Changes in Bone Matrix Mineralization After Growth Hormone Treatment in Children and Adolescents...
Transcript of Changes in Bone Matrix Mineralization After Growth Hormone Treatment in Children and Adolescents...

Original Investigation
Changes in Bone Matrix Mineralization After Growth HormoneTreatment in Children and Adolescents With Chronic Kidney
Failure Treated by Dialysis: A Paired Biopsy Study
Kamilla Nawrot-Wawrzyniak, PhD,1 Barbara M. Misof, PhD,1 Paul Roschger, PhD,1
Małgorzata Panczyk-Tomaszewska, MD,2 Helena Ziółkowska, MD,2
Klaus Klaushofer, MD,1 and Nadja Fratzl-Zelman, PhD1
Background: Patients with chronic kidney disease (CKD) develop renal osteodystrophy with alterations inbone turnover, mineralization, and volume (TMV). A specific skeletal complication in children is growthimpairment, which currently is treated by recombinant human growth hormone (rhGH). The effects on bonematerial properties are poorly understood. This study assesses the effects of rhGH treatment on bone matrixmineralization.
Study Design: Observational study.Setting & Participants: 18 short children and adolescents (aged 3.6-16 years) with CKD on dialysis
therapy.Predictor: rhGH treatment for 1 year.Outcomes: Tetracycline-labeled bone biopsy classified according to the TMV system.Measurements: Bone mineralization density distribution (BMDD) was evaluated by quantitative backscat-
tered electron imaging in trabecular and cortical compartments. Additional data for patients’ height andbiochemical bone serum parameters were obtained.
Results: Prior to rhGH treatment, our cohort showed low bone turnover and high mineralization densitiesversus reference data: Camean (weighted mean calcium content) in cancellous bone, �3.3% (P � 0.04);Camean in cortical bone, �6.7% (P � 0.001); Capeak (mode of the BMDD) in cancellous bone, �5.0% (P �0.001); Capeak in cortical bone, �8.2% (P � 0.001); Cawidth (heterogeneity in mineralization), no significantdifference for cancellous (P � 0.2) and cortical (P � 0.1) bone; Cahigh (portion of fully mineralized bone) incancellous bone, 5-fold greater (P � 0.001); Cahigh in cortical bone, 14-fold greater (P � 0.001); Calow (portionof low mineralized bone) in cancellous bone, �23.9% (P � 0.02); Calow in cortical bone, –22.2% (P � 0.05).After rhGH treatment, height increased by 9.1 cm (P � 0.001) and bone turnover indices to normal values orbeyond. Matrix mineralization was lesser and more heterogeneous compared to baseline: Cawidth for cancel-lous bone, �15.3% (P � 0.001); Cawidth for cortical bone, �34.1% (P � 0.001). Camean, Capeak, and Cahigh forcancellous bone and Camean and Capeak for cortical bone were no longer significantly different from referencedata. Cahigh for cortical bone dramatically decreased after treatment but was still substantially greater thanreference data.
Limitations: Low case number per TMV subgroup, no measurements of fibroblast growth factor 23.Conclusions: Children and adolescents with CKD and growth deficiency are at risk of having low bone
turnover. rhGH treatment improves height and concomitantly bone modeling/remodeling, which appearsbeneficial for bone matrix mineralization.Am J Kidney Dis. 61(5):767-777. © 2013 by the National Kidney Foundation, Inc.
INDEX WORDS: Bone mineralization density distribution (BMDD); quantitative backscattered electron imaging(qBEI); bone histomorphometry; renal osteodystrophy; children and adolescents with chronic kidney disease(CKD); growth hormone therapy.
Skeletal alterations, termed renal osteodystrophy,occur early during a decrease in kidney function
and are common in patients with chronic kidneydisease (CKD).1-4 Renal osteodystrophy is consideredas a multifactorial disorder of bone remodeling and isdiagnosed in bone biopsies as histologic types classi-fied from low bone formation (adynamic bone) to
From the 1Ludwig Boltzmann Institute of Osteology at HanuschHospital of WGKK and AUVA Trauma Centre Meidling, 1stMedical Department, Hanusch Hospital, Vienna, Austria; and2Department of Pediatrics and Nephrology, Medical University ofWarsaw, Warsaw, Poland.
Received April 7, 2012. Accepted in revised form December 12,
2012. Originally published online February 27, 2013.Am J Kidney Dis. 2013;61(5):767-777
increased bone turnover (osteitis fibrosa), with orwithout features of abnormal mineralization of thebone matrix.3,5,6
Alteration in mineralization has been shown to bethe first skeletal abnormality in children and adoles-cents with CKD stage 2 and the prevalence increaseswith progression of CKD.1,5,7-10 Affected patients
Address correspondence to Nadja Fratzl-Zelman, PhD, LudwigBoltzmann Institute of Osteology, Trauma Center Meidling, Kund-ratstr 37, A-1120 Vienna, Austria. E-mail: [email protected]
© 2013 by the National Kidney Foundation, Inc.0272-6386/$36.00
http://dx.doi.org/10.1053/j.ajkd.2012.12.010767

Nawrot-Wawrzyniak et al
also often experience growth retardation due to distur-bance of the somatotropic hormone axis, leading to arelative growth hormone (GH) insensitivity and func-tional IGF-1 (insulinlike growth factor 1) deficiency.As a result, chondrocyte differentiation and theirsubsequent expansion within the epiphyseal growthplate are impaired.11-13 Recombinant human GH(rhGH) has been used successfully for many years tocompensate growth failure in children and adoles-cents with CKD who are on conservative or dialysistreatment, as well as to reverse the growth-depressingeffects of glucocorticoids after kidney transplanta-tion.2,12,14-16 However, to evaluate the impact of CKDon bone development and the therapeutic effect of GHtherapy, not only bone mass and bone microarchitec-ture, but also bone material quality should be as-sessed. A key determinant of stiffness, strength, andtoughness of bone material is the degree of mineraliza-tion of the bone matrix, which can be determined byquantitative backscattered electron imaging in biopsysamples prepared for histology and histomorphom-etry.17 Hence, bone mineralization density distribu-tion (BMDD) describes the degree and distribution ofmineral content of the bone matrix (which reflects therate of bone turnover) and the mineralization kinetics(speed of mineral deposition within the newly formedosteoid).18,19 Moreover, a recently established set ofBMDD reference data enables comparison of mineral-ization status between children, adolescents, and youngadults with and without bone disorders.20
In the present study, we focused on bone materialproperties in 18 children and adolescents on dialysistherapy before and after 1 year of rhGH treatment.Bone histomorphometry was performed on pairedbiopsy specimens and renal osteodystrophy was char-acterized according to the recently recommended TMVsystem that addresses bone turnover, mineralizationdefects, and abnormalities in bone volume.1 Further-more, we evaluate BMDD before and after rhGHtreatment and compared all data to the referencecohort.20
METHODS
StudyPopulation
The present study population comprised 18 whites with CKDstage 5D, 11 treated by continuous peritoneal dialysis and 7 treatedby hemodialysis,21 and is part of a larger cohort reported previ-ously.9 We reused all available paired biopsy samples with intactbone compartments and sufficient residual bone material for histo-morphometry and quantitative backscattered electron imaging anal-ysis. All patients were treated with calcium carbonate as phosphatebinder, alfacalcidol administered at a mean dosage of 0.008-0.3�g/kg body weight per week (daily or in intermittent doses), andcalcium carbonate at a dosage of 55-334 mg/kg body weight per
day. Indication for “pulse” doses of alfacalcidol was according to768
parathyroid hormone (PTH) level (abnormally high) as evaluatedduring clinical monitoring. Calcium carbonate was administratedindividually according to phosphorus level.
None of the patients had fractures or received a kidney trans-plant between bone biopsies. Plain radiographs of the left handwere obtained to confirm delayed skeletal age according to theGreulich-Pyle scale.22 Subsequently, children and adolescents weretreated for 12 months with rhGH (daily subcutaneous application,1.0-1.1 IU/kg/wk). Relevant clinical data are listed in Table 1.
BoneSerumParameters
The following relevant bone parameters were assessed in fastingblood serum at the day of bone biopsy: calcium, phosphorus, intactPTH (detection of the peptide containing amino acids 1-84 byimmunoradiometric assay [Incstar Corp]),23 and alkaline phospha-tase (ALP; by the kinetic method). Serum concentrations ofosteocalcin were determined in 11 patients by radioimmunoassay(Incstar Corp).23
BoneBiopsy, Histomorphometry, andTMVClassification
Prior to each bone biopsy, tetracycline was administered orallyin a dosage of 10 mg/kg/d for 3 days, with a 10-day interval fordynamic measurements of bone formation. Transiliac bone biop-sies were performed 4-6 days after the last dose of tetracyclinewith a Bordier trocar (6-mm inner diameter). Undecalcified bonesamples were embedded in polymethylmethacrylate.20 Consecu-tively, 3-�m sections were stained with a modified Goldner’strichrome method, and 10-�m sections were used for fluorescentmicroscopy. Histomorphometric analyses were performed withoriginal magnification �100 for structural and �200 for static anddynamic parameters (ocular �10 and objective �10 or �20,respectively) by means of an Axiophot microscope (Zeiss) equippedwith an AxioCam videocamera (Zeiss). The images obtained wereanalyzed further using NIH Image software versions 1.62 and 1.63(developed at the US National Institutes of Health and available atrsb.info.nih.gov/nih-image). Bone histomorphometry was per-formed according to Parfitt et al.24
Classification of renal osteodystrophywas assessed by interpre-tation of histology and histomorphometry indexes according to theTMV system1,2 as previously done by Bakkaloglu et al.3 Allparameters were compared with published references from Glo-rieux et al.25
QuantitativeBackscattered Electron Imaging
The remaining tissue blocks were prepared by grinding andpolishing, and surface planes containing bone tissue were coatedby carbon for quantitative backscattered electron imaging analysisin the scanning electron microscope as reported elsewhere.17,26
Trabecular and cortical BMDD were determined using a digitalscanning electron microscope (DSM 962; Zeiss) equipped with a4-quadrant semiconductor backscattered electron detector.17,26,27
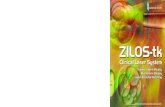
BMDD parameters are shown in Fig 1. The outcomes werecompared to the published reference BMDD of healthy children,adolescents, and young adults.20
Statistical Evaluation
Statistical analysis was performed using SigmaStat for Win-dows, version 2.03 (SPSS Inc). Because sample sizes within thepatient cohort and in particular within the TMV subgroups wererelatively small, all outcomes (clinical, histomorphometry, andBMDD) were given as median values with interquartile ranges.Comparisons after treatment versus baseline and cortical versus
cancellous BMDD variables were based on Wilcoxon signed tests.Am J Kidney Dis. 2013;61(5):767-777

alysi
Bone Matrix Mineralization in Young People With CKD
Comparison of the BMDD outcomes to reference BMDD data20
was done using Mann-Whitney rank sum tests. Correlation ofBMDD variables with bone formation rate per bone surface orALP level was analyzed by Spearman rank order correlation.Statistical significance was considered at P � 0.05.
RESULTS
Clinical Characteristics andBone-TurnoverMarkers
rhGH treatment led to significant height gains in thetotal cohort. Patients’ clinical characteristics and bio-chemical markers are listed in Table 1. Correctedcalcium levels were within the reference range, inde-pendent of treatment. Serum phosphorus levels wereelevated and not significantly altered by rhGH therapy.PTH and osteocalcin levels were markedly increasedin most patients, independent of therapy. Neverthe-less, PTH values �300 pg/mL were found solely in 2patients before and 3 patients after treatment.
The median ALP activity value was within thenormal range before treatment and was the onlybiochemical parameter that was significantly in-creased by rhGH treatment (to nearly double the
Table 1. Clinical Data and Serum Values Fr
Parameters Before Treatment
Clinical characteristics:No. of patients 18Male sex 13Age (y) 11.2 [3.6 to 13.7]
Pubertal stage (Tanner scale)I 15II 3
Height (cm) 126.9 [114.3 to 133.7]
Height z score �2.65 [�3.13 to �2.27]
Skeletal retardation (y) 2.9 [1.80 to 4.18]
BMI z score �0.45 [�0.80 to �0.20]
Time on dialysis (mo) 22.35 [8.9 to 32.6]
Serum parametersCalciumb (mmol/L) 2.29 [2.19 to 2.47]Phosphorus (mmol/L) 1.93 [1.89 to 2.14]Parathyroid hormone (pg/mL) 59 [39 to 183]Osteocalcinc (ng/mL) 56.0 [36.4 to 61.7]Alkaline phosphatase (U/L) 236 [134 to 338]
Concurrent medicationAlfacalcidol (�g/kg/wk) 0.080 [0.05 to 0.12]d
Calcium carbonate (mg/kg/d) 125.0 [80.0 to 166.0]d
Note: Paired data. Values for categorical variables are givenrange].
Abbreviations: BMI, body mass index; rhGH, recombinant humaP value from signed Wilcoxon test, comparing before versus abCorrected for serum albumin level.cPaired data from 11 patients were available.dMean dose 1 month before bone biopsy sample and serum an
normal activity level). Concurrent alfacalcidol and
Am J Kidney Dis. 2013;61(5):767-777
calcium carbonate medication did not significantlychange during rhGH therapy.
TMVClassification andBoneHistomorphometry ofEntire Cohort
Histomorphometric indexes needed for the TMVclassification of each patient were assessed accordingto guidelines1,5 and compared with the correspondingage-related reference values for healthy children, ado-lescents, and young adults.25 Results are listed inTable 2.
Before treatment, 7 patients were identified as hav-ing low bone formation (adynamic bone disease, n �5; osteomalacia, n � 2), 7 as having mixed uremicosteodystrophy, and 4 as having normal bone. Tetracy-cline labeling was detected in all biopsy samplesexcept within the adynamic bone disease group, inwhich samples from 2 patients showed only singlelabeling and one patient’s sample had no labeling.
After treatment, double labeling was present in allsamples. Most patients were classified as having mixeduremic osteodystrophy (n � 11). There were no more
ll Patients Before and After rhGH Treatment
After Treatment Pa Reference Range
136.0 [123.2 to 144.1] �0.001
�2.40 [�2.97 to �1.70] �0.001
— —
�0.30 [�0.63 to 0.00] 0.6
— —
2.42 [2.21 to 2.55] 0.4 2.05-2.601.86 [1.48 to 2.49] 0.8 1.16-1.8
71 [54 to 214] 0.6 10-5583.9 [48.8 to 144.6] 0.08 1.8-6.6
407 [214 to 516] 0.009 80-280
0.094 [0.060 to 0.160]d 0.5140.0 [115.0 to 188.0]d 0.1
mber; values for continuous variables, as median [interquartile
owth hormone.reatment.
s were performed.
om A
as nu
an grfter t
cases of adynamic bone disease or osteomalacia. Two
769

Nawrot-Wawrzyniak et al
cases of osteitis fibrosa (before treatment, one of thesecases had been classified as osteomalacia and the otheras mixed uremic osteodystrophy) representing the high-bone-turnover edge of the renal osteodystrophy spec-trum were newly identified. In these 2 patients, serumdata consistently showed severe hyperparathyroidism(serum PTH levels of �900 pg/mL), with one of themhaving exceptional ALP levels �1,200 U/L.
Table 3 lists measured histomorphometric data fromthe entire cohort in comparison to reference values.25
In general, dynamic indexes of bone formation ap-peared low before treatment and significantly in-creased to normal values or even higher after treat-ment. There was marked augmentation in mineralizingsurface per bone surface, mineralizing surface perosteoid surface, and bone formation rate per bonesurface, which all had approximately doubled whenmeasured after treatment. Concomitantly, prior totreatment, mineralization lag time was found to bemarkedly prolonged compared to that after treatment.Very high mineralization lag times after therapy wereobserved solely in 2 patients (1 had no tetracyclinelabeling and the other had exceptionally high mineral-ization lag time before therapy). In contrast to thedynamic indexes, static or structural indexes of thetotal cohort were not significantly altered after treat-
ment.770
BoneHistomorphometry andSerumALPofTMVSubgroups
rhGH treatment led within each TMV subgroup toan increase in bone formation rate, mineralizing sur-face, and serum ALP levels (Fig 2). Most remarkably,following rhGH treatment, all 5 patients classified
Table 2. TMV Classification Before and After rhGH Treatment
rhGH Treatment ABD OM NB MUO OF
Before 5 2 4 7 0
After 0 0 5 11 2
Note: Entire cohort, N � 18, paired biopsy specimens. Eachparameter was considered normal, decreased, or increasedwhen found within, below, or above 1 standard deviation, respec-tively, of age-related reference ranges.25
Abbreviations and definitions: ABD, adynamic bone disease,defined as low bone turnover with low or normal amount of osteoid;MUO, mixed uremic osteodystrophy, defined as combination ofhigh or low bone turnover with abnormal histologic mineralizationindexes and bone volume; NB, normal bone, defined as boneturnover, histologic mineralization indexes, and bone volume pertissue volume within normal range; OF, osteitis fibrosa, defined ashigh bone turnover, increased number of active osteoblasts andosteoclasts, abnormal osteoid seams and fibrosis of the bonemarrow; OM, osteomalacia, defined as low bone turnover withincreased osteoid formation; rhGH, recombinant human growthhormone; TMV, system that addresses bone turnover, mineraliza-
Figure 1. Example of bone mineral density dis-tribution (BMDD) measurements of a paired biopsyspecimen from a patient with adynamic bone dis-ease. (A) Backscattered electron image from thetransiliac bone biopsy before and after recombinanthuman growth hormone (rhGH) treatment. (B) Cor-responding BMDD histograms of this patient (solidline is pre-rhGH treatment and dotted line is follow-up) in comparison with those of reference data froma young population.20 BMDD variables derived fromthe histograms are the mean (weighted mean)Camean and the most frequent calcium concentrationCapeak (mode, peak position of the BMDD) in thesample, the width of the distribution Cawidth (fullwidth at half maximum) reflecting the heterogeneityin matrix mineralization, the fraction of low mineral-ized bone (Calow) showing the percentage of bonearea mineralized �17.68 wt% Ca, and the fractionof fully mineralized bone (Cahigh) showing the per-centage of bone area mineralized �25.30 wt% Ca.The cutoff level at 17.68 wt% Ca corresponds to the5th percentile and the cutoff level at 25.30 wt% Cacorresponds to the 95th percentile of the referenceBMDD of adults.17,27 Note that the BMDD peak ofthe patient is shifted to the left, toward lower cal-cium concentrations after treatment.
tion defects, and abnormalities in bone volume.2
Am J Kidney Dis. 2013;61(5):767-777

le lab
Bone Matrix Mineralization in Young People With CKD
before treatment as having adynamic bone diseasealso showed a marked increase in osteoblast andosteoclast surfaces and osteoid indexes. Four of these5 patients were classified as having mixed uremicosteodystrophy due to the presence of increased os-teoid accumulation and/or increased mineralizationlag time and one patient had features of normal bone.Both patients classified as having osteomalacia beforetreatment also showed a marked decrease in osteoidthickness and a marked increase in osteoclast surfaceper bone surface. Interestingly, these patients also hadthe highest serum ALP levels independent of treat-ment. After treatment, one of the latter patients wasclassified as having normal bone, whereas the otherpatient showed features of osteitis fibrosa. Aftertherapy, patients in the histologically heterogeneousgroup of mixed uremic osteodystrophy remained clas-sified as having either mixed uremic osteodystrophy(n � 4) or normal bone (n � 2); one patient developedosteitis fibrosa. In contrast, of the 4 patients withhistologic features of normal bone before treatment, 3were classified as having mixed uremic osteodystro-phy after therapy (the remaining patient retained thenormal bone classification). The 5 patients who wereclassified as having normal bone after treatment also
Table 3. Histomorphometric Da
Histomorphometric Parameter Before Treatment
BV/TV (%) 25.2 [21.6-30.2]
Tb.Th. (�m) 121 [105-132]
Tb.N (mm�1) 2.13 [1.76-2.57]
Ct.Wib (mm) 0.60 [0.40-0.68]
Ct.Pob (%) 7.7 [3.8-9.3]
OV/BV (%) 5.90 [2.72-9.14]
OS/BS (%) 45.8 [35.4-56.1]
O.Th. (�m) 10.3 [6.7-15.0]
Ob.S/BS (%) 1.6 [0.5-3.4]
Oc.S/BS (%) 0.8 [0.3-1.5]
BFR/BS (�m/y) 21.6 [11.0-34.9]
MAR (�m/d) 1.36 [0.86-1.72]
MS/BS (%) 4.3 [2.7-6.4]
Aj.AR (�m/d) 0.12 [0.05-0.23]
MS/OS (%) 8.4 [5.2-14.3]
Mltc (d) 55.3 [44.0-118.2]
Note: N � 18, paired data. Values are given as median [interqstandard deviation (range) for all studied children from Glorieux e
Abbreviations: Aj.AR, adjusted mineral apposition rate; BFR/tissue volume; Ct.Po, cortical porosity; Ct.Wi, cortical width; Mmineralizing surface per bone surface; MS/OS, mineralizing ssurface; Oc.S/BS, osteoclast surface per bone surface; OS/BS,osteoid volume per bone volume; rhGH, recombinant human gro
aP values from Wilcoxon signed rank comparison of before verbSixteen sets of paired data (16 patients had biopsy samples wcFifteen sets of paired data (for the 3 patients who had no doub
had serum phosphorus levels within the normal range
Am J Kidney Dis. 2013;61(5):767-777
independent of whether levels were elevated or nor-mal before treatment (data not shown).
BMDDof Entire Cohort
Before treatment, parameters of the BMDD (Camean
[weighted mean calcium content], Capeak [mode of theBMDD], Cawidth [heterogeneity in mineralization],Calow [portion of low mineralized bone], and Cahigh
[portion of fully mineralized bone] as shown andfurther described in Fig 1A) showed abnormally highbone matrix mineralization in both cancellous andcortical bone compared with reference values20 and ashift toward normal range after treatment (Fig 1B;Table 4).
Before treatment, Camean and Capeak were higherthan normal (�3.3% [P � 0.05] and �5.0% [P �0.001], respectively, in cancellous bone and �6.7%[P � 0.001] and �8.2% [P � 0.001], respectively, incortical bone). Further, compared with reference val-ues, Cahigh was 5-fold greater in cancellous bone andabout 14-fold greater in cortical bone (both P �0.001).
After treatment, there was a clear shift towardlower matrix mineral content, reflected by a decreasein Camean and Capeak, which were no longer signifi-
fore and After rhGH Treatment
er Treatment Pa Reference
[24.5-34.0] 0.2 23.9 � 5.3 (13.5-35.5)
[109-143] 0.5 139 � 28 (87-193)
[2.04-2.67] 0.3 1.72 � 0.23 (1.17-2.40)
[0.51-0.76] 0.1 0.96 � 0.35 (0.35-1.81)
[4.9-12.2] 0.4 Not defined
[3.27-8.94] 0.7 2.42 � 1.22 (0.41-4.15)
[32.5-53.1] 0.5 24.9 � 10.0 (4.9-54.3)
[7.6-14.5] 0.8 6.4 � 1.4 (3.9-10.0)
[1.5-4.9] 0.1 7.2 � 4.1 (1.0-17.0)
[0.5-2.5] 0.07 1.09 � 0.58 (0.27-2.94)
[24.3-75.7] 0.01 39.3 � 17.5 (6.8-78.4)
[1.30-1.93] 0.2 0.89 � 0.14 (0.57-1.44)
[3.7-14.5] �0.05 11.9 � 4.5 (3.3-22.1)
[0.19-0.56] 0.006 0.44 � 0.13 (0.13-0.86)
[9.9-37.3] 0.01 50.0 � 15.6 (15.2-98.1)
[20.1-44.1] �0.05 15.5 � 4.8 (8.7-29.1)
e range], except for reference data, which are given as mean �5
one formation rate per bone surface; BV/TV, bone volume permineral apposition rate; Mlt, mineralization lag time; MS/BS,
e per osteoid surface; Ob.S/BS, osteoblast surface per boneoid surface per bone surface; O.Th, osteoid thickness; OV/BV,ctor; Tb.N, trabecular number; Tb.Th, trabecular thickness.fter rhGH treatment.th cortices available before and after treatment).els at baseline, MAR was set to zero and Mlt was not available).
ta Be
Aft
27.7
122
2.40
0.62
6.0
3.77
37.5
10.4
3.1
1.3
45.3
1.59
7.8
0.39
20.7
32.1
uartilt al.2
BS, bAR,
urfacoste
wth fasus aith bo
cantly different from reference data. Most remark-
771

Nawrot-Wawrzyniak et al
ably, Cahigh also dramatically decreased in both bonecompartments: in cancellous bone to normal rangeand in cortical bone to �78% of the pretreatmentlevel, although it was still 3 times higher than normal.Concomitantly, there also was a significant increase inheterogeneity of mineralization Cawidth in cancellous(�15.3% [P � 0.001] vs normal) and cortical bone(�34.1% [P � 0.001] vs normal). Calow did notchange significantly from baseline, but after treat-ment, it was significantly higher than normal (�76%[P � 0.001]).
TMVSubgroups
BMDD outcomes in each of the different TMVsubgroups before and after treatment are shown in Fig3A and B and, with the exception of the normal bonecases, reflect the effect of rhGH treatment in the entirestudy cohort, namely, a general decrease in cancellousand cortical Camean, Capeak, and Cahigh and an increase
in Cawidth and Calow.772
In particular, the highest values for Camean, Capeak,and Cahigh were found in the adynamic bone diseasegroup followed by the mixed uremic osteodystrophygroup before treatment, which all reached normalvalues after treatment. Both patients with osteomala-cia showed the highest values for Calow before andafter treatment and the highest value for Cawidth aftertreatment. Interestingly, those with normal bone alsohad BMDD values within the normal range except forCahigh, which was slightly increased. After treatment,only the median value for Calow was increased com-pared with reference data.
Correlations of BMDDVariables
BMDD parameters of cancellous bone obtainedbefore rhGH treatment in the entire cohort werecorrelated strongly with bone formation rate per bonesurface (Table 5). Camean, Capeak, and Cahigh showedinverse relationships and Cawidth and Calow showedpositive correlations with bone formation rate per
Figure 2. Relevant bone histomorpho-metric indexes and serum alkaline phospha-tase levels before and after recombinant hu-man growth hormone treatment within thedifferent TMV subgroups. Data points andbars show median (25th, 75th percentile)values of paired data. Normal range com-prises the mean � 1 SD of the referencedata (age range, 1.5-22.9 years) from Glo-rieux et al.25 Open symbols correspond tothe value before treatment; filled symbols, tothe same patients after treatment. Note thatthe TMV subgroup is always that determinedbefore treatment. Abbreviations: ABD, ady-namic bone disease; MUO, mixed uremicosteodystrophy; NB, normal bone; OM, os-teomalacia; TMV, system that addressesbone turnover, mineralization defects, andabnormalities in bone volume.
bone surface. Additionally, ALP level was correlated
Am J Kidney Dis. 2013;61(5):767-777

Bone Matrix Mineralization in Young People With CKD
positively with Camean and negatively with Calow
values. After treatment, BMDD parameters were cor-related with neither bone formation rate nor ALP level(P ranging from 0.07-0.9).
DISCUSSION
To our knowledge, this is the first study of theeffects of growth hormone treatment on bone matrixmineralization in children and adolescents with CKD.The hallmark in these patients is growth retardationthat worsens when kidney function decreases,12 but itis not known how intrinsic bone material propertiesare affected by rhGH therapy. Before treatment, ourstudy cohort showed skeletal retardation of nearly 3years, low bone turnover, and abnormally high bonematrix mineralization. After treatment, the medianvalue for height was increased by 9.1 cm and matrixmineralization in cancellous and cortical bone wasshifted toward the normal range. Median PTH valueswere not markedly altered, but ALP levels were in-creased significantly.
Prior to treatment, we observed no cases of in-creased bone turnover in our cohort: the most preva-lent TMV subtype was mixed uremic osteodystrophyfollowed by adynamic bone disease and single casesof normal bone and osteomalacia.13 The associationbetween growth retardation and adynamic bone hasbeen described previously,28 but is still a controversialissue in the field. It is widely recognized that bonemetabolism in children and adolescents is more com-
Table 4. BMDD Results for Cancellous and
BMDD Parameters Before Treatment
Cancellous boneCamean (wt%Ca) 21.65c [20.57-22.19]Capeak (wt%Ca) 22.75d [21.66-23.08]Cawidth (wt%Ca) 3.53 [3.24-4.07]Calow (%) 7.61c [7.01-10.35]Cahigh (%) 4.49d [1.37-8.67]
Cortical boneCamean (wt%Ca) 21.83d [20.82-22.57]Capeak (wt%Ca) 22.88d [21.84-23.57]Cawidth (wt%Ca) 4.07f [3.81; 4.77]Calow (%) 7.05 [4.85-10.07]Cahigh (%) 6.38d,g [2.40-13.24]
Note: Paired data. Data are given as median [interquartile rangAbbreviations and definitions: BMDD, bone mineralization dens
of low mineralized bone; Camean, weighted mean calcium contenrhGH, recombinant human growth hormone; see Fig 1 legend for
aComparison of paired data before and after treatment: n �patients, only 1 cortex was available in 1 of their biopsy samples)
bn � 54 for cancellous and n � 53 for cortical BMDD in referencP � 0.05, dP � 0.001 versus normal reference data; eP � 0.00
group (comparison for n � 16 paired data before or after rhGHversus normal reference data.
plex than in adults because bones are not just remod-
Am J Kidney Dis. 2013;61(5):767-777
eled, but also modeled to grow in width and length.Hence, bone turnover and concomitantly bone histo-morphometric parameters vary during skeletal devel-opment, being more elevated during growth spurts ininfancy and puberty.13,25,29-31 We took advantage ofhistomorphometric reference data for children andadolescents being available for specific age rangesand classified each patient according to the approp-riate control group to get more accurate informationfor all relevant histologic descriptors.25 Of note, allour patients were in a prepubertal stage (Tanner scaleI or II) before initiating treatment despite 12 of thembeing aged 9.9-16 years.
Most remarkably, the histomorphometric finding ofa low-bone-turnover state before initiating treatmentwas completely consistent with quantitative backscat-tered electron imaging results showing abnormallyhigh bone matrix mineralization in cancellous andcortical bone.20 In principle, the BMDD curve isdependent on 2 processes: bone turnover and thekinetics of bone mineralization of the newly formedosteoid.17-19 It is well established that once mineraliza-tion starts in the unmineralized osteoid, a biphasicincrease in mineral content occurs. During the firstfew days, the mineral content increases rapidly up to70% of its final value, a phase referred as primarymineralization.18,19,32 In the subsequent phase re-ferred as secondary mineralization, the speed of min-eral deposition becomes much lower and it takesmonths to years for the newly formed young bone
ical Bone Before and After rhGH Treatment
After Treatment Pa Reference Datab
.24 [20.06-21.18] 0.07 20.95 (0.57)
.61 [20.74-22.04] 0.02 21.66 (0.52)00d [3.81-4.65] 0.06 3.47 [3.12; 3.64]02d [7.43-13.63] 0.2 6.14 [4.95; 7.99].45 [0.55-2.68] 0.002 0.90 [0.44; 1.48]
.92 [19.50-21.23] 0.003 20.45e [19.69; 20.98]
.71 [20.10-22.27] 0.004 21.14e [20.62; 21.71]1d,e [4.42-5.72] 0.004 3.81e [3.38; 4.35].93 [8.52-19.88] 0.03 9.06e [6.34; 14.96]38h [0.65-2.78] �0.001 0.46g [0.28; 1.18]
as mean (SD), P values show the effect of treatment.stribution; Cahigh, portion of fully mineralized bone; Calow, portion
eak, mode of the BMDD; Cawidth, heterogeneity in mineralization;er information.r cancellous BMDD, n � 16 for cortical BMDD (because for 2
ta.20
� 0.05, gP � 0.01 versus cancellous bone within the same studyent and for n � 53 paired data in reference cohort); hP� 0.01
Cort
20214.
11.1
1920
5.1141.
e] ority di
t; Cap
furth18 fo.ce da1, fPtreatm
packet to complete the remaining 30% of mineraliza-
773

e disies in
Nawrot-Wawrzyniak et al
tion. In a situation of normal mineralization kinetics,increased bone turnover leads to a shift of the BMDDpeak to lower mineral content values because theaverage mineralization period for the bone packets isdecreased. Conversely, a decrease in bone turnovershifts the BMDD toward higher mineralization den-
Figure 3. Bone mineral density distribution variables beforedifferent TMV groups: (A) cancellous bone (Cn) and (B) corticalvalues for paired data. Normal range comprises mean � 1 SFratzl-Zelman et al.20 Open symbols correspond to values prior tthat the TMV subgroup is always that determined before treatmmode of the BMDD; Cawidth, heterogeneity in mineralization; Calo
bone; MUO, mixed uremic osteodystrophy; ABD, adynamic bonaddresses bone turnover, mineralization defects, and abnormalit
Table 5. Correlation of BMDD Measures of Cancellous BoneBefore rhGH Treatment
BMDDVariable
Correlation WithHistomorphometric
BFR/BS P
CorrelationWith
Serum ALP P
Camean �0.72 �0.001 �0.51 0.03
Capeak �0.69 0.001 �0.45 0.06
Cawidth 0.52 0.02 0.46 0.06
Calow 0.58 0.01 0.63 0.005
Cahigh �0.55 0.02 �0.37 0.1
Note: N � 18. Data are Spearman rank order correlationcoefficients and corresponding P values.
Abbreviations and definitions: rhGH, recombinant humangrowth hormone; ALP, alkaline phosphatase; BFR/BS, boneformation rate per bone surface; BMDD, bone mineralizationdensity distribution; Cahigh, portion of fully mineralized bone;Calow, portion of low mineralized bone; Camean, weighted meancalcium content; Capeak, mode of the BMDD; Cawidth, heterogene-ity in mineralization; rhGH, recombinant human growth hormone;
see Fig 1 legend for further information.774
sity because of prolonged duration of mineralizationfor the bone packets. In the latter case, BMDD reflectsan increased amount of older and higher mineralizedbone packets.17,33 Hence, the 4.5-fold increase inCahigh found in our pretreated cohort is particularlyunusual in growing children and adolescents andinstead corresponds to adults, who are characterizedby much lower bone remodeling rates.17,20 Evaluationof the single TMV subgroups confirmed that theelevated Camean, Capeak, and Cahigh values were foundmainly in the adynamic bone disease and mixeduremic osteodystrophy groups, whereas in normalbone subtypes, these BMDD parameters were mostlywithin normal range or slightly higher. It is worthnoting that our findings do not contradict currentobservations showing a high prevalence of mineraliza-tion defects as defined by histology in children, adoles-cents, and young adults with CKD on dialysistherapy.3,10 In contrast to histology, quantitative back-scattered electron imaging measures the mineral con-tent of the bone matrix, whereas the unmineralizedosteoid remains “invisible” and is not included in theBMDD outcomes.
Consistent with the observed increase in bone turn-over after rhGH treatment, we found in our cohort a
after recombinant human growth hormone treatment within the(Ct). Data points and bars show median (25th, 75th percentile)interquartile range around the median of reference data fromtment; filled symbols, to the same patients after treatment. Notebbreviations: Camean, weighted mean calcium content; Capeak,
rtion of low mineralized bone; Cahigh, portion of fully mineralizedease; NB, normal bone; OM, osteomalacia; TMV, system thatbone volume.
andboneD oro treaent. Aw, po
shift toward normal reference BMDD mirrored by
Am J Kidney Dis. 2013;61(5):767-777

Bone Matrix Mineralization in Young People With CKD
decreased Camean, Capeak and Cahigh and increasedCawidth and Calow values. Moreover, the decrease inCamean and Capeak values was found in every sub-group except normal bone, for which BMDD alreadywas within normal range before treatment. The in-crease in mineralization heterogeneity with Cawidth
and Calow values above normal range most likely islinked to the increased formation of new bone matrixand was found in all TMV subgroups.
Cortical width in these transiliac bone biopsysamples was not markedly increased after therapy. Ingeneral, in healthy children, the increase in corticalthickness of the iliac bone is very slow. This is relatedto the fact that modeling activity during growth leadsto an outward drift of the cortical compartments,whereas only the internal cortex increases inwidth.25,29,34 During modeling drift, trabeculae be-come incorporated into the inner cortex and the spacebetween them fills up with new bone tissue, leading toa transient decrease in matrix mineralization.29,34 As adirect consequence, the lower mineralization densityin the cortex compared to trabecular bone is linkedintimately to skeletal growth. Consistently, we foundafter rhGH treatment in our patients with CKD a trendtoward lower and more heterogeneous matrix mineral-ization in cortical than in cancellous bone, similar tothat observed in the reference cohort,20 another indica-tion of increased bone metabolic activity. The de-crease in mineral content of the bone matrix as mea-sured by quantitative backscattered electron imagingis in line with result of a previous peripheral quantita-tive computed tomography study showing a continu-ous decrease in cortical mineral density of the radiusin prepubertal growth hormone-deficient children af-ter rhGH treatment.35
For further information about the relationship ofBMDD outcomes with bone turnover in patients, weconducted correlation analyses with bone formationrates. Considering the total cohort before rhGH treat-ment, we observed that Camean was always high whenbone formation rate was low and vice versa. Thismeans that bone turnover rate is a strong predictor ofBMDD and changes in mineralization kinetics do notseem to be an influencing factor. Moreover, a strongassociation between serum ALP level and mean cal-cium content and percentage of low mineralized areaparameters was found. On the one hand, ALP level isincreased in patients with CKD and severe hyperpara-thyroidism, and on the other hand, it mirrors osteo-blast activity, which increases in periods of growth.Our results show that except for one patient with ALPvalues �1,200 U/L, the other values did not exceedtwice the normal range. Therefore, we interpreted theincrease in ALP levels after rhGH treatment as an
increase in bone turnover rates that drives the degreeAm J Kidney Dis. 2013;61(5):767-777
of bone matrix mineralization to lower values in ourcohort, confirming previous findings.35
It is worth noting that patients classified as havingadynamic bone disease, representing a homogeneouslow-bone-turnover subgroup with increased mineral-ization density, showed a marked increase in boneformation rate after rhGH treatment paralleled by aconsistent decrease in bone matrix mineralization.The latter caused a decrease in the range of BMDDvariables and the lack of significant correlations withbone formation rate and ALP level after rhGH.
This study has several limitations: Sample size perTMV subgroup was low.23,36 Also, it would have beenimportant to examine circulating levels of fibroblastgrowth factor 23, a newly described phosphaturichormone that has critically elevated levels from theonset of kidney failure, impacting directly on bonematrix mineralization and mineral homeostasis.37-39
Unfortunately, when the original study was initiated,the role of fibroblast growth factor 23 was mostlyunknown and assays were not available.9
In conclusion, the present data obtained from pairedbiopsy specimens from children and adolescents withCKD before and after rhGH treatment indicate thatalterations in bone material properties result fromabnormal bone turnover rather than from disturbedmineralization kinetics. Histomorphometry and quan-titative backscattered electron imaging analysis in ourgrowth-deficient patients showed low bone turnoverand consistently increased bone matrix mineraliza-tion. One year of therapy with rhGH led to a boost inbone turnover, reflected by an increase in height,histomorphometric indexes of bone formation rate,and serum ALP levels and a shift of BMDD towardthe normal range. Whether these changes are benefi-cial for biomechanical competence of bone after rhGHtreatment is unknown. Nevertheless, it can be con-cluded from the present data that growth retardation inaffected children and adolescents might be associatedwith impaired bone turnover and that GH treatmentnot only corrects height deficits, but also increases therate of bone turnover, which is a necessary conditionfor growth and concomitant normal bone matrix min-eralization.
ACKNOWLEDGEMENTSThe authors thank Dr Andrzej Debinski for preparation and
embedding of the biopsy specimens and Phaedra Messmer, DanielaGabriel, and Sonja Lueger for excellent technical assistance andperforming the quantitative backscattered electron imaging mea-surements.
Support: This study was supported by the AUVA (Researchfunds of the Austrian Workers’ Compensation Board) and theWGKK (Viennese Sickness Insurance Funds).
Financial Disclosure: The authors declare that they have no
relevant financial interests.775

Nawrot-Wawrzyniak et al
REFERENCES1. Moe S, Drueke T, Cunningham J, et al. Definition, evalua-
tion, and classification of renal osteodystrophy: a position state-ment from Kidney Disease: Improving Global Outcomes (KDIGO).Kidney Int. 2006;69(11):1945-1953.
2. KDIGO clinical practice guideline for the diagnosis, evalua-tion, prevention, and treatment of chronic kidney disease-mineraland bone disorder (CKD-MBD). Kidney Int Suppl. 2009;(3):S1-S130.
3. Bakkaloglu SA, Wesseling-Perry K, Pereira RC, et al. Valueof the new bone classification system in pediatric renal osteodystro-phy. Clin J Am Soc Nephrol. 2010;5(10):1860-1866.
4. Malluche HH, Mawad HW, Monier-Faugere MC. Renalosteodystrophy in the first decade of the new millennium: analysisof 630 bone biopsies in black and white patients. J Bone MinerRes. 2011;26(6):1368-1376.
5. Malluche HH, Monier-Faugere MC. Renal osteodystrophy:what’s in a name? Presentation of a clinically useful new model tointerpret bone histologic findings. Clin Nephrol. 2006;65(4):235-242.
6. Borzych D, Rees L, Ha IS, et al. The bone and mineraldisorder of children undergoing chronic peritoneal dialysis. KidneyInt. 2010;78(12):1295-1304.
7. Lobao R, Carvalho AB, Cuppari L, et al. High prevalence oflow bone mineral density in pre-dialysis chronic kidney diseasepatients: bone histomorphometric analysis. Clin Nephrol. 2004;62(6):432-439.
8. Yalcinkaya F, Ince E, Tumer N, Ensari A, Ozkaya N. Spec-trum of renal osteodystrophy in children on continuous ambulatoryperitoneal dialysis. Pediatr Int. 2000;42(1):53-57.
9. Ziolkowska H, Paniczyk-Tomaszewska M, Debinski A,Polowiec Z, Sawicki A, Sieniawska M. Bone biopsy results andserum bone turnover parameters in uremic children. Acta Paediatr.2000;89(6):666-671.
10. Wesseling-Perry K, Pereira RC, Tseng CH, et al. Earlyskeletal and biochemical alterations in pediatric chronic kidneydisease. Clin J Am Soc Nephrol. 2012;7(1):146-152.
11. Tonshoff B, Kiepe D, Ciarmatori S. Growth hormone/insulin-like growth factor system in children with chronic renal failure.Pediatr Nephrol. 2005;20(3):279-289.
12. Mehls O, Wuhl E, Tonshoff B, Schaefer F, Nissel R,Haffner D. Growth hormone treatment in short children withchronic kidney disease. Acta Paediatr. 2008;97(9):1159-1164.
13. Mahesh S, Kaskel F. Growth hormone axis in chronickidney disease. Pediatr Nephrol. 2008;23(1):41-48.
14. Haffner D, Schaefer F, Nissel R, Wuhl E, Tonshoff B,Mehls O. Effect of growth hormone treatment on the adult heightof children with chronic renal failure. German Study Group forGrowth Hormone Treatment in Chronic Renal Failure. N EnglJ Med. 2000;343(13):923-930.
15. Hokken-Koelega AC, Saenger P, Cappa M, Greggio N.Unresolved problems concerning optimal therapy of puberty inchildren with chronic renal diseases. J Pediatr Endocrinol Metab.2001;14(suppl 2):945-952.
16. Panczyk-Tomaszewska M, Ziolkowska H, Debinski A, Sie-niawska M. Vitamin D metabolite requirements in dialysed chil-dren receiving recombinant human growth hormone. Nephrol DialTransplant. 2000;15(3):375-378.
17. Roschger P, Paschalis EP, Fratzl P, Klaushofer K. Bonemineralization density distribution in health and disease. Bone.2008;42(3):456-466.
18. Ruffoni D, Fratzl P, Roschger P, Klaushofer K, WeinkamerR. The bone mineralization density distribution as a fingerprint of
the mineralization process. Bone. 2007;40(5):1308-1319.776
19. Ruffoni D, Fratzl P, Roschger P, Phipps R, Klaushofer K,Weinkamer R. Effect of temporal changes in bone turnover on thebone mineralization density distribution: a computer simulationstudy. J Bone Miner Res. 2008;23(12):1905-1914.
20. Fratzl-Zelman N, Roschger P, Misof BM, et al. Normativedata on mineralization density distribution in iliac bone biopsies ofchildren, adolescents and young adults. Bone. 2009;44(6):1043-1048.
21. Levey AS, Eckardt KU, Tsukamoto Y, et al. Definition andclassification of chronic kidney disease: a position statement fromKidney Disease: Improving Global Outcomes (KDIGO). KidneyInt. 2005;67(6):2089-2100.
22. Greulich W. Radiographic Atlas of Skeletal Development ofthe Hand and Wrist. Palo Alto, CA: Stanford University Press;1993.
23. Wesseling K, Bakkaloglu S, Salusky I. Chronic kidneydisease mineral and bone disorder in children. Pediatr Nephrol.2008;23(2):195-207.
24. Parfitt AM, Drezner MK, Glorieux FH, et al. Bone histomor-phometry: standardization of nomenclature, symbols, and units.Report of the ASBMR Histomorphometry Nomenclature Commit-tee. J Bone Miner Res. 1987;2(6):595-610.
25. Glorieux FH, Travers R, Taylor A, et al. Normative data foriliac bone histomorphometry in growing children. Bone. 2000;26(2):103-109.
26. Roschger P, Fratzl P, Eschberger J, Klaushofer K. Validationof quantitative backscattered electron imaging for the measure-ment of mineral density distribution in human bone biopsies. Bone.1998;23(4):319-326.
27. Roschger P, Gupta HS, Berzlanovich A, et al. Constantmineralization density distribution in cancellous human bone.Bone. 2003;32(3):316-323.
28. Kuizon BD, Goodman WG, Juppner H, et al. Diminishedlinear growth during intermittent calcitriol therapy in childrenundergoing CCPD. Kidney Int. 1998;53(1):205-211.
29. Parfitt AM, Travers R, Rauch F, Glorieux FH. Structuraland cellular changes during bone growth in healthy children. Bone.2000;27(4):487-494.
30. Szulc P, Seeman E, Delmas PD. Biochemical measurementsof bone turnover in children and adolescents. Osteoporos Int.2000;11(4):281-294.
31. Rauchenzauner M, Schmid A, Heinz-Erian P, et al. Sex- andage-specific reference curves for serum markers of bone turnoverin healthy children from 2 months to 18 years. J Clin EndocrinolMetab. 2007;92(2):443-449.
32. Roschger P, Dempster DW, Zhou H, et al. New observationson bone quality in mild primary hyperparathyroidism as deter-mined by quantitative backscattered electron imaging. J BoneMiner Res. 2007;22(5):717-723.
33. Boivin G, Meunier PJ. Changes in bone remodeling rateinfluence the degree of mineralization of bone. Connect TissueRes. 2002;43(2-3):535-537.
34. Rauch F, Travers R, Glorieux FH. Cellular activity on theseven surfaces of iliac bone: a histomorphometric study inchildren and adolescents. J Bone Miner Res. 2006;21(4):513-519.
35. Schweizer R, Martin DD, Schwarze CP, et al. Cortical bonedensity is normal in prepubertal children with growth hormone(GH) deficiency, but initially decreases during GH replacementdue to early bone remodeling. J Clin Endocrinol Metab. 2003;88(11):5266-5272.
36. Schmitt CP, Mehls O. Mineral and bone disorders in chil-dren with chronic kidney disease. Nat Rev Nephrol. 2011;7(11):624-
634.Am J Kidney Dis. 2013;61(5):767-777

Bone Matrix Mineralization in Young People With CKD
37. Hruska KA, Mathew S. The roles of the skeleton andphosphorus in the CKD mineral bone disorder. Adv ChronicKidney Dis. 2011;18(2):98-104.
38. Wesseling-Perry K, Pereira RC, Wang H, et al. Relationship
between plasma fibroblast growth factor-23 concentration andAm J Kidney Dis. 2013;61(5):767-777
bone mineralization in children with renal failure on peritonealdialysis. J Clin Endocrinol Metab. 2009;94(2):511-517.
39. Quarles LD. Role of FGF23 in vitamin D and phosphatemetabolism: implications in chronic kidney disease. Exp Cell Res.
2012;318(9):1040-1048.777














![Indigenous Enhanced Mineralization Pyrene, Benzo[a]pyrene ...Indigenous soil microorganism mineralization experiments. All of the mineralization experiments were performed by using](https://static.fdocuments.us/doc/165x107/5e7c41b0b7c4ef64181e5e16/indigenous-enhanced-mineralization-pyrene-benzoapyrene-indigenous-soil-microorganism.jpg)