Cardio drugs
-
Upload
nhelia-santos-perez -
Category
Documents
-
view
1.670 -
download
5
Transcript of Cardio drugs

Cardiovascular Drugs

Learning Objectives
• Students will be able to:– Discuss the major categories of drugs as
they relate to the treatment of Cardiac Disease.
– Describe the major effects of various medications on cardiac function.
– Discuss major nursing implications when administering above medications.

Antihyperte
nsi
ve

Hypertension• Defined as a consistent elevation of the
systolic or diastolic blood pressure above 140/90mm Hg
• On two elevated readings (sitting and supine) on separate office visits
• Two types hypertension– Primary: no known cause– Secondary: consequence of underlying
disease or condition

CLASSIFICATION OF HYPERTENSION
Hypertension is classified as follows: • Prehypertension: BP 120 to 139 / 80 to
89 mm Hg
• Hypertension, Stage 1: BP 140 to 159 / 90 to 99 mm Hg
• Hypertension, Stage 2: systolic BP greater than or equal to 160 or diastolic BP greater than or equal to 100 mm Hg.

Goal with hypertension:
• Two primary regulatory factors:– Blood flow (volume)– Peripheral Vascular Resistance (PVR)
• Goal is to optimise these two in order to get pressure below 140/90 mm Hg

o

Pharmacotherapy
•Primary:•Diuretics•ACE Inhibitors•ARBs•Beta-blockers•Calcium channel blockers
•Alternate:•Alpha1-blockers
•Alpha2-blockers
•Direct-acting vasodilators
•Peripheral adrenergic antagonist


Diuretics
Therapeutic Effects (overall)
• General site of action is the nephron structure in the kidney (exact area depends on drug)
• Increases urine formation and output resulting in a net loss of H2O from the body and decreased BP

Loop Diuretics
Mechanism of action:
• Inhibits Na+ and Cl- resorption in the loop of Henle and so H2O (water follows sodium)
• Dilates blood vessels

Loop Diuretics
Therapeutic effects:• Potent diuresis resulting in substantial fluid loss• Treats edema associated with CHF and hepatic or
renal disease
Adverse effects:• hypokalemia • metabolic alkalosis• dehydration (hypovolemia), leading to hypotension • dose-related hearing loss (ototoxicity)

Loop DiureticsSpecific Drugs• furosemide• Torsemide• bumetanide
Nursing actions:• Monitor I/O and BP• Monitor effects of Lanoxin (digoxin) • Baseline and close monitoring of K+• Assess for:
• Dehydration• Hypotension• Hearing loss

ThiazideMechanism of action:
– inhibit the sodium-chloride transporter in the distal tubule. Because this transporter normally only reabsorbs about 5% of filtered sodium, these diuretics are less efficacious than loop diuretics in producing diuresis and natriuresis.

ThiazideTherapeutic effects:
– Excretion of Na+, Cl-, K+ and H2O without altering pH
– Treatment of edema
Side effects– Hypokalemia– Headache, dizziness

ThiazideSpecific Drug• Hydrodiuril (hydrochlorthiazide)• Zaroxolyn (Metolazone)

NCs: ThiazideNursing actions:
• Monitor I/O, BP and K+
• Monitor effects of Lanoxin (digoxin)
• Monitor electroytes
• Adequate dietary K+
• Monitor uric acid
• Crosses placenta and into breastmilk

Potassium Sparing Diuretics
Mechanism of action:• antagonize the actions of aldosterone (aldosterone
receptor antagonists) at the distal segment of the distal tubule. This causes more sodium (and water) to pass into the collecting duct and be excreted in the urine.
Therapeutics effects:• Diuresis• Decreased K+ excretion

Potassium Sparing Diuretics cont
Adverse effects:• Electrolyte imbalance with potential
elevation in K+ • Headache, dizziness
Prototype:• Aldactone (spironolactone)

NCs: Potassium Sparing Diuretics
Nursing actions:– Monitor I/O, BP and K+ – Monitor effects of Lanoxin (digoxin)– No salt substitutes or K+ rich foods– Contraindicated:
• Pregnancy, lactation
• Initial and follow-up uric acid levels
• Monitor CBC
• Watch for s/s of infection
• Spironalactone
• Gynecomastia
• Testicular atrophy
• Hirsutism

Calcium Channel Blockers
Mechanism of action:• Inhibits transport of calcium into
myocardial and smooth muscle cells• Dilates peripheral arterioles, decreasing
afterload• Decreases heart contractility (negative
ionotrope)• Decreases SA node firing rate and
conductivity of AV node (negative chronotrope)

Calcium Channel Blockers cont.
Therapeutic Effects:• Lowers HR and BP- Depending on drug in
class
• Decreases myocardial O2 demand
• Decreases coronary artery spasm
• Decreases angina and rhythm disturbances

Calcium Channel Blockers cont.
Side effects:• Bradycardia, reflex tachycardia
• Peripheral edema
Interactions:• Other antihypertensives and diuretics
(increased hypotensive effects)

Calcium Channel Blockers cont.
Prototypes:• Calan (verapamil), Cardiazem (diltiazem)
and Norvasc (amlodipine)Nursing considerations:• Monitor BP, HR, I/O, daily weight, side
effects• Focus assessment-cardiac and pulmonary

NCs: Calcium Channel Blockers
• Baseline ECG, HR, BP
• Frequent assessment of VS
• Contraindicated:• complete heart block
• Pregnancy Category C
• No grapefruit juice
• May worsen Heart Failure
• Evaluate any c/o chest pain

e

Angiotensinogen in plasma
Juxtaglomerular cells-kidney
↓Serum Sodium ↓Blood volume
Angiotensin I
Kidney tubules
Angiotensin II
Adrenal Cortex
↑Sodium resorption
(H2O resorbed
with sodium); ↑
Blood volume
RENIN
Angiotensin-Angiotensin-converting converting
enzymeenzyme
ALDOSTERONE
Intestine, sweat
glands, Salivary glands
Via vasoconstriction of arterial smooth muscle
RENIN-ANGIOTENSIN-ALDOSTERONE RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM (RAAS)SYSTEM (RAAS)

Angiotensin Converting Enzyme Inhibitors (ACE-I)- “prils”
• Mechanism: Blocks interaction between Angiotensin I and Renin, preventing production of Angiotensin II
• Angiotensin II not produce resulting in decreased vasoconstriction and decreased afterload
• Decreased aldosterone production results in decreased Na and H2O reabsorption so decreased BP

Angiotensin Converting Enzyme Inhibitors (ACE-I)- “prils” cont.
• Adverse Effects– Most common: dry, nonproductive cough– Dizziness, increased potassium levels
• Interactions: Other antihypertensives and diuretics (increased hypotensive effects)
• Prototypes:
• Vasotec (enalapril) and Zestril (lisinopril)


te

NCs: ACE Inhibitors
• Baseline VS• Captopril- oral dose 1 hour pc• First dose phenomenon• IV: monitor BP carefully• Monitor for Angioedema• Monitor K+, CBC• Assess for S/S infection• Pregnancy Category D• Assess for minor side effects

Angiotensin II Receptor Blockers (ARB’s)- “sartans”
• Mechanism of action: Blocks binding of Angiotensin II to its receptor sites
• Therapeutic effects– Decreased BP: Decreased vasoconstriction,
decreased vascular resistance, decreased afterload– Major use is afterload reduction in CHF and MI– Frequently a second line treatment for patients who
do not tolerate ACE-I

Angiotensin II Receptor Blockers (ARB’s)- “sartans” cont.
• Adverse effects– Most common is headache
• Interactions: Other antihypertensives and diuretics (increased hypotensive effects)
• Prototype:
• Cozaar (losartan) and Diovan (valsartan)

Angiotensin II Receptor Blockers (ARB’s)- “sartans” cont
Nursing considerations
• Monitor BP, I/O, daily weight, side effects
• Monitor Potassium levels and renal function
• Reinforce patient education
• Contraindicated to pregnant women
• Can be taken without regard to food
• First Dose Phenomenon
• Orthostatic BP checks
• Monitor renal, hepatic, and electrolyte level

Beta Blockers- “ololsMechanism of action:
• Cardioselective: Bind to and block B1 receptors on the hearts conduction system and throughout the myocardium
• Nonselective: bind to, and block, B1 and B2 receptors (heart and lungs)
• Decreases heart contractility (Negative ionotrope) reducing O2 requirements of myocardial cells
• Decrease SA node firing rate (negative chronotrope)

Beta Blockers- “olols cont.
Therapeutic Effects– Decreased heart rate and decreased
myocardial oxygen demand
– Decreased angina
– Fewer rhythm disturbances
– Decreased renin release

Beta Blockers- “olols cont.
Adverse effects:– Dysrhythmias (bradycardia), heart
failure– Bronchospasm / bronchoconstriction– Fatigue, depression, impotence
Interactions:– Other antihypertensives and diuretics
(increased hypotensive effects)

Beta Blockers- “olols cont.
Prototypes:– Inderal (propranolol), Lopressor (metoprolol)
and Tenormin (atenolol)
Nursing Actions:– Monitor BP, HR, I/O, daily weight, side effects– Focus assessment-cardiac and pulmonary– Contrindicated with some dysrhythmias, CHF
and some lung diseases

NCs: Beta-adrenergic Blockers
• May take two weeks for optimal therapeutic response
• Check BP and pulse prior to dose• Monitor cardiac function• Assess for:
• Respiratory distress• Bradycardia, heart block, fatigue, activity
intolerance
• DO NOT STOP SUDDENLY


y

Alpha1-adrenergic Antagonists
Mechanism of action-selectively inhibits alpha-1 adrenergic receptors. Blockages of the alpha-1 adrenergic action on the vascular smooth muscles lead to a decrease in vascular resistance and antihypertensive activity.

NCs: Alpha1-adrenergic Blockers
• First dose phenomenon
• Assess BP prior to and during RX
• Persistent orthostatic hypotension
• Assess for:• Weakness, dizziness, headache, GI
complaints
• Closely monitor elderly


Direct Vasodilators
• Relaxes smooth muscle in arterioles < PVR
• Highly effective but many side effects (some serious)• Reflex tachycardia • Sodium/water retention
• Not a first choice drug • Primary use: emergency situations where
immediate ↓ in BP is needed

NCs: Direct Vasodilators
• Monitor: VS, ECG, SpO2 during RX
• Assess for increased HR
• BP q 5 min if not continuous monitor
• Contraindicated: hypersensitivity, CAD, rheumatic mitral valve disease, CVA, renal insufficiency, SLE
• Priapism- medical emergency

Direct Vasodilators
• IV Nitroprusside (Nitropress):• Continuously monitored• Only dilute in D5W• Brown color; protect from light
• Minoxidil (Loniten):• BP & pulse both arms, three positions• Assess for orthostatic hypotension
• Diazoxide (Hyperstat):• For hypetensive crisis in L&D

Cardiac Glycosides,
Antianginals,
Antidysrhythmics

Cardiac Glycosides
• AKA digitalis glycosides
• Group of drugs that inhibit the sodium-potassium pump, thus increasing intracellular calcium which causes cardiac muscle fibers to contract more efficiently

Action Potential

Cardiac Glycosides
Therapeutic Effects
1.Positive Inotropic action
2.Negative Chronotropic action
3.Negative Dromotropic effect

Inotropes

Inotropes• Agents that affect myocardial contraction
• Positive Inotropes– Cardiac glycosides– Catecholamines
• Negative Inotropes– BB – CCB– Class IA & IC anti-arrhythmics

Class Participation
Which of the following is an example of a positive inotrope?
a) Docusate
b) Digoxin
c) HCTZ
d) Propranolol
e) Nitroglycerin

Class Participation
Which of the following is an example of a positive inotrope?
a) Docusate
b) Digoxin
c) HCTZ
d) Propranolol
e) Nitroglycerin

Cardiac Glycosides • Prototype: Digoxin (Lanoxin®, Digitek®,
Lanoxicaps®)

Digoxin MOA

Digoxin (cont’d) Nursing Responsibilities– Assess heart rate before administration; if
below 60 bpm withhold the drug.– Monitor serum potassium– Assess for signs of Digitalis toxicity
• Bradycardia• GI manifestations (anorexia, nausea, vomiting and
diarrhea)• Dysrhythmias• Altered visual perceptions• In males: gynecomastia, decreased libido and
impotence

Chronotropes

Chronotropes• Agents that change heart rate
– affects the nerves controlling the heart– changes the rhythm produced by the SA node

Chronotropes (cont’d)
• Positive Chronotropes– Atropine– Quinidine– Dopamine– Dobutamine– Epinephrine– Isuprel
• Negative Chronotropes– Beta-blockers– Acetylcholine– Digoxin– Diltiazem– Verapamil– Ivabradine– Metoprolol

Positive ChronotropePrototype: Atropine
• belladonna alkaloid
• d,l-hyoscyamine
• Anticholinergic
• Uses
– Symptomatic bradycardia
– Aspiration prophylaxis
– Produces mydriasis
– Organophosphate toxicity
– Adjunct nerve agent & insecticide poisoning

Atropine (cont’d)
• MOA– competitive inhibitor at autonomic postganglionic
cholinergic receptors
• Clinical effects– “anti-SLUD” Salivation, Lacrimation, Urination,
Digestion, Defecation– ↓ in salivary bronchial, & sweat gland secretions;
mydriasis; changes in heart rate; contraction of the bladder detrusor muscle and of the GI smooth muscle; ↓ gastric secretion; and ↓ GI motility

Nursing Responsibilities
• Monitor HR---note rhythm, quality, and rate
• Monitor I&O
• Assess for dryness or mucus membranes
• Monitor GI function

Anti-anginal Drugs

Antianginal Drugs
• Prototype: Nitrites & Nitrates
• BB• Calcium Channel
Blockers (CCBs)

Angina Pectoris Definition:Angina: Choking or suffocation.Pectoris: Chest.
Angina pectoris, is the medical term used to describe acute chest pain or discomfort.Angina occurs when the heart’s need for oxygen increases beyond the level of oxygen available from the blood nourishing the heart.
It has 3 types • Stable Angina• Un stable angina & • Variant Angina (Prinzmetal’s or resting angina) :

Types of Angina • Stable angina:
– People with stable angina have episodes of chest discomfort that are usually predictable. That occur on exertion or under mental or emotional stress.Normally the chest discomfort is relieved with rest, nitroglycerin (GTN) or both.
– It has a stable pattern of onset, duration and intensity of symptoms.

• Unstable angina:
– It is triggered by an un predictable degree of exertion or emotion.
– (progressive), more severe than stable. Characterized by increasing frequency & severity. Provoked by less than usual effort, occurring at rest &
– interferes with pt lifestyle.

• Variant Angina (Prinzmetal’s or resting angina) :occur spontaneously with no relationship to activity. Occurs at rest due to spasm. Pt discomfort that occurs rest usually of longer duration. Appears to by cyclic & often occurs at about the same time each day (usually at night). Thought to be caused by coronary artery spasm

Symptoms of Angina

Nitrites/Nitrates
• Previously known as “coronary dilators”
• Main effect: to produce general vasodilation of systemic vein & arteries– ↓preload & ↓afterload – ↓ cardiac work & oxygen consumption
• 2 main uses– Angina attacks– Angina prophylaxis

Class Participation
Which is the PREFERRED route for nitroglycerin during angina attacks?
a) Topical (ointment 2%)
b) IV infusion
c) Transdermal
d) SL
e) Extended release tablets/capsules

Class Participation
Which is the PREFFERED route for nitroglycerin during angina attacks?
a) Topical (ointment 2%)
b) IV infusion
c) Transdermal
d) SL
e) Extended release tablets/capsules

Drug
(Trade Name)
Common Dosage
Onset Duration
Amyl nitrate
(Vaporole®)
0.3 ml inhalation
30-60 sec 10 min
ISDN
(Isordil®)
2.5 - 10 mg SL
5 - 30 mg po qid
2-5 min 2 - 4 hr
Nitroglycerin
(Nitro-bid®) 2% ointment 15 min 4 - 8 hr
(Nitrostat®) 0.3 - 0.6 mg SL 1-3 min 10 - 45 min
(Nitrogard®) 1,2,3 mg XR tab 30 min 8 - 12 hr
(Transderm-
Nitro®)
2.5 - 15 mg/day
Transdermal patch
30-60 min 24 hr

MOA
Direct relaxation of arterial and venous smooth muscle – Venodilation predominates at therapeutic doses which
reduces preload – Arteriodilation at high doses (high therapeutic/toxic)
which produces hypotension compensated by sympathetics (heart/vascular)to produce tachycardia

Nitroglycerin (NG) • Indications
– Angina– Acute MI– HF– HTN– Hypertensive emergency– Hypotension induction– Peri/postoperative HTN– Pulmonary edema– Pulmonary HTN

NG (cont’d)• Dosing
– 1 tablet (0.3 mg, 0.4 mg, or 0.6 mg strength) SL, dissolved under the tongue or in buccal pouch immediately following indication of anginal attack
– During drug administration, the patient should rest, preferably in the sitting position
– Symptoms typically improve within 5 minutes. If needed for immediate relief of stable angina symptoms, SL nitroglycerin may be repeated every 5 minutes as needed, up to 3 doses

NG (cont’d)• Adverse Effects
– dizziness or fainting– flushing of the face or
neck– headache, this is
common after a dose, but usually only lasts for a short time
– irregular heartbeat, palpitations
– nausea, vomiting
• Contraindication:– sildenafil (Viagra®)– tadalafil (Cialis®)– vardenafil (Levitra®)
• Lab monitoring not necessary

Antidysrhythmics
Antiarrhythmics

What are Arrhythmias?• Cardiac disorder of
– Rate– Rhythm– Impulse generation– Conduction of electrical
impulses in the heart• Causes
– May develop from a diseased heart
– Consequence of chronic drug therapy
• Symptoms– Mild palpitations
cardiac arrest• Treatment goal
– Covert arrhythmia to a normal rhythm

Antidysrhythmics/Antiarrhythmics
• Uses– restore normal cardiac
rhythm– Successful conversion
of an arrhythmia depends on the type of arrhythmia present

Antidysrhythmics/Antiarrhythmics
• 4 major classes – Class I
• Class IA• Class IB• Class IC
– Class II– Class III– Class IV

Cardiac Action Potential
4: resting membrane potential; steady K+ flux
0: Na+ influx into cell
1: K+ efflux
2: K+ efflux & Ca+ influx
3: K+ efflux

Antiarrthymics: Class I
• Na channel blockers
• Common features– Local anesthetic activity– Interferes with movement of Na ions– Slow conduction velocity– Prolong refractory period – Decreases automaticity of the heart

Class IA• Quinidine (Quinidine sulfate®,
Quinaglute®, Quinidex®, Cardioquin®)
• Disopyramide (Norpace®)
• Procainimide (Procainimide HCI®, Procan®, Procanabid®, Pronestyl®)

Class 1A – Quinidine
• Derived from cinchona tree• Depresses both the myocardium & conduction
system• Overall effect: slows heart rate• Pharmacokinetics
– Well absorbed in GI tract after po administration– Metabolized to several active metabolites– Primarily excreted by urinary tract– Cardiac poison when large amounts are present in
blood

Class 1A – Quinidine (cont’d)• Adverse Effects
– N/V, diarrhea, weakness, fatigue, cinchonism
• Drug Interactions– Hyperkalemia– Digitalis – propranolol
• Monitoring– CBC – ECG – serum quinidine concentrations (target range
2-6 µg/ml or higher)
• CI: AV block

Class IB
• prototype: Lidocaine (Xylocaine®)
• Tocainide (Tonocard®)
• Mexiletene (Mexitel®)
• Phenytoin (Dilantin®)

Lidocaine – Class IB
• MOA: blocks influx of Na fast channel
• Indication: ventricular arrhythmias

Lidocaine – Class IB (cont’d)
• Common Adverse Effects– anxiety, nervousness– dizziness, drowsiness– feelings of coldness, heat, or numbness; or
pain at the site of the injection– N/V
• Monitoring – serum lidocaine concentrations (target range
2-6 µg/ml): parenteral use

Class IC
• prototype: Flecainide (Tambocor®)
• Propafenone (Rhythmol®)

Flecainide – Class IC
• MOA– Blocks fast Na channels depresses the upstroke of the
action potential, which is manifested as a decrease in the maximal rate of phase 0 depolarization.
– significantly slow His-Purkinje conduction and cause QRS widening
– shorten the action potential of Purkinje fibers without affecting the surrounding myocardial tissue.
• Indications– Afib– Atrial flutter– Ventricular tachycardia prophylaxis

Flecainide – Class IC• Adverse Reactions
– visual impairment, dizziness, asthenia, edema, abdominal pain, constipation, headache, fatigue, and tremor, N/V, arrhea, dyspepsia, anorexia, rash, diplopia, hypoesthesia, paresthesia, paresis, ataxia, flushing, increased sweating, vertigo, syncope, somnolence, tinnitus, anxiety, insomnia, and depression.
• Avoid in– CHF– Acute MI– Hx of MI (LVEF < 30%)
• Monitoring– ECG – serum creatinine/BUN: baseline

Class II – Beta Blockers
• Propranolol (Inderal®) • Acebutolol (Sectral®) • Atenolol (Tenormin®) • Betaxolol (Kerlone®) • Bisoprolol (Zebeta®) • Carvedilol (Coreg®) • Esmolol (Brevibloc®)• Metoprolol(Toprol®, Lopressor®) • Nadolol (Corgard®) • Timolol (Blocadron®)

Propranolol Warning• 2 situations in which propranolol requires
extreme caution– AV block– CHF– Asthma or emphysema

Class III
• K+ channel blockers
• Drugs:– Prototype: Amiodarone (Cordarone)– Bretylium (Bretylol)– Sotalol (Betapace)

Amiodarone – Class IIIMOA
– noncompetitively inhibits alpha- and beta-receptors,– possesses both vagolytic and calcium-channel
blocking properties– relaxes both smooth and cardiac muscle
• Indications– Vfib– Vtach

Amiodarone – Class III (cont’d)
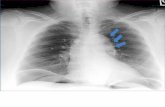
• Monitoring– CBC – chest x-ray – ECG – ophthalmologic exam – thyroid function tests (TFTs)

Class IV
• Ca channel blockers
• Drugs– Adenosine (Adenocard ®)– Diltiazim (Cardizem®, Tiazac®) – Verapamil (Dovera®, Isoptin®, Calan®)
• Clinical Effects– widen the blood vessels– may decrease the heart’s pumping strength

Sympathomimetics

Sympathomimetics• 2 classes:
– α- agonist
• Phenylephrine
• Clonidine
• Oxymetazoline
• Tetrahydralazine
• Xylometazoline
– β-agonist
• Prototype: Epinephrine
• Norepinephrine
• Dopamine
• Dobutamine
• Isoproterenol
• SE:– hypertension, – excessive cardiac
stimulation– cardiac arrhythmias – Long-term use increases
mortality in heart failure patients.
• CI– CAD

Epinephrine
• “fight or flight “hormone
• Aka “adrenaline”
• increases heart rate and stroke volume
• dilates the pupils
• constricts arterioles in the skin and gastrointestinal tract while dilating arterioles in skeletal muscles

Epinephrine MOA

Epinephrine (cont’d)
• Indications– Vfib– Ventricular asystole– Cardiac arrest– Pulseless electrical
activity
• IV Dosage– IV: 1 mg (10 ml of a
1:10,000 solution) IV; may repeat every 3-5 minutes
– Each dose may be given by peripheral injection followed by a 20 ml flush of IV fluid.

Epinephrine
• Common Adverse Effects– anxiety or nervousness– dry mouth– drowsiness or dizziness– headache– increased sweating– nausea– weakness or tiredness
• Monitoring– ECG: in patients receiving IV therapy

Vasopressors

Vasopressors• Vasoconstrictors vs. Vasodilators• 2 Vasoconstrictor Classes
– Sympathomimetics– Vasopressin Analogs
• Vasodilators• Alpha-adrenoceptor antagonists (alpha-blockers) • Angiotensin converting enzyme (ACE) inhibitors• Angiotensin receptor blockers (ARBs)• Beta2-adrenoceptor agonists (b2-agonists)• Calcium-channel blockers (CCBs)• Centrally acting sympatholytics• Direct acting vasodilators• Endothelin receptor antagonists• Ganglionic blockers• Nitrodilators• Phosphodiesterase inhibitors• Potassium-channel openers• Renin inhibitors

Vasoconstrictor• any agent that produces vasoconstriction
and a rise in blood pressure (usually understood as increased arterial pressure)
• Drugs– Prototype: Vasopressin– Epinephrine– Dobutamine– Dopamine – Norepinephrine

Vasopressin• aka : “ADH”• MOA
– ↑ the resorption of water at the renal collecting ducts
– Vasoconstrictive property: stimulates the contraction of vascular smooth muscle in coronary, splanchnic, GI, pancreatic, skin, and muscular vascular beds

Vasopressin (cont’d)
Indications: – Cardiac arrest– Cardiogenic shock– Cardiopulmonary resuscitation– Hypotension– Septic shock– Diabetes Insipidus

Vasopressin (cont’d)
• Dosage for cardiac arrest including ventricular asystole and pulseless electrical activity (PEA) during cardiopulmonary resuscitation (CPR)– IV or intraosseous dosage:
• Adults: A single dose of 40 units IV (or intraosseous) may be given one time to replace the first or second dose of epinephrine during cardiac arrest
• Do not interrupt cardiopulmonary resuscitation to administer drug therapy.

Vasopressin (cont’d)• Adverse Effects
– Cardiovascular: Cardiac arrest; circumoral pallor; arrhythmias; decreased cardiac output; angina; myocardial ischemia; peripheral vasoconstriction; and gangrene
– CNS: Tremor; vertigo; “pounding” in head– Dermatologic: Sweating; urticaria; cutaneous gangrene– GI: Abdominal cramps; nausea; vomiting; passage of gas– Hypersensitivity: Anaphylaxis (cardiac arrest and/or
shock) has been observed shortly after injection– Respiratory: Bronchial constriction.
• Monitoring– serum osmolality – serum Na

Anticoagulants

Antiplatelets/Anticoagulants
• Prevents/interferes with coagulation• Uses
– deep vein thrombosis (DVTs), pulmonary embolism, myocardial infarctions & strokes in those who are predisposed

Types of Antiplatelets/Anticoagulants
• Antiplatelets– Aspirin– Dipyridamole– Thienopyridines
• Clopidogrel (Plavix)• Ticlopidine (Ticlid)
– Glycoprotein IIb/IIIa antagonists• Abciximab (ReoPro)• Eptifibatide (Integrelin)• Tirofiban (Aggrastat)

Antiplatelets/Anticoagulants
• Anticoagulants– Heparin– LMWH
• Enoxaparin (Lovenox®)• Dalteparin (Fragmin®)• Tinzaarin (Innohep®)
– Factor Xa inhibitors• Fondaparinux (Arixtra®)
– Direct Thrombin Inhibitors• Argatroban • Lepirudin (Refludan®)
– Oral Anticoagulants• Prototype: Warfarin

Coagulation Cascade

Warfarin – Oral Anticoagulant
• MOA: Warfarin inhibits the synthesis of vitamin K-dependent coagulation factors II, VII, IX, and X and anticoagulant proteins C and S

Warfarin (cont’d)
• Indications– Stroke– DVT– Post MI– Afib– Cardiomyopathy

Warfarin Warnings
Bleeding Risk!• Warfarin can cause major or fatal bleeding• Risk factors for bleeding
– 65 years of age and older– history of GI bleeding– Hypertension– cerebrovascular disease– anemia, malignancy– Trauma– renal function impairment– long duration of warfarin therapy.
• Pregnancy Category X

Warfarin (cont’d)• SE
– Hemorrhage: Signs of severe bleeding resulting in the loss of large amounts of blood depend upon the location and extent of bleeding. Symptoms include: chest, abdomen, joint, muscle, or other pain; difficult breathing or swallowing; dizziness; headache; low blood pressure; numbness and tingling; paralysis; shortness of breath; unexplained shock; unexplained swelling; weakness
Nursing responsibilitiesPatients should be instructed about prevention measures to minimize risk of bleeding and to
report immediately to health care provider signs and symptoms of bleeding
– prothrombin time (PT) – stool guaiac – bleeding– DDIs
• NSAIDs• 3 G’s
– Garlic – Ginger– Ginsing
– Vitamin K intake

Class Participation Question #5:
Which foods are high in vitamin K?

Class Participation Question #5:
Which foods are high in vitamin K?

Fibrinolytic Enzymes

Fibrinolytic Enzymes• “clotbusters”
• MOA: stimulate the synthesis of fibrinolysin which breaks the clot into soluble products
• Drugs– Urokinase (Abbokinase®)– Anistreplase (Eminase®)– Alteplase (Activase®)– Reteplase (Retevase®)– Prototype: Streptokinase (Strepase®)

Streptokinase (cont’d)• Indications
– Acute MI– Acute ischemic stroke– Pulmonary embolism– Lysis of DVT
• Dose Administration– Parental infusion (usually IV)– Deep vein or arterial thrombosis
• IV: 250,000 IU over 30 min followed by 100,000 IU per hour up to 72 hours

Streptokinase (cont’d)
• Adverse Effects– Hemorrhage– Concomitant use of heparin, oral
anticoagulants, NSAIDs is NOT recommended because of the increased risk of bleeding
– Allergic reactions

Streptokinase (cont’d)

Antilipidemics

Antilipidemics
• Drugs that lower down abnormal blood lipid levels.

Types of antilipidemics– Statin drugs work by inhibiting the synthesis of cholesterol in the
liver. Liver enzymes must be regularly monitored. (ex. Simvastatin)
– Niacin, a water-soluble B vitamin, is highly effective in lowering LDL and triglyceride levels by interfering with their synthesis. Niacin also increases HDL levels better than many other lipid-lowering drugs.(Ex. Niacin SR)
– Fibric acid derivatives work by accelerating the elimination of VLDLs and increasing the production of apoproteins A-I and A-II. (ex. Lipofen, Tricor)
– Bile-acid sequestrants increase conversion of cholesterol to bile acids and decrease hepatic cholesterol content. The primary effect is a decrease in total cholesterol and LDLs. (ex. Questran)

Side effects
• Constipation
• Peptic ulcer
• Flushing
• Headache

Nursing responsibilities
• Monitor client’s lipid levels
• Observe for signs of GI upset
• Instruct to take with sufficient fluids or meals
• Low fat diet
• Instruct not to abruptly stop intake

Questions?