Blood and Tissue Nematodes of Human Beings. FILARIAL PARASITES OF HUMAN BEINGS.
Blood Tissue Nematodes
-
Upload
afif-mamen -
Category
Documents
-
view
240 -
download
3
Transcript of Blood Tissue Nematodes
-
8/10/2019 Blood Tissue Nematodes
1/27
Blood and Tissue Nematodes
General Characters1-Adult worms live in the lymphatic, subcutaneous
connective tissue or body cavities.
2- Female worms are viviparous.
3- The early first-stage larvae, known as microfilariae
that have no differentiated organs inside, instead
there are columns of cells with prominent nuclei.
4- Filarial worms are transmitted through the bite of aninsect vector.
-
8/10/2019 Blood Tissue Nematodes
2/27
Filarial worms
They include the following species:
1- Wuchereria bancrofti.
2- Brugia malayi.
3- Onchocerca volvulus.
4- Loa loa.
5- Mansonella perstans.
6- Mansonella ozzardi.
-
8/10/2019 Blood Tissue Nematodes
3/27
Infective stage:
Filariform larva [3rd stage larva]:
It is about 1.5-2 mm x 20 um, with
cylindrical oesophagus and lies in
the labium of mosquito vector.
Mode of infection:
During bite by mosquito I.H,
filariform larva pierces human skin
through the puncture wound.
-
8/10/2019 Blood Tissue Nematodes
4/27
Wuchereria bancrofti
Disease: Bancroftian filariasis, wuchereriasis,elephantiasis.
D. H.: Man.
I.H. (vector): Female CulexMosquitoes.
Habitat: Lymphatic tissues of lower limbs &
external genitalia.
Microfilariae appear in the peripheral blood
by night [nocturnal periodicity] & disappearby day time.
-
8/10/2019 Blood Tissue Nematodes
5/27
Geographical distribution
Tropical & subtropical countries.
-
8/10/2019 Blood Tissue Nematodes
6/27
-
8/10/2019 Blood Tissue Nematodes
7/27
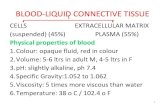
Morphology
Microfilaria:250-300x8 m in length & surrounded by a loose
sheath.
Body forms smooth (graceful) curves, has rounded anterior end
and tapering tail. Both ends are free of nuclei. It has a nocturnal
periodicity.
-
8/10/2019 Blood Tissue Nematodes
8/27
Nocturnal [microfilarial]periodicity theories
1- Biological adaptation between M.F. & night biting activity ofmosquito.
2- Chemical attraction between M.F. & saliva of mosquito.
3- During sleep, decrease oxygen content & increase carbon dioxide
content stimulate M.F. to migrate from blood vessels of lung toperipheral blood.
4- Khalils theory: Blockage of lymphatics; during day on upright
position of the patient; prevents M.F. to find their way to the
circulation.By night time & during sleep, relaxation of the patients body will
open the lymphatics allowing M.F. to reach the peripheral blood.
-
8/10/2019 Blood Tissue Nematodes
9/27
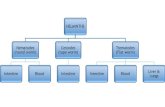
Life cycle of Wuchereria bancrofti
-
8/10/2019 Blood Tissue Nematodes
10/27
Life cycle
A- Development in man:
1- When an infected mosquito bites man to take a
blood meal, infective larvae are deposited on human
skin usually in pairs, penetrate the skin through the
bite wound or by its own activity.
2- Larvae pass to lymphatic vessels & nodes where
they mature in about one year & mate. The adult
worms are found in lymphatic of lower limbs, groin &
epididymis in males and labial glands in females.
3- Female mosquitoes produce many sheathedmicrofilariae which appear in peripheral blood at night
between 10 PM- 2 AM reaching a peak about
midnight [nocturnal periodicity].
-
8/10/2019 Blood Tissue Nematodes
11/27
Life cycle
B- Development in mosquito:
4- Microfilariae are taken up by a female mosquito
when it sucks a blood meal.
5- In the stomach of mosquito, microfilariae loose their
sheath, penetrate the wall of mid gut & migrate to the
thoracic muscles where they develop into infective
larvae.
6- Development in the mosquito takes 2-3 weeks.
Each ingested microfilaria develops into one filariform
larva [cyclo-developmental transmission].
7- Infective larvae migrate to the head region within
the labium ready to be transmitted when mosquito
takes another blood meal.
-
8/10/2019 Blood Tissue Nematodes
12/27
Pathogenesis & Clinical picture
1- Many infections are asymptomatic & are
detected only by blood examination.
2- The main pathology of filariasis is caused
mainly by living or dead adult worms.
3- Incubation period: one year or more.
The disease passes in 2 stages:
I-Acute (inflammatory) stage.
II- Chronic (obstructive) stage.
-
8/10/2019 Blood Tissue Nematodes
13/27
I- Acute (inflammatory) stage
Due to immune response to toxic products of living or dead
adult worms with superimposed 2nd infection.
There is infiltration with plasma cells, eosinophils &
macrophages in & around affected area.
Microfilariae cause less pathology.
Acute stage is characterized by
recurrent attacks of fever, lymphangitis & lymphadenitis.
-
8/10/2019 Blood Tissue Nematodes
14/27
-
8/10/2019 Blood Tissue Nematodes
15/27
II- Chronic (obstructive) stage
Fibrosis following the inflammatory process around worms & presence
of coiled worms inside lymphatics result in:
a- Dilatation of lymphatics leading to varicosity as hydrocele,
scrotal lymphoedema and lymphatic varices.
Hydrocele is the most common chronic manifestation & results from
accumulation of straw lymphatic fluid in sacs around testes.
b- Rupture of distended lymphatics proximal to the obstruction e.g. in
the pleural sac (chylothorax), peritoneal cavity (chylous ascitis), tunica
vaginalis of testis (chylocele), intestine (chylous diarrhea) or in urinary
passages (chyluria) with passage of microfilariae with urine.
c- Elephantiasis: Thickening & hypertrophy of the skin & subcutaneous
connective tissue of legs and genitalia [scrotum, penis& vulva] due to
disturbance of lymph drainage.
-
8/10/2019 Blood Tissue Nematodes
16/27
Mechanism of Elephantiasis
Increased permeability of obstructed lymphatic walls, leading to
leakage of lymph rich in protein under the skin causing cellular
proliferation of connective tissue & deposition of fibrous tissue.
Clinically: At first, the swelling is pitting but later becomes non-
pitting then the skin becomes thickened, rough, fissured and
susceptible to ulceration and 2nd infections with bacteria or
fungi.
Elephantiasis occurs after persistent high infection
for 5-10 years.
-
8/10/2019 Blood Tissue Nematodes
17/27
Bancroftian filariasis & Elephantiasis
-
8/10/2019 Blood Tissue Nematodes
18/27
-
8/10/2019 Blood Tissue Nematodes
19/27
II- Laboratory diagnosis
a- Detection of M.F. in peripheral blood at night [between 10 pm
& 2 am] by
1- Wet drop: for living moving microfilariae.
2- Giemsa stained thin & thick smears: show the
morphological characters of microfilariae .
3- Concentration method: if M.F. are scanty;
* Knott's technique: In a centrifuge tube, mix 5-10 ml of blood withequal volume of 2% formaline. Allow the mixture to stand for 10
minutes then centrifuge. Decant the supernatant and examine
the sediment for microfilariae.
* Nucleopore filter technique: Filtration of 1-5 ml of heparinized
blood through 5 m Nucleopore filter then stain & examine thefilter on a slide.
Provocative testTo obtain blood at day time, give the patient 50-100 mg DEC orally &
examine the blood within 30- 60 min.
-
8/10/2019 Blood Tissue Nematodes
20/27
Laboratory diagnosis (Cont.)
b- Detection of M.F. in chylous urine or in fluid aspirated from
hydrocele or peritoneal cavities.c- Demonstration of the adults worms in lymph node biopsy.
d- Immunodiagnosis
1- Skin test with antigenic extract of the dog filaria Dirofilaria
immitis.2- IHAT, IFAT and ELISA: for detection of filarial antibodies.
3- Detection of filarial antigens is specific & sensitive and can
detect early infection saving patients from complications of the
disease.
e- Molecular techniques: PCR.
f- High eosinophilia.
==
-
8/10/2019 Blood Tissue Nematodes
21/27
III- Imaging techniques
a- Ultrasonography: Viable adults may be seen
moving in lymphatics (filarial dance sign).
b- X-ray: shows calcified worms.
c- Lymphangiography: Shows lymphatic changes
e.g. dilatation of vessels.
-
8/10/2019 Blood Tissue Nematodes
22/27
Treatment
1- Antifilarial drugs:
a- Diethylcarbamazine [DEC]: 6mg/Kg/day for 12days, repeated every 6 months as long as the patient
remains microfilaraemic or has symptoms.
b- Ivermectin: Single oral dose of 150 ug/Kg body weight.
c- Combination of DEC & ivermectin: gives better results.
2- General measures:
Rest, antibiotics, antifungal, physiotherapy & bandaging.
3- Elephantoid tissues: Corrected surgically.
Prevention & control1- Mosquito control.
2- Treatment of patients.
-
8/10/2019 Blood Tissue Nematodes
23/27
Occult Filariasis
* Clinical conditions of hyper-sensitivity reactions tomicrofilarial antigens.
* The classical features of lymphatic filariasis are absent.
* Microfilariae are not seen in peripheral blood (due to its
destruction in the lung by the immune response) but
adult worms and microfilariae may be seen in the tissues.
* The condition may be caused by Wuchereria bancrofti,
Brugia malayi or by some animal filarial worms.
-
8/10/2019 Blood Tissue Nematodes
24/27
Tropical pulmonary eosinophilia (TPE)
TPE is the most important manifestation of occult filariasis.
There are low-grade fever, loss of weight, anorexia & pulmonary
symptoms (as dry nocturnal cough, asthmatic attacks), persistent
hyper-eosinophilia & glandular enlargement.
The condition is associated with a high level of filarial antibodies and
elevated IgE level.
These symptoms are relieved by ant-filarial therapy
[diethylcarbamazine (DEC)].
-
8/10/2019 Blood Tissue Nematodes
25/27
Brugia malayi
Similar to W. bancrofti in life cycle, diagnosis, treatment& control and differs as regards:
1- Disease: Malayan filariasis.
2- Distribution: Far East.3- I.H. (Vector):
Female Mansoniamosquito.
4- Reservoir hosts: Cats & monkeys.
5- Habitat: Lymphatic of upper limbs.
-
8/10/2019 Blood Tissue Nematodes
26/27
Microfilaria of Brugia malayi
Has loose sheath, with kinky curves & tail end
with 2 deeply stained nuclei; one in front of the other.
Microfilaria shows non periodicity or nocturnal periodicity
-
8/10/2019 Blood Tissue Nematodes
27/27
Pathogenesis & clinical features are also similar to bancroftian
filariasis, but hydrocele is rare.
Brugian filariasis: Elephantiasis affects legs below the knees
and arms below elbows.