Boyd 2015
description
Transcript of Boyd 2015

Clinica Chimica Acta 450 (2015) 31–38
Contents lists available at ScienceDirect
Clinica Chimica Acta
j ourna l homepage: www.e lsev ie r .com/ locate /c l inch im
Developing optimized automated rule sets for reporting hemolysis,icterus and lipemia based on a priori outcomes analysis
Jessica M. Boyd a, Richard Krause a, Gayle Waite b, William Hui b, Elham Yazdi b,David Wilmink b, Isolde Seiden-Long a,⁎a Department of Pathology and Laboratory Medicine, University of Calgary and Calgary Laboratory Services, Canadab Gamma-Dynacare Medical Laboratories, Canada
Abbreviations: HIL, Hemolysis, icterus, lipemia; CLSIInstitute; LIS, Laboratory information system.⁎ Corresponding author at: Foothills Medical Centre, 1
T2N 2T9, Canada.E-mail address: [email protected] (I. Seiden-
http://dx.doi.org/10.1016/j.cca.2015.07.0060009-8981/© 2015 Elsevier B.V. All rights reserved.
a b s t r a c t
a r t i c l e i n f oArticle history:
Received 2 June 2015Received in revised form 3 July 2015Accepted 6 July 2015Available online 8 July 2015Keywords:HemolysisIcterusLipemiaAutomated indices
Background: There is limited information about the effects of instituting CLSI Document C56A recommendedworkflows for the automated detection of hemolysis, lipemia and icterus (HIL) in different clinical laboratoriesand patient populations. We describe a process to develop and tailor automated reporting rules that are appro-priate for the local laboratory population.Methods: Automated decision algorithms were generated and applied to 2 high volume labs serving communityand hospital populations. Proposed rules were applied to the datasets offline to predict the outcomes, and thenwere further optimized prior to implementation.Results: Introduction of automated serum indices decreased HIL flagging compared to manual flagging. Hemoly-sis flagging was the greatest in all 3 patient populations, and was successfully reduced for LD, CK and AST by op-timized rules that incorporated both theH-index result and the analyte result. Changes inflagging rateswere also
patient population specific, particularly for icterus which was a problem in hospitalized populations but not inthe community. Overall, concordance between manual and automated flagging methods was very low in bothlaboratories.Conclusions:Wedemonstrate that flagging algorithmsmay not be universally transferable due to lab specific andpopulation specific factors and demonstrate the benefits of local, a priori testing of algorithms prior toimplementation.© 2015 Elsevier B.V. All rights reserved.
1. Introduction
Hemolysis, icterus and lipemia (HIL) interferences are common pre-analytical sources of error in the clinical laboratory [1–4]. Determinationof HIL interferences has traditionally been done by manual visual grad-ing by technologists; however, this process is highly subjective and var-iable [5–7]. Serum indices are a semi-quantitative measurement of HILinterference, using spectrophotometric measurement and mathemati-cal correction to determine the level of interference. Serum indices areless subjective than manual grading, can be automated, and negligiblyimpact turnaround times [8].
CLSI document C56A provides guidance on the use of serum indicesfor measurement of HIL interference [1]. It recommends selection ofassay specific HIL cut-offs, above which HIL interferences will affect re-sults, and development of algorithms to deal with samples exceeding
, Clinical Laboratory Standards
403-29 St. NW, Calgary, Alberta
Long).
the HIL cut-offs (e.g., cancelation, report with comment). HIL cut-off se-lection and algorithm design is left to the discretion of each laboratory.
Although serum indices have been available for several years, thereis limited information about their implementation in clinical laborato-ries, either for selection of assay specific HIL cut-offs or developmentof algorithms. One study has looked at retrospective development andimplementation of algorithms for processing HIL interferences [6]. Theauthors investigated the changes to HIL flagging after switching fromvisual inspection to automated indices and found large increases in flag-ging for all 3 interferences. Test specific flagging rateswere not includedso it is uncertain if the flagging increaseswere seen acrossmany tests ordominated by a few interference prone assays. It is also unknown if in-creased flaggingwould be seen in other patient populations (communi-ty vs. hospital). The large increase in flagging suggests that flagginganalysis prior to implementationmay be necessary in order tominimizethe impact of introducing automated serum indices on lab workflowand provide adequate notification to physicians of the anticipatedchanges to reporting.
We outline a process to develop and test an HIL algorithm with theoverall goal of producing a process that can identify specimens with in-terference levels relevant to the tests ordered; alert technologists to the

32 J.M. Boyd et al. / Clinica Chimica Acta 450 (2015) 31–38
interference if intervention is required; provide interpretive informa-tion to physicians about specimens with interference; cancel the leastnumber of tests; and avoid adverse effects caused by failure to report re-sults with HIL interference.
2. Materials and methods
2.1. Ethics
This project is classified as quality assurance in nature by our institu-tional Co-joint Health Research Ethics Board and is granted exemptstatus for research ethics review.
2.2. Demographics
Data from 2 high-volume community labs and one group of hospitallabs were analyzed in this study (Table 1). Lab A is a high volume lab inOntario, Canada with 3 locations serving western, central and easternOntario. Labs B1 and B2 serve the same city in Alberta, Canada. Lab B1is a centralized, high volume laboratory serving the community popula-tion while Lab B2 is a combination of 5 urban hospital labs serving dif-ferent sub-populations. Labs B1 and B2 were analyzed separatelybecause of the differences in population served, instrumentation andtest menus.
2.3. Lab inclusion rationale
2.3.1. Patient populationNo data is currently available comparing the application of identical
HIL algorithms to different patient populations (e.g. hospital vs. commu-nity, community vs. community). To address this, 2 community labs(Labs A and B1) and onehospital lab (Lab B2)were included in the pres-ent study.
2.3.2. Effect on existing methods to detect HIL interferenceOnly one study investigating one lab has been published describing
the effects of switching frommanual grading to automated serum indi-ces. To determine if the same effects are seen in other labs making thistransition, data from 2 labs were included (Labs A and B2).
No data is available to determine if the index cut-offs and algorithmsneed to be periodically evaluated and revised or if they can be left aloneindefinitely. In this study, Lab B1was included to evaluate this question,as it was re-evaluating its automated serum index rules as it changed itsanalyzers from Roche Modular P/E to Roche Cobas c701/e602. Cut-offchanges were observed for some tests because of methodology changes(e.g. calcium from o-cresolphenol to NM-BAPTA) or because Roche stat-ed different HIL cut-offs for the same test run on different analyzers (e.g.TBIL c701 I index= 90, c501 I-index= 1000). In addition, there was in-terest in determining if the algorithm could bemodified to cancel fewertests, as the lab had experienced some calls about too many tests beingcanceled.
Table 1Key demographics of Labs A, B1 and B2.
Patient population Lab A
Community
Average # of tests per day during data collection period 77,319# of chemistry tests on menu 55# of days data collected 7 (Nov 28–Dec 4, 20Total number of tests performed during data collection period 541,236Total number of tubes analyzed during data collection period 66,668Instrumentation Roche Modular P anLocation where rule sets are applied In house developedLIS In house developed
2.4. Measurement of serum indices
All instruments used in this study were from Roche Diagnostics(Laval, QC) (Table 1) and used the same serum index measurementprinciple [9]. To confirm that serum index values were consistentamong analyzers within each lab, several specimens representing arange of HIL values were split and analyzed across all analyzers withineach lab. All results were within 10%.
2.5. Tests included in the analysis
Serum indices were collected on a combined 80 tests between the 3labs (see Supplemental Table S1 for test abbreviations and methodolo-gies). HIL flagging rates were not available if the lab did not performthe test or if it was performed on an instrument that was not collectingserum indices.
2.6. Selection of HIL cut-offs and decision algorithm development
2.6.1. Desired outcomes and assumptionsFive objectives were used to guide cut-off selection and algorithm
development: identify specimens with interference levels relevant tothe tests ordered; alert technologists to the presence of interferencewhen intervention is required; aid physicians with interpretation oftest results from samples with interference; cancel the least numberof tests; and avoid adverse effects caused by failure to report resultswith HIL interference.
The algorithm was also designed to reduce manual technologist in-terventions asmuch as possible. The effect of introducing the algorithmwas determined by assessing sample flagging and cancelation rates in 2different laboratories, serving 3 different populations. This allowed forassessment of lab specific and population specific factors requiring re-finement of the algorithms with the ultimate goal of reportingmore re-sults with better interpretive information to physicians. By performingthis analysis a priori, the impact on laboratory workflows could be de-termined and the process refined prior to implementation.
2.6.2. HIL cut-off selectionSelection of test-specific HIL cut-offs is discussed in Section 3.1.
2.6.3. Rule setsThe 3 sets of comment and cancelation rules assayed in this study
are baseline rules (the existing HIL flagging process in place in eachlab), proposed rules (automated HIL indices with test specific commentand cancelation cut-offs chosen using manufacturers' package inserts,information from literature [10], and CLSI guideline C56A [1]); and op-timized rules (use of alternative cut-offs or interference clearing strate-gies to increase the number of reportable results). Five or more flagsunder proposed rules were used as the trigger for consideration of anoptimized rule for any test.
The general process used to develop and refine the serum index rulesets is illustrated in Supplemental Fig. S1. Specific details about the 3
Lab B1 Lab B2
Community Hospital
22,713 15,38145 47
11) 14 (Oct 16–30, 2013) 21 (Jan 13–Feb 3, 2014)317,986 323,01848,245 48,460
d E170 Roche c701 and e602 Roche c501 and e601LIS IBM AS400 Roche Cobas IT Middleware Roche Cobas IT MiddlewareLIS IBM AS400 Cerner Millennium Cerner Millennium

33J.M. Boyd et al. / Clinica Chimica Acta 450 (2015) 31–38
rule sets for each interference in each lab are given below and in Supple-mental Table S2.
2.6.3.1. Hemolysis (H)2.6.3.1.1. Baseline policies. Lab A and Lab B2 both used manual visual
inspection with comparison to a hemolysis grading chart. In Lab A, he-molyzed tubes had a hemolysis letter value flag applied to all the testson the tube but no chartable comment. In Lab B2, a flag and chartablecomment indicating slight, moderate or gross hemolysis was appliedto one test on the hemolyzed tube, chosen by the technologist.
Lab B1 had previously instituted automated serum indices and deci-sion rules. All tests were canceled with comment with H-index N 500,unless a lower cut-off was indicated by the package insert (e.g., potassi-um cancelation cut-off was 300).
2.6.3.1.2. Proposed rules. Identical proposed ruleswere applied at all 3labs. Tests were canceled at H-index ≥600 (unless a higher cut-off wasindicated by the package insert) and comment code HEMC applied(Supplemental Table S3). For tests where an H-index cut-off b 600was indicated by the manufacturer, results were reported with a com-ment indicating the direction of interference if known (commentcodes HEM1, HEMU, and HEMD).
2.6.3.1.3. Optimized rules. Hemolysis optimized rules used referenceintervals in addition to the H-index to determine clinically significantinterference. The criteria for hemolysis optimized rule generationwere N5 comment flags under proposed rules (chosen by the authorsas a significant flagging rate in the absence of any recommended qualityindicators for acceptable incidence of hemolysis); unidirectional inter-ference only, and critical valuesmust be only at one end of the referenceinterval (high or low, but not both).
Under optimized rules, samples with H-index above the flaggingcut-off but b600, would be given a hemolysis flag and comment codeonly if the test result was outside reference range. In this study, opti-mized rules were generated for AST, CK and LD.
2.6.3.2. Icterus (I)2.6.3.2.1. Baseline policies. Lab A used manual visual inspection by
comparison to a visual grading chart with results reportedwith an icter-us flag but no comment. Labs B1 and B2 did not have any policies re-garding icterus prior to this study; all test results were reportedwithout review or comment.
2.6.3.2.2. Proposed rules. Identical proposed ruleswere applied at all 3labs. Samples exceeding I-index cut-offs were reportedwith a commentindicating the direction of interference if known (comment codes ICT1,ICTU, and ICTD).
2.6.3.2.3. Optimized rules.Optimized rules required a dilution of spec-imens with a high degree of icterus. Optimized rules were consideredfor testswith I-index interference levels b15 (GGT, creatinine) in hospi-tal specimens.
2.6.3.3. Lipemia (L)2.6.3.3.1. Baseline policies. Labs A and B2 visually inspected tubes for
lipemia. In Lab A, moderately lipemic tubes were reported with alipemia letter value flag without comment. Grossly lipemic tubes hadall tests canceled with comment. In Lab B2, lipemic samples wereultracentrifuged, rerun and reported with a comment. In Lab B1, themiddleware alerted the technologist if the instrument L-index wasexceeded for a particular test. The sample would be ultracentrifuged,rerun with indices and reported with a comment if the ultracentrifugedL-index b lipemia cut-off. In Labs B1 and B2, ultracentrifugation was notperformed for triglycerides, HDL, cholesterol, or ammonia tests. Ammo-nia samples were diluted to reduce handling time.
2.6.3.3.2. Proposed rules. Identical proposed ruleswere applied at all 3labs. Samples N L-index cut-off were ultracentrifuged. The test and indi-ces were there rerun and the result reported with a comment (LIP1) iftheultracentrifuged L-index b L cut-off. Ultracentrifugationwasnot per-formed for triglycerides, HDL, cholesterol, or ammonia tests.
2.6.3.3.3. Optimized rules. Lipemia optimized rules were the same asthe proposed rules.
2.7. Data collection and analysis
Serum index data were collected from all 3 labs for the time periodsspecified in Table 1. In Labs A and B2, automated indiceswere turned onfor data collection purposes only, which prevented impact to patient re-sult reporting. In Lab B1, where automated indices were already in use,data were collected without affecting the existing flagging processes.
A different process was required in each lab to obtain baseline flag-ging rates. In Lab A, manual comment flags were obtained from theLIS. In Lab B2, manual comment and cancelation flags were obtainedfrom the LIS. In Lab B1, baseline flagging rates were modeled using theinstrument data files in order to capture the canceled tests that werenot transferred to the LIS. Flagging rates were modeled using MicrosoftExcel 2007.
2.8. Study limitations
Several limitationswere identifiedwith this study. Indiceswere onlyemployed on the high volume analyzers at all 3 labs. Although moretests are run at these locations, other analyzers were not included ornot able to measure serum indices. Data from Lab A do not includeany samples canceled under baseline policies as this information couldnot be retrieved from the LIS. Therefore, cancelation rates for Lab Amay be underestimated in this analysis. In Labs A and B1, baseline poli-cies did not collect index data on tubes that only had immunoassay testsordered. Indices were performed if the specimen had both immunoas-say and chemistries ordered. Therefore, flagging rates for immunoassaymodule tests may be underestimated. In Lab B2, baseline policies indi-cated adding comment flags to one result on the tube, chosen by thetechnologist. For the flagging analysis, we have only counted the testto which the flag was applied, not the other tests on the tube. For can-celed specimens, all tests on the tubewere canceled andwere all includ-ed in the analysis. Physicians were not surveyed to determine if theinterpretive comments were of use to them.
3. Results and discussion
A process for developing HIL cut-off and decision algorithms for usewith automated serum indices was developed. The implementation ofHIL cut-offs and decision algorithms was studied in 3 high volume lab-oratories that served distinct patient populations (community or hospi-tal) and had different pre-existing policies for detecting HIL interference(manual inspection or automated serum indices) (Tables 2–4).
3.1. Proposed rule set development
3.1.1. Selection of test specific cut-offsCut-offs for HIL interference were mainly drawn from the manufac-
turers' package inserts (objective: identify specimens with interferencelevels relevant to the tests ordered). Most manufacturers provide this in-formation; however, it is important to understand how they reportserum indices (e.g., numeric value, bin number) and the criteria usedto determine significant interference with the assay (e.g., biological var-iation, consensus of an advisory panel [1], ±10% recovery from the ini-tial concentration [10–12]) as this can cause variation in HIL cut-offsbetween different platforms and vendors. Roche (whose instrumentswere used in this study) reports serum indices as a value (e.g., H-index of 101) and uses ±10% recovery from the initial concentrationas their criteria for significant interference with an assay. Roche HILcut-offswere used to generate the proposed rule set, with the exceptionof hemolysis cut-off for potassium. The Roche cut-off of H-index= 300,was considered to be too high to be used as awarning level [10], and thelower cut-off of H-index = 100 was chosen instead.

Table 2Hemolysis index flagging counts for selected tests.
Test Lab A Lab B1 Lab B2
# of tests Baselinea Proposed/Optimizedb # of tests Baseline Proposed/Optimizedb # of tests Baselinea Proposed/Optimizedb
ALT 36,202 563 0 22,846 34 3 12,642 9 32ALP 22,038 325 0 12,616 0 7 10,732 6 33AST 11,901 187 86/29 2377 12 23/7 1888 2 76/50CO2 1627 8 0 20,757 0 0 35,809 37 5DBIL 168 4 13 3518 9 45 2684 6 333NBIL 1 1 1 NP NP NP 1099 32 54TBIL 14,796 146 0 7935 0 0 11,399 32 0CL 24,858 310 0 20,950 0 0 35,846 37 3CHOL 30,214 218 0 20,857 0 0 NP NP NPCK 16,369 230 33/5 6246 28 12/1 2423 4 21/13CREA 43,144 303 0 26,099 0 0 34,898 51 2FERR 22,559 206 1 16,888 0 0 NP NP NPGGT 5077 117 5 10,495 4 5 8388 0 23GLU 32,673 292 0 22,625 0 0 17,584 9 1HDL 29,883 213 0 19,591 0 0 NP NP NPLD 1323 20 257/38 2598 25 98/25 8276 7 1175/531MG 1647 26 0 3366 0 0 10,792 12 1PHOS 2511 24 0 3663 2 2 8440 9 14K 31,546 470 42 21,706 32 18 36,202 567 288NA 30,115 404 0 21,471 0 0 36,221 50 3TSH 29,854 134 0 23,461 0 0 NP NP NPTRIG 30,108 266 0 19,863 0 0 NP NP NPUIBC 1742 10 5 8245 29 52 NP NP NP
NP = test was not performed by this lab.a Baseline flagging for Labs A and B2 was performed manually.b Optimized rules counts are only shown for the tests for which they were developed (AST, LD and CK for H-index).
34 J.M. Boyd et al. / Clinica Chimica Acta 450 (2015) 31–38
3.1.2. Decision algorithm developmentAn algorithmwas developed to determine the processing of samples
exceeding HIL cut-offs. Decision algorithms can have varying degrees ofcomplexity ranging from sample cancelation to implementation ofstrategies aimed at reducing or compensating for interference in orderto produce a reportable result (e.g., flagging of only clinically significantresults [1,11], mathematical correction [13–15], reduction of interfer-ence (e.g., dilution, ultracentrifugation) [13,16,17], or analysis using adifferent method).
In the developed algorithm, an action (e.g. appending a comment,manual reduction of interference, and cancelation) was required anytime a sample exceeded the HIL cut-off for a particular test. For lipemiaand icterus, this involved ultracentrifugation (lipemia) or dilution (ic-terus) to reduce or clear the interference. The technologist was alertedby the middleware (in Labs B1 and B2) or the laboratory informationsystem (in Lab A) that manual intervention was required (objective:
Table 3Icteric index flagging counts for selected tests.
Test Lab A Lab B1
# of tests Baselinea Proposed # of tests Base
ALT 36,202 43 0 22,846 0ALB 9093 17 0 9742 0ALP 22,038 39 0 12,616 0AST 11,901 20 0 2377 0CHOL 30,214 19 0 20,857 0CK 16,369 17 0 6246 0CREA 43,144 41 0 26,099 0GGT 5077 12 0 10,495 0GLU 32,673 27 0 22,625 0HDL 29,883 19 0 19,591 0PHOS 2511 2 0 3663 0TRIG 30,108 19 0 19,863 0NTRIG NP NP NP NP NPURATE 15,432 17 0 4085 0
NP = test was not performed by this lab.a Baseline flagging for Labs A and B2 was performed manually.
alert technologists to the presence of interference when intervention is re-quired). Following ultracentrifugation or dilution, the sample wasrerun and reported with a comment if the I or L index was below thecut-off (objectives: cancel the least number of tests, avoid adverse effectscaused by failure to report results with HIL interference). For hemolysis,a different approach was used by setting separate alert and cancelationcut-offs. The Roche H-index cut-off from the package insert was used asan alert cut-off, abovewhich the result was reportedwith a comment. Acancelation cut-off of H-index = 600 was chosen as representative ofgross hemolysis and that the tubewas not acceptable for testing (unlessotherwise indicated by the package insert). Thiswas done in order to in-crease the number of reportable results by only canceling grossly hemo-lyzed specimens (objective: cancel the least number of tests). The onlyexception to the cancelation rule at H-index = 600 was potassium,where the alert cut-off was 100 (as mentioned above) and the cancel-ation cut-off was 300.
Lab B2
line Proposed # of tests Baselinea Proposed/Optimized
0 12,642 0 00 6566 0 00 10,732 0 00 1888 0 08 NP NP NP0 2423 0 013 34,898 0 125/288 8388 0 53/50 17,584 0 00 NP NP NP0 8440 0 611 NP NP NPNP 152 0 90 998 0 0

Table 4Lipemic index flagging counts for selected tests.
Test Lab A Lab B1 Lab B2
# of tests Baselinea Proposed # of tests Baseline Proposed # of tests Baselinea Proposed
ALT 36,202 369 3 22,846 47 47 12,642 1 18ALB 9093 76 1 9742 0 0 6566 2 1ALP 22,038 117 0 12,616 0 0 10,732 2 0AST 11,901 215 1 2377 9 9 1888 0 5TBIL 14,796 149 3 7935 0 125 11,399 2 1CL 24,858 176 3 20,950 0 2 35,846 0 0CHOL 30,214 59 1 20,857 2 0 NP NP NPCK 16,369 44 3 6246 0 0 2423 0 0CREA 43,144 185 0 26,099 0 0 34,898 1 0FERR 22,559 54 0 16,888 0 0 NP NP NPFRUC 555 95 0 NP NP NP NP NP NPGGT 5077 125 0 10,495 0 0 8388 0 0GLU 32,673 115 2 22,625 0 0 17,584 0 0HDL 29,883 57 0 19,591 2 2 NP NP NPK 31,546 244 0 21,706 0 2 36,202 25 0TP 2765 49 4 2974 0 0 2352 0 0NA 30,115 226 4 21,471 0 2 36,221 0 0TSH 29,854 51 0 23,461 0 0 NP NP NPURATE 15,432 49 1 4085 0 0 998 0 0UREA 4466 118 4 4619 0 0 11,314 2 0
NP = test was not performed by this lab.a Baseline flagging for Labs A and B2 was performed manually.
35J.M. Boyd et al. / Clinica Chimica Acta 450 (2015) 31–38
All tests where HIL cut-offs were exceeded had an interpretive com-ment appended, providing additional information to the physician as tothe interference detected and effect on the result (SupplementalTable S3) (objective: aid physicians with interpretation of test resultsfrom samples with interference).
The developed proposed rules were modeled on data from all 3 labsto assess changes in flagging rates and to determine if further rule re-finement was required (optimized rules) (objective: avoid adverse ef-fects caused by failure to report results with HIL interference).
3.2. Flagging analysis
3.2.1. HemolysisIntroduction of automated serum indices at Lab A resulted in a 91%
decrease in the total number of samples flagged for hemolysis (com-ment and cancel) compared to manual flagging (Baseline N = 5076[0.9% of total]; Proposed N = 450 [0.1% of total]). This suggests thatmanual inspection at Lab A resulted in application of hemolysis flagsto tests that were not affected at that level of hemolysis. This is illustrat-ed in the flagging analysis from several tests from Lab A including ALT,ALP, CL, CHOL, CREA, GLU, HDL, TRIG, and NA (Table 2). A significantpart of this decrease may be attributed to a change in flagging policywhere only affected tests on a given specimen received flags under op-timized rules, whereas all tests on an identified specimenwould receiveflags under baseline rules. A major exception to the overall flagging de-crease was LD, where index flagging increased by 1100% (Baseline N=20 flags [1.5% of LD results]; Proposed N = 257 [19.4% of LD results]),which is due to the low H-index LD cut-off value of 15.
In Lab B1, implementation of proposed rules caused only a slight in-crease in the total hemolysis flagging rates (comment and cancel)(Baseline N = 277 [0.05% of total]; Proposed N = 283 [0.05% of total];2% increase). The changes are due to different H-index cut-offs for cer-tain tests between the Modular P (baseline rules) and the c702 ande601 (proposed rules). Although expected to be similar, there are some-times significant differences in the HIL cut-offs provided by the manu-facturer for the same test on different platforms. A good example ofthis from our study is DBIL, where despite having similar chemistrieson the 2 platforms, the H index cut-offs were very different (60 for theModular P; 25 for the c702). This cut-off change resulted in an increasein DBIL flagging from 9 to 45, and demonstrates how existing indexrules need to be re-evaluated after reagent and vendor changes. Other
examples included increased LD flagging (Baseline: 25, Proposed: 98)due to the change in H-index cut-off of 60 to 15. Conversely, ALT flag-ging decreased from 34 flags under baseline to 3 flags under proposedrules due to H-index cut-off changes of 60 to 200.
In Lab B2, proposed rules resulted in a 110% increase in flagging(Baseline N = 1047 [0.2% of total]; Proposed N = 2204 [0.40% oftotal]). This was largely due to increased flagging of LD and DBIL (LDBaseline N = 7 [0.1% of LD results], LD Proposed N = 1175 [14.2% ofLD results]; DBIL Baseline N = 6 [0.2% of DBIL results], DBIL ProposedN = 333 [12.4% of DBIL results]). For LD, this increase (which was alsoobserved to a lower extent in Lab A), is due to the low H-index cut-offfor this test of 15, which can be difficult to detect visually. Further anal-ysis of the DBIL results showed that themajority of the H-index flags forthis test were on samples from babies, which is likely due to the collec-tion method (heel poke) and the collectors (nurses instead of lab staff).Hemolysis falsely lowers DBIL results, which could make an elevatedDBIL appear to be in the normal range. Further investigation of DBIL or-ders on children b 1 year of age revealed that most samples with H-index 25–500 did not have a hemolysis comment appended to the re-sult and had DBIL values within the reference range. Of samples withH-index N 500, 4 of 13 did not have an associated hemolysis comment,demonstrating that even grossly hemolyzed samples were not alwaysflagged under baseline policies; however all were identified using de-veloped decision algorithm. Conversely, proposed rules decreased po-tassium flagging (Baseline N = 567 [1.6% of potassium results],Proposed N = 288 [0.8% of potassium results]; 49% decrease overall).Under Lab B2 baseline policies, the hemolysis comments used potassi-um as an example of a test affected by hemolysis. This may have result-ed in hemolysisflags being consistently attached to the potassium resultby technologists, even though the Roche c6000 H-index cut-offs arelower for DBIL (25) and LD (15) than for potassium (100). Comparedto Lab A, which also used manual flagging but saw a decrease in overallflagging following implementation of automated indices, the resultsfrom Lab B2 further demonstrate the variability seen with manual flag-ging and that flagging can increase or decrease depending on the labwhen switching to automated indices.
3.2.2. Optimized rulesProposed rules analysis greatly increased hemolysis flagging for
some tests. In order to refine hemolysis flagging, optimized rules weregenerated that only flagged a result if clinically significant changes

36 J.M. Boyd et al. / Clinica Chimica Acta 450 (2015) 31–38
were observed (Section2.6.3.1.3) (objectives: identify specimenswith in-terference levels relevant to the tests ordered, avoid adverse effects causedby failure to report results with HIL interference).
Based on these criteria, only AST, CK and LD qualified for hemolysisoptimized rule generation. Since hemolysis falsely elevates results forall 3 theses, the optimized rules were designed so that a hemolysisflag was applied to these tests only if the H-index was above the testspecific cut-off and the test result was above the reference range.When the new rules were modeled using the data, hemolysis flaggingrates were reduced for all 3 tests by N60% in Labs A and B1 and N30%in Lab B2 (Table 2).
3.3. Icterus
3.3.1. Proposed rulesAs with hemolysis, use of automated I-index reduced total icteric
flagging in Lab A (Baseline 332 [0.06% of total]; Proposed 0; 100% reduc-tion) (Table 3). This also shows that Lab A had relatively low rates oficteric specimenswhich is expected in a community setting. One poten-tial limitation of this data analysis is that Lab A may not have capturedsufficient icteric specimens in the time frame being examined due tothe low frequency of icterus in the studied population.
Labs B1 and B2 did not have a baseline process for investigating ic-teric interference. In Lab B1, application of proposed rules determinedthat 13 creatinine, 11 triglycerides, 8 cholesterol and 8 GGT resultswould have been flagged (total of 40) over the 3 week data collectionperiod. This indicated that icteric interference was not a large concern
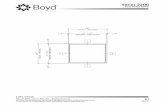
Fig. 1. Optimized r
in this community population, which is similar to the observation inLab A. However, in the absence of icterus reporting rules, even the rela-tively rare icteric community samples could have been missed by theclinician (objective: avoid adverse effects caused by failure to report re-sults with HIL interference). Upon audit, it was noted that 4/40 of theseicteric samples did not actually have a bilirubin on the order, thus theflag adds clinical value to the reporting.
Analysis of the hospital population from Lab B2 showed that ictericinterference was an issue (200 icteric flags generated) that had beenlargely overlooked until the implementation of these rule sets. Themost highly flagged test was creatinine (N= 125 [0.4% of creatinine re-sults]) followed by GGT (N= 53 [0.6% of GGT results]). This is a reflec-tion of the lower icteric cut-offs for these tests of 15 and 20 respectively,on the Roche c501 platform. None of these samples were flagged underbaseline policies, as no rules for monitoring icterus were in place. In ad-dition, when compared to the 2 community populations from Labs Aand B1, these results clearly demonstrate how patient population canaffect flagging rates for different interferences.
3.3.2. Optimized rulesOptimized rules for icterus involved diluting the sample to below the
cut-off I-index and then rerunning it. They were considered for any testwith N5 icteric flags under proposed rules. No icteric optimized ruleswere developed for Labs A and B1 because of the low prevalence of ic-teric specimens. However, optimized rules were developed for CREAand GGT in Lab B2. This could not be evaluated on our test data set asthe samples had already been analyzed and no existing icterus
ule workflow.

Table 5Tube flagging concordance between manual flagging and automated serum indices in Labs A and B2.
Tubes flagged
Hemolysis Lipemia Icterus
Baseline Proposed Both Baseline Proposed Both Baseline Proposed Both
Lab A 480 411 72 369 4 2 54 0 0Lab B2 754 1750 364 37 19 4 0 139 0
37J.M. Boyd et al. / Clinica Chimica Acta 450 (2015) 31–38
intervention step was in place. Testing of the CREA and GGT optimizedrules was performed, and indicated that the CREA rule needed furtheroptimization to make the workload manageable for technologists (293samples over 6months). Investigation of the I-index cut-off for CREA in-dicated that results did not significantly change until I-index of 30 (Sup-plemental Fig. S2). Further investigation determined that the flaggingrate could be further reduced by only performing dilution on sampleswith a CREA N 100. The final optimized rule (dilution only if Iindex ≥ 30 and CREA N 100) reduced sample dilution by 77%. Thesamedilution studywas conducted forGGT and therewas no significantinterference from Icterus until I index ≥ 55, which reduces GGT dilutionsfrom 53 to 5 (91%). This further highlights the need to assess the effectsof automated indices on each patient population and the value of testingrule sets prior to implementation.
3.4. Lipemia
3.4.1. Proposed rulesProposed rules in Lab A resulted in a decrease in flagging for all tests
(Baseline N = 2814 [0.5% of total]; Proposed N = 37 [0.007% of total];99% decrease) (Table 4).
In Lab B1, total lipemia flagging rates increased by 160% (Baseline74 [0.01% of total], Proposed 193 [0.04% of total]). This was due to anincrease in TBIL flagging (Baseline N = 0 [0.0% of TBIL results]; Pro-posed N = 125 [1.6% of TBIL results]), as a result of a lower lipemiacut-off (L-index of 90) indicated in the package insert for the c701reagent compared to the Modular P reagent. This appeared unusualand was further investigated. When TBIL interference was verifiedin-house using an intralipid reagent, no significant lipemic interfer-ence was found to an index level of ≥600. Changing the lipemia flag-ging settings to this level reduced the flagging rates by 98%. Thisexample highlights that it is sometimes insufficient to implementthe manufacturer's recommendations without at least some in-house interference validation studies.
In Lab B2, proposed rules reduced total flagging by 33% (BaselineN = 39 [0.007% of total]; Proposed N = 26 [0.005% of total]). Thisencompassed a decrease in flagging for potassium (Baseline N = 25[0.1% of potassium results]; Proposed N = 0) and increases in flaggingfor ALT (Baseline N = 1 [0.0% of ALT results]; Proposed N = 18 [0.1%of ALT results]) and AST (Baseline N= 0 [0.0% of AST results]; ProposedN = 5 [0.3% of AST results]).
No optimized rules were developed as ultracentrifugation proce-dures were already included in the proposed rules. Ultracentrifuga-tion was successful in clearing lipemic interference using data fromLabs B1 and B2 which already had ultracentrifugation proceduresin place under baseline policies. Ultracentrifugation has beenrecommended as the preferred method to reduce lipemia interfer-ences [3].
3.5. Final algorithm
The final version of the algorithm is shown in Fig. 1, including Lab B2specific rules for icteric interferencewith creatinine and GGT. Examplesof the optimized rules are shown in Supplemental Table S4.
3.6. Flagging concordance
Tube flagging concordance between baseline (manual) andproposed (automated indices) rules sets were performed for Labs Aand B2 (Table 5). Poor concordance was observed between manualand automated HIL flagging at both labs, which has been observedpreviously [5,7].
4. Conclusions
A process is described to select test specific cut-offs and develop de-cision algorithms for specimens with HIL interference. Interference wasidentified using automated serum indices with test specific HIL cut-offs.The instrumentmiddleware or LIS alerted technologists to the presenceof lipemia or icterus that needed ultracentrifugation or dilution. Testswith interference above the cut-off had an interpretive commentappended to the result. The number of test cancelations was limitedby flagging tests with lower levels of hemolysis interference instead ofcanceling them and by using interference reduction strategies forlipemia and icterus. Flagging analysis allowed for the development ofoptimized rules tailored for certain tests and patient populations to en-sure that clinically significant interference was reported. The develop-ment of optimized rules also ensured that more test results werereported (with a comment) in order to avoid any adverse events by fail-ing to report results. Analysis of the HIL flagging rates clearly demon-strated the effect of lab specific and population specific factors.Hemolysis flagging under proposed rules decreased in Lab A, but in-creased in Lab B2 demonstrating how lab specific processes for manualflagging play a role in flagging analysis. Lab B1 showed that flaggingrules need to be re-evaluated when changing instrument platforms,even from the same manufacturer. The effect of patient populationwas demonstrated by the differences seen in icteric flagging for creati-nine and GGT between community and hospital populations. Taken to-gether, this indicates that serum index algorithms are not universallytransferrable between labs or patient populations. An increase or de-crease in overall HIL flagging will depend on the lab in question, theirexisting process and the population they serve. The authors presentthis workflow for developing site-appropriate rule sets as a resourcefor labs intending to implement automated index reporting in their lab-oratories. It also applies to labs seeking strategies to further optimizetheir interference reporting processes. The lack of publicly availablerule sets in this area of lab medicine leaves every lab trying to designthe whole system from first principles. The current work clearlydemonstrates the benefits of determining flagging rates prior to imple-mentation of automated serum index algorithms in order to better un-derstand the effect on the laboratory workflow.
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.cca.2015.07.006.
Acknowledgements
The authors thank Tihomir Curic and Dan Henne for their assistancein obtaining data from the laboratory information system in Lab B2, andJenette Bourbonnie and Bernice Frandle for their assistance in compar-ing index measurements between analyzers in Labs B1 and B2.

38 J.M. Boyd et al. / Clinica Chimica Acta 450 (2015) 31–38
References
[1] CLSI, C56A: Hemolysis, Icterus and Lipemia/Turbidity Indices as Indicators of Inter-ference in Clinical Laboratory Analysis; Approved Guideline. CLSI Document C56-A, Clinical and Laboratory Standards Institute, Wayne, PA, 2012.
[2] G. Lippi, N. Blanckaert, P. Bonini, et al., Haemolysis: an overview of the leading causeof unsuitable specimens in clinical laboratories, Clin. Chem. Lab. Med. 46 (2008)764–772.
[3] P.L. Walker, M.A. Crook, Lipaemia: causes, consequences and solutions, Clin. Chim.Acta 418 (2013) 30–32.
[4] K.W. Ryder, M.R. Glick, S.J. Glick, Incidence and amount of turbidity, hemolysis, andicterus in serum from outpatients, Lab. Med. 22 (1991) 415–418.
[5] M.R. Glick, K.W. Ryder, S.J. Glick, J.R. Woods, Unreliable visual estimation of the in-cidence and amount of turbidity, hemolysis, and icterus in serum from hospitalizedpatients, Clin. Chem. 35 (1989) 837–839.
[6] H.J. Vermeer, E. Thomassen, N. de Jonge, Automated processing of serum indicesused for interference detection by the laboratory information system, Clin. Chem.51 (2005) 244–247.
[7] R. Hawkins, Discrepancy between visual and spectrophotometric assessment ofsample haemolysis, Ann. Clin. Biochem. 39 (2002) 521–522.
[8] G. Lippi, P. Avanzini, D. Campioli, et al., Systematical assessment of serum indicesdoes not impair efficiency of clinical chemistry testing: a multicenter study, Clin.Biochem. 46 (2013) 1281–1284.
[9] Roche, Serum indices: reduction of clinical errors in laboratory Medicine, 2007.
[10] G. Lippi, G.L. Salvagno, M. Montagnana, G. Brocco, G.C. Guidi, Influence of hemolysison routine clinical chemistry testing, Clin. Chem. Lab. Med. 44 (2006) 311–316.
[11] G. Steen, H.J. Vermeer, A.J. Naus, B. Goevaerts, P.T. Agricola, C.H. Schoenmakers, Mul-ticenter evaluation of the interference of hemoglobin, bilirubin and lipids onSynchron LX-20 assays, Clin. Chem. Lab. Med. 44 (2006) 413–419.
[12] J.Z. Ji, Q.H. Meng, Evaluation of the interference of hemoglobin, bilirubin, and lipidson Roche Cobas 6000 assays, Clin. Chim. Acta 412 (2011) 1550–1553.
[13] H.J. Vermeer, G. Steen, A.J.M. Naus, B. Goevaerts, P.T. Agricola, C.H.H. Schoenmakers,Correction of patient results for Beckman Coulter LX-20 assays affected by interfer-ence due to hemoglobin, bilirubin or lipids: a practical approach, Clin. Chem. Lab.Med. 45 (2007) 114–119.
[14] R.C. Hawkins, Correction and reporting of potassium results in haemolysed samples,Ann. Clin. Biochem. 43 (2006) 88–89.
[15] M.M. Mansour, H.M. Azzazy, S.C. Kazmierczak, Correction factors for estimating po-tassium concentrations in samples with in vitro hemolysis: a detriment to patientsafety, Arch. Pathol. Lab. Med. 133 (2009) 960–966.
[16] H.J. Vermeer, G. Steen, A.J. Naus, B. Goevaerts, P.T. Agricola, C.H. Schoenmakers, Cor-rection of patient results for Beckman Coulter LX-20 assays affected by interferencedue to hemoglobin, bilirubin or lipids: a practical approach, Clin. Chem. Lab. Med. 45(2007) 114–119.
[17] A. Saracevic, N. Nikolac, A.M. Simundic, The evaluation and comparison of consecu-tive high speed centrifugation and LipoClear(R) reagent for lipemia removal, Clin.Biochem. 47 (2014) 309–314.