Cardio
Click here to load reader
-
Upload
lilly-daye -
Category
Documents
-
view
9 -
download
0
description
Transcript of Cardio
-
1. ACE inhibitors -ACE -I (drugs ending in "pril" captopril) -Inhibit conversion of angiotension I toangiotension II resulting in reduced saltand water retention.
2. ACE inhibitors -Promote vasodilatation and diuresisdecreasing blood volume, resulting in adecrease in the heart's workload-May be the first medication prescribed -Monitor patient for hyperkalemia andhypotension.
3. Acute CoronarySyndrome orAcute MyocardialInfarction
Life threatening condition characterizedby the formation of localized necroticarea within the myocardium
4. Aldosteroneantagonists(ALDO ANT)
-Methyldopa (Aldomet), clonidine(Catapres)-Acts on CNS, affecting norepinephrine
5. AnginaDiagnosticFindings
-ECGRestingExercise-Coronary Angiogram Remains the gold standard in diagnosingthe percentage of blockage in coronaryarteries.
6. Angina Pectoris Clinical syndrome usually characterizedby episodes of pain or pressure inanterior chest, caused by insufficientcoronary blood flow.
7. AnginaPharmacologicTherapy
-Nitrates*Dilates vessels, causing decreasedperipheral resistance, decreased BP andpooling of blood in the body- adrenergic blockers*Decrease HR, BP and contractility ofheart-Calcium channel blockers*Act on SA node to slow heart rate anddecrease strength of heart musclecontraction-Antiplatelet and Anticoagulants*Prevents platelet aggregation andsubsequent thrombosis, which impedesblood flow-Oxygen
8. AnginaPrecipitatingFactors
-Physical exertion-Temperature extremes-Eating a heavy meal-Emotional stress-Smoking-Sexual activity.
9. AngiotensinReceptor Blockers(ARB)
-Angiotensin receptor blockers (drugsending in "sartan" losartan or Cozaar)-Block the effects of angiotensin II atthe receptor site.-Reduces peripheral resistance.
10. Arterial Ulcers -Typically small, circular and deep-On tips of toes or in the web spacesbetween the toes-Gangrene of toe results from traumato area-Pain is described as intermittentclaudication.-No Edema (not enough blood)
11. ArteriosclerosisMedicalManagement
-Avoid particular stimuli*Cold*Tobacco*Stress-Pharmacologic*Calcium channel blocker (nifedipine:low dose vasodilator)
12. ArteriosclerosisNursing Diagnosis
-Ineffective or altered peripheral tissueperfusion r/t compromised circulation-Chronic pain r/t impaired ability ofperipheral vessels to supply tissueswith oxygen-Risk for Impaired Skin Integrity r/tdecreased peripheral circulation-Deficient knowledge regarding self-care activities.
13. ArteriosclerosisNursinginterventions
-Improving Peripheral ArterialCirculation*Position of extremity*Exercise-Promoting Vasodilation andPreventing *Vascular Compression*Smoking cessation.*Warm blanket to abdomen.*Avoid cold temperatures.*Adequate loose fitting clothing.
14. ArteriosclerosisNursinginterventions (2)
-Relieving Pain*Analgesic administration*Slow increase in exercise andformation of collateral circulation-Maintaining Tissue Integrity*Avoid trauma to area*Sturdy, well fitting foot wear.*Careful examination and care of feet.*Good nutrition for cell health.
Cardiovascular NursingStudy online at quizlet.com/_987fq
-
15. ArteriosclerosisPrevention andMedicalManagement
-Modification of Risk Factors-Lower cholesterol*Diet*Medications-Maintain normal blood pressure-Smoking cessation-Increasing activity-Manage diabetes-Surgery to clear occlusion in artery.
16. Atherosclerosis Accumulation of lipids, calcium, bloodcomponents, and fibrous tissue on theintima of large and medium-sizedarteries.
17. AtherosclerosisRisk Factors
-Modifiable*Nicotine*Diet*Hypertension*Diabetes*Obesity *Stress*Sedentary lifestyle*C-reactive protein
18. Benign -Premature atrial contractions (PAC)-Premature ventricular contractions(PVC) Coffee excess.
19. Beta Blockers -Drugs ending in "olol" atenolol-Block the sympathetic nervous system(beta-adrenergic receptors) to slowheart, reduce its pumping force andlower BP.
20. Beta-blockers -Reduces stimulation and slows theheart-Side effects may include dizziness,hypotension and bradycardia.-Hold them if Bp is >60 Bpm
21. Blood ChemistryTests related toCardiovascularSystem
-Na+control of fluid volume-K+major role in cardiac electrophysiologicfunction*Hypokalemia*Hyperkalemia-Ca++ *neuromuscular activity andautomaticity*Hypocalemia*Hypercalemia-FBS or Hemoglobin A1C
22. Blood PressureClassification
Systolic DiastolicNormal
-
31. Classification ofValvular HeartDisease
-Stenosed valves Narrow opening that reduces the flowof blood from one chamber to the next.-Insufficient (incompetent) valveImproper closure of valve that allowsblood to regurgitate (flow backward)and returns to the chamber it camefrom.-ProlapseStretching of an atrioventricular heartvalve leaflet into the atrium duringsystole.
32. Coronary ArteryDisease
-There are no symptoms in 80% ofpatients-Must be a critical deficit in bloodsupply to heart in proportion todemands for oxygen and nutrients-Most common manifestation ofmyocardial ischemia is acute onset ofchest pain.
33. Coronary ArteryDisease symptoms
-Continuum related to location anddegree of vessel obstruction-Angina pectoris-Myocardial infarction-Heart failure-Sudden cardiac death.
34. Diagnostic profilefor acute MI
Plasma analysis of key cardiac iso-enzymes and other bio-markers:-CK and CK-MB-Myoglobin-Troponin T and I
35. Digitalis: digoxin(Lanoxin)
-Increases force of myocardialcontraction and slows conductionthrough AV node-CO is increased and body is betterperfused.-Small therapeutic window.
36. Diuretics -Loop diuretics Lasix (furosemide)-Thiazide diuretics (hydrochlorothiazide, hydrothiazide)-Potassium sparing diuretics.
37. Dysrhythmias Life threatening (Ventricledysrhytmias)-Ventricular tachycardia (Flush back)-Ventricular fibrillation (quiver)-Asystole (no heart activity)(Decrease cardiac output and tissueperfusion)
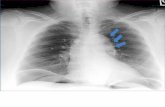
38. Electrocardiogram(ECG)
-A graphic study of the electricalactivity of the myocardium to determinetransmission of cardiac impulsesthrough the muscles/conduction tissue.
39. EndocarditisNursingManagement
-Monitor temperature-Assess heart sounds-Signs and symptoms of embolization andorgan damage.
40. EndocarditisNursingManagementand Process.
-Diagnosing and treating group A beta-hemolytic streptococcal pharyngitis(common in school-age children) canprevent rheumatic fever and rheumatic heartdisease-Teaching people to recognize and seekmedical treatment for streptococcalpharyngitis.
41. EndocarditisSymptoms
-Fever (intermittent/absent)-Heart murmur-Headache-Small, painful nodules on fingers.
42. ExerciseCardiacStress Test
-Walking on a treadmill - usually 9 to 12minutes with increases in speed and inclineof treadmill every 2 to 3 minutes based uponprotocol used-Exercise bicycle - with increase inresistance at set intervals.
43. ExerciseCardiacStress TestInterventions
-Pt. needs to fast for 4 hours before test andavoid stimulants (tobacco, caffeine)-Some cardiac medications (beta adrenergicblockers) may be held-Equipment to be used and need to have anIV -Symptoms to report during testing.
44. Heart FailureDiagnostic
-B-type natriuretic peptide (BNP) is keyindicator of Heart Failure-Low pulse oximetry readings
-
47. HypertensionAssessment andDiagnosticEvaluation
-Retinal examination-Urinalysis for renal damage-Blood Chemistry*Electrolytes*FBS*Total and HDL cholesterol levels*BUN or Creatinine- 12 lead EKG-Chest x-ray.
48. HypertensionClinicalManifestations
-Usually NO symptoms other thanelevated blood pressure-Symptoms seen related to vascularand organ damage*Left ventricular hypertrophy*Heart failure*Renal failure *Stroke- Are seen late and are serious.
49. Improve RespiratoryFunction
-Administer O2 and monitorsaturations levels-T, C, DB-Prevent fluid overload in lungs
50. Left Sided HeartFailure
-Blood backs up into the pulmonarysystem causing pulmonarycongestion or fluid in the lungs.-Cardiac output is decreased whichmeans less blood enters the systemiccirculation-The body than does not receiveoxygen and nutrients.
51. Left Sided HeartFailure ClinicalManifestation
-Pulmonary congestion/edema*Dyspnea*Orthopnea*PND paroxysmal nocturnal dyspnea*Cough that is dry at first but thanbecomes moist over time and issometimes blood tinged*Crackles (Dry cough).
52. Left Sided HeartFailure ClinicalManifestation (2)
-Decreased cardiac output*Decreased oxygen saturation*Cerebral hypoxia/ Confusion*Oliguria (decreased urine output)*Weak pulses*Fatigue and weakness-Clinical Manifestations of HeartFailure may not be detected until thedisease is advanced
53. LifestyleModificationsHypertension
-Weight reduction.-Dietary approaches.-Dietary sodium reduction.-Physical activity.-Moderation of alcoholconsumption.
54. MedicalManagementHypertension
-SBP 140 or less-DBP 90 or lessPersons with diabetes mellitus or chronicrenal disease have a lower goal pressureof 130/80.
55. MI -Unrelieved ischemia of > 15 minutescauses irreversible damage to themyocardium (necrosis)-Area of the myocardium is permanentlydestroyed.
56. MI Othertherapies
-Oxygen-Bed rest-Continuous ECG monitoring-Evaluate for indications for reperfusiontherapy*Percutaneous coronary intervention*PTCA -Percutaneous Transluminal *Coronary Angioplasty *Coronary Artery Stent Placement*Artherectomy*Thrombolytic therapy.
57. MIPharmacologicalTherapy
-ASA 162-325 mg-Nitroglycerin-Morphine-Beta-blocker-Heparin-ACE inhibitor within 24 hours (acts onBP).
58. MI Symptoms -Shortness of breath, indigestion, nausea,anxiety-Cool, pale and moist skin.-Symptoms cannot always bedistinguished .
59. Modifiable RiskFactors:EssentialHypertension
-Obesity-Sedentary life style-Alcohol-Stress-Smoking -High sodium diet-Oral contraceptives-Decreased Estrogen-Elevated serum cholesterol
60. Myocarditis -Uncommon infection of the heart musclecaused by viral, bacterial or fungalinfection-Infection causes immune response whichdamages heart muscles causing dilationof heart and degeneration of heartmuscles-Presenting symptoms are flu-like-Organism must be identified and thentreated.
-
61. MyocarditisNursingManagement
-Treat infections-Rest-Fluids-Monitor for dysrhythmias (SOB, Skips)-Monitor for heart failure.
62. Non-modifiableRisk Factors:EssentialHypertension
-Family history-Age-Gender-Race & ethnicity
63. NursingImplications:ACE
-Hypotension reversed by fluidreplacement-Used with thiazide diuretic anddigoxin.
64. NursingImplications:ALDO ANT
-Rebound htn is common (educatecontinue taking to avoid rebound)-SE: dry mouth, drowsiness dizziness,nasal congestion, severe depression,constipation, fatigue, headache,sleepiness.
65. NursingImplications:ARB
-Monitor for hyperkalemia.
66. NursingImplications BetaBlockers
-Check heart rate (60) and BP beforegiving-May cause mental depression-Indicated for patients with stable andsilent angina-Avoid sudden discontinuation.
67. NursingManagement andProcess
-The diagnosis-Progressive nature of the disease-Teatment plan-Signs and symptoms of heart failure-To report new symptoms or changes in-symptoms to the health care provider -The need for prophylactic antibiotictherapy before any invasive procedure.
68. NursingResponsibility forcardiaccatheterization
-Prior to procedure:*Confirm consent has been signed*NPO 8-12 hours*ECG monitoring*Patent IV line*Resuscitation equipment on hand-After procedure:*Assess site for hematoma, circulationto affected extremity, ECG, HR*Bed rest for 2-6 hours with leg straight*Monitor for chest pain.
69. PercutaneousCoronaryIntervention
-Percutaneous transluminal coronaryangioplasty (PTCA) is used to open blockedcoronary arteries and resolve ischemia-Balloon, at tip of catheter, is inflated andplaque is pushed against the wall-Stent may be placed over the balloon andleft in place-Fluoroscopy is used to guide catheter.
70. Pericarditis -Inflammation of the pericardium(membranous sac that surrounds heart)-Has multiple causes : bacteria, virus,fungus, parasites, renal failure, MI, chesttrauma.
71. PericarditisNursingManagement
-Assess and treat pain-Bed rest to promote healing-Elevate HOB and lean forward to decreasepain and dyspnea -Education and reassurance that the pain isnot a heart attack-Monitor for heart failure.
72. PericarditisSymptoms
-Creaky or scratchy friction rub heard mostclearly at the left lower sternal border-Chest pain that becomes worse when thepatient takes a deep breath or lie down-May be relieved when patient leansforward and/or is in sitting position.
73. PeripheralVascularDisorders Symptoms
Depends on the organ or tissue affected-Intermittent claudication - hallmarkAching/cramping that occurs with samedegree of exercise or activity and relievedwith rest-Pain at rest.
74. PharmacologicCardiac StressImaging
-Patients who cannot walk on treadmill oruse exercise bike may undergopharmacologic stress test with imaging-Vasodilation of coronary arteries withmedications mimics the effect of exercise
75. Process for thePatient withHypertension
Assessment-Proper measuring of BP at frequentintervals -Assess apical and peripheral pulse-Monitor electrolytes and instruct patient onelectrolyte replacement therapy ifapplicable.
76. Promoteadequatetissueperfusion
-Bedrest -Oxygen therapy.
77. PulmonaryEmbolismSymptom
-SOB
-
78. Raynaud's Disease -Intermittent arterial vaso-occlusion, usually of the fingertipsor toes-Brought on by trigger such as coldor stress-Often occurs in young women.-White hands.
79. Reduce venous stasisand preventulcerations
-Avoid prolong standing, sitting orcrossing the legs-Elevation of legs above the heart-Sleep with the foot of the bedelevated-Use of elastic compressionstockings
80. Relieving Pain andOtherSigns/Symptoms ofIschemia
-Administration of medications-Oxygen therapy-Bed rest with elevation of headand torso.
81. Report immediately tothe physician or clinic
-Weight gain of more than orequal to 2-3 lbs in 1 day or 5 lb in 1week-Loss of appetite-Unusual shortness of breath withactivity-Swelling of ankles, feet orabdomen-Persistent cough-Development of restless sleep;increase in the number of pillowsneeded to sleep
82. Right Sided HeartFailure
-Blood backs up into the systemiccirculation.-Fluid accumulates behind thechambers that fail first.-Congestion occurs in the liver,gastrointestinal tract andperiphery (arms and legs).
83. Right Side HeartFailure ClinicalManifestation
-Pronounced jugular neck vein(JVD).-Pitting edema(Peripheral/Perineal/sacral).-Ascitis (Pain).-Hepatomegaly.-Weight gain. (2-3 lbs in 1 day or 5lb in 1 week)-Increase urine output.-Frequent nocturnal urination.
84. Stable Angina -Infrequent predictable andconsistent pain -Occurs on exertion, by apredictable degree of exercise-Treatable with rest ornitroglycerides or both.
85. Stage 2 HTNwithoutcompellingindications
-Continue lifestyle modifications-Usually on 2-drug combination-Thiazide diuretic (HCTZ) and ACE-1/ARB/BB/CCB
86. Step CareManagement ofHypertension
-Step 1 Lifestyle modifications (Diet, exercise)
87. Therapies HeartFailure
-Nutritional Therapy*Low-sodium (2-3 g/day) diet *Avoid excessive fluid intake-Oxygen therapy*May become necessary as heart failureprogresses *Based on patient SpO2.
88. ThrombosisClinicalManifestations
-Edema and swelling.-Warm skin and erythema.-Tenderness.-Homans is an unreliable sign.
89. Types of Angina -Stable -Unstable.
90. Unstable Angina -Triggered by an unpredictable degree ofexertion or emotions-May occur at rest and last longer thanstable angina-Increasing frequency and severity overtime that is not relieved by rest andNTG.
91. Use ofNitroglycerine
-When pain occurs instruct patient to Stop activities and rest-Use NTG *Repeat every 5 minutes if pain is notrelieved*Call 911 if the pain is not relieved in 15minutes.
92. Valvular HeartDisease
Occurs when valves are compromisedand do not open and close properly.
93. Varicose Veins -Abnormally dilated, tortuous,superficial veins caused by incompetentvenous valves-Impaired blood return due toincompetent valves-Seen more frequently in women and inpeople whose occupations requireprolonged standing.
94. Varicose VeinsClinicalManifestations
-Dull aches, muscle cramps, increasedmuscle fatigue, ankle edema andheaviness of the legs-Cause of chronic venous insufficiency-More susceptible to injury andinfections.
-
95. Varicose Veins Nursing Process -Instruct patient to avoid standing for extended periods of time-Elevate legs when seated-Compression stocking should be worn-Weight reduction-ExerciseWeight reduction, if factor
96. Venous Stasis -Results from obstruction of venous valves in legs or a reflux of blood throughthe valves.
97. Venous Thrombosis Causes -Endothelial damage (Surgery)-Venous stasis (rest)-Altered or hyper-coagulation (surgery, hepatic diseases, Birth control pills)
98. Venous Ulcers -Feet and ankles are edematous-Ulcerations are in area of the medial or lateral malleolus-Typically are large, superficial and highly exudative-Superficial (Not Deep)
99. Women's hearts are: Smaller and have smaller cardiac arteriesCardiac arteries occlude more easily resting rate stroke volume ejection fraction
100. Women tend to have atypical signs/symptomsof MI:
-Shoulder/upper back pain-SOB-Fatigue.
Cardiovascular Nursing