Brainstem Glioma in Adults
Transcript of Brainstem Glioma in Adults
Brainstem gliomas in adults ContributorsHerbert B Newton MD, author. Dr. Newton, Director of the Division ofNeuro-oncology at Ohio State University, has received honorariumsfrom Schering-Plough and UCB Pharma for speaking engagements andfrom Genentech for service on an advisory board. Edward J Dropcho MD, editor. Dr. Dropcho of Indiana UniversityMedical Center received an honorarium from Merck for a speakingengagement and a consulting fee from Genentech as a member of areview panel.
Publication datesOriginally released February 20, 1996; last updated November 12,2010; expires November 12, 2013
SynonymsMedullary glioma; Midbrain glioma; Pontine glioma
Key points
• Brainstem gliomas are much less common in adults than in children. • Brainstem gliomas are a very heterogeneous group of tumors, butare often quite aggressive and difficult to treat, with relatively shortsurvival times. • Surgical resection of brainstem gliomas can be performed inselective focal tumors. For more diffuse tumors, resection isimpossible, and a biopsy is preferred. In many cases of diffuse pontinetumors, MRI can be diagnostic. • Radiotherapy is always necessary for high-grade tumors, but maynot be needed for fully resected low-grade tumors. In general,radiotherapy is required for most brainstem gliomas. • Chemotherapy has minimal activity against most high-gradebrainstem gliomas, but it may be helpful in less aggressive tumortypes.
Historical note and nomenclature
The earliest descriptions of brainstem tumors in the literature weremade in the 1930s (Buckley 1930; Gibbs 1932; Hare and Woolf 1934;Bailey 1935). In a review of 1737 verified brain tumors operated on byHarvey Cushing, Buckley found 25 located within the pons, the majorityof which were astrocytomas (Buckley 1930). Gibbs noted thatbrainstem tumors were most common in children and estimated thatthe comparative incidence in adults was only 10% (Gibbs 1932). A
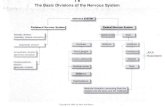
Folder Path
Neurology > Neuro-oncology > Tumors bytissue type > Braintumors > Primary braintumors in adults >Intraaxial brain tumors> Gliomas > Brainstemgliomas in adults
Quick Reference
Sections of Summary
- Historical note andnomenclature
- Clinical manifestations
- Clinical vignette
- Etiology
- Pathogenesis andpathophysiology
- Epidemiology
- Prevention
- Differential diagnosis
- Diagnostic workup
- Prognosis andcomplications
- Management
- Pregnancy
- Anesthesia
- ICD codes
- OMIM
Supplemental Content
- Associated disorders
- Related summaries
- Differential diagnosis
- Demographics
References
- References cited
Related Items
Illustrations
- Brainstem glioma (01)
- Brainstem glioma (02)
- Brainstem glioma (03)
- Brainstem glioma (04)
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
1 of 57 03/31/2011 12:46 PM
review by Hare and Woolf of 432 pediatric brain tumors seen at theNeurological Institute of New York included only 7 tumors of thebrainstem (Hare and Woolf 1934). In a study evaluating diffuse pontinegliomas in children, Bailey was one of the first authors to drawattention to the high frequency of misdiagnosis in this population(Bailey 1935). Guillain and colleagues and Globus and colleagues werethe first to document in detail brainstem tumors affecting the course ofthe aqueduct of Sylvius (Guillain et al 1936; Globus et al 1945). In alater review, Guillain was one of the first to document the behavior ofexophytic brainstem tumors, in a review of 250 intracranial neoplasms(Guillain et al 1945). The first author to study a population of adultpatients with brainstem gliomas was White, who evaluated a series of44 patients accumulated over 31 years at the Neurological Institute inNew York (White 1963). The mean age of the patients was 42 years(range 17 to 68 years); most of those studied pathologically hadastrocytic tumors of various grades. The clinical presentation andcourse of patients in this adult brainstem glioma series was similar to acomparable series of pediatric patients studied earlier at theNeurological Institute.
Clinical manifestations The clinical evolution and neurologic findings of adult patients withbrainstem gliomas are similar to those seen in children and adolescents(White 1963; Tokuriki et al 1986; Maria et al 1993a; Freeman andFarmer 1998; Selvapandian et al 1999; Donaldson et al 2006). Thelength of time from onset of symptoms to diagnosis ranges from 2 to10 months in most cases (median 4 to 5 months) and depends on thelocation of the tumor within the brainstem, the severity of initialsymptoms, and the rapidity of progression of disease. In general, themost common initial neurologic complaints consist of gaitabnormalities, visual disturbances, weakness, and headache (White1963; Tokuriki et al 1986; Grigsby et al 1989b; Packer et al 1992;Maria et al 1993a; Schild et al 1998; Selvapandian et al 1999;Guillamo et al 2001). Gait disturbance occurs in 40% to 80% ofpatients and is caused by weakness or spasticity from pyramidal tractdysfunction, ataxia, or a combination of these factors. In the study byWhite, 77% of an adult cohort of 44 patients complained of gaitdisturbance, and in the study by Tokuriki and colleagues, 42% of adultpatients had a similar complaint (White 1963; Tokuriki et al 1986).Visual disturbances, which develop in 20% to 70% of patients, usuallymanifest as diplopia (horizontal more common than vertical). In thestudy by White, diplopia was the second most common complaint(White 1963). Headache and focal weakness develop in 15% to 55% ofadult patients (White 1963; Tokuriki et al 1986; Grigsby et al 1989b).The headaches can be caused by several mechanisms, includingexpansion of the brainstem with traction on surrounding meninges andvarying degrees of hydrocephalus. These headaches often occur in the
- Brainstem glioma (05)
- Brainstem glioma (06)
- Brainstem glioma (07)
- Brainstem glioma (08)
- Brainstem glioma (09)
- Brainstem glioma (10)
- Brainstem glioma (11)
- Brainstem glioma (12)
- Brainstem glioma (13)
Patient Handouts
- Brain anatomy
- Brain basics
- Brain tumors
- Brain tumors:symptoms anddiagnosis
- Brain tumors: tumortypes
Web Resources
Clinical Trials
- NIH: Gliomas
Google Scholar
- Other articles on thistopic
PubMed
- Other articles on thistopic
About Links
- About Web Resources
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
2 of 57 03/31/2011 12:46 PM
suboccipital region, but their location can vary and may extend into theupper cervical area. In some patients, there may be a periorbitalcomponent of headache pain. Focal weakness can involve the face aswell as 1 or more limbs and is usually asymmetric. Other commonsymptoms that developed in 15% to 40% of patients includeddysarthria, focal numbness of the face or body, dysphagia, nausea andemesis, hearing loss, vertigo, tinnitus, and personality changes (White1963; Tokuriki et al 1986; Schild et al 1998; Selvapandian et al 1999).Dysarthria developed in 40% of patients in the study by White and wasusually caused by disturbance of cerebellar function or corticobulbarpathways. Focal numbness was described by 35% of patients andranged from hemisensory loss to numbness in 1 section of a limb.Dysphagia was a complaint in 10% to 30% of patients. The level ofswallowing dysfunction can vary from slight difficulty handling liquids orsolids to gross aspiration. Similar to other brain tumor patients, thisgroup may also underestimate their level of swallowing difficulty(Newton et al 1994). Nausea, emesis, and other related symptomssuch as gastroesophageal reflux were present in 10% to 30% ofpatients and, in rare cases, can be the sole presenting complaint(White 1963; Wood et al 1985; Tokuriki et al 1986; Mahony et al 1987;Frank et al 1989; Grigsby et al 1989b; Mann et al 1998). Thesesymptoms are probably caused by tumor-related compression of thevomiting center in the floor of the fourth ventricle, nucleus ambiguus,and dorsal vagal motor nucleus (Frank et al 1989; Mann et al 1998). Itis not uncommon for patients with this type of "gastrointestinal"presentation to be extensively worked up for gastrointestinal problems(eg, barium swallow, upper gastrointestinal series, endoscopy), oftendelaying the necessary neurologic evaluation and diagnosis. Treatmentof the tumor may result in improvement of these "gastrointestinal"symptoms (Wood et al 1985; Frank et al 1989). Mann and colleaguesreported a 30-year-old man who developed unremitting emesis over a21-month period (Mann et al 1998). A complete gastrointestinal workupwas negative and neurologic function was normal. An MRI scanrevealed a small enhancing brainstem tumor in the low midbrain. Theemesis responded dramatically to dexamethasone. Alterations inpersonality are well documented in children with brainstem gliomas andcan occur in adults as well; they were present in 15% to 18% of thepatients studied by White (White 1963; Packer et al 1992; Maria et al1993a). At the time of diagnosis, the most common neurologic signs ofbrainstem gliomas in adults are pyramidal tract and cerebellardysfunction, cranial nerve palsies, nystagmus, and gait difficulty (White1963; Tokuriki et al 1986; Grigsby et al 1989b; Packer et al 1992;Maria et al 1993a; Schild et al 1998; Selvapandian et al 1999;Guillamo et al 2001). In 65% to 75% of patients, pyramidal tractdamage is noted, with contralateral weakness in an upper motor neuron
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
3 of 57 03/31/2011 12:46 PM
pattern (White 1963; Tokuriki et al 1986). Over half of these cases willhave hemiparesis or hemiplegia; monoparesis and tetraparesis aremuch less common. Two thirds of all patients have associated extensorplantar responses and asymmetric reflexes. Cerebellar involvementmanifests as gait ataxia, limb dysmetria, or dysarthria in 65% to 80%of patients, most often caused by damage to corticopontocerebellarpathways or the cerebellar peduncles (White 1963; Tokuriki et al1986). Cerebellar dysfunction contributes to the high incidence ofnystagmus in this population and is noted in approximately 80% of allpatients (Miller 1988). The nystagmus is usually horizontal (65% to70%) and gaze-evoked, less often during primary position.Infrequently, patients have vertical or rotary nystagmus. Cranial nerve signs occur in the majority of patients (White 1963;Tokuriki et al 1986). In general, abnormalities of the lower cranialnerves (cranial nerves VIII through XII) are more common in adultsthan children and are usually caused by medullary tumors (Tokuriki etal 1986). The most frequent cranial nerve sign is palsy of cranial nerveVII, manifested by facial weakness in 50% to 80% of patients. Facialweakness is usually unilateral, but can be bilateral (5% to 7% ofcases). Dysfunction of cranial nerves V (sensory), VI, IX, and X arenext most common, each occurring in 45% to 55% of patients. Facialsensory loss is ipsilateral and variable in severity and can involve anyor all of the trigeminal divisions depending on the region of tumorgrowth. Bulbar dysfunction caused by palsy of cranial nerves IX and Xcan range from mild palatal weakness to frank dysphagia, dysarthria,and aspiration. Decreased hearing is found in 40% to 45% of patientsand can be caused by disturbance of the cochlear nuclei, trapezoidbody, or other structures along the cranial nerve VIII pathways.Dysfunction of cranial nerves III, V (motor), XI, or XII can be noted in20% to 30% of patients, whereas palsy of cranial nerve IV is rare.Other neuro-ophthalmological cranial nerve signs include papilledema,gaze paralysis (mainly horizontal), and anisocoria, each noted inapproximately 25% of patients in the study by White (White 1963).Disturbances of sensation are found in 35% to 55% of patients andusually present as a hemisensory deficit. Unusual or rare neurologic signs and symptoms that may seemunrelated to a brainstem neoplasm can develop, such as isolatedinability to sneeze, unilateral astereognosis, symptomatic cataplexy,isolated knee pain, and pathological emotions (eg, laughter, labilitydue to pseudobulbar palsy) (Feinsod et al 1980; Martin et al 1991;Rutka et al 1991; D'Cruz et al 1994). Uncommon neuro-ophthalmologicabnormalities can also occur, including relative afferent pupillarydefects, upbeat nystagmus, fatigable ptosis, and false-positiveedrophonium testing for cranial nerve palsies (Gilman et al 1977; Miller1988; Dirr et al 1989; King et al 1991; Ragge and Hoyt 1992). Facialmyokymia and hemifacial spasm, which typically occur secondary to
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
4 of 57 03/31/2011 12:46 PM
benign pathology outside the CNS, can occasionally be caused bybrainstem gliomas, especially those arising in the pons (Miller 1988;Westra and Drummond 1991; Krauss et al 1993; Gutmann and Hopf1994). In some cases, the facial manifestations may be the presentingfeature of the tumor and can persist for many years before thediagnosis is confirmed. Rarely, brainstem gliomas can affect regions within the medulla orpons that are involved in control of respiration and blood pressure(Rodriguez et al 1982; Hsu et al 1984; Tobias and Heideman 1991;Valente et al 1993; Siderowf et al 1996; Wilken et al 1997; Gaviani etal 2005). Apnea, apneusis, hypoventilation, and hyperventilation mayoccur when a tumor damages the lower brainstem pathways andnuclear regions responsible for respiratory control (Rodriguez et al1982; Tobias and Heideman 1991; Valente et al 1993; Siderowf et al1996; Wilken et al 1997). Apneusis is characterized by markedprolongation of inspiration and can lead to life-threatening sequelaesuch as bradycardia, reduced oxygen saturation, and hypercapnia(Wilken et al 1997). Treatment with buspirone, a 5-HT1A serotonergicreceptor agonist, can convert apneustic breathing patterns to normal(Wilken et al 1997). Gaviani and coworkers describe a patient whodeveloped central neurogenic hyperventilation from a brainstem tumorthat was associated with significant lactate peaks within the tumor(Gaviani et al 2005). The hyperventilation responded to an oralcontinuous release preparation of morphine. Symptoms related to bloodpressure dysregulation, especially orthostatic hypotension andsecondary cardiac syncope, can also develop due to abnormalities ofcentral autonomic control and disturbance of the afferent arc of thebaroreceptor reflex (Hsu et al 1984). Abnormalities of these vitalstructures are conjectured to be responsible for the rare adult patientswho present with sudden death from brainstem tumors (Dolinak et al2004).
Clinical vignette A 31-year-old woman with an unremarkable past medical historyinitially presented with diplopia. A workup consisting of severalnoncontrast CT scans of the brain and a neurologic examination wasessentially normal. The neurologic symptoms progressed over the next5 months, prompting a second opinion and an enhanced MRI scan ofthe brain. The MRI demonstrated an enhancing mass in the left pons,compatible with brainstem glioma. A biopsy revealed fibrillaryastrocytoma grade II. Postoperatively the patient did well except forloss of hearing on the left side. No further treatment was offered atthis point. Her neurologic status deteriorated further with significantweakness and spasticity on the right side, gait instability, anddysphagia. A follow-up MRI scan 6 months later showed further growthof the tumor. A second surgery was then performed that removedtissue that was of higher grade-fibrillary astrocytoma grade III. After
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
5 of 57 03/31/2011 12:46 PM
recovery from surgery, she underwent 6 weeks of external beamradiation therapy. Her function improved during radiation, withreduction of right-sided weakness, dysphagia, and gait imbalance. Sixmonths later, she noted progressive right arm weakness and spasticity,headache, and gait difficulty. During the next 7 weeks, left-sidedweakness and spasticity, dysarthria, and more severe dysphagiadeveloped. Another MRI scan demonstrated further progression andgrowth of the brainstem tumor. The patient was then referred for chemotherapy evaluation. Herbaseline neurologic examination was remarkable for normal mentation,dysarthric speech, paralysis of abduction in both eyes, adduction in theright eye, diminished corneal reflex in the left eye, lower motor neuronfacial paralysis on the left, reduced hearing and facial sensation on theleft, poor gag response bilaterally, spasticity of all 4 limbs right greaterthan left, 3+/5 right hemiparesis, hyperactive reflexes right greaterthan left, right-sided extensor plantar response, exaggerated Hoffmansigns bilaterally, and severe gait ataxia. She was placed into theintraarterial carboplatin (200 mg/m2 X 2 days, q3 to 4 weeks) andintravenous etoposide (100 mg/m2 X 2 days, q3 to 4 weeks) protocol.After 6 cycles of chemotherapy the patient was improved neurologicallyand had a partial response (ie, 50% to 99% reduction) by MRI. Sheremained stable through 4 more cycles of intraarterial chemotherapy,over a total of 9.5 months, before radiologic progression. Treatmentwas changed to intravenous BCNU (200 mg/m2, q6 to 8 weeks). Thepatient remained stable for 4 more months before further neurologicdeterioration developed. She was then taken off all treatment and died6 weeks later.
Etiology The cells of origin of most brainstem gliomas are transformedastrocytes. In rare cases, these tumors can occur after transformationof oligodendroglial cells or ependymal cells or from mixtures ofneoplastic astrocytes and neurons (ganglionic cells; ie, ganglioglioma).
Pathogenesis and pathophysiology On pathological examination, brainstem gliomas of adults are similarin appearance to brainstem tumors from children. However, thedistribution of tumors is different in the 2 groups. In children, over75% of brainstem gliomas arise within the pons, 20% occur in themedulla, and 10% develop in the midbrain (Tokuriki et al 1986; Packeret al 1992; Maria et al 1993a). In adult cases, 56% of tumors developin the pons, 30% arise from the medulla, and 12% occur in themidbrain (Tokuriki et al 1986; Wang et al 2000). On gross inspection,the brainstem is usually swollen or deformed. The swelling can bediffuse, most commonly within the pons (ie, classic "pontinehypertrophy"), or it can be a more focal, lobulated, or an asymmetricalteration of normal medullary, pontine, or midbrain architecture.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
6 of 57 03/31/2011 12:46 PM
Tumors that cause symmetric expansion of the brainstem are usuallydiffuse, infiltrative, fibrillary astrocytomas of varying grade (oftenmalignant). Intrinsic focal tumors, or those with a predominantlyexophytic growth pattern, are more commonly of lower grade andreduced infiltrative potential (Tokuriki et al 1986; Packer et al 1992;Maria et al 1993a; 1993b; Freeman and Farmer 1998). The exophyticregions of tumor are typically located on the floor of the fourthventricle, within the cerebellopontine angles, or extending from theanterior aspects of the pons or midbrain into the prepontine orperimesencephalic cisterns. Ventrally exophytic tumor can frequentlyencase and displace the basilar artery, usually without causingsecondary arterial thrombosis, ischemia, or infarction. Cysts may bepresent in low- or high-grade brainstem gliomas in up to one third ofcases. In malignant tumors, the cysts often contain hemorrhage andnecrotic debris. Large cysts or regions of tumor that encroach on theventricular system (eg, floor of third ventricle, fourth ventricle,cerebral aqueduct) may cause hydrocephalus (Packer et al 1992; Mariaet al 1993a). In slowly growing focal tumors of the midbrain tectum,hydrocephalus may develop in an indolent fashion as the neoplasmslowly compresses the cerebral aqueduct (Vandertop et al 1992;Squires et al 1994). On rare occasions, gross deposits of tumor can beseen at a distance from the primary site within the brainstem (Packeret al 1983; Silbergeld et al 1988; Maria et al 1993a). Tumor depositsare most common at the base of the brain, along the brainstem, andon the surface of the spinal cord and cauda equina. Distant metastasestend to occur more frequently in high-grade tumors, but can develop inlow-grade fibrillary or pilocytic astrocytomas. At the microscopic level, the vast majority of brainstem tumors inadults and children are of astrocytic lineage and appear similar toastrocytic tumors in other CNS locations (White 1963; Mantravadi et al1982; Tokuriki et al 1986; Maria et al 1993a; Schild et al 1998).Fibrillary astrocytomas of various grades, growing in a diffuse or focalpattern, are the most commonly diagnosed neoplasms. A smallsubgroup of patients has pilocytic astrocytomas, whereas rare histologicdiagnoses include oligodendroglioma, ganglioglioma,ependymoblastoma, hemangioma, mixed glioma, and primitiveneuroectodermal tumors (Queiroz et al 1975; Garcia et al 1984; Kunaet al 1991; Alvarez et al 1996; Lee et al 1998; Fisher et al 2000;Zagzag et al 2000). Initial antemortem histological evaluation discloseslow-grade, well-differentiated pathology in approximately 60% ofbiopsy and resection specimens; malignant pathology, usuallyanaplastic astrocytoma or glioblastoma multiforme, is found in 40%(White 1963; Alvisi et al 1985; Tokuriki et al 1986; Shibamoto et al1989; Bricolo et al 1991; Rajshekhar and Chandy 1995). In contrast,autopsy studies demonstrate a higher percentage of malignantpathology, approximately 60% to 90% (Mantravadi et al 1982; Grigsby
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
7 of 57 03/31/2011 12:46 PM
et al 1989a; Shibamoto et al 1989). This discrepancy is explained bythe selection bias in autopsy materials toward more aggressive tumorsand the tendency of well-differentiated tumors to undergo malignantdegeneration during clinical progression. Furthermore, autopsy studiessuggest that tumor spread and grade of malignancy depend on the siteof origin of the neoplasm (Mantravadi et al 1982). In a study of 25autopsied brainstem glioma patients (41% over 20 years of age),Mantravadi and colleagues found that pontine tumors were more likelythan midbrain or medullary tumors to invade adjacent regions of brainand to have malignant histology (71% of pontine tumors were eitheranaplastic astrocytoma or glioblastoma multiforme) (Mantravadi et al1982). Low-grade fibrillary brainstem astrocytomas can demonstrate either adiffuse or a focal growth pattern but appear similar histologically. Theyare classified as astrocytoma, grade I or II, using the Kernohan or St.Anne-Mayo classification schemes, or as astrocytoma grade II by theWorld Health Organization (Coons and Johnson 1994). The tumors showa mild increase in cellularity and are composed of cells with astrocyticmorphology. Cellular and nuclear atypia and pleomorphism areminimal. Rosenthal fibers are densely eosinophilic rod-shapedstructures that may be present in some tumors. Low-grade tumorsgenerally stain strongly with glial fibrillary acidic protein. Malignantfeatures such as mitoses, endothelial proliferation, and regions ofnecrosis are not present. The growth pattern of low-grade fibrillary brainstem astrocytomas isto insinuate cells from the growing edge of the tumor between andalong adjacent nerve fiber fascicles and pial-limiting membranes,expanding in accordance with the surrounding anatomy down a "path ofleast resistance" (Epstein and Farmer 1993; Maria et al 1993b; Coonsand Johnson 1994). Destruction of tissue and infiltration into graymatter is minimal. Because of the orientation of the pial-limitingmembranes surrounding the brainstem and the alignment of theinternal fiber tracts, enlargement of slowly growing, low-grade tumorsis more likely to be directed toward the floor of the fourth ventricle andcerebellopontine angle regions, where there is less resistance toexpansion (Epstein and Farmer 1993). This explains the high frequencyof exophytic growth noted in these areas. Low-grade tumors are alsoless invasive and infiltrative than more malignant tumors because of areduced capacity to attach to, enzymatically degrade, and migratethrough localized tissue extracellular matrix proteins (Maria et al1993b). High-grade fibrillary brainstem astrocytomas usually grow in a diffusefashion, but, on occasion, they may have a more focal or exophyticpresentation (Lee et al 1998). They are classified as either anaplasticastrocytoma or glioblastoma multiforme, which correspond toastrocytoma grades 3 or 4, respectively, of the Kernohan, St.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
8 of 57 03/31/2011 12:46 PM
Anne-Mayo, and World Health Organization classification schemes(Coons and Johnson 1994). These tumors demonstrate medium to highcellularity, with reduced amounts of cytoplasm, extensive nuclear andcellular pleomorphism, endothelial proliferation, mitotic figures, and, insome cases, necrosis. When tumor cells infiltrate into graymatter, they tend to cluster around neurons (ie, perineuronalsatellitosis) and collect in subpial and subventricular zones. Bothanaplastic astrocytoma and glioblastoma multiforme are histologicallyheterogeneous tumors, but this is especially so for glioblastomamultiforme, in which it is not uncommon to have low-grade regions ofastrocytoma near areas containing numerous mitoses, endothelialproliferation, and necrosis. High-grade astrocytomas also stain withglial fibrillary acidic protein, but in general the staining is less intenseand more irregular than in low-grade tumors. Recent work by Jallo andcolleagues has investigated the development of a reliable animal modelthat reproduces the aggressive growth characteristics of malignantbrainstem gliomas (Jallo et al 2006). The authors injected 9Lgliosarcoma cells or F98 glioma cells into the anterior pons of Fischerrats, using stereotactic techniques. The growth of the tumors was veryreliable and led to the onset of hemiparesis within a mean of 16.5 daysin 100% of the animals. Histopathologically, the tumors were similar tohigh-grade brainstem gliomas in humans. The growth pattern of high-grade brainstem astrocytomas is differentfrom that of low-grade tumors. The extent of infiltration andinvasiveness into adjacent normal brain is more pronounced. Inaddition, as these tumors enlarge, they more often damage or destroythe underlying normal brain parenchyma. Structural limitations togrowth within the brainstem, such as the anterior and lateralpial-limiting membranes and various large nerve fiber bundles, are noteffective against high-grade tumors and do not direct growth likelow-grade neoplasms (Epstein and Farmer 1993; Maria et al 1993b).This indiscriminate growth pattern explains the reduced frequency ofexophytic extension in high-grade tumors, whose tendency is toinfiltrate axially within the brainstem, although exophytic growth canoccur in rare cases (Lee et al 1998). The invasive and infiltrativenature of high-grade tumors is related to their highly developed abilityto interact with, degrade, and migrate through specific substratemolecules found within the extracellular matrix of surrounding normalbrainstem parenchyma (Maria et al 1993b). Pilocytic astrocytomas typically arise in the dorsal pons, withsubsequent growth rostrally through the brainstem, but can developanywhere (Fisher et al 2000). They are usually focal, indolent,slow-growing neoplasms and often have an exophytic component(Khatib et al 1994). Pilocytic astrocytomas are designated astrocytoma,grade I by the World Health Organization (Coons and Johnson 1994).On microscopic evaluation they most often display a biphasic pattern of
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
9 of 57 03/31/2011 12:46 PM
loose, microcystic areas, alternating with more dense regions composedof elongated, "hairlike" astrocytic cells. Rosenthal fibers andgranular bodies are often numerous in the dense regions of tumor.Aggressive features can be present, including cellular atypia, occasionalmitoses, multinucleated cells, focal necrosis, and prominentvasculature. However, these elements do not indicate malignancy oralter the more favorable prognosis and improved survival of patientswith this type of brainstem tumor. Some authors feel pilocyticastrocytomas of the brainstem should be classified separately fromfibrillary astrocytomas in this region because of their vastly differentclinical presentation and extended survival (Fisher et al 2000). Gangliogliomas of the brainstem are uncommon tumors composed ofan admixture of neoplastic neuronal (ie, ganglionic) and astrocytic cells(Garcia et al 1984; Kuna et al 1991; Coons and Johnson 1994). Theastrocytic portion of the tumor predominates and is usually classified asbeing fibrillary and of low grade. Mitoses and other aggressive featuresare generally absent. Gangliogliomas are typically slow growing andwell circumscribed, without significant infiltration. In a literature reviewof 14 patients with brainstem gangliogliomas by Garcia and colleagues,5 were older than 18 years of age (36%), and in 11 of the patients(78.5%) the medulla was the site of neoplastic origin (Garcia et al1984). Rarely, other types of mixed glioma can develop within thebrainstem in adults (eg, mixed anaplastic oligodendroglioma orependymoma) (Lee et al 1998). Techniques that can measure the biological potential of brainstemgliomas include Ki-67 and bromodeoxyuridine labeling studies, andfunctional brain imaging using SPECT or PET scans. Both labelingmethods quantitatively assess the proliferating fraction and, therefore,the inherent aggressiveness of a tumor (ie, labeling index). Ki-67reacts with cells in G1, S, and G2M phases, whereasbromodeoxyuridine labels only cells in S phase. For fibrillaryastrocytomas, in general, Ki-67 and bromodeoxyuridine labeling indicesincrease with grade, whereas for all pilocytic tumors the indices tend tobe low (Ito et al 1992; Jaros et al 1992). Several authors haveevaluated brainstem gliomas using functional imaging methods todifferentiate between tumor progression and radiation necrosis(Bruggers et al 1993). Bruggers and colleagues studied a brainstemglioma patient with serial MRI and 18-fluorodeoxyglucose PET scans(Bruggers et al 1993). The PET scans demonstrated increasinglyhypermetabolic activity, which was helpful in differentiating betweentumor progression and radiation necrosis when MRI scans remainedstable. Autopsy revealed a diffuse, viable glioblastoma multiformewithout evidence of radiation necrosis. Cytogenetic and chromosomal studies of brainstem astrocytomas areuncommon, most likely due to the paucity of tissue available foranalysis following surgery, which is usually a small biopsy. However,
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
10 of 57 03/31/2011 12:46 PM
they are probably similar to astrocytomas of the same grade fromother CNS locations (Rey et al 1987; Jenkins et al 1989). Few studies have assessed the role of oncogenes and tumorsuppressor genes in the origin of brainstem gliomas. The mostcomplete study is by Louis and colleagues, who evaluated archival orautopsy tissue from 7 patients with brainstem glioblastoma multiforme(2 patients 16 years of age) for abnormalities related to epidermalgrowth factor receptor amplification, loss of heterozygosity ofchromosomes 10 and 17, and mutations within the p53 gene usingpolymerase chain reaction-based techniques (Louis et al 1993). None ofthe tumors demonstrated any amplification of the epidermal growthfactor receptor gene. Four of 7 tumors (57%) had allelic loss ofchromosome 10. Four tumors were also shown to have lost portions ofthe short arm of chromosome 17 (57%; all included the regioncontaining the p53 gene, 17p13.1). The p53 gene was mutated in 5 of7 tumors (71%). Four of these 5 cases were p53 genes on theremaining allele of tumors that had lost heterozygosity, whereas thefifth was from a tumor with both copies of 17p. Two of the p53mutations caused base changes that resulted in amino acidsubstitutions (Arg Cys, Arg Leu), whereas a third resulted in a stopcodon. The authors concluded that these results were consistent withprevious data suggesting that a subset of glioblastoma multiforme thatdevelops in younger patients is derived from lower-grade, diffuse,fibrillary astrocytomas (von Deimling et al 1993). The lower-gradetumors and subgroup of glioblastoma multiforme are characterized byallelic loss of 17p, p53 mutations, and a lack of epidermal growthfactor receptor amplification. These data are in agreement with Zhangand colleagues, who found mutations within the p53 gene in 8 of 13pontine anaplastic astrocytomas (62%; 4 patients 16 years of age)(Zhang et al 1993). Of 15 total mutations detected, 11 were missensemutations that resulted in amino acid substitutions. Another report hasdemonstrated similar results using immunohistochemical methods, withp53 accumulation more frequently noted in the higher-grade tumors(Badhe et al 2004). A report by Lang and colleagues describes an adultpatient with a brainstem anaplastic astrocytoma that did not showevidence for loss of heterozygosity of chromosomes 10 or 17p,mutations within the p53 gene, or amplification of the epidermalgrowth factor receptor gene (Lang et al 1994). Molecular analysis of 7pediatric patients with primitive neuroectodermal tumors of thebrainstem did not disclose p53 mutations (Zagzag et al 2000). This issimilar to primitive neuroectodermal tumors of the cerebellum andcerebrum, which are also lacking in abnormalities of p53. A molecularanalysis of 28 specimens of pediatric brainstem gliomas has detected ahigh incidence of amplification and overexpression of ERBB1 (ie, EGFR)(Gilbertson et al 2003). The degree of ERBB1 expression correlatedclosely with increasing tumor grade (p<0.001) and was not related to
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
11 of 57 03/31/2011 12:46 PM
p53 status. The percentage of EGFRvIII mutations in the amplifiedspecimens could not be determined with the techniques used. Theauthors suggest that ERBB1 signaling is important for the pathogenesisof many pediatric brainstem gliomas and that molecular therapeuticagents designed to target this pathway (eg, ZD1839; Iressa) should beevaluated. Verification of ERBB1 amplification and expression status inbrainstem gliomas in adults remains unclear. Using high-resolutionsingle nucleotide polymorphism (SNP)-based DNA microarray analysis,a series of 11 samples from patients with diffuse pontine gliomas wasanalyzed (Zarghooni et al 2010). In 36% of the cohort, gains in copynumber (range 4 to 18) were noted for platelet-derived growth factorreceptor alpha (PDGFR-alpha). Expression of PDGFR-alpha was notedin all tumor samples. In 3 cases, low-level gains were present forpoly(ADP-ribose) polymerase (PARP)-1. Pathway analysis also notedgenes with loss of heterozygosity in the DNA repair pathway. Theauthors suggested that PDGFR-alpha and PARP-1 might be rationaltargets to consider for molecular therapy of brainstem gliomas. Using an implanted C6 glioma model of brainstem glioma in rats, Liuand coworkers attempted to discern differences in the growth patternsand biology of the juvenile and adult animals (Liu et al 2008). Adultrats presented with focal neurologic symptoms and had more focalhistology within the pons. In contrast, juvenile rats had a more rapidpresentation and a more diffuse neurologic presentation, with ataxia,cranial nerve deficits, and incontinence. Histologically, the tumors weremore diffuse and infiltrative throughout the entire brainstem. Inaddition, tumors in juvenile rats had a higher Ki-67 labeling index anda lower rate of apoptosis. The median survival was significantly higherin the adult rats (p < 0.05). The authors concluded that the immaturerat brainstem may offer or create a more permissive cellularenvironment, allowing tumor cells to be more invasive.
Epidemiology The exact incidence and prevalence of brainstem gliomas in adults isunknown. In children they make up 10% to 20% of pediatric primarybrain tumors (Newton 1994; Freeman and Farmer 1998; Donaldson etal 2006). Furthermore, approximately 70% to 75% of these neoplasmsdevelop by 20 years of age (Maria et al 1993a). By comparison, theincidence in the adult population is estimated to be 9 to 10 times lowerthan that in children, roughly 0.5% to 2.0% (White 1963; Tokuriki et al1986; Linstadt et al 1991; Newton 1994). In a study by Gibbsexamining 1383 primary intracranial tumors in patients aged 16 to 70years, only 1% were located within the pons or midbrain (Gibbs 1932).Tokuriki and colleagues reviewed 3044 adult primary brain tumors overa 35-year period (Tokuriki et al 1986). Intrinsic tumors of thebrainstem were found in 16 cases, an incidence of only 0.52%.However, in smaller series of brainstem glioma patients, the proportionof adults may be larger, ranging from 10% to 35% (White 1963;
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
12 of 57 03/31/2011 12:46 PM
Grigsby et al 1989b). The vast majority of brainstem gliomas aresporadic, but they can be familial on rare occasions (Schianchi andKraus-Ruppert 1980; Fitzgerald 2000).
Prevention There are no known measures to prevent the development of abrainstem glioma in de novo patients or in those at risk fromassociated disorders (eg, neurofibromatosis type 1).
Differential diagnosis The differential diagnosis of brainstem gliomas in adults consists ofother mass lesions or disease processes that can present with aprogressive brainstem syndrome and includes other neoplasms,parasitic cysts, viral and postviral brainstem encephalitis, infarction,tuberculoma, demyelinating syndromes, vascular malformations,abscesses, radionecrosis, and chronic meningitis of various etiologies(Frank et al 1988; Franzini et al 1988; Abernathy et al 1989; Smith1990; Maria et al 1993a; Rajshekhar and Chandy 1995; Lakhan andHarle 2009). Neoplastic considerations include metastases to thebrainstem or posterior fossa, as well as primary brain tumors of theposterior fossa or skull base such as meningioma, acousticschwannoma, dermoid cyst, medulloblastoma, ependymoma, andepidermoid cyst. Infectious considerations include parasitic cysts fromcysticercosis, which have a predilection for the fourth ventricularregion, tuberculomas or pyogenic abscess formation of the posteriorfossa, viral encephalitis involving the brainstem, and chronic meningitiswith basilar exudate (eg, tuberculosis, cryptococcus neoformans).Demyelinating syndromes refer mainly to multiple sclerosis, whichoften presents with multifocal brainstem signs and symptoms, and topostinfectious brainstem encephalitis, which is considered to be anautoimmune-mediated demyelinating process following viral exposure.In a recent case report, a 48-year-old woman demonstrated aprogressive brainstem syndrome, along with encephalopathy andhallucinations (Lakhan and Harle 2009). She was thought to have anacute demyelinating encephalopathy or collagen vascular disease, andshe was treated with plasmapheresis, without benefit. At autopsy, alarge brainstem glioma was noted, which involved the pons, medulla,and cerebellum. Cerebrovascular processes include brainstem infarction(although these tend to occur rather acutely), hemorrhage, and variousvascular malformations (ie, arteriovenous malformation, capillarytelangiectasia, cavernous angioma) that can become symptomaticbecause of mass effect or spontaneous hemorrhage. Although CT and MRI will usually help to discriminate betweenbrainstem glioma and other disease processes within the posteriorfossa, they are not 100% sensitive or specific and may lead onoccasion to false-positive or false-negative diagnoses (Frank et al1988; Franzini et al 1988; Abernathy et al 1989; Rajshekhar and
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
13 of 57 03/31/2011 12:46 PM
Chandy 1995). In a study by Frank and colleagues, 17% of 38 patientswith a preoperative diagnosis of a brainstem tumor had a nonneoplasticlesion at biopsy, usually a vascular abnormality or malformation (Franket al 1988). In 24 adult patients with expanding brainstem masses,25% had nonneoplastic diagnoses following stereotactic biopsy (Franziniet al 1988). Rajshekhar and Chandy describe a series of 71 patientswith brainstem lesions in which 19.4% had diagnoses other thanbrainstem glioma following biopsy (Rajshekhar and Chandy 1995). Thisgroup of nongliomatous lesions included nonspecific chronicinflammation (4 patients), granulomatous inflammation (2 patients),epidermoid cyst (2 patients), pyogenic abscess (2 patients), andencephalitis (1 patient). In a subgroup of 7 patients with thepreoperative CT diagnosis of glioma in which benign lesions were foundat biopsy, the diagnoses included encephalitis, epidermoid cyst, andtuberculoma. In the study by Abernathy and colleagues, 26 patients (20over 18 years old) with pontine mass lesions were biopsied forsuspected brainstem tumors (Abernathy et al 1989). Ten of 26 patients(38.5%) had a benign diagnosis, including cryptococcal abscess,arteriovenous malformation, demyelination, infarction, andradionecrosis.
Diagnostic workup In patients with neurologic signs and symptoms suggestive of abrainstem glioma, neuroimaging with CT or MRI is the most criticaldiagnostic test. These studies should be performed with and withoutcontrast media for the most accurate visualization of the mass, toassess the relationship of the mass to other posterior fossa anatomy,and to assist in differential diagnosis. The appearance of brainstemgliomas in adults on CT or MRI is similar to that in children. In general,both CT and MRI demonstrate enlargement and asymmetry within thebrainstem, most commonly the pons, with minimal edema formationaround the tumor (Tokuriki et al 1986; Shibamoto et al 1989; Smith1990; Packer et al 1992; Maria et al 1993a; 1993b; Donaldson et al2006). However, MRI has been shown to be superior to CT fordiagnosing brainstem gliomas, with a sensitivity and specificity forpathology approaching 100% (Bradac et al 1985; Hueftle et al 1985;Lee et al 1985; Packer et al 1985; Zimmerman et al 1985; Raffel et al1988; Barkovich et al 1990; Smith 1990; Packer et al 1992; Maria et al1993a; 1993b; Bognar et al 1994; Fischbein et al 1996). Thisimprovement in diagnostic accuracy is due to several factors, includinga lack of bone artifact in the posterior fossa, increased sensitivity tointratumoral water content, and the multiplanar capability of MRI,especially the midsagittal view. In 10% to 20% of cases, MRI willdetect tumors that are not discernible by CT, especially small, focaltumors or those that occur within the midbrain. This is important forpatients who have hydrocephalus on CT, but with no evidence on thescan for an intrinsic brainstem tumor. All of these patients should be
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
14 of 57 03/31/2011 12:46 PM
studied with MRI because some of them will harbor neoplasms thatmight benefit from earlier diagnosis and treatment (Raffel et al 1988).The anatomical configuration within the brainstem, extent ofinfiltration, presence of an exophytic component or leptomeningealseeding, and degree of enhancement are visualized in more detail withMRI (Bradac et al 1985; Hueftle et al 1985; Lee et al 1985; Packer etal 1985; Zimmerman et al 1985; Donahue et al 1998). Despite theseadvantages, MRI is similar to CT in its inability to consistentlydifferentiate between neoplastic and benign lesions or to correlate theappearance of a given lesion with a specific pathologic diagnosis. Inaddition, recent data would suggest that even with MRI, there issignificant interobserver variability in the measurement of diffusebrainstem gliomas. Because of this variability, the authors suggest thatfor clinical trial purposes, the measurements of brainstem gliomasshould be made by a single neuroradiologist (Hayward et al 2008). When using MRI for the initial assessment of brainstem gliomas, it isrecommended that T1- and T2-weighted nonenhanced imaging, as wellas T1-weighted gadolinium-enhanced imaging, be performed in boththe axial and midsagittal planes (Barkovich et al 1990; Packer et al1992; Donaldson et al 2006). Doing this will provide the mostinformation on the size, extent, and other characteristics of the tumornecessary for treatment decisions such as extent of surgery and designof radiation ports, and for detailed comparison at follow-up. Onnonenhanced T1-weighted images, brainstem gliomas generallydemonstrate hypointense signal compared to normal white matter(Hueftle et al 1985; Lee et al 1985; Packer et al 1985; Zimmerman etal 1985; Barkovich et al 1990; Packer et al 1992; Maria et al 1993a). On proton density and T2-weighted images, increased signal intensityis usually noted within the mass. Because the degree ofperitumoral edema is typically insignificant in these tumors, the extentof abnormal T2-weighted signal is believed to represent bulky tumorand any associated infiltration. Following administration of gadolinium,T1-weighted images show variable amounts of enhancement, withpatterns similar to that seen on CT: negligible, ring-enhancing,partial/focal, and diffuse. The exophytic components of tumorsare usually found in the basilar subarachnoid spaces or cerebellopontineangles, and they frequently enhance in a diffuse fashion. Disturbanceor encasement of the basilar artery by exophytic tumor in theprepontine cistern is clearly seen on MRI. Additional features thatcan demonstrate enhancement and suggest more aggressive behaviorare subpial extension, subependymal extension, ill-defined tumormargins, necrosis, and the presence of daughter nodules (Maria et al1993a; 1993b). The presence of acute or old hemorrhage within tumoris easily determined by MRI, although it is uncommon at presentation,occurring in approximately 6.25% of cases as reported in a recentpaper (Broniscer et al 2006). However, symptomatic hemorrhage is
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
15 of 57 03/31/2011 12:46 PM
noted in nearly 20% of patients after diagnosis during the course oftherapy. On rare occasions, MRI can demonstrate brainstem tumorsinfiltrating along or encasing the lower cranial nerves (Yousry et al2004; Ree et al 2005). Some authors report the importance of thisinformation in presurgical planning of exophytic brainstem tumors(Yousry et al 2004). A recent study correlating MRI and PET findingsnoted that diffuse pontine gliomas were always of high-grade pathology(ie, glioblastoma multiforme or anaplastic astrocytoma), with variableexophytic features (Kwon et al 2006). PET scans were hypermetaboliconly in the tumors with glioblastoma multiforme pathology. However,some glioblastomas and all of the anaplastic astrocytomas werehypometabolic, as were the low-grade tumors. New MRI techniques,such as diffusion tensor imaging (DTI), are also being applied tobrainstem gliomas (Helton et al 2006; 2008). DTI allows for a moredetailed and quantitative evaluation of the fiber tracts in the brainstemand shows the degree of involvement of these tracts by tumor.Preliminary data suggest that DTI demonstrates superior visualizationand quantification of tumor involvement in the motor, sensory, andtransverse pontine tracts in comparison to conventional MRI. Inaddition, DTI appears to be able to demonstrate axonal degenerationwithin the motor and sensory tracts of the brainstem in these patients(Helton et al 2008). Several authors have applied MRI as a tool for classification ofbrainstem tumors into groups with treatment-related and prognosticsignificance (Epstein and Wisoff 1988; 1990; Barkovich et al 1990;Epstein and Farmer 1993; Fischbein et al 1996; Guillamo et al 2001).Epstein and colleagues have classified brainstem tumors into 4 groups:diffuse, focal, cystic, and those that occur at the cervicomedullaryjunction (Epstein and Wisoff 1988; 1990; Epstein and Farmer 1993).Diffuse tumors are most common and have the worst prognosis,generally arising within the pons and demonstrating a hypointensesignal that usually does not enhance after contrast. Extension into themedulla and midbrain is often noted. Sagittal views typicallydemonstrate significant pontine hypertrophy. Focal tumors generallymeasure less than 2.5 cm in diameter, have no associated edema, andenhance with contrast. They are more likely to have an exophyticcomponent, pilocytic histology, and a better prognosis than diffusetumors (Khatib et al 1994). Cystic tumors that contain an enhancingmural nodule have an excellent prognosis similar to that of cerebellarpilocytic astrocytomas. If the tumor has an enhancing solid componentin addition to an enhancing cyst wall, it is usually malignant and carriesa poor prognosis. Tumors of the cervicomedullary junction are often oflow grade, rarely extend above the pontomedullary junction (thoughoccasionally growing caudally into the cervical spinal cord), and have afavorable prognosis. They are well delineated on sagittal MRI.Barkovich and colleagues have characterized the MRI scans of 87
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
16 of 57 03/31/2011 12:46 PM
"high-risk" brainstem glioma patients with respect to tumor location oforigin, focality, direction and extent of growth, degree of brainstemenlargement, degree of exophytic growth, hydrocephalus, hemorrhage,necrosis, and presence or absence of cyst (Barkovich et al 1990). Theauthors found a significant difference in survival based on the primarylocation of the tumor (p = 0.02): no deaths in 6 cases of midbrainlesions, 50% survival at 2 years for medullary tumors, and only 20%survival at 2 years for pontine tumors. The degree of brainstemenlargement had an inverse relationship with survival (p = 0.05): no ormild versus moderate or severe. Similarly, degree of infiltration wasinversely related to survival (p = 0.005). The presence of a tumor cystdenoted a more favorable outcome (p = 0.03). Some authors have begun to apply MRI technology to monitormagnetic resonance spectroscopy (MRS) of tumors, including brainstemgliomas. A recent report by Laprie and colleagues used a multivoxelversion of this technique to monitor brainstem gliomas during and aftertreatment (Laprie et al 2005). A series of 24 MRS studies on 8 patientswas performed, and the data suggested that longitudinal multivoxelMRS was feasible, reliable, and potentially superior to univoxeltechniques for evaluating response to radiotherapy and other treatmentmodalities. Recently, 2 patients were described that had undergonelongitudinal MRS monitoring of their diffuse brainstem gliomas duringtherapy (Thakur et al 2006). Although there was a brief interval ofclinical improvement after radiation therapy, the MRS signaturedemonstrated further elevation of the Cho/Cr and Cho/NAA ratios,more consistent with progression. This was confirmed at the nextfollow-up visit, when both patients were noted to have clinicaldeterioration. The authors suggest including MRS in the routineradiological evaluation of patients with brainstem gliomas. Although CT is not as accurate as MRI, it can still discern the presenceof a brainstem tumor over 90% of cases, especially if the lesion iswithin the pons and has an exophytic component (Kingsley and Kendall1979; Bilaniuk et al 1980; Abernathy et al 1989; Maria et al 1993a;1993b; Selvapandian et al 1999). With unenhanced CT, the tumorusually appears hypodense or isodense compared to normal surroundingbrain. Effacement of the basal cisterns, displacement and deformityof the fourth ventricle, and disturbance of the basilar artery areadditional early signs of tumor. Tumor enhancement is variable,occurring in approximately 50% of tumors. Exophytic portions are mostlikely to demonstrate strong enhancement. Diffuse, infiltrative tumorsare generally hypodense and most often show partial or negligibleenhancement (Bilaniuk et al 1980; Tokuriki et al 1986; Shibamoto et al1989; Smith 1990). Focal tumors, with or without exophyticcomponents, are more likely to demonstrate diffuse or ringlikeenhancement. Hydrocephalus is noted in 25% to 30% of tumors and isespecially common in tumors affecting the midbrain tectal region
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
17 of 57 03/31/2011 12:46 PM
(Kingsley and Kendall 1979; Bilaniuk et al 1980; Bognar et al 1994).Cystic changes are noted in 10% to 15% of cases and can beassociated with low- or high-grade tumors (Kingsley and Kendall 1979;Bilaniuk et al 1980; Smith 1990). CT is limited by beam-hardeningartifact in the posterior fossa, which reduces sensitivity for small, focallesions and is often unable to properly gauge the extent of tumorinfiltration within the brainstem (Smith 1990; Packer et al 1992; Mariaet al 1993a; 1993b). Cerebrospinal fluid analysis and evoked potentials are rarely indicatedfor diagnosis of brainstem gliomas in the era of CT and MRI. Ifcerebrospinal fluid is evaluated, it is usually normal (Packer et al1992). In 15% to 20% of patients, there may be a mild pleocytosis(less than 20 cells) and elevation of cerebrospinal fluid protein. Rarely,malignant cells may be noted on cytologic examination in thosepatients with leptomeningeal spread of tumor (Packer et al 1983).Auditory evoked potentials have also been used for the diagnosis ofbrainstem gliomas, although they may be more useful for themonitoring of these patients during neurosurgical procedures (Nodar etal 1980; Packer et al 1992).
Prognosis and complications The overall prognosis for survival and intact neurologic function inadults with brainstem gliomas is rather poor, but prognosis variessomewhat depending on the histology, location, and type of tumor (ie,diffuse, focal, exophytic, cystic) (Schild et al 1998; Fisher et al 2000).Reports of survival from the time of onset vary widely among authors,ranging from a mean of 19.2 months (median 12.5 months, 13 adultcases) in the group described by Tokuriki and colleagues, to a mean of27.7 months (30 adult cases) in the cohort analyzed by White (White1963; Tokuriki et al 1986; Packer et al 1992; Maria et al 1993a). Datafrom the radiation oncology literature are similar, with mediansurvivals ranging from 7.6 to 16.1 months (average median survival13.6 months) in a collective cohort of 85 adult patients (Edwards et al1989; Shrieve et al 1992; Guiney et al 1993; Prados et al 1995). In thestudy by Guiney and colleagues, tumors located in the pons had asignificantly adverse affect (p=0.035) on survival when compared toother brainstem locations (Guiney et al 1993). Similar results havebeen noted by Schild and colleagues with 5-year survival of 54% withlesions outside the pons and 21% for those with lesions within the pons(p=0.04) (Schild et al 1998). However, some authors have not foundsignificant survival differences based on tumor location (Edwards et al1989). In most of the studies from the radiation oncology literature,the percentage of patients surviving at 2 years was between 40% and50% (Kim et al 1980; Shrieve et al 1992). In a group of adult patientswith pontine gliomas, the 3-year survival was 33% in a study byGuiney and colleagues (Guiney et al 1993). In contrast, a cohort ofpatients with pontine gliomas reported by Grigsby and colleagues had
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
18 of 57 03/31/2011 12:46 PM
5-year survivals of 46.6% (Grigsby et al 1989c). In studies that wereable to compare survival between groups of adult and pediatricbrainstem glioma patients who had received radiation therapy, resultswere comparable (Kim et al 1980; Grigsby et al 1989c; Guiney et al1993). In contrast, in a study by Landolfi and colleagues of 19 adultpatients (median age 40 years) with brainstem gliomas as diagnosedby MRI scan, they noted a median survival of 54 months and a 5-yearsurvival of 45% (Landolfi et al 1998). The authors concluded thatbrainstem tumors may be less aggressive in adults than in children,even when located within the pontine parenchyma. Similar conclusionshave been made by Guillamo and colleagues, who suggest that diffusetumors may be less aggressive and of lower grade in adults than inchildren (Guillamo et al 2001). In a review of 48 adult patients withbrainstem gliomas, 46% of the cohort had a diffuse presentation onMRI. However, of the biopsied patients, 82% had benign histology witha median survival of 7.3 years. Numerous authors have evaluated brainstem glioma patients usingunivariate and multivariate analyses to determine both positive andnegative prognostic factors. The vast majority of the data are derivedfrom pediatric brainstem glioma patients (Albright et al 1986; Cohen etal 1986; Barkovich et al 1990; Packer et al 1992; Fischbein et al1996). Fewer studies have included adult patients for prognosticevaluation (Edwards et al 1989; Grigsby et al 1989b; 1989c;Shibamoto et al 1989; Shrieve et al 1992; Guiney et al 1993; Pradoset al 1995; Schild et al 1998; Schulz-Ertner et al 2000; Guillamo et al2001). In most of the studies, race, gender, extent of surgicalresection, and age did not reach significance in univariate ormultivariate analyses. The location of the tumor was a significantfactor in several studies. Patients with tumors located in the pons oftenhad shorter survival times (p = 0.035), whereas Shibamoto andcolleagues noted that patients with midbrain tumors often survivedlonger (p < 0.05) (Grigsby et al 1989b; Shibamoto et al 1989; Guineyet al 1993; Schild et al 1998). The histological grade of the tumor wassignificant (p < 0.05) in a few studies, such that patients withmicroscopically evident malignant features or the diagnosis ofglioblastoma multiforme had a poorer prognosis and shorter survival(Grigsby et al 1989c; Shibamoto et al 1989). One of the mostconsistently important prognostic factors was duration of symptomsprior to diagnosis. In many studies, patients with longer symptomduration had longer survival times; conversely, those patients withshorter symptom duration had shorter survival times (Edwards et al1989; Grigsby et al 1989c; Packer et al 1992; Guiney et al 1993;Prados et al 1995; Fisher et al 2000). The type of tumor (ie, diffusevs. focal) had prognostic implications in several reports; patients withdiffuse tumors had significantly shorter survival and time to tumorprogression (p = 0.012 and p = 0.005, respectively) (Edwards et al
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
19 of 57 03/31/2011 12:46 PM
1989; Prados et al 1995; Fischbein et al 1996; Schild et al 1998).Fisher and colleagues report a series of 76 patients in which thepresence of an abducens nerve palsy at diagnosis was associated withpoor survival (p less than 0.0001) (Fisher et al 2000). Schulz-Ertnerand colleagues evaluated 26 adults in their analysis of prognosticfactors in a series of 41 brainstem glioma patients (Schulz-Ertner et al2000). The only significant prognostic factors for survival in theunivariate and multivariate analyses were the presence of clinical orradiological response 6 weeks after treatment. A few authors havereported that patients with neurofibromatosis type 1 and brainstemgliomas have an improved prognosis over those tumor patients withoutneurofibromatosis type 1 (Milstein et al 1989; Raffel et al 1989; Molloyet al 1995; Pollack et al 1996; Bilaniuk et al 1997). In a review of 21neurofibromatosis type 1 patients with brainstem tumors, only 10 hadradiographic or clinical progression during a 9-year follow-up period(Pollack et al 1996). In 4 of these patients specific therapy wasrequired; 1 required biopsy, 3 required excision, and 2 requiredradiotherapy. All 4 lesions were histologically low-grade and remainedstable after treatment. Bilaniuk and colleagues studied 25 patients withneurofibromatosis type 1 that had brainstem tumors (diffuse in 12 of25 patients) (Bilaniuk et al 1997). MRI evidence of tumor growthoccurred in 8 patients (32%), all with diffuse tumors. Two patients withdiffuse tumors died of progressive disease. The authors concluded thatalthough patients in their series had a better overall prognosis thanbrainstem glioma patients without neurofibromatosis type 1, thetumors did not always behave in a benign, indolent manner (especiallydiffuse lesions) and were more dangerous than other tumor types foundin patients with neurofibromatosis type 1. Some authors recommendusing pontine midsagittal diameters in combination with magneticresonance spectroscopy to differentiate “benign” pontine enlargementassociated with neurofibromatosis type 1 from the more malignantdiffuse brainstem glioma (Broniscer et al 1997). Patients withneurofibromatosis type 1 and pontine enlargement had lesions thatwere significantly smaller than diffuse brainstem gliomas. In addition,the N-acetylaspartate peaks were consistently preserved in theneurofibromatosis type 1 patients without diffuse tumors, suggestingretained neuronal elements within the brainstem. In a study ofprognostic factors in a large adult cohort, univariate analysis suggestedthat age of onset less than 40 years, duration of symptoms greaterthan 3 months before diagnosis, Karnofsky performance status greaterthan 70, low-grade histology, and absence of "necrosis" on MRI wereall favorable prognostic variables (Guillamo et al 2001). Onmultivariate analysis, only duration of symptoms, histological grade ofthe tumor, and presence of "necrosis" on MRI were significant andindependent prognostic variables. A recent study by Kesari and colleagues evaluated prognostic
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
20 of 57 03/31/2011 12:46 PM
variables in a cohort of 101 adult patients with brainstem glioma(Kesari et al 2008). On multivariate analysis, ethnicity, tumor location,clinical grade of the tumor, and patient age at diagnosis all had asignificant effect on survival. Non-Caucasian patients had a hazard ratio4.19 times larger than Caucasian patients (p = 0.0004). Patients withdiffuse pontine tumors had a hazard ratio 3.58 times larger thanpatients with tumors of the cervicomedullary junction (p = 0.0006).The hazard ratio for patients with clinically high-grade tumors was 2.81times larger than those with low-grade tumors (p = 0.0017). Patientswith an older age at diagnosis had a hazard ratio 1.34 times larger thanyounger patients (p = 0.0032). In general, adults with brainstemgliomas had a better prognosis than children with similar tumors. Theoverall survival for all patients at 5 and 10 years was 58% and 41%,respectively. Several authors have studied prognostic factors in relation toinformation obtained from CT or MRI scans. Shibamoto and colleaguesevaluated the correlation between prognostic factors and CT features(Shibamoto et al 1989). They found a significant association betweenestimated tumor volume and survival. Patients with tumors less than 6cm3 survived longer than those with tumors between 6 and 20 cm3 (pless than 0.05) and larger than 20 cm3 (p less than 0.005).Furthermore, patients with tumors demonstrating diffuse contrastenhancement survived longer than patients with tumors that had ringenhancement (p less than 0.05). In an MRI study by Barkovich andcolleagues, a significant (p = 0.02) survival advantage was evident formidbrain tumors (Barkovich et al 1990). The 2-year survival forpatients with midbrain tumors was 100%, whereas for patients withmedullary and pontine tumors it was 50% and 20%, respectively. Itwas further noted that patients in whom tumors produced only limitedenlargement of the brainstem, or were focal with limited infiltration,had significantly better survival than patients with more diffuse tumors.This is in contrast to the study by Nelson and colleagues, who noted asignificant correlation (p=0.005) between the onset of necrosis, asimaged by CT or MRI, and subsequent survival (Nelson et al 1994).Over one third of patients with pontine tumors had evidence of necrosisat diagnosis and had a median survival of 6.5 months. For thosepatients who developed necrosis after diagnosis, the median survivalwas 9.0 months. Similar results regarding the presence of necrosishave been reported by others (Guillamo et al 2001). In an MRI studyevaluating the impact of gadolinium enhancement on outcome, nocorrelation was noted overall or within specific subgroups (eg, pons,midbrain) (Fischbein et al 1996). However, only a small number ofpatients were evaluated with both MRI and histological data. Theseresults are in contrast to data from Lesniak and colleagues, whostudied 89 patients with brainstem gliomas and noted thatenhancement within the tumor imparted a positive prognosis (Lesniak
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
21 of 57 03/31/2011 12:46 PM
et al 2003). The majority of these tumors were low-grade andresponded well to aggressive surgical resection. A recent review of MRIfindings in 39 cases of diffuse intrinsic pontine glioma evaluated theprognostic significance of several pretreatment and posttreatmentimaging features, including rostral or caudal tumor extension,metastases, basilar artery encasement, necrosis, intratumoralhemorrhage, enhancement, hydrocephalus, and dorsal exophyticcomponents (Hargrave et al 2008). None of the MRI parameters hadany prognostic significance. In a similar study, Liu and colleaguesattempted to correlate MRI features at presentation with response toradiotherapy (Liu et al 2009). Thirty patients with brainstem gliomawere analyzed; 23 were rated as responders to treatment, whereas 7were classified as nonresponders. There were no statistically significantdifferences in MRI features between the groups. However, necrosis andenhancement were more common in responders, whereas tumorsurrounding the basilar artery, compression of the fourth ventricle, andextension into the cerebellum were more common in nonresponders. Complications of brainstem gliomas vary depending on the size,location, and type of tumor. The most common complication ishydrocephalus, which occurs in 25% to 30% of patients as seen on CTor MRI (Kingsley and Kendall 1979; Bilaniuk et al 1980; Bognar et al1994; Guillamo et al 2001). Hydrocephalus is especially common intumors of the midbrain, midbrain tectum, and cerebral aqueduct, wherethe incidence at diagnosis approaches 100% (Ho 1982; Bognar et al1994; Squires et al 1994). Leptomeningeal tumor spread is acomplication that occurs in 10% to 50% of patients antemortem, but isoften detected more frequently in autopsy studies (Kepes et al 1976;Mantravadi et al 1982; Packer et al 1983; 1992; Silbergeld et al 1988;Grigsby et al 1989a; Shibamoto et al 1989; Maria et al 1993a;Donahue et al 1998; Guillamo et al 2001). The symptoms may bepresent at diagnosis but more often develop during local tumorprogression. Rarely, brainstem tumors can spread outside the CNS,causing extraneural metastases (Kepes et al 1976; Choi et al 1981;Rosemberg et al 1988; Newton et al 1992). Extraneural metastasesusually develop in the context of tumors that have already extendedinto the leptomeninges. Common sites for extraneural metastases fromastroglial brainstem tumors include the lung, pleura, and lymph nodes(Newton et al 1992). In patients with leptomeningeal tumor and ashunting device, spread to the intraperitoneal cavity may occur andcause increased abdominal girth, ascites, and abdominal pain (Newtonet al 1992). Although rare (ie, less than 5%), seizures and otherepisodes of altered consciousness have been reported in brainstemglioma patients (White 1963; Grigsby et al 1989c; Packer et al 1992).Patients with dysphagia may develop pneumonia as a complication oftracheal aspiration of food or oral secretions (Newton et al 1994).Symptoms of aspiration include coughing or choking during intake of
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
22 of 57 03/31/2011 12:46 PM
solids or liquids. However, in some patients with dysphagia, symptomscan be minimal or nonexistent, such that aspiration remains clinicallysilent until pneumonia is well established (Newton et al 1994).
Management The role of surgical therapy is more limited for patients withbrainstem gliomas than for patients with tumors at other sites becauseof the intrinsic risks of aggressive surgery in this location (Packer et al1992; Maria et al 1993a; Mursch et al 2005; Donaldson et al 2006).This is especially true for more diffuse and infiltrative tumors. Despitethese restrictions and limitations, surgical intervention is still animportant aspect of management for many patients with brainstemneoplasms. The morbidity and mortality associated with surgery of thebrainstem have been substantially reduced over the past 15 to 20 yearsdue to improved neuroimaging with MRI, advances in microsurgicalinstrumentation and technique, use of intraoperative real-timeultrasound and evoked potential monitoring, application of the CO2laser and ultrasonic aspirator, and improvements in both open andstereotactic approaches to the brainstem (Albright and Sclabassi 1985;Fasano et al 1986; Hood et al 1986; Pimenta et al 1986; Abernathy etal 1989; Hood and McKeever 1989; Epstein and Wisoff 1990; Rusyniaket al 1992; Rajshekhar and Chandy 1995). In addition, the applicationof computerized 3-D surgical navigation systems for removal ofbrainstem tumors has further improved the ability to resect withminimal morbidity (Wang et al 2000). The ability of MRI to moreaccurately define the anatomy and infiltrative extent of brainstemtumors improves the ability of the neurosurgeon to decide if surgery isfeasible and, more importantly, if it is appropriate (Epstein and Wisoff1990; Packer et al 1992). By MRI classification, tumors most amenableto surgical intervention include focal lesions of the midbrain or pons,cystic astrocytomas without cyst wall enhancement, cervicomedullaryneoplasms, and the exophytic components of tumors (Epstein andWisoff 1988; 1990; Giunta et al 1989; Barkovich et al 1990; Bricolo etal 1991; Packer et al 1992; Pollack et al 1993; Freeman and Farmer1998; Selvapandian et al 1999; Wang et al 2000; Yeh et al 2002).Real-time ultrasound imaging has been reported by many authors as anexcellent method during surgery to verify tumor location, depth, andboundaries (Fasano et al 1986; Rusyniak et al 1992). Variations inechogenicity allow for differentiation of solid tumor from areas ofcalcification, cyst, and edema. Similarly, the use of evoked potentials(auditory or somatosensory) during surgery allows for real-timemonitoring of potential damage to the brainstem and often decreasesmorbidity (Albright and Sclabassi 1985; Fasano et al 1986; Epstein andWisoff 1990; Rusyniak et al 1992). Significant improvements incomputerized CT- and MRI-guided stereotactic techniques have alsocontributed to the reduction of surgical morbidity and mortalityassociated with brainstem tumors. In the majority of reports, surgical
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
23 of 57 03/31/2011 12:46 PM
mortality was 1% to 3%, whereas morbidity ranged between 3% and7% (Hood et al 1986; Frank et al 1988; Giunta et al 1989; Rajshekharand Chandy 1995). A transfrontal or transcerebellar approach to biopsywas used in most of these studies, with diagnostic yields between 90%and 100%. Although modern neurosurgical techniques allow for acceptablemorbidity and mortality when accessing masses within the brainstem ofadults, the literature remains unclear about which lesions should besurgically approached and how aggressive that intervention should be.Many authors feel strongly that all brainstem lesions should at least bebiopsied because of the high rate (10% to 30%) of nonneoplasticlesions that have been reported in many surgical series (Fasano et al1986; Hood et al 1986; Artigas et al 1988; Frank et al 1988; Franziniet al 1988; Abernathy et al 1989; Giunta et al 1989; Rajshekhar andChandy 1995; Xu et al 1997; Massager et al 2000). Nonneoplasticlesions found at biopsy include chronic inflammation, granulomatousinflammation, gliomatosis, cysts, abscesses, infarction, necrosis,tuberculoma, encephalitis, vascular malformations, and regions ofdemyelination. Biopsies are strongly recommended to provide definitivehistological diagnosis prior to further therapeutic recommendations.This approach would prevent patients with nonneoplastic lesions fromreceiving empiric radiation therapy. A significant counter argument isthat biopsies provide small pieces of tissue that may not be diagnosticor that may suggest a lower-grade tumor (Packer et al 1992; Albright1996). In tumors as heterogeneous as gliomas, this can be a significantshortcoming of the technique. Other authors do not feel all patientsshould undergo biopsy or attempted surgical resection, reserving theseprocedures for carefully selected, prognostically favorable patients.Epstein and colleagues recommend an aggressive approach (ie, radicalsubtotal excision) for the more "benign" tumors, based on their reviewof a series of 92 patients classified by MRI and clinical criteria (Epsteinand Wisoff 1988; 1990). Tumors in this "benign" group usually hadlow-grade pathology and included focal, nonenhancing cystic andcervicomedullary lesions. Radical subtotal excision of 50% to 60% offocal and cystic tumors and 80% to 90% of cervicomedullary tumorscould be achieved with the use of evoked potential monitoring,Cavitron ultrasonic surgical aspirator, laser, and intraoperativeultrasound. Most of these patients were neurologically stabilized orimproved following resection and enjoyed prolonged survivals. Incontrast, all diffuse tumors and those with contrast-enhancing cystwalls were histologically malignant and did not benefit from surgicalintervention, except for cyst drainage in tumors with mass effect.Epstein and colleagues recommend surgery only for the carefullyselected "benign" tumors, especially if the intent is to perform aresection. For most diffuse and malignant cystic tumors, the typicalclinical presentation and MRI findings will obviate the need for surgical
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
24 of 57 03/31/2011 12:46 PM
intervention. This view is in agreement with Albright and others, whoargue that in patients with a typical history and clinical presentation ofa brainstem glioma in which the MRI shows a diffuse lesion, surgicalintervention is unnecessary because the histology is virtually alwaysmalignant (Albright et al 1993; Albright 1996; Freeman and Farmer1998; Landolfi et al 1998). More aggressive, open surgical approachesare advocated by other groups to allow for microsurgical resectionswithin the brainstem (Alvisi et al 1985; Fasano et al 1986; Bricolo et al1991; Xu et al 1997). However, radical extirpation has only provedpossible in low-grade tumors (mainly focal or cervicomedullary) thathad pilocytic or grade I/II fibrillary astrocytic histology. Focal tumors ofthe midbrain are reported by some authors as ideal lesions for anaggressive, open approach for microsurgical resection (Pendl et al1990; Pendl and Vorkapic 1991; Lapras et al 1994; Wang et al 2000).In 7 adult patients with focal midbrain tumors who underwentaggressive microsurgical resection by Pendl and Vorkapic, all had eitherstable or improved Karnofsky ratings following surgery (Pendl andVorkapic 1991). The mean survival following surgery was 31.0 months,even though only 2 patients received postoperative radiation therapy.Tumors of the midbrain tectum are also thought to be accessible forresection, although this approach involves more severe mortality(8.3%) and morbidity (33.3%) than a simple biopsy (Lapras et al1994). In a series of 35 midbrain gliomas (mean age 26.6 years),Wang and colleagues used a neuronavigation system to performaggressive resections (Wang et al 2000). Total resection was possiblein 19 cases. Nine patients with malignant histology (AA or glioblastomamultiforme) received postoperative radiotherapy. Twenty-three of thepatients (65.7%) were able to resume independent living. Cysticbrainstem gliomas should be considered for cyst drainage if they arenot amenable to radical excision, as this may improve localizedpressure on brainstem structures (Hood and McKeever 1989; Akhtarand Lewis 1994). In patients with cysts that have recurred followingprior aspiration, after external radiation therapy, or that are causingrapid neurologic deterioration, stereotactic intracavitary placement of32-phosphorus may stabilize further cyst development and result inneurologic improvement (Hood and McKeever 1989). Another subgroupof brainstem tumors that are candidates for aggressive, open surgicalextirpation is dorsally exophytic lesions (Epstein and Wisoff 1990;Bricolo et al 1991; Packer et al 1992; Maria et al 1993a; Pollack et al1993; Xu et al 1997). These tumors are typically slow growing,histologically benign, and noninfiltrative. The majority of patients withdorsally exophytic tumors can undergo radical subtotal resection andenjoy prolonged survival without further therapy (Pollack et al 1993).Recent reports suggest that stereotactic biopsy can be guided by acombination of MRI and PET data (Massager et al 2000; Pirotte et al2007). In a series of 30 patients with brainstem masses, MRI and PET
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
25 of 57 03/31/2011 12:46 PM
were considered complementary in determining the proper location forbiopsy and obtaining diagnostic tissue. In some cases, PET defined a“hot spot” appropriate for biopsy more clearly than the correspondingMRI. However, in 37% of the cases, MRI and PET were discordant withthe pathology and the clinical treatment plan as defined by the finalhistological diagnosis. The authors concluded that although MRI and PETimprove the diagnostic yield when biopsying brainstem mass lesions,neuroimaging alone cannot provide the necessary information to directtreatment in all cases, and histological examination will often berequired. A more recent update by the authors, in a new series of 20patients, verified the original observations of the utility of PET toimprove the targeting of stereotactic biopsy for brainstem gliomas(Pirotte et al 2007). In addition, authors have been using intraoperativeMRI for more detailed information regarding surgical approach andextent of resection (Lam et al 2001). The use of MRI guidance shouldbe even more helpful in adults with brainstem gliomas because therewill be more room to maneuver in the posterior fossa. Adult patients with dorsal midbrain tumors (ie, tectal) are considereda special, indolent subgroup that should be carefully evaluated beforeattempting aggressive intervention (Yeh et al 2002). After a review of5 patients, Yeh and colleagues concluded that most of these patientscan be followed by serial MRI scans and may remain stable withoutintervention, except for occasional diversionary shunting. Tumor-specific therapy should be reserved for patients with clinical or MRIevidence of growth. A recent review of microneurosurgical treatment in a series of 16consecutive adult patients was not as favorable as some of the resultsnoted above (Mursch et al 2005). Of the 16 patients, 9 had diffusepontine tumors, 6 had more craniocaudal-oriented lesions, and 1 had acystic tumor of the pons. Gross total resection was achieved in only 2patients, whereas another 9 had subtotal resections. Postoperatively,11 patients experienced neurologic deterioration, with significantrecovery noted in only 4 of the cohort. The authors suggested that therate of recovery after surgery was much less than what is reported inpediatric brainstem glioma patients treated with surgery. In addition,they questioned the benefit of surgical intervention in adult patientswith brainstem glioma. After reviewing the neurosurgical literature, the current author doesnot recommend a surgical biopsy or attempted resection in thosepatients with a classic, diffuse brainstem glioma as defined by MRI.The vast majority of these tumors will have high-grade histology andbehave in a malignant fashion. All other brainstem masses should atleast undergo an attempted biopsy, due to the high rate ofnonneoplastic lesions found in many series. In the hands of anexperienced neurosurgeon, carefully selected brainstem tumors (focalmidbrain, dorsally exophytic, nonenhancing cystic, cervicomedullary,
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
26 of 57 03/31/2011 12:46 PM
etc.) can undergo radical subtotal resection. Once the diagnosis of brainstem glioma has been made, by eithersurgery or MRI, the mainstay of therapy in most adult patients will beexternal beam radiation therapy. Early reports from the pre-CT and CTera demonstrated a dose-response effect in brainstem gliomas.Extended survival only occurred in those patients receiving 4500 cGy ormore. Additional conventional radiation therapy trials have used focalports utilizing doses ranging from 4400 to 6500 cGy, with the majorityof patients receiving more than 5000 cGy (Grigsby et al 1989b; 1989c;Shibamoto et al 1989; Guiney et al 1993; Guillamo et al 2001;Donaldson et al 2006; Hargrave et al 2006). In the study by Shibamotoand colleagues, which included 27 adults (61% with high-gradetumors), 77% of patients with noncontrast-enhancing tumors, 64% ofthose with diffuse contrast-enhancing tumors, and 50% of tumors withring enhancement demonstrated a complete or partial response(Shibamoto et al 1989). Despite these promising initial results, theoverall 5-year survival rate was only 23%. A similar 5-year survivalrate of 28.7% was noted by Grigsby and colleagues in a cohort of 27adult patients (Grigsby et al 1989b). In an analysis of 21 adult patientswith pontine gliomas, Guiney and colleagues noted clinical orradiological improvement in 77% (Guiney et al 1993). However, themedian survival was only 15 months, with a 3-year survival rate of33%. In a review of 37 patients with midbrain tumors (16 over 16years of age) treated with conventional radiation doses of 4500 to 5000cGy, Franklin noted an overall median survival of 10 months, with a2-year survival rate of 23% (Franklin 1991). If the patients receivingmore than 5000 cGy were analyzed separately, the median survivalincreased to 14.5 months. Because of the evidence for a dose-response effect with conventionalirradiation and the fact that brainstem tumors are mainly a focaldisease, alternative treatment schedules have been studied in anattempt to administer higher total doses without an increase inneurotoxicity (Packer et al 1992; Maria et al 1993a). The mostpromising alternative schedule is hyperfractionated radiation therapy, inwhich a larger number of smaller fractions (eg, 100 to 120cGy/fraction, twice daily) are administered over an equivalenttreatment interval to a larger total dose (eg, 6800 to 7800 cGy). Therationale for hyperfractionation relates to frequency of fractions, doseper fraction, total dose, repair of sublethal radiation damage, andoxygen dependence, which have been reviewed elsewhere (Edwards etal 1989; Linstadt et al 1991; Packer et al 1992; Shrieve et al 1992;Maria et al 1993a). Hyperfractionated protocols have demonstratedmarginal improvement in overall and progression-free survival inpediatric patients with brainstem gliomas at doses between 7000 and7200 cGy (Packer et al 1992; Maria et al 1993a; Hargrave et al 2006).There have been few reports of hyperfractionated protocols for adult
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
27 of 57 03/31/2011 12:46 PM
patients with brainstem gliomas. The earliest study was from Edwardsand colleagues, who evaluated 19 adults as part of a larger cohort in aphase I-II trial of 100 cGy twice a day to a total dose of 7200 cGy(Edwards et al 1989). After the completion of radiotherapy, themajority of patients had stable disease as indicated by MRI, whereasless than a third showed reduction in tumor volume. The mediansurvival was 7.6 months, with a median time to tumor progression of5.5 months. In the study by Linstadt and colleagues, 14 adult patientswere treated with hyperfractionated radiation (100 cGy twice a day) toa median dose of 7200 cGy (Linstadt et al 1991). All but 1 patientimproved or remained neurologically stable following treatment. The3-year actuarial survival rate was 59%, with a projected mediansurvival in excess of 5 years. However, there were no glioblastomamultiforme patients in this cohort; most had moderately anaplasticastrocytomas. Shrieve and colleagues analyzed the results of a cohortthat included 45 adult patients who received between 6600 and 7800cGy of hyperfractionated radiotherapy (Shrieve et al 1992). Themedian survival was 15.8 months, with 1- and 2-year survival rates of68% and 53%, respectively. Survival was not significantly different forpatients who received doses greater than 7200 cGy and those withdoses less than or equal to 7200 cGy. When comparing these resultswith their previous experience in adult brainstem glioma patients usingconventional radiotherapy, there was a trend toward improved outcomewith hyperfractionation (p = 0.08). Their conclusion was thathyperfractionated radiotherapy was an effective treatment for adultswith brainstem gliomas and that 7200 cGy was the preferred dosage. Ina review of patients who had received 7800 cGy of hyperfractionatedradiotherapy, Prados and colleagues included 45 adults (Prados et al1995). Tumor size, as indicated by CT or MRI, decreased in 30%, wasstable in 39.5%, and increased in 29.6%. The median survival of theadult patients was 16.1 months, with a median time to tumorprogression of 11.4 months. The median survival was almost identicalto that reported by Shrieve and colleagues using 7200 cGy, promptingthe authors to conclude that hyperfractionated radiation therapy to7800 cGy did not improve survival and was associated with greatertoxicity. Several studies in adults and children suggest thathyperfractionated protocols do not impart a survival advantage overconventional radiation treatment (Botturi and Fariselli 1998; Freemanand Farmer 1998; Schild et al 1998; Mandell et al 1999; Hargrave et al2006). In a pediatric study by Mandell and colleagues, 132 children withdiffuse brainstem tumors were randomized to receive eitherconventional (180 cGy/day, 5400 cGy total) or hyperfractionated (117cGy twice per day, 7020 cGy total) irradiation over 6 weeks incombination with cisplatin chemotherapy (Mandell et al 1999). Themedian time to progression was 6 months for conventional therapy and5 months for hyperfractionated treatment. Similarly, median survival
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
28 of 57 03/31/2011 12:46 PM
was 8.5 months for conventional therapy and 8 months for patientsreceiving hyperfractionation. In a study from the Mayo Clinic, 40patients (median age 29.5 years) with brainstem tumors were reviewedfor response to irradiation; 9 of the patients received hyperfractionatedtherapy (Schild et al 1998). No survival advantage could bedemonstrated in the cohort treated with hyperfractionated radiotherapy. In an attempt to improve efficacy of radiotherapy, severalinvestigators have begun to use radiosensitizers. Marcus and colleaguesadded etanidazole, a hypoxic-cell sensitizer, to 66 Gy ofhyperfractionated irradiation in a phase I study of 18 children withbrainstem glioma (Marcus et al 2003). The maximum tolerated dose ofetanidazole was 42 mg/m2, with cutaneous rash as the dose-limitingtoxicity. A similar phase I study by Sanghavi and colleagues usedtopotecan in combination with conventional radiotherapy for 17 childrenwith brainstem tumors (Sanghavi et al 2003). Topotecan is atopoisomerase I inhibitor that is known to convert sublethal radiation-induced DNA damage into lethal double-strand DNA breaks. Themaximum tolerated dose of topotecan was 0.40 mg/m2 per day duringradiotherapy, with neutropenia as the dose limiting toxicity. Asubsequent phase II study of topotecan and concomitant irradiationused the same dosing schedule in a series of 32 patients withmalignant diffuse brainstem gliomas (Bernier-Chastagner et al 2005).In 40% of the cohort, partial responses were noted. However, theresponses were short-lived, and the 12-month survival rate was only25.5%. In addition, the overall median survival was only 8.3 months,similar to other studies of radiation therapy alone. The authorsconcluded that the addition of topotecan could not be recommended.Another recent approach has been to add weekly RMP-7 (300 ng/kg)and intravenous carboplatin (35 mg/m2 per day) during the course ofirradiation in a phase I trial of newly diagnosed brainstem gliomapatients (Packer et al 2005). RMP-7 is a bradykinin analog thattransiently increases permeability across the blood-brain barrier andmay allow higher concentrations of carboplatin to reach tumor cells.The treatment was relatively well tolerated, but no conclusions could bedrawn regarding efficacy of the protocol, although the estimatedmedian survival of the cohort was more than 11 months. A similarphase II study using a different dosing regimen of RMP-7 (600 ng/kg)and intravenous carboplatin (target AUC of 3.5 mg per min/ml per day)was applied to 12 patients with brainstem and other high-grade gliomas(Warren et al 2006). Although the regimen was relatively well toleratedexcept for hematological toxicity, none of the brainstem gliomapatients responded. Although brachytherapy has demonstrated improved survival forpatients with supratentorial gliomas, few authors have applied thistechnique to brainstem tumors because of the inherent dangers ofradiation exposure in this location. Mundinger and colleagues have used
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
29 of 57 03/31/2011 12:46 PM
iodine-125 and iridium-192 as temporary or permanent radiationsources for 55 patients (mean age 22.5 years) with nonresectablelow-grade brainstem gliomas, most of which were focal lesions of themidbrain (Mundinger et al 1991). The majority of patients (61%) hadpilocytic astrocytomas, whereas all others had low-grade protoplasmicor fibrillary astrocytomas. The 5-year survival rates were 54.8% for theiodine-125 group and 26.9% for the iridium-192 group; these rateswere marginally significantly different (p = 0.03). Mortality for theprocedure was 2.4%, with a morbidity of 6.2%. Radiosurgery is a technique that is able to deliver photon radiation towell-circumscribed volumes of tumor deep within the brain. Severalauthors have applied it to patients with brainstem gliomas (Loeffler etal 1992; Kihlstrom et al 1994; Schulz-Ertner et al 2000; Fuchs et al2002; Donaldson et al 2006; Yen et al 2007; Combs et al 2009). Intheir series of 7 patients with midbrain tectal low-grade gliomas whoranged in age from 6 to 40 years (mean 18 years), Kihlstrom andcolleagues administered doses of 1400 to 3500 cGy in 1 fraction using asingle isocenter (Kihlstrom et al 1994). In 5 of the 7 cases, the tumorshrank progressively after treatment. All 7 patients remain alive, withmean follow-up time of 6 years. Patients treated with the higher doses(eg, 1800 to 3500 cGy) developed significant complications, includingradionecrosis and progression of neurologic deficits. The authorsconcluded that radiosurgery was useful adjunctive therapy in this groupof tumors when using a recommended dose of 1200 to 1400 cGy.Loeffler and colleagues, in their series of 41 malignant glioma patientstreated with radiosurgery, included 1 adult with a brainstemglioblastoma multiforme (Loeffler et al 1992). That patient received1000 cGy to the 80% isodose line following external beamradiotherapy. Treatment has resulted in a partial response, with clinicalimprovement and cessation of steroids after 6 months of follow-up. Ina series of 41 patients with brainstem glioma (26 adults), Schulz-Ertnerand colleagues used fractionated stereotactic conformal radiosurgerywith a linear accelerator (Schulz-Ertner et al 2000). The field wasshaped with a multileaf collimator, for a median total dose of 5400 cGyto the 90% isodose line. Clinical improvement was noted in 19 of 41patients (46.3%), whereas objective radiological responses occurred in12 of 41 patients (29.3%). Median time to progression was 23 months,with a median overall survival of 40 months. The treatment wastolerated well and the authors concluded that this approach wassuperior to conventional irradiation with parallel-opposed ports due tothe use of a smaller, more precise treatment volume. Fuchs andcolleagues used gamma knife radiosurgery with a median dose of 12Gy for a series of 21 patients with brainstem gliomas that were mostlyadult (median age 23 years) (Fuchs et al 2002). Ten patientsresponded with stable disease, whereas 3 had objective responses.Clinical improvement was noted in 5 patients. The median overall
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
30 of 57 03/31/2011 12:46 PM
survival was 20.7 months. A recent report describes the use of GammaKnife as the primary method of treatment in 20 patients with focalbrainstem lesions (Yen et al 2007). There were 4 complete responsesand 12 partial responses/minor responses during a mean follow-upperiod of 78.0 months. The remaining patients were stable or clinicallyimproved. A recent report by Combs and colleagues described the results ofusing fractionated stereotactic radiosurgery in a cohort of 85 patientswith brainstem gliomas (Combs et al 2009). The median age atprimary diagnosis was 26 years of age, with only 31 patients under 18years of age. A median dose of 54 cGy was administered in 1.8 Gyfractions to a median target volume of 101 mL. The medianprogression-free survival (PFS) was 52 months, with PFS rates at 12and 24 months of 70% and 63%, respectively. Radiosurgery was welltolerated and did not appear to have a dose-response relationship inthis group of patients. Patients who are suspected of having leptomeningeal metastasis froma brainstem glioma should be evaluated on an individual basis and, ifclinically indicated, undergo an evaluation of CSF (including cytologyand tumor markers such as beta-glucuronidase and beta2-microglobulin), MRI of the spine with gadolinium, and myelography(Packer et al 1983; 1992). In patients without evidence of infection,abnormal levels of tumor markers can improve diagnostic sensitivity.Patients with proven leptomeningeal seeding should then be consideredfor craniospinal axis irradiation and intrathecal chemotherapy. Typicaldoses for craniospinal axis irradiation are 3000 to 3500 cGy. In patientswith clinical and imaging evidence for focal bulky involvement byleptomeningeal tumor, radiation can be administered to a localizedfield with generous margins, using doses of 3500 to 4500 cGy. Over the past 2 decades, chemotherapy has had little impact on theoverall survival of patients with brainstem gliomas (Packer et al 1992;Maria et al 1993a; Freeman and Perilongo 1999; Donaldson et al 2006;Hargrave et al 2006). The vast majority of data regardingchemotherapy are from the pediatric literature, as summarized byMaria and colleagues (Maria et al 1993a). A compilation of 18 studiesusing various chemotherapy regimens for brainstem tumors in childrenencompasses 261 patients. Of this cohort, 48 patients (18.4%)responded, including 21 with partial responses and 27 with stabledisease; there were no complete responses. The most effective singleagents were carboplatin and cyclophosphamide. Unfortunately, all ofthe responses were brief, as tumors rapidly progressed throughchemotherapy. A phase III trial of irradiation with or without adjuvantlomustine, vincristine, and prednisone was reported by Jenkin andcolleagues (Jenkin et al 1987). The overall 5-year survival rate was20% for both groups, suggesting that chemotherapy did notsignificantly affect outcome. In the study by Levin and colleagues, 28
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
31 of 57 03/31/2011 12:46 PM
patients (including 2 adults) were treated with 5-fluorouracil andlomustine before irradiation, followed by hydroxyurea and misonidazoleduring radiotherapy (Levin et al 1984). The median survival was 11months, which, when compared with prior trials, was no better thanradiation therapy alone. Similarly, a Children's Cancer Group studycombining hyperfractionated radiotherapy (7200 cGy) and intravenousrecombinant beta-interferon did not demonstrate improved efficacyover conventional radiotherapy alone (median time to progression 5months; median survival 9 months) (Packer et al 1996). Severalstudies have attempted high-dose chemotherapy with autologous bonemarrow transplantation in pediatric brainstem glioma patients (Bouffetet al 1997; 2000; Dunkel et al 1998). Bouffet and colleagues usedhigh-dose BCNU (800 mg/m2) on 8 patients with brainstem glioma(Bouffet et al 1997). One patient briefly stabilized for a few monthswhereas the other 7 patients rapidly progressed. In a similar study of24 children with diffuse pontine gliomas, Bouffet and colleagues usedhigh-dose busulfan (150 mg/m2) and thiotepa (300 mg/m2) followedby autologous bone marrow transplantation (Bouffet et al 2000). Themedian time to clinical progression was 5 months, with an overallmedian survival of 10 months. Dunkel and colleagues used high-dosethiotepa and etoposide, either alone or in combination with BCNU orcarboplatin, in 16 patients with diffuse pontine tumors (Dunkel et al1998). The median survival was 4.7 months for patients with recurrentdisease and 11.4 months for patients with newly diagnosed tumors.High-dose therapy did not improve survival over conventionaltreatment and was associated with considerable toxicity. A Children'sCancer Group study used intravenous idarubicin (5 mg/m2 per day for3 days, every 21 days) for patients with relapsed brain tumors,including 13 with brainstem gliomas (Arndt et al 1998). None of the 12brainstem glioma patients able to be evaluated responded totreatment. In an attempt to increase dose intensity for newlydiagnosed malignant glioma patients, Jakacki and colleagues usedtime-compressed, dose-intensive lomustine, procarbazine, andvincristine in combination with peripheral blood stem-cell support andconcurrent irradiation (Jakacki et al 1999). Of their cohort of 6 patientswith diffuse pontine brainstem gliomas, 2 had partial responses and 1had a minor response. The median time to radiographic progressionwas 5 months, with a median overall survival of 11 months. In asimilar study of 22 assessable patients with newly diagnosed brainstemgliomas, Broniscer and colleagues used a combination of irradiation andconcurrent tamoxifen (200 mg/m2 per day) (Broniscer et al 2000).There were 8 partial responses, 3 minor responses, and 8 patients withstable disease. The overall median survival was 10.3 months. Allen andcolleagues performed a phase I/II trial of intravenous carboplatin andhyperfractionated irradiation (100 cGy twice a day; 7200 cGy totaldose) in 34 children with brainstem gliomas (Allen et al 1999). The
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
32 of 57 03/31/2011 12:46 PM
maximum tolerated dose of carboplatin was 110 mg/m2 over 7 weeksof radiation. The median progression-free survival was 8 months andthe overall survival was 12 months. A phase II study by the Children'sCancer Group compared preirradiation carboplatin, etoposide, andvincristine versus cisplatin, cyclophosphamide, etoposide, andvincristine (Jennings et al 2002). Neither regimen was able to improveresponse rate, time to progression, or overall survival relative to priorstudies of brainstem glioma patients treated with radiotherapy with orwithout chemotherapy. In a phase II study by Burzynski andcolleagues, intravenous bolus injections of antineoplaston A10 andAS2-1 were administered to a series of 12 patients with recurrentbrainstem gliomas, including 1 adult and 4 teenagers (Burzynski et al2003). Five patients had brief objective responses, for a 2-year survivalrate of 33.3%. More recently, Ronghe and colleagues reported theirexperience using vincristine and carboplatin for pediatric patients withunresectable and/or recurrent low-grade astrocytomas of the brainstem(Ronghe et al 2010). Sixteen patients received treatment, and all werestill alive at the time of the report, with 9 objective responses onneuroimaging (1 complete response, 8 partial responses/minorresponses), and another 4 that remained stable. Overall, 68% of thecohort remained progression-free, with a median follow-up of 57months. Few chemotherapy studies of brainstem gliomas have included morethan a few adult patients. However, the experience with chemotherapyin adults has been similar to that of children, with few durableresponders (Landolfi et al 1998; Schild et al 1998). In a review of 21patients treated with 5-fluorouracil, lomustine, hydroxyurea, and6-mercaptopurine at progression after radiation therapy, Rodriguez andcolleagues included 4 adults (Rodriguez et al 1988). The ages rangedfrom 16 to 25 years, with a mean of 19.75 years. The overall meansurvival of the adult cohort was 11.9 months, with a mean time toprogression of 5.1 months. Chamberlain has used chronic oral etoposide(50 mg/m2 per day for 21 days every 5 weeks) to treat 12 patients,including 4 adults (age range 18 to 49 years), with recurrent brainstemgliomas (Chamberlain 1993). The overall results demonstrated 6radiographic responses with a median duration of response of 8months. Of the adult patients, 2 had partial responses of 4 and 12months' duration, whereas the remaining 2 had progressive disease. Ina group of 3 adult patients (age range 18 to 59 years) with pontinegliomas given chemotherapy after irradiation, Fujiwara and colleaguesused monthly intraarterial ACNU (80 mg/m2), cisplatin (40 mg/m2), orcarboplatin (300 mg/m2) in addition to oral etoposide (25 mg/day) andintravenous beta-interferon (Fujiwara et al 1994). One patient with agrade II astrocytoma had a complete response after 8 cycles ofintraarterial carboplatin and remained in remission 24+ months afterdiagnosis. Another patient with an anaplastic astrocytoma had a partial
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
33 of 57 03/31/2011 12:46 PM
response to ACNU that lasted through 4 cycles of treatment, followedby progression and expiration 14 months after diagnosis. The lastpatient had a grade II astrocytoma that did not initially respond toACNU, but did demonstrate a partial response to intraarterial cisplatinthat lasted for 3 cycles (survival 15 months). The authors concludedthat this regimen was well tolerated and effective in brainstem gliomapatients. In 2 studies of adult brainstem glioma patients reported fromMemorial Sloan-Kettering Cancer Center and the Mayo Clinic,chemotherapy was unable to significantly impact survival (Landolfi etal 1998; Schild et al 1998). Trofosfamide is an alkylating agent with asimilar structure to cyclophosphamide but with improved lipid solubilityand excellent enteral absorption. Wolff and colleagues were unable todemonstrate any survival benefit in a trial of trofosfamide (100 mg/m2per day) and etoposide (40 mg/m2 per day) when added to irradiationin a group of pediatric patients with glioblastoma multiforme, including8 with tumors of the brainstem (Wolff et al 2000). These results werecorroborated by the same group in another study with an enlargedcohort of 20 patients with pontine glioma (Wolff et al 2002). A recent multi-institutional study evaluated the use of temozolomide(200 mg/m2 x 5 days every 28 days for 6 cycles) after the completionof irradiation in newly diagnosed patients with brainstem glioma(Broniscer et al 2005). Thirty-three patients were treated, includingseveral young adults. The median time to progression was 8.8 months,with a median overall survival and 1-year survival rate of 12 monthsand 48%, respectively. The authors concluded that temozolomide wasnot very active in this group of patients and did not improve their poorprognosis. An Italian study in adult patients with brainstem gliomaseems to corroborate this pediatric data. Salmaggi and colleaguestreated 18 adults with chemoradiation using temozolomide (75mg/m2/day), followed by up to 9 cycles of adjuvant temozolomide(200 mg/m2/day x 5 days). The addition of temozolomide toirradiation did not seem to add any survival benefit and did not resultin any complete or partial responses (Salmaggi et al 2008). The lack ofimproved treatment response when temozolomide is added toradiotherapy has been verified in a recent report of a group of pediatricbrainstem glioma patients (Chiang et al 2010). Hall and colleaguesreport an aggressive approach to chemotherapy of diffuse pontineglioma, using intraarterial carboplatin or methotrexate in combinationwith blood-brain barrier disruption (BBBD) and intravenouscyclophosphamide and etoposide (Hall et al 2006). Eight patients (1adult, 2 teenagers) received the regimen, resulting in 2 partialresponses and 5 stable diseases, with a median time to tumorprogression of 15 months. The overall median survival of the cohortwas 27 months. Bevacizumab is a new chemotherapy drug recently approved by theU.S. Food and Drug Administration for treatment of recurrent
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
34 of 57 03/31/2011 12:46 PM
glioblastoma multiforme (Newton 2009). It is a humanized monoclonalantibody targeted against vascular endothelial growth factor and haspotent antiangiogenic and antiedema activity. Several recent casereports suggest that bevacizumab may have activity in some adultpatients with brainstem gliomas (Raza and Donach 2009; Torcuator etal 2009). In the first report by Torcuator and colleagues, the authorsdescribed a 43-year-old woman with a diffuse pontine tumor whoinitially received chemoradiation with temozolomide (Torcuator et al2009). She progressed after only 1 cycle of adjuvant temozolomide andwas then started on combination therapy with bevacizumab andirinotecan every 2 weeks. After 8 months of treatment, the patientexperienced improvement in neurologic function, and the MRI scanshowed some reduction in FLAIR abnormality and enhancement.Irinotecan was stopped because of fatigue and neutropenia;bevacizumab was continued for another 4 months. The patient hasremained stable off treatment. Raza and Donach described an adultpatient with a newly diagnosed brainstem glioma who receivedradiotherapy in combination with temozolomide and bevacizumab,followed by adjuvant treatment with both drugs (Raza and Donach2009). This patient also had improvement of FLAIR and enhancementon MRI scan, and now remains stable off treatment after 30 months.Another case report describes the use of intraarterial bevacizumab, incombination with mannitol-induced disruption of the blood-brainbarrier, in a 43-year-old male with a recurrent malignant brainstemglioma (Riina et al 2010). The procedure was well tolerated, withpostprocedure imaging showing a reduction in enhancement within thetumor. There were no procedural or vascular complications from thetreatment. In a recent report from the Pediatric Brain TumorConsortium of 17 patients with recurrent diffuse pontine glioma, thecombination of bevacizumab and irinotecan did not appear to have anysignificant activity in terms of clinical stabilization or by neuroimagingcriteria (Gururangan et al 2010). Animal work by Sandberg and colleagues suggests that convection-enhanced delivery of chemotherapy may be applicable to brainstemgliomas (Sandberg et al 2002). In studies using rats, it was determinedthat one-time convection-enhanced chemotherapy infusions could besafely applied to the brainstem. Convection-enhanced deliverybypasses the blood-brain barrier and can achieve high localconcentrations of infusate. Further studies will evaluate the tolerabilityof multiple infusions and the use of various forms of chemotherapy.Another series of studies in rats has tested the safety and tolerabilityof interstitial infusion of IL13-PE38QQR into the brain stem(Souweidane et al 2004). IL13-PE38QQR is a recombinant immunotoxincomprised of a modified Pseudomonas exotoxin moiety conjugated tothe human derived T-cell cytokine, IL-13. Infusion of IL13-PE38QQRinto the pons at a concentration of 10 µg/ml for up to 2 weeks was well
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
35 of 57 03/31/2011 12:46 PM
tolerated without clinical or histological toxicity. Similar studies inprimates have evaluated the safety and toxicity of chronic carboplatininfusions directly into the pons (Storm et al 2003). Overall, infusion ofcarboplatin up to 0.26 mg/ml for 1 month was well tolerated withoutsignificant clinical or radiographic toxicity. Neurotoxicity was noted forinfusion doses of 2.6 mg/ml for 1 month. Further studies from thesame authors in a monkey model have infused carboplatin into thepons at 0.42 µl/h to deliver 0.025, 0.075, 0.25, and 0.75 mg/kg by day30 (Strege et al 2004). Lethargy and ataxia were noted after 2 weeksin animals given 0.25 mg/kg and after 4 weeks in animals given 0.075mg/kg. Lower doses were tolerated well without systemic orneurotoxicity. More recent studies of convection-enhanced deliveryusing a rat model verified the safety of infusion using 1, 2, or 3catheters. However, when the catheters were used to infusecarboplatin, drug-related neurotoxicity was noted. Mild neurologicdeficits that developed in the animals after cannula implantationresolved in the placebo group but were more permanent in thecarboplatin treated animals. The authors stressed the development ofless neurotoxic chemotherapy drugs to be used for this kind of regionalchemotherapy (Thomale et al 2009). The current author has used chemotherapy to treat 3 adult patientswith brainstem glioma who ranged in age from 33 to 63 years (mean47.3 years). The first patient was a 63-year-old man with a rightmidbrain anaplastic astrocytoma that remained stable for 7 monthsduring monthly intravenous carmustine (200 mg/m2). Thetumor was unchanged when the patient expired from aspirationpneumonia. The second patient is a 47-year-old woman with a pilocyticastrocytoma of the left middle cerebellar peduncle that had progressedbefore and after radiation therapy. She has been treated with orallomustine (110 mg/m2) and intravenous vincristine (1.4 mg/m2) every6 weeks and remains stable during the first 9 months of therapy. Thethird patient is a 32-year-old woman with a large brainstem anaplasticastrocytoma centered in the pons. She has been treated with 6monthly cycles of intraarterial carboplatin (200 mg/m2 for 2 days) andintravenous etoposide (100 mg/m2 for 2 days), resulting in a partialresponse (defined as a 50% to 99% reduction in tumor volume on CTor MRI). The management of the general aspects of care of adultpatients with brainstem gliomas is similar to that of patients with otherbrain tumors (Newton 1994). In those rare patients with seizures,adequate control can usually be achieved with first-line agents likephenytoin or carbamazepine. Monotherapy should always be attemptedwith both agents before considering a second-line agent such asvalproic acid, gabapentin, or phenobarbital. Because the majority ofbrainstem glioma patients have some degree of elevated intracranial orlocalized tumor-related pressure, dexamethasone should be prescribedin the lowest dose that will improve symptoms (eg, 1 to 4 mg 4 times
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
36 of 57 03/31/2011 12:46 PM
daily) (Packer et al 1992; Newton 1994). Following stabilization ofpressure-related symptoms and initiation of more definitive therapy,dexamethasone should be carefully tapered to minimize potentialcomplications (Newton 1994). Dysphagia is a relatively commonproblem in brainstem glioma patients because of tumor-relateddamage to medullary swallowing centers (Newton et al 1994). In allpatients with symptoms of dysphagia, regardless of the apparentseverity of the complaints, a thorough swallowing evaluation should beperformed. Patients with incipient or well-established hydrocephalusshould be evaluated and, if appropriate, treated with a CSFdiversionary shunt procedure (Packer et al 1992; Maria et al 1993a).
Pregnancy Pregnancy does not affect the clinical behavior of brainstem gliomas.
Anesthesia Several anesthetic concerns specific to brainstem gliomas are nottypically encountered with other brain tumors. In rare patients,especially adults, tumors may involve regions within the medulla orpons that affect respiration and blood pressure control (Rodriguez et al1982; Hsu et al 1984; Tobias and Heideman 1991; Valente et al 1993).Apnea, hypoventilation, and hyperventilation may occur when abrainstem tumor damages the lower brainstem pathways and nuclearregions responsible for respiratory control (Rodriguez et al 1982; Kunaet al 1991; Tobias and Heideman 1991; Valente et al 1993). Thealterations in PaO2, PaCO2, and pH caused by these respiratoryconditions may affect the approach to anesthesia. Abnormal bloodpressure control, especially orthostatic hypotension and secondarycardiac syncope, can also develop in these patients due to disturbancesof central autonomic control and the afferent arc of the baroreceptorreflex (Hsu et al 1984). In those patients particularly at risk, cardiacpacing should be considered. In addition, concerns regarding the presence or absence of elevatedintracranial pressure during the induction, maintenance, and emergencefrom anesthesia are common to surgical therapy of any brain tumor(LaSala et al 1991). In patients with brainstem gliomas who haveelevated intracranial pressure, care should be taken withpremedications to avoid agents that produce excessive sedation andventilatory depression, as these could exacerbate intracranial pressure.Hypotonic fluids should also be avoided whenever possible. During theinduction and maintenance of anesthesia, agents should be chosen thatminimize hypertension, cerebral vasodilation, chest wall rigidity, andhypercapnia (LaSala et al 1991). The author would like to thank Dr. Carl Boesl for his efforts inpreparing the neuropathological slides and Mr. David Carpenter forexpert editorial assistance.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
37 of 57 03/31/2011 12:46 PM
ICD codesICD-9:Malignant neoplasm of brain stem: 191.7 ICD-10:Malignant neoplasm of brain stem: C71.7
OMIMGlioma of brain, familial: #137800
Associated disordersMedullary astrocytomaMidbrain astrocytomaNeurofibromatosis type 1Pilocytic brainstem gliomaPontine astrocytoma
Related summariesBrainstem gliomas in childhoodCerebellar astrocytomaLow-grade gliomas (astrocytomas)Malignant astrocytomasNeurofibromatosis type 1Neurofibromatosis type 1 and intracranial neoplasms of childhoodPilocytic astrocytoma in adults
Differential diagnosisother mass lesions or diseasesprogressive brainstem syndromeother neoplasmsparasitic cystsviral brainstem encephalitispostviral brainstem encephalitisinfarctiontuberculomademyelinating syndromesvascular malformationsabscessesradionecrosischronic meningitismetastases to brainstem or posterior fossaprimary brain tumors of posterior fossa or skull basemeningiomaacoustic schwannomadermoid cystmedulloblastoma
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
38 of 57 03/31/2011 12:46 PM
ependymomaepidermoid cystviral encephalitis involving brainstemchronic meningitis with basilar exudatetuberculosiscryptococcus neoformansmultiple sclerosispostinfectious brain encephalitisbrainstem infarctionbrainstem metastaseshemorrhagevascular malformationsarteriovenous malformationcapillary telangiectasiacavernous angiomanonneoplastic lesionnonspecific chronic inflammationgranulomatous inflammationepidermoid cystpyogenic abscesscryptococcal abscesscysticercosisencephalitisposterior fossa metastases
DemographicsFor more specific demographic information, see the Epidemiology,Etiology, and Pathogenesis and pathophysiology sections of this clinicalsummary.
Age19-44 years45-64 years65+ years
PopulationNone selectively affected.
OccupationNone selectively affected.
Sexmale=female
Family historyfamily history may be obtained
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
39 of 57 03/31/2011 12:46 PM
Heredityheredity may be a factor
References citedAbernathy CD, Camacho A, Kelly PJ. Stereotaxic suboccipitaltranscerebellar biopsy of pontine mass lesions. J Neurosurg1989;70:195-200. Akhtar N, Lewis TT. Management of midbrain cyst with repeated CTguided aspiration. Neuroradiology 1994;36:642-3. Albright AL. Diffuse brainstem tumors: when is a biopsy necessary?Pediatr Neurosurg 1996;24:252-5. Albright AL, Guthkelch AN, Packer RJ, Price RA, Rourke LB. Prognosticfactors in pediatric brain-stem gliomas. J Neurosurg 1986;65:751-5. Albright AL, Packer RJ, Zimmerman R, Rorke LB, Boyett J, HammondGD. Magnetic resonance scans should replace biopsies for the diagnosisof diffuse brain stem glioma: a report from the Children's CancerGroup. Neurosurgery 1993;33:1026-30. Albright AL, Sclabassi RJ. Use of the Cavitron ultrasonic surgicalaspirator and evoked potentials for the treatment of thalamic and brainstem tumors in children. Neurosurgery 1985;17:564-8. Allen J, Siffert J, Donahue B, et al. A phase I/II study of carboplatincombined with hyperfractionated radiotherapy for brainstem gliomas.Cancer 1999;86:1064-9. Alvarez JA, Cohen ML, Hlavin ML. Primary intrinsic brainstemoligodendroglioma in an adult. Case report and review of the literature.J Neurosurg 1996;85(6):1165-9. Alvisi C, Cerisoli M, Maccheroni ME. Long-term results of surgicallytreated brainstem gliomas. Acta Neurochir 1985;76:12-7. Arndt CA, Krailo MD, Steinherz L, Scheithauer B, Liu-Mares W, ReamanGH. A phase II clinical trial of idarubicin administered to children withrelapsed brain tumors. Cancer 1998;83:813-6. Artigas J, Ferszt R, Brock M, Kazner E, Cervos-Navarro J. Therelevance of pathological diagnosis for therapy and outcome of brainstem gliomas. Acta Neurochir Suppl 1988;42:166-9. Badhe PB, Chauhan PP, Mehta NK. Brainstem gliomas - Aclinicopathological study of 45 cases with p53 immunohistochemistry.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
40 of 57 03/31/2011 12:46 PM
Indian J Cancer 2004;41:170-4. Bailey P. Concerning diffuse pontine gliomas in childhood. ActaNeuropathol Esthoniana 1935;60:199-214. Barkovich AJ, Krischer J, Kun LE, et al. Brain stem gliomas: aclassification system based on magnetic resonance imaging. PediatrNeurosurg 1990-91;16:73-83. Bernier-Chastagner V, Grill J, Doz F, et al. Topotecan as aradiosensitizer in the treatment of children with malignant diffusebrainstem gliomas: results of a French Society of Paediatric OncologyPhase II Study. Cancer 2005;104(12):2792-7. Bilaniuk LT, Molloy PT, Zimmerman RA, et al. Neurofibromatosis type1: brain stem tumours. Neuroradiology 1997;39:642-53. Bilaniuk LT, Zimmerman RA, Littman P, et al. Computed tomographyof brain stem gliomas in children. Radiology 1980;134:89-95. Bognar L, Turjman F, Villanyi E, et al. Tectal plate gliomas. Part II: CTscans and MR imaging of tectal gliomas. Acta Neurochir1994;127:48-54. Botturi M, Fariselli L. Clinical results of unconventional fractionationradiotherapy in central nervous system tumors. Tumori1998;84(2):176-87. Bouffet E, Khelfaoui F, Philip I, Biron P, Brunat-Mentigny M, Philip T.High-dose carmustine for high-grade gliomas in childhood. CancerChemother Pharmacol 1997;39(4):376-9. Bouffet E, Raquin M, Doz F, et al. Radiotherapy followed by high dosebusulfan and thiotepa. A prospective assessment of high dosechemotherapy in children with diffuse pontine gliomas. Cancer2000;88:685-92. Bradac GB, Schorner W, Bender A, Felix R. MRI (NMR) in the diagnosisof brain-stem tumors. Neuroradiology 1985;27:208-13. Bricolo A, Turazzi S, Cristofori L, Talacchi A. Direct surgery forbrainstem tumours. Acta Neurochir Suppl 1991;53:148-58. Broniscer A, Gajjar A, Bhargava R, et al. Brain stem involvement inchildren with neurofibromatosis type 1: role of magnetic resonanceimaging and spectroscopy in the distinction from diffuse pontine
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
41 of 57 03/31/2011 12:46 PM
glioma. Neurosurgery 1997;40:331-8. Broniscer A, Iacono L, Chintagumpala M, et al. Role of temozolomideafter radiotherapy for newly diagnosed diffuse brainstem glioma inchildren. Results of a multiinstitutional study (SJHG-98). Cancer2005;103:133-9. Broniscer A, Laningham FH, Kocak M, et al. Intratumoral hemorrhageamong children with newly diagnosed, diffuse brainstem glioma. Cancer2006;106(6):1364-71. Broniscer A, Leite CC, Lanchote VL, Machado TM, Cristofani LM.Radiation therapy and high-dose tamoxifen in the treatment of patientswith diffuse brainstem gliomas: Results of a Brazilian cooperativestudy. J Clin Oncol 2000;18:1246-53. Bruggers CS, Friedman HS, Fuller GN, et al. Comparison of serial PETand MRI scans in a pediatric patient with a brainstem glioma. MedPediatr Oncol 1993;21:301-6. Buckley RC. Pontine gliomas: a pathologic study and classification oftwenty-five cases. Arch Pathol 1930;9:779-819. Burzynski SR, Lewy RI, Weaver RA, et al. Phase II study ofantineoplaston A10 and AS2-1 in patients with recurrent diffuse intrinsicbrain stem glioma: A preliminary report. Drugs R D 2003;4(2):91-101. Chamberlain MC. Recurrent brainstem gliomas treated with oral VP-16.J Neurooncol 1993;15:133-9. Chiang KL, Chang KP, Lee YY, et al. Role of temozolomide in thetreatment of newly diagnosed diffuse brainstem glioma in children:experience at a single institution. Childs Nerv Syst2010;26(8):1035-41. Choi BH, Holt JT, McDonald JV. Occult malignant astrocytoma of ponswith extracranial metastasis to bone prior to craniotomy. ActaNeuropathol 1981;54:269-73. Cohen ME, Duffner PK, Heffner RR, Lacey DJ, Brecher M. Prognosticfactors in brainstem gliomas. Neurology 1986;36:602-5. Combs SE, Steck I, Schulz-Ertner D, et al. Long-term outcome ofhigh-precision radiotherapy in patients with brain stem gliomas: resultsfrom a difficult-to-treat patient population using fractionatedstereotactic radiotherapy. Radiother Oncol 2009;91(1):60-6.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
42 of 57 03/31/2011 12:46 PM
Coons SW, Johnson PC. Pathology of primary intracranial malignantneoplasms. In: Morantz RA, Walsh JW, editors. Brain tumors. Acomprehensive text. New York: Marcel Dekker, 1994;3:45-108. D'Cruz OF, Vaughn BV, Gold SH, Greenwood RS. Symptomaticcataplexy in pontomedullary lesions. Neurology 1994;44:2189-91. Dirr LY, Donofrio PD, Patton JF, Troost BT. A false-positiveedrophonium test in a patient with a brainstem glioma. Neurology1989;39:865-7. Dolinak D, Matshes E, Waghray R. Sudden unexpected death due to abrainstem glioma in an adult. J Forensic Sci 2004;49(1):1-3. Donahue B, Allen J, Siffert J, Rosovsky M, Pinto R. Patterns ofrecurrence in brain stem gliomas: evidence for craniospinaldissemination. Int J Rad Oncol Biol Phys 1998;40:677-80. Donaldson SS, Laningham F, Fisher PG. Advances toward anunderstanding of brainstem gliomas. J Clin Oncol 2006;24(8):1266-72. Dunkel IJ, Garvin JH, Goldman S, et al. High dose chemotherapy withautologous bone marrow rescue for children with diffuse pontine brainstem tumors. J Neurooncol 1998;37:67-73. Edwards MS, Wara WM, Urtasun RC, et al. Hyperfractionated radiationtherapy for brain-stem glioma: a phase I-II trial. J Neurosurg1989;70:691-700. Epstein F, Wisoff JH. Intrinsic brainstem tumors in childhood: surgicalindications. J Neurooncol 1988;6:309-17. Epstein F, Wisoff JH. Surgical management of brain stem tumors ofchildhood and adolescence. Neurosurg Clin North Am 1990;1:111-21. Epstein FJ, Farmer JP. Brain-stem glioma growth patterns. J Neurosurg1993;78:408-12. Fasano VA, Urciuoli R, Ponzio RM, Lanotte MM. The effects of newtechnologies on the surgical management of brainstem tumors. SurgNeurol 1986;25:219-26. Feinsod M, Bentin S, Moscovitch M, Wald U. Brainstem tumorpresenting with unilateral astereognosis. Ann Neurol 1980;8:191-2.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
43 of 57 03/31/2011 12:46 PM
Fischbein NJ, Prados MD, Wara W, Russo C, Edwards MS, Barkovich AJ.Radiologic classification of brain stem tumors: correlation of magneticresonance imaging appearance with clinical outcome. Pediatr Neurosurg1996;24:9-23. Fisher PG, Breiter SN, Carson BS, et al. A clinicopathologicalreappraisal of brain stem tumor classification. Identification of pilocyticastrocytoma and fibrillary astrocytoma as distinct entities. Cancer2000;89:1569-76. Fitzgerald LF. Case report. Familial brainstem glioma. Clin NeurolNeurosurg 2000;102:106-8. Frank F, Fabrizi AP, Frank-Ricci R, Gaist G, Sedan R, Peragut JC.Stereotactic biopsy and treatment of brain stem lesions: combinedstudy of 33 cases. Acta Neurochir 1988;42:177-81. Frank Y, Schwartz SB, Epstein NE, Beresford HR. Chronic dysphagia,vomiting and gastroesophageal reflux as manifestations of a brain stemglioma: a case report. Pediatr Neurosci 1989;15:265-8. Franklin CI. The role of radiotherapy in the control of midbraintumours. Australas Radiol 1991;35(1):72-4. Franzini A, Allegranza A, Melcarne A, Giorgi C, Ferraresi S, Broggi G.Serial stereotactic biopsy of brain stem expanding lesions.Considerations on 45 consecutive cases. Acta Neurochir Suppl1988;42:170-6. Freeman CR, Farmer JP. Pediatric brain stem gliomas: a review. Int JRad Oncol Biol Phys 1998;40:265-71. Freeman CR, Perilongo G. Chemotherapy for brain stem gliomas.Childs Nerv Syst 1999;15:545-53. Fuchs I, Kreil W, Sutter B, Papaethymiou G, Pendl G. Gamma kniferadiosurgery of brainstem gliomas. Acta Neurochir Suppl2002;84:85-90. Fujiwara T, Ogawa T, Irie K, Tsuchida T, Nagao S, Ohkawa M. Intra-arterial chemotherapy for brain stem glioma: report of four cases.Neuroradiology 1994;36:74-9. Garcia CA, McGarry PA, Collada M. Ganglioglioma of the brain stem.Case report. J Neurosurg 1984;60:431-4.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
44 of 57 03/31/2011 12:46 PM
Gaviani P, Gonzalez RG, Zhu JJ, Batchelor TT, Henson JW. Centralneurogenic hyperventilation and lactate production in brainstem glioma.Neurol 2005;64:166-7. Gibbs FA. Frequency with which tumours in various parts of the brainproduce certain symptoms. Arch Neurol Psychiatr (Chicago)1932;28:969-89. Gilbertson RJ, Hill DA, Hernan R, et al. ERBB1 is amplified andoverexpressed in high-grade diffusely infiltrative pediatric brain stemglioma. Clin Cancer Res 2003;9(10 Pt 1):3620-4. Gilman N, Baloh RW, Tomiyasu U. Primary position upbeat nystagmus.A clinicopathologic study. Neurology 1977;27:294-8. Giunta F, Grasso G, Marini G, Zorzi F. Brain stem expanding lesions:stereotactic diagnosis and therapeutical approach. Acta Neurochir Suppl(Wien) 1989;46:86-9. Globus JH, Kuhlenbeck H, Weller D. Tumors of the aqueduct ofSylvius: blastomatous formations of varied origin, limited to themesencephalon. J Neuropathol Exp Neurol 1945;1:207-23. Grigsby PW, Garcia DM, Ghiselli R. Analysis of autopsy findings inpatients treated with irradiation for thalamic and brain stem tumors.Am J Clin Oncol 1989a;12:255-8. Grigsby PW, Garcia DM, Simpson JR, Fineberg BB, Schwartz HG.Prognostic factors and results of therapy for adult thalamic andbrainstem tumors. Cancer 1989b;63:2124-9. Grigsby PW, Thomas PR, Schwartz HG, Fineberg BB. Multivariateanalysis of prognostic factors in pediatric and adult thalamic andbrainstem tumors. Int J Radiat Oncol Biol Phys 1989c;16:649-55. Guillain G, Bertrand I, Gruner J. Les gliomes infiltrés du tronc cérébral.Paris: Masson, 1945. Guillain G, Bertrand I, Messimy R. Sténose de l'aqueduc de Sylvius parune tumeur très limitée. Rev Neurol 1936;66:533-40. Guillamo JS, Monjour A, Taillandier L, et al. Brainstem gliomas inadults: prognostic factors and classification. Brain 2001;124:2528-39. Guiney MJ, Smith JG, Hughes P, Yang C, Narayan K. Contemporarymanagement of adult and pediatric brain stem gliomas. Int J Radiat
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
45 of 57 03/31/2011 12:46 PM
Oncol Biol Phys 1993;25:235-41. Gururangan S, Chi SN, Young Poussaint T, et al. Lack of efficacy ofbevacizumab plus irinotecan in children with recurrent malignant anddiffuse brainstem glioma: a Pediatric Brain Tumor Consortium study. JClin Oncol 2010;28(18):3069-75. Gutmann L, Hopf HC. Facial myokymia and contraction persisting 20years: a case of pontine glioma. Muscle Nerve 1994;17:1461-3. Hall WA, Doolittle ND, Daman M, et al. Osmotic blood-brain barrierdisruption chemotherapy for diffuse pontine gliomas. J Neurooncol2006;77(3):279-84. Hare CC, Woolf A. Intramedullary tumours of the brain stem. ArchNeurol Psychiatry (Chicago) 1934;32:1230-52. Hargrave D, Bartels U, Bouffet E. Diffuse brainstem glioma in children:critical review of clinical trials. Lancet Oncol 2006;7(3):241-8. Hargrave D, Chuang N, Bouffet E. Conventional MRI cannot predictsurvival in childhood diffuse intrinsic pontine glioma. J Neurooncol2008;86(3):313-9. Hayward RM, Patronas N, Baker EH, Vezina G, Albert PS, Warren KE.Inter-observer variability in the measurement of diffuse intrinsicpontine gliomas. J Neurooncol 2008;90(1):57-61. Helton KJ, Phillips NS, Khan RB, et al. Diffusion tensor imaging of tractinvolvement in children with pontine tumors. AJNR Am J Neuroradiol2006;27(4):786-93. Helton KJ, Weeks JK, Phillips NS, et al. Diffusion tensor imaging ofbrainstem tumors: axonal degeneration of motor and sensory tracts. JNeurosurg Pediatrics 2008;1(4):270-6. Ho KL. Tumors of the cerebral aqueduct. Cancer 1982;49:154-62. Hood TW, Gebarski SS, McKeever PE, Venes JL. Stereotaxic biopsy ofintrinsic lesions of the brain stem. J Neurosurg 1986;65:172-6. Hood TW, McKeever PE. Stereotactic management of cystic gliomas ofthe brain stem. Neurosurgery 1989;24:373-8. Hsu CY, Hogan EL, Wingfield W, et al. Orthostatic hypotension withbrainstem tumors. Neurology 1984;34:1137-43.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
46 of 57 03/31/2011 12:46 PM
Hueftle MG, Han JS, Kaufman B, Benson JE. MR imaging of brain stemgliomas. J Comput Assist Tomogr 1985;9:263-7. Ito S, Hoshino T, Shibuya M, Prados MD, Edwards MS, Davis RL.Proliferative characteristics of juvenile pilocytic astrocytomasdetermined by bromodeoxyuridine labeling. Neurosurgery1992;31:413-9. Jakacki RI, Siffert J, Jamison C, Velasquez L, Allen JC. Dose-intensive,time-compressed procarbazine, CCNU, vincristine (PCV) with peripheralblood stem cell support and concurrent radiation in patients with newlydiagnosed high-grade gliomas. J Neurooncol 1999;44(1):77-83. Jallo GI, Volkov A, Wong C, Carson BS, Penno MB. A novel brainstemtumor model: functional and histopathological characterization. ChildsNerv Syst 2006;22(12):1519-25. Jaros E, Perry RH, Adam L, et al. Prognostic implications of p53protein, epidermal growth factor receptor, and Ki-67 labeling in braintumors. Br J Cancer 1992;66:373-85. Jenkin RD, Boesel C, Ertel I, et al. Brain-stem tumors in childhood: aprospective randomized trial of irradiation with and without adjuvantCCNU, VCR, and prednisone. J Neurosurg 1987;66:227-33. Jenkins RB, Kimmel DW, Moertel CA, et al. A cytogenetic study of 53human gliomas. Cancer Genet Cytogenet 1989;39:253-79. Jennings MT, Sposto R, Boyett JM, et al. Preradiation chemotherapy inprimary high-risk brainstem tumors: phase II study CCG-9941 of theChildren's Cancer Group. J Clin Oncol 2002;20(16):3431-7. Kepes JJ, Striebinger CM, Brackett CE, Kishore P. Gliomas(astrocytomas) of the brain-stem with spinal intra- and extraduralmetastases: report of three cases. J Neurol Neurosurg Psychiatry1976;39:66-76. Kesari S, Kim RS, Markos V, Drappatz J, Wen PY, Pruitt AA. Prognosticfactors in adult brainstem gliomas: a multicenter, retrospectiveanalysis of 101 cases. J Neurooncol 2008;88(2):175-83. Khatib ZA, Heideman RL, Kovnar EH, et al. Predominance of pilocytichistology in dorsally exophytic brain stem tumors. Pediatr Neurosurg1994;20:2-10.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
47 of 57 03/31/2011 12:46 PM
Kihlstrom L, Lindquist C, Lindquist M, Karlsson B. Stereotacticradiosurgery for tectal low-grade gliomas. Acta Neurochir Suppl1994;62:55-7. Kim TH, Chin HW, Pollan S, Hazel JH, Webster JH. Radiotherapy ofprimary brain stem tumors. Int J Radiat Oncol Biol Phys1980;6(1):51-7. King JT, Galetta SL, Flamm ES. Relative afferent pupillary defect withnormal vision in a glial brainstem tumor. Neurology 1991;41:945-6. Kingsley DP, Kendall BE. The CT scanner in posterior fossa tumors ofchildhood. Br J Radiol 1979;52:769-76. Krauss JK, Wakhloo AK, Scheremet R, Seeger W. Facial myokymia andspastic paretic facial contracture as the result of anaplasticpontocerebellar glioma. Neurosurgery 1993;32:1031-4. Kuna ST, Smickley JS, Murchison LC. Hypercarbic periodic breathingduring sleep in a child with a central nervous system tumor. Am RevRespir Dis 1991;142:880-3. Kwon JW, Kim IO, Cheon JE, et al. Paediatric brain-stem gliomas:MRI, FDG-PET and histological grading correlation. Pediatr Radiol2006;36(9):959-64. Lakhan SE, Harle L. Difficult diagnosis of brainstem glioblastomamultiforme in a woman: a case report and review of the literature. JMed Case Reports 2009;3:87. Lam CH, Hall WA, Truwit CL, Liu H. Intra-operative MRI-guidedapproaches to the pediatric posterior fossa tumors. Pediatr Neurosurg2001;34(6):295-300. Landolfi JC, Thaler HT, DeAngelis LM. Adult brainstem gliomas.Neurology 1998;51:1136-9. Lang FF, Miller DC, Koslow M, Newcomb EW. Pathways leading toglioblastoma multiforme: a molecular analysis of genetic alterations in65 astrocytic tumors. J Neurosurg 1994;81:427-36. Lapras C, Bognar L, Turjman F, et al. Tectal plate gliomas. Part I:Microsurgery of the tectal plate gliomas. Acta Neurochir1994;126:76-83. Laprie A, Pirzkall A, Haas-Kogan DA, et al. Longitudinal multivoxel MR
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
48 of 57 03/31/2011 12:46 PM
spectroscopy study of pediatric diffuse brainstem gliomas treated withradiation therapy. Int J Rad Oncol Biol Phys 2005;62:20-31. LaSala PA, Frost EA, Boehm FH. Intracranial tumors. In: Frost EA,editor. Clinical anesthesia in neurosurgery. 2nd ed. Boston:Butterworth-Heinemann, 1991;10:245-63. Lee BC, Kneeland JB, Walker RW, Posner JP, Cahill PT, Deck MD. MRimaging of brainstem tumors. AJNR Am J Neuroradiol 1985;6:159-63. Lee TT, Galarza M, Petito CK, Heros RC. Exophytic malignantbrainstem mixed glioma in an adult: a case report. J Neurooncol1998;37:123-9. Lesniak MS, Klem JM, Weingart J, Carson BS. Surgical outcomefollowing resection of contrast-enhanced pediatric brainstem gliomas.Ped Neurosurg 2003;39(6):314-22. Levin VA, Edwards MS, Wara WM, Allen J, Ortega J, Vestnys P.5-Fluorouracil and 1-(2-choroethyl)-3-cyclohexyl-1-nitrosourea (CCNU)followed by hydroxyurea, misonidazole, and irradiation for brain stemgliomas: a pilot study of the brain tumor research center and theChildren's Cancer Group. Neurosurgery 1984;14:679-81. Linstadt DE, Edwards MS, Prados M, Larson DA, Wars WM.Hyperfractionated irradiation for adults with brainstem gliomas. Int JRadiat Oncol Biol Phys 1991;20:757-60. Liu AK, Brandon J, Foreman NK, Fenton LZ. Conventional MRI atpresentation does not predict clinical response to radiation therapy inchildren with diffuse pontine glioma. Pediatr Radiol2009;39(12):1317-20. Liu Q, Liu R, Kashyap MV, et al. Brainstem glioma progression injuvenile and adult rats. J Neurosurg 2008;109(5):849-55. Loeffler JS, Alexander E, Shea WM, et al. Radiosurgery as part of theinitial management of patients with malignant gliomas. J Clin Oncol1992;10:1379-85. Louis DN, Rubio MP, Correa KM, Gusella JF, von Deimling A. Moleculargenetics of pediatric brain stem gliomas. Application of PCR techniquesto small and archival brain tumor specimens. J Neuropathol Exp Neurol1993;52:507-15. Mahony MJ, Kennedy JD, Leaf A, Matthew DJ, Milla PJ. Brain stem
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
49 of 57 03/31/2011 12:46 PM
glioma presenting as gastro-esophageal reflux. Arch Dis Child1987;62:731-3. Mandell LR, Kadota R, Freeman C, et al. There is no role forhyperfractionated radiotherapy in the management of children withnewly diagnosed diffuse intrinsic brainstem tumors: results of apediatric oncology group phase III trial comparing conventional vs.hyperfractionated radiotherapy. Int J Rad Oncol Biol Phys1999;43:959-64. Mann SD, Danesh BJ, Kamm MA. Intractable vomiting due to abrainstem lesion in the absence of neurological signs or raisedintracranial pressure. Gut 1998;42:875-8. Mantravadi RV, Phatak R, Bellur S, Liebner EJ, Haas R. Brain stemgliomas: an autopsy study of 25 cases. Cancer 1982;49:1294-6. Marcus KJ, Dutton SC, Barnes P, et al. A phase I trial of etanidazoleand hyperfractionated radiotherapy in children with diffuse brainstemglioma. Int J Rad Oncol Biol Phys 2003;55(5):1182-5. Maria BL, Esiin TA, Quisling RG. Brainstem and other malignantgliomas: II. Possible mechanisms of brain infiltration by tumor cells. JChild Neurol 1993b;8:292-305. Maria BL, Rehder K, Eskin TA, et al. Brainstem glioma: I. Pathology,clinical features, and therapy. J Child Neurol 1993a;8:112-28. Martin RA, Handel SF, Aldama AE. Inability to sneeze as amanifestation of medullary neoplasm. Neurology 1991;41:1675-6. Massager N, David P, Goldman S, et al. Combined magnetic resonanceimaging- and positron emission tomography-guided stereotactic biopsyin brainstem mass lesions: diagnostic yield in a series of 30 patients. JNeurosurg 2000;93:951-7. Miller NR. Neuro-ophthalmologic topographic diagnosis of tumors andrelated conditions. In: Miller NR, editor. Walsh and Hoyt's clinicalneuro-ophthalmology. Vol. 3. 4th ed. Baltimore: Williams & Wilkins,1988:1210-5. Milstein JM, Geyer JR, Berger MS, Bleyer WA. Favorable prognosis forbrainstem gliomas in neurofibromatosis. J Neurooncol 1989;7:367-71. Molloy PT, Bilaniuk LT, Vaughan SN, et al. Brainstem tumors inpatients with neurofibromatosis type 1: a distinct clinical entity.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
50 of 57 03/31/2011 12:46 PM
Neurology 1995;45:1897-902. Mundinger F, Braus DF, Krauss JK, Birg W. Long-term outcome of 89low-grade brain-stem gliomas after interstitial radiation therapy. JNeurosurg 1991;75(5):740-6. Mursch K, Halatsch ME, Markakis E, Behnke-Mursch J. Intrinsicbrainstem tumours in adults: results of microneurosurgical treatment of16 consecutive patients. Br J Neurosurg 2005;19(2):128-36. Nelson MD, Soni D, Baram TZ. Necrosis in pontine gliomas: radiationinduced or natural history? Radiology 1994;191:279-82. Newton HB. Primary brain tumors: review of etiology, diagnosis, andtreatment. Am Fam Physician 1994;49:787-97. Newton HB. Bevacizumab: Review of development, pharmacology, andapplication to brain tumors. Clin Med Therap 2009;1:1577-97. Newton HB, Newton C, Pearl D, Davidson T. Swallowing assessment inprimary brain tumor patients with dysphagia. Neurology1994;44:1927-32. Newton HB, Rosenblum MK, Walker RW. Extraneural metastases ofinfratentorial glioblastoma multiforme to the peritoneal cavity. Cancer1992;69:2149-53. Nodar RH, Hahn J, Levine HL. Brain stem auditory evoked potentials indetermining site of lesion of brain stem gliomas in children.Laryngoscope 1980;90:258-66. Packer RJ, Allen J, Nielsen S, Petito C, Deck M, Jereb B. Brainstemglioma: clinical manifestations of meningeal gliomatosis. Ann Neurol1983;14:177-82. Packer RJ, Krailo M, Mehta M, et al. Phase 1 study of concurrent RMP-7and carboplatin with radiotherapy for children with newly diagnosedbrainstem gliomas. Cancer 2005;104(6):1281-7. Packer RJ, Nicholson HS, Vezina LG, Johnson DL. Brainstem gliomas.Neurosurg Clin North Am 1992;3:863-79. Packer RJ, Prados M, Phillips P, et al. Treatment of children with newlydiagnosed brain stem gliomas with intravenous recombinantbeta-interferon and hyperfractionated radiation therapy. A Children'sCancer Group phase I/II study. Cancer 1996;77:2150-6.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
51 of 57 03/31/2011 12:46 PM
Packer RJ, Zimmerman RA, Luerssen TG, et al. Brainstem gliomas ofchildhood: magnetic resonance imaging. Neurology 1985;35:397-401. Pendl G, Vorkapic P. Microsurgery of intrinsic midbrain lesions. ActaNeurochir Suppl 1991;53:137-43. Pendl G, Vorkapic P, Koniyama M. Microsurgery of midbrain lesions.Neurosurgery 1990;26:641-8. Pimenta LH, Pimenta TM, Pimenta AM. CO2 laser in brain stemgliomas. Lasers Surg Med 1986;6:142-5. Pirotte BJ, Lubansu A, Massager N, Wikler D, Goldman S, Levivier M.Results of positron emission tomography guidance and reassessment ofthe utility of and indications for stereotactic biopsy in children withinfiltrative brainstem tumors. J Neurosurg 2007;107(5):392-9. Pollack IF, Hoffman HJ, Humphreys RP, Becker L. The long-termoutcome after surgical treatment of dorsally exophytic brain-stemgliomas. J Neurosurg 1993;78:859-63. Pollack IF, Shultz B, Mulvihill JJ. The management of brainstemgliomas in patients with neurofibromatosis 1. Neurology1996;46:1652-60. Prados MD, Wara WM, Edwards MS, Larson DA, Lamborn K, Levin VA.The treatment of brain stem and thalamic gliomas with 78 Gy ofhyperfractionated radiation therapy. Int J Radiat Oncol Biol Phys1995;32:85-91. Queiroz LS, Lopes de Faria J, Cruz Neto JN. An ependymoblastoma ofthe pons. J Pathol 1975;115:207-10. Raffel C, Hudgins R, Edwards MS. Symptomatic hydrocephalus: initialfindings in brainstem gliomas not detected on computed tomographicscans. Pediatrics 1988;82:733-7. Raffel C, McComb JG, Bodner S, Gilles FE. Benign brain stem lesions inpediatric patients with neurofibromatosis: case reports. Neurosurgery1989;25:959-64. Ragge NK, Hoyt WF. Midbrain myasthenia: fatigable ptosis, "lid twitch"sign, and ophthalmoparesis from a dorsal midbrain glioma. Neurology1992;42:917-9.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
52 of 57 03/31/2011 12:46 PM
Rajshekhar V, Chandy MJ. Computerized tomography-guidedstereotactic surgery for brainstem masses: a risk-benefit analysis in 71patients. J Neurosurg 1995;82:976-81. Raza S, Donach M. Bevacizumab in adult malignant brainstem gliomas.J Neurooncol 2009;95(2):299-300. Ree A, Jain R, Rock J, Rosenblum M, Patel SC. Direct infiltration ofbrainstem glioma along the cranial nerves. J Neuroimag2005;15:197-9. Rey JA, Bello MJ, de Campos JM, Kusak ME, Moreno S. Chromosomalcomposition of a series of 22 human low-grade gliomas. Cancer GenetCytogenet 1987;29:223-37. Riina HA, Knopman J, Greenfield JP, et al. Balloon-assistedsuperselective intra-arterial cerebral infusion of bevacizumab formalignant brainstem glioma. A technical note. Interv Neuroradiol2010;16(1):71-6. Rodriguez LA, Prados M, Fulton D, Edwards MS, Silver P, Levin V.Treatment of recurrent brain stem gliomas and other central nervoussystem tumors with 5-fluorouracil, CCNU, hydroxyurea, and6-mercaptopurine. Neurosurgery 1988;22:691-3. Rodriguez M, Baele PL, Marsh HM, Okazaki H. Central neurogenichyperventilation in an awake patient with brainstem astrocytoma. AnnNeurol 1982;11:625-8. Ronghe M, Hargrave D, Bartels U, et al. Vincristine and carboplatinchemotherapy for unresectable and/or recurrent low-grade astrocytomaof the brainstem. Pediatr Blood Cancer 2010;55(3):471-7. Rosemberg S, Lopes MB, Elks L, Teixeira MJ, Serrano VA. Extraneuralmetastasis of a brainstem astrocytoma in a child: clinicopathologicalreport. Clin Neuropathol 1988;7:131-3. Rusyniak WG, Ireland PD, Radley MG, Pilcher WH, Okawara SH.Ultrasonographic and electrophysiological adjuncts to surgery within thebrain stem: technical note. Neurosurgery 1992;31:798-801. Rutka JT, George RE, Davidson G, Hoffman HJ. Low-gradeastrocytoma of the tectal region as an unusual cause of knee pain:case report. Neurosurgery 1991;29:608-12. Salmaggi A, Fariselli L, Milanesi I, et al; Associazone Italiana di Neuro-
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
53 of 57 03/31/2011 12:46 PM
oncologia. Natural history and management of brainstem gliomas inadults. A retrospective Italian study. J Neurol 2008;255(2):171-7. Sandberg DI, Edgar MA, Souweidane MM. Convection-enhanced deliveryinto the rat brainstem. J Neurosurg 2002;96:885-91. Sanghavi SN, Needle MN, Krailo MD, Geyer JR, Ater J, Mehta MP. Aphase I study of topotecan as a radiosensitizer for brainstem glioma ofchildhood: first report of the Children's Cancer Group-0952. Neurooncol2003;5(1):8-13. Schianchi P, Kraus-Ruppert R. Familial brain tumors:rhombencephalon-astrocytoma grade I in father and son. ActaNeuropathol 1980;52:153-5. Schild SE, Stafford SL, Brown PD, et al. The results of radiotherapy forbrainstem tumors. J Neurooncol 1998;40:171-7. Schulz-Ertner D, Debus J, Lohr F, Frank C, Hoss A, Wannenmacher M.Fractionated stereotactic conformal radiation therapy of brain stemgliomas: outcome and prognostic factors. Radiother Oncol2000;57(2):215-23. Selvapandian S, Rajshekhar V, Chandy MJ. Brainstem gliomas:comparative study of clinico-radiological presentation, pathology andoutcome in children and adults. Acta Neurochir 1999;141:721-7. Shibamoto Y, Takahashi M, Dokoh S, Tanabe M, Ishida T, Abe M.Radiation therapy for brain stem tumor with special reference to CTfeature and prognosis correlations. Int J Radiat Oncol Biol Phys1989;17:71-6. Shrieve DC, Wara WM, Edwards MS, et al. Hyperfractionated radiationtherapy for gliomas of the brainstem in children and in adults. Int JRadiat Oncol Biol Phys 1992;24:599-610. Siderowf AD, Balcer LJ, Kenyon LC, Nei M, Raps EC, Galetta SL.Central neurogenic hyperventilation in an awake patient with a pontineglioma. Neurology 1996;46:1160-2. Silbergeld D, Berger M, Griffin B, et al. Brainstem glioma with multipleintraspinal metastases during life: case report and review of theliterature. Pediatr Neurosci 1988;14:103-7. Smith RR. Brain stem tumors. Semin Roentgenol 1990;25:249-62.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
54 of 57 03/31/2011 12:46 PM
Souweidane MM, Occhiogrosso G, Mark EB, Edgar MA. Interstitialinfusion of IL13-PE38QQR in the rat stem. J Neurooncol2004;67(3):287-93. Squires LA, Allen JC, Abbott R, Epstein FJ. Focal tectal tumors:management and prognosis. Neurology 1994;44:953-6. Storm PB, Clatterbuck RE, Liu YJ, et al. A surgical technique for safelyplacing a drug delivery catheter into the pons of primates: Preliminaryresults of carboplatin infusion. Neurosurg 2003;52(5):1169-77. Strege RJ, Liu YJ, Kiely A, et al. Toxicity and cerebrospinal fluid levelsof carboplatin chronically infused into the brainstem of a primate. JNeurooncol 2004;67(3):327-34. Thakur SB, Karimi S, Dunkel IJ, Koutcher JA, Huang W. LongitudinalMR spectroscopic imaging of pediatric diffuse pontine tumors to assesstumor aggression and progression. AJNR Am J Neuroradiol2006;27(4):806-9. Thomale UW, Tyler B, Renard VM, et al. Local chemotherapy in the ratbrainstem with multiple catheters: a feasibility study. Childs Nerv Syst2009;25(1):21-8. Tobias JD, Heideman RL. Primary central hyperventilation in a childwith a brainstem glioma: management with continuous intravenousfentanyl. Pediatrics 1991;88:818-20. Tokuriki Y, Handa H, Yamashita J, Okumura T, Paine JT. Brainstemglioma: an analysis of 85 cases. Acta Neurochir 1986;79:67-73. Torcuator R, Zuniga R, Loutfi R, Mikkelsen T. Bevacizumab andirinotecan treatment for progressive diffuse brainstem glioma: casereport. J Neurooncol 2009;93(3):409-12. Valente S, De Rosa M, Culla G, Corbo GM, Ciappi G. An uncommoncase of brainstem tumor with selective involvement of the respiratorycenters. Chest 1993;103:1909-10. Vandertop WP, Hoffman HJ, Drake JM, et al. Focal midbrain tumor inchildren. Neurosurgery 1992;31:186-94. von Deimling A, von Ammon K, Schoenfeld D, Wiestler OD, SeizingerBR, Louis DN. Subsets of glioblastoma multiforme defined bymolecular genetic analysis. Brain Pathol 1993;3:19-26.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
55 of 57 03/31/2011 12:46 PM
Wang C, Zhang J, Liu A, Sun B, Zhao Y. Surgical treatment of primarymidbrain gliomas. Surg Neurol 2000;53:41-51. Warren K, Jakacki R, Widemann B, et al. Phase II trial of intravenouslobradimil and carboplatin in childhood brain tumors: a report from theChildren's Oncology Group. Cancer Chemother Pharmacol2006;58(3):343-7. Westra I, Drummond GT. Occult pontine glioma in a patient withhemifacial spasm. Can J Ophthalmol 1991;26:148-51. White HH. Brain stem tumors occurring in adults. Neurology1963;13:292-300. Wilken B, Lalley P, Bischoff AM, et al. Treatment of apneusticrespiratory disturbance with a serotonin-receptor agonist. J Pediatr1997;130:89-94. Wolff JE, Molenjkamp G, Westphal S, et al. Oral trofosfamide andetoposide in pediatric patients with glioblastoma multiforme. Cancer2000;89(10):2131-7. Wolff JE, Westphal S, Molenkamp G, et al. Treatment of paediatricpontine glioma with oral trophosphamide and etoposide. Br J Cancer2002;87(9):945-9. Wood JR, Camilleri M, Low PA, Malagelada JR. Brainstem tumorpresenting as an upper gut motility disorder. Gastroenterology1985;89:1411-4. Xu QW, Bao WM, Mao RL, Jiang DJ, Yang GY. Surgical treatment ofsolid brain stem tumors in adults: a report of 22 cases. Surg Neurol1997;48:30-6. Yeh DD, Warnick RE, Ernst RJ. Management strategy for adult patientswith dorsal midbrain gliomas. Neurosurg 2002;50:735-40. Yen CP, Sheehan J, Steiner M, Patterson G, Steiner L. Gamma knifesurgery for focal brainstem gliomas. J Neurosurg 2007;106(1):8-17. Yousry I, Muacevic A, Olteanu-Nerbe V, Naidich TP, Yousry TA.Exophytic pilocytic astrocytoma of the brain stem in an adult withencasement of the caudal cranial nerve complex (IX-XII): presurgicalanatomical neuroimaging using MRI. Eur Radiol 2004;14:1169-73. Zagzag D, Miller DC, Knopp E, et al. Primitive neuroectodermal tumor
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
56 of 57 03/31/2011 12:46 PM
of the brainstem: investigation of seven cases. Pediatrics2000;106:1045-53. Zarghooni M, Bartels U, Lee E, et al. Whole-genome profiling ofpediatric diffuse intrinsic pontine gliomas highlights platelet-derivedgrowth factor receptor alpha and poly (ADP-ribose) polymerase aspotential therapeutic targets. J Clin Oncol 2010;28(8):1337-44. Zhang S, Feng X, Koga H, Ichikawa T, Abe S, Kumanishi T. p53 genemutations in pontine gliomas of juvenile onset. Biochem Biophys ResCommun 1993;196:851-7. Zimmerman RA, Bilaniuk LT, Packer R, et al. Resistive NMR of brainstem gliomas. Neuroradiology 1985;27:21-5. **References especially recommended by the author or editor forgeneral reading.
Home | Support | Contact Us | Privacy Policy | Terms and Conditions of Use
Copyright© 2001-111 MedLink Corporation. All rights reserved.
Brainstem gliomas in adults https://www.medlink.com/cip.asp?uid=MLT000TT
57 of 57 03/31/2011 12:46 PM