Careplan #2
Transcript of Careplan #2
-
7/29/2019 Careplan #2
1/30
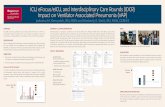
MIAMI DADE COLLEGE - MEDICAL CENTER CAMPUS - SCHOOL OF NURSINGNUR 1025L: Fundamentals Nursing Clinical
Students Name: Francisco J Ortiz Date:_06/15/13_ Clients Initials: ____EP____ Admission Date:_06/24/2011
Age: 75yr DOB: ______02/19/1936_____ Sex: X Male Female Race/Ethnicity: White/______________Support System: _____No living family membes _________________________________________________________
Religion: _Catholic__________
MEDICAL HISTORYALLERGIES: _NKA_Admitting Medical Diagnosis (es): COPD, hypertension, A Flutter, seizure disorder, dementia
Chief Complaint: patient states shortness of breath
History of Present Illness: Pt is a 75 year old who is complaining of shortness of breath. The patientreports that he can ambulate but limited. The patient denies any pain.
Past Medical History (include past surgical history):Heavy smoker , 2 to 3 packs a day. No alcohol abuse, no drug abuse
Clients (Parents)Understanding of Illness: patient understands and full aware of condition
Stage of Development: Erickson Ego Integrity vs. Despair _ Freud: According to Freud, the genitalstage lasts throughout adulthood. He believed the goal is to develop a balance between all areas of
life. Piaget _ Formal Operational
____Special Developmental Considerations: N/AHeight: 65 inches Weight: 117.1 kg Placement in Growth Chart: _N/AImmunizations: Patient refused flu vaccine
VITAL SIGNSTime Taken: ______0900_________ Activity: ______________ Position: ____wheel chair__________
1
-
7/29/2019 Careplan #2
2/30
T_36.1 P72 R 16 BP _111/68Baseline (Normal Age for Age):T_ 36.137.8 P_60 -100 R_12-20_ BP120/80 _
NUTRITIONDiet: REGULAR Food Preferences:_EXTRA SYRUP IN BREAKFAST, COFFEE AFTER LUNCH, COOKIEAFTER DINNERNutritional Requirements: (Cal/Kg/Day): 2100 CAL/KG/DAY Total Calories per Day: _1900___________Fluid Requirements (Ml/Kg/Day): __________________________________ ________________Total Fluids per Day:_______________________________
Special Treatments: ____________N/AMedications atHome:_N/A_____________________________________________________________________________________________________________________________________________________________________________________________________________
2
-
7/29/2019 Careplan #2
3/30
Medication(s) Worksheet
NAMECLASSIFICATI
ON
DOSE/ROUTE/FREQUENCY SAFE RANGE
MECHANISMOF ACTION
INDICATIONS SIDEEFFECTS
NURSINGCONSIDERATIOS AND PATIEN
EDUCATION
3
-
7/29/2019 Careplan #2
4/30
PHENYTOIN 100mg daily by mouth Limits seizurepropagation byaltering iontrans- port.May alsodecreasesynaptictransmission.Antiarrhythmicproperties as aresult ofshortening theactionpotential anddecreasingautomaticity.
Treatment/prevention of tonic-clonic(grand mal)seizures andcomplex partialseizures.
CNS:SUICIDAL
THOUGHTS,ataxia,agitation,confusion,dizziness,drowsiness,dysarthria,dyskinesia,extrapyramidal syndrome,headache,insomnia,weakness.EENT:diplopia,nystagmus.CV:hypotension
Monitor closely fonotable changesbehavior that couindicate theemergence orworsening ofsuicidal thoughtsbehavior ordepression.
Assess patient fophenytoinhypersensitivitysyndrome (feverskin rash,lymphadenopathRash usuallyoccurs within thefirst 2 wk oftherapy.Hypersensitivitysyndrome usuallyoccurs at 38 wkbut may occur up
to 12 wk afterinitiation oftherapy. May leato renal failure,rhabdomyolysis, hepatic necrosis;may be fatal.
4
-
7/29/2019 Careplan #2
5/30
MEMANTINE 10mg 1 tab daily bymouth
Binds to CNSN-methyl-D-aspartate(NMDA) re-ceptor sites,preventingbinding ofglutamate, anexcitatoryneurotransmitter.
Moderate tosevere Alzheimersdementia.
CNS:dizziness,fatigue,headache,sedation. CV:hypertension.Derm: rash.GI: weightgain. GU:urinaryfrequency.Hemat:anemia.
Assess cognitivefunction (memorattention,reasoning,language, abilityperform simpletasks) periodicallduring therapy.
Lab Test
Considerations:May cause anem
5
-
7/29/2019 Careplan #2
6/30
CITALOPRAM 10mg 1 tab daily bymouth
Selectivelyinhibits thereuptake ofserotonin inthe CNS.
Depression. NS:NEUROLEPTICMALIGNANTSYNDROME,SUICIDAL
THOUGHTS,apathy,confusion,drowsiness,insom- nia,weakness,agitation,amnesia,anxiety, p li-bido,dizziness,fatigue,impairedconcentration, qdepression,migraineheadache.EENT: ab-
normalaccommodation. Resp:cough.
Monitor moodchanges duringtherapy.
Assess for suicidtendencies,especially duringearly therapy anddose changes.
Restrict amount drug available topatient. Risk maybe increased inchildren,adolescents, andadults 24 yr. Aftstarting therapy,children,adolescents, andyoung adultsshould be seen bhealth careprofessional at
least weekly for 4wk, every 3 wk fothe next 4 wk, anon advice of heacare professionathereafter.
6
-
7/29/2019 Careplan #2
7/30
ENALAPRIL 5mg 1 tab daily bymouth
ACE inhibitorsblock theconversion ofangioten- sin Ito thevasoconstrictor angiotensinII. ACE in-hibitors alsoprevent thedegradation ofbradyki- ninand othervasodilatoryprostaglandins. ACE inhibitorsalso q plasmarenin levelsand p al-dosteronelevels. Netresult issystemicvasodila- tion.
Alone or withother agents in themanagement ofhypertension.
CNS:dizziness,drowsiness,fatigue,headache, in-somnia,vertigo,weakness.Resp: cough,dysp- nea.CV:hypotension,chest pain,edema,tachy- cardia.Endo:hyperuricemia. GI: tastedisturbances,abdominalpain,anorexia,consti-pation,
diarrhea,nausea,vomiting.
Hypertension:Moor blood pressureand pulsefrequently duringinitial doseadjustment andperiodically durintherapy. Notifyhealth careprofessional ofsignificant chang
7
-
7/29/2019 Careplan #2
8/30
CLONAZEPAM 0.5MG daily by mouthAnticonvulsanteffects may bedue topresynapticinhibition.Producessedativeeffects in theCNS, probablyby stimulatinginhibitoryGABA recep-tors.
Prophylaxis of:Petit mal, Petit malvariant, Aki- netic,Myoclonic seizures.Panic disorder withor withoutagoraphobia.
CNS:SUICIDAL
THOUGHTS,behavioralchanges,drowsiness,fatigue,slurredspeech,ataxia, seda-tion,abnormal eyemovements,diplopia,nystag- mus.Resp:increasedsecretions.CV: palpita-tions. GI:constipation,diarrhea,hepatitis,weight gain.
GU: dysuria,nocturia,urinaryretention.
Observe andrecord intensity,duration, andlocation of seizuractivity.
Assess degree anmanifestations oanxiety and menstatus (orientatio
mood, behavior)prior to andperiodically durintherapy.
8
-
7/29/2019 Careplan #2
9/30
Medication(s) Worksheet
CLASSIFICATION NAME
DOSE/ROUTE/FREQUENCY SAFE RANGE
MECHANISM
OF ACTION
INDICATIONS
SIDE EFFECTS NURSINGCONSIDERATIONS
AND PATIENTEDUCATION
LEVALBUTEROL
45MCG PRN R-enantiomerof racemicalbuterol.Binds tobeta- 2adrenergicreceptors inairwaysmoothmuscleleading toactivation ofadenylcyclase and in-creasedlevels ofcyclic-3, 5-adenosinemono-phosphate(cAMP).
Bronchospasm due toreversibleairwaydisease(short-termcontrolagent).
CNS: anxiety,dizziness,headache,nervousness.Resp:PARADOXICALBRONCHOSPASM (excessiveuse ofinhalers),increasedcough,turbinateedema. CV:tachycardia.GI: dyspepsia,vomiting.Endo:hyperglycemia.F and E:hypokalemia.Neuro: tremor.
Assess lung sounds,pulse,and bloodpressure beforeadministration andduring peak of med-ication. Note amount,color, and character ofsputum produced.Closely monitorpatients on higherdose for adverseeffects.
9
-
7/29/2019 Careplan #2
10/30
PREDNISONE 60MG DAILY PRN Inpharmacologic doses,all agentssuppress in-flammationand thenormalimmuneresponse. Allagents havenumerousintensemetaboliceffects (seeAdverseReactions/Side Effects).S
Management ofadrenocorticalinsufficiency.
CNS:depression,euphoria,headache, qintra- cranialpressure(children only),personalitychanges,psychoses,restlessness.
These drugs areindicated for manyconditions. Assessinvolved systemsbefore and periodicallyduring therapy.
10
-
7/29/2019 Careplan #2
11/30
Aspirin 81mg daily PO Inhibits thesynthesis ofprostaglandins that mayserve asmediators ofpain andfever,primarily inthe CNS.Has nosignificantanti-inflammatory propertiesor GItoxicity.
Mild pain.Fever.
GI: HEPATICFAILURE,HEPATOTOXICI
TY (overdose).GU: renalfailure (highdoses/chronicuse). He- mat:neutropenia,pancytopenia,leukopenia.Derm: rash,urticaria.
Assess overall healthstatus and alcoholusage beforeadministeringacetaminophen.Patients who aremalnourished orchronically abusealcohol are at higherrisk of developinghepato- toxicity withchronic use of usualdoses of this drug.
Assess amount,frequency, and type ofdrugs taken in patientsself-medicating,especially with OTCdrugs. Prolonged useof acetaminophenincreases the risk ofadverse renal effects.For short-term use,
combined doses ofacetaminophen andsalicylates should notexceed therecommended dose ofeither drug givenalone.
11
-
7/29/2019 Careplan #2
12/30
PATHOPHYSIOLOGY-BRIEF TEXTBOOK PICTURE WITH CLIENT COMPARISONDefinition, Etiology, Incidence, Pathophysiology, Diagnostic tests, Signs & symptoms, Medical
treatments
Textbook Client
Pathology- Chronic obstructive pulmonarydisease (COPD) is characterised by poorlyreversible airflow obstruction and an abnormalinflammatory response in the lungs. The latterrepresents the innate and adaptive immuneresponses to long term exposure to noxiousparticles and gases, particularly cigarettesmoke. All cigarette smokers have some
12
-
7/29/2019 Careplan #2
13/30
inflammation in their lungs, but those whodevelop COPD have an enhanced or abnormalresponse to inhaling toxic agents. This amplifiedresponse may result in mucous hypersecretion(chronic bronchitis), tissue destruction(emphysema), and disruption of normal repairand defence mechanisms causing small airwayinflammation and fibrosis (bronchiolitis).Classification- The twofold nature of thepathology has been studied in thepast.Furthermore, in recent studies, manyauthors found that each patient could beclassified as presenting a predominantlybronchial or emphysematous phenotype bysimply analyzing clinical, functional, andradiological findings or studying interestingbiomarkers.Etiology- The primary cause of COPD is exposureto tobacco smoke. Overall, tobacco smokingaccounts for as much as 90% of COPD risk.
Cigarette smoking induces macrophages torelease neutrophil chemotactic factors andelastases, which lead to tissue destruction.Clinically significant COPD develops in 15% ofcigarette smokers, although this number isbelieved to be an underestimate. Age ofinitiation of smoking, total pack-years, andcurrent smoking status predict COPD mortality.
People who smoke have an increased annualdecline in FEV1: the physiologic normal declinein FEV1 is estimated to be 20-30 ml/y, but therate of decline in COPD patients is generally 60
13
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1463976/figure/fig1/ -
7/29/2019 Careplan #2
14/30
ml/y or greater.
Statistics-
The National Health Interview Survey reports theprevalence of emphysema at 18 cases per 1000persons and chronic bronchitis at 34 cases per1000 persons.[24] While the rate of emphysemahas stayed largely unchanged since 2000, therate of chronic bronchitis has decreased.Another study estimates a prevalence of 10.1%in the United States.[25] However, the exactprevalence of COPD in the United States isbelieved to be underestimated. This is largelydue to the fact that it is an underdiagnosed (andundertreated) disease, because most patientsdo not present for medical care until the diseaseis in a late stage.
The exact prevalence of COPD worldwide islargely unknown, but estimates have variedfrom 7-19%. The Burden of Obstructive LungDisease (BOLD) study found a global prevalenceof 10.1%.[26] Men were found to have a pooledprevalence of 11.8% and women 8.5%. Thenumbers vary in different regions of the world.Cape Town, South Africa, has the highestprevalence, affecting 22.2% of men and 16.7%of women.
14
-
7/29/2019 Careplan #2
15/30
15
-
7/29/2019 Careplan #2
16/30
DIAGNOSTIC TESTS
Test(i.e. X-Ray, MRI, EEG, EKG)
RESULTSDate, Result, Significance
NOT APPLICABLE
16
-
7/29/2019 Careplan #2
17/30
17
-
7/29/2019 Careplan #2
18/30
Laboratory values
CHEMISTRYPROFILE
NORMALVALUES
CLIENTSVALUES
HEMOTOLOGY
NORMALVALUES
CLIENTS VALUES
DATE DATE
DATE DATE DATE
DATE
SODIUM 135-145
Meq/L
138
2/21/13
WBC 3.8-10.8
K/uL
4.6
2/21/13
POTASSIUM 3.5- 5.1mEq/L
4.62/21/13
RBC 3.80-5.20 3.56*2/21/13
CHLORIDE 98-108mEq/L
1082/21/13
HGB 11.8-15.4g/dl
11.8*
CO2 19-34 24.02/21/13
HCT 41-50 34.5*
CALCIUM 8.2-10.3mg/dL
8.32/21/13
MCV 79.4-94.8fL
96.9*2/21/13
GLUCOSE 70-105mg/dL
852/21/13
MCH
BUN 7-25 mg/
Dl
23
2/21/13
MCHC 25.6-32.2
pg
34.2
2/21/13CREATININE 0.6-1.2
mg/dL1.12/21/13
PLATELETS 11.5-15.0%
1092/21/13
PHOSPHORUSCHOLESTEROL
DIFFERENTIAL
TOTALPROTEIN
6.4-8.9g/dL
6.42/21/13
NEUTROPHILS
ALBUMIN 3.5-5.0g/dL
3.532/21/13
SEGMENTS
ALBUMIN/GLOBULIN RATIO
2.922/21/13
BANDS
18
-
7/29/2019 Careplan #2
19/30
AST (SGOT) 13-39 U/L 272/21/13
LYMPHOCYTES
ALT (SGPT) 7-52 U/L 152/21/13
EOSINOPHILS
TOTALBILIRUBIN
0.3-1.0mg/dL
BASOPHILS
AMYLASE MONOCYTES
LIPASECOAGULATION
STUDIESPTT
SODIUM 135-145Meq/L
1382/21/13
WBC 3.8-10.8 K/uL 4.62/21/13
POTASSIUM 3.5- 5.5mEq/L
4.62/21/13
RBC 3.80-5.20 3.56*2/21/13
CHLORIDE 98-108mEq/L
1082/21/13
HGB 11.8-15.4g/dl 11.8*
CO2 19-34 24.02/21/13
HCT 34.5*
CALCIUM 8.2-10.3mg/dL
8.32/21/13
MCV 96.92/21/13
GLUCOSE 70-105mg/dL 852/21/13 MCH
BUN 7-25 mg/Dl
232/21/13
MCHC 34.22/21/13
CBC BMP
Hgb Na+
Cl-
BUNWBC Plts Glucose
Hct K+ HCO3 Creatinine
19
-
7/29/2019 Careplan #2
20/30
URINALYSISCOLOR YELLOWAPPEARANCE CLEARSP. GRAVITY 1.015 MISCELLANEOUS
TESTPH 5 TEST NORMAL
VALUESCLIENTS VALUES
DATE DATE DATEGLUCOSE NORMA
L
URINE
CULTURE
PENDI
NG
06/10/1
3KETONE NEGATIVE
OCCULT BLOODPROTEIN NEGATI
VEBILRUBIN NEGATI
VEUROBILINOGEN NORMA
LNITRITE NEGATI
VELEUCOCYTE NEGATI
VE
CASTWBCRBCCRYSTALSSQUAMOUSCELLS/ EPITHELIALCELLS
Relate the clinical significance of abnormal lab values above:
RBC(LOW)- INDICATIONS:-Low RBC count leads to anemia. Anemia can be caused by blood loss,decreased blood cell production, increased blood cell destruction, or hemodilution.
20
-
7/29/2019 Careplan #2
21/30
HGB(LOW)- INDICATIONS:- Low Hct leads to anemia. Anemia can be caused by blood loss, decreasedblood cell production, increased blood cell destruction, and hemodilution. Causes of blood lossinclude menstrual excess or frequency, gastrointestinal bleeding, inflammatory bowel disease, andhematuria. Decreased blood cell production can be caused by folic acid deficiency, vitamin B12deficiency.
HCT (HIGH)- INDICATIONS:- High Hct leads to polycythemia. Polycythemia can be caused bydehydration, decreased oxygen levels in the body, and an overproduction of RBCs by the bone
marrow. Dehydration from diuretic use, vomiting, diarrhea, excessive sweating, severe burns, ordecreased fluid intake decreases the plasma component of whole blood, thereby increasing the ratioof RBCs to plasma, and leads to a higher than nor- mal Hct. Causes of decreased oxygen includesmoking, exposure to carbon monoxide, high altitude, and chronic lung disease, which leads to amild hemoconcentration of blood
MCV(HIGH)- INDICATIONS- Lipemia will falsely increase the Hgb measurement, also affecting the meancorpuscular volume (MCV) and MCHC.
Head to Toe Assessment
General Appearance:The pt is resting comfortably in no acute distressHead & Hair: Norm cephalic and atraumatic
Face: Norm cephalic and atraumatic
Eyes: Norm cephalic and atraumaticEars: Norm cephalic and atraumaticNose: Turbinates bright red and swollen, mucous pink, no swellingLips/Mouth/Throat: No cracking/ lesions on lips, mouth is clean and free from debris, mild breath odor.Neck:
21
-
7/29/2019 Careplan #2
22/30
Chest/Breast:Clear to palpation and auscultation lateral chest is larger than anterior/posterior diameter.Lungs:Clear to auscultation; no abnormal sounds heard.Heart:Normal rhythm sounds heart at the fine precordial points.Abdomen/Kidneys:Normal bowel sounds, no masses, lumps, or tenderness found.Genitalia (Internal Exam Deferred): N/ARectum (Internal Exam Deferred): N/AExtremities:No edema clubbing or cyanosisBack: no deformities
R.O.M.: Limited range of motion. Patient is in the wheelchair bound.Document findings on next page
22
-
7/29/2019 Careplan #2
23/30
23
-
7/29/2019 Careplan #2
24/30
Plan of Care
Priority Nursing Diagnosis:
Risk Nursing Diagnosis: Impaired Gas Exchange related to Altered oxygen supply as evidenceby:Supporting Data:
Subjective:Patient states I can hardly breathe when I walkObjective:patient spoke in short sentences
Expected Outcome (Goals)
Long Term: Patient will be able to provide self-care with less fatigue and dyspnea by discharge
Short Term: After 4 hrs. Of nursing interventions, the client will demonstrate behaviors to improve airway
clearance. e.g. cough effectively and expectorate secretions
Nursing InterventionsNursing Actions Scientific Principle
and/or RationaleEvaluation Modification of Plan of
Care
Pt will maintain clear lungfields and remain free ofsigns of respiratorydistress throughouthospital stay
Auscultate breathsounds Q1- 2 .Presence of crackles,wheezes maysignify airwayobstruction, leading toor exacerbatingexisting hypoxia.
Pt demonstratedeffective coughingtechniques for studentnurse
Monitor vital signs:Auscultate breath sounds,
Respiratory systemmay become
BP is 111/68 Lungsounds are clear to
24
-
7/29/2019 Careplan #2
25/30
heart rate and rhythm,respirations q 4 hours.
decompensated.Tachycardia andchanges in bloodpressure may bepresent because ofpain, anxiety andreduced cardiacoutput.
auscultation, respiratoryrate is between 20 to 24breaths per minute andpulse is at 72
Assess peripheral pulses,
capillary refill, skin turgor,and mucous membranes q4 hours.
Indicators of level of
hydration andadequacy of circulatingvolume.
Mucous membrane are
moist, capillary refill isless than 2 seconds andskin turgor has increased
Pt will maintain a patentairway at all time
Monitor resp. rate,depth, and effort, useof accessory muscles,nasal flaring, andabnormal breathingpatterns. respiratory rate, useof accessory muscles,nasal flaring,
and abdominalbreathing may indicatehypoxia.
Pts airway remainedopen
Identify priority of learningneeds within the overallcare plan as soon aspossible.
Teaching standardizedcontent that thepatient already knowswastes valuable timeand hinders criticallearning. Adults learnmaterial that is
The patientverbalizes understandingof priority learning needs.
25
-
7/29/2019 Careplan #2
26/30
important to them
Provide a quietatmosphere withoutinterruption within 2 hoursof admission.
A calm quietenvironment assiststhe patient withconcentrating morecompletely.
The patient is verycomfortable in herprivate room and readyto express her concernsregarding her healthcare.
Encourage questionsbefore and after eachteaching.
Questions facilitateopen communicationbetween patient andhealth careprofessionals, andallow verification ofunderstanding of giveninformation and theopportunity to correctmisconceptions
The patient askedquestions regarding herregimen, diet andconcerns when injectingherself.
Elevate head of bed,
assist patient to assumeposition to ease work of
breathing. Include periods
of time in prone position
as tolerated. Encourage
deep-slow or pursed-lip
breathing as individually
needed/ tolerated.
Oxygen delivery may
be improved by uprightposition and breathing
exercises to decrease
airway collapse,
dyspnea, and work of
breathing. Note: Recen
t research supports use
of prone position to
increase Pao2.
The patient tolerateddeep breathing exercisesafter showing correcttechniques
26
-
7/29/2019 Careplan #2
27/30
Monitor vital signs and
cardiac rhythm.
Tachycardia, dysrhyth
mias, and changes in
BP can reflect effect of
systemic hypoxemia
on cardiac function.
Patient blood pressuredropped to a stable levelafter medications weregiven
Monitor level of
consciousness/mental
status. Investigate
changes.
Restlessness and
anxiety are common
manifestations of
hypoxia. WorseningABGs accompanied by
confusion/somnolence
are indicative of
cerebral dysfunction
due to hypoxemia.
Patient was alert aftermaking necessarychanges
Evaluate level of activity
tolerance. Provide calm,
quiet environment. Limit
patients activity or
encourage bed/chair rest
during acute phase. Have
patient resume activitygradually and increase as
individually tolerated.
During
severe/acute/refractory
respiratory distress,
patient may be totally
unable to perform
basic self-care
activities because ofhypoxemia and
dyspnea. Rest
interspersed with care
activities remains an
important part of
treatment regimen. An
exercise program is
aimed at increasing
endurance and
Patient toleratedambulating from chair tobed after a short rest
27
-
7/29/2019 Careplan #2
28/30
strength without
causing severe
dyspnea and can
enhance sense of well-
being.
CARE PLAN RUBRICStudent: ___________________________________ Date: ______________________
CATEGORIES POSSIBLE POINTS
YOURPOINTS
COMMENTS
SUBJECTIVE DATA(Relevant and timely and quotedfrom patient)
10
OBJECTIVE DATA(Includes vital signs, physicalassessment findings, diagnostictests and procedures, relevantmedications, etc.)
10
NURSING DIAGNOSIS(NANDA, R/T, AEB)
20
GOAL 20
28
-
7/29/2019 Careplan #2
29/30
(Condition, Time Frame,Parameters, and must be realistic)
INTERVENTIONS ANDRATIONALES(Assess, Assist, and Teach)
20
EVALUATION OF CARE PLAN(Evaluate each nursing action foreffectiveness)
10
MODIFICATION OF CARE PLAN(Modify patient care plan based onpatients response to interventions)
10
*TOTAL SCORE:
*Student must obtain score of > 77% in order to obtain a grade of S on the weekly care plan.
Reviewed with student: ______________________________ Date: ___________________Signature
29
-
7/29/2019 Careplan #2
30/30