Case Study Congestive Heart Failure
-
Upload
cynthia-lee -
Category
Documents
-
view
375 -
download
0
Transcript of Case Study Congestive Heart Failure
Running head: Congestive Heart Failure: A Comprehensive Study 1
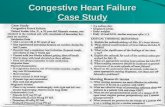
Congestive Heart Failure: A Comprehensive Case Study
Cynthia T. Lee
University of Arizona
Congestive Heart Failure 2
Congestive Heart Failure: A Comprehensive Case Study
The patient is a 65-year-old African-American male with a history of coronary artery
disease, essential hypertension, tobacco-use, abdominal, aortic, and renal artery aneurysms, and
Hepatitis C. His surgical history includes a L4-L5 laminectomy (in 2010) and a coronary artery
bypass graft (in 2007). His chief complaint for his visit to the emergency department (ED) was
back pain. Upon ED assessment, the patient was found to have signs and symptoms of heart
failure: dyspnea, weight gain, abdominal distension, bilateral leg edema, and complaints of
fatigue. Diagnostic tests were performed and confirmed heart failure (see Physician’s Orders and
Diagnostic Tests section). The patient was then transferred to the cardiac floor with the medical
diagnosis of congestive heart failure. The patient’s heart failure is categorized as a New York
Heart Association (NYHA) class III, which means the patient is comfortable at rest usually, but
is limited upon exertion. Less than ordinary physical activity causes dyspnea, angina pain,
palpitations, or fatigue (Lewis et al., 2014)
The patient is a retired veteran who graduated from high school with his diploma. He
states that he is a smoker and smokes two packs of cigarettes per day. The patient mentioned that
he has been doing this for the past thirty years and has not tried quitting in the past. This retired
veteran also drinks two beers on a daily basis. He has a body mass index (BMI) of 34.4, which
places him in the obese category. The patient does not engage in any routine physical activity,
and leads a sedentary lifestyle.
This veteran resides at home with his wife; he is her primary caregiver. They have three
sons, all of which have families of their own. He is currently worried about his wife since she
recently had a stroke. The patient is alert and oriented, and has a friendly disposition. He is
cooperative, and responds appropriately to instruction. The patient is allergic to beta-lactam
Congestive Heart Failure 3
antimicrobials, and is currently on two liters of oxygen via nasal cannula. He does not use any
ambulatory aids, nor does he have a history of falls. The patient does not exhibit suicide ideation
and does not have any barriers to learning.
Physiology
The cardiovascular system is made up of the heart and blood vessels. The blood vessels
are arranged into two loops: systemic circulation and pulmonary circulation. While the heart
contracts, it simultaneously pumps blood into both loops (Lewis et al, 2014) The heart is capable
of making adjustments in stroke volume to meet the body’s changing metabolic needs (Fletcher
&Thomas, 2001). The intrinsic elasticity of the myocardium allows optimal ventricular emptying
(cardiac output) without an increase in myocardial oxygen requirement or variation in average
arterial pressure (Fletcher &Thomas, 2001).
The cardiovascular system affects all other body systems as well, especially the
respiratory, renal, and digestive system. The respiratory system is responsible for four main
functions: supplying oxygen to the body for the production of energy, removing carbon dioxide
as a waste products of energy reactions, maintain homeostasis of arterial blood, and maintaining
heat exchange (Lewis et al., 2014). The renal system filters waste from the bloodstream and
produces urine to expel it from the body. The kidneys play an important role in that system; it
prevents the buildup of extra fluid in the body, keeps electrolyte levels stable, and makes
hormones that help regulate blood pressure (Lewis et al., 2014). The digestive system main
functions are to digest and absorb nutrients.
Pathophysiology
It is estimated that 5.1 million people currently have heart failure in the United States
(Lewis et al., 2014). According to the American Heart Association, over 600,000 new cases are
Congestive Heart Failure 4
diagnosed each year (Lewis et al., 2014). Nearly 10% of Americans over the age of 65 have
symptomatic heart failure, and approximately 20% of the asymptomatic individuals over the age
of 40 have some evidence of myocardial dysfunction (McCance & Huether, 2014). Hypertension
and coronary artery disease (CAD) are the primary risk factors for heart failure, both of which
are seen in the patient’s medical history. Other predisposing factors are the patient’s advanced
age, use of tobacco, and obesity (Lewis et al., 2014).
Heart failure is a condition that results from an abnormality in myocardial function. This
abnormality causes the heart the inability to deliver enough oxygenated blood to meet the
metabolic needs of the rest of the body (Fletcher & Thomas, 2001). When the right and left
ventricles fail to pump, pulmonary and systemic venous hypertension develops, which results in
the syndrome of CHF. The syndrome of CHF is associated with dyspnea upon rest and exertion,
lower extremity edema, and activity intolerance (Fletcher & Thomas, 2001). The patient
experiences all of these manifestations. He complained about shortness of breath upon exertion,
has +2 pitting edema, and does not engage in much physical activity.
Systolic dysfunction is characterized by an ejection fraction of less than 40%; this results
from the depression of the contractile force of the myocardium which often times results in a thin
and dilated heart muscle that is incapable of maintaining an adequate cardiac output (Fletcher &
Thomas, 2001). Systolic dysfunction is the most common cause of CHF and most often results
from myocardial infarction. Diastolic dysfunction is impairment in the diastolic filing of the left
ventricle and is secondary to the loss of muscle fiber elasticity. Diastolic dysfunction is
associated most often with long standing hypertension. Decreased ventricular compliance
(increased stiffness) and impaired ventricular relaxation are the mechanisms responsible for
diastolic dysfunction (Fletcher & Thomas, 2001). Impairment in the diastolic filling of the left
Congestive Heart Failure 5
ventricle can be the result of ischemia, hypertrophy, reduction in beta-adrenergic tone, or
increased myocardial connective tissue. The increased work of the left ventricle eventually
causes hypertrophy of the muscle, which further decreased the contractility of the muscle fiber
and results in impaired relation. The hypertrophied left ventricle is unable to adequately fill,
leading to decreased stroke volume, decreased cardiac output, and symptoms of CHF (Fletcher &
Thomas, 2001). The low cardiac output simulates the compensatory neuro-hormonal systems
that increase circulating blood volume and filling pressures and results in further pulmonary
congestion. The patient’s chest x-ray confirmed the patient’s pulmonary congestion. Crackles are
audible in the lower bases of the patient’s lungs, and he suffers from dyspnea.
Other body organs are affected by CHF: the lungs, kidney, liver, intestines, and
peripheral extremities. The lungs may become congested with fluid thereby increasing activity
intolerance. The reduced function of the kidneys can cause the body to retain more fluid
(McCance & Huether, 2014). Fluid may also accumulate in the liver, which impairs its ability to
produce essential proteins and rid toxins in the body. Intestines may be less efficient in its
absorption of nutrients and medicine. The retained fluid may accumulate in the extremities,
causing peripheral edema.
Physicians Orders and Diagnostic Tests
The physician’s orders for this patient were a fluid restriction of less than 1500mL per
day, strict measurement of inputs and outputs, a cardiac diet, and daily weights. These are all
common orders for those diagnosed with CHF. These orders were easy to enforce because the
medical staff measured the patient’s intake of liquids after every meal and were aware of how
many times his pitcher was filled a day. The patient also uses a urinal, so his urine output was
measured frequently. When an order is put in for a cardiac diet, a low-sodium food tray is sent up
Congestive Heart Failure 6
to the patient’s room for every meal. The diagnostic tests performed on the patient were labs, a
chest x-ray and also an abdominal/ pelvic x-ray. The patient’s hemoglobin levels were low. This
lab measures the gas-carrying ability of red blood cells. When this lab value is low, it indicates
excess fluid volume, which is a common manifestation of CHF. The patient had pitting edema
and a distended abdomen. The patient’s blood urea nitrogen (BUN) values were high. An
increased level of BUN indicates a reduction of the glomerular filtration rate, which means the
kidneys are having problems. If the kidneys are struggling, this supports why there is excess
fluid volume. For a more comprehensive list of lab results, see Appendix B. The purpose of the
chest x-ray was for the patient’s shortness of breath. Crackles were also heard in the lower lobes
of the lungs. The x-ray results showed pulmonary congestion, which is a manifestation of CHF.
The patient had a distended stomach, so an order for an abdominal x-ray was placed. This x-ray
showed an accumulation of fluid in the abdomen. There were no signs of obstruction (Appendix
C).
Medications
The patient’s medical regime is fairly extensive, so only those concerning CHF will be
discussed in this section. For a list of the patient’s full medication regime, please see Appendix A
The medications most commonly used to treat CHF are ACE inhibitors, beta-blockers, and
diuretics (Fletcher & Thomas, 2001). The patient is on the ACE inhib itor lisinopril, which is the
generic of Zestril or Prinivil. He currently gets a 40mg tablet by mouth daily. This drug works by
inhibiting the enzymatic conversion of angiotensin I to angiotensin II, a vasoconstrictor.
Lisinopril decreases both the afterload and preload. This medication also decreases water
retention, by inhibiting the stimulation of adrenal cortex to release aldosterone (Fletcher &
Thomas, 2001). Specifically for the patient, this medication treats his hypertension and his CHF.
Congestive Heart Failure 7
The nurse should monitor the patient’s neutrophil levels, blood pressure, and CHF symptoms.
The patient is very cooperative when taking his medications, and his blood pressure (though
high) has stayed stable for the clinical week.
The patient is on the beta-blocker carvedilol, which is the generic for Coreg. The patient
is taking a 3.125 mg tablet by mouth twice a day. This medication is a nonselective vasodilating
beta-blocker with moderate alpha-blocker activity. The therapeutic effects of carvedilol are to
decrease heart rate and blood pressure, improve cardiac output, and slow CHF progression
(Fletcher & Thomas, 2001). Carvedilol also improves renal hemodynamics in patients with CHF.
Nursing implications of this medication are to monitor blood pressure and pulse frequently
during dose adjustment and periodically during therapy. The nurse should also monitor daily
weight and intake and output. Again, the patient is cooperative in taking his medication. His
blood pressure remained steady for the clinical week, and his bilateral lower leg edema lessened
from a +2 to a +1.
The patient is on the diuretic furosemide, which is the generic for Lasix. He is taking
furosemide in two forms: intravenous push (IVP) and by tablet. His dosages are 40mg/4ml IVP
and a 40mg tablet every twelve hours. Diuretics inhibit the reabsorption of sodium and chloride
at the different sites in the renal tubules (Fletcher & Thomas, 2001). This patient abdomen is
distended, and he has pitting edema in his lower extremities. Furosemide was prescribed to the
patient specifically for the excess fluid in his system. Nursing implications for this medication
are to monitor patient’s fluid status: document intake and output, monitor blood pressure, and
check peripheral pulses. The patient’s blood pressure remained steady for the rest of the clinical
week. His radial, dorsal pedis, and post tibialis pulses were palpable bilaterally. The patient’s
bilateral, pitting edema reduced from a +2 to a +1.
Congestive Heart Failure 8
The patient is also taking acetylsalicylic acid also known as aspirin. He takes an 81mg
tablet once a day. Aspirin is an antiplatelet agent that has been proven to reduce ischemic events
in patients recovering from a myocardial infarction and patients with angina (Fletcher and
Thomas, 2001). Patients with heart failure secondary to CAD should be prescribed aspirin. The
nurse should assess for pain and monitor for any adverse reactions.
Nursing Diagnoses
Being that the patient was recently diagnosed with congestive heart failure, the nursing
diagnoses are focused on the manifestations from this chronic condition. It was understood that
the patient’s chief complaint was back pain; however, the back pain was a chronic condition that
the patient was aware of. He agreed that his treatment should be focused on CHF and mentioned
that he would like to learn more about his condition. The patient mentioned that his back pain
was a “lost cause.”
The first nursing diagnosis developed for the patient is impaired gas exchange related to
pulmonary congestion secondary to congestive heart failure as evidenced by decreased oxygen
saturations of 83%-90%, shortness of breath upon exertion, headache upon waking, smoking,
and crackles in the bilateral bases. The goal for this diagnosis is to maintain adequate oxygen and
carbon dioxide exchange. The smart, measureable, attainable, realistic, and time-based
(SMART) outcome for this diagnosis is the patient’s oxygen saturation will be at 92% or higher
by the end of the clinical week.
The interventions developed for this diagnosis are: monitor oxygen saturation using pulse
oximetry, work with the patient to determine which strategies help alleviate dyspnea, and
educate the patient on the rationale behind smoking cessation. The rational for the first
intervention is that pulse oximetry is useful in tracking and adjusting supplemental oxygen
Congestive Heart Failure 9
therapy (Lewis et al, 2014). The patient was hooked up to the pulse oximeter for the remainder
of the clinical week. If his oxygen saturation level went below 90%, the machine would start
beeping to alert the healthcare staff. Then the staff would adjust the oxygen as needed or tell the
patient to take deeper breaths. The rationale for the second intervention is that self-management
enables patients to use effective methods that manage their illness, which leads to more positive
outcomes (Lewis, et al., 2014). The patient stated that his dyspnea worsens when he is moving
around. The rationale for the third intervention is that by educating the patient on how
interventions are focused on the needs of his personal care and how the illness progresses,
patient’s symptom management is improved (Lewis et al., 2014). The patient verbalized that he
was willing to quit smoking, and that he has not smoked since he was admitted. His only concern
was if he would have resources if he needed them after his hospital stay, in which, I provided
him a handout.
The outcome for this diagnosis was fully met. By the end of my clinical week, the
patient’s oxygen saturation was at a 94% on two liters of oxygen via nasal cannula, and his
headache dissipated. The patient also stated that there was a reduction in his shortness of breath
as he moved from his bed to his chair.
The second nursing diagnosis is excess fluid volume related to the increase of venous
pressure and the decrease of renal perfusion secondary to congestive heart failure as evidenced
by patient’s rapid weight gain of twenty pounds in two months, adventitious breath sounds, and
bilateral edema in the lower extremities. The goal for this diagnosis is to reduce peripheral
edema. The SMART outcome for this diagnosis is that the patient’s bilateral lower leg pitting
edema will reduce from a +2 to a +1 by the end of the clinical week.
Congestive Heart Failure 10
The interventions for this patient are: educate the importance of restricting liquid intake
to 1500mL per day, educate the importance of reducing sodium intake to less than 2400mg per
day, and administer diuretic medications in a timely manner. The rational for the first and second
intervention is that decreasing fluid and sodium intake decreases extracellular water, which also
decreases edema, reduces activity intolerance, and enhances quality of life (Ramirez et al, 2004).
The patient verbalized understanding that his liquid intake should be less than 1.5 of those
hospital pitchers. He also verbalized that to help with thirst, he could suck on ice chips. The
patient also was able discuss which foods were high in sodium, for example, chips, canned
foods, microwaveable foods, and processed foods. He verbalized his understanding that products
that contain high sodium will cause water retention. The rational for the third intervention is that
administering heart failure medications can reduce mortality and morbidity and improve quality
of life and symptoms in heart failure patients (Clark, 2004). The patient was very cooperative in
taking his medications. He only refused heparin occasionally.
The outcome for this diagnosis was fully met. By the end of the clinical week the
patient’s pitting edema reduced from +2 to +1. The patient’s diuretics were administered on
time. The staff was well aware of his fluid restriction, and he had an order for a cardiac diet. The
patient’s legs looked less swollen, and he did not gain weight during the clinical week.
The third nursing diagnosis is activity intolerance related to imbalance of the patient’s
oxygen supply and demand as evidenced by dyspnea, shortness of breath, and weakness. The
goal for this diagnosis is to achieve a program of activity that balances physical exertion with
energy conservation techniques. The SMART outcome for this diagnosis is that the patient will
be able to ambulate to and from the bathroom five times by the end of the nursing shift.
Congestive Heart Failure 11
The interventions developed for this intervention are: allow for periods of rest before and
after exertion periods such as baths, treatments, meals, and physical activity, encourage that the
patient ambulates 30 minutes a day three times a week, and help the patient with energy
conservation pertaining to activities of daily living (ADLs). The rational for the first intervention
is that both physical and emotional rest help to lower arterial pressure and reduces the
myocardium workload (Lewis et al., 2014). The patient was told that he might need to take more
breaks than he was used to, and that this was common with heart failure. He verbalized that he
understood. The patient also demonstrated his understanding after he took his shower. He sat in
the shower for ten minutes before getting up to change. The rational for the second intervention
is that aerobic exercise can reduce mortality and morbidity and improve quality of life in patients
with mild to moderate heart failure (Clark et al., 2004). The patient verbalized understanding that
he should try to walk for thirty minutes three times a week. He mentioned that it would be a
challenge, but he would try his best. The patient was observed to be moving around more in his
room. The rational for the third intervention is that by simplifying the workload of ADLs, the
patient will experience less discomfort (Lewis et al., 2014). He would be able to complete his
normal activities without overly exerting himself. The patient was able to verbalize activities in
which he could modify to conserve energy, such as shaving, brushing his teeth, and combing his
hair on a stool rather than standing.
The outcome for this diagnosis was partially met. The patient ambulated to and from the
bathroom three times before the end of the nursing shift. The patient started breathing more
rapidly and complained of shortness of breath. He did take breaks between each ambulation to
and from the bathroom.
Congestive Heart Failure 12
Review of Literature
Fayazi, Zarea, Abbasi, and Ahmadi (2012) conducted a study to determine the effect of a
home-based walking program on the performance and quality of life in heart failure patients. The
design of this study was a quasi-experimental trial that compared eight weeks of a home-based
walking exercise program in a training group versus a control group. Assessments of
performance and quality of life were measured in both groups at entry and after eight weeks. The
study was conducted in a hospital that is linked to Iran University of Medical Sciences and also
in the patient’s homes. The design of the study was approved by the local hospital and informed
consent was obtained from the participating patients.
The sample size of this study consisted of sixty New York Heart Association (NYHA)
class II and III heart failure patients. Those included were between the ages of 40-75, had heart
failure for a duration of more than six months, a left ventricular ejection fraction of equal to or
less than forty percent, a documented ejection fraction conducted within the past year by
echocardiogram, stabilization on cardiac medications for at least six months prior to study
enrollment, and stable mild-to-moderate heart failure NYHA class II and III (Fayazi et al., 2012).
Those excluded from the study were those with chronic obstructive pulmonary disease (COPD),
documented ventricular tachycardia, exercise-induced ischemia, uncontrolled hypertension,
uncontrolled diabetes, orthopedic diseases, neurological diseases, renal insufficiency,
psychotropic usage, and psychiatric disorders (Fayazi et al., 2012). The individuals in both
groups matched according to age, sex, body mass index (BMI), heart failure, disease intensity,
disease duration, smoking status, and ejection fraction. The groups were split evenly, 30 in the
training group and 30 in the control group.
Congestive Heart Failure 13
The study used the Minnesota Living with Heart Failure Questionnaire (MLHFQ) to
assess quality of life. This questionnaire assessed the patient’s perception of the effects of heart
failure on the socioeconomic, psychological, and physical aspects of their life (Fayazi et al.,
2012). Patients responded to twenty-one questions using a six-point Liker scale, with 0 being the
best and 5 being the worst. Functional performance was measured by distance the patient was
able to reach in a six-minute period. Physical symptoms were observed by the investigator or
reported by the patients themselves.
The thirty individuals allotted to the exercise group were further instructed to keep a daily
activity log reporting heart rate, perceived exertion rating, exercise performed, duration of
exercise, and any symptoms experienced (Fayazi et al., 2012). These logs were collected
biweekly. These individuals walked for thirty minutes daily and participated in other exercises
three days a week for eight weeks. Those in the training group also received daily phone calls to
monitor adherence, progress, answer questions, and provide feedback.
Initial MLHFQ scores did not show any significant differences between the two groups;
however the statistical paired t-tests and Wilcoxon test showed there were significant differences
between mean QOL scores at entry and after eight weeks in the training group, and no significant
difference was seen between the control group at entry and after eight weeks (Fayazi et al.,
2012). The scores of the socioeconomic, physical, and psychological aspects in the training
group decreased from entry to after eight weeks. In the control group, only the psychological
decreased. Results from the six-minute walk test (6MWT) showed that there were not any
significant differences between the training and the control group initially (Fayazi et al., 2012).
Statistical paired t-tests demonstrated that significant differences existed between average
walking distance on the 6MWT at entry and after eight weeks in the training group, while there
Congestive Heart Failure 14
were not any significant differences in the pre and post test of the control group. Average
exercise time in the training group from week one to weak eight increased. Repeated measure
tests showed significant differences.
The NYHA class III patients in the training group had the greatest increase in distance
walked on the 6MWT and the most improvement in QOL scores and exercise time. The training
group experienced no adverse events during the 8-week program. This study demonstrates that
CHF patients can perform exercise training safely (Fayazi et al., 2012). Exercise training also
showed improvement in the different QOL aspects: physical, psychological and socioeconomic.
Functional performance improved in the training group significantly compared to the control
group as measured by the 6MWT.
A home-based exercise program can increase exercise capacity, performance, and quality
of life in CHF patients. This applies to the case study patient in that he is a NYHA class III
patient. He currently lives a sedentary lifestyle, and shows symptoms of dyspnea, fatigue, and
peripheral edema. By implementing a walking program for the patient, his CHF symptoms may
reduce and his QOL may improve. ADLs will be less of a challenge.
Ramirez, Martinez, Tejeda, Gonzalez, David, and Lafuente (2004) conducted a study to
determine the effects of nutritional intervention on the clinical status and quality of life in heart
failure patients. Patients in the intervention group had a diet with decreased intakes of sodium
(less than 2400mg per day) and fluids (less than 1500mL per day). These patients were found to
have a decrease in extracellular fluid, which results in reduced development of edema, an
elevated functional class, and an enhancement in quality of life due to their permitted
engagement of social activities. This study supports two of the interventions developed for the
case study patient: educate the importance of restricting liquid intake to 1500mL per day and
Congestive Heart Failure 15
educate the importance of reducing sodium intake to less than 2400mg per day. This study
implies that should the patient follow these restrictions, his edema will reduce and his activity
intolerance will decrease.
Clark, Davidson, Currie, Karimi, Duncan, and Thompson (2010) composed an article
about the importance of understanding and promoting effective self-care to heart failure patients.
This article lists evidence-based practices and categorizes them into sections: pharmacologic
treatment, diet and lifestyle, behavioral and lifestyle management, symptom monitoring, and
emerging therapies. Since this list is very comprehensive, all the interventions developed for the
patient are one of the points listed in this article. This article makes the implication that if the
patient follows the aforementioned interventions, his health status will improve.
Congestive Heart Failure 16
References
Clark, A., Davidson, P., Currie, K., Karimi, M., Duncan , A., & Thompson, D. (2010).
Understanding and promoting efective self-care during heart failure. Current Treatment
Options in Cardiovascular Medicine , 1-9.
Fayazi, S., Zarea, K., Abbasi, A., & Ahmadi, F. (2013). Effect of home-based walking on
performance and quality of life in patients with heart failure. Scandinavian Journal of
Caring Sciences , 246-252.
Fletcher, L., & Thomas, D. (2001). Congestive heart failure: understanding the pathophysiology
and management . Journal of the American Academy of Nurse Practitioners , 13 (6), 249-
257.
Lewis, S., Dirksen, S., Heitkemper, M., Bucher, L. (2014). Medical-surgical nursing:
Assessment and management of clinical problems (9th ed.). St. Louis, MO: Elsevier
Mosby.
McCance, K. L., &Huether, S. E. (2014).Pathophysiology: The biologic basis for disease in
adults and children (7th ed.).Brashers, V. L., & Rote, N. S. (eds.) St. Louis, MO:
ElsevierMosby.
Ramirez, C., Martinez , C., Tejeda, O., Gonzalez, R., David, N., & Lafuente, A. (2004). Effects
of a nutritional intervention on body composition, clinical status, and quality of life in
patients with heart failure. Nutrition , 890-895.
Valerand, A., Sanoski, C., & Deglin, J. (2014). Davis’s drug guide for nurses (14th ed.).
Philadelphia, PA: FA Davis Company.
I have reviewed the Code of Academic Integrity and can attest that this document is consistent with the provisions of the code and represents my own original work. Signed: Cynthia Lee
Congestive Heart Failure 17
Appendix A:
Drug Name
Generic and
Brand & Time
Due
Classification
and
Mechanism
of action
Actions and
Indications
Patient
dose,
Route,
and
frequency
Most common or
serious side effects
Contraindications &
Major Interactions
Nursing Interventions
and Patient Teaching
Atorvastatin Calcium Tablet
(Lipitor)
0900
Therapeutic: lipid-lowering
agents Pharmacologi
c: HMG-CoA reductase inhibitors
Action:
Inhibits 3-hydroxy-3-methylglutary
l-coenzyme A (HMG-CoA)
reductase, an enzyme which is responsible
for catalyzing an early step
in the synthesis of cholesterol.
Actions: • Lowering of
total and LDL cholesterol and
triglycerides. Slightly increases HDL
cholesterol. • Reduction of
lipids/cholesterol reduces the risk of
myocardial infarction and
stroke sequelae. • Slows the progression of
coronary atherosclerosis
with resultant decrease in coronary heart
disease-related events.
Indication: Lowering
cholesterol
40 mg tab PO daily
Abdominal cramps, constipation, diarrhea,
flatus, heartburn, rashes
Contraindications: • Hypersensitivity;
• Active liver disease or unexplained persistent
elevations in AST and ALT
Drug interations: CYP3A4 enzyme, bile
acid sequestrants (cholestyramine, colestipol), bile acid
sequestrants, cyclosporine,
gemfibrozil, itraconazole, colchicine, erythromycin,
clarithromycin, nelfinavir, ritonavir,/
saquinavir, lopinavir,/ ritonavir, fasamprenavir, digoxin, oral
contraceptives, warfarin
Food: grapefruit juice
Nursing intervention: Obtain a diet history,
especially with regard to fat consumption.
Patient teaching: Instruct patient to notify health
care professional if unexplained muscle pain,
tenderness, or weakness occurs, especially if accompanied by fever or
malaise
Congestive Heart Failure 18
Lisinopril Tablet (Zestril or
Prinivil)
0900
Functional class:
Antihypertensive,
angiotensin-converting enzyme 1
(ACE) inhibitor
Chemical class: Enalaprilat
lysine analog
Mechanism of action: Selectively
suppresses renin-
angiotensin-aldosterone system;
inhibits ACE, thereby
preventing conversion of angiotensin I
to angiotensin II
Action: Mild to moderate
hypertension, adjunctive
therapy of systolic CHF, acute MI
Indication:
Heart and blood pressure
40mg tab PO daily
CNS: vertigo, depression, stroke,
insomnia, paresthesias,
headache, fatigue, asthenia, dizziness CV: Chest pain,
hypotension, sinus tachycardia
EENT: blurred vision, nasal congestion,
GI: nausea, vomiting, anorexia,
constipation, flatulence, GI irritation, diarrhea,
hepatic failure, hepatic necrosis
GU: Proteinuria, renal insufficiency, sexual dysfunction,
impotence INTEG: rash,
pruritus MISC: muscle cramps,
hyperkalemia RESP: dry cough,
dyspnea SYST: Angioedema, anaphylaxis, toxic
epidermal necrolysis
Contraindications: Hypersensitivity;
• History of angioedema with previous use of
ACE inhibitors; • Concurrent use with aliskiren in patients with
diabetes or moderate-to-severe renal impairment
(CCr <60 mL/min) Drug interactions:
diuretics, antihypertensive agents,
potassium supplements, potassium-sparing diuretics, or potassium-
containing salt substitutes, angiotensin
II receptor antagonists, aliskien, NSAIDs, COX-2 inhibitors, and lithium
Nursing interventions: Monitor WBC--if
neutrophils <100/mm3, d/c
Baseline renal and hepatic function pre admin
Evaluate response: ↓BP, CHF symptoms
Teach: Taper off med gradually
Rise slowly--orthostatic hypotension
Avoid increasing K+ in diet Report dry cough
Congestive Heart Failure 19
Morphine I.R. Tab
(Astramorph PF, AVINza,
Duramorph PF, Embeda, Infumorph,
Kadian, MS Contin)
0500, 1100, 1700, 2300
Classification Therapeutic: opioid
analgesics Pharmacologi
c: opioid agonists
Mechanism of action: Binds
to opiate receptors in the CNS.
Alters the perception of
and response to painful stimuli while
producing generalized
CNS depression.
Action: Decrease in severity of pain.
Addition of naltrexone in
Embeda product is designed to prevent abuse
or misuse by altering the
formulation. Naltrexone has no effect unless
the capsule is crushed or
chewed. Indication: Pain
30mg tab PO q6h
Confusion, sedation, hypotension, constipation,
respiratory depression
Contraindications: Hypersensitivity; • Some products contain
tartrazine, bisulfites, or alcohol and should be
avoided in patients with known hypersensitivity; • Acute, mild,
intermittent, or postoperative pain
(extended/sustained-release); • Significant respiratory
depression (extended/sustained-
release); • Acute or severe bronchial asthma
(extended/sustained-release);
• Paralytic ileus (extended/sustained-release);
Drug interactions: MAO
inhibitors, alcohol,sedative/ hypnotics, clomipramine,
barbituates, tricyclic antidepressants,
antihistamines, partial-
Nursing intervention: Assess type, location, and intensity of pain
prior to and 1 hr following PO, subcut,
IM, and 20 min (peak) following IV administration. When
titrating opioid doses, increases of 25-50%
should be administered until there is either a 50% reduction in the
patient's pain rating on a numerical or visual
analogue scale or the patient reports satisfactory pain relief.
When titrating doses of short-acting morphine, a
repeat dose can be safely administered at the time of the peak if previous
dose is ineffective and side effects are minimal.
Assess level of consciousness, BP, pulse, and respirations
before and periodically during administration. If
respiratory rate is
Congestive Heart Failure 20
antagonist opioid analgesics,
buprenorphine, nalbuphine, butorphaol,
pentazocine, warfarin, cimetidine
Drug-natural products: kava-kava, valerian, and
chamomile
<10/min, assess level of sedation. Physical
stimulation may be sufficient to prevent
significant hypoventilation. Subsequent doses may
need to be decreased by 25-50%. Initial
drowsiness will diminish with continued use.
Patient Teaching: Instruct patient how and
when to ask for pain medication.
Morphine SR
Tab (Astramorph PF,
AVINza, Duramorph PF, Embeda,
Infumorph, Kadian, MS
Contin) 0900, 2100
Therapeutic:
opioid analgesics
Pharmacologic: opioid agonists
Mechanism of
action: Binds to opiate receptors in
the CNS. Alters the
perception of and response to painful
stimuli while
Action:
Decrease in severity of pain.
Addition of naltrexone in Embeda product
is designed to prevent abuse
or misuse by altering the formulation.
Naltrexone has no effect unless
the capsule is crushed or chewed.
30mg tab
PO bid
Confusion, sedation,
hypotension, constipation,
respiratory depression
Contraindications:
Hypersensitivity; • Some products contain
tartrazine, bisulfites, or alcohol and should be avoided in patients with
known hypersensitivity; • Acute, mild,
intermittent, or postoperative pain (extended/sustained-
release); • Significant respiratory
depression (extended/sustained-release);
• Acute or severe
Nursing intervention:
Assess type, location, and intensity of pain
prior to and 1 hr following PO, subcut, IM, and 20 min (peak)
following IV administration. When
titrating opioid doses, increases of 25-50% should be administered
until there is either a 50% reduction in the
patient's pain rating on a numerical or visual analogue scale or the
patient reports
Congestive Heart Failure 21
producing generalized
CNS depression.
Indication: Pain bronchial asthma (extended/sustained-
release); • Paralytic ileus
(extended/sustained-release);
Drug interactions: MAO inhibitors,
alcohol,sedative/ hypnotics, clomipramine, barbituates, tricyclic
antidepressants, antihistamines, partial-
antagonist opioid analgesics, buprenorphine,
nalbuphine, butorphaol, pentazocine, warfarin,
cimetidine Drug-natural products:
kava-kava, valerian, and chamomile
satisfactory pain relief. When titrating doses of
short-acting morphine, a repeat dose can be safely
administered at the time of the peak if previous dose is ineffective and
side effects are minimal. Assess level of
consciousness, BP, pulse, and respirations before and periodically
during administration. If respiratory rate is
<10/min, assess level of sedation. Physical stimulation may be
sufficient to prevent significant
hypoventilation. Subsequent doses may need to be decreased by
25-50%. Initial drowsiness will diminish
with continued use. Patient Teaching:
Instruct patient how and when to ask for pain
medication. Prazosin HCL Cap
(Minipress)
Classification Therapeutic:
antihypertensi
Actions: • Lowering of
BP.
2mg cap PO bid
Dizziness, headache, weakness, first-dose
orthostatic
Contraindication: hypersensitivity
Nursing intervention: Monitor BP and pulse
frequently during initial
Congestive Heart Failure 22
0900, 2100
ves Pharmacologi
c: peripherally acting
antiadrenergics
Mechanism of action: •
Dilates both arteries and veins by
blocking postsynaptic
alpha1-adrenergic receptors.
• Decreases contractions
in smooth muscle of prostatic
capsule.
• Decreased cardiac preload
and afterload. • Decreased
symptoms of prostatic hyperplasia
(urinary urgency,
urinary hesitancy, nocturia)
Indication:
PTSD, Blood pressure and prostate higher
dose
hypotension, palpitations
Drug interactions: alcohol,
antihypertensives, nitrates, NSAIDs
dosage adjustment and periodically throughout
therapy. Report significant changes.
Patient teaching: Instruct patient to take
medication at the same time each day. Take
missed doses as soon as remembered. If not remembered until next
day, omit; do not double doses. Instruct patient
and family on proper technique for BP monitoring. Advise them
to check BP at least weekly and to report
significant changes.
Albuterol 0.5%
nebulizer (Accuneb, ProAir HFA,
Proventil HFA, Ventolin HFA,
Ventolin Diskus, VoSpire ER)
0700, 1300,
Therapeutic:
bronchodilators Pharmacologi
c: adrenergics
Mechanism of Action: Binds to beta2-
adrenergic
Action:
Bronchodilation
Indication:
2.5mg/
.5vial, 1 ampule neb RT tid
Nervousness,
restlessness, tremor, paradoxical brochospasm, chest
pain, palpitations, anaphylactic shock
Contraindications:
Hypersensitivity to adrenergic amines Interactions:
Drug-Drug: adrenergic agents,
MAO inhibitors, beta blockers, potassium-losing diuretics
Drug-Natural Products:
Nursing
interventions: Assess lung sounds, BP, and pulse. Monitor
pulmonary function tests before initiating
therapy. Observe for paradoxical bronchospasm.
Patient
Congestive Heart Failure 23
1900 receptors in airway
smooth muscle,
leading to activation of adenyl
cyclase and increased
levels of cyclic-3´, 5´-adenosine
monophosphate (cAMP).
Increases in cAMP activate
kinases, which inhibit
the phosphorylation of myosin
and decrease intracellular
calcium. Decreased intracellular
calcium relaxes
smooth muscle airways.
• Relaxation
guarana, tea, coffee
teaching: Instruct patient to take as directed and to
contact health care professional if sob is not
relieved. Educate patient to prime unit with 4 sprays before use.
Congestive Heart Failure 24
of airway smooth
muscle with subsequent
bronchodilation. • Relatively
selective for beta2
(pulmonary ) receptors.
Aspirin
Acetylsalicylic acid, Acuprin,
ASA, Aspergum, Aspir-Low, Aspirtab, Bayer,
Easprin, ecotrin, Entophen,
Halfprin, Healthprin, Zorprin
0900
Therapeutic:
antipyretics, nonopioid
analgesics Pharmacologic: salicylates
Mechanism of
Action: Produce analgesia and
reduce inflammation
and fever by inhibiting the production of
prostaglandins.Decreases
platelet aggregation.
Action:
Analgesia. Reduction of
inflammation. Reduction of fever.
Decreased incidence of
transient ischemic attacks and MI.
Indication:
prevent MI and strokes
81mg tab
PO daily
Dyspepsia, epigastric
distress, nausea, GI bleeding, allergic
reactions (anaphylaxis and laryngeal edema included)
Contraindication:
Hypersensitivity to aspirin or other
salicylates, bleeding disorders or thrombocytopenia
Drug interactions:
warfarin, heparin, heparin-like agents, thrombolytic agents,
dipyridamole, ticlopidine, clopidogrel,
tirofiban, eptifibatide, ibuprofem, cefoperazone, cefotetan,
valprioc acid, penicillins, phenytoin, methotrexate,
valproic acid, oral hypoglycemic agents, sulfonamides, urinary
acidification, alkalization
Nursing Intervention:
Patients who have asthma, allergies, and
nasal polyps or who are allergic to tartrazine are at an increased risk for
developing hypersensitivity
reactions. Assess pain and limitation of movement; note type,
location, and intensity before and at the peak
(see Time/Action Profile) after administration.
Assess fever and note associated signs
(diaphoresis, tachycardia, malaise, chills).
Congestive Heart Failure 25
of the urine, antacids, diuretics, ACE
inhibitors, NSAIDs Drug-natural Products:
arnica, chamomile, clove feverfew, garlic, ginger, ginkgo, panax ginseng,
Food Interactions: foods
capable of acidifying the urine
Patient teaching: Teach patient to avoid
concurrent use of alcohol with this medication to
minimize possible gastric irritation; 3 or more glasses of alcohol per
day may increase risk of GI bleeding. Teach
patient to avoid taking concurrently with acetaminophen or
NSAIDs for more than a few days, unless directed
by health care professional to prevent analgesic nephropathy.
Calcium citrate
tab (Cal-Citrate 250, Citrical, Citrical
Liquitab)
0900, 2100
Classification
Therapeutic: mineral and electrolyte
replacements/supplements
Mechanism of action:
Essential for nervous,
muscular, and skeletal systems.
• Maintain
Action:
Replacement of calcium in deficiency
states. Control of
hyperphosphatemia in end-stage renal
disease without promoting
aluminum absorption.
Indication:
400mg tab
PO bid
Arrhythmias and
constipation
Contraindications:
hypercalcemia, renal calculi, and ventricular fibrillation.
Drug interactions:
digoxin, antacids, tetracyclines, fluoroquinolones,
phenytoin, iron salts, calcium channel
blockers, etidronate, risedronate, atenolol, diuretics (thiazide),
sodium polysterene
Nursing interventions:
Observe patient closely for symptoms of hypocalcemia
(paresthesia, muscle twitching, laryngospasm,
colic, cardiac arrhythmias, Chvostek's or Trousseau's sign).
Notify physician or other health care professional
if these occur. Protect symptomatic patients by elevating and padding
siderails and keeping bed
Congestive Heart Failure 26
cell membrane
and capillary permeability.
• Act as an activator in the
transmission of nerve
impulses and contraction of cardiac,
skeletal, and smooth
muscle. • Essential for bone
formation and blood
coagulation. • Treatment of hyperphospha
temia in end-stage renal
disease.
Treatment and prevention of
hypocalcemia.
sulfonate
Drug-food: cereals, spinach, rhubarb
in low position.
Patient teaching: Instruct patients on a regular
schedule to take missed doses as soon as possible, then go back to
regular schedule.
Carvedilol tab
(Coreg, Coreg CR)
0900, 2100
Classification
Therapeutic: antihypertensi
ves Pharmacologic: beta
blockers
Actions: •
Decreased heart rate and BP.
• Improved cardiac output, slowing of the
progression of
3.125mg
tab PO bid
Dizziness, fatigue,
weakness, diarrhea, erectile dysfunction,
hyperglycemia, bradycardia, HF, pulmonary edema,
Stevens-Johnson
Contraindications:
History of serious hypersensitivity reaction
(Stevens-Johnson syndrome, angioedema, anaphylaxis);
• Pulmonary edema;
Nursing interventions: •
Monitor BP and pulse frequently during dose
adjustment period and periodically during therapy. Assess for
orthostatic hypotension
Congestive Heart Failure 27
Mechanism of
action: Blocks stimulation of
beta1(myocardial) and beta2 (pulmonary,
vascular, and uterine)-
adrenergic receptor sites. • Also has
alpha1 blocking
activity, which may result in
orthostatic hypotension.
HF and decreased risk
of death.
Indication: Heart failure progression
syndrome, toxic epidermal becrolysis,
anaphylaxis, angioedema
• Cardiogenic shock; • Bradycardia, heart
block or sick sinus syndrome (unless a
pacemaker is in place); • Uncompensated HF requiring IV inotropic
agents (wean before starting carvedilol);
• Severe hepatic impairment; • Asthma or other
bronchospastic disorders.
Drug interactions: general anesthetics, IV phenytoin, diltiazem,
verapamil, digoxin, amiodarone, fluconazole,
antihypertensives, alcohol, nitrates, clonidine, thyroid
preparations, nsulins, oral hypoglycemic
agents, theophylline, dopamine, dobutamine, MAO inhibitor,
cimetidine, NSAIDs, rifampin, digoxin,
cyclosporine.
when assisting patient up from supine position.
• Monitor intake and output ratios and daily
weight. Assess patient routinely for evidence of fluid overload
(peripheral edema, dyspnea, rales/crackles,
fatigue, weight gain, jugular venous distention). Patients may
experience worsening of symptoms during
initiation of therapy for HF.
Patient teaching: Instruct patient to take
medication as directed, at the same time each day, even if feeling well. Do
not skip or double up on missed doses. Take
missed doses as soon as possible up to 4 hr before next dose. Abrupt
withdrawal may precipitate life-
threatening arrhythmias, hypertension, or myocardial ischemia.
Teach patient and family
Congestive Heart Failure 28
how to check pulse and BP. Instruct them to
check pulse daily and BP biweekly. Advise patient
to hold dose and contact health care professional if pulse is <50 bpm or
BP changes significantly. Folic Acid tab
(folate, Folvite, vitamin B)
0900
Classification
Therapeutic: antianemics, vitamins
Pharmacologic: water
soluble vitamins
Action: Required for
protein synthesis and red blood cell
function. Stimulates the
production of red blood cells, white
blood cells, and platelets.
Action:
Restoration and maintenance of normal
hematopoiesis.
Indication: For vitamin deficiency
1mg tab
PO daily
Derm: rash.
CNS: irritability, difficulty sleeping, malaise, confusion.
Misc: fever.
Contraindication:
Uncorrected pernicious, aplastic, or normocytic anemias (neurologic
damage will progress despite correction of
hematologic abnormalities)
Drug interactions: pyrimethamine,
methotrexate, trimethoprim, triamterene,
sulfonamides, sulfasalazine, antacids,
cholestyramine, estrogens, phenytoin, phenobarbital,
primidone, carbamazepine,
corticosteroids
Nursing intervention:
Assess patient for signs of megaloblastic anemia (fatigue, weakness,
dyspnea) before and periodically throughout
therapy. Patient teaching: Instruct
patient to notify health care professional if rash
occurs, which may indicate hypersensitivity.
Furosemide inj. Solution
(Lasix)
Classificatio
n: loop
diuretics
Action: Diuresis
and subsequent
40mg/4ml IVP q12h
Erythema multiforme, stevens-johnson
syndrome, toxic
Contraindications:
hypersensitivity, cross-
sensitivity with thiazides
Nursing Interventions:
Assess fluid
status: document and
Congestive Heart Failure 29
0900, 2100
Action:
inhibits reabsorption
of sodium and chloride, increases
renal excretion of
water, sodium, chloride,
magnesium, potassium,
and calcium.
mobilization of excess fluid,
decreased BP
Indication: Excess fluid
epidermal necrolysis dehydration,
hypocalcemia, hypochloremia,
hypokalemia, hypomagnesemia, hyponatremia,
hypovolemia, metabolic alkalosis
and sulfonamides, hepatic coma or anuria,
alcohol intolerance Interactions:
antihypertensives, nitrates, or alcohol, other diuretics, amphotericin
B, stimulant laxatives, corticosteroids, lithium,
cisplatin, NSAIDs, methotrexate, sucralfate, cholestyramine,
colestipol, salicylate, cyclosporine.
monitor fluids (I/O). Monitor BP and
pulse. Assess patient for allergy to sulfonamides,
tinnitus and hearing loss, and skin rash. monitor electrolytes, renal and
hepatic function, serum glucose, and uric acid
levels. Patient
teaching: Instruct
patient to change positions slowly to
minimize orthostatic hypotension, teach patient S/S to report to
the health care provider such as rash, muscle
weakness, cramps, nausea, dizziness, numbness, or tingling of
extremities occurs. Teach patients to
continue taking medication even if feeling better and teach
patient about additional therapies for
hypertension.
Furosemide tab
(Lasix)
Classificatio
n: loop
Action: Diuresis
and subsequent
40mg tab
PO q12h
Erythema multiforme,
stevens-johnson
Contraindications:
hypersensitivity, cross-
Nursing Interventions:
Assess fluid
Congestive Heart Failure 30
0900, 2100
diuretics
Action:
inhibits
reabsorption of sodium and chloride,
increases renal
excretion of water, sodium,
chloride, magnesium,
potassium, and calcium.
mobilization of excess fluid,
decreased BP
Indication: Excess fluid
syndrome, toxic epidermal necrolysis
dehydration, hypocalcemia,
hypochloremia, hypokalemia, hypomagnesemia,
hyponatremia, hypovolemia,
metabolic alkalosis
sensitivity with thiazides and sulfonamides,
hepatic coma or anuria, alcohol intolerance
Interactions:
antihypertensives, nitrates, or alcohol, other
diuretics, amphotericin B, stimulant laxatives,
corticosteroids, lithium, cisplatin, NSAIDs, methotrexate, sucralfate,
cholestyramine, colestipol, salicylate,
cyclosporine.
status: document and monitor fluids
(I/O). Monitor BP and pulse. Assess patient for
allergy to sulfonamides, tinnitus and hearing loss, and skin rash. monitor
electrolytes, renal and hepatic function, serum
glucose, and uric acid levels. Patient
teaching: Instruct patient to change
positions slowly to minimize orthostatic hypotension, teach
patient S/S to report to the health care provider
such as rash, muscle weakness, cramps, nausea, dizziness,
numbness, or tingling of extremities
occurs. Teach patients to continue taking medication even if
feeling better and teach patient about additional
therapies for hypertension.
Congestive Heart Failure 31
Heparin inj
0700, 1500, 2300
Classificatio
n: anticoagul
ant, antithromboti
cs Action: prevention of
thrombus formation and
extension of existing thrombi.
Indication: Blood thinning
5,000 units/ml
SQ tid
Bleeding, Heparin-induced
thrombocytopenia (with or without
thrombosis), anemia
Contraindications:
hypersensitivity,
uncontrolled bleeding, severe
thrombocytopenia, open wounds, benzyl alcohol products in premature
infants Interactions:
Drug-drug: drugs that affect platelet functions including NSAIDs,
aspirin. Drugs that cause hypoprothrombinemia,
concurrent use of thrombolytics, warfarin Drug-natural products:
arnica, anise, chamomile, clove, dong quai, fever
few, garlic, ginger, and panax ginseng
Nursing Interventions:
Assess for signs of
bleeding and hemorrhage, assess
patient for evidence of additional or increased thrombosis, observe
injection sites for hematomas, ecchymosis,
or inflammation. Monitor aPTT and hematocrit,
platelet count Patient teaching: Teach
patient to report symptoms of unusal bleeding or
burising. Instruct patient not to take medications
containing aspirin or NSAIDs. Teach patient to use a soft toothbrush
and electric razor.
Isosorbide dinitrate tab (Dilatrate-SR,
Isordil)
0900, 1500, 2100
Classification Therapeutic: antianginals
Pharmacologic: nitrates
Mechanism of action:
Produce
Action: Relief and prevention of anginal
attacks.
Indication: Chest pain
20mg tab PO tid
Dizziness, hypotension, tachycardia
Contraindications: • Hypersensitivity; • Concurrent use of
sildenafil, vardenafil, or tadalafil.
Drug interactions: sildenafil, tadalafil,
vardenafil alcohol, beta
Nursing Interventions: Assess location, duration, intensity, and
precipitating factors of anginal pain.
• Monitor BP and pulse routinely during period of dosage adjustment.
Congestive Heart Failure 32
vasodilation (venous
greater than arterial).
• Decrease left ventricular end-diastolic
pressure and left
ventricular end-diastolic volume
(preload). Net effect is
reduced myocardial oxygen
consumption. • Increase
coronary blood flow by dilating
coronary arteries and
improving collateral flow to ischemic
regions.
blockers, calcium channel blockers, and
phenothiazines
Patient teaching: Instruct patient to take
medication as directed, even if feeling better.
Take missed doses as soon as remembered; doses of isosorbide
dinitrate should be taken at least 2 hr apart (6 hr
with extended-release preparations); daily doses of isosorbide
mononitrate should be taken 7 hr apart. Do not
double doses. Do not discontinue abruptly.
Thiamine tab
(Vitamin B1) 0900
Classification
Therapeutic: vitamins Pharmacologi
c: water
Action:
Replacement in deficiency states.
100mg tab
PO daily
Vascular collapse and
agioedema
Contraindication: •
Hypersensitivity; • Known alcohol intolerance or bisulfite
hypersensitivity (elixir
Nursing Intervention:
Assess for signs and symptoms of thiamine deficiency (anorexia, GI
distress, irritability,
Congestive Heart Failure 33
soluble vitamins
Mechanism of
action: Required for carbohydrate
metabolism.
Indication: vitamin
deficiency
only). Drug intervention: None
signficant
palpitations, tachycardia, edema, paresthesia,
muscle weakness and pain, depression,
memory loss, confusion, psychosis, visual disturbances, elevated
serum pyruvic acid levels).
• Assess patient's nutritional status (diet, weight) prior to and
throughout therapy.
Patient teaching: Teach patient that foods high in thiamine include cereals
(whole grain and enriched), meats
(especially pork), and fresh vegetables; loss is variable during cooking.
Hydralazine tab (Hydralazine)
0900, 1500, 2100
Classification Therapeutic:
antihypertensives Pharmacologi
c: vasodilators
Mechanism of action: Direct-acting
peripheral
Action: Lowering of BP
in hypertensive patients and decreased
afterload in patients with
HF. Indication:
Blood pressure
50mg tab PO tid
Tachycardia, drug-induced lupus
syndrome, sodium retention
Contraindication: Hypersensitivity;
• Some products contain tartrazine and should be avoided in patients with
known intolerance.
Drug interactions: alcohol, antihypertensives,
nitrates, MAO inhibitors,
Nursing interventions: Monitor BP and pulse
frequently during initial dose adjustment and periodically during
therapy. About 50-65% of Caucasians,
Black, South Indians, and Mexicans are slow
acetylators at risk for toxicity, while 80-90%
Congestive Heart Failure 34
arteriolar vasodilator.
epinephrine, NSAIDs, beta blockers,
metoprolol, propranolol
of Eskimos, Japanese, and Chinese are rapid
acetylators at risk for decreased levels and
treatment failure. Patient teaching: nstruct
patient to take medication at the same
time each day; last dose of the day should be taken at bedtime. Take
missed doses as soon as remembered; do not
double doses. If more than 2 doses in a row are missed, consult health
care professional. Must be discontinued
gradually to avoid sudden increase in BP. Hydralazine controls but
does not cure hypertension.
Magnesium Sulfate inj (Magnesium
Sulfate)
1000 (one time)
Classification Therapeutic: mineral and
electrolyte replacements/
supplements Pharmacologic:
minerals/elect
Action: Replacement in deficiency
states.
Indication: Magnesium Deficiency
2gm/50ml IVPB one infusion
over 120 minutes
diarrhea Contraindications: Hypermagnesemia; • Hypocalcemia;
• Anuria; • Heart block;
Drug interactions: calcium channel blockers
and neuromuscular
Nursing intervention: Monitor pulse, BP, respirations, and ECG
frequently throughout administration of
parenteral magnesium sulfate. Respirations should be at least 16/min
before each dose.
Congestive Heart Failure 35
rolytes
Mechanism of action:
Essential for the activity of many
enzymes. • Plays an
important role in neurotransmis
sion and muscular
excitability.
blocking agents Patient teaching: Teach
purpose of medication to patient and family
Congestive Heart Failure
36
Appendix B
Lab Data
(per Level) Description of Lab Test Normal
Value
Admissi
on
Result
10/16/14
Recent
Result
10/21/14
Recent
Result
10/22/14
Pathophysiology explanation of
abnormal lab value, including trends
and correlation with disease process
WBC
--Measurement of total number of leukocytes;
--Provide clues to etiology; --WBC differential – determination of whether each
kind of WBC is present in proper proportion
4000-
11,000 /µL (4.0-11.0 x
10^3/µL)
4.3 4.1 Not Accessed
Neutrophils
(ANC)
Primary phagocytic cells
involved in acute inflammation
50-70% of WBC differenti
al (0.5-0.7 SI
units)
56.9 51.9 Not
Assessed
Lymphocyte
Form the basis of cellular and
humoral immune responses (B and T cells); transiently circulate in blood & reside in lymphoid
tissues
20-40% of WBC
differential (0.2 –
0.4 SI units)
18.2 17.8 Not Assessed
<20% -- corticosteroid therapy; whole body irradiation
Monocytes
Potent phagocytic cells; only present in blood for short amount of time before migrating
to tissues to become macrophages
4-8% of
WBC differenti
al (0.04-0.08 SI units)
19 22.9 Not
Assessed
>8% -- chronic inflammatory disorders;
acute infections
Hemoglobin
(Hgb)
Measurement of gas-carrying
ability of RBC
Females: 11.7-16.0
g/dL Males:
12.2 11.1 Not
Assessed
Hemodilation (excess fluid volume;
Congestive Heart Failure
37
13.2-17.3 g/dL
Hematocrit (Hct)
Measurement of packed cell
volume of RBCs expressed as percentage of total blood
volume
Females:
35-47% Males:
39-50%
37.8 36.8 Not Assessed
Increase and decreases are the results of the same conditions that increase/decrease hemoglobin (Hgb)
Platelets
# of platelets available to maintain platelet clotting
function (not a measure of quality)
150,000 –
400,000/ µL
116,000 101,000 Not
Assessed
<100,000/ µL (thrombocytopenia) – bleeding, spontaneous hemorrhaging
may occur
Serum Na Main extracellular electrolyte
determining blood volume
135-145
mEq/L 138 139 139
Serum K
Major intracellular electrolyte;
found in most body fluids; total K content is about 4000 mEq – serum K indicates ECF
concentration
3.5-5.0 mEq/L
4.4 4 4
Serum Cl
Anion that works as an
electrolyte to maintain body fluid and acid/base balances
96-106
mEq/L 92 95 94
<96 –respiratory acidosis
Serum CO2 Measure of the bicarbonate level 23-29 mEq/L
30 30 30
>29 – compensated respiratory acidosis,
breathing disorders
BUN
Blood urea nitrogen Used to detect renal problems Concentration of urea in blood is
regulated by rate which kidney excretes urea – reflects GFR and urine-concentrating capacity
6-20
mg/dL 25 20 23
Increases as GFR (glomerular filtration rate) decreases; rises in states of dehydration and acute and chronic renal
failure; varies as a result of altered protein intake and protein catabolism
Creatinine
More reliable than BUN as a determinant of renal function
Creatinine is end product of muscle and protein metabolism and is released at a constant rate
0.6-
1.1mg/dL 1.9 1.3 1.4
>1.1 - impaired renal function,
congestive heart failure
Congestive Heart Failure
38
Glucose
Fasting glucose test is the measurement of the level of sugar in the blood after not
eating or drinking for at least 8 hours
Fasting: 70-99
mg/dL
84 99 91
Ca Necessary ion for many fundamental metabolic processes
8.6-10.2 mg/dL
Not assessed
Not Assessed
10.1
Mg Major intracellular cation; Small amount is in serum (1%).
1.5-2.5 mg/dL
Not assessed
Not Assessed
1.3 <1.5 –severe malabsorption; low levels cause renal conservation of Mg; renal
tubular dysfunction, uses of diuretics
Prothrombin Time (PT)
---Determination of prothrombin activity
---Generally ordered in relation to a bleeding problem to
determine the effects of anticoagulant such as warfarin
11-16 sec.
16.2 Not Assessed
Not Assessed
>16 sec – Warfarin therapy; deficiency of factors I, II, V, VII, & X; vitamin K deficiency; liver disease
International Normalized Ratio (INR)
---Standardized system of
reporting PT based on a reference calibration model and
calculated by comparing the patient’s PT with a control value ---Generally ordered in relation
to a bleeding problem to determine the effects of
anticoagulant such as warfarin
2-3 1.3 Not Assessed
Not Assessed
High levels indicate an issue in clotting factors seen in PT test;
Troponin
To assist in evaluating
myocardial muscle damage related to disorders such as myocardial infarction.
<0.5 ng/mL
(Negative)
<.01 Not Assessed
Not Assessed
Congestive Heart Failure
39
Appendix C
Tests
Purpose of Test
(For THIS patient)
Date of
Test
Test Results
Abdomen 3 or more views Abdominal distention 10/16/2014 Fluid in the abdomen, no obstruction observed Chest 2 views PA & LAT Pt shortness of breath 10/16/2014 Found pulmonary vascular congestion