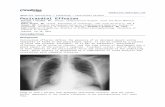
A Rare Case of Unilateral Pleural Effusion in a Pediatric ...
Case Study (CAP With Effusion
Transcript of Case Study (CAP With Effusion

P A T H O P H Y S I O L O G Y
Page 17
I. INTRODUCTION
This is a case of a 42-year-old woman who was diagnosed with Community
Acquired Pneumonia with effusion at the Right Lung.
Community-acquired pneumonia (CAP) is a disease in which individuals who
have not recently been hospitalized develop an infection of the lungs (pneumonia). CAP
is a common illness and can affect people of all ages and often causes problems like
difficulty in breathing, fever, chest pains, and a cough. CAP occurs because the areas
of the lung which absorb oxygen (alveoli) from the atmosphere become filled with fluid
and cannot work effectively.
Community acquired pneumonia occurs throughout the world and is a leading
cause of illness and death. Causes of CAP include bacteria, viruses, fungi, and
parasites. CAP can be diagnosed by symptoms and physical examination alone, though
x-rays, examination of the sputum, and other tests are often used. Individuals with The
kind of disease sometimes require treatment in a hospital and are primarily treated with
antibiotic medication.
Community-acquired pneumonia develops in people with limited or no contact
with medical institutions or settings. The most commonly identified pathogens are
Streptococcus pneumoniae, Haemophilus influenzae, and atypical organisms (ie,
Chlamydia pneumoniae, Mycoplasma pneumoniae, Legionella sp). Symptoms and
signs are fever, cough, pleuritic chest pain, dyspnea, tachypnea, and tachycardia.

P A T H O P H Y S I O L O G Y
Page 17
Diagnosis is based on clinical presentation and chest x-ray. Treatment is with
empirically chosen antibiotics. Prognosis is excellent for relatively young or healthy
patients, but much pneumonia, especially when caused by S. pneumoniae or influenza
virus, are fatal in older, sicker patients.
Etiology
Many organisms cause community-acquired pneumonia, including bacteria,
viruses, and fungi. Pathogens vary by patient age and other factors 1: Pneumonia:
Community-Acquired Pneumonia in Children 2: Pneumonia: Community-Acquired
Pneumonia in Adults but the relative importance of each as a cause of community-
acquired pneumonia is uncertain, because most patients do not undergo thorough
testing, and because even with testing, specific agents are identified in < 50% of cases.
S. pneumoniae, H. influenzae, C. pneumoniae, and M. pneumoniae are the most
common bacterial causes. Pneumonia caused by chlamydia and mycoplasma are often
clinically indistinguishable from pneumonias with other causes. Common viral agents
include respiratory syncytial virus (RSV), adenovirus, influenza viruses,
metapneumovirus, and parainfluenza viruses. Bacterial superinfection can make
distinguishing viral from bacterial infection difficult.
C. pneumoniae accounts for 2 to 5% of community-acquired pneumonia and is
the 2nd most common cause of lung infections in healthy people aged 5 to 35 yr. C.
pneumoniae is commonly responsible for outbreaks of respiratory infection within
families, in college dormitories, and in military training camps. It causes a relatively
benign form of pneumonia that infrequently requires hospitalization. Chlamydia psittaci
pneumonia (psittacosis) is rare and occurs in patients who own or are often exposed to
birds.
A host of other organisms cause lung infection in immunocompetent patients,
although the term community-acquired pneumonia is usually reserved for the more
common bacterial and viral etiologies.
Q fever, tularemia, anthrax, and plague are uncommon bacterial syndromes in
which pneumonia may be a prominent feature; the latter three should raise the
suspicion of bioterrorism.
Adenovirus, Epstein-Barr virus, and coxsackievirus are common viruses that
rarely cause pneumonia. Varicella virus and hantavirus cause lung infection as part of

P A T H O P H Y S I O L O G Y
Page 17
adult chickenpox and hantavirus pulmonary syndrome; a coronavirus causes severe
acute respiratory syndrome.
Common fungal pathogens include Histoplasma capsulatum (histoplasmosis)
and Coccidioides immitis (coccidioidomycosis). Less common fungi include
Blastomyces dermatitidis (blastomycosis) and Paracoccidioides braziliensis
(paracoccidioidomycosis). Pneumocystis jiroveci commonly causes pneumonia in
patients who have HIV infection or are immunosuppressed.
Parasites causing lung infection in developed countries include Toxocara canis
or T. catis (visceral larva migrans), Dirofilaria immitis (dirofilariasis), and Paragonimus
westermani (paragonimiasis). (For a discussion of pulmonary TB or of specific
microorganisms, see Mycobacteria.)
Symptoms include malaise, cough, dyspnea, and chest pain. Cough typically is
productive in older children and adults and dry in infants, young children, and the
elderly. Dyspnea usually is mild and exertional and is rarely present at rest. Chest pain
is pleuritic and is adjacent to the infected area. Pneumonia may manifest as upper
abdominal pain when lower lobe infection irritates the diaphragm. Symptoms become
variable at the extremes of age; infection in infants may manifest as nonspecific
irritability and restlessness; in the elderly, as confusion and obtundation.
Signs include fever, tachypnea, tachycardia, crackles, bronchial breath sounds,
egophony, and dullness to percussion. Signs of pleural effusion may also be present
(see Mediastinal and Pleural Disorders: Symptoms and Signs). Nasal flaring, use of
accessory muscles, and cyanosis are common in infants. Fever is frequently absent in
the elderly.
Symptoms and signs were previously thought to differ by type of pathogen, but
presentations overlap considerably. In addition, no single symptom or sign is sensitive
or specific enough to predict the organism. Symptoms are even similar for noninfective
lung diseases such as pulmonary embolism, pulmonary malignancy, and other
inflammatory lung diseases.
Diagnosis
Chest x-ray
Consideration of pulmonary embolism
Sometimes identification of pathogen

P A T H O P H Y S I O L O G Y
Page 17
Diagnosis is suspected on the basis of clinical presentation and is confirmed by
chest x-ray (see Table 3: Pneumonia: Probability of Pneumonia Given Chest X-ray
Infiltrate ). The most serious condition misdiagnosed as pneumonia is pulmonary
embolism, which may be more likely in patients with minimal sputum production, no
accompanying URI or systemic symptoms, and risk factors for thromboembolism (see
Table 1: Pulmonary Embolism (PE): Risk Factors for Deep Venous Thrombosis and
Pulmonary Embolism).
Chest x-ray almost always demonstrates some degree of infiltrate; rarely, an
infiltrate is absent in the first 24 to 48 h of illness. In general, no specific findings
distinguish one type of infection from another, although multilobar infiltrates suggest S.
pneumoniae or Legionella pneumophila infection and interstitial pneumonia suggests
viral or mycoplasmal etiology.
Hospitalized patients should undergo WBC count and electrolytes, BUN, and
creatinine testing to classify risk and hydration status. Two sets of blood cultures are
often obtained to detect pneumococcal bacteremia and sepsis, because about 12% of
all patients hospitalized with pneumonia have bacteremia; S. pneumoniae accounts for 2⁄3 of these cases. Whether the results of blood cultures alter therapy commonly enough
to warrant the expense is under study. Pulse oximetry or ABG should also be done.
Pathogens: Attempts to identify a pathogen are not routinely indicated;
exceptions may be made for critically ill patients, patients in whom a drug-resistant or
unusual organism is suspected (eg, TB, P. jiroveci), and patients who are deteriorating
or not responding to treatment within 72 h.
The use of Gram stain and culture of sputum for diagnosis is of uncertain benefit,
because specimens often are contaminated and because overall diagnostic yield is low.
Samples can be obtained noninvasively by simple expectoration or after hypertonic
saline nebulization for those unable to produce sputum. Alternatively, patients can
undergo bronchoscopy or endotracheal suctioning, either of which can be easily done
through an endotracheal tube in mechanically ventilated patients. Testing should
include mycobacterial and fungal stains and cultures in patients whose condition is
deteriorating and in those unresponsive to broad-spectrum antibiotics.
Additional tests are indicated in some circumstances. Patients at risk of
Legionella pneumonia (eg, patients who smoke, have chronic pulmonary disease, are >
40, receive chemotherapy, or take immunosuppressants for organ transplantation)
should undergo testing for urinary Legionella antigen, which remains present long after
treatment is initiated, but the test detects only L. pneumophila serogroup 1 (70% of

P A T H O P H Y S I O L O G Y
Page 17
cases). A 4-fold rise in antibody titers to ≥ 1:128 (or a single titer of ≥ 1:256 in a
convalescent patient) is also considered diagnostic. These tests are specific (95 to
100%) but are not very sensitive (40 to 60%); thus, a positive test indicates infection,
but a negative test does not exclude it.
Infants and young children with possible RSV infection should undergo rapid
antigen testing of specimens obtained with nasal or throat swabs. No other tests for viral
pneumonias are done; viral culture and serologic tests are rarely clinically warranted.
PCR testing for mycoplasma and chlamydia species, although not widely available,
holds promise as a highly sensitive and specific rapid diagnostic test and is likely to play
a greater role as PCR technologies are refined.
Reason for choosing Pneumonia as our case
This case study aims to identify patient’s health needs and problems in order to
identify goals to promote the general health of the patient by providing proper
intervention through the application of nursing process.
We have chosen this case study in order to identify and determine the general
health problems and needs of the patient with an admitting diagnosis of Community
Acquired Pneumonia. This study also intends to help patient as well as its significant
others to promote health and medical understanding of such condition through the
application of the nursing theories and nursing skills.
Our inadequate knowledge on Community Acquired Pneumonia motivated us to
study the case suffered by most of my patients in medical ward. I wanted to have
enough knowledge regarding this condition so that I could apply and handle such this
kind of condition correctly.

P A T H O P H Y S I O L O G Y
Page 17
II. CLIENT’S PROFILE
A. Socio-demographic Data
Patient Y is a 42-year-old, female, single, a Roman Catholic from Lam-an, Ozamis
City, Misamis Occidental. The patient was admitted for the first time at Northern
Mindanao Medical Center last June 24, 2010; 3:00 pm. She arrived at the hospital,
awake and conscious with chief complaints of dyspnea and persistent cough. She was
then diagnosed with Community Acquired Pneumonia with Pleural Effusion. She
currently weighs 41 kilograms from the previous weight of 50 kilograms and she is 5’3
tall. She was hospitalized last May 5, 2010 at Mayor Hilario Ramos Regional Training
and Teaching Hospital due to appendicitis and undergone appendectomy.
The patient usually uses over-the-counter drugs to manage health problems like
fever and headache. Patient denied the use of tobacco, alcohol or illicit drug use, drinks
coffee, cola or tea about 4-5 times a week and can consume 1½ glass. She has no
known food allergies but patient is allergic to Myrin P-forte.
B. Vital Signs
The patient’s vital signs are so important, since it provides a baseline data in
determining what are the alterations in body function. Any change from normal is
considered to be an indication of the person’s state of health and provides clues to the
physiological functioning of the body.
The patient had the following vital signs: blood pressure: 110/70 mmHg, pulse
rate: 83 bpm, respiratory rate: 26 cpm, temperature: 38ºC.
C. History of Present Illness
A month PTA, she began to have an undocumented fever, temporarily relieved
by paracetamol 500 mg, associated with cough, body malaise with poor appetite. No
consultation done. No medication taken. 8 days PTA, she began to have dyspnea which
prompted consultation and subsequent admission at Mayor Hilario Ramos Training and
Teaching hospital where she was diagnosed with Polycythemia vera and Essential
thrombocytosis. She was referred to Celo Hospital because of incidence of decrease
BP.
She was brought to and admitted at Maria Reyna Hospital last June 6, 2010.
There was onset of pleural effusion and R thoracentesis was done 3 hours after
admission. 2 days later, CTT was done at R hemithorax.

P A T H O P H Y S I O L O G Y
Page 17
D. Health Patterns Assessment
1. Health Perception – Health Management Pattern (pre-hospitalization)
Patient X doesn’t have regular consultations to physicians if she doesn’t
feel any deviation of his health status. She doesn’t drink any alcoholic
beverages or smoke and has no known food and drug allergies. Patient X is a
worker from Misamis Occidental Hospital where she works as a secretary.
She is the only person who works in the family.
2. Nutrition
Patient X is not eating well and the appetite is poor. She wasn’t
experiencing nausea or vomiting either. She has no discomforts in terms of
eating. But because of her disease condition, she was not eating well. She
has rapid weight loss from 50 kg to 41 kg within a short span of time (1
month). The client has Chest Thoracostomy Tube draining well at the right
mid-axillary line.
3. Elimination Pattern
Mrs. X ‘s stool as described by her as yellowish in color, defecates
everyday with no discomforts.
Urinates approximately 3-4 times a daywith 100-200 cc per urination.
Urine is slightly hazy in color but had no problem in control.
4. Activities of daily living (Pre-hospitalization)
The client is working as a secretary from one of the hospitals located at
Misamis Occidental. Her duty hours is from 8 am to 5pm. She works
extremely hard because her 2 sons are already in college and her husband
has no work.
a. Activity-Exercise Pattern (while confined)
Describe the patient’s functional abilities
a. Feeding: dependent
b. Bathing: dependent
c. Toileting: dependent
d. Bed mobility: dependent
e. Dressing: dependent
f. Grooming: dependent
g. General mobility: dependent

P A T H O P H Y S I O L O G Y
Page 17
The patient need assistance in doing Range of Motion, thus, it
requires assistance coming from the significant others and/or the attending
nurse.
5. Cognitive- Perceptual Pattern
The patient can understand & speak visayan, Filipino and English
Patient is able to recall recent and past events and is oriented to time, person
and place. He has the ability to explain things clearly and can make simple
decisions. Patient can understand instructions as well as can perceive pain.
Though, pain is not verbalized by the client. She takes prescribed medicines,
takes vitamins daily and exercises regularly and used over-the-counter drugs
as well.
6. Sleep and Rest Pattern
She usually sleeps 8 hours/day. He has no history of sleep
disturbances.prayers as well as singing lullaby was one of the effective
methods to induce her sleeping.
7. Self Perception and Self-concept Pattern (self esteem, body image)
Patient believes she ca surpass these problems that she is going through
and she will go back to work so soon. She can maintain eye contact, able to
talk well, speech is audible
Emotional reaction to present condition: Check only:
Calm: √
Depressed: √
Anxious: √
Angry: ____________
Fearful: √
Irritable: √
Worried: √
The patient was generally calm and easy to have conversation with but
verbalized that she was worried and fearful because of th rcent condition that
she’s experiencing thus, it bothers her a lot every time there is procedure that
is being performed. In addition to that, she was anxious due to financial
constraints as well as she was depressed because with her condition she
cannot do activities of daily living independently and worse, she can’t work
and provide the needs of her family since she’s the only member in the family

P A T H O P H Y S I O L O G Y
Page 17
that has work.
8. Role and Relationship Pattern
Patient verbalized having good family relationship. She has been a
good mother to her sons and a good wife to his husband. She verbalized
having good relationship with friends.
9. Coping –Stress Tolerance Pattern
Patient was calm but sometimes irritable, anxious, worried and depressed.
She handles stress through sleeping.
10.Values-Belief Pattern
The patient is a Roman Catholic and believes no superstitions. She
together with her family attends mass every Sundays and both of the couples
were active in the Couples for Christ.
E. Physical Assessment
1. Neurological Assessment
Orientation Fully oriented
Appropriate behavior/communication Responsive and coherent
Level of Consciousness Conscious
Emotional State Anxious (sometimes)
2. Skin
General Color Pallor
Texture rough
Turgor elastic
Temperature Warm
Moisture Dry

P A T H O P H Y S I O L O G Y
Page 17
3. Head
Facial Movements Symmetrical
Fontanels Closed
Hair Fine
Scalp Clean
4. Eyes
Lids Symmetrical
Preorbital Region Intact/full
Conjunctiva Pale
Sclera Anicteric
Reaction to light R- Brisk
L- Brisk
Reaction to accommodation Uniform constriction / Convergence
Visual Acuity normal
Peripheral Vision normal
5. Nose
Septum Midline
Mucosa Pinkish
Patency Both patent
Gross Smell Normal/symmetrical
Sinuses Non-tender

P A T H O P H Y S I O L O G Y
Page 17
6. Ears
External Pinnae Normoset; Symmetrical
Tympanic Membrane Intact
Gross Hearing Normal
7. Mouth
Lips Pallor; cracked
Mucosa Pinkish
Tongue Midline
Teeth complete
Gums Pinkish
8. Neck
Trachea Midline
Thyroids Non-palpable
Others Normal ROM
9. Pharynx
Uvula Midline
Tonsils Not Inflamed
Posterior Pharynx Not Inflamed
Mucosa Pinkish

P A T H O P H Y S I O L O G Y
Page 17
10.Abdomen
General Normal
Configuration Symmetrical
Bowel Sounds Normoactive
Percussion Tympanitic
11.Back and Extremities
Range of Motion Normal
Muscle tone and strength Fair
Spine Midline
Gait normal
12.Cardiovascular Status
Precordial Area Flat
Point of Maximal Impulse (PMI) 5th ICS, midclavicular line
Heart Sounds Regular
Peripheral Pulses Regular
Capillary Refill 2 seconds
13.Respiratory Status
Breathing Pattern Irregular
Shape of Chest AP:L:2:1
Lung Expansion Symmetrical
Vocal/Tactile Fremitus Symmetrical
Percussion Resonant
Breath Sounds crackles
Cough Non-productive

P A T H O P H Y S I O L O G Y
Page 17
III. ANATOMY AND PHYSIOLOGY
The Lungs
The lungs lie within the thoracic cavity on either side of the heart. They are cone-
shaped, with the apex above the first rib and the base resting on the diaphragm. Each
lung is divided into superior and inferior lobes by an oblique fissure. The right lung is
further divided by a horizontal fissure, which creates a middle lobe. The right lung,
therefore, has three lobes; the left lobe has only two. In addition to these 5 lobes, which
are visible externally, each lung can be subdivided into about 10 smaller units
(bronchopulmonary segments). Each segment represents the portion of the lung that is
supplied by a specific tertiary bronchus. These segments are important surgically,
because a diseased segment can be resected without the need to remove the entire
lobe or lung. The two lungs are separated by a space (the mediastinum) where the
heart, aorta, vena cava, pulmonary vessels, esophagus, part of the trachea and bronchi,
and the thymus gland are located.
The lungs contain gas, blood, thin alveolar walls, and support structures. The
alveolar walls contain elastic and collagen fibers; these form a three-dimensional,
basket-like structure that allows the lung to inflate in all directions. These fibers are
capable of stretching when a pulling force is exerted on them from outside of the body
or when they are inflated from within. The elastic recoil helps in return the lungs to their
resting volume.

P A T H O P H Y S I O L O G Y
Page 17
The lung itself is covered with a membrane called the visceral (or pulmonary)
pleura. The visceral pleura are adjacent to the lining of the thoracic cavity which is
called the parietal pleura. Between the two membranes is a thin, serous fluid which acts
as a lubricant – reducing friction as the two membranes slide across one another when
the lungs expand and contract with respiration. The surface tension of the pleural fluid
also couples the visceral and parietal
pleura to one another, thus preventing the lungs from collapsing. Since the potential
exists for a space between the two membranes, this area is called the
pleural cavity or pleural space
The respiratory system is situated in the thorax, and is responsible for gaseous
exchange between the circulatory system and the outside world. The respiratory system
is divided into two systems namely the upper respiratory system, which composed of
the nasal cavity, pharynx and larnyx: and the lower respiratory system, which are the
trachea, bronchus, bronchioles and the alveoli.
ORGANS OF THE RESPIRATORY SYSTEM
THE LOWER RESPIRATORYTHE UPPER RESPIRATORY
NOSENASAL CAVITYPHARYNX
LARYNXBRONCHIAL TREELUNGS

P A T H O P H Y S I O L O G Y
Page 17
UPPER RESPIRATORY TRACT
Respiration is defined in two ways. In common usage, respiration refers to the
act of breathing, or inhaling and exhaling. Biologically speaking, respiration strictly
means the uptake of oxygen by an organism, its use in the tissue, and the release of
carbon dioxide. By either definition, respiration has two main functions: to supply the
cells of the body with the oxygen neede for metabolism and to remove carbon dioxide
formed a waste product from metabolism. This lesson describes the components of the
upper respiratory tract.
The upper respiratory tract conducts air from outside the body to the lower
respiratoty tract and helps to rotect the body from irritating substances. The upper
respiratory tract consists of the following stuctures:
The nasal cavity, the mouth, the pharynx, the epiglottis, the larynx, and the upper
trachea. The esophagus leads to the digestive tract.
One of the feature of both the upper and lower respiratory tracts is the
mucociliary apparatus that protects the airways from irritating substances, and is
composed of the celiated cells and mucus-producing glands in the nasal epithelium.
The glands produce a layer of mucus that traps unwanted particles as they are inhaled.
These are swept towards the posterior pharynx, from where they are either swallowed,
spat out, snezzed, or blown out.
Air passes through each of the structures of the upper respiratory tract on its way
to the lower respiratory tract. When a person at rest inhales, air enters via the nose and
mouth. The nasal cavity filters, warms, and humidifies air. The pharynx or throat is a
tube like structure that connects the back of the nasal cavity and mouth to the larynx, a
passageway for air, and the esophagus, a passageway for food. The pharynx servs as
a common hallway for the respitarory and digestive tracts, allowind both air and food to
pass through before entering the appropriate passageways.

P A T H O P H Y S I O L O G Y
Page 17
The pharynx contains a specialized flap-like structure called the epiglottis that
lower over the larynx to prevent the inhalation of food and liquid into the lower
respiratory tract.
The larynx or voice box, is a unique structure that contains the vocal cords, which
are essential for human speech. Small and triangular in shape, the larynx extends from
the epiglottis to the trachea.the larynx helps control movement of the epiglottis. In
addition, the larynx has specialized muscular folds that close it off and also prevent
food, foreighn objects, and secretions such as saliva from entering the lower respiratory
tract.
Mechanism of Breathing
To take a breath in, the external intercostal muscles contract, moving the ribcage
up and out. The diaphragmmoves down at the same time, creating negative pressure
within the thorax. The lungs are held to the thoracic wall by the plueral membranes and
so expand outward as well. This creates negative pressure within the lungs, and so air
rushes in through the upper and lower airways.
Expirations are mainly due to the natural elasticity of the lungs, which tend to
collapse if they are not held against the thoracic wall. This mechanism behind lung
collapse if there is air in the pleural space (pneumothorax)
How does the respiratory system work?
The respiratory system works with the body to help our body function correctly. One of
the things it does is it gives our cells/blood oxygen to take to the rest of our body.

P A T H O P H Y S I O L O G Y
Page 17
IV. PATHOPHYSIOLOGY
PREDISPOSING FACTORS:
Age (High Risk)(42 years old) Gender: female
PR ECIPITATING FACTORS:
Exposure to crowded placesExposure to stressLifestyleExposure to air pollutionHospitalizationOccupational status
Organisms may enter respiratory tract through inspiration, aspiration or inhalation
of oral secretions
Normal pulmonary defense mechanisms (cough reflex, mucociliary transport and
pulmonary macrophages) usually protects against infection. However, in susceptible
host, these defenses are either suppressed or overwhelmed by the invading organism.
Inflammation and edema of the lung parenchyma
Accumulation of cellular debris and exudates
The invading organism multiplies and releases damaging toxins
Lung tissue fills with exudates and fluid changing from an airless state to consolidated
state.

P A T H O P H Y S I O L O G Y
Page 17
Inflamed and fluid-filled alveolar sacs cannot exchange oxygen and
carbon dioxide effectively
Alveolar exudates tends to consolidate, so it is increasingly
difficult to expectorate
Kinin
Bradykinin
Vasodilation
Myocardial Depressan
t Factor
Clotting Cascade
Thromboxane release
Vascular Thrombi
Pulmonary Constriction
Increase Hydrostatic
Pressure
Increase Lymphatic
Flow
Fluid transudation into alveolus
Thickened alveolar
membrane impairing the exchange of Oxygen and
Carbon Dioxide
Fluid fills the intestitium
and alveolar spaces
Impaired Oxygen Diffusion
Decrease Cardiac Output
Dysrhythmias
Decrease Venous
Decrease BP
Fever
ChillsMalaise
Cough Pleuritic pain
Dyspnea Rales and cracles upon auscultation

P A T H O P H Y S I O L O G Y
Page 17
Interpretation:
The defense mechanisms of the lungs lose effectiveness and allow organism to
penetrate the sterile lower respiratory tract, where inflammation develops. Disruption of
the mechanical defenses of cough and ciliary’s motility leads to colonization of the lungs
and subsequent infection. Inflamed and fluid-filled alveolar sacs cannot exchange
oxygen and carbon dioxide effectively.
Systemic inflammation leads to release of cytokines and other chemical
mediators. The cytokines activate alveolar macrophages and recruit neutrophils to the
lungs, which in turn release leukotrienes, oxidants, platelet-activating factor, and
proteases. These substances damage capillary endothelium and alveolar epithelium,
disrupting the barriers between capillaries and airspaces. Edema fluid, protein, and
cellular debris flood the airspaces and interstitium, causing disruption of surfactant,
airspace collapse, and ventilation-perfusion mismatch leading to decreased lung
expansion and eventually may lead to acute respiratory failure if ;left untreated.

P A T H O P H Y S I O L O G Y
Page 17
VIII. DISCHARGE PLANNING/ HEALTH TEACHINGS
M-Medication to take
Instruct and explain to the patient that the medication is very important to
continue depending on the duration that the doctor ordered for the total recovery of the
patient.
E- Exercise
Encourage and instruct the patient to do proper breathing exercise.
T- Treatment
Advice the patient to relax in order to recover in his present condition. Instruct
the patient to minimize the exposure to an environment such as dusty and smoky area,
which airborne micro organism is present that can be a high risk factor that may cause
severity of his condition.
H- Health teaching
Encouraged and explain to the patient that it is important to maintain proper
hygiene to prevent further infection. Instruct the patient to take a bath every day and
explain that bathing early in the morning is not a factor or cause of having pneumonia.
Instruct to increase fluid intake of the patient.
O-Out Patient follow-up
Regular consultation to the physician can be factor for recovery and to assess
and monitor the patient’s condition
D-Diet
Diet as tolerated, meaning, the patient can eat everything until she can. Diet
plays a big role in fast recovery so that, instruct the patient to take nutritious food such
as green leafy vegetable and fruits.

P A T H O P H Y S I O L O G Y
Page 17
Additional Health Teaching
Home Care
Take your medication exactly as directed. Don’t skip doses. Continue taking your
antibiotics as directed until they are all gone—even if you start to feel better. This
will prevent the pneumonia from coming back.
Drink at least 8 glasses of water daily, unless directed otherwise. This helps to
loosen and thin secretions so that you can cough them up.
Use a cool-mist humidifier in your bedroom. Be sure to clean the humidifier daily.
Coughing up mucus is normal. Don’t use medications to suppress your cough
unless your cough is dry, painful, or interferes with your sleep. You may use an
expectorant if ordered by your doctor.
Learn percussion and postural drainage. These are techniques that can help you
cough up extra mucus. This extra mucus can trap germs in your lungs. Ask your
healthcare provider for instructions. Perform these techniques 3 times a day until
your lungs are clear.
Warm compresses or a moist heating pad on the lowest setting can be used to
relieve chest discomfort. Use several times a day for 15-20 minutes at a time. (To
prevent injuring your skin, be sure the temperature of the compress or heating
pad is warm, not hot.)
Get plenty of rest until your fever, shortness of breath, and chest pain go away.
Plan to get a flu shot every year.
Ask your doctor about a pneumonia vaccination.
Take the entire course of any prescribed medications. After a patient’s
temperature returns to normal, medication must be continued according to the
doctor’s instructions, otherwise the pneumonia may recur. Relapses can be far
more serious than the first attack.
Get plenty of rest. Adequate rest is important to maintain progress toward full
recovery and to avoid relapse.
Drink lots of fluids, especially water. Liquids will keep patient from
becoming dehydrated and help loosen mucus in the lungs.
Keep all of follow-up appointments. Even though the patient feels better, his
lungs may still be infected. It’s important to have the doctor monitor his
progress.
Encourage the guardians to wash patient’s hands. The hands come in
daily contact with germs that can cause pneumonia. These germs enter one’s

P A T H O P H Y S I O L O G Y
Page 17
body when he touch his eyes or rub his nose. Washing hands thoroughly and
often can help reduce the risk.
Tell guardians to avoid exposing the patient to an environment with too
much pollution (e.g. smoke). Smoking damages one’s lungs’ natural
defenses against respiratory infections.
Give supportive treatment. Proper diet and oxygen to increase oxygen in the
blood when needed.
Protect others from infection. Try to stay away from anyone with a
compromised immune system. When that isn’t possible, a person can help
protect others by wearing a face mask and always coughing into a tissue.
IX. RELATED LEARNING EXPERIENCE
Medical ward is the ward where were assigned for, for the 4 weeks duty, we have
encountered several restrain with regards to the implementation. It was not easy that we
are dealing with our lives. But we did not loss hope because it’s our responsibility to
care ant to address the patients need.

P A T H O P H Y S I O L O G Y
Page 17
Three nights of multi-tasking and time management even though we are busy in
other major subject but yet we try our best to do these case study correctly and to avoid
correction about this work. but then again caring patient in medical ward is hard, hard,
because this is our first time to exposed in this ward with different kind of diseases that
some are not easy to handle and hard also because some of significant other are
uncooperative and non compliant, but at last we really succeed. It inst that smooth to
establish an interacting relationship specially that most of the patients significant other
institution has a low educational attainment/low class status. Therefore, we cannot
expect them to fully comprehend the instruction we have imparted. However, it was a
wonderful experience since we were handle different condition of the patient and we
performed some procedure which weren't return demonstrate yet. Fortunately, there is
our clinical instructor and our PCI who persistently supervised us and assisted us to
make it through with just minimal errors.
However, this our 4th time to manage group case study in different setting, adding to
that is the fear of making a physiologic structure of our client with a different kind of
diseases, we have learned to thorough assess our patient to comply with the
indispensable. Also we have acquired ourselves with regards to establish rapport with
our patient to have trusting relationship. But enjoy with other people helps you identify
your strength and weakness, and it aids in modifying what is somehow negative in our
attitude. Most and for all we thank to god for the guidance always and for giving wisdom
and knowledge to do this case study successful.....
X. SOURCES:
WEB:
http://nursingcrib.com/nursing-care-plan/nursing-care-plan-community-acquired-
pneumonia/

P A T H O P H Y S I O L O G Y
Page 17
http://merck-ut.merck.com/mmpe/sec05/ch052/ch052b.html
http://en.wikipedia.org/wiki/Community-acquired_pneumonia
BOOKS:
Nurse’s Pocket Guide 11th edition (Diagnoses, Prioritized interventions, and
Rationales)
By:
Marilyn E. Doenges
Mary Frances Moorhouse
Alice C. Murr
Nursing 2003 Drug Handbook 23rd edition
By: Springhouse Lippincott Williams and Wilkins