Cataract
-
Upload
kornflakes -
Category
Documents
-
view
12 -
download
1
description
Transcript of Cataract

Cataract

Cataract
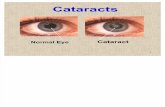
Is a condition that develops in the lens of the eye. It is an opacity of
the eye’s normally clear, transparent crystalline lens. Cataracts are
made from a protein that has altered from its natural state
(denaturation), destroying and eventually prohibiting required light
from entering into the retina, the part of the eye that receives light.
Often cataracts cause no problems for many years but as the
cataract mature, the cloudiness increases on the lens, the light
reaching the retina decreases and significant sight loss and
perhaps blindness can result. Cataracts are considered a condition
and not a disease therefore they develop for multiple reasons.



Anatomy and Physiology
The eye is a sensitive, highly specialized sense organ subject to various disorders, many of which lead to impaired vision. The eye is available for external examination, and its anatomy is more easily assessed that many other body parts.
The eyeball, or globe, sits in a protective bony structure known as the orbit. Lined with muscle and connective and adipose tissue, the orbit is about 4 cm high, wide, and deep, and it shaped roughly like a four sided pyramid, surrounded on three sides by thesinuses; ethmoid, frontal and maxillary. The optic nerve and the optalmic artery enter the orbits at its apex through the optic foramen. The eyeball is moved through all fields of gaze by the extraocular muscles.

The eyelids, composed of thin elastic skin that covers striated
and smooth muscles, protect the anterior portion of the eye.
The upper lid normally covers the upper most portion of the iris
and is innervated by the oculomotor nerve. The lid margins contain
meimbomian glands, the inferior and superior puncta, and the
eyelashes. The triangular spaces formed by the junction of the
eyelids are known as the inner or median canthus and the outer or
lateral canthus. With every blink of the eyes , the lids wash the
cornea and conjunctiva with tears.
The conjunctiva, a mucous membrane, provides a barrier to the
external environment and nourishes the eye. The bulbar
conjunctiva covers the sclera, whereas the palpebral conjunctiva
lines the inner surface of the upper and the lower eyelids.

The sclera commonly known as the white of the eye,
is a dense fibrous structure that comprises the posterior five sixths of the eye. The sclera helps to maintain the shape of the eyeball and protects the intraocular contents from trauma .
The conjunctiva meets the cornea at the limbus at the outermost edge of the iris. The cornea, a transparent, avascular, domelike structure, forms the most anterior portion of the eyeball and is the main refracting surface of the eye. It is composed of the five layers: epithelium, Brownman’s membrane, stroma, Descemet’s membrane, and endothelium. Behind the cornea lies the anterior chamber, filled with a continually replenished supply of aqueous humor, which nourishes the cornea.

The uvea consist of the iris, the ciliary body, and the
choroid. The iris, or the colored part of the eye, is highly
vascularized, pigmented collection of fibers surrounding
the pupil. The pupil is a space that dilates and constrict
in response to light.

Pathophysiology The three most common type of senile cataracts are defined by their location in the lens: nuclear, cortical and posterior subcapsular.A Nuclear cataract is associated with myopia, which worsens when the cataracts progresses. If dense, the cataract severelyblurs vision. A Cortical cataract involves the anterior, posterior, or equatorial cortex of the lens. A cataract in the equator of the cortex does not interfere with the passage of light through the center of the lens and has little effect on vision. Cortical cataracts progress at a highly variable rate. Vision is worst in very bright light.Posterior Subcapsular cataracts occur in front of the posterior capsule. This type typically develops in younger people and, in some cases, is associated with prolonged corticosteroid use, inflammation or trauma. Near vision is diminished, and the eye is increasingly sensitive to glare from bright light.

Causes of Cataracts Aging
Congenital disorders Genetic abnormalities Maternal rubella during 1st trimester Traumatic Complicated cataract Glaucoma Retinal detachment Diabetes Mellitus Retinitis pigmentosa Hypoparathyroidism Myotonic Dystrophy Atopic dermatitis Exposure to ionizing radiation or infrared rays

Drugs that are toxic to the lens
Prednisone
Ergot alkaloids
Dinitrophenol
Napthalene
Phenothiazines
Pilocarpine
Exposure to ultraviolet rays.

Clinical Manifestation
Diminished visual acuity, disabling sensitivity to glare, painless, dimmed or blurred vision with distortion of images, poor night vision.
Myopic shift, astigmatism, monocular diplopia, brunescence (color values shift to yellow brown) and reduced light transmission.
Yellowish, gray or white pupil Frequent changes in eyeglass prescription.

Assessment and Diagnostic findings
Physical examination Degree of visual acuity is directly
proportionate to density of the cataract Snellen visual acuity test Opthalmoscopy Slit lamp bimicroscopic examination A-scan ultrasonography Contrast sensitivity test Glare test

Medical Management
There is no medical treatment for cataracts,
although use of vitamin C, betacarotine and
vitamin E is being investigated. Glasses or
contact, bifocal or magnifying lenses may
improve vision. Mydriatics can be used as short
termed treatment to dilate pupils and allow
more light to enter the retina, although this
increases glare.

Surgical Management
Two surgical techniques are available: Intracapsular cataract extraction (ICCE) and extracapsular cataract extraction (ECCE) including phacoemulsification. Less than 15% of people require surgery.
Indications for surgery are loss of vision that interferes with normal activates or a cataract that is causing glaucoma. Cataracts are removed under local anesthesia on an outpatient basis. Restoration of visual function through a safe and minimally invasive procedure is the surgical goal. Lens replacement may involve aphakic eyeglasses, contact lens, and intraocular lens implants. When both eyes have cataracts, one eye is surgically treated at a time, providing for the first eye to recover.

Intracapsular Cataract Extraction
The entire lens is removed and fine
sutures close the incision. It is
infrequently performed today: however it
is indicated when there is a need to
remove the entire lens, such as a
subluxated cataract.

Extracapsular Cataract Extraction
Achieves the intactness of smaller incisional wounds and maintenance of the posterior capsule of the lens, reducing post operative complications, particularly aphakik retinal detachment and cystoid macular edema. In ECCE, a portion of the anterior capsule is removed, allowing extraction of the lens nucleus and cortex. This surgery facilitates insertion of an intraocular lens.

Phacoemulsification
This method of extracapsular surgery uses an
ultrasonic device that liquefies the nucleus and
cortex, which are then suctioned out through a
tube. Because the incision is even smaller than
the standard ECCE, the wounds heals more
rapidly and there is early stabilization of
refractive error and less astigmatism.

Lens Replacement
After removal of the crystalline lens, the
patient is referred to as aphakic (without
lens). The lens which focuses light on the
retina, must be replaced for the patient to
see clearly

Assessment
Obtain a health history
Assess for visual acuity
Assess for milky white pupil due to lens opacity
Assess for blinding glare

Diagnosis
Disturbed visual sensory perception related to altered sensory reception, status of sense organs and therapeutically restricted environment possibly evidenced by diminished acuity, visual distortions and change in visual response to stimuli.
Risk for injury: Risk factor may include poor vision, reduced hand/eye coordination.
Anxiety related to alteration in visual acuity, threat of permanent loss of vision /independence, possibly evidenced by expressed concerns, apprehension and feelings of uncertainty.
Deficient knowledge regarding ways of coping with altered abilities, related to misinterpretation or cognitive limitation.

Planning and Goal
The major goals of the patient may
include improved sensory function,
preventing injury, reducing anxiety and
enhanced knowledge regarding ways of
coping.

Nursing Interventions
1. Managing and Improving sensory function Approach patient with a decreased field of
vision on the side where visual perception is intact.
Teach patient to turn and look in the direction in the defective visual field to compensate for the loss: make eye contact with the patient and draw attention to the affected side
Provide eyeglasses to improve vision.

2. Preventing injury
Protect patient from injury
Instruct the patient not to carry heavy object
Instruct the client not to bend
Assist the client when moving
3. Reducing Anxiety
Establish a therapeutic relationship with the patient.
Re available to client for listening and talking.
Provide comfort measures.
Assist client to develop self awareness.
Acknowledge anxiety/fear.

4. Enhancing Knowledge or Learning
Ascertain level of knowledge.
Provide information relevant to the situation.
Provide positive reinforcement.
Provide active role in client learning process.
Provide for feedback and evaluation learning.

Evaluation Expect patient outcome
1. Shows improvement in sensory function
2. Remains free of injury
3. Reports being less anxious
4. Participates in learning process

















![Overview of Congenital, Senile and Metabolic Cataractrelated cataract [7] and metabolic cataract [8]. Congenital & Senile Cataract Cataract is a clouding of the eye’s natural lens](https://static.fdocuments.us/doc/165x107/5f361b7a353bcc123d74d127/overview-of-congenital-senile-and-metabolic-cataract-related-cataract-7-and-metabolic.jpg)