Broncial Asthma
description
Transcript of Broncial Asthma

BRONCHIAL ASTHMADR. HUSSEIN ALMEAMAR
MBChB, MSc, MRCP (UK)
1

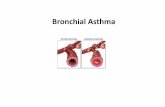
• Chronic inflammatory disorder of the airways characterized by recurrent episodes of wheezing, breathlessness, chest tightness and coughing, particularly at night and in the early morning.
Definition :
2

Prevalence:
3
age 13-14 --> 9-13%

4
currently affects 235 million people (WHO)
Prevalence:

• The pathophysiology of asthma is complex and involves the following components:
• Airway inflammation
• Intermittent airflow obstruction
• Bronchial hyper-responsiveness
pathophysiology:
5

Airway inflammation:
The inflammatory response includes mononuclear cell and eosinophil infiltration, mucus hypersecretion, desquamation of the epithelium, smooth muscle hyperplasia, and airway remodelling .
pathophysiology:
6

• Airway hyperesponsiveness --> exaggerated response to exogenous and endogenous stimuli.
• Mechanisms --> direct stimulation of airway smooth muscle and indirect stimulation by pharmacologically active substances from mediator-secreting cells such as mast cells
• The degree of airway hyperesponsiveness generally correlates with the clinical severity of asthma.
pathophysiology:
7

Aetiology:
Genetic Environmente.g. ADAM 33 on chromosome 20
e.g. the ‘hygiene hypothesis’
Theories

Triggers and causes:

• The principal symptoms of asthma are wheezing attacks, chest tightness, breathlessness and cough.
• Nocturnal Symptoms (usually worst during the night) --> highest between the hours of 4:00 am and 6:00 am
clinical features:
10

• Spirometry and Peak expiratory flow rate (PEFR).
• Spirometry : measure FEV1 and VC to identifies the obstructive defect, severity and demonstration of bronchodilators reversibility. A reduced ratio of FEV1 to FVC, when compared with predicted values, demonstrates the presence of airway obstruction.
• PEF important in demonstrating the variable air flow limitation that characterises the disease (on waking,before and after bronchodilator and before bed.
Investigations:
11
Lung function tests

12
Investigations:
The diurnal variation in PEFR is a good measure of asthma activity, assessing severity and response to treatment.

• The diagnosis of asthma is predominantly clinical and based on a characteristic history.
Supportive evidence is provided by the demonstration of variable airflow obstruction.
Diagnosis:
13

14
Diagnosis:
14
Reversibility test
Clinical history compatible with asthma plus either/or :
• FEV1 ≥ 15% increase following administration of a bronchodilator/trial of corticosteroids (Prednisolone 30 mg daily for 2 weeks
• > 20% diurnal variation on ≥ 3 days in a week for 2 week on PEF diary
• FEV1 ≥ 15% decrease after 6 mins of exercise

✴
✴
Other investigations:
✴ Blood and sputum tests: peripheral blood eosinophilia, sputum differential eosinophil count of greater than 2% .
✴ Skin tests Skin-prick tests (SPT)
✴Chest X-ray to pulmonary infiltrate of allergic bronchopulmony aspergilosis, to exclude pneumothorax in acute sever asthma
✴ Histamine or methacholine bronchial provocation test

MANAGEMENT:
16

17
Control of extrinsic factors:
• Avoid causative allergens such as pets, moulds.
• Avoid active and passive smoking
• Avoid NSAIDs, B blockers.
Diagnosis:
17
MANAGEMENT:

–Johnny Appleseed
“Type a quote here.”
18
Occasional symptoms.Less frequent than
daily
Daily symptoms

Introduction:
19
Levels of asthma control (according to GINA):
MANAGEMENT:
In the past 4 weeks, has the patient had:Daytime symptoms more than twice/week? Any night waking due to asthma? Reliever needed more than twice/week? Any activity limitation due to asthma?
Uncontrolled = none of these Partly controlled = 1-2 of these Uncontrolled = 3-4 of these

Medications:
20
Short-acting relievers Inhaled β2 agonists (e.g. salbutamol , terbutaline) Long-acting relief/disease controllers
Inhaled long-acting β2 agonists (e.g. salmeterol, formoterol) Inhaled corticosteroids (e.g. beclometasone, budesonide, fluticasone) Compound inhaled salmeterol and fluticasone Sodium cromoglycate Leukotriene modifiers (e.g. montelukast)
Other agents with bronchodilator activity Inhaled antimuscarinic agents (e.g. ipratropium, oxitropium) Theophylline preparations Oral corticosteroids (e.g. prednisolone)
Steroid-sparing agents

β2-Adrenoceptor agonists
★Potent bronchodilators (relax the bronchial smooth muscle). ★Effective in relieving symptoms but do little for the underlying airways inflammation.
Short-acting β agonists (SABAs) : salbutamol, terbutaline
• Alone for Mildest asthmatics with intermittent attacks.• At any step, as and when required from step 1 to step 5
long-acting β2-adrenoceptor agonists (LABAs): salmeterol or formoterol
• Poorly controlled asthmatics on standard doses of inhaled steroids
Prognosis:
21
Medications:

Introduction:
22
LABAs :Improve symptoms and lung function and reduce exacerbations in patients. Should never be used alone but always in combination with an inhaled corticosteroid. Increasingly.
Ex of fixed-dose combinations with corticosteroids (LABA+ ICS)
formoterol/budesonide salmeterol/fluticasone
Medications:

Inhaled corticosteroids (ICS):
Indication: all asthma patients with regular persistent symptoms even mild symptoms, (from step 2 upwards).
• Ex: Beclometasone, budesonide, fluticasone, mometasone and triamcinolone.
• Only 10% and 25% of the ICS will reach the airways depending on inhaler technique and aerosol device.
• S.E of ICSs: oral candidiasis, and hoarseness. systemic side effects are less likely than with oral steroids but can occur with high-dose inhaled corticosteroids.
Introduction:
23
Medications:

Introduction:
24
Medications:

Introduction:
25
Antimuscarinic bronchodilators
mainly indicated during asthma exacerbations.
EX: ipratropium bromide
Leukotriene modifiers, Ex: Montelukast (Singulair®)
Targets one of the principal asthma mediators by inhibiting the cysteinyl LT
receptor.
LTRAs should be tried in any patient who is not controlled on low to medium doses of inhaled steroids.
A 4-week trial of LTRA therapy is recommended before a decision is made to continue or stop.
Medications:

Introduction:
26
Omalizumab
Its a monoclonal antibody--> bind to IgE
Indication in asthma according to NICE:
Confirmed allergic IgE mediated asthma as an add on for patients aged 6 and above if they needed continuous or frequent oral corticosteroids (4 or more courses in the previous year)
Most important side effects
- Local injection site side effects
- Allergy and anaphylaxis (should monitor the patient after injection and prepare anaphylaxis medications)
Dose
According to weight and IgE level
- Subcutaneous injection every 2-4 weeks
Efficacy of the drug should be monitored for all patients
Is there a new medication?
Cost around the 1000 usd/month

During the course of asthma , patient may experience exacerbation which characterised by increase in the symptoms and deterioration in lung function.
Most common causes of exacerbations:
• viral infections.
• moulds.
• pollens.
• air pollution.
Exacerbations of asthma:
27

Exacerbations of asthma:
28

Short courses of ‘rescue’ oral corticosteroids (prednisolone 30–60 mg daily) for two weeks are often required to regain control.
Indications for ‘rescue’ courses include:
symptoms and PEF progressively worsening day by day
sleep disturbance by asthma.
diminishing response to an inhaled bronchodilator .
severe symptoms require treatment with nebulised or injected bronchodilators.
Introduction:
29
Management of mild to moderate exacerbations:
Exacerbations of asthma:

Management of acute severe asthma:
30
1. assessment of the patient. 2.Oxygen 40–60% is given. 3.The PEFR, O2 saturation. 4.Administer repeat salbutamol 5 mg + ipratropium bromide 500 µg
by oxygen-driven nebuliser
5.Hydrocortisone 200 mg i.v. is given 4-hourly for 24 hours.
6.Prednisolone is continued at 60 mg orally daily for 2 weeks.

31
7.Arterial blood gases are measured; if the PaCO2 increased, ventilation may be required.
8.A chest X-ray is performed to exclude pneumothorax.
9.One of the following intravenous infusions is given if no improvement is seen:
IV magnesium sulphate 1.2–2.0 g over 20 mins, or
aminophylline 5 mg/kg loading dose over 20 mins followed by a continuous infusion at 1 mg/kg/hr.
10. No improvement – urgent; transfer to ITU
Management of acute severe asthma….

• The outcome from acute severe asthma is generally good. Death is fortunately rare.
• Although asthma often improves in children as they reach their teens, the disease frequently returns in the 2nd, 3rd and 4th decades.
• Airways remodelling accelerates the contribute to the decline in lung function over time.
Prognosis:
32

References:
33

34
Thank you