Bone Conducting Hearing Implants€¦ · Join BATOD to get THE Magazine for professionals working...
Transcript of Bone Conducting Hearing Implants€¦ · Join BATOD to get THE Magazine for professionals working...

Join BATOD to get THE Magazine for professionals working with deaf children
www.batod.org.uk
British Association of Teachers of the Deaf
Bone ConductingHearing Implants
An abridged versionof the January 2015
BATOD magazinecontaining articles
about BCHIs

From your editorI am delighted that Sue Archbold,
CEO of the Ear Foundation, last year
persuaded me that Bone Conducting
Hearing Implants would be an
excellent topic for a magazine. She
also suggested this abridged version
of the magazine containing only the
BCHI articles which would then reach a much wider
audience.You will see from the articles that there is a
wealth of information about various aspects of these
devices. But there is more than just technical and
practical information – there are excellent pieces from
users – the parent voice and the pupil voice are well
represented amongst these articles. There is also a
thought-provoking article from an adult reflecting on her
experience with a BCHI as a child.
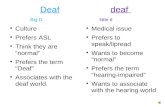
There are various names for Bone Conducting Hearing
Implants and it can become very confusing! The term
BAHA (Bone Anchored Hearing Aid) is often used, but
Baha is a registered trademark belonging to Cochlear.
Other terms include Bone Conduction Hearing
Implants/Devices. We have tried to be careful and
consistent in this magazine, but with many contributions
it is difficult to do so, and some terms have been used
historically and appear in papers referred to.
I hope that you will enjoy this special publication and
that it stimulates you to join BATOD so that you can
receive further full editions of the Association magazine.
You will be reading this because you are not already a
member. Please visit the membership page of our
website to find out about different categories of
member. You don't need to be a Teacher of the Deaf to
join nor do you have to be in the UK!
www.batod.org.uk The Association ► Membership
Magazine Editor
Bone ConductingHearing ImplantsDéjà vu... 1
What is a BCHI? 4
Interviews with Natasha and George 7
Living with my new BAHA 4 9
BCHI and radio aids 11
We Couldn't be Prouder – Sophie’s story 13
Sources of information 16
BCHI – a parent’s perspective 18
Arti’s BCHI Experience 19
Review – Tell it like it is! 20
Testing a bone conducting hearing implant 21
Freddie 22
Bethan 24
Active bone conduction 26
Skin care 27
Need to contact BATODabout other matters?Talk to Executive Officer Paul Simpson
email: [email protected]
answerphone/fax: 0845 6435181
Contents
Cover Photographs: Some of the BCHI users featured in this magazine.
For information on advertising rates see www.batod.org.uk
8 25

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 1
I feel as if I have been here before – 25 years ago! At that
stage, The Ear Foundation was established to fund the
first cochlear implants for children in the UK, as they
weren’t available on the NHS. At that time many Teachers
of the Deaf were very sceptical about this surgical
development and various comments I received included:
“no child I taught would ever have one..”, “Seen one,
seen them all....”, “it’s just a fashion... like grommets...”
Fast forward 25 years, and what about another form of
hearing technology: bone conducting hearing implants?
Do we realise what potential they have for large groups
of children or are we sceptical about another surgical
intervention? In other countries, such as the
Netherlands, bone conducting hearing implants are
routinely used for those children who need them; what
about in the UK? Do you work with any children with
these implants? Or have you children on your case load
who need one? The excellent BATOD magazine
seemed an ideal way to make up-to-date information
available, so the theme of this edition is bone conducting
hearing implants... and that is the first problem! What do
we call them? They have been called Bone Anchored
Hearing Aids (BAHA) but that is not possible, as the
Cochlear device is called Baha..... other names include
bone conducting hearing systems, and now many
cochlear implant centres have been renamed Auditory
Implant Centres, and the term commonly now used is
Bone Conducting Hearing Implants. However, this also
includes the fitting of soft bands – not implants at all!
Hopefully, other articles in this edition will clarify what
BCHI offer, and what they don’t offer.
Did you know?
l There are about 12,000 wearers of bone conducting
hearing implants in the UK
l They are suitable for those who cannot be aided by
the usual air conduction hearing aids
l Increasing numbers of children are considered – and
can be fitted by around four years of age when the
bones of the skull are mature
l Increasing numbers of young children are receiving
soft bands – from a few weeks old
l Bilateral bone conducting hearing implantation is
available
l A bone conducting hearing implant and an air
conduction hearing aid can be worn – one on each ear
l Bone conducting hearing implants can be used with
FM systems and accessories and remote
microphone.
The history of BCHI is an interesting one, which largely
came from dental expertise. The earliest references to
bone conduction aids are as far back as the 16th
Century with rod devices being used to transmit
vibrations via the teeth. The concept of hearing by bone
conduction was first popularised in the 1930s by Von
Bekesy. He discovered that cochlear hair cell excitation
was the same irrespective of whether the sound wave
pathway was via air or bone conduction. The
development of the carbon microphone and magnetic
receiver in the early 20th century led to the advent of the
bone conduction vibrator. The first modern bone
conduction hearing devices were adapted from existing
body worn air conduction aids where the receiver was
replaced with a vibrating receiver mounted on a tight
fitting headband to hold it onto the mastoid bone.
The challenges faced by
bone conduction aids led
to the idea of directly
coupling the transducer to
the skull. A Swedish
orthopaedic surgeon,
Professor Branemark,
serendipitously discovered
osseointegration. He had
been doing research on
blood flow in the rabbit
using a titanium inspection
chamber inserted into
bone. These chambers
integrated into the bone,
and the principle of
osseointegration (defined as ‘the formation of a direct
interface between an implant and bone, without
intervening soft tissues’) was established. Having
discovered that titanium could integrate into living bone,
the first application was in dental implants and the first
bone anchored hearing device was fitted in 1977 by
Tjellstrom.
A bone conducting hearing implant is effectively a
“middle ear bypass”, consisting of three parts:
l The implant: a tiny titanium screw implanted into the
skull, providing an anchor for the abutment and sound
processor
l An abutment which is attached to the implants
l The sound processor which acts as the middle ear,
converting the sound waves into vibrations, passed
through the implant to the bone, and hence to the
inner ear.
Déjà vu...It is 25 years since the first cochlear implants appeared in the UK to mixed opinion.
Sue Archbold reveals that there are similar mixed feelings about bone conducting
hearing implants
Professor Branemark

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
2 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
For young children, soft band systems are available, with
the sound processor placed on an elasticated head band
from a few weeks old. The usual referral pathway is
shown above.
The Ear Foundation now collects data from ten centres
implanting both children and adults and this is on our
website, continually updated; the data can be found as
the National Bone Conducting Hearing Implants
Registry at www.earfoundation.org.uk
A major problem for bone conducting hearing implants is
that the group of children who benefit from BCHI are
those whose hearing needs may not be apparent. For
example, those with chronic ear disease, those with
single-sided deafness, those born with genetic and
congenital syndromes which affect the development of
the skull bones and the inner and outer ears. These
children may not have profound hearing losses, but their
deafness may considerably affect their linguistic and
educational progress. For example, we know that
profoundly deaf children are achieving better
educational outcomes than severely deaf children, and
that profoundly and severely deaf children are achieving
better educational outcomes than mild or moderately
deaf children (NatSIP, 2013).
Single-sided deafness or a mild/moderate deafness
impacts on a child’s ability to hear in noisy
surroundings, and to hear the quieter sounds of speech
– which may contain grammatical markers and the
more subtle features of speech. A mild/moderate
hearing loss has been shown to impact on the
development of language and reading skills (Moeller,
Tomblin, Connor, Jerger, 2007) and on their functioning
in class (Most, 2004).
For those with a unilateral loss, language is likely to be
delayed (Bess et al 1998; Leiu, 2004; Lieu et al 2010;
Cone et al, 2010). A unilateral loss also affects the
development of pragmatic skills (Most & Peled, 2007); one
parent, interviewed in our study (Mulla et al, 2013) said:
“Unfortunately what we then still encountered was, wellshe’s got one ear and she’s just not listening. And in factI got hold of her school records and they, its actually onthere and I quote, from them, from memory because I’llnever forget it “class teacher feels (child’s name) usesher deafness as an excuse... we actually had herwithdrawn from school in the September.” (F004)
This is often overlooked, and it is just these children who
are likely to be overlooked in the classroom as their
needs are not obvious, and when prioritising case loads
in times of financial challenge are less likely to be
supported by services. Increasingly, Bone Conducting
Hearing Implants are being considered for those
children with very complex needs.
For those with a conductive loss, the impact on learning
in the classroom may be unrecognised, but there is

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 3
growing evidence of the benefit of soft bands and boneconducting implants for these groups (Doshi et al, 2013);Christiansen et al, (2010).
Bone conducting hearing implants require ongoing care,and for teachers there may be some uncertainty abouttheir care: with a percutaneous plug it can beconcerning. As one mother commented:
l “Yeah we’ve had that with the practice nurse (at GP).I couldn’t get a dressing put on it. She wouldn’t touchthe swelling – she was worried about it. Touching it.”(F006)
Cleaning the area requires confidence – which needs tocontinue into independence.
“Yeah Mum and Dad used to clean it every day andI think when I went to Uni I had to keep that up. Yeahand I did go to the nurse – they weren’t as good atcleaning it as my Mum and Dad were. And I think Dadhad to come with me to the nurse as well, to show themhow to clean it... I think at Uni the nurses were a bitreluctant.” (F002)
Ongoing care obviously relies on multi-professionalworking and trust... and even more liaison betweenmedical, audiological and educational services than atpresent. This edition will illustrate some excellentexamples; let us not restrict the options for these groupsof children because of lack of information. There aremany studies showing improved quality of life andlearning outcomes after BCHI gathered by surgicalteams. Thanks to BATOD for this opportunity to providesome information on current practice .... but let’s notforget a look to the future, and recognise the need toexplore the impact of these children in education, togather some real-life long term evidence of the potentialbenefits and the challenges.
Sue Archbold is the Chief Executive Officer of the EarFoundation.
References Bess FH, Murphy JD, Parker RA (1998). Children withminimal sensori-neural hearing loss: prevalence, educationalperformance and functional status. Ear & Hearing.19,339-354
Christiansen L, Richter G, Dornhoffer J (2010). Update onbone-anchored hearing aids in paediatric patients withprofound sensorineural hearing loss. Archives ofOtolaryngology Head & Neck Surgery. 136: 175-7
Cone BK, Wake M, Tobin S, Poulakis Z, Rickards FW (2010).Slight, mild sensori-neural hearing loss in children:audiometric, clinical and risk factor profiles.Ear & Hearing. 31, 2, 202-212
Doshi J, Banga R, Child A, Lawrence R, Reid A, Proops D,McDermott AL (2013). Quality of Life Outcomes after bone-anchored hearing devices surgery in children withsingle-sided sensorineural deafness. Otology andNeurotology. 13, 34-1, 100-103
Lieu J (2004). Speech language and EducationalConsequences of Unilateral hearing loss in children. Archivesof Otolaryngology Head & Neck Surgery 130: 524-30
Lieu JEC, Tye-Murray N, Karzon RK, Piccirillo JS (2010).Unilateral hearing loss is associated with worse speech andlanguage scores in children. Pediatrics. May 10
NATSIP (2013) Outcomes Benchmarking Report
Moeller MP, Tomblin B, Connor CM, Jerger S (2007). Currentstate of knowledge, language and literacy of children withhearing impairment. Ear & Hearing. 28, 740-753
Most T (2004). The effects of degree and type of hearing losson children’s performance in class. Deafness and EducationInternational 6: 154-166
Most T & Peled M (2007). Perception of SuprasegmentalFeatures of Speech by Children With Cochlear Implants andChildren With Hearing Aids. Journal of Deaf Studies andDeaf Education. Vol 12. Issue 3. 350-361
Mulla I, Wright N, Archbold S (2013). Views and Experiencesof families on Bone-Anchored Hearing Aid Use with Children:A study by interview. Deafness and Education International.15, 2, 70-90
BATOD represents you at various meetings andwe may be asked for demographic information.If you provide these details and keep them up-to-date it will help us to help you. Log into theBATOD website and then ► My Details
www.batod.org.uk

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
4 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
A bone conducting hearing instrument (BCHI) is a
hearing aid system that allows sound to be conducted
through the temporal bone directly to the cochlea (inner
ear). This is known as bone conduction as it carries the
sound through the bone in the skull. Sound vibrations
are delivered to the skull by a processor which
stimulates the cochlea. This process bypasses the usual
air conduction pathway of the ear canal and middle ear.
Who is suitable for BCHI?
BCHI devices are suitable for children with permanent or
longstanding conductive hearing loss, single sided
deafness or mixed (conductive with sensorineural
component) hearing loss. This could be congenital (from
birth) or acquired. Suitable candidates can have either
no previous experience with hearing aids or have
already trialled a conventional air conduction hearing aid.
Conductive hearing loss
Many children with a permanent or longstanding
conductive hearing loss could benefit from a BCHI.
The hearing loss can either be unilateral (in one ear) or
bilateral (in both ears).
Conductive hearing losses could be caused by
l middle ear disease
l perforation (hole) of the ear drum
l collapsed or very narrow ear canals
l atresia/microtia – a malformation of the ear canal or
outer ear
l long standing glue ear
l otosclerosis – fusing of bones in the middle ear
l ongoing or chronic ear infections
l syndromes – such as Down syndrome and
Treacher Collins.
As the BCHI sends sound directly through to the cochlea
via bone conduction, the conductive element of the
hearing loss is bypassed. Studies suggest that patients
with an average air-bone gap of 30 dB or more will
experience advantages with a BCHI compared to air
conduction hearing aids. This is because less
amplification is required as the cochlea is stimulated
directly, as opposed to an air conduction aid where more
gain is required to get sound through the part of the ear
that has the conductive hearing problem.
Single sided deafness (SSD)
Children with SSD and satisfactory hearing in their
better ear could benefit from a trial with a BCHI.
What is a BCHI? Laura Marl and Maureen O’Hare give an overview of Bone
Conducting Hearing Instruments
Fig 1. Diagram illustrating sound transmission with a BCHI
Fig 2. Audiogram illustrating a left sided conductive hearing loss
Fig 3. Illustration ofcontralateral routingof signal via boneconduction

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 5
The BCHI picks up sound from the deaf side and sends
it via bone conduction to the better ear’s cochlea. This
gives the child the perception of hearing sound from the
deaf side which could possibly help with sound
localisation and improve the signal to noise ratio.
This can be a suitable option for children who have a
congenital or acquired SSD.
Mixed hearing loss
Many children with a mixed hearing loss, in either one or
both ears may be suitable candidates for a BCHI. Bone
conduction thresholds up to 55 dB can be considered.
Children with an air-bone gap of 30 dB or more are
suitable candidates. Children with a greater air-bone gap
will perceive significantly increased benefit.
How the BCHI is worn
There are two different ways that BCHIs can be worn:
on a softband or on a surgically implanted
abutment/magnet.
Softbands
It is possible to fit a child with a BCHI on a softband from
a very young age. Early access to sound amplification is
vital for a child’s development, speech and language
skills and educational progress. If a child has a bilateral
hearing loss, then consideration should be given to a
bilateral BCHI fitting. The softband can be substituted
with an Alice band for older children.
The softband is used to hold the BCHI transducer
against the skin at the back of the ear over the mastoid
bone. It is important that the softband has sufficient
tension to hold the BCHI in place; otherwise the sound
quality will be poor and the device may give feedback.
Softbands are available in a range of sizes and are
adjustable to enable adequate tension. Different designs
and colours are available. It is recognised that bone
conduction sound transmission via a softband is not as
Fig 4. Audiogram illustrating right sided SSD
Fig 5. Illustration of a left sided mixed hearing loss
Fig 6. Examples of softbands from different manufacturers

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
6 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
effective as through an implant as the amplified sound
has to travel across the skin tissue. If the child
demonstrates good outcomes with the softband then an
implanted BCHI can be considered.
Implanted option
The BCHI can be worn without a softband as a
permanent solution. This involves a surgical procedure
to implant a titanium screw into the skull. Surgery can
only be performed when a child has sufficient skull
thickness to allow the implant to be inserted and
retained. For the majority of children, surgery can be
considered from the age of four to five years upwards.
However, for some children with additional medical
conditions/syndromes, the skull thickness may not be
suitable until they are significantly older. If the device is
implanted before the child has appropriate skull
thickness, there is an increased probability that the
implant will fall out.
Before anyone is considered for a surgically implanted
BCHI, it is essential they have a full audiological
assessment and a trial of the BCHI on a softband. If they
are deemed suitable candidates and the trial is
successful, both the child and parents will need to be
counselled about the surgery and expected outcomes.
There are two ways of retaining the BCHI processor:
1. Abutment (transcutaneous)
Once the titanium screw is implanted into the mastoid
bone, an abutment can be attached which then
protrudes a little way
through the skin over
the mastoid bone.
The bone conduction
processor then clips on
and off the abutment
with a snap coupling.
Comparing the BCHI
worn on the softband
to when worn on the
abutment, there tends
to be an average of
10-15 dB improvement
in sound conducted.
As the abutment protrudes through the skin, hygiene is
very important. The site must be carefully monitored and
cleaned every day to ensure it does not become
infected. Children must have easy access to their BCHI
service for treatment if required.
2. Magnet (percutaneous)
It is possible for a BCHI to be worn attached to a
magnet so there is no abutment protruding through the
skin. There are two different methods to attach the
magnet to the bone of the skull.
a. The first process is the same as the transcutaneous
option, but instead of an abutment a magnet is inserted
under the skin which attaches to the titanium screw
implant. A second magnet is then attached to the sound
processor which connects with the internal
percutaneous magnet, holding the processor in place
and allowing sound vibrations to be transmitted through
the skull to the cochlea.
This process of sound transmission is not as effective
as the transcutaneous abutment. Therefore, the magnet
is currently only a suitable option for children with
satisfactory bone conduction thresholds in at least one
ear (i.e. not mixed losses). Currently this option is only
available to children 8 years old or above.
b. The second method does not use a titanium screw in
the skull but a floating mass transducer (FMT) that is
housed within the bone of the skull and screwed into
place. The FMT is attached to a coil magnet which sits
under the skin. The outer processor is held in place
externally by a second magnet. This system delivers
sound by bone conduction to the cochlear via vibrations
from the FMT.
This is a suitable option for children with bone
conduction thresholds of up to 45 dBHL. A recent
approval has been given for this type of BCHI to be
used in children over the age of 5.
The percutaneous magnet is a fairly new development
in the BCHI field, so may not be widely available in all
implant centres.
Parents and professionals working with the child can
Fig 9. Illustration of percutaneous BCHI using an FMT
Fig 8. Illustration of percutaneous BCHI
Fig 7. Transcutaneous abutment
Continued at base of opposite page ►

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 7
test the device by
performing
listening tests
using a test rod.
The BCHI is
turned on and
held firmly against
the mastoid. The
ear canals are
then occluded,
which simulates a
temporary
conductive
hearing loss. The listening check can reassure parents
and teachers that the device is functioning correctly.
Further information regarding BCHI can be found on the
Ear Foundation website (www.earfoundation.org.uk),
the National Deaf Children’s Society website
(www.ndcs.org.uk) or by contacting your local Audiology
Service who can refer children for assessment at a
BCHI implant centre.
Laura Marl and Maureen O’Hare are both Audiologistsworking at Alder Hey Children’s Hospital in Liverpooland are part of the BCHI team.
Pictures courtesy of Cochlear, Oticon and Bruckhoff.Fig 10. Illustration of test rod
My name is Natasha and I am in Year
10 at High school.
I like craft and drawing. I study
Geography, Art, Textiles and Drama at
school (as well as all the other mandatory
subjects). I really enjoy Art! I love it so
much!
I have two sisters and three pets –
Poppie and Titch (dogs) and I walk them
every night! I also have a cat called
Jessie.
I do get extra help in school; it helps me
reach my full potential!
Basically my BCHI is a bone anchored
hearing aid that snaps on to a titanium
abutment; I feel that it really helps me and
that I wouldn't be able to manage without
it! I do use a radio aid – it helps me hear
better in lessons and really makes a
difference!
The best three ways someone could help
me in class are:
1 Look at me when speaking
2 Make sure they speak clearly and have
a clear lip pattern so I can lip read them
3 Speak directly and use the radio aid.
In the future, I would like to be a teacher!
I have wanted to be a teacher since I was
little! I also would like to work at Disney
World Orlando!
Interviews with Natashaand GeorgeElizabeth Reed-Beadle introduces two young BCHI users
►What is a BCHI? – continued from bottom of previous page
Continued on next page ►

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
8 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
George is in the final year of his A level studies
in a mainstream High school
I am in my last year of A level study, I have two
Oticon Ponto Power Bone anchored hearing aids.
I have been asked to write about the use of my
radio aid in school.
I use the radio aid every day! It has become an
essential part of studies during A levels.
I find the radio aid especially useful during Physics
and Chemistry when we have an experiment to do,
as the teachers may wander when explaining the
practical and giving instructions. Particularly if it's
an assessed practical, it is vital to ensure I hear all
instructions, and the radio aid is perfect for this.
The radio aid is always useful. However, when a
teacher is talking to other students it can transmit
what they are saying to the receiver and can be a
distraction at times. Fortunately, the transmitter
has a mute button which can prevent this from
happening.
The radio aid has made a massive difference to
my school life; before, when my teachers used to
wander around I never used to be able to hear
them clearly all the time, and this has helped me to
ensure I can hear my teachers clearly all the time.
My teachers are all very happy to wear the FM and
all of them see it as a new
toy that's fun to wear and
think it's a marvel that such
a thing exists to help people
who are hard of hearing.
I would highly recommend
the FM system to anybody
who feels like they are not
getting the full extent of
their education, as it’s vital
to ensure you hear and take
in everything your teachers
are telling you.
Elizabeth Reed-Beadle isan Educational Audiologistat Virtual School SensorySupport, Norfolk.
Have you the skills and inclination to come forward to be afellow Foundation Trustee to support and help shape its work in
improving the education of the deaf children and young people?
Our current focus is Acoustics Find out more www.batodfoundation.org.ukContact us [email protected]

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 9
When I was 11 years old, I had a perforated eardrum
due to an infection I got from swimming. I was finally
referred to an ENT consultant and 45 years later I am
still under their care. When I was 18, I had a radical
mastoidectomy as I had an inflammation of the mastoid
bone. This left me with a mild hearing loss and
consequently I started to speak with a louder voice
than before as I couldn’t monitor my voice properly.
Over the years I have suffered from many ear
infections and my hearing thresholds have dropped
because of this, and about twelve years ago, they
dropped to a moderate level (50/60 dB loss) and my
voice got even louder. To compensate for this, I would
always make sure people were on my right-hand side,
and I’d sit at the front of any group, use my good ear
for the phone, have the TV and car radio on loud and
ask people to repeat things.
Years ago, one of my students had a BAHA and the rep
from the original BAHA company came to talk to my
colleagues and me about them as part of our
professional development in audiology. It set me
thinking, so I asked my ENT consultant to refer me to
Hope hospital in Salford where they performed this
procedure. After assessment by audiology and another
ENT consultant, I had to trial a post-aural digital hearing
aid. I loved it but had a constant wet ear so I tried a soft
band BAHA and that seemed better. After listening to
what was involved in acquiring a BAHA I decided to go
ahead and a date for my day surgery was set!
A bone anchored hearing aid is one of many different
hearing aids prescribed on the National Health Service,
alongside digital hearing aids and cochlear implants.
Even though it is a hearing aid, the funding for this type
of aid comes out of a different budget from other types
of aids and your local PCT and doctor have to agree to
it. About two years ago, I
attended a BAHA day for
professionals at the Ear
Foundation and it was
here that I learnt about this
funding. I had never known
anything about this as my
operation and fitting had
gone ahead with no
problems at all.
Traditionally a titanium
plug is surgically implanted
into the mastoid bone, an
abutment is connected to the plug and a sound
processor is connected to the abutment. Titanium is
used for the plug because the body osseointegrates the
titanium and it conducts like bone – this is called the
Branemark Principle. The procedure took about an hour
under local anaesthetic and I chatted to the surgeon as
he was working. It was like root canal work at the
dentist, as you can hear and feel everything but it
doesn’t hurt. Honestly!
I now have a titanium abutment in my skull just behind
my left ear, up to the right and not in the way of my
glasses. After three months, when the metal had
embedded into the bone, I returned to get my BAHA
which clipped into the abutment. The whole process
from request to actually wearing the BAHA took about
12 months.
It took me a while to get used to clipping the BAHA in
without getting my hair caught in it. It is dark in colour to
match my hair so it is almost invisible. Initially I had the
volume on low but as my brain got used to bilateral
sound, it was reset to a higher level. I hadn’t realised
how my brain used to cross over sound, and what noise
I had been missing. I was given a soft brush to brush off
any dead skin that collects around the abutment, a box
to keep it in and a transparent tube for others to test the
aid by clipping the aid to it and placing it on their
mastoid bone. The NHS will replace it once if I lose it,
have repaired it when required and I’m now on my third
upgrade which is a digital
one. The previous two were
analogue ones.
I was fitted with a standard
BAHA last summer but I had
so many problems with
feedback it really drove me
crazy!! It went bananas
when I sat in my kitchen and
the washing machine was
spinning and when there
was any high pitched sound,
it whistled very loudly due to
feedback which others could
hear. I talked to my specialist
Audiologist at Salford about
these issues and he tried to
reset it. I talked to my ENT
consultant, Mr Rothera
about this and he had told
Living with my new BAHA 4Mary Fortune shares her experiences of obtaining and wearing her new
state of the art BAHA

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
1 0 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
Cochlear about these problems of feedback. As I was a
ToD and had an abutment that would support another
device from another company, he agreed that I could
trial another bone anchored hearing aid with feedback
management. This all meant that the audiology
department would have to commission a new company
which would take time. In the meantime Cochlear had
been developing a new BAHA with feedback
management so I was one of the first to try the new
BAHA 4 in the North West in Spring of this year! Many
thanks to manager Pat Clough and my specialist
audiologists Glen Robinson and Gemma Jones at
Salford Royal.
It has many new features: the main one being the Dual
Track Feedback Manager, a special program to deal
with wind noise when out walking (I have three to toggle
through: the first for all-round sound, the second for
direct sound in front such as when listening to the radio
in the car and the third program for walking) and being
able to receive phone calls via Bluetooth. To use this
feature you need a Cochlear Wireless phone clip which
has to be connected via Bluetooth to your BAHA and
you can buy this as one of the many accessories
available. I have one which is great once I had learnt
how to use it correctly!
On the plus side, it has enabled me to regulate the
volume of my voice and people have said I do speak
more quietly than before. I can now hear whispers on
my left-hand side and people talking in the back of the
car more clearly. It is great to hear music and sound in
stereo, especially at the cinema and theatre and to
answer my phone in the car via Bluetooth. I feel I can
be a positive role model for my students and I
completely understand how easy it is to forget your
hearing aid in the morning when you are in a hurry!
On the down side, the hearing aid can flick off when
taking a top off or when holding an umbrella too close to
the head and the abutment isn’t fully flush with my skull
so I can feel it when I lie on my left-hand side in bed. In
fact when I was trying to use a cordless Radio system
with my BAHA, there was too much interference due to
the scarring around it so I had a slightly longer
abutment screwed in. It also means I can wear a hat
without taking off my BAHA now.
At the Ear Foundation training day I was also
introduced to a new way of fitting a bone anchored
hearing aid using a magnetic implant by a company
called Sophono. All I know is that is means that there is
no abutment sticking out of your head. Just recently one
of my FE students has had this procedure but as he
hasn’t got his bone anchored hearing aid yet, I can’t
compare it to my BAHA. Would I want this type of bone
anchored hearing aid if I had the choice now? I’m not
sure but I wouldn’t be without my new BAHA 4!
Mary Fortune is a ToD in Stockport. She is also an NEC member.
ToD email forumNeed an answer or some advice?
Ask your fellow Teachers of the Deaf…This open email forum has been used to
♦ share information about research projects
♦ ask for ideas for presenting curriculum information
♦ get help from colleagues across the UK
♦ discuss
– buying and using radio aids for use at home,– issues relating to pay and conditions of
Teachers of the Deaf– speech discrimination testing
Find out more visit www.batod.org.uk > home page
Reminder for current and future members:
BATOD manages this forum which is hosted by the
Department for Education. Any information about
changes of email address or other enquiries should
be sent to [email protected]
Increase your skillsCheck the BATOD website calendar forcourses that expand your knowledgeand skills as a ToD or audiologist. Links to many of the providerwebsites.www.batod.org.uk ►EVENTS
On your first visit you need your BATODmembership number (on the label sheet inthe Magazine mailing), the post code yourmagazine comes to and an email addressthat you will need to quote when you log in.Click REGISTER and follow the instructions.
Have you registered yet?
Make sure you can access the members’
information and ‘hidden’ files for members only?

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 1 1
Elizabeth explains: As the years have passed the
technology available to enable children to experience
sound has become more and more sophisticated. My
first encounter with a child and a bone anchored hearing
instrument was over twenty years ago. It was a simple
instrument which clipped to a titanium abutment
implanted into the child's mastoid bone. The aid was
either on or off; it was a no frills instrument but it allowed
this child with atresia to experience sound. Now, in
2014, the technology has moved on and today a
Teacher of the Deaf may find him or herself working with
a young child with a bone anchored hearing instrument
attached to a soft headband before they are old enough
to have the surgery to implant the abutment.
I work in a large rural county; we are quite a large team
of peripatetic and resource based staff and as such
each member of the team needs to be knowledgable
about types of hearing instruments worn by the children
in the county and especially those on their caseload.
Once qualified as a Teacher of the Deaf, CPD is very
important in order to keep informed about current
hearing technology.
Exactly what does a Teacher of the Deaf need to know
about bone conducting hearing instruments and where
does that information come from?
Colleagues in my team cited the following as being
important information to know about children on their
caseload with a bone conducting hearing instrument
(BCHI);
A Aetiology and how that may affect the
child's functioning. For example is the
issue purely a middle ear condition or is
there a cosmetic element to the
condition eg; microtia and atresia
(malformation of the pinna and ear
canal)?
B Unaided and aided hearing thresholds.
It is important to provide INSET to
mainstream staff about what an
individual child can and cannot hear
with the BCHI. They may be reluctant to
wear it and if mainstream staff
understand what benefit it gives they
may be more encouraging in getting the
child to wear the BCHI.
C Type of BCHI and how it is worn; hard
or soft band and whether surgery is
impending is important information
needed to ensure consistency of approach by
mainstream staff on the wearing of the device(s).
D How the BCHI works and how to troubleshoot;
confidence in handling the device and in training
mainstream staff in its use and care.
E What FM receiver fits the BCHI; at the moment one
size does not fit all and this can be an issue for
Sensory Support teams, not only financially but
practically too having to assimilate knowledge of
various receivers.
F The time to have "hands on" practice with the BCHI,
including troubleshooting, battery fitting, listening,
and FM fitting.
Where does all this information come from?
1 The local hospital audiologists may be willing to train
individuals when the child is at clinic. They may be
willing to provide an annual update to a team
meeting.
2 It is always worth asking the company which provides
the model of BCHI used in your area if they will come
and provide some training. This may be more of an
overview rather than a "hands on" session but if you
don't ask you don't get!
3 Company websites are useful, as are independent
charity websites and a list can be found in this
magazine of sources of information. (See page 22)
BCHI and radio aidsTwo bite bars and a bag of chips – Elizabeth Reed-Beadle and
Imran Mulla talk about working with children with a bone
conducting instrument in 2014
Team of Teachers of the Deaf in training on BCHIs

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
1 2 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
4 The BATOD magazine and regional and national
training days.
Are there any essential pieces of equipment to have
in your ToD toolkit when you have a child with a BCHI on
your caseload?
The following may be useful:
l batteries
l a bite bar for testing if the BCHI is working, although it
is possible to test this without one
l hearing aid wipes, as it is good practice to use them
to handle the BCHI initially.
Do schools need to take extra care? A care plan is
always a good idea and essential if the child has an
abutment.
This is not an exhaustive list and if the practice in your
area does something different, please tell BATOD about
it so we can share information.
Does all this happen in the reality of the busy schedules
Teachers of the Deaf run? In my team yes it does. We
believe it is vital for Teachers of the Deaf to keep
themselves up to date especially in today's world where
technology does not stand still for long!
BCHI and FM
There are currently two types of BCHI in use in the UK –
from Oticon, the Ponto family and from Cochlear, the
BAHA family. These BCHIs can be FM enabled but take
different receivers.
The Oticon BCHIs use a special receiver with three
straight pins and the Cochlear devices use a Europin
Direct Audio Input (DAI) which enables an MLX type of
receiver to be plugged in directly. It's an issue for
sensory teams as the BAHA receiver can only be used
with the Oticon instrument and usually has to be bought
separately. The Oticon family instruments have to be
programmed for FM but once the audiology clinic has
done its job the FM fitting can be done in school the
usual way.
The mainstream teacher of a Reception aged child
recently fitted with a Ponto Pro power on a softband
reports that the use of a radio aid has been beneficial to
the child, she commented:
“It is obvious that he can hear whoever is speaking and
wearing the transmitter because his responses are
faster. We use the radio aid when the children are on the
carpet listening and the child is much more responsive
to my voice. The transmitter is worn by whichever adult
is working with child and all the adults have noticed a
difference in the child’s responses to questions and
eagerness to communicate. Remembering to mute the
transmitter is difficult for us all but we will get used to
doing that.”
This was the school’s first experience of a child with a
BCHI and a radio aid. The child uses a Phonak Inspiro
transmitter and a BAHA FM receiver.
BCHI and remote microphone technology
Imran gives further information: Both Cochlear and
Oticon Medical devices have improved receiver
connectivity options in their latest device models. The
BAHA 4, Cochlear’ s most recent bone conduction
device, still has the Europin Direct Audio Input (DAI)
which allows for RM/FM receivers to be fitted in directly.
Other accessories that can be fitted into the BAHA 4 DAI
include the audio adapter (3.5mm jack which can be
used in place of headphones) and the Cochlear BAHA
telecoil. The BAHA 4 also has a range of proprietary
wireless accessories that connect directly to the device,
including Mini Microphone, Phone Clip, Remote Control
and TV Streamer. The Mini Microphone wirelessly
transmits the speaker’s voice directly, improving signal
to noise ratios at distances of approximately seven
metres, without the need for a receiver device as this is
built into the BAHA 4. However, this does not replace the
need for an FM system in the classroom. For more
information on the BAHA 4 connectivity options see the
following webpage: www.cochlear.com ►Cochlear
Products ►Baha® Bone Conduction Implants
►Baha 4 Sound Processor ►Wireless accessories
The Oticon Medical Ponto Plus and Plus Power are the
most recent bone conducting devices from Oticon
Medical and both have wireless connectivity with the
Ponto Streamer. The Ponto Streamer has multiple
connectivity functions allowing direct connectivity with
Bluetooth enabled devices like mobile phones, mp3
players, tablets and laptops. It also has a built-in Europin
DAI socket where an RM/FM receiver can be plugged in
allowing for wireless streaming of the RM/FM signal to
one or both Ponto Plus devices. Other connectivity
options with the Ponto Streamer include proprietary
connection with the Oticon Connect Line system of
accessories including the Connect Line microphone and
TV streamer. The Connect Line Microphone can be
used at distances of approximately 15 metres and
transmits the signal wirelessly through the Ponto
Streamer to the Ponto Plus processor. For more
information on Oticon wireless connectivity options
please see the following webpage:
www.oticonmedical.com►Our Products
►Wireless►Ponto Streamer – wireless opportunities
Below are some useful websites when searching for the
compatibility of various RM/FM receivers with different
hearing devices: www.comfortaudio.com►professionals
►Support and service►Compatibility Guide
(on the bottom left hand corner select type then the
option to select brand, series and model comes up).
www.phonakpro.com/uk►support►compatibility
►FM Configurator
(select brand from the drop list, and the option to select
product line and hearing instrument comes up).
Elizabeth Reed-Beadle is an Educational Audiologistat Virtual School Sensory Support, Norfolk.Imran Mulla is Consultant Research Audiologist at The Ear Foundation.

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 1 3
Hi, my name is Fiona. I am 30 years old and married to
Colin. We have two beautiful children, Sophie and
Caleb. We live in Lisburn, Northern Ireland. I would love
to share Sophie’s journey so far with you.
On 7th December 2010, at 8.31pm we were blessed with
a beautiful daughter, Sophie Faith Ross. I remember so
clearly the moment the midwife said "It's a girl". The
picture on my husband Colin's face was priceless. He
had secretly wanted a 'daddy's girl'. We had so much
love already for this little bundle. As I lay thinking about
how proud I was of myself for surviving labour I heard
the words "she has a wee folded ear". Colin tells me that
I replied "Aw just like mine" (I have a quirky fold at the
top of one of my ears). Then I saw a slightly worried look
from Colin. He brought Sophie over to me so I could
have a look for myself. At first glance I wasn't concerned
as they did literally look like they were folded over and
just need unfolded. The midwife tried to reassure us and
suggested that it might be a case of her having some
kind of procedure to correct them. I was so delighted to
have my baby in my arms that I didn't dwell on her ears.
No one else seemed that worried so I wasn't.
Back down on the ward we sat in awe of Sophie. She
was simply gorgeous. Neither of us really mentioned her
ears. We both then started to look more closely at them
and fiddled with them. Suddenly things seemed
worse...there was no hole/canal. What was there for her
ear didn't seem much and it didn't look like they could be
unfolded to me. My mind went into overdrive. Could she
hear me? Did I cause this? Why had her ear not
formed? Was she deaf? To be honest even though my
head was spinning with unanswered questions I still
wasn't overly concerned. The joy of holding Sophie
outweighed everything.
The next day we carried out all the usual routines that
come with a newborn – feeding, bathing, changing
nappies, settling and all the while I wondered whether
she could hear my voice. This seemed to be the most
pressing question on my mind. Later in the afternoon a
paediatrician came round to see us. He was quite a
quiet man who barely introduced himself. He examined
Sophie very carefully as we sat in silence. Then came
the words I didn't want to hear..."So does deafness run
in your family?". His words broke my heart and as I
looked over at Colin I could see in his eyes that his heart
was broken too. The doctor left to get us some
information and returned with a printed out sheet. He
explained that he thought she had a condition called
microtia and that we would be seeing an ENT doctor the
next day. I sobbed for Sophie. Why her? We were
moved to a private room for privacy. Visitors came and
went and this was a distraction from the reality of the
situation but deep within I was devastated.
It's probably a good time to give you some info on
microtia as, like me back then, you might never have
heard of it. Microtia literally translated from the Greek
means ‘little ear’. It is the medical word to describe a
small or absent ear. Most children with microtia will have
some degree of hearing loss on the affected side. This is
because the middle ear, which contains the eardrum
and tiny ear bones, is affected as well as the outer ear.
In some children the ear canal is blocked or absent, so
sound waves cannot pass through the ear in the normal
way. Generally, although the outer and middle ear are
affected, the inner ear is healthy so some options for
restoring hearing are available. Children with bilaterial
microtia will usually need some form of hearing aid at a
young age to enable them to develop speech. This is
We Couldn't be Prouder – Sophie’s storyFiona Ross describes her daughter Sophie’s life with microtia and her journey from
birth to age four, happily living with bilateral implants
My first cuddles with Sophie
I couldn't stop staring at this wee beauty

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
1 4 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
often a ‘bone conduction hearing aid’ that transmits
sound waves to the inner ear through the bones of the
skull. In very young children, these hearing aids are
usually on a headband, but as a child grows older a
‘bone anchored hearing aid’ might be suggested.
Our appointment with the ENT doctor the next day was
extremely informative and reassuring. He took time to
explain exactly what microtia was and answered all of
the questions we had. He gave us a general plan as to
what would happen next and referred us on to the
surgeon he described as the best consultant for the job.
Things seemed to be a bit clearer and we were able to
enjoy our daughter with a bit more hope.
At around a month old we met with our consultant and
Sophie had her hearing tested. It was decided that she
would be fitted with a bone conduction aid which would
be on a headband. We were so excited that she would
finally be able to hear! Alongside this, other
professionals became involved. Sophie was referred to
speech and language therapy and a Teacher of the Deaf
was assigned to us. In March 2011 she was fitted with
her hearing aid. This was another moment that I
remember so well. As the hearing aid was turned on and
I spoke – she cried. I also cried! After a few minutes she
got used to being able to hear and was enjoying
listening to everyone! Another milestone in her little life.
Fast forward 2.5 years to September 2013. Sophie is
nearly three and has worn her hearing aid religiously
every day. She has reached various milestones in these
three years including being discharged from speech
therapy. We couldn't be prouder. We have had regular
reviews with our consultant who monitors her progress
and plans ways forward. One of these will be her getting
an implant for her hearing aid. This is commonly done
around the age of four when the skull is thick enough.
We now had the opportunity to trial bilateral hearing aids
to see if they brought any improvement to directional
sound. Again we were very excited as this was another
development in improving Sophie's hearing. She
received her second hearing aid at the end of
September.
Coming into 2014 we saw a huge improvement in her
hearing. She started to show some directional
responses to sound and now relies heavily on both
hearing aids to hear. If one turns off or falls off she would
describe it as 'not being able to hear properly'. She is
now approaching the age for implant...eek! Our
consultant is keen to go ahead but wants to implant one
side only. This is what he knows best. Bilateral implants
have never been done before in Northern Ireland. As
Sophie's mum my views were different. I see daily how
she relies on both of her aids. I have seen the
improvements two aids have made. It was my job with
the support of others to convince him to implant
bilaterally and in one operation.
As parents we want what's best for our children. Sophie
is too small to make decisions so it is up to us to make
the best decisions for her. If I had a pound for every time
I doubted our decision I would be very rich. Maybe the
consultant is right? Is one implant enough? Are we
rushing into this? Should we wait for further
developments in technology? The list of questions is
Sophie being fitted with her BAHA softband
Sophie enjoying some toast after her operation

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 1 5
endless. Deep down I knew it was the right decision as
I know my little girl best.
To be honest it didn't take as much convincing as we
thought. We put forward our thoughts and feelings and
the next thing we were signing on the dotted line. Sophie
was finally on the waiting list for bilateral implants. She
would be the first child in Northern Ireland to receive
them. We finally got the phone call to say Sophie’s
operation would be on the 3rd September. I experienced
a mixture of emotion all at once. Excitement, nerves,
relief and the doubt crept in again too! We explained to
Sophie that she would be getting diamonds (much
prettier than screws) which she would be able to click
her hearing aids onto. She was as excited as we were
especially at the prospect of not having to wear a
headband anymore.
On the day of surgery Sophie was an absolute star! She
was so brave. Everything went smoothly and to plan.
Her skull was a little thinner than expected so we have
to wait a bit longer before we can 'go live'. Her
'diamonds' have to be cleaned every day to prevent
infection and this will be a lifelong routine. We are very
much looking forward to getting her new hearing aids
hooked up at the end of November!
When I look back on the past four years I can't be
anything but proud of what we have achieved as a
family with the support of our wider family, friends and
professionals such as Patrice, who was Sophie’s speech
therapist, and Fionnuala, Sophie’s Teacher of the Deaf.
Fionnuala continues to support Sophie and us as a
family. She visits us at home and spends time assessing
Sophie and offering invaluable advice. Sophie’s
favourite times with her are when she brings the toys!
She also visits Sophie in nursery to make sure that her
additional needs are accommodated. Sophie has
reached so many milestones with ease and is happily
settled in nursery. In years to come when bilateral
implants are the norm in Northern Ireland, I will be
delighted to tell her she was the first ever!
Fiona Ross is Sophie’s Mum.
Our beautiful Sophie loving life!
Searching for a QToD?Job vacancies can be advertised on the
BATOD website at a cost of £250.00If you have to re-advertise the same post,
the cost is reduced to £150.00
Teaching Section – Situations Vacantwww.batod.org.uk
one of our most popular pages – especially on aMonday with hundreds of ‘hits’!!!
email your Word file [email protected]
with instructions about invoicing and your advertshould appear very soon afterwards
AND REMAIN VISIBLE until after the deadline!
Your email address will be an active link sopotential applicants can contact you directly
Embedded logos should be sent asadditional .jpg or .gif files as well
Value for money advertising
Why not follow us on Twitter?
@BATOD_UK

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
1 6 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
As with other hearing technologies, developments in
bone conducting hearing implants are taking place fast,
and it is important to keep up to date, to provide
accurate information for parents, young people and
families. Useful information can be obtained from:
► The Ear Foundation website:
www.earfoundation.org.uk provides information,
downloadable information leaflets, user stories, a user
forum, and shop for accessories if you look in the Bone
Conducting Hearing Implants section of the Hearing
Technologies section. In the download section you will
also be able to find an edition of ENT News which has
several interesting articles on the surgical and scientific
aspects of bone conducting hearing implants. The site
also has a booklet for parents and children about getting
a bone-anchored hearing processor, and the research
section has reports from research studies into bone
conducting hearing implants. The site also provides a
shop where Cochlear and Oticon Medical spares can be
obtained.
► At ndcs.org.uk you will
find their booklet on
information for
parents and
families on
bone anchored
hearing aids,
and their
Quality
Standards
booklet on bone
anchored
hearing aids.
► Cochlear.com provides information on Baha® bone
conducting hearing implants and their Baha® users app
► Oticonmedical.com provides information on their
Ponto system
► Sophono website for those interested in Sophono
devices https://sophono.com/
Sources of informationThere is a wealth of information available on the subject of BCHIs and Sue Archbold
gathers together a useful collection of resources

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 1 7
► Medel.com for information about their
Bonebridge system, an active middle ear implant,
and for user stories
► Down’s website for those interested in
Down’s syndrome http://www.downs-syndrome.org.uk/
► Goldenhar website, for those interested in Goldenhar
syndrome http://www.goldenhar.org.uk/
► Bana UK, for those with acoustic neuroma
http://www.bana-uk.com
► nhs.uk for the latest commissioning guidelines for
BCHI and the latest criteria and recommended practice.
Tablet ♦ smartphone ♦ PC ♦ laptopNo matter how you access it, the BATOD
website provides members with a wealth ofinformation, advice and materials to support
professionals working in deaf education
EXPLORE!!
news ♦ events ♦ resources ♦ jobsExplore the fantastic resource that is
www.batod.org.uk

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
1 8 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
Reuben lost complete hearing in his right ear when he
was two years old, after suffering from Pneumococcal
Meningitis.
Shortly after starting school Reuben started to wear a
wireless cross hearing aid, which helped him to pick up
more sound on his right side; however, it was far from
ideal. One of the biggest issues was that he now had a
mould in his good hearing ear, blocking sound from the
ear that he had grown to rely on. Whilst his audiologist
was able to make adjustments to bring his hearing up on
this side it sometimes felt like “robbing Peter to pay Paul”.
The size of the aids also meant battery life was
extremely short and we recently found out that Reuben
had not always felt comfortable in alerting his teacher.
This meant he wasn’t keeping up in class and was also
getting told off for not paying attention. Reuben also
suffered from regular ear infections in his hearing ear
and at times like this he was like a child with next to no
hearing - he relied on copying others and lip reading but
this was exhausting for him.
It was incredibly frustrating for him and for us; with the
best will in the world, trying to make people aware of his
need for good positioning of him and the teacher in the
class room, as well as his inability to localise sound, was
not always easy. I found myself constantly trying to
convey to the adults with whom Reuben interacted, the
need for him to see their faces when they spoke to him,
to clearly articulate their words and to not keep moving
about, but, be it teachers, after-school club or lunch-time
staff I often felt like I was unable to really explain how
hard it was for him. When hearing and listening continue
to be difficult for an eight-year old boy the option to just
switch off and not make the effort was by far the easiest.
A year ago, following a consultation at Birmingham
Children’s Hospital, Reuben began the assessment
process as a candidate for a BCHI and started to wear an
Oticon Pronto Pro on a softband. We knew that a boy
wearing a softband would be likely to draw some
unwanted attention and so agreed with his year group
teachers that I would come into school and explain it to
his year 3 peers. This was incredibly useful and
something I would recommend in a similar situation.
When he started to wear the softband it was accepted as
quite normal and the children were interested in how it
helped him.
It was obvious straight away that the BCHI far better
suited Reuben. He gained hearing on the side of his
non-hearing ear but not at the detriment of the hearing he
did still have on the other side. We also saw signs of him
getting a better perspective of where sound was coming
from and the ability to cope better when there was
increased background noise. He did however find the
band got uncomfortable and it became a habit for him to
take it off at afternoon playtime and not put it back on until
the next day. This amounted to more than five hours a
day where he was at a distinct disadvantage to his peers.
In the last couple of months, Reuben did begin to become
far more conscious of the softband and so it was with
great relief that he had the two stage operation to have
the abutment put into his skull. This brought with it the
benefit of further increased hearing, no pressure on the
head from the BCHI and of course no soft band.
It is still early days (the BCHI has been worn on the
abutment since early November 2014) but so far the
results, especially the level of hearing gained, have
been phenomenal – I would go as far as saying life-
changing! He wears his BAHD all day, every day and is
learning to understand and give names to the new
noises that he hears on a daily basis. It is only now that
he is hearing this full spectrum of sound that I can see
just how much he has missed out on in the past. For a
child with single sided deafness the consequences of
not having full hearing are more subtle and so often
overlooked but when we don’t hear, and can’t
distinguish the everyday sounds in our environment
(sounds that pass a person with normal hearing by) our
ability to interact and form a connection with our
environment is far harder. For a nine-year old boy this
interaction and connection are vital in helping him reach
his full potential both now and in the future.
Louise Savage is Reuben’s mum.
BCHI – a parent’sperspectiveLouise Savage explains how her son's implant is helping him achieve his potential

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 1 9
This year marks 20 years since I was fitted with my first
bone conducting hearing implant (BCHI). As I was only a
little five year old girl at the time, it was up to my parents
to make the biggest decision of my life. Luckily for me, it
was the best decision they’ve ever made.
Why I have a BCHI
I was born with Treacher Collins Syndrome (TCS), a
genetic condition affecting the growth and development
of bones in the face and ears. There is a wide spectrum
of severity and I am fortunate to have a very mild case.
My parents suspected very early on that I had a hearing
loss as my speech was delayed and I wasn’t reacting to
normal everyday sounds. I was finally diagnosed with a
moderate bilateral conductive hearing loss when I was
two years old. Shortly after, I was fitted with ‘behind-the-
ear’ hearing aids.
Although these hearing aids were good, they were not
very suitable for me. I suffered from frequent ear
infections and wax build up. My parents also struggled
to keep the hearing aids in my ears. At one point, they
even had to resort to using double-
sided sticky tape to help the hearing
aids stay in!
Getting the BCHI
Thankfully one day an ENT consultant
at my local hospital mentioned that I
might be suitable for a bone conducting
hearing implant. Unlike today, softband
trials didn’t exist, so my parents had to
go by the word of doctors. Once they
were convinced, we were soon on our
way to Birmingham Children’s Hospital
for my assessment. However, like many
other people, there was another battle
to secure the funding for my implant
and new hearing aid.
But, after a long few months, I was
sitting in Birmingham Children’s
Hospital waiting to have the operation
that would change my life forever. I
don’t remember much about the
operation, just waking up afterwards
with the biggest bandage on my head
and receiving the cutest teddy bear as
my get well present.
Three months later, I was finally fitted
with my BCHI. On the day of my fitting,
I went shopping with family and it was
clear my parents had made the best decision. After a
few months, my parents noticed that my speech had
improved; I was more confident and doing better at
school.
Growing up with my BCHI
After my operation, I remember going back to school
and showing everyone my new hearing aid and telling all
my friends how it helped me to hear better. My
classmates were all fascinated by it and I got to be the
‘cool kid’ for a while. As I was the first BCHI user many
people had encountered, my Teacher of the Deaf (ToD)
was always on hand to explain to my teachers and
support staff what this new hearing aid was, how it
worked and what to do if any problems occurred.
I can still remember the first time my ToD showed me
my first radio aid. It was this strange looking box with
wires longer than I was. I wasn’t very keen on it, but my
ToD said it would help me hear the teacher better at
school. Needless to say, she was right; I was able to
hear the teacher perfectly whilst cutting out the noisy
Arti’s BCHI ExperienceArti Patel explains why she regards her BCHI as her prized possession

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
2 0 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
classroom. Thankfully, technology has moved on miles
from then and today’s FM systems are much smaller
and wireless too – allowing both teacher and student to
move around the classroom as they need.
As with any hearing aid, there are advantages and
disadvantages. My journey with my BCHI has been a bit
of a rollercoaster, but it’s definitely all worth it. I seem to
have very sensitive skin and I am prone to flare-ups
around the abutment. However, these are only minor
issues and I can still wear my hearing aid and carry on
with my day. Growing up, my parents cleaned the area
daily which takes as long as it does to clean your teeth.
However, today I am able to maintain it myself (much to
the relief of my parents)!
During secondary school and university, I had no
hesitation telling the world about my BCHI. On the few
occasions that other students saw my BCHI, they were
never sure what it was and I was always pleased to see
the look on their faces as I explained that it’s a hearing
aid and not some hi-tech music gadget.
Life today with my BCHI
As my hearing aid is very discreet and hidden
underneath my huge hair, many people are unaware of
my hearing loss. I’ve been very fortunate that my
friends, family and employers have understood my
hearing loss and taken a keen interest in my hearing aid.
There has been a huge development in bone conducting
hearing technology over the last few years and I can’t
wait to see what comes next. Although I’ve been offered
a second BCHI, I’m comfortable at the moment with just
one. Sometimes, I also wear a second BCHI on a
headband at times during large meetings and it’s been
great to actually hear something behind me!
My BCHI is my most prized possession (even more than
my mobile) and I’m pleased to be in a position where
I can share my experience and raise awareness of the
brilliant piece of technology. The BCHI gives me the
confidence I need, knowing that it’s going to help me
hear with clarity and I’m not missing out on anything. It is
with huge thanks to my parents and elder sister, along
with the support of many health and education
professionals, that I’ve been able to come this far.
Arti Patel is a Membership Assistant at The NationalDeaf Children's Society, a volunteer with The EarFoundation and Trustee of the Treacher Collins FamilySupport Group, working to increase awareness of BCHIs.
Tell it like it is!Author Cochlear implanted children’s support
group
Publisher www.gemini-print.co.uk
Reviewer Corinda M. Carnelley, Teacher of theDeaf, London Borough of Croydon
However empathetic one is, however many counselling
courses one has attended, ultimately there are not
many ToDs who know what it is like to have a deaf
child, or an implanted child. Yes, we know the theory
behind the practice; yes, we know about targets, Ling
sounds, and mapping, but we don’t actually know what
it is like to live on a daily basis with a small person who
cannot hear or who relies on highly expensive
technology to access sound.
Parents, by their very nature, tend to want to compare
their children with others, and even those who are not
comparing overtly are probably doing so covertly. This
book is an amazing window into the world of other
parents, implanted children, successes, and challenges.
The book itself is A4 format and each page is one family’s
story. What makes it stand out from other similar
publications is that it is written by parents, for parents. It
has a couple of very clear explanatory pages at the
beginning about what is a cochlear implant, sound
processors, and why parents should consider
implantation. However, one of its greatest strengths is
the most extraordinary indexes – you can search for
stories by cause of deafness, by implant scenario, by
method of communication, educational placement,
grandparent stories, teenager
stories, and more. The book itself
is not long – 80 pages, but it is
very easy to find what you are
looking for.
So, however much as
professionals we tell parents
that comparisons are invidious,
that all children are different
and all circumstances are different – parents do actually
want to be able to look and say, “This happened for this
child so it may happen for mine.”
I loaned the book to a mother whose child was about to
be bi-laterally implanted. When I asked her about it a
couple of weeks later she said, “It was amazing” and “It
became my bible and my homework all rolled into one.”
Perhaps, most telling, when I asked her if I might have it
back to put in the Service library she said, “I thought you
said if I liked it I could keep it.” Target achieved.
The CICS Group (Cochlear Implanted Children's
Support Group) is a completely voluntary charity run by
parents who have children who use cochlear implants.
The Group offers contact, information and support and
events for families whose children already have cochlear
implants and for those who are considering an implant
for their deaf child
For further information or to order copies contactTricia Kemp at [email protected]. Single copies are available free (although a donation tocover p & p would be appreciated). Otherwise thebooklets are available in boxes of 36 for which there is a delivery charge.
Reviews

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 2 1
For both ToDs and parents, it is important to carry out
daily listening checks on hearing instruments, especially
for young children, to ensure that they are performing to
their optimum.
Connevans, in conjunction with the Ewing Foundation
Technicians, developed a special listener for both the
Cochlear Baha and Oticon Medical Ponto sound
processors so that you can carry out these daily
listening checks easily.
The Baha/Ponto Listener consists of a
stainless steel stem that is mounted with
a transducer into an acrylic base. The
vibrations from the BCHI processor are
transmitted via the stem to the
transducer and turned into an electrical
signal. The signal is then amplified
using either a Crescendo portable
amplifier or the FM Accessories
Tester and listened to with a pair of
headphones. ToDs who themselves
wear hearing instruments can use a
neckloop or direct input cable to listen instead.
This allows you to check each day that the sound is
consistent. The listener is suitable for use with
bone anchored processors by both Cochlear and
Oticon Medical.
It is important to mount the sound
processor correctly onto the stem or
you risk damaging the processor.
Please follow the instructions
supplied with the listener in order to
mount the sound processor correctly.
You can also listen to a Baha sound
processor using a shaped piece of
plastic called a bite bar supplied by
Cochlear, which is gripped between
your teeth with the sound processor
mounted on the end. The vibrations
from the processor are
conducted along your
jaw bone to the
cochlear and heard
as sound. Personally, I
found it uncomfortable
to use and not very hygienic.
BCHI processors can be used with Radio Aids with
either ear level receivers or body worn receivers.
The Baha/Ponto Listener is particularly useful for
checking that the Radio Aid is working correctly and that
the audio level into the sound processor is giving an FM
Advantage to the user.
The listener can be used in the following way in order to
set up or check a Radio Aid system:
1 Connect the Sound Processor to the Baha/Ponto
Listener and adjust the volume so that it is
comfortable.
2 Ask a colleague to talk to you at arm’s length distance
from the sound processor and make a mental note of
the volume level.
3 Connect the Radio Aid system and turn it on. Your
colleague should then take the transmitter and walk to
the other side of the room whilst talking normally into
the microphone at 150mm from the mouth.
4 If you can, adjust the volume level of the receiver so
that your colleague’s voice is louder by approximately
10 dB than just through the Sound Processor alone.
This will subjectively give you the FM Advantage that
is required. If the volume cannot be adjusted you will
at least be able to check that volume level through the
radio aid is achieving an FM Advantage. This process
is the same for all makes of radio aid, including the
new Roger systems from Phonak.
The Baha/Ponto Listener is also useful for making sure
that the Audio Adaptors that are available for connecting
the processors to audio devices such as MP3 players,
radios, TVs, computers etc.
are working correctly.
In conclusion, any Teacher of
the Deaf who has a BCHI user
on their caseload should have
one of these handy devices in
their arsenal.
John Popplestone is a directorof Connevans Limited.
Testing a bone conductinghearing implantJohn Popplestone stresses the importance of regular testing and shows how a
Baha/Ponto Listener can be used to test Cochlear and Oticon Medical instruments
Cochlearprocessors fitinside the mount
Oticon Medicalprocessors fitover the mount

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
2 2 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
History
Freddie was referred to the Paediatric Hearing Implant
Centre at St Thomas’ Hospital, London and was seen
for an initial assessment in November 2009.
Freddie was born at full-term by emergency caesarean
section at Farnham Hospital. He was referred to Great
Ormond Street Children’s Hospital following his birth due
to suspected CHARGE syndrome. The clinical genetics
team at GOS confirmed the diagnosis of CHARGE in
February 2009.
Freddie failed the newborn hearing screen and was
referred to local audiology; he was 4-6 months old.
Initially his hearing loss was suspected to have a
conductive element possibly due to middle ear effusion
and therefore grommets were fitted in June 2009. He
then had ABR testing in August 2009 by local audiology,
which was reported as highly indicative of a bilateral
severe-to-profound sensori-neural hearing impairment.
Freddie was subsequently fitted with high powered
hearing aids but did not make any progress. He was
then referred for cochlear implant assessment.
Audiological Information
Freddie was assessed by the Hearing Implant Team for
suitability for cochlear implantation. Initially it was difficult
to get audiometric behavioural responses for air
conduction or bone-conduction stimuli. Therefore whilst
under general anaesthetic for scanning, objective tests
were performed. ABR testing showed that Freddie did
have a profound sensorineural hearing loss in the left
ear but in the right ear his bone conduction thresholds
were within normal limits. Therefore following objective
testing it was found that he had good cochlear function
with a severe conductive overlay. The CT scan revealed
bilateral oval window atresia and absent stapes bones
with MRI scanning revealing a hypoplastic nerve on the
left side.
As Freddie had good right sided cochlear function he
was not a cochlear implant candidate. It was decided by
the team and family that surgical BAHA would be
appropriate management in his case. Due to Freddie’s
age, he was 2 years 3 months old at this stage, he was
fitted with a Bone Anchored Hearing Aid (BAHA) on a
softband until his skull was thick enough to have a
surgical BAHA.
Functional Listening
Freddie was an excellent softband BAHA user wearing
the aid practically all waking hours. Freddie could detect
all the Ling sounds /a/, /e/, /oo/, /m/, /sh/ and /s/ with his
BAHA, indicating that he had good access to all the
frequencies in the speech spectrum. Mum reported that
his listening steadily improved and that he was making
more and more vocalisations.
Freddie was seen in the Specialist Clinic in December
2011 when he was four years old and it was decided
that the surgical BAHA could now take place and he was
listed for surgery.
FreddieMarsha Jenkins introduces Freddie, who has CHARGE syndrome, and describes
how he came to be a very successful user of a BAHA

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 2 3
Surgery and Outcomes
Freddie had two stage BAHA surgery, with stage one in
May 2012 and stage two in December 2012. The BAHA
processor was fitted and activated in April 2013. Freddie
is an excellent user wearing his processor every day at
home and at school. Freddie conditions beautifully for
play audiometry and gives excellent aided responses
across the speech frequencies. At his last review
appointment in September 2014 he managed to perform
automated speech perception testing. Freddie tackled
the Toy Discrimination Test. This test measures the
loudness level at which a child can identify familiar
words with 71% accuracy. Freddie was seated in front of
a touch screen computer where ten toys were pictured.
He was asked to “Point to the X”. Instructions were
presented at varying loudness levels depending on the
accuracy of Freddie’s response. Freddie did very well in
his very first attempt, identifying the toys with 71%
accuracy at 45 dBHL. This was fantastic work.
Freddie has been a delight to work with over the last
four years; the team looks forward to working with him in
the future and monitoring his continued progress. Well
done Freddie!
Marsha Jenkins is Principal Clinical Scientist (Audiology)at St Thomas' Hearing Implant Centre (Paediatric).
Our FreddieFreddie was born on the 7th November 2007. He was
born with a facial palsy and had trouble feeding;
because of this he was taken straight to the special care
baby unit. He was a 9 pound 6 ounce baby, and he
looked huge compared to all the premature babies.
Once admitted to special care, he was given a hearing
test, which showed he was deaf, but the diagnosis and
the extent of his hearing loss took a while to find.
Along with other problems, including a mild case of
CHARGE Syndrome, we had to spend a lot of time at
various hospitals. Eventually Freddie was diagnosed
with middle ear hearing loss, which meant he had a
small amount of hearing in his right ear, so would be
eligible for a BAHA, not a cochlear implant as we first
thought.
Because of his hearing loss, Freddie has quite bad
balance, so has had a number of falls and has cut his
head open quite a few times, so we have had quite a
few trips to A & E.
He was using a BAHA on a band to begin with which
meant he was getting some sound; then in May 2012 he
had the first part of his implant which involved an
operation to place a metal plate into his skull. I think
when Freddie was put to sleep it was more traumatic for
us than him – bless him, he was brilliant. Freddie woke
up after the operation with a large bandage round his
head and was very unhappy, trying to pull it off, but
eventually calmed down. His head took a couple of
weeks to heal including regular checks with the doctors.
By December 2012 Freddie was due for the second part
of his operation, which involved an abutment being
attached on the outside of his head where the metal
plate was put in his skull. The abutment is just like the
popper on a coat or jacket that the hearing aid is
inserted into. By April 2013 it was time to switch it on;
this meant the hearing aid he wore on a band would
now be popped on to the abutment on his head, which
gave much better hearing. It was very emotional when
he had his hearing aid switched on as the first thing he
did was mimic the sound of the door opening, and he
had a big smile on his face.
It took some time getting used to the BAHA but
eventually he got used to it and wears it all day at
school. He is coming on leaps and bounds at school,
and has just had a fantastic report
at parents’ evening. He also signs
and it is lovely to watch Freddie
and his little brother George
signing to each other and playing
nicely. Sometimes it's a bit of a
struggle at home with mummy and
daddy, as like any child he can
sometimes be quite naughty, but
we are getting there.
Freddie's speech is coming along
really well also, and he is doing so
well in all areas of his life. He also
has regular eye checks, a growth
hormone injection every night and
checks with urology and genetics.
We're very proud of our Freddie,
he is a real little character and
"charms" everyone he meets with
his big brown eyes. He is turning
out to be a strong and happy boy.
Anna Bridel is Freddie’s mum.

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
2 4 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
I was born with microtia to my right ear which literally
means ‘small ear’ and meant that I was born with an
under developed right ear. In my case I was born with
grade 3 which meant I literally just had a peanut-sized
fold of skin/tissue instead of an ear. Due to being born
with microtia I had no hearing at all in my right ear, as I
had no external ear, so there was nowhere for me to
physically be able to hear sounds. However, my left ear
was completely normal and thankfully had no hearing
issues.
Things were definitely hard for me at school even before
I had realised this for myself, such as when I was in
infant school I thought everything was completely
normal and I didn't think I was different in the slightest.
However I did struggle, as I found out some
years later from my parents; for example I
struggled a lot with knowing where sounds
were coming from. I used to always have to
be sitting near to my class teacher when on
the carpet and had one to one support from
a classroom assistant.
It was only as I got older, towards the age
of eight, that I began to realise that I wasn't
the same as everyone else but different,
although still being young I didn't
understand why I was different from
everyone else. I began being bullied which
then affected my self-esteem and
confidence and I felt like it was a bad thing
being different. The bullying made me very
self-conscious including about my hair and
I tried to make my ear as unnoticeable as I
could and kept it covered with my hair
(except in PE). The bullies made me feel
embarrassed to be who I am and to ask for
any help with my hearing, so I did often fall
behind in class as I was too scared to ask
the teacher to repeat things.
I decided in 2006 I wanted to have my ear
reconstructed using my rib cartilage, so that
when I went up to secondary school, the
older kids wouldn't notice my ear or not as
much as they would have done at that time.
This was done in two stages, the first being
in 2006 and the second being in 2007 –
both of them were done at Great Ormond
Street Hospital in London by my surgeon
and consultant Neil Bulstrode. The results
were a lot better than I ever expected them
to be and my surgeon went above and beyond any
images I had in my mind, I hadn't expected it to look as
realistic as it did.
However I did still get bullied in secondary school and
worse than I had in juniors.
It wasn't until I left school and started college that I
began to feel confident and happy about my ear (even
though I was happy with my ear once reconstructed) but
this was like a different form of happy and I felt like I
could put everything behind me and move on into the
future and I wanted my ear to be a part of that, as it still
was a part of me. I started researching and looking into
microtia more, as I was very determined to find
BethanBethan describes her life with microtia which led to her being bullied at school and
the difficulties she encountered in trying to get fitted with a BCHI

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 2 5
someone, anyone else out there, who had a little ear like
mine. Luckily I did find out more information so that I
fully understood what microtia was and why my ear was
different. I also came across a support group on
Facebook called Microtia Mingle UK which was and still
is a HUGE help and it helped me to be connected with
other people and their families of all different ages who
had microtia. I found out about Bone Conducting
Hearing Implants through one of the meet ups arranged
by this group, where I met two girls similar in age to me
who were wearing them and explained to me and my
parents what they were and how they worked.
The day after that Mingle my dad rang my consultant
and surgeon Neil Bulstrode at GOSH to ask him about
Bone Conducting Hearing Implants and whether this
was something that could be suitable for me. He
agreed to speak to me and my dad at my next
appointment, which wasn't too far away and arranged
for me to go and see someone within the audiology
department to trial a Bone Conducting Hearing Implant
on a headband and I knew within seconds of it being
activated that I both wanted and needed to have one,
as it made such a huge improvement before it was
even in place properly, and was honestly the most life-
changing moment of my life.
Unfortunately we were told that due to my age (I was
16) I was unable to have the surgery done at GOSH.
However they were happy to refer me to the Royal
National Throat, Nose, Ear Hospital, also in London
and not that far away from GOSH. However,
unfortunately we had a long hard battle of getting the
Bone Conducting Hearing Implant due to the hospital
losing my information and not having a record of me
and then ending up with the same appointment multiple
times. We then had problems with my left ear as they
noticed that there was a loss in that ear too and so that
had to be resolved first and I had a regular hearing aid
fitted in January 2013. I eventually had my bone
conducting implant fitted in January this year and
although I had a few setbacks at the beginning with
regular infections, things are looking up and, fingers
crossed, are all going well. I honestly love having my
bone conducting implant and I wouldn't be without it
now, and I really don't know how I was without it for all
those years before.
My blog has now been up for 3 years. I'm completelybully free and growing in confidence and happiness withevery day and opportunity given to me with raisingawareness such as I recently gave a speech about myjourney with Microtia at the launch party of Microtia UK,a UK based charity for Microtia where I spoke to over400 people including medical professionals such asprofessors, surgeons, doctors and researchers as wellas those with Microtia and their friends, family andgeneral supporters.
http://www.microtiamingle.co.uk/
Deafness & Education International
Did you know that as a member ofBATOD, you are entitled to free online access to Deafness &Education International?
Volume 13 (2011), 4 issues a year
Editors: Linda Watson (University ofBirmingham, UK) & P Margaret Brown(University of Melbourne, Australia)
To access the latest journal articles, just follow thesesimple instructions:
1. Go to www.batod.org.uk
2. Log in as a member with your email address and BATOD password
3. Click on Publications
4. Click on Journal
5. Click on Deafness & Education International
6. Follow the link to the online journal content atIngentaConnect
Online access available for BATOD members
Did you know that as a member ofBATOD, you are entitled to freeonline access to Deafness &Education International?
Editors: Linda Watson(University of Birmingham, UK) & P Margaret Brown(University of Melbourne, Australia)
To access the latest journal articles, just follow thesesimple instructions:
1. Go to www.batod.org.uk
2. Log in as a member with your email address andBATOD password
3. Click on Publications
4. Click on Journal: Deafness and EducationInternational
5. Click on Deafness & Education International6. Follow the link to the online journal content at
IngentaConnect
Now available
BATODmemberrate
£5.00
Order your electronic copy from [email protected] quote your membership number
£10.00Updated
Like us on FacebookBritish Association of Teachers of the Deaf

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
2 6 • © B A T O D M a g a z i n e • J a n u a r y 2 0 1 5
The world’s first, and only, active bone conduction implant,the Bonebridge, is now available to help transform the livesof children over five years old.
Bonebridge is the first bone conduction implant system touse transcutaneous, intact-skin technology. This means thatthe implant is positioned completely under the surface of theskin, so that the protective role of the skin is fully preserved.This is especially importantfor children because itmeans the risk of externalinfection is significantlyminimised.
As active implants directlystimulate the cochlear, asopposed to passive systems which require an externaltransducer to transfer the energy through the patient’s skinfirst, audiological outcomes are improved. Additionally activeimplants require reduced skin pressure to retain theprocessor as the transducer is internal. This means thatchildren with a Bonebridge will wear their processors longeras they’re more comfortable to wear, and naturally this willimprove their hearing experience and development.
Hearing through the bones of the skullThe award-winning technology allows children and adultswith conductive hearing loss or single-sided deafness tohear again by actively transmitting sound through the bonesof the skull.
Like all MED-EL hearing implant systems, Bonebridge hastwo components: internally, the active implant and externallythe audio processor. The active implant converts the signalsfrom the audio processor into mechanical vibrations. Theseare transferred to the bones of the skull, which conduct thesound waves to the inner ear.
NEW – Introducing the SAMBAThe Bonebridge system includes the SAMBA* audioprocessor which allows users to connect to smart phones,FM receivers and other assistive listening deviceswirelessly. Thisstate of the artaudio processoris compact, verylightweight (7g inc. magnet),and easily hiddenunder hair.
Intelligent sound adapter The SAMBA distinguishes between different hearingsituations and automatically adjusts to the most appropriatesetting so users can hear speech and music in both noisyand quiet environments. The audio processor also has theability to learn and recognise manual adjustments that theuser regularly makes regularly, for example, if the useralways re-adjusts the volume in a quiet environment, theSAMBA recognises and stores this information.
Adaptive directional microphones – background noiseis a thing of the pastThe adaptive directional microphone automatically identifiesand minimises noise interference.
This feature is particularly helpful in situations where thereis loud background noise, such as in a classroom or theplayground.
Speech tracking – razor sharp speech from alldirectionsThis special feature automatically recognises the directionfrom which speech is coming and adjusts the directionalityof the microphone. In a classroom this means that a pupilbenefits from the optimum focus on speech; this works inthe same way for adults when driving.
Individual adaptable programmes The user can select one of five programs, each with its ownindividual settings, for particular situations (e.g. for noisyenvironments or for TV & music). This makes the SAMBAquick and easy to use.
Wireless connectivityThe SAMBA can be connected to external devices viaBluetooth or telecoil. This enables th signal from a FMsystem, assistive listening device, mobile phone, or MP3player to be transmitted wirelessly and with no loss of soundquality. These wireless connectivity functions are availablewith the Siemens miniTEKTM.
Backwards compatibility for added reassuranceOne factor that is especially important for children is thatMED-EL implant users can always benefit fromtechnological innovation in the future. MED-EL externalaudio processors are always backwards compatible withimplants meaning everyone can access the very latestprocessor technology at the time of their upgrade.
Sarah Humphreys, UK & Eire Vibrant Business UnitManager comments: “MED-EL strives to be at the forefrontof scientific innovation and offer patients with hearing lossa range of solutions that allow them to overcome hearingloss as a barrier to communication. The connectivity of ourlatest audio processor is a huge step forward in allowingpatients to communicate in the digital age, with moderndevices such as mobile phones connecting seamlessly tothe implant.”
The innovative Bonebridge implant system is now beingused worldwide with a high level of patient satisfaction,comfort and reliability with the system. For more informationabout this award winning technology and the full range ofMED-EL hearing implant solutions, visit: www.medel.com.
* The SAMBA audio processor is pending regulatory approval
Active bone conductionMED-EL introduce Bonebridge, active bone conduction with intuitive audio
processing, which is now approved for children

B o n e C o n d u c t i n g H e a r i n g I m p l a n t s
© B A T O D M a g a z i n e · J a n u a r y 2 0 1 5 · 2 7
The first bone anchored hearing aid was implanted at
Birmingham Children’s Hospital in 1988. Since then we
have implanted many children and have one of the
largest programmes in the United Kingdom. A bone
anchored hearing aid may be implanted for a variety
reasons but the wound care and aftercare are
essentially the same for any child with these devices.
There are currently two manufacturers who provide
bone anchored hearing aids: Cochlear and Oticon.
The advice for each device is the same too!
The surgery itself is usually done in two stages for
children. The first stage is when the implant is placed in
the skull of the child. The second stage is performed
about three months later when the abutment is placed
on the implant. The reason why there is a time delay is
to allow time for the bone in the skull to grow around the
implant. This is called osseointegration. Both stages are
mostly performed as a day case.
After the abutment is placed, I will see the child a week
after surgery to remove the dressings. On that same day
we try and fit the sound processor.
After the dressing is removed there are a number of
things that a parent/carer needs to do to ensure that the
skin around the abutment is cared for.
Cleaning the abutment
I advise that the abutment is cleaned on a daily basis.
This is to remove any debris from around the abutment,
rather like cleaning your teeth every day! I advise the
parent/carer that they can clean the abutment in a
variety of ways; with a soft toothbrush, with some cotton
buds or with a non-alcohol wipe. It’s the child’s and
parent/carer’s choice, but the message is the abutment
needs to be cleaned. Older children can wash the area
themselves in the shower or bath. I advise that the child
then asks somebody to take a look at the abutment
every couple of days just to check that the skin around
the abutment is OK. If debris is left around the abutment,
it can lead to a local skin infection which may be painful
and is also a nuisance.
Washing hair
From experience over the years, parents/carers have
informed me that simple baby shampoo is the best as it
doesn’t seem to irritate the skin around the abutment.
I advise that they can use a cool hairdryer around the
abutment to rid the area of any moisture. It is essential
that hair does not wrap itself around the abutment as it
can cause a local skin infection.
Skin infections
From time to time a child may get a skin infection around
the abutment. I advise that if the child has a skin
infection, the parent/carer should apply some antiseptic
cream to the area as soon as they can. I give them a
tube of cream and let the GP know what cream they
should use if there is a problem. If you notice that the
skin around the abutment is red, swollen, sore or
discharging, please inform the parent/carer as soon as
possible.
Swimming
Swimming is fine for a child with a bone anchored
hearing aid. Clearly the child needs to remove the sound
processor before entering the water. I would advise that
the abutment is rinsed when the child comes out of the
pool as swimming pool water can be quite dirty!! Rinsing
can be done with some plain tap water.
Accidents at school
Any accidents relating to the abutment should be
reported to the parent/carer. Unfortunately accidents do
happen! If the abutment is loose it can cause a local skin
infection. A loose abutment can also make the sound
processor whistle. The parent/carer should then contact
the nurse or their surgeon at their hospital and we can
give the necessary advice.
Pain
Pain from the abutment site is unusual. It can be treated
with simple analgesia. Any pain experienced by the child
should be reported to the parent/carer.
Advice for school
If at any time you would like to attend an appointment
at the ENT clinic with the child, we would be more than
happy to see you. Clearly you would need to get
permission from the parent/carer and the child
first. I know many Teachers of the Deaf who have
attended find the experience very useful for their
own learning.
Radio aids
Some of the children will benefit from radio aids in the
classroom setting. This is something that you may need
to assess when the child has been fitted with the
sound processor.
Useful websites
NDCS – National Deaf Children’s Society –
www.ndcs.org.uk
Ear Foundation – www.earfoundation.org.uk
Cochlear – www.cochlear.com
Oticon – www.oticonmedical.com
Jo Williams is an Advanced Nurse Practitioner ENT –Birmingham Children’s Hospital –[email protected]
Skin careJo Williams talks about the importance of wound care and after care following bone
anchored hearing aid surgery

Officers of Nations and Regions
BATOD contacts and Magazine Distribution
Northern Ireland [email protected]: Revolving postSecretary: Valerie McCreedyTreasurer: Antonette Burns
Scotland [email protected]: Catherine FinestoneSecretary: Jean McAllisterTreasurer: Elaine Harris
Wales [email protected]: Sallie Durbridge Secretary: Lisa WhitneyTreasurer: Rhian Gibbins
East [email protected]: Jo SayersSecretary: Trina RankinTreasurer: Joanne Hughes
Articles, information and contributions for theAssociation Magazine should be sent to:
BATOD National Executive Officer: Paul SimpsonTel/fax: 0845 6435181 Email: [email protected] should Association information and general queries.
Advertisements for the Association Magazine should be sent to:Elizabeth Reed-Beadle, BATOD Advertising Manager142 New Road, Hethersett, NR9 3HGTel: 01603 812111 Email: [email protected]
Full guidelines for submissions and abstracts of paperspublished in the Journal ‘Deafness & EducationInternational’ are to be found atwww.maney.co.uk/instructions_for_authors/deiEnquiries related to the Journal to: Dr Linda Watson, email: [email protected]
Manuscripts should be submitted online atwww.editorialmanager.com/dei
Midland [email protected]: post vacantSecretary: Angie WoottenTreasurer: Alison Garside/Robert Miller
North [email protected]: Sue DennySecretary: Trish CopeTreasurer: Sandy Goler
South [email protected]: Meryl HuntSecretary: Stevie MayhookTreasurer: Meryl Hunt
South West [email protected]: Post vacantSecretary: Hazel SutherlandTreasurer: Post vacant
DISCLAIMERThe Editors and the Association do not necessarily
endorse items or the contents of advertisementspublished in the Magazine and cannot accept
responsibility for any inaccuracies.Please note that items from this Magazine
may not be reproduced without the consent ofBATOD and the source must be acknowledged.
Photocopying items may breach copyright.
BATOD Magazine distribution by: The Creative Adult Project,
The John Townsend Trust, Victoria Road, Margate, Kent CT9 1NB
Association Magazine: ISSN 1366-0799
Published by: The British Association of Teachers of the Deaf,
21 Keating Close, Rochester, Kent ME1 1EQ
Printed by: Berforts Information Press Ltd
Southfield Road, Eynsham, Oxford OX29 4JB
Magazine Project Manager: Rosi Hearnshaw
BATOD membershipBATOD activities are funded from your membership fee and some advertising income. Colleagues who share your Magazine and Journal also benefit from BATOD negotiations withgovernment and other influential bodies ‒ but they are not contributing! Persuade your colleagues to join BATOD and you will receive 10% of their membership fee as an‘introduction fee’.
Full details of membership plus membership form are available at www.batod.org.uk ►The Association ►BATOD Membership
ToDs in training will be entitled to a £20 reduction in annual membership fee when the CourseTutor countersigns the membership application form for those paying by Direct Debit (applies for up to 2 years; payable at the end of the year).
The BATOD Membership Secretary may be contacted via [email protected] BATOD Treasurer may be contacted via [email protected]