Carbon monoxide and cyanide poisoning
-
Upload
krishna-vasudev -
Category
Health & Medicine
-
view
94 -
download
7
Transcript of Carbon monoxide and cyanide poisoning
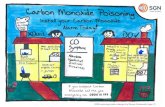
- 1. CARBON MONOXIDE POISONING
- 2. Carbon Monoxide (CO) An odorless, colorless, tasteless gas Results from incomplete combustion of carbon- containing fuels Gasoline, wood, coal, natural gas, propane, oil, and methane Affects 40 50,000 Americans annually who need to seek care Kills an additional 6,000 persons annually in the USA CO is the #1 cause of poisoning in industrialized countries
- 3. Sources of Carbon Monoxide any combustible item Homes Cigarette smoke House fires Automobile exhaust fumes Worksites Including fumes from propane-powered equipment like forklifts Commercial structures Smoke from charcoal-fired cook stoves & ovens
- 4. Sources contd Heat provided to homes Gas-fueled heaters Wood burning stoves Indoor stoves Camp stoves Gas-powered generators Recreational environments Recreational vehicles Boat exhaust fumes
- 5. What Effect Does Carbon Monoxide Have on Hemoglobin? Hemoglobin molecules each contain four oxygen binding sites Carbon monoxide binds to hemoglobin This binding reduces the ability of blood to carry oxygen to organs Hemoglobin occupied by CO is called carboxyhemoglobin Body systems most affected are the cardiovascular and central nervous systems
- 6. Effects of Carbon Monoxide Oxygen cannot be transported because the CO binds more readily to hemoglobin (Hgb) displacing oxygen and forming carboxyhemoglobin Premature release of O2 prior to reaching distal tissue leads to hypoxia at the cellular level Inflammatory response is initiated due to poor and inadequate tissue perfusion Myocardial depression from CO exposure Dysrhythmias, myocardial ischemia, MI Vasodilation from increased release of nitric oxide; worsening tissue perfusion and leading to syncope
- 7. Half-life of Carbon Monoxide Half-life time required for half the quantity of a drug or other substance to be metabolized or eliminated CO half-life on 21% room air O2 4 - 6 hours CO half-life on 100% O2 80 minutes CO half-life with hyperbaric O2 22 minutes
- 8. CO Levels Fresh air 0.06 - 0.5 ppm Urban air 1 300 ppm Smoke filled room 2 16 ppm Cooking on gas stove 100 ppm Actively smoking 400 500 ppm cigarette Automobile exhaust 100,000 ppm
- 9. Expected Carboxyhemoglobin Levels Non-smokers 5% Smokers up to 10% 5 6% for a 1 pack per day smoker 7 - 9% for a 2-3 pack per day smoker Up to 20% reported for cigar smokers Urban commuter 5%
- 10. CO Poisoning Symptoms are often vague, subtle, and non-specific; can easily be confused with other medical conditions; Flu nausea, headaches Food poisoning - nausea Cardiac and respiratory conditions shortness of breath, nausea, dizziness, lightheadedness CO enters the body via the respiratory system Poisoning by small amounts over longer periods of time or larger amounts over shorter time periods
- 11. Exposure Limits For CO OSHA 50 ppm as an 8-hour-weighted average NIOSHA 35 ppm as an 8-hour-weighted average Set lower than OSHA based on cardiac effects of CO
- 12. Symptoms of CO Poisoning Related to Levels and Exposure Time 50 ppm no adverse effects with 8 hours of exposure (OSHA limit) 200 ppm mild headache after 2-3 hours 400 ppm serious headache and nausea after 1-2 hours (life-threatening >3 hours) 800 ppm headache, nausea, dizziness after 45 minutes; collapse and unconsciousness after 2 hours; death within 2-3 hours 1000 ppm loss of consciousness after 1 hour
- 13. Levels & Exposure Time Contd Source: NFPA Fire Protection Handbook, 20th Edition 1600 ppm headache, nausea, dizziness after 20 minutes; death within 1 hour 3200 ppm headache, nausea, dizziness after 5-10 minutes; collapse and unconsciousness after 30 minutes; death within 1 hour 6400 ppm headache, dizziness after 1-2 minutes; unconsciousness and danger of death after 10 -15 minutes 12,800 ppm immediate physiological effects; unconsciousness and danger of death after 1-3 minutes
- 14. Carbon Monoxide Absorption Dependent upon: Minute ventilation Amount of air exchanged in the lungs within one minute Duration of exposure The longer the exposure, the more the absorption Concentration of CO in the environment The higher the concentration, the greater the toxicity Concentration of O2 in the environment The lower the O2 concentration to begin with, the faster the symptoms will develop higher altitudes closed spaces
- 15. CO Levels with Related Signs and Symptoms >5% - mild headache 6-10% - mild headache, SOB with exertion 11-20% - moderate headache, SOB 21-30% - worsening headache, nausea, dizziness, fatigue 31-40% - severe headache, vomiting, vertigo, altered judgment 41-50% - confusion, syncope, tachycardia 51 60% - seizures, shock, apnea, coma
- 16. Signs and Symptoms CO Poisoning Carboxyhemoglobin levels of 60% Fatal Death Cherry red skin is not listed as a sign An unreliable finding
- 20. Increased Risks Health and activity levels can increase the risk of signs and symptoms at lower concentrations of CO Infants Women who are pregnant Fetus at greatest risk because fetal hemoglobin has a greater affinity for oxygen and CO compared to adult hemoglobin Elderly Physical conditions that limit the bodys ability to use oxygen Emphysema, asthma Heart disease Physical conditions with decreased O2 carrying capacity Anemia iron-deficiency & sickle cell
- 21. CDC Diagnostic Criteria Suspected CO exposure Potentially exposed person but no credible threat exists Probable CO exposure Clinically compatible case where credible threat exists Confirmed CO exposure Clinically compatible case where biological tests have confirmed exposure
- 22. Patient Assessment Continuously monitor SpO2 and SpCO levels Remember that SpO2 may be falsely normal If EMS has used a CO-oximeter, findings to be reported to the ED staff Generally, results >3% indicate suspicion for CO exposure in non-smoker Cardiac monitor 12 lead EKG obtained and transmitted to ED
- 23. Pulse Oximetry Device to analyze infrared signals Measures the percentage of oxygenated hemoglobin (saturated Hgb) Can mistake carboxyhemoglobin for oxyhemoglobin and give a false normal level of oxyhemoglobin Never rely just on the pulse oximetry reading; always correlate with clinical assessment
- 24. Treatment CO Poisoning Increasing the concentration of inhaled oxygen can help minimize the binding of CO to hemoglobin Some CO may be displaced from hemoglobin when the patient increases their inhaled oxygen concentrations Treatment begins with high index of suspicion and removal to a safer environment Immediately begin 100% O2 delivery
- 25. Treatment CO Poisoning Guidelines from different sources may vary when to initiate treatment based on SpCO levels Report levels to the ED MD Remember >5% in non-smokers is abnormal Treatment levels vary significantly If you do not have a CO-oximeter to use, maintain a heightened level of suspicion and base treatment on symptoms Monitor for complications Seizures Cardiac dysrhythmias Cardiac ischemia
- 26. CO Poisoning and CPAP CPAP could assist in fully oxygenating hemoglobin If considered, EMS to contact Medical Control for permission to use CPAP The ECRN would need to relay report to the ED MD to obtain an order for CPAP
- 27. Long Term Effects CO Exposure Hypoxemia follows CO exposure Effects of hypoxemia from CO exposure is dependent on presence of underlying diseases Hypoxemia can cause the formation of free radicals dangerous chemicals
- 28. Long Term Cardiovascular Effects Myocardial injury from hypoxia and cellular damage Pump failure Cardiac ischemia Later development cardiovascular complications Premature death especially if myocardial damage at the time of initial exposure Factors increasing myocardial injury risk Male gender History hypertension GCS 10% Nitrites can also cause hypotension
- 42. Signs and Symptoms Methemoglobinemia 1-3% SpMet normal, asymptomatic 3-15% SpMet slight grayish-blue skin 15 20% - asymptomatic but cyanotic 25 50% - headache, dyspnea, confusion, weakness, chest pain 50 -70% - altered mental status, delirium Methemoglobinemia is also a complication when Benzocaine (to decrease the gag reflex) is used even under normal 2 second spray time frame
- 43. Cyanokit This kit uses hydroxocobalamin A form of Vitamin B12 (cyanocobalamin) Binds with the cyanide ion Eliminated through the kidneys Preferred kit if concomitant CO and cyanide poisoning suspected Significant signs and symptoms with low CO levels Decreased cardiac output, decreased heart rate Hypotension, shock, and falling ETCO2 levels Signs & symptoms of CO and cyanide poisoning indistinguishable
- 44. Arsenic Poisoning
- 45. Arsenic in the World Arsenic is ubiquitous in the environment. It ranks 20th in abundance in the earth's crust, 14th in seawater, and 12th in the human body. 20th 14th 12th
- 46. Possible Arsenic poisoning Today, arsenic poisoning occurs through industrial exposure, from contaminated wine or moonshine, or because of malicious intent. The possibility of heavy metal contamination of herbal preparations and so-called nutritional supplements must also be considered.
- 47. Poisonous Compounds of Arsenic Arsenic oxide or Arsenic Trioxide It is the most common form of arsenic used. It is also known as White Arsenic. No taste or smell and is sparingly soluble in water. It is heavier than water by three and half times but freely floats on water.
- 48. Uses Of Arsenic Fruit sprays Sheep-dips Weed-killers Rat poisons Fly papers Calico printing Taxidermy Preserving timber and skin against white ants
- 49. Mode Of Action Arsenic interferes with cellular respiration by combining with the sulphydryl groups of mitochondrial enzymes. It particularly targets vascular endothelium leading to increased permeability, tissue edema and hemorrhage, especially in the intestinal canal.
- 50. Mode Of Action Locally it causes irritation of the mucous membranes and remotely depression of the nervous system. Arsenic also interferes with glycolysis.
- 51. Circumstances Of Poisoning It is cheap Easily obtained Colourless No smell No taste Small quantity is required to cause death. Can be easily administered with food or drink. Onset of symptoms is gradual Symptoms simulate those of Cholera. Arsenic is the most popular Homicidal poison
- 52. Circumstances Of Poisoning Disadvantages Of Arsenic: It delays putrefaction Can be detected in completely decomposed bodies. Can be found in bones, hairs and nails for several years. Can be detected in charred bones or ashes.
- 53. Signs And Symptoms 1. The Fulminant type 2. The Gastroenteric Type
- 54. The Fulminant type Massive doses of arsenic when rapidly absorbed cause death in one to three hours from shock and peripheral vascular failure. All the capillaries are markedly dilated, especially in the splanchnic area with a marked fall of blood pressure.
- 55. The Gastroenteric Type This is the common form of acute poisoning and resembles bacterial food poisoning. Symptoms usually appear half to one hour after ingestion, but may be delayed many hours especially when arsenic is taken with food. Burning and colicky pain in the esophagus, stomach and bowel occur. Intense thirst and severe vomiting which may be projectile are the common symptoms.
- 56. Signs And Symptoms Acute severe arsenic poisoning Vital signs - Tachycardia and hypotension, even shock CNS - Altered mental status, delirium, coma, and seizures (acute encephalopathy) Frequently, patients exposed to arsenic have a garlic smell to their breath and tissue fluids.
- 57. Signs And Symptoms Arsine gas exposure manifests with an acute hemolytic anemia and striking chills. Hemoglobinuria causes the urine to appear black, and the patient becomes rapidly obtunded and shocky. Shaking chills are often described in these patients. Frequently, patients exposed to arsenic have a garlic smell to their breath and tissue fluids.
- 58. Signs And Symptoms Acute exposures generally manifest with the cholera-like gastrointestinal symptoms of vomiting (often times bloody) and severe diarrhea (which may be rice-watery in character and often bloody); these patients will experience acute distress, dehydration (often), and hypovolemic shock.
- 59. Chronic toxicity is more insidious and may manifest as a classical dermatitis (hyperkeratosis with a classical "dew drops on a dusty road" appearance) Telugu Doctors.co.in
- 60. whitish lines (Mees lines) that look much like traumatic injuries are found on the fingernails. Contact dermatitis may also be induced in occupational arsenic poisoning. Arsenic dust coming into contact with the skin produces four main types of reactions: 1. Toxic 2. Eczematous 3. Combined toxic and eczematous and 4. Reactions characterized by follicular lesions. Telugu Doctors.co.in
- 61. Laboratory Studies Complete Blood Count Microcytic Hypochromic Anemia Obtain a CBC with indices and a reticulocyte. Acute hemolytic anemia is the rule with arsine exposure. Type and screen or crossmatch blood for the transfusion in patients exposed to arsine gas.
- 62. Laboratory Studies 1. Serum Magnesium 2. Serum Potassium 3. Serum Sodium 4. Serum Calcium 5. Serum Chloride Serum Electrolytes Do Serum electrolytes in patients with Diarrhea and Vomiting Telugu Doctors.co.in
- 63. Laboratory Studies Blood arsenic concentrations should not exceed 50 mcg/L. The reported half-life of arsenic in blood immediately following ingestion is in hours, while whole- body clearance may be in days or months and is apparently dose- related. Serum Electrolytes Plasma Arsenic Analyser Serum Arsenic Analysis Telugu Doctors.co.in
- 64. Laboratory Studies Urine spot test for arsenic 24-hour urine collection for total arsenic excretion Methylarsonic acid (MMA) and dimethylarsenic acid (DMA) metabolites of arsenic in the body Urine analysis Telugu Doctors.co.in
- 65. Laboratory Studies Reports of prolongation of the QT and ventricular fibrillation after acute arsenic intoxication make careful attention to cardiac status imperative. ECG Changes Telugu Doctors.co.in
- 66. Laboratory Studies Nerve conduction studies may confirm Peripheral neuropathy An abdominal radiograph may reveal the presence of radio- opaque densities Other Tests Telugu Doctors.co.in
- 67. Treatment and management Airway Breathing Circulation Pre-Hospital care Emergency Department Hemodynamic stabilization to counteract GI loses Orogastric lavage for acute arsenic poisoning Whole bowel irrigation with polyethylene glycol may be effective to prevent GI tract absorption of arsenic. Telugu Doctors.co.in
- 68. Treatment and management Dimercaprol (BAL in Oil): First-line agent for treating arsenic poisoning. May be administered to patients with renal failure. Succimer (DSMA): used only in childhood lead poisoning. Dimerval (DMPS): accepted DOC for treating most heavy metal poisonings. Chelation Agents Telugu Doctors.co.in
- 69. Treatment and management Hemodialysis is especially useful in a patient with arsenic poisoning with renal failure or with impending renal failure. Hemodialysis Telugu Doctors.co.in
- 70. THANK YOU