary catecholamines when compared to urine from normal volunteers [29],
which may diffuse from sprouted sympathetic nerves in the mucosa and the detrusor,
and may contribute to alterations in the permeability of the GAG-layer [23, 29, 30].
Peeker and co-workers explored the neurogenic nature of BPS/IC,
determining by immunohistochemistry the presence and density of nerve fibers
containing tyrosine hydroxylase (TH, a sympathetic fibers marker) [12]. These authors
observed that the number of TH immunoreactive fibers was significantly increased in
BPS/IC patients when compared to control groups, suggesting an increase in the
activity of the peripheral sympathetic nervous system, and therefore indicating a
primary etiology [11, 12].
BPS/IC patients often exhibit an exaggerated response to stress, as observed
in patients with anxiety disorders [30]. This can be related with dysfunction of the
sympathetic nervous system [30, 31]. Furthermore, Charrua and co-workers
demonstrated through the TILT test (tilt table test) that BPS/IC patients presented an
increased sympathetic activity and confirmed an increase in noradrenaline levels in the
urine of BPS/IC patients [9, 29, 30]. These observations presume overstimulation of
adrenergic receptors present in the urinary bladder. The urinary bladder expresses
different subtypes of α-adrenoceptors and β-adrenoceptors. The most abundantly
expressed are the α1A, α1D and β3 subtypes. The α1A subtype is expressed in the
bladder urothelium and body [32, 33]. Curiously, it is thought that the α1A adrenoceptor
is activated only when an excess of norepinephrine exists in the urine or in the blood
[32]. The α1D subtype is expressed in the detrusor muscle, in the urothelium, and has
almost exclusively intracellular expression [32, 34, 35]. Both α- and β-adrenoceptors
are involved in mediating the responses to the endogenous noradrenaline [36]. β3
subtype is mainly expressed in the urothelium and when stimulated by mirabegron, a
β3 –adrenoceptor agonist, it decreases detrusor contractility and the urinary frequency.
So, the β3 subtype seems to not be involved in bladder pain or any change in bladder
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 27
morphology [36]. Therefore, the present study will focus on α-adrenoceptors, namely
on α1A and α1D.
2.1. Nociceptive pathway modulation by adrenoceptors
The overstimulation of adrenoceptors, in an animal model of rats chronically
treated with phenylephrine, leads to pain, vesical hyperactivity, alterations in urothelium
and mastocytosis, all signs and symptoms observed in patients with BPS/IC [30]. Pain
and increased void frequency were dependent on capsaicin-sensitive primary afferents
activation since desensitization of these fibers with high doses of capsaicin reverses
the phenylephrine-mediated effects [37, 38], demonstrating a possible relation between
the adrenergic and nociceptive activity. Hence, one of the aims of the present study is
to demonstrate the involvement of adrenoceptors in the appearance of BPS/IC
symptoms and that these receptors cross-talk with nociceptive receptors. In this study
we will focus on TRPV1, a receptor expressed in afferent bladder nerves, forming a
close contact with the bladder epithelium, in urothelial cells and in myofibroblasts [37,
38, 39, 40]. It has been suggested that TRPV1 is overexpressed in the bladder of
patients with BPS/IC [39, 41, 42]. Furthermore, it has been shown that the TRPV1
receptor is essential for pain arousal and for an increase in bladder frequency during
cystitis [43, 44].
One possible mechanism through which the adrenoceptor could act over TRPV1
is by an intracellular mechanism that will lead to its later sensitization. TRPV1 can be
sensitized through phosphorylation by different kinases, such as protein kinase A
(PKA), protein kinase C (PKC) and calmodulin-dependent kinase II (CaMKII), or by
membrane lipids such as phosphothylinositol (4,5)-biphosphate (PIP2), which is
cleaved by phospholipase (PLC) [45]. All these enzymes can be activated upon
adrenoceptors stimulation.
Another possible mechanism is that adrenoceptor activity can indirectly modulate
TRPV1 activity by acting on other receptors. Cannabinoid receptors are one example
[46]. The expression of cannabinoid receptor 1 (CB1), which co-localizes with TRPV1,
increases in patients with chronic bladder pain syndromes [47]. Furthermore, systemic
administration of cannabinoid agonists reduced pain induced by bladder inflammation
and increased the voiding interval [47], a mechanism that involves inhibition of bladder
afferent nerves [48]. TRPV1 and CB1 have common agonists, such as anandamide
[46, 49]. Anandamide is a lipid, which is an endocannabinoid, and can have analgesic
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 28
effects in animal models of inflammatory pain [49, 50]. Anandamide can be degraded
by FAAH (fatty acid amide hydrolase), an enzyme present in the human and rat
urothelium [50, 51, 52]. It is thought that when administrated at low doses, anandamide
acts on CB1, but at high doses, anandamide acts on TRPV1 [46, 47]. Although the
inhibition of FAAH by URB597, an inhibitor of FAAH, has been referred to suppress
peripheral hyperalgesia induced by bladder inflammation [50], no studies have been
conducted in BPS/IC.
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 30
II. Aims
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 32
II. Aims
This work has three main goals:
The first goal is to demonstrate the involvement of adrenoceptors in the
appearance of BPS/IC symptoms, by characterizing the adrenoceptors subtypes
involved in the appearance of pain and organ motility changes and by characterizing
which adrenoceptor subtypes are involved in the bladder histological changes
observed in rats submitted to chronic adrenergic stimulation.
The second aim is to evaluate the cross-talk between adrenoceptors and
TRPV1 during chronic adrenergic stimulation.
The third aim is to understand how endocannabinoids modulate bladder pain
and hyperactivity during cystitis.
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 34
III. Material and Methods
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 36
III. Material and Methods
1. Experimental Animals
Adult female Wistar rats (175-200g) and adult C57BL/6J mice (20-25g) were
bought from Charles River Laboratories (Barcelona, Spain). TRPV1 Knockout (KO)
mice (20-25g) were bought from Jackson Laboratories (Bar Harbor, Maine, USA). All
animals were maintained at 22 ᵒC, with 60% humidity, under inverted light-dark cycle
(12h/12h), and provided with water and food ad libitum. All experiments were
performed according to the European Communities Council Directive of 24 November
1986 (86/609/EEC), after approval from Ethical Committee of the Faculty of Medicine
of University of Porto and from Direcção Geral de Alimentação e Veterinária.
2. Chronic adrenergic stimulation
Chronic adrenergic stimulation was induced in mice and rats, by performing
daily subcutaneous injections, for 14 days, with 2.5 mg phenylephrine (PHE)/Kg body
weight (Sigma-Aldrich).
2.1. Blockade of alpha1-adrenoceptors
For α1-adrenoceptor subtype blockade, rats orally received specific α1-
adrenoceptor subtypes antagonists, concomitantly with the daily chronic adrenergic
stimulation (n=6 for each group) (see table 1). Rats receiving vehicle were used as
negative controls (group A). Rats receiving phenylephrine were used as positive control
(group B) (see attachment 1).
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 37
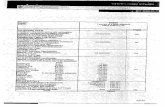
Table 1. Experimental groups of Wistar rats submitted to chronic adrenergic stimulation and alpha-adrenoceptors antagonists.
Group Treatment Dose
C α1A-AR antagonista (Silodosin (Urorec®, Recordati) 0.2 mg/ Kg
D α1D-AR antagonist (Naftopidi, *) 0.9375 mg/ Kg
E α1-AR antagonist (Prazosin, Sigma-Aldrich) 0.05 mg/ Kg
*Naftopidil was a kind gift from Prof. Igawa from Department of Continence Medicine, University of Tokyo, Tokyo, Japan
2.1.1. Pain behavior test
Visceral pain behavior tests were performed before and 14 days after beginning
the treatment, in all animals from all groups and treatments used.
Visceral pain behavior was evaluated using a mechanical hyperalgesia test,
adapted from Laird et al., 2001 [53]. Animals were placed in individual chambers (230x
170x 140 mm) with a wire mesh floor and allowed to acclimate for 20 min or until cage
exploration stopped (Figure 2a). This test was performed in the lower abdominal
region, and consists in touching this region with one of a series of Von Frey
monofilaments (rated at 4, 6, 8, 10, 15, 26 and 60g for rats, or rated 0.008, 0.02, 0.04,
0.07 and 0.16g for mice). Filaments were applied 5 seconds perpendicularly with
enough strength to cause the monofilament to slightly bend (see figure 2b). Each
monofilament was tested 5 times with an interval of 30 seconds between
monofilaments. It was considered a positive response when the animal reacted to the
filament (abdomen retraction or jump) in at least three of the five filament applications.
In case of no response to the filament, the next-stronger monofilament was applied.
Figure 2. Animals placed in individual chambers to perform visceral pain behavior test (figure 2a), in the lower abdominal region
using a series of Von Frey monofilaments (figure 2b), according to Laird et al., 2001 [53].
A
B
B
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 38
2.1.2. Organ motility test
Organ motility tests were also assessed before and 14 days after beginning the
treatment, in all animals from all groups and treatments used.
Urinary spots were used to analyze voiding frequency (urinary spots/ h). For
this, the animals were placed in boxes with filter paper during one hour (figure 3).
Figure 3. Animals placed into boxes with filter paper to analyze alterations on bladder motility.
2.1.3. Cystometry
In animals submitted to chronic adrenergic stimulation with PHE, cystometries
were performed at day 15 after beginning the treatment with PHE alone or with each
antagonist of α1-adrenoceptor subtypes, under anesthesia with urethane (1.2 g/ Kg
body weight, subcutaneously), with the body temperature maintained at 37ᵒC with a
heating pad. The bladder dome was exposed through a small, low abdominal incision.
A 20 gauge needle was inserted in the bladder dome and saline solution was infused
(6 mL/ h) (figure 4). After a period of 30 minutes of stabilization, the infusion of saline
solution was recorded for 2 hours, to analyze bladder reflex activity (number of bladder
contractions/ minute).
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 39
Figure 4. Animals under cystometry, over a heating pad and with a 20 gauge needle inserted in the bladder dome to infuse a saline solution.
2.1.4. Tissue harvesting and processing
Two hours after the beginning of cystometry, animals were transcardially
perfused with Tyrode´s solution followed by paraformaldehyde 4% (see attachment 2).
L6 spinal cord segments were harvested and sectioned at 40 µm. The urinary bladders
were harvested, fixed by immersion in 10% buffered formalin, for 24 hours, embedded
in paraffin, sectioned at 10-12 µm and mounted on poly-L-lysine-coated slip.
2.1.5. Immunohistochemistry
L6 spinal cord segments were sectioned and immunoreacted against Fos
protein, a pain and neuronal activity marker (see attachment 3 and 5 for a more
detailed protocol). The number of Fos immunopositive cells were determined under the
light microscopy Zeiss Axioskop 40.
Bladder sections were immunoreacted against caspase 3, a marker of cellular
apoptosis, to analyze urothelium integrity (see attachment 4 and 5 for a more detailed
protocol). Slides were observed under fluorescence microscope Zeiss Apotome and
images were acquired.
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 40
2.1.6. Bladder Histological Evaluation
To assess urothelium integrity, bladder sections were stained for Hematoxylin-
Eosin (see attachment 6 for a more detailed protocol) and the thickness of the
urothelium and the extension of lesion was determined using AxioVision 4.0.
To analyze mast cell infiltration, bladder sections were stained with Toluidine
Blue (see attachment 7 for a more detailed protocol). Images were acquired and the
number of mast cells was counted. Bladder mucosa areas were determined using
ImageJ 1.47v software.
2.2 Cross-talk between adrenoceptors and TRPV1
To evaluate the cross-talk between α-adrenoceptor and TRPV1, TRPV1
knockout mice (n=6) were submitted to chronic adrenergic stimulation with
phenylephrine for 14 days. Furthermore, a control group with wild type mice injected
with saline solution and a group of wild type mice injected with phenylephrine were
used (n=6 for each group). Pain behavioral tests (as described in 2.1.1) were
performed.
To verify if chronic adrenergic stimulation enhances TRPV1 response, adult
female Wistar rats (n=6) were submitted to chronic adrenergic stimulation with
phenylephrine daily for 14 days. At the end of treatment, animals were submitted to a
cystometry (as described in 2.1.3). After saline infusion, 50µM capsaicin (TRPV1
agonist, Sigma-Aldrich) was infused. This procedure was repeated in another group of
four animals injected with saline, used as control group (n=4).
3. Cannabinoid system and TRPV1 cross-talk during cystitis
3.1 LPS-induced cystitis
Cystitis was induced by intravesical instillation of 0.5 mL of lipopolysaccharide
(LPS, Sigma-Aldrich) 5 mg/ mL, for 1h, in female Wistar rats (n=6 for each drug
application). Control animals were instilled with saline solution (n=6).
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 41
3.2 Pain behavior test
Visceral pain behavior tests (as described in 2.1.1) were performed before
inflammation, 24h after LPS instillation and after 1 µM URB937 injection.
3.3 Cystometries
Twenty-four hours after LPS or saline instillation (n=6 for each drug application),
cystometry was performed as described in 2.1.3. After a period of 30 minutes of
stabilization, URB397 (Cayman Chemical Company) was given intravenously in doses
of 0.01, 0.1, 1, 5 and 10 µM (cumulative doses) to LPS- and saline-treated animals.
Since the dose most effective to reduce bladder reflex activity induced by
cystitis was 1µM of URB, it was used 1µM of URB937 + 10 µM MJ15 (CB1 antagonist,
Tocris Bioscience), 1µM URB937 + 0.3 mg/ Kg SR144528 (CB2 antagonist, Cayman
Chemical Company) to determine the involvement of each cannabinoid receptor in
FAAH induced blockade.
Since 7 mg/kg induced bladder hyperactivity, 1µM URB937 + 1.4 µg/ Kg
SB366791 (TRPV1 antagonist, Tocris Bioscience) were used to analyze the
involvement of TRPV1.
At the end of the cystometry, bladders were harvested and the cystitis was
confirmed histologically.
4. Data presentation
Data are presented as mean ± standard deviation and comparison between the
paired data were performed by using the Student´s t test. For multiple comparisons, the
statistical analysis was performed using the Dunn’s Multiple Comparisons Test
(ANOVA – One-way analysis of variance non-parametric). P values inferior to 0.05
were considered statistically significant.
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 43
IV. Results
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 45
IV. Results
1. Blockade of alpha1-adrenoceptors
1.1 Pain behavior test
Control animals presented a score of 41.2 ± 21. It was observed that animals
treated with PHE had a decreased mechanical pain threshold compared with the
control, with a score of 6.7 ± 2.4 (P<0.001, figure 5). The blockade with Silodosin or
Prazosin reversed the effect of PHE to 20.8 ± 19.3 and 14.2 ±7.0, respectively.
Naftopidil was unable to reverse PHE induced referred pain, 6.0 ± 2.5 (P<0.001, figure
5).
Figure 5. Graph bar showing lower abdominal mechanical pain threshold using Von Frey filaments. After chronic adrenergic
stimulation with 2.5 mg of PHE/kg body weight, animals presented a decrease in the mechanical pain threshold (*** P < 0.001 comparing to control). Co-treatment with silodosin and prazosin abolished abdominal mechanical pain threshold. Naftopidil was
unable to reverse PHE effect (*** P<0.001).The statistical analysis were performed using the Dunn’s Multiple Comparisons Test
(ANOVA – One-way analysis of variance non-parametric).
0,0
10,0
20,0
30,0
40,0
50,0
60,0
70,0
Control PHE PHE +Silodosin
PHE +Naftopidil
PHE +Prazosin
Fila
me
nt
(g)
Visceral pain test
***
***
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 46
1.2 Organ motility test
Control animals had 2.8 ± 1.0 urinary spots/ h. PHE treatment induced an
increase in the number of urinary spots/ h to 7.8 ± 3.3, when compared to control group
(P<0.05, figure 6). In animals submitted to treatment with PHE concomitantly with
Silodosin or Prazosin the number of urinary spots/ h is similar to control animals, 4.8 ±
3.3 and 4.3 ± 4.6 urinary spots/h, respectively (figure 6). Animals treated with Naftopidil
had an increase in the number of urinary spots/h to 9.2 ± 2.6 (P<0.01) (figure 6).
Figure 6. Graph bar showing the voiding frequency (urinary spots/ h) of control animals, animals submitted to chronic adrenergic stimulation with PHE (PHE group) and animals submitted to chronic adrenergic stimulation with PHE and α-adrenoceptors
antagonist (group PHE+ Silodosin, PHE+ Naftopidil and PHE+ Prazosin). The statistical analysis were performed using the
Dunn’s Multiple Comparisons Test (ANOVA – One-way analysis of variance non-parametric).
1.3 Cystometry
Control animals had 0.4 ± 0.1 bladder contractions/ min. PHE treated animals
had an increased bladder reflex activity, reading values of 1.9 ± 0.9 bladder
contractions/min (P<0.001, figure 7). Adrenoceptors antagonists Silodosin or Prazosin
were able to reverse PHE-induced bladder reflex activity to values of 0.7 ± 0.2 and 0.7
± 0.2 bladder contractions/ min, respectively (figure 7). Co-treatment with Naftopidil
also increased bladder reflex activity to 1.9 ± 0.4 bladder contractions/ min (P<0.001)
(figure 7).
0,0
2,0
4,0
6,0
8,0
10,0
12,0
14,0
Control PHE PHE +Silodosin
PHE +Naftopidil
PHE +Prazosin
Uri
nar
y sp
ots
/ h
Urinary spots
*
**
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 47
Figure 7. Graph bar showing the bladder reflex activity (bladder contractions/ minute) of control animals, animals submitted to
chronic adrenergic stimulation with PHE (PHE group) and animals submitted to chronic adrenergic stimulation with PHE and α-adrenoceptors antagonist (group PHE+ Silodosin, PHE+ Naftopidil and PHE+ Prazosin). The statistical analysis were performed
using the Dunn’s Multiple Comparisons Test (ANOVA – One-way analysis of variance non-parametric).
1.4 Immunohistochemistry
The L6 spinal cord segment of control animals had 5 ± 3 immunopositive cells.
PHE treated animals had an increase in the number of Fos immunopositive cells/
section to 33 ± 6 (P<0.01, figure 8). The blockade with Silodosin or Prazosin reverses
the effect induced by PHE to 8 ± 3 and 4 ± 0.5, respectively. Blockade with Naftopidil
also increased the number of Fos immunoreactive cells for 21 ± 7 (P<0.05) (figure 8).
0,00
0,50
1,00
1,50
2,00
2,50
3,00
Control PHE PHE +Silodosin
PHE +Naftopidil
PHE + Prazosin
Bla
dd
er
con
trac
tio
ns/
min
Bladder reflex activity
***
***
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 48
Figure 8. Graph bar showing the spinal Fos expression (number of Fos immunopositive cells/ section). Chronic adrenergic
stimulation with 2.5 mg PHE/ kg body weight, increase the number of Fos immunopositive cells/ section (** P<0.01).Co-treatment with Silodosin or Prazosin reverse the effect induced by PHE. Treatment with Naftopidil also increase spinal Fos expression. The
statistical analysis were performed using the Dunn’s Multiple Comparisons Test (ANOVA – One-way analysis of variance non-
parametric).
.
Bladder sections from control animals showed no staining for caspase 3 (figure
9A). The bladder of animals that received chronic adrenergic stimulation presented
caspase 3 staining in the urothelium (figure 9B). Naftopidil induced cellular apoptosis,
as observed by caspase 3 staining (figure 9D). Bladder of animals that received
Silodosin or Prazosin, were not stained for caspase 3 (figure 9C and 9E, respectively).
Figure 9. Bladder sections immunoreacted against caspase 3. A) control group. B) PHE group. C) PHE and Silodosin. D) PHE and
Naftopidil. E) PHE and Prazosin.
0
5
10
15
20
25
30
35
40
45
Control PHE PHE+Silodosin
PHE+Naftopidil
PHE+Prazosin
Nº
of
Fos
IR+
cells
/se
ctio
n
Spinal Fos expression
A B
C
D E
**
*
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 49
1.5 Bladder histological evaluation
Bladder sections from controls stained for Hematoxylin-Eosin exhibited an
urothelium without disruption. Treatment with PHE and antagonists (Naftopidil or
Prazosin) increased the percentage of low urothelium to 53% ± 15, 82% ± 14 and
46.9% ± 17,7, respectively (P<0.001, figure 10). Adrenoceptor antagonist Silodosin
reversed the effect of PHE for 12% ± 13 (figure 10).
Figure 10. Graph bar showing the urothelium integrity (percentage of low urothelium) of bladder sections stained with
Hematoxylin-Eosin. PHE, PHE +Naftopidil and PHE +Prazosin increase the percentage of low urothelium (*** P<0.001). Administration of Silodosin or Silodosin + Naftopidil reverses the effect induced by PHE. The statistical analysis were performed
using the Dunn’s Multiple Comparisons Test (ANOVA – One-way analysis of variance non-parametric).
Bladder sections from control animals stained for Toluidine Blues presented 8 ±
4 mast cells/ mm2 (figure 11). Treatment with PHE increased the number of mast cells
in mucosa layer to 17 ± 6 (P<0.05, figure 11). Co-administration of PHE and Naftopidil
also increased the number of mast cells/ mm2 to 20 ± 5 (P<0.01, figure 11).
Adrenoceptors antagonists Silodosin or Prazosin reversed the effect of PHE to values
of 14 ± 4 and 16 ± 8, respectively (figure 11).
0,0
20,0
40,0
60,0
80,0
100,0
Control PHE PHE +Silodosin
PHE +Naftopidil
PHE +Prazosin
Pe
rce
nta
ge o
f lo
w u
roth
eliu
m
Urothelium Integrity
***
***
***
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 50
Figure 11. Graph bar showing the mast cells (mast cells/ mm2) in bladder sections stained with Toluidine Blue. PHE increase the
number of mast cells (* P<0.05).Co-treatment with Naftopidil also increase the number of mast cells (** P< 0.01). Administration
of Silodosin or Prazosin reverses the effect induced by PHE. The statistical analysis were performed using the Dunn’s Multiple Comparisons Test (ANOVA – One-way analysis of variance non-parametric).
2. Cross-talk between adrenoceptors and TRPV1
2.1 Pain behavior test
Control animals (WT saline) had a score of 0.09 ± 0.06 (figure 12). Chronic
adrenergic stimulation in wild type animals decreased mechanical pain threshold
compared to control to 0.008 ± 0.0 (P<0.05, figure 12). Administration of PHE to
knockout (KO) TRPV1 animals increased the pain threshold to values similar to those
of the control group (figure 12).
0
5
10
15
20
25
30
control PHE PHE +Silodosin PHE +Naftopidil PHE +Prazosin
Mas
t ce
lls/
mm
2
Mast cells
*
**
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 51
Figure 12. Graph bar showing lower abdominal mechanical pain threshold using Von Frey filaments. PHE administration to WT animals decrease pain threshold (*P<0.05). The statistical analysis were performed using the Dunn’s Multiple Comparisons Test
(ANOVA – One-way analysis of variance non-parametric).
2.2 Cystometry
Control animals under cystometry presented a value of 0.58 ± 0.21 bladder
contractions/ minute. Administration of 50 µM of capsaicin to these animals increased
the number of bladder contractions to 0.90 ± 0.18, presenting a variation of 0.33 ± 0.15
(figure 13). Animals treated with PHE had 1.73 ± 1.02 bladder contractions/ minute
(figure 13). Capsaicin administration increased the number of bladder contractions to
2.68 ± 1.28, when compared to animals treated with PHE (figure 13), presenting a
variation of 0.95 ±0.37 (figure 13).
Figure 13. Graph bar of bladder reflex activity (bladder contractions/ minute) evaluated during cystometry with saline and capsaicin
(CAP) in control Wistar rats and in female Wistar rats submitted to chronic adrenergic stimulation with PHE.
0,00
0,05
0,10
0,15
0,20
WT saline WT PHE KO TRPV1 PHE
Fila
me
nt
(g)
Visceral pain test
0,00
0,20
0,40
0,60
0,80
1,00
1,20
1,40
Control PHE
DFr
eq
ue
ncy
Bladder reflex activity
*
*
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 52
3. Cannabinoid system and TRPV1 cross-talk during cystitis
3.1 Cystometries
Control animals presented 0.5 ± 0.1 bladder contractions/ minute. Animals with
cystitis presented an increase in the number of bladder contractions/ minute to 2.1 ±
0.6 (figure 14). 1µM of URB937 reversed the bladder hyperactivity (0.7 ± 0.2 bladder
contractions/ minute in LPS-treated animals, figure 14). 5 µM and 10 µM of URB937
increased bladder hyperactivity (1.3 ± 0.4 and 2.4 ± 0.8 bladder contractions/ minute,
respectively, in LPS-treated animals, figure 14).
Figure 14. Line graph of bladder reflex activity of control animals and LPS-treated animals submitted to different concentrations of URB937.
Control animals instilled with vehicle had 0.5 ± 0.1 bladder contractions/ minute.
Administration of URB937 1µM alone or concomitantly with CB2 antagonist SR144528
to control animals did not change the bladder reflex activity (0.5 ± 0.2 and 0.4 ± 0.1,
respectively, figure 15).
Animals with cystitis (n=6) had 0.9 ± 0.1 bladder contractions/ minute.
Administration of URB937 alone or co-administrated with CB2 antagonist SR144528 in
these animals did not change significantly the number of bladder contractions (0.7 ±
0.2 and 0.55 ± 0.07, respectively) (figure 15).
0,0
0,5
1,0
1,5
2,0
2,5
3,0
3,5
saline 0.01 µM 0.1 µM 1 µM 5 µM 10 µM
Bla
dd
er
con
trac
tio
ns/
min
URB (mM)
Bladder reflex activity
LPS
control
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 53
Figure 15. Graph bar of bladder reflex activity of control animals and LPS-treated animals submitted to URB937 and SR144528 (CB2 antagonist). Administration of URB937 alone or with CB2 antagonist decrease the number of bladder contractions/ minute.
The statistical analysis were performed using the Dunn’s Multiple Comparisons Test (ANOVA – One-way analysis of variance non-
parametric).
Control animals instilled with vehicle had 0.5 ± 0.1 bladder contractions/ minute
(figure 16). Administration of URB937 1µM alone or concomitantly with CB1 antagonist
MJ15 to these animals did not change the bladder reflex activity (0.5 ± 0.2 and 0.6 ±
0.2, respectively, figure 16).
Animals with cystitis (n=6) had 1.42 ± 0.23 bladder contractions/ minute
(P<0.001 compared to control). Administration of URB937 in these animals decreased
the number of bladder contractions to 0.7 ± 0.2 (figure 16). Animals administrated with
URB and the CB1 antagonist (MJ15) had an increase in bladder reflex activity to 1.9 ±
0.8 (P<0.01) compared with LPS-inflamed animals instilled with vehicle (figure 16).
0,0
0,2
0,4
0,6
0,8
1,0
Vehicle URB 1uM URB 1uM +SR144528(CB2 antagonist)
Bla
dd
er
con
trac
tio
ns/
min
Bladder reflex activity
Naive animals
LPS-inflamedanimals
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 54
Figure 16. Graph bar of bladder reflex activity of control animals and LPS-inflamed animals submitted to URB937 and MJ15 (CB1
antagonist). LPS-inflamed animals have an increase in the number of bladder contractions, when compared to control (*** P<0.001). Administration of URB937 in LPS-inflamed animals reduces the number of bladder contractions/ minute. Co-
administration of URB937 and CB1 antagonist increase bladder reflex activity (** P<0.01). The statistical analysis were performed
using the Dunn’s Multiple Comparisons Test (ANOVA – One-way analysis of variance non-parametric).
Control animals (n=3) instilled with vehicle had 0.4 ± 0.2 bladder contractions/
minute (figure 17). Administration of URB937 1 µM alone or concomitantly with TRPV1
antagonist SB366791 did not change the bladder reflex activity (0.4 ± 0.2 and 0.4 ± 0.2,
respectively, figure 17).
Animals instilled with LPS (n=3) and vehicle had 1.2 ± 0.2 bladder contractions/
minute. Administration of URB937 on animals with cystitis increased the number of
bladder contractions to 2.4 ± 0.8 (figure 17). Co-administration of URB937 and TRPV1
antagonist SB366791 in LPS-inflamed animals decreased the number of bladder
contractions/ minute to 1.3 ± 0.6 (figure 17).
0,0
0,5
1,0
1,5
2,0
2,5
3,0
Vehicle URB 1uMURB 1 uM +MJ15 (CB1 antagonist)
Bla
dd
er
con
trac
tio
ns/
min
Bladder reflex activity
Naive animals
LPS-inflamedanimals
***
**
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 55
Figure 17. Line graph of bladder reflex activity of control animals and LPS-inflamed animals submitted to URB937 and SB366791
(TRPV1 antagonist). Administration of URB937 in LPS-inflamed animals increases the number of bladder contractions/ minute. Co-administration of URB937 and TRPV1 antagonist in LPS-inflamed animals decrease the number of bladder contractions/
minute. The statistical analysis were performed using the Dunn’s Multiple Comparisons Test (ANOVA – One-way analysis of
variance non-parametric).
3.2 Pain behavior test
Control animals presented a score of 18 ± 7. Animals with cystitis had a
decreased mechanical pain threshold compared with the control, with values of 1 ± 1
(P<0.001, figure 18). Administration of 1µM of URB937 increased the pain threshold to
7 ± 3 (figure 18), when compared to control group.
0,0
0,5
1,0
1,5
2,0
2,5
3,0
3,5
Vehicle URB 10 uM URB 10uM+SB366791 (TRPV1
antagonist)
Bla
dd
er
con
trac
tio
ns/
min
Bladder reflex activity
naive animals
LPS- treated animals
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 56
Figure 18. Graph bar showing lower abdominal mechanical pain threshold using Von Frey filaments. Instillation of LPS decreases
the pain score (*** P<0.001). Administration of URB937 increased pain threshold. The statistical analysis were performed using the
Dunn’s Multiple Comparisons Test (ANOVA – One-way analysis of variance non-parametric).
3.3 Immunohistochemistry
Control animals had 5 ± 3 Fos immunopositive cells/ section (figure 19).
Instillation of LPS increased the number of Fos immunopositive cells/ section to 31 ±
12 (P<0.01, figure 19).
Animals instilled with LPS and administrated with URB937 had a decrease in
the number of Fos immunopositive cells/ section to 15 ± 8 (P<0.05, figure 19).
0
5
10
15
20
25
30
Control LPS URB
Fila
me
nt
(g)
Visceral pain test ***
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 57
Figure 19. Graph bar of expression of Fos protein in control animals, LPS-inflamed animals and in LPS+1µM URB937. Instillation
of LPS increase the number of Fos immunopositive cells, when compared to control (** P<0.01). Animals instilled with LPS and administrated with URB937 had a decrease in the number of Fos immunopositive cells, when compared to LPS-inflamed animals (*
P<0.05). The statistical analysis were performed using the Dunn’s Multiple Comparisons Test (ANOVA – One-way analysis of
variance non-parametric).
0
5
10
15
20
25
30
35
40
45
Control LPS LPS+ 1 uM URB
Nu
mb
er
of
Fos-
exp
ress
ing
cells
Expression of Fos protein
** *
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 59
V. Discussion
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 61
V. Discussion
The major outcomes of the present work were:
1. Alpha1A-adrenoceptors mediate pain induced by chronic adrenergic
stimulation;
2. Chronic adrenergic stimulation-mediated effects occur through a TRPV1-
dependent mechanism, which involves the receptor sensitization;
3. Endocannabinoids modulate visceral pain and bladder activity, through CB1
and TRPV1 receptor, during cystitis.
1. Alpha1A-adrenoceptors mediate pain induced by chronic adrenergic
stimulation
The present experiments confirm that chronic adrenergic stimulation with PHE
induces visceral pain behavior in animals and bladder hyperactivity, which are a
characteristic exhibited by BPS/IC patients [30]. Administration of PHE and Silodosin
(α1A-adrenoceptor antagonist) reversed visceral pain behavior and reversed the
bladder hyperactivity induced by PHE. It is known that urinary bladder express alpha-
adrenoceptors [54, 55, 56, 57, 58, 59]. The α1-adrenoceptors can be found throughout
the urinary bladder [34, 35, 60]. In the bladder of healthy individuals, there is no
evidence of an outstanding alpha-adrenergic stimulation. However, under pathologic
conditions, it is known that there is an increase in the density of α-adrenoceptors,
insomuch, that the noradrenaline-induced response in the bladder is converted from
relaxation to contraction [54], which can contribute to the bladder hyperactivity
observed in some disorders like BPS/IC.
In the present work, the animals under chronic adrenergic stimulation also
presented an increase in spinal Fos protein expression, indicating that PHE induces
activation of nociceptive pathways coming from the bladder. Patients with BPS/IC
present an increase both in nociceptive fibers containing substance P (SP) and in
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 62
urinary substance P [2, 61, 62]. This increase has a positive correlation with the
severity of pain felt by those patients [2]. The reduction of Fos expression by the
blockade of α1A-adrenoceptor suggest that this receptor alters the activity of primary
afferents. Its blockade may lead to a decrease the transmission of nociceptive
information to central nervous system, which could result in a decrease in pain and
vesical activity.
Chronic adrenergic stimulation with PHE induced mast cell infiltration, a sign
similar to the one observed in patients with BPS/IC [1, 2, 6, 9, 26]. This could be a
consequence of nociceptive fibers activation since the release of SP is known to cause
degranulation and activation of mast cells present nearby nerve terminals [2]. The
blockade of α1A-adrenoceptor inhibited mast cell migration induced by mast cell
activation, showing that this receptor is somehow involved in the chemotaxis of these
inflammatory cells. Hence, α1A-adrenoceptor blockers present themselves as good
targets to overcome pain and inflammation associated with BPS/IC.
Chronic adrenergic stimulation also induced urothelium disruption as observed
by an increase in the percentage of degraded urothelium and the immunoreactivity for
the pro-apoptotic molecule caspase 3. Patients with BPS/IC exhibit disruption in the
urothelium similar to the ones observed in the present work [1, 2, 6, 9, 23]. In fact, it
was observed that the urothelium from BPS/IC patients was immunopositive for
caspase 3 [63, 64]. Charrua et al. has observed that the urothelium from animals
submitted to chronic adrenergic stimulation with PHE was immunopositive for caspase
3 [30]. The blockade of α1A-adrenoceptor reversed the urothelium damage induced by
PHE, possible by blocking apoptosis, showing that this effect resulted from adrenergic
overactivity. The urothelium has a barrier function, to prevent the diffusion of urine
constituents for the underlying tissues [14, 65]. Urothelial damage allows the diffusion
of urinary solutes which may activate sensory nerve endings, leading to pain,
inflammation and urinary frequency. Hence, the reversion of urothelium damage will
possible contributes to an improvement of all other symptoms observed in BPS/IC
patients. In fact, patients that receive pentosan polysulfate sodium, known to decrease
the permeability of urothelium, reported an improvement of pain, urgency and
frequency [1, 7, 13, 18, 22].
Chronic adrenergic stimulation with phenylephrine increased bladder reflex
activity, as previous demonstrated by Charrua et al. [30]. The increase in bladder reflex
activity can be translated as an increase in the number of bladder contraction per
minute, which means that the urinary frequency increases. This increase in urinary
frequency is also reported in patients with BPS/IC [1, 2, 4, 22]. The blockade of α1A-
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 63
adrenoceptor reverses the increase in bladder reflex activity, which means that, under
pathologic conditions, this receptor is involved in the increase of urinary frequency.
2. Chronic adrenergic stimulation-mediated effects occur through a TRPV1-
dependent mechanism, which involves the receptor sensitization
Pain and increased frequency were dependent of capsaicin sensitive primary
afferents activation since desensitization of these fibers with capsaicin reverses the
phenylephrine mediated effect [40, 41]. These results indicate that there is relation
between adrenergic activity and nociceptive activity. TRPV1 has been shown to be
essential for the development of bladder pain and hyperactivity during cystitis [38, 43,
46] being the urinary bladder nociceptive receptor per excellence [37, 38, 39, 63]. In
fact, TRPV1 is overexpressed in the urinary bladder of patients with BPS/IC [39, 41,
42].
Hence, in this work it was hypothesized that adrenoceptors interact with TRPV1
inducing the PHE-mediated effects. In fact, TRPV1 knockout mice chronically treated
with PHE did not feel pain nor presented any of the bladder changes observed in their
wild type littermates. These results show that TRPV1 activity is downstream to α-
adrenoceptors activation.
It was also hypothesized that adrenoceptor sensitized TRPV1 by an intracellular
mechanism. In the present work it was observed that PHE-treated animals had higher
bladder frequency upon capsaicin stimulation than control animals. This seems to point
to a sensitization of TRPV1. In fact, α-adrenoceptors activation is known to trigger the
Gq/11 signaling pathway, therefore promoting the activation of phospholipase C (PLC),
phospholipase A2 (PLA2) and phospholipase D (PLD) [37, 38]. In turn, these enzymes
lead to mobilization of Ca2+ from intracellular stores and activation of mitogen-activated
kinase and phosphathylinositol (4,5)-biphosphate (PIP2) kinase pathways, which
causes vasoconstriction. The influx of calcium and the consequential increase of
intracellular calcium concentration are necessary for the desensitization of TRPV1.
Many signaling pathways, like calmodulin (CaM) and the decrease of PIP2, are
implicated in desensitization of TRPV1 [37, 66]. The process of sensitization of TRPV1
is made by phosphorylation, by different kinases, like protein kinase A (PKA), protein
kinase C (PKC) and calmodulin-dependent kinase II (CaMKII), or by membrane lipids
such as PIP2, which is cleaved by phospholipase (PLC). It is known that TRPV1 needs
to be phosphorylated by CaMKII to be activated by vanilloids [67]. All these enzymes
are known to sensitize TRPV1 [68].
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 64
3. Endocannabinoids modulate visceral pain and bladder activity, through CB1
and TRPV1 receptor, during cystitis
The administration of URB937 did not produce any effect on the bladder
frequency nor pain behavior of control animals. Furthermore, administration of URB937
concomitantly with exogenous cannabinoids, such as SR144528, MJ15 or SB366791,
also did not produce any effect on bladder frequency.
The administration of 1 mM URB937 to animals with cystitis reversed bladder
hyperactivity. However, at doses of 5 and 10 mM URB937 induced an increase of
bladder frequency. FAAH blockade increases endocannabinoids levels [49].
Anandamide (AEA) is one of those molecules. AEA is known to act both in CB1 and
TRPV1 receptors, which are co-expressed in most nociceptive primary sensory
neurons in bladder [46, 47].
In fact, previous work has demonstrated that anandamide could contribute to
the development of hyperalgesia and hyperreflexia by activating TRPV1 [46]. Hence, it
was hypothesized that when low doses of URB are used, endocannabinoids levels may
reach a plateau that lead to CB1 activation. Increasing endocannabinoids levels by
further blocking FAAH, they will act on TRPV1. In fact, the reversion of 1 mM URB
effect by blocking CB1 receptor demonstrated the involvement of this receptor.
It is known that administration of cannabinoid agonists reduce pain induced by
bladder inflammation [47]. In this work, FAAH inhibition reversed bladder pain induced
by inflammation. This result is corroborated by a decrease in Fos expression at L6
spinal cord level after URB937 application. Altogether these results suggest that FAAH
inhibition and, subsequently, endocannabinoids are involved in the activation of
nociceptive pathways.
In summary, it is possible that during bladder painful syndrome/ interstitial
cystitis there is an interaction between several pathways, namely α1A-adrenoceptors,
TRPV1 and CB1, as shown in the following schematic drawing:
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 67
VI. Conclusion
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 69
VI. Conclusion
The present work confirmed that chronic adrenergic stimulation with
phenylephrine induces visceral pain, mast cell infiltration, apoptosis of urothelial cells
and activation of nociceptive pathways. Silodosin (antagonist of α1A-adrenoceptor
subtype) seems to be more effective than naftopidil or prazosin (α1D and α1-
adrenoceptor antagonist) to reduce the effects induced by chronic adrenergic
stimulation with phenylephrine.
According to previous studies, this work showed that TRPV1 are involved in
bladder hyperactivity, as well as CB1. However, it is necessary more studies to better
understand the role of these receptors in bladder hyperactivity, a characteristic of
BPS/IC.
Thus, we can conclude that BPS/IC results from the activation and the cross-
talk between different pathways, possibly involving α-adrenoceptors, TRP channels
(TRPV1 and possibly TRPV4) and cannabinoid receptors (CB1).
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 71
VII. Future work
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 73
VII. Future work
This work allows characterizing the adrenoceptors subtypes involved in pain,
organ motility and bladder histological changes in an animal model of BPS/IC. These
results suggest that silodosin (antagonist of α1A-adrenoceptor subtype) seems to be
more effective to reduce the effects induced by chronic adrenergic stimulation with
phenylephrine. Furthermore, BPS/IC seems to be a result of the cross-talk between
different pathways, involving α-adrenoceptors, TRPV1 and cannabinoid receptors
(CB1). However the role of these receptors in bladder hyperactivity is not completely
understood.
Besides TRPV1 and CB1, there are more nociceptive receptors such as P2X3,
which could be also involved in bladder hyperactivity [69]. Activation of P2X3 and TRP
channels by bladder distension or chemical stimuli can release some mediators like
ATP, Ach (acetylcholine) and NGF (nerve growth factor) [70]. It is also known that
patients with BPS/IC present altered levels of APF (anti-proliferative factor), NGF,
BDNF (brain derived nerve factor), and interleukins, among others [71].
Some authors, observed a decrease in the microvascular density in the
suburothelium in patients with BPS/IC, suggesting that hypoxia can be a cause of the
disease [1, 25]. To clarify this idea, would be interesting to study the effect of chronic
bladder ischemia in bladder function and morphology and in sympathetic activity, using
a rat model of atherosclerosis-induced chronic bladder ischemia.
Thus, there are many questions that can be studied in a future work. Which are
the connections between the adrenoceptor pathways and the nociceptive pathways,
namely at the expression and function of TRP (TRPV1 and TRPV4) receptors? What
are the roles of CB1 and P2X3 in this process? Will NGF, BDNF and interleukins be
involved in BPS/IC? How ischemia influences BPS/IC characteristics? Can ischemia
stimulus induce sympathetic overactivity and how these can induce the changes
observed in patients with BPS/IC?
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 74
The role of TRPV4 and P2X3 can be assessed using PHE-treated animals
administrated with agonists and antagonists of these receptors and using co-cultures of
DRG and urothelial cells treated with PHE. The activity of these receptors can be
determined by calcium imaging technique.
To assess the role of neurothrophins and interleukins, control animals and
ovariectomized animals can be submitted to chronic adrenergic stimulation with PHE
for 14 days. Urine samples can be collected before, at day 8 and day 14 after
beginning the treatment, to determine neurothrophins and interleukins levels by ELISA.
The levels of neurothrophins and interleukins can also be determined in urine from
BPS/IC patients and aged matched normal volunteers.
To verify if an ischemic stimulus induces chronic sympathetic overactivity and
verify whether this sympathetic overactivity induces bladder changes observed in
BPS/IC patients, that an animal model of atherosclerosis-induced chronic bladder
ischemia, like described by Nomiya et al., 2012 [72], can be used.
After ischemic insult and at different time points, the levels of plasmatic and
urine noradrenaline can be measured by ELISA and HPLC. Organ expression of
tyrosine hydroxylase and dopamine-β-hydroxylase, by immunohistochemistry and
western blot, respectively, can be also assessed. Furthermore, visceral pain behavior
and organ motility and integrity can be evaluated at different point times, as well as
spinal Fos expression and inflammatory signs.
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 76
VIII. References
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 78
VIII. References
[1] International Continence Society (ICS) – Incontinence: Management. Abrams P,
Cardozo L, Khoury S, Neim A. Edition 2005, volume 2, chapter 23 by P. Hanno
[2] Marshall K. Interstitial cystitis: understanding the syndrome. Altern Med Rev. 2003,
8(4): p. 426-436
[3] Patel R, Calhoun EA, Meenan RT, O’Keeffe Rosetti MC, Kimes T, Clemens JQ.
Incidence and clinical characteristics of interstitial cystitis in the community. Int
Urogynecol J Pelvic Floor Dysfunct. 2008, 19(8): p. 1093-1096
[4] Birder LA, Hanna-Mitchell AT, Mayer E, Buffington CA. Cystitis, co-morbid disorders
and associated epithelial dysfunction. Neurourol Urodyn. 2011, 30(5): p. 668-672
[5] Chelimsky G, Heller E, Buffington CA, Rackley R, Zhang D, Chelimsky T. Co-
morbidities of interstitial cystitis. Front Neurosci. 2012, doi: 10.3389/fnins.2012.00114
[6] French L, Bhambone N. Interstitial cystitis/ painful bladder syndrome. Am Fam
Physician. 2011, 83(10): p. 1175-1181
[7] International Painful Bladder Foundation (IPBF) – Interstitial Cystitis/ Bladder Pain
Syndrome: Diagnosis & Treatment. Jane M. Meijlink. Edition 2013. ISBN number: 90-
810327-1-2
[8] Ito T, Ueda T, Homma Y, Takei M. Recent trends in patient characteristics and
therapeutic choices for interstitial cystitis: analysis of 282 Japanese patients. Int J Urol.
2007, 14(2): p. 1068-1070
[9] Lutgendorf SK, Latini JM, Rothrock N, Zimmerman MB, Kreder KJ Jr. Autonomic
response to stress in interstitial cystitis. J Urol. 2004, 172(1): p. 227-231
[10] Nickel J Curtis. Interstitial cystitis: etiology, diagnosis and treatment. Can Fam
Phys. 2000, 46: p. 2430-2440
[11] Payne RA, O’ Connor RC, Kressin M, Guralnick ML. Endoscopic ablation of
Hunner´s lesion in interstitial cystitis patients. Can Urol Assoc J. 2009, 3(6): p. 473-477
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 79
[12] Peeker R, Aldenborg F, Dahlström A, Johansson S, Li JY, Fall M. Increased
tyrosine hydroxylase immunoreactivity in bladder tissue from patients with classic and
nonulcer interstitial cystitis. J Urol. 2000, 163(4): p. 1112-1115.
[13] Peeker R, Fall M. Treatment guidelines for classic and non-ulcer Interstitial cystitis.
Int Urogynecol J. 2000, 11: p. 23-32
[14] van de Merwe JP, Nordling J, Bouchelouche P, Bouchelouche K, Cervigni M,
Daha K, Elneil S, Fall M, Hohlbrugger G, Irwin P, Mortensen S, van Ophoven A,
Osborne JL; Peeker R, Richter B, Riedl C, Sairanen J, Tinzl M, Wyndaele JJ.
Diagnostic criteria, Classification and Nomenclature for Painful Bladder Syndrome/
Interstitial cystitis: An ESSIC proposal. Eur Urol. 2008, 53(1): p. 60-67
[15] Tripp DA, Nickel JC, Wong J, Pontari M, Moldwin R, Mayer R, Carr LK, Doggweiler
R, Yang CC, Mishra N. Nordling J. Mapping of pain phenotypes in female patients with
bladder pain syndrome/ interstitial cystitis and controls. Eur Urol. 2012, 62(6): p. 1188-
1194
[16] Lee ES, Lee SW, Lee KW, Kim JM, Kim YH, Kim Me. Effect of transurethral
resection with hydrodistention for the treatment of ulcerative interstitial cystitis. Korean
J Urol. 2013, 54(10): p. 682-688
[17] Hunner GL. Elusive ulcer of the bladder: further notes on a rare type of bladder
ulcer with report of 25 cases. Am J Obstet. 1918, 78: p. 374-395
[18] Fall M, Oberpenning F, Peeker R. Treatment of bladder pain syndrome/ Interstitial
cystitis 2008: Can we make evidence-based decisions? Eur Urol. 2008, 54: p. 65-78
[19] Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck
P, Victor A, Wein A. The standardization of terminology in lower urinary tract function:
report from the standardization sub-committee of the International Continence Society.
Urology. 2003, 61(1): p. 37-49
[20] Nordling J, Anjum FH, Bade JJ, Bouchelouche K, Bouchelouche P, Cervigni M,
Elneil S, Fall M, Hald T, Hanus T, Hedlund H, Hohbrugger G, Horn T, Larsen S,
Leppilahti M, Mortensen S, Nagendra M, Oliveira PD, Osborne J, Riedl C, Sairanen J,
Tinzl M, Wyndaele JJ. Primary evaluation of patients suspected of having interstitial
cystitis (IC). Eur Urol. 2004, 45(5): p. 662-669
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 80
[21] Campbell DJ, Tenis N, Rosamilia A, Clements JA, Dwyers PL. Urinary levels of
substance P and its metabolites are not increased in interstitial cystitis. BJU Int. 2001,
87(1): p. 35-38
[22] European Association of Urology (EAU) – Guidelines on chronic pelvic pain. Fall
M, Baranowski AP, Elneil S, Engeler D, Hughes J, Messelink EJ, Oberpenning F, de C.
Williams AC. Edition 2008, 1-100
[23] Lundeberg T, Liedberg H, Nordling L, Theodorsson E, Owzarski A, Ekman P.
Interstitial cystitis: correlation with nerve fibers, mast cells and histamine. Br J Urol.
1993, 71(4): p. 427-429
[24] Moutzouris DA, Falagas ME. Interstitial cystitis: an unsolved enigma. Clin J Am
Soc Nephrol. 2009, 4(11): p. 1844-1857
[25] Berry SH, Elliot MN, Suttorp M, Bogart LM, Stoto MA, Eggers P, Nyberg L,
Clemens JQ. Prevalence of symptoms of bladder pain syndrome/ interstitial cystitis
among adult female in United States. J Urol. 2011, 186(2): p. 540-544
[26] Oravisto KJ. Epidemiology of interstitial cystitis. Ann Chir Gynaecol Finn. 1975,
154: p. 2035-2037
[27] Ito T, Miki M, Yamada T. Interstitial cystitis in Japan. BJU Int. 2000, 86(6): p. 634-
637
[28] Curhan GC, Speizer FE, Hunter DJ, Curhan SG, Stampfer MJ. Epidemiology of
interstitial cystitis: a population based study. J Urol. 1999, 161(2): p. 549-552
[29] Stein P, Torri A, Parsons L. Elevated urinary norepinephrine in interstitial cystitis.
Urology. 1999, 53(6): p. 1140-1143
[30] Charrua A, Pinto R, Taylor A, Canelas A, Ribeiro-da-Silva A, Cruz CD, Birder LA,
Cruz F. Can the adrenergic system be implicated in the pathophysiology of bladder
pain syndrome/ interstitial cystitis? A clinical and experimental study. Neurourol
Urodyn. 2013, doi: 10.1002/nau.22542
[31] Somogyi GT, Tanowitz M, de Groat WC. Prejunctional facilitatory α1-adrenoceptors
in the rat urinary bladder. Br J Pharm. 1995, 114: p. 1710-1716
[32] Yanase H, Wang X, Momota Y, Nimura T, Kawatani M. The involvement of
urothelial α1A adrenergic receptor in controlling the micturition reflex. Biomed Res.
2008, 29(5): p. 239-244
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 81
[33] Lee G, Park H, Park HS, Lee JG. Modulation of alpha1 adrenergic receptors on
urinary bladder in rat spinal cord injury model. Int Neurourol J. 2012, 16(2): p. 62-68
[34] Chen Z, Minneman K. Recent progress in α1-adrenergic receptor research. Acta
Pharmacol Sin. 2005, 26(1): p. 1281-1287
[35] Kim JH, Shim JS, Kang SC, Shim KS, Park JY, Moon DG, Lee JG, Bae JH. Effects
of spinal and peripheral injection of α1A or α1D adrenoceptor antagonists on bladder
activity in rat models with or without bladder outlet obstruction. Int Neurourol J. 2011,
15(4): p. 199-205
[36] Moro C, Tajouri L, Chess-Williams R. Adrenoceptor function and expression in
bladder urothelium and lamina propria. Urology. 2013, 81(1): p. 211.e1-e7
[37] Yamada T, Ugawa S, Ueda T, Ishida Y, Kajita K, Shimada S. Differential
localizations of the transient receptor potential channels TRPV4 and TRPV1 in the
mouse urinary bladder. J Histochem Cytochem. 2009, 57(3): p. 277-287
[38] Andersson KE, Gratzke C, Hedlund P. The role of the transient receptor potential
(TRP) superfamily of cation-selective channels in the management of the overactive
bladder. BJU International. 2010, 106(8): p. 1114-1127
[39] Birder LA. TRPs in bladder diseases. Biochim Biophys Acta. 2007, 1772(8): p.
879-884
[40] Charrua A, Reguenga C, Cordeiro JM, Correia-de-Sá P, Paule C, Nagy I, Cruz F,
Avelino A. Functional transient receptor potential vanilloid 1 is expressed in human
urothelial cells. J Urol. 2009, 182(6): p. 2944-2950
[41] Liu BL, Yang F, Zhan HL, Feng ZY, Zhang ZG, Li WB, Zhou XF. Increased
severity of inflammation correlated with elevated expression of TRPV1 nerve fibers and
nerve growth factor on interstitial cystitis/ bladder pain syndrome. Urol Int. 2014, 92(2):
p. 202-208
[42] Homma Y, Nomiya A, Tagaya M, Oyama T, Takagaki K, Nishimatsu H, Igawa Y.
Increased mRNA expression of genes involved in pronociceptive inflammatory
reactions in bladder tissue of interstitial cystitis. J Urol. 2013, 190(5): p. 1925-1931
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 82
[43] Charrua A, Cruz CD, Cruz F, Avelino A. Transient receptor potential vanilloid
subfamily 1 is essential for the generation of noxious bladder input and bladder
overactivity in cystitis. J Urol. 2007, 177(4): p. 1537-1541
[44] Charrua A, Cruz CD, Narayanan S, Gharat L, Gullapalli S, Cruz F, Avelino A.
GRC-6211, a new oral specific TRPV1 antagonist, decreases bladder overactivity and
noxious bladder input in cystitis animal models. J Urol. 2009, 181: p. 379-386
[45] Charrua A, Avelino A, Cruz F. Modulation of urinary bladder innervation: TRPV1
and botulinum toxin A. Handb Exp. Pharmacol. 2011, 202: p. 345-374
[46] Dinis P, Charrua A, Avelino A. Yaqoob M, Bevan S, Nagy I, Cruz F. Anandamide-
evoked activation of Vanilloid Receptor 1 contributes to the development of bladder
hyperreflexia and nociceptive transmission to spinal dorsal horn neurons in cystitis. J
Neurosci. 2004, 24(50): p. 11253-11263
[47] Walczak JS, Cervero F. Local activation of cannabinoid CB1 receptors in the
urinary bladder reduces the inflammation-induced sensitization of bladder afferents.
Mol Pain. 2011, 7: 31 doi: 10.1186/1744-8069-7-31.
[48] Wang ZY, Wang P, Bjorling DE. Activation of cannabinoid receptor 2 inhibits
experimental cystitis. Am J Physiol Regul Integr Comp Physiol. 2013, 304(10): p. 846-
853
[49] Starowicz K, Makuch W, Korostynski M, Malek N, Slezak M, Zychowska M,
Petrosino S, Petrocellis L, Cristino L, Przewlocka B, di Marzo V. Full inhibition of spinal
FAAH leads to TRPV1-mediated analgesic effects in neuropathic rats and possible
lipoxygenase-mediated remodeling of anandamide metabolism. PLoS One. 2013, 8(4):
e60040, doi: 10.1371/journal.pone.0060040
[50] Merriam FV, Wang ZY, Hillard CJ, Stuhr KL, Bjorling DE. Inhibition of fatty acid
amide hydrolase suppresses referred hyperalgesia induced by bladder inflammation.
BJU Int. 2011, 108(7): p.1145-1149
[51] Bakali E, Elliott RA, Taylor AH, Willets J, Konie JC, Tincello DG. Distribution and
function of the endocannabinoid system in the rat and human bladder. Int Urogynecol
J. 2013, 24(5): p. 855-863
[52] Tambaro S, Casu MA, Mastinu A, Lazzari P. Evaluation of selective cannabinoid
CB(1) and CB(2) receptor agonists in a mouse model of lipolysaccharide-induced
interstitial cystitis. Eur J Pharmacol. 2014, 15(729): p. 67-74
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 83
[53] Laird JM, Martinez-Caro L, Garcia-Nicas E, Cervero F. A new model of visceral
pain and referred hyperalgesia in the mouse. Pain. 2001, 92(3): p. 335-342
[54] Golubeva AV, Zhdanov AV, Mallel G, Dinan TG, Cryan JF. The mouse
cyclophosphamide model of bladder pain syndrome: tissue characterization, immune
profiling, and relationship to metabotropic glutamate receptors. Physiol Rep. 2014,
2(3): p. e00260, doi: 10.1002/phy2.260
[55] Juszczak K, Gil K, Wyczolkowski M, Thor PJ. Functional, histological structure and
mastocytes alterations in rat urinary bladders following acute and chronic
cyclophosphamide treatment. J Physiol Pharm. 2010, 61(4): p. 477-482
[56] Boddy AV, Yule SM. Metabolism and pharmacokinetics of oxazaphosphorines.
Clin Pharmacokinet. 2000, 38(4): p. 291-304
[57] Batista CKLP, Brito GAC, Souza MLP, Leitão BTA, Cunha FQ, Ribeiro RA. A
model of hemorrhagic cystitis induced with acrolein in mice. Braz J Med Biol Res.
2006, 39(11): p. 1475-1481
[58] Dunaway S, Yu Q, Larson DF. Effect of acute alpha adrenergic stimulation on
cardiac function. Perfusion. 2007, 22(4): 289-292
[59] Thiele RH, Nemergut EC, Lynch C. The clinical implications of isolated Alpha1
adrenergic stimulation. Anesth Analg. 2011, 113: p. 297-304
[60] Széll EA, Yamamoto T, de Groat WC, Somogyi GT. Smooth muscle and
parasympathetic nerve terminals in the rat urinary bladder have different subtypes of α1
adrenoceptors. Br J Pharmacol. 2000, 130(7): p. 1685-1691
[61] Hohenfellner M, Nunes L, Schmidt RA, Lampel A, Thüroff JW, Tanagho EA.
Interstitial cystitis: increased sympathetic innervation and related neuropeptide
synthesis. J Urol. 1992, 147(3): p. 587-591
[62] Pang X, Marchand J, Sant GR, Kream RM, Theoharides TC. Increased number of
substance P positive nerve fibers in interstitial cystitis. Br J Urol. 1995, 75(6): p. 744-
750
[63] Shie JH, Liu HT, Kuo HC. Increased cell apoptosis of urothelium mediated by
inflammation in interstitial cystitis/ painful bladder syndrome. Urology. 2012, 79(2): p.
484.e7-13. doi: 10.1016/j.urology.2011.09.049
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 84
[64] Lee JD, Lee MH. Activation of extrinsic apoptotic pathways from bladder biopsy in patients with interstitial cystitis/ painful bladder syndrome. Urology. 2013, 82(6): 1451.e7-11. doi: 10.1016/j.urology.2013.08.042
[65] Yu W, Hill WG, Apodaca G, Zeidel ML. Expression and distribution of transient
receptor potential (TRP) channels in bladder urothelium. Am J Physiol Renal Physiol.
2011, 300 (1): p. 49-59
[66] Everaerts W, Vriens J, Owsianik G, Appendino G, Voets T, De Ridder D, Nilius B.
Functional characterization of transient receptor potential channels in mouse urothelial
cells. Am J Physiol Renal Physiol. 2010, 298(3): p. 692-701
[67] Jung J, Shin JS, Lee SY, Hwang SW, Koo J, Cho H, Oh U. Phosphorylation of
vanilloid receptor 1 by Ca2+/ calmodulin-dependent kinase II regulates its vanilloid
binding. J Bio Chem. 2004, 279(8): p. 7048-7054
[68] Planells-Cases R, García-Sanz N, Morenilla-Palao C, Ferrer-Montiel A. Functional
aspects and mechanisms of TRPV1 involvement in neurogenic inflammation that leads
to thermal hyperalgesia. Pflugers Arch. 2005, 451(1): p. 151-159
[69] Ford AP. In pursuit of P2X3 antagonists: novel therapeutics for chronic pain and
afferent sensitization. Purinergic Signalling. 2012, 8(1): p. 3-26
[70] Fowler CJ, Griffiths D, de Groat WC. The neural control of micturition. Nat Rev
Neurosci. 2008, 9(6): p. 453-466
[71] Birder LA, Hanna-Mitchell AT, Mayer E, Buffington CA. Cystitis, co-morbid
disorders and associated epithelial dysfunction. Neurorol Urodyn. 2011, 30(5): p. 668-
672
[72] Nomiya M, Yamaguchi O, Andersson KE, Sagawa K, Aikawa K, Shishido K,
Yanagida T, Yazaki J, Takahashi N. The effect of atherosclerosis-induced chronic
bladder ischemia on bladder function in the rat. Neurourol Urodyn. 2012, 31(1): p. 195-
200
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 86
IX. Attachments
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 88
IX. Attachments
1. Phenylephrine and antagonist solutions
The phenylephrine (Sigma-Aldrich P6126-5G) solution used for chronic
adrenergic stimulation both in rat and mice was daily injected at 2.5 mg/ Kg body
weight. This solution vehicle was saline solution.
Silodosin (antagonist of alpha1A- adrenoceptor) were used in a concentration of
0.2 mg/ Kg. Naftopidil (antagonist of alpha1D- adrenoceptor) were used in a
concentration of 0.9375 mg/ Kg. The solution vehicle was saline solution.
Prazosin (non-specific antagonist of alpha1-adrenoceptor) were used in a
concentration of 0.05 mg/ Kg. The solution vehicle was saline solution.
2. Cystometry, tissue harvesting and processing solutions
During cystometry, saline solution was infusecd (1.8 mL/ h) into the bladder
dome of anaesthetized animals (urethane 1.2 mg/ Kg).
During perfusion, the fixative and Tyrode´s solution were prepared as follows:
- Paraformaldehyde 4% (for 1L): 250 mL paraformaldehyde 16%, 250 mL
Phosphate buffer 0,4M pH 7.2 and 500 mL bidestilled water);
- Tyrode’s solution (for 1L): 6.80g NaCl; 0.40g KCl; 0.32g MgCl2.6H2O; 0.10g
MgSO4.7H2O; 0.17g NaH2PO4.H20; 1.00g glucose and 2.20g NaHCO3).
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 89
L6-S1 spinal cord segments were sectioned at 40 µm and the cuts were stored
at -20ᵒC in crioprotectant. To prepare this solution, 500 mL of phosphate buffer 0.1M
pH 7.2, 300g of sucrose and 300 mL of ethyleneglycol were used
3. Immunoreaction against Fos in spinal cord segments
L6-S1 spinal cord segments were sectioned and immunostained for Fos protein,
like described below:
The segments were washed 3 times with PBS (5 minutes each), following a
wash with ethanol 50% in elix for 10 minutes, to permeabilize the membranes and
allow better entry of the substrate.
The slides were incubated in ethanol 50% and 330 µL of H2O2 for 30 minutes, to
inhibit the endogenous peroxidase. After this, the sections were washed with ethanol
50% for 10 minutes and with PBS for 5 minutes.
Next, the slides were incubated with PBST/ NSS 10% for 1 hour.
Afterwards, there was an incubation in the primary antibody α- c Fos
(Calbiochem) diluted 1: 10000 in PBST/ NSS 2% for 2 days at 4ᵒC.
The slides were washed 3 times (10 minutes each) with PBST/ NSS 2% and
incubated with secondary antibody biotinylated swine α-rabbit (Palex Medical) diluted
1:200 in PBST/NSS 2% for 1 hour.
Then, the slides were washed twice (10 minutes each) with PBST/ NSS 2%,
with PBST for 10 minutes and incubated with ABC, during at least one hour, to amplify
the final signal (avidin binds to the biotin of the secondary antibody).
Next, the slides were washed 3 times with PBST (for 10 minutes each time),
with PBS for 10 minutes and with Tris-HCl 0,1M for 10 minutes, to remove the excess
of secondary antibody- ABC complex, or just ABC.
The slides were incubated with diaminobenzidine (DAB), which is a
chromogenic substrate of peroxidase. In the presence of H2O2, the enzyme forms a
brown and insoluble precipitate where there is enzyme, and therefore the antigen
under study.
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 90
Finally, the sections were washed with Tris-HCl 0,1 M for 5 minutes and with
PBS for 5 minutes. Finally, the slides were mounted with EuKit (National Diagnostics)
and observed on light microscopy (Zeiss Axioskop 40).
4. Immunoreaction against caspase 3 in bladder sections
Bladder sections were immunoreacted against caspase 3, a marker of cellular
apoptosis, to analyze urothelium integrity.
Briefly, the slides were washed 3 times with xylene (5 minutes each time),
washed with ethanol 100% 3 times (5 minutes each), 3 times with ethanol 90% (for 5
minutes each), 3 times with ethanol 75% (for 5 minutes each) and 3 times with distilled
water (for 5 minutes each).
Then, slides were incubated with citrate buffer 2 g/L pH 6, in the microwave for
15 minutes, and left to cool, for 30 minutes.
After this, the slides were washed with PBS 2 times (for 10 minutes each), with
1% H2O2 in methanol for 10 minutes and with PBS for 10 minutes.
Next, the slides were incubated with PBST/NSS 10% for 1h and, after this, with
primary antibody rabbit anti-caspase 3 (Abcam) diluted 1:500 in PBST/NSS 2% for 2
days at 4ᵒC.
The slides were washed with PBST/NSS 2% 3 times for 10 minutes each time,
and incubated with secondary antibody 488 goat anti-rabbit 1:3000 (Invitrogen) in
PBST/NSS 2% for 1h.
After this, the slides were washed with PBST/NSS 2% 2 times (10 minutes
each), with PBST for 10 minutes and with PBS for 10 minutes.
Finally, the slides were mounted with glycerol and observed on fluorescence
microscope (Zeiss Apotome).
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 91
5. Preparation of solutions for immunoreaction
Phosphate buffered saline (PBS) is a buffered solution used in biological
research, and containing sodium chloride, sodium phosphate and, in some cases,
potassium chloride and potassium phosphate. This solution helps to maintain a
constant pH. PBST results from addition of Tween 20 or Triton X-100 to PBS. The
Triton X-100 permeabilizes the cells, facilitating the entry of the antibody into the cells.
PBS 0.1M (for 1L): 100 mL of stock solution of PBS 10x and 900 mL of distilled
water.
PBST (for 1L): 888 mL of distilled water, 100 mL of PBS 10x and 12 mL of
Triton X-100 at 25%.
Triton X-100 25% (for 12 ml): 3 mL of Triton X-100 and 9 mL of distilled water.
PBST/ NSS 10% contains PBST and NSS (normal swine serum).
PBST/NSS 10% (for 8 mL): 800 µL of NSS and 7.2 mL of PBST.
PBST/NSS 2% (for 8 mL): 160 µL of NSS and 7.84 mL of PBST.
For incubation with ABC (Vector Laboratories), use 1 µL of A and 1 µL of B per
200 µL of PBST. For example, to prepare 3.2 mL of PBST is necessary to add 16 µL of
A and 16 µL of B. This solution needs to be prepared, at least, 30 minutes prior to use
and placed in the shaker.
To prepare DAB (diaminobenzidine), first add 5 µL of H2O2 at 30% in 20 mL of
Tris-HCl (0,05 M pH=7.6), and then add 10 mg of DAB.
FCUP
Characterization of an animal model of Bladder painful syndrome/ Interstitial cystitis 92
6. Hematoxylin-Eosin staining in bladder sections
Bladder sections were washed with xylene for 10 minutes, to remove paraffin.
After this, the slides were washed with ethanol 100% (2 minutes), ethanol 90%
(2 minutes) and ethanol 70% (2 minutes).
The slides were washed with water for 10 minutes, and then the cuts were
stained with Hematoxylin for 3 minutes.
After staining, the slides were placed under current water for 15 minutes.
Then, the slides were stained with eosin for 30 seconds, and washed with
ethanol 70%, ethanol 90% and ethanol 100% (only for some seconds in each one).
The slides were washed with xylene for 10 minutes, mounted with EuKit and
observed under the light microscope.
7. Toluidine Blue staining in bladder sections
Bladder sections were washed with xylene for 10 minutes to remove paraffin.
After this, the slides were washed with ethanol 100% (2 minutes), ethanol 90%
(2 minutes) and ethanol 70% (2 minutes).
The slides were washed with water for 10 minutes, and then the cuts were
stained with Toluidine Blue for 4 minutes.
After staining, the slides were placed under current water for 15 minutes.
Then, the slides were washed with ethanol 70%, ethanol 90% and ethanol
100% (only for some seconds in each one).
The slides were washed with xylene for 10 minutes, mounted with EuKit and
observed under the light microscope.