Biosafety Manual - Arizona State University
Transcript of Biosafety Manual - Arizona State University

ASU Biosafety Manual 1
Biosafety Manual
Arizona State University Department of Environmental Health & Safety
Last Updated: July 2012

ASU Biosafety Manual 2
F O R E W O R D
The Biosafety Manual has been adopted by Arizona State University to be a resource for information, guidelines,
policies, and procedures that will enable and encourage those working in the laboratory environment to work
safely and to eliminate, or reduce, the potential for exposure to biological hazards. The Department of Environmental Health and Safety has developed this manual to help ensure compliance with the following
federal, state, and local regulations:
7 Code of Federal Regulations § 331
9 Code of Federal Regulations § 121
18 United States Code § 175b
29 Code of Federal Regulations § 1910.1030
42 Code of Federal Regulations § 72
42 Code of Federal Regulations § 73
42 Code of Federal Regulations § 1003
49 Code of Federal Regulations, Parts 171-180
Arizona Administrative Code, Article 14, Biohazardous Medical Waste and Discarded Drugs
Centers for Disease Control & Prevention/National Institutes of Health. Biosafety in Microbiological and Biomedical Laboratories.
National Institutes of Health. Guidelines for Research Involving Recombinant DNA Molecules.
Public Act 107-188, HR3448
The Biosafety Manual provides a compilation of suggested work practices, protocols and systems to work safely
at Arizona State University. The Biosafety Manual should not be considered the only reference for health and safety concerns. It is intended that the Principal Investigator (PI) and supervisory personnel will supplement this
information with instruction and guidance regarding specific practices and procedures unique to the work being done in their laboratories. In addition, the Department of Environmental Health and Safety is always available to
address health and safety concerns.
The Biosafety Manual will be reviewed at least annually by the Department of Environmental Health and Safety
and the Institutional Biosafety Committee.
July 19, 2012
Leon Igras, Director Date Environmental Health and Safety
July 19, 2012 David Gillum, Biosafety Officer Date
Environmental Health and Safety

ASU Biosafety Manual 3
Table of Contents
I. PREFACE ............................................................................................................................................ 6
II. INTRODUCTION ................................................................................................................................. 6
A. Scope ........................................................................................................................................... 6
B. Regulatory Requirements and Guidelines ........................................................................................ 6
C. Select Agents and Toxins ............................................................................................................... 7
D. Risk Group Classifications .............................................................................................................. 8
E. Laboratory Biosafety Levels ........................................................................................................... 8
F. Animal Biosafety Levels ............................................................................................................... 10
G. Biohazardous Waste .................................................................................................................... 12
H. Biohazardous Waste Handling ...................................................................................................... 12
I. Biological Safety Audits ............................................................................................................... 13
III. RESPONSIBILITIES ........................................................................................................................... 14
A. Arizona State University............................................................................................................... 14
B. Institutional Biosafety Committee ................................................................................................. 14
C. Department of Environmental Health & Safety/Biosafety Officer ..................................................... 15
D. Office of Research Integrity and Assurance ................................................................................... 16
E. Deans, Directors, and Chairs ........................................................................................................ 16
F. Responsible Official ..................................................................................................................... 16
G. Principal Investigator ................................................................................................................... 17
H. Laboratory Employees ................................................................................................................. 18
I. Institutional Animal Care and Use Committee ............................................................................... 18
J. Other Organizations .................................................................................................................... 19
K. Visitors, Vendors, and Contractors ............................................................................................... 19
IV. INCIDENT REPORTING ...................................................................................................................... 20
A. Reportable Incidents and Violations ............................................................................................. 20
B. Principal Investigator Responsibilities ........................................................................................... 20
C. Biosafety Officer Responsibilities .................................................................................................. 20
D. Institutional Responsibilities ......................................................................................................... 20
E. Institutional Official Responsibilities .............................................................................................. 21
V. BIOHAZARDOUS RESEARCH PROJECT REGISTRATION AND APPROVAL ............................................... 22
A. Introduction................................................................................................................................ 22
B. Registration and Approval Process ............................................................................................... 22
C. Additional Information and Requirements ..................................................................................... 23
1. Select Agents and Toxins ....................................................................................................... 23
2. Human Blood and Tissue ....................................................................................................... 23

ASU Biosafety Manual 4
3. Animal Handling .................................................................................................................... 23
4. Recombinant DNA Materials ................................................................................................... 24
5. Environmental Samples ......................................................................................................... 24
6. Protective Clothing Beyond the Laboratory ............................................................................. 24
7. Food and Beverages in the Laboratory ................................................................................... 25
VI. TRAINING FOR WORKING SAFELY WITH BIOHAZARDOUS AGENTS ..................................................... 26
VII. LABORATORY PROCEDURES AND EQUIPMENT ................................................................................... 27
A. Exposure Control ........................................................................................................................ 27
Laboratory Practice and Technique ........................................................................................ 27 1.
Safety Equipment (Primary Barriers) ...................................................................................... 27 2.
Facility Design (Secondary Barriers) ....................................................................................... 28 3.
B. Biological Safety Cabinets (BSCs) ................................................................................................. 28
VIII. GUIDELINES FOR GOOD LABORATORY PRACTICES ............................................................................ 31
A. Guidelines for Good Laboratory Practices at BSL-1 ........................................................................ 31
1. Standard Microbiological Practices .......................................................................................... 31
2. Special Practices ................................................................................................................... 32
3. Safety Equipment (Primary Barriers and Personal Protective Equipment) .................................. 32
4. Laboratory Facilities (Secondary Barriers) ............................................................................... 32
B. Guidelines for Good Laboratory Practices at BSL-2 ........................................................................ 33
1. Standard Microbiological Practices .......................................................................................... 33
2. Special Practices ................................................................................................................... 34
3. Safety Equipment (Primary Barriers and Personal Protective Equipment) .................................. 35
4. Laboratory Facilities (Secondary Barriers) ............................................................................... 36
C. Guidelines for Good Laboratory Practices at BSL-3 ........................................................................ 36
1. Standard Microbiological Practices .......................................................................................... 37
2. Special Practices ................................................................................................................... 38
3. Safety Equipment (Primary Barriers and Personal Protective Equipment) .................................. 39
4. Laboratory Facilities (Secondary Barriers) ............................................................................... 39
IX. EMERGENCY RESPONSE PROCEDURES .............................................................................................. 42
A. Decontamination ......................................................................................................................... 42
B. Exposure to Biohazards ............................................................................................................... 43
C. Spills of Biohazards ..................................................................................................................... 44
D. Spills Inside a Biological Safety Cabinet (BSC) ............................................................................... 44
E. Small Spill of Material Outside of a BSC ........................................................................................ 45
F. Large Spill of Biohazardous Material (>500 ml) Outside of a BSC ................................................... 45
G. Small Spill (<500 ml) of Recombinant DNA Materials ..................................................................... 45
H. Large Spill (>500 ml) of Recombinant DNA Materials in a BSC ....................................................... 45

ASU Biosafety Manual 5
I. Large Spill (>500 ml) of Recombinant DNA Materials outside of a BSC ........................................... 46
J. Spill of Recombinant DNA Materials in a Centrifuge ....................................................................... 47
K. Reporting Exposures ................................................................................................................... 47
X. TRANSFERS, PACKAGING, AND SHIPPING OF BIOLOGICAL MATERIALS ............................................... 48
A. Transfers .................................................................................................................................... 48
B. Packaging ................................................................................................................................... 48
C. Packaging with Dry Ice ................................................................................................................ 50
D. Labeling ..................................................................................................................................... 50
E. Shipping and Transportation Methods and Requirements ............................................................... 50
F. Other Permits ............................................................................................................................. 52
XI. SECURITY ........................................................................................................................................ 53
XII. COMPLIANCE .................................................................................................................................... 54
XIII. RECORDKEEPING .............................................................................................................................. 55
XIV. PROGRAM EVALUATION .................................................................................................................... 56
Appendix A: Definitions ............................................................................................................... 60
Appendix B: Lab-Specific Biosafety Manual Template .................................................................... 61
Appendix B-1: Floor Diagram ....................................................................................................... 73
Appendix B-2: Health Hazard Assessment Worksheet .................................................................... 74
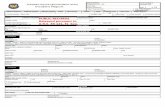
Appendix B-3: IBC Application Documentation .............................................................................. 82
Appendix B-4: Suggested Format for the Lab-Specific Biosafety Manual ......................................... 83
Appendix C: Special Considerations for Select Agents and Toxins ................................................... 84

ASU Biosafety Manual 6
I. PREFACE
The Arizona State University (ASU) Biosafety Manual is intended to be a resource for information,
guidelines, policies, and procedures that will enable and encourage those working in the laboratory environment to work safely and to eliminate, or reduce, the potential for exposure to biological hazards.
The information presented here also reflects the requirements and guidelines of federal and state
regulations. The most current version of the ASU Biosafety Manual is available on-line on the ASU Environmental Health & Safety (EH&S) website.
II. INTRODUCTION
A. Scope
The ASU Biosafety Manual is applicable to all laboratory, research, teaching, service, and support activities that may involve exposure to biohazards. Biohazards are microorganisms, microbial
toxins, or other biological agents that can infect and/or cause disease in humans, animals, or plants. Biohazards may include bacteria, bacterial toxins, viruses, fungi, rickettsia, prions,
protozoans, parasites, genetically-modified organisms, or recombinant DNA molecules. In
addition, biohazards include human blood, body fluid, tissues, and cell lines of human origin. Biohazards are often referred to as infectious agents or etiological agents.
Biosafety encompasses the knowledge, techniques, equipment, and facilities necessary to
prevent or minimize an exposure to, or release of, a biological agent. The mission of the Biosafety Division in the ASU Department of Environmental Health and Safety is to assure a safe
and healthy environment for individuals working with biohazards and to protect the community
and environment by preventing the release and exposure to biohazards.
B. Regulatory Requirements and Guidelines
Guidance documents from the National Institutes of Health (NIH) and the Centers for Disease
Control and Prevention (CDC) form the basis for the biosafety practices included in this manual. There are additional guidance documents and regulations imposed by various funding agencies
that individual PIs must be aware of and incorporate into their Lab-Specific Biosafety Manuals. Biosafety requirements must be followed to ensure the continuation of grant funding
from federal agencies and for health and safety purposes.
The NIH Guidelines for Research Involving Recombinant DNA Molecules (NIH Guidelines) detail
procedures and practices for the containment and safe conduct of various forms of recombinant DNA research, including research involving genetically modified plants and animals, as well as
human gene transfer. The NIH Guidelines:
Mandate the establishment of an Institutional Biosafety Committee for the review and
oversight of biological research;
Outline roles and responsibilities for biosafety; and
Establish the practices, procedures, and conditions under which recombinant DNA
activities must be conducted.
All institutions, including ASU, receiving NIH funding for recombinant DNA activities must comply with the NIH Guidelines. Researchers at institutions that are subject to the NIH Guidelines must
comply with the requirements even if their individual projects are not funded by NIH. Non-
compliance with the NIH Guidelines may result in suspension, limitation, or termination of financial assistance for the research project and of NIH funds for other
recombinant DNA activities at ASU or the requirement for prior NIH approval of any and/or all recombinant DNA projects at ASU.

ASU Biosafety Manual 7
The CDC/NIH manual, Biosafety in Microbiological and Biomedical Laboratories (BMBL), describes
the appropriate measures and facilities for work with all microbial agents, including bacterial, viral, fungal, parasitic, rickettsial, and prion agents as well as toxins of biological origin.
The requirements described in the Occupational Safety and Health Administration’s (OSHA)
Bloodborne Pathogens regulation (29 CFR § 1910.1030) apply to work with human blood, tissue,
organs, body fluids, and cell cultures. Special training, medical surveillance, procedures, and equipment that must be in place for protection against bloodborne pathogens, needlesticks, and
other sharps injuries, are described in the ASU Exposure Control Plan.
Handling and disposal of biohazardous waste is regulated by OSHA under the Bloodborne Pathogens regulation and by state and federal statutes. The procedures for biohazardous waste
handling are described in the ASU Biological Waste Handling Procedures.
The requirements for packaging and shipment of biohazardous materials are provided in the
Department of Transportation’s hazardous materials regulation 49 CFR, Parts 171 – 180. In addition, permits may be required to ship biological materials. Please refer to the CDC Etiological
Agent Import Permit Program and the Animal and Plant Health Inspection Service (APHIS) permit
program. Information on shipping procedures that comply with these regulations is found in the section on “Shipping and Transportation Methods and Requirements” in this manual.
Specific requirements for handling toxins found in 29 CFR § 1910.1450 Occupational Exposure to
Hazardous Chemicals in Laboratories are covered in the ASU Chemical Hygiene Plan. Information on ASU’s radiation safety program is found in the Radioactive Materials Manual.
C. Select Agents and Toxins
Select agents are particular microorganisms and toxins specifically identified in federal
regulations. Select agents also include specific genetically modified microorganisms or genetic elements that contain specific nucleic acid sequences. The most current list is found on the CDC’s
website at http://www.selectagents.gov/.
The following toxins are not regulated as select agents or toxins if the amount under the control
of a principal investigator, treating physician or veterinarian, or commercial manufacturer or distributor does not exceed, at any time, the amounts indicated in the table below.
HHS Select Agent Toxins CAS # Threshold Amount
Abrin 1393-62-0 100 mg
Botulinum neurotoxins 93384-43-1 0.5 mg
Clostridium perfringens epsilon toxin 100 mg
Conotoxin 76862-65-2 / 156467-85-5 100 mg
Diacetoxyscirpenol (DAS) 2270-40-8 1000 mg
Ricin 96638-28-7 100 mg
Saxitoxin 35523-89-8 100 mg
Shiga-like ribosome inactivating proteins 100 mg
Shigatoxin 75757-64-1 100 mg
Staphylococcal enterotoxins 11100-45-1 5 mg
T-2 toxin 21259-20-1 1000 mg
Tetrodotoxin 4368-28-9 100 mg

ASU Biosafety Manual 8
The ASU Biosafety Manual, when used in combination with the Lab-Specific Biosafety
Manual, is designed to meet the federal requirements of the Department of Health and Human Services (HHS) Standard “Possession, Use, and Transfer of Select Agents and Toxins; Final Rule“
(42 CFR § 73) and the Department of Agriculture (USDA) Standard, “Agricultural Bioterrorism Protection Act of 2002; Possession, Use, and Transfer of Biological Agents and Toxins; Final Rule“
(7 CFR § 331 and 9 CFR § 121). All laboratory specific requirements for these regulations can be
found in the appendix titled “Special Considerations for Select Agents and Toxins.”
D. Risk Group Classifications
According to the CDC/NIH document, Biosafety in Microbiological and Biomedical Laboratories, also known as the BMBL, the three primary hazardous characteristics associated with biological
agents include:
The capability of an agent to infect and cause disease in a susceptible human or animal
host;
The virulence of an agent as measured by the severity of disease; and
The availability of preventive measures and effective treatments for the disease.
By taking the route of transmission of the disease into consideration, a standardized methodology
was developed to classify biological agents into four different risk groups (please see the table
below). Knowing the risk group of an agent assists researchers and safety professionals in determining the appropriate safety protocols to be followed.
Risk Group (RG) Classifications
RG-1 RG-2 RG-3 RG-4
Agents that are not associated with disease
in healthy adult humans.
Agents that are associated with human disease which is rarely serious and for which
preventive or therapeutic
interventions are often available.
Agents that are associated with serious or lethal human disease for which preventive or
therapeutic interventions may be
available (high individual risk but low
community risk).
Agents that are likely to cause serious or lethal
human disease for which preventive or
therapeutic interventions are not usually available (high individual risk and high
community risk).
E. Laboratory Biosafety Levels
CDC and NIH have established four levels of biosafety, based on the degree of hazard associated with a microbial agent, to describe the combination of laboratory practices and techniques, safety
equipment, and facilities needed to protect against exposure. The BMBL outlines four different biological safety levels that are appropriate for the operations performed in a laboratory, the
documented or suspected routes of transmission of the biological agent, and the laboratory
function or activity. These four biosafety levels (BSL) require successively more stringent practices and facilities as work moves from the least restrictive, BSL-1, to work with the highest
hazard level of BSL-4. Exposure to biohazardous agents may be prevented or limited by establishing and following the appropriate biosafety level practices and conditions. The
requirements for each laboratory biosafety level can be found in the BMBL.
The following bullets provide a brief summary of the four biological safety levels:
BSL-1 is required for work involving well-characterized agents not known to consistently
cause disease in immunocompetent adult humans, and present minimal potential hazard
to laboratory personnel and the environment.

ASU Biosafety Manual 9
BSL-2 is required for work involving agents that pose moderate hazards to personnel
and the environment.
BSL-3 is required for clinical, diagnostic, teaching, research, or production facilities
where work is performed with indigenous or exotic agents that may cause serious or potentially lethal disease through the inhalation route of exposure.
BSL-4 is required for work with dangerous and exotic agents that pose a high individual
risk of aerosol-transmitted laboratory infections and life-threatening disease that is frequently fatal, for which there are no vaccines or treatments, or a related agent with
unknown risk of transmission.
Note: No research with biohazardous agents at BSL-4 is permitted in Arizona State University
facilities.
Personal protective equipment varies depending upon the biological safety level. Please refer to the table below for specific requirements for each of the four biological safety levels.
Biological Safety - Personal Protective Equipment (PPE) Requirements*
BSL-1 BSL-2 BSL-3 BSL-4
Protective laboratory coats, gowns, or uniforms recommended preventing contamination of personal clothing.
Protective eyewear worn when conducting procedures that have the potential to create splashes of microorganisms or other hazardous materials.
Personnel who wear contact lenses in laboratories should also wear eye protection.
Gloves must be worn to protect hands from exposure to hazardous materials.
Protective laboratory coats, gowns, smocks, or uniforms must be worn while working with hazardous materials.
Eye and face protection (goggles, mask, face shield or other splatter guard) must be used for anticipated splashes or sprays of infectious or other hazardous materials when the microorganisms are handled outside the Biological Safety Cabinet (BSC) or physical containment device.
Personnel who wear contact lenses in laboratories should also wear eye protection.
Gloves must be worn to protect hands from exposure to hazardous materials.
Eye, face and respiratory protection should be used in rooms containing infected animals.
Protective laboratory clothing with a solid-front, such as tie-back or wrap-around gowns, scrub suits, or coveralls must be worn.
Eye and face protection (goggles, mask, face shield or other splash guard) must be used for anticipated splashes or sprays of infectious or other hazardous materials. [All procedures involving the manipulation of infectious materials must be conducted within a BSC, or other physical containment devices.]
Personnel who wear contact lenses in laboratories must also wear eye protection.
Gloves must be worn to protect hands from exposure to hazardous materials.
Eye, face, and respiratory protection must be used in rooms containing infected animals.
Not permitted at ASU.
Please refer to the CDC/NIH document, “Biosafety in Microbiological and Biomedical Laboratories” for PPE requirements.
* Safety is improved when PPE is used in combination with physical containment devices or equipment, such as Biological Safety Cabinets (BSCs).

ASU Biosafety Manual 10
F. Animal Biosafety Levels
Similar to the BSL, there are four animal biosafety levels (ABSL). These four animal biosafety
levels are required for the use of experimentally-infected animals housed in indoor research facilities (e.g., vivaria), and also in the maintenance of laboratory animals that may naturally
harbor zoonotic infectious agents. As a general principle, the biosafety level (facilities,
practices, and operational requirements) recommended for working with infectious agents in vivo and in vitro are comparable with the animal biosafety level.
The four animal biosafety levels provide increasing levels of protection to personnel and to the
environment, and are recommended as minimal standards for activities involving infected laboratory animals. The four ABSLs describe animal facilities and practices applicable to work
with animals infected with agents assigned to Biosafety Levels 1-4, respectively. Investigators
that are inexperienced in conducting these types of experiments should seek help in designing their experiments from individuals who are experienced in this special
work.
The following bullets provide a brief summary of the four biological safety levels:
ABSL-1 is required for work in animals involving well-characterized agents that are not
known to cause disease in immunocompetent adult humans, and present minimal
potential hazard to personnel and the environment. ABSL-2 is suitable for work involving laboratory animals infected with agents associated
with human disease and pose moderate hazards to personnel and the environment, and
also addresses hazards from ingestion as well as from percutaneous and mucous membrane exposure.
ABSL-3 is required for work with laboratory animals infected with indigenous or exotic
agents, agents that present a potential for aerosol transmission, and agents causing
serious or potentially lethal disease. ABSL-4 is required for work with animals infected with dangerous and exotic agents that
pose a high individual risk of aerosol-transmitted laboratory infections and life-
threatening disease that is frequently fatal, for which there are no vaccines or treatments; or a related agent with unknown risk of transmission.
Note: No research with biohazardous agents at BSL-4 is permitted in Arizona State University facilities.
In addition to animal biosafety consideration, laboratory animal facilities, operational practices,
and quality of animal care must meet applicable standards and regulations (e.g., Guide for the Care and Use of Laboratory Animals and Laboratory Animal Welfare Regulations) and that
appropriate species have been selected for animal experiments. The USDA has also developed
facility parameters and work practices for handling agents of agriculture significance.
Personal protective equipment varies depending upon the biological safety level. Please refer to the following table for specific requirements for each of the four biological safety levels.

ASU Biosafety Manual 11
Animal Biological Safety - Personal Protective Equipment (PPE) Requirements*
ABSL-1 ABSL-2 ABSL-3 ABSL-4
Protective laboratory coats, gowns, or uniforms recommended to prevent contamination of personal clothing.
Eye, face, and respiratory protection should be used in rooms containing infected animals.
Protective eyewear must be worn when conducting procedures that have the potential to create splashes of microorganisms or other hazardous materials.
Personnel who wear contact lenses should also wear eye protection when entering areas with potentially high concentrations or airborne particulates.
Gloves must be worn to prevent skin contact with contaminated, infectious, and hazardous materials, and when handling animals.
Protective laboratory coats, gowns, or uniforms must be worn while in areas where infectious materials and/or animals are housed or manipulated.
Eye and face protection (mask, goggles, face shield or other splatter guard) must be worn when performing manipulations or activities that may result in splashes or sprays from infectious or other hazardous materials and when the animal or microorganisms must be handled outside the BSC or physical containment device.
Personnel who wear contact lenses should also wear eye protection when entering areas with potentially high concentrations or airborne particulates.
Gloves must be worn to prevent skin contact with contaminated, infectious and hazardous materials and when handling animals.
Eye, face, and respiratory protection should be used in rooms containing infected animals.
Disposable personal protective equipment, such as non-woven olefin cover-all suits, wrap-around or solid-front gowns, should be worn (over uniforms or scrub suits) before entering areas where infectious materials and/or animals are housed or manipulated. Front-button laboratory coats are unsuitable.
Eye, face, and respiratory protection must be used in rooms containing infectious materials and in areas where animals are housed or manipulated. [All procedures involving the manipulation of infectious materials must be conducted within a BSC, or other physical containment devices.]
Personnel who wear contact lenses in laboratories must also wear eye protection.
Gloves must be worn to prevent skin contact with contaminated, infectious, and hazardous materials and when handling animals. Double-glove practices should be used.
Boots, shoe covers, or other protective footwear, are used to prevent cross-contamination.
Not permitted at ASU.
Please refer to the CDC/NIH document, “Biosafety in Microbiological and Biomedical Laboratories” for PPE requirements.
* Safety is improved when PPE is used in combination with physical containment devices or equipment, such as Biological Safety Cabinets (BSCs).
It is the responsibility of institutional management to provide facilities, staff, and established practices that reasonably ensure appropriate levels of environmental quality, safety, security and
care for the laboratory animal. There are unique hazards associated with infected animals that must be understood by personnel with animal contact. Animal activity may create aerosols, and
bites and scratches can occur.

ASU Biosafety Manual 12
G. Biohazardous Waste
According to the State of Arizona, biohazardous waste is defined as:
1) Any solid waste which is generated in the diagnosis, treatment, or immunization of a
human being or animal or in any research relating to that diagnosis, treatment, or
immunization, or in the production or testing of biological materials. 2) Animal carcasses, body parts, and bedding of animals that have been infected with
agents that produce, or may produce, human infection. 3) Discarded cultures and stocks generated in the diagnosis, treatment, or immunization of
a human being or animal or in any research relating to that diagnosis, treatment or
immunization, or in the production or testing of biological. 4) Discarded products and materials containing blood or blood components.
5) Discarded organs and body parts removed during surgery. 6) Discarded sharps used in animal or human patient care, medical research, or clinical
laboratories. Examples of sharps include:
Hypodermic needles;
Syringes;
Pipettes;
Pipette tips;
Scalpel blades;
Blood vials;
Needles attached to tubing;
Broken and unbroken glassware;
Slides; and
Coverslips.
As a best management practice, EH&S manages discarded preparations made from genetically altered living organisms and their products as biohazardous waste. For example, recombinant
DNA waste materials used in research laboratories is considered biohazardous waste.
H. Biohazardous Waste Handling
Wastes associated with biological research materials must be disposed of in special ways. Examples of potentially hazardous items include:
All sharps (e.g., glass implements, needles, syringes, blades, coming from facilities using
infectious materials).
Biologically-cultured stocks and plates.
Agents (of any biosafety level) containing recombinant DNA.
Human blood, tissues, organs, and cell lines.
Transgenic plants and animals.
Any regulated biohazardous material.
In order for the biological waste to be removed by EH&S, the following procedures must be
followed:
Biological wastes derived from human sources (e.g., blood, body fluids, tissues, tumors,
human cell lines) are hazardous biological wastes and should be placed in a red or
orange biohazard bag. Autoclave the bag under appropriate time and temperature and place it in a red drum for removal by hazardous waste personnel.
BSL-1 materials containing recombinant DNA must be autoclaved or the DNA must be
denatured with bleach.

ASU Biosafety Manual 13
Bacteria, viruses, or other microorganisms that are known human pathogens should also
be put into a red or orange bag, autoclaved, and placed in a red drum for removal by
hazardous waste personnel. Sharps and sharp objects such as glass, syringes, disposable pipettes, and pipette tips
that may be contaminated with biological waste (human or non-human) or pathogenic
material should be placed in a rigid, leak-proof, puncture-resistant container. The container is autoclaved and then placed in a red drum for removal by hazardous waste
personnel.
Non-human biological wastes are handled by the same methods as human biological wastes: placed in autoclave bags, autoclaved, and put into red drums for removal by
hazardous waste personnel.
When your “red-bag,” “yellow drum,” or liquid hazardous waste is ready for removal, call
Environmental Management at (480) 965-3899 to arrange a pick-up, or submit a hazardous
waste pick-up request. If you need any other assistance or have questions, please feel free to contact Environmental Health & Safety at (480) 965-1823.
There are additional requirements for disposing of select agents and toxins. Please see the
appendix titled “Special Considerations for Select Agents and Toxins.”
I. Biological Safety Audits
EH&S audits laboratories at least once a year. The safety audit typically includes an evaluation of the autoclave, biological safety cabinet, microbiological techniques, emergency and safety
equipment, storage of biohazardous material, general housekeeping, and review of the Lab-
Specific Biosafety Manual. Please refer to the ASU Biosafety & Biosecurity inspection checklists for more information about the biosafety audit form used by EH&S.
EH&S will make every attempt to schedule laboratory audits with faculty members. However, if
the principal investigator is unavailable or is unresponsive, EH&S will proceed with the safety
audit. EH&S may also conduct unannounced accident investigations. Please be aware that federal, state, and local inspectors may also conduct unannounced inspections.
Following the biological safety survey, a report listing the safety concerns is sent to the faculty
member responsible for the laboratory. The faculty member is responsible for correcting the
hazards. If the faculty member fails to correct the hazard, a second notice is sent to the department head with a copy to the faculty member. Follow-up audits may be conducted in
laboratories with extremely hazardous conditions and/or numerous violations.

ASU Biosafety Manual 14
III. RESPONSIBILITIES
The biological safety program at ASU developed from the University’s commitment to address and comply
with the NIH Guidelines regarding safe research with recombinant DNA and associated biohazardous materials as well as the HHS and USDA regulations on select agents and toxins. The Institutional
Biosafety Committee (IBC) and the department of Environmental Health & Safety (EH&S) provide
oversight of ASU’s biological safety program. The roles and responsibilities of ASU faculty and staff are described in this section.
A. Arizona State University
ASU has instituted and maintains a biosafety program for personnel who may be exposed to
biological hazards (biohazards) during the performance of their duties. The biosafety program is
designed to achieve regulatory compliance and to provide a means for employees to be informed about and protected from biohazards. To maintain regulatory compliance and to protect
personnel from biohazards, Arizona State University must:
Appoint a Biological Safety Officer (BSO) for the institution.
Ensure appropriate training is provided to personnel conducting research with biohazardous or recombinant DNA materials.
Ensure that research conforms to the provisions of the NIH Guidelines. Establish an Institutional Biosafety Committee with adequate expertise and training.
Establish and maintain a health surveillance program for personnel. Implement policies for safe conduct of biological and recombinant DNA research.
Report any significant problems, violations or significant research-related accidents or
illnesses to the NIH OBA within 30 days.
B. Institutional Biosafety Committee
The Institutional Biosafety Committee (IBC) shall be constituted of a minimum of five (5) voting
members. Collectively, the membership shall have experience and expertise in recombinant DNA technology and the capability to assess the safety of recombinant DNA research and identify any
potential risks to public health or the environment. The IBC shall include at least one individual with expertise in plant, plant pathogen, or plant pest containment principles and one scientist
with expertise in animal containment principles. At least two members shall not be affiliated with
the institution (apart from their membership on the committee) and shall represent the interest of the surrounding community with respect to public health and protection of the environment.
The Biological Safety Officer (BSO) for the campus must be a voting member of the IBC. A quorum will consist of a simple majority. A passing vote will be a simple majority of members
present; minority views will be recorded in the minutes. The committee’s current membership may be obtained by contacting ORIA at http://researchintegrity.asu.edu/.
The responsibilities of the Institutional Biosafety Committee (IBC) include, but are not limited to, the following:
Address biosafety issues related to experimentally infected laboratory animals.
Adopt policies supporting the safe use of biological materials and the elimination or
reduction of exposure to potentially biohazardous materials and agents. Assess the facilities, procedures, practices, training and expertise of personnel involved in
research utilizing recombinant DNA and/or biohazardous materials. Determine necessity of health surveillance of personnel.
Direct development of appropriate procedures to oversee the possession and/or use of recombinant DNA and biohazardous materials.
Ensure training for IBC members, staff, Principal Investigators, and laboratory staff.
Facilitate the registration of biological research by providing materials and information to Principal Investigators.

ASU Biosafety Manual 15
Make a final determination of physical and biological containment for recombinant DNA
and biohazardous materials, and modify containment levels as necessary. Notify the Principal Investigator of the results of the IBC’s review, approval, or
disapproval. Obtain specific review, registration and/or approval from NIH/OBA for research that falls
under Sections III-A, III-B, III-C and Appendix M of the NIH Guidelines. Review and report any significant problems, violations of the NIH Guidelines and any
significant research-related accidents or illnesses to the Institutional Official and to the
appropriate authorities. Review, approve and oversee research utilizing recombinant DNA and biohazardous
materials, conducted at or sponsored by the University, for adherence with the NIH Guidelines, the BMBL, and University policies. This pertains to the initial and continuing
reviews and modifications to the currently approved research.
Review and approve research involving the use of select agents and toxins. Review research involving recombinant DNA and other potentially biohazardous agents.
Set biosafety containment levels as required by the NIH Guidelines. Suspend or terminate disclosure approval for the possession or use of recombinant DNA
and biohazardous materials, where the IBC finds non-compliance or that such use or
possession poses undue risk to research personnel or a threat to the health and safety of the community.
Periodically review the IBC policies and procedures and modify them as necessary to ensure appropriate biosafety measures and adherence with federal and state
requirements. Review research disclosures that include the possession and/or use of recombinant DNA
and biohazardous materials for compliance with NIH Guidelines. As part of the review
process, the IBC will do the following:
o Conduct an independent assessment of the containment levels (i.e., BSL-1, BSL-2, BSL-3) in collaboration with EH&S, as required by the NIH Guidelines.
o Conduct an assessment of the facilities, procedures, practices, training, and expertise
of personnel conducting research involving recombinant DNA and biohazardous materials.
o Ensure adherence with all surveillance, data reporting, and adverse event reporting requirements set forth in the NIH Guidelines for recombinant DNA.
Submit membership roster (completed by the ASU ORIA) including members’ biographical sketches to the NIH Office of Biotechnology Activities (OBA).
According to the NIH Guidelines, the IBC must review and approve architectural designs for new
facilities and renovations to existing facilities where recombinant DNA research may be performed. The IBC has delegated the authority to EH&S to review and approve these
documents on their behalf.
C. Department of Environmental Health & Safety/Biosafety Officer
The responsibilities of EH&S and the Biological Safety Officer (BSO) include, but are not limited
to, the following:
Advise researchers on proper waste disposal methods based on federal and state
regulations. Assist in the development of emergency plans for handling accidental spills and
personnel contamination. Consult with researchers on issues of biosafety and the safe use of biological materials in
the laboratory.
Investigate laboratory accidents involving recombinant DNA research. Develop protocols and procedures to address issues of biosafety.

ASU Biosafety Manual 16
Develop, implement, and maintain the university’s biosafety program.
Develop, implement, and maintain the university’s program for select agents and toxins. Perform periodic inspections to ensure that laboratory standards are rigorously followed.
Promote regulatory compliance and a safe laboratory environment. Provide advice on laboratory security.
Provide oversight of the ASU Bloodborne Pathogen Program and conduct training for
laboratory personnel with such exposure. Provide technical advice to Principal Investigators and the Institutional Biosafety
Committee on research safety procedures. Provide training in the safe use and practices for those working with potentially
biohazardous materials and activities. Report to the Institutional Biosafety Committee and the institution any significant
problems, violations of the NIH Guidelines, and any significant research-related accidents
or illnesses of which the Biological Safety Officer becomes aware unless the Biological Safety Officer determines that a report has already been filed by the Principal
Investigator. Work in conjunction with the IBC and the ORIA to review all registration forms for
research proposals submitted by Principal Investigators.
D. Office of Research Integrity and Assurance
Accepts all IBC forms from PIs for research involving any of the following: 1)
recombinant DNA, 2) biohazardous agents, and 3) select agents and toxins, and coordinates their review with the IBC and EH&S.
Reviews biological Material Transfer Agreements (MTA) and coordinates approval with
EH&S. Accepts research protocols involving the use of animals and coordinates review by the
Institutional Animal Care and Use Committee (IACUC). Accepts research protocols involving the use of human subjects and coordinates review
by the Institutional Review Board (IRB).
E. Deans, Directors, and Chairs
Ensure that registration forms are completed by each Principal Investigator conducting
research involving biohazardous materials (microorganisms, microbial toxins, or other
biological agents that can infect and/or cause disease in humans, animals, or plants), human blood, body fluid, tissues, and cell lines of human origin, genetically-modified
organisms, and recombinant DNA molecules.
F. Responsible Official
A Responsible Official (RO) is required under the HHS and USDA select agent regulations. This
individual’s responsibilities can be found in the applicable regulations. Although this list is not intended to be a complete list, critical responsibilities include:
Developing and implementing safety, security, and emergency response plans.
Allowing only approved individuals to have access to select agents or toxins.
Providing appropriate training for safety, security and emergency response. Transferring select agents or toxins only to registered individuals.
Providing immediate notice of any theft, loss, or release of a select agent or toxin. Providing proper laboratory facilities to contain and dispose of select agents and toxins.
Maintaining complete records relating to select agents as defined in 42 CFR 73.15. Reporting the identification of a select agent or toxin as a result of diagnosis, verification,
or proficiency testing.
Submitting changes in the registration information by promptly notifying the CDC or Animal and Plant Health Inspection (APHIS)/USDA in writing. This includes modifications

ASU Biosafety Manual 17
to the list of individuals that have been approved to work or access select agents,
changes in work locations, and changes in protocols or objectives of the studies. Conducting regular inspections, at least annually, of the laboratory where select agents
or toxins are stored or used to ensure compliance with all procedures and protocols of this safety plan. The results of these inspections must be documented and any
deficiencies must be corrected and documented.
The RO for Arizona State University is:
Leon C. Igras, Director, EH&S
The Alternate Responsible Officials (ARO) for Arizona State University is:
David Gillum, Associate Director of Biosafety/Biosecurity, EH&S
Steven Hunter, Associate Director, EH&S
Irene Mendoza, Assistant Biosafety Officer, EH&S
G. Principal Investigator
A scientist, trained and knowledgeable in appropriate laboratory techniques, safety procedures, and hazards associated with handling biohazardous agents must be responsible for the conduct
of work with any biohazardous agents or materials. This individual should consult with biosafety
or other health and safety professionals with regard to risk assessment. Responsibilities of the Principal Investigator (PI) include:
Accept direct responsibility for the health and safety of those working with biohazardous
materials and/or select agents and toxins in the laboratory. Adhere to IBC-approved emergency plans for handling accidental spills and personnel
contamination.
Be adequately trained in good microbiological techniques. Comply with shipping requirements for biohazardous.
Develop specific biosafety standard operating procedures for biohazardous materials used in the laboratory.
Ensure compliance by laboratory personnel with relevant regulations, guidelines, and
policies. Ensure personal protective equipment is provided and used.
Ensure proper training and instruction for laboratory personnel in safe practices and protocols, including, at a minimum, training in aseptic techniques and biology of the
organism(s) used. Please refer to the ASU Lab-Specific Biosafety Training Checklist. Ensure the integrity of the physical containment (e.g., biological safety cabinets) and the
biological containment (e.g., purity, genotypic and phenotypic characteristics) through
annual testing and certification. Inform the laboratory staff of the reasons and provisions for any precautionary medical
practices advised or requested (e.g., vaccinations or serum collection). Instruct and train laboratory staff in: (i) the practices and techniques required to ensure
safety, and (ii) the procedures for dealing with accidents.
Propose appropriate microbiological practices and laboratory techniques to be used for the research.
Provide to all laboratory staff the protocols that describe the potential biohazards and the precautions to be taken.
Remain in communication with the IBC throughout the conduct of the project.
Report any significant problems pertaining to the operation and implementation of containment practices and procedures in writing to the Biological Safety and other
authorities, as appropriate. Submit a disclosure to the Institutional Biosafety Committee (IBC) for review and
approval or disapproval.

ASU Biosafety Manual 18
Supervise laboratory staff to ensure that the required safety practices and techniques are
employed. Correct work errors and conditions that may result in accidents, injuries, or the release of biohazardous materials.
PIs are also responsible for full compliance with the NIH Guidelines during the conduct of
recombinant DNA research.
Determine whether the recombinant DNA research is subject to the NIH Guidelines. Develop specific biosafety standard operating procedures for recombinant DNA materials
used in the laboratory.
Obtain IBC approval before initiating recombinant DNA research subject to the NIH Guidelines.
Petition OBA, with notice to the IBC, for proposed exemptions from the NIH Guidelines. Propose physical and biological containment levels in accordance with the NIH Guidelines
when registering research with the IBC.
Report any significant problems, violations of the NIH Guidelines, or any significant research-related accidents and illnesses to the Biological Safety Officer,
Greenhouse/Animal Facility Director, Institutional Biosafety Committee, NIH/OBA, and
other authorities, as appropriate, within 30 days. Seek OBA approval, in addition to IBC approval, to conduct experiments specified in
Sections III-A and III-B of the NIH Guidelines. Seek the NIH Office of Biotechnology’s (OBA) determination of containment for
experiments that require a case-by-case review. Submit any subsequent changes (e.g., changes in the source of DNA or host-vector
system) to the disclosure to the IBC for review and approval or disapproval.
H. Laboratory Employees
Participate in appropriate training and instruction and ensure that they are adequately
trained and fully understand the instructions.
Fully comprehend all biological agents and select agents and toxins being used in the lab and the potential risks associated with exposure, as well as fully understanding the
associated emergency response procedures. Follow all laboratory practices and protocols and comply with all applicable policies,
procedures, and guidelines.
Complete any necessary medical surveillance. Report all thefts, security incidents, accidents, spills, or contamination incidents to
supervisor.
I. Institutional Animal Care and Use Committee
The Institutional Animal Care and Use Committee (IACUC) works in cooperation with the
Occupational Health Nurse, the Director of the Department of Animal Care and Technologies (DACT), and the University Veterinarian, to advise investigators and animal care personnel on the
potential biohazards and risk of physical injury associated with laboratory animals and on the procedures for reducing or eliminating exposure. It also ensures compliance with all applicable
regulations, policies, and procedures based on the Public Health Service Policy on Humane Care
and Use of Laboratory Animals.
DACT ensures that biosafety cabinets in animal facilities are certified as needed. DACT and the University Veterinarian provide training to all animal users in proper
methodology and safe animal handling. ORIA ensures that all employees receive appropriate training and maintains those records.

ASU Biosafety Manual 19
J. Other Organizations
Other committees, including the Human Subjects Committee, Radiation Safety Committee, and
the Department of Public Safety must:
Consult and coordinate with the IBC and EH&S on any proposals under their purview
which involve the use of potentially biohazardous materials or activities.
K. Visitors, Vendors, and Contractors
All visitors, vendors, and contractors must:
Comply with all security requirements and procedures.
Be accompanied by a Department of Justice approved person at all times while in areas with select agents or toxins; and
Use personal protective equipment provided for them by the laboratory.
NOTE: Contractors must ensure that appropriate personal protective equipment is available
for their own workers.

ASU Biosafety Manual 20
IV. INCIDENT REPORTING
A. Reportable Incidents and Violations
Incidents or problems involving recombinant DNA and/or biohazardous materials must be immediately reported to the Biological Safety Officer (BSO). Examples of reportable significant
incidents include but are not limited to any overt exposure, such as a needle stick, splash, and
contamination due to equipment failure, and any potential exposure to biohazardous materials. A significant event may also occur from a containment breach, which may be subsequently
determined to pose either an overt or potential exposure to individuals. It should be noted that waste from recombinant DNA research is considered biohazardous and incidents involving
improper disposal of recombinant DNA must also be reported. Questions regarding reportable incidents should be directed to the BSO.
Failure by research personnel to follow federal and institutional regulations, guidelines, policies and/or procedures may also require reporting to the appropriate institutional, local, state and/or
federal agencies. Violations may include but are not limited to conduct of new or ongoing research without appropriate federal or institutional registration, review, approval or oversight.
B. Principal Investigator Responsibilities
The Principal Investigator and their personnel must report any significant incident, violation of the NIH Guidelines, or any significant, research-related accidents and illnesses immediately by
contacting the BSO. Examples of incidents and violations include:
Overt exposures, which are defined as exposures that result in direct personnel exposure
to biohazardous materials such as injection, spills, splashes or aerosol inhalation.
Potential exposures, which are defined as exposures that have a high risk of exposing
personnel to biohazardous materials such as spills, containment failure while working with the agent or equipment failure that may produce aerosols.
Any exposure (overt or potential) in a BSL-3 laboratory.
Overt exposure in BSL-1 or BSL-2 laboratories.
Any illness that may be caused by the agents used in the laboratory.
Any incident involving the improper disposal of recombinant DNA.
C. Biosafety Officer Responsibilities
The Biological Safety Officer (BSO) is required, by the NIH Guidelines, to report to the IBC:
• All violations of the NIH Guidelines and significant incidents. • Any significant research-related accidents or illnesses.
D. Institutional Responsibilities
The IBC is required, by the NIH Guidelines, to report to the appropriate University official and to
the NIH/OBA within 30 days any significant incidents, violations of the NIH Guidelines, or any significant research-related accidents and illnesses. The IBC will be responsible to determine
what actions, if any, are necessary. For example the IBC may choose to change the frequency of lab inspections, or change the biosafety level of the disclosure, based on results of the incident.
Other IBC reporting requirements (to OBA and other agencies) include but are not limited to:
• Research involving recombinant DNA or biohazardous materials without prior IBC approval.
• Lax security, unsafe procedures used in a laboratory setting, improper disposal of recombinant waste.

ASU Biosafety Manual 21
• Significant changes to proposed research risk without prior notification and approval by
IBC.
Some incidents must be reported to OBA on an expedited basis. Spills or accidents in BSL-2 laboratories (involving recombinant DNA) resulting in an overt exposure must be immediately
reported to OBA. In addition, spills or accidents involving recombinant DNA occurring in high
containment (BSL-3 or higher) laboratories resulting in an overt or potential exposure must be immediately reported to OBA. The IBC will report to the appropriate institutional official, who, in
turn will report to OBA, any of the above-described incidents.
Institutional violations that will be reported to the appropriate college or department head may include but are not limited to:
• Lapses in disclosure approval. • Failure to comply with institutional and federal regulations, guidelines, and policies.
• Unsafe work practices.
E. Institutional Official Responsibilities
Upon receiving a report from the IBC, the Institutional Official (IO) will directly report:
• In writing any problems with or violations (non-compliance) of the NIH Guidelines, or any
significant incident, accidents, or illnesses related to recombinant DNA, to the NIH/OBA within 30 days or immediately for overt exposure to a BSL-2 agent or potential/overt
exposure to a BSL-3 agent.
• Any significant research-related illness or accident that may be hazardous to the public health and cooperate with state and local public health departments.

ASU Biosafety Manual 22
V. BIOHAZARDOUS RESEARCH PROJECT REGISTRATION AND APPROVAL
A. Introduction
Each PI is responsible for the preparation of registration documents for all research involving
potentially biohazardous materials, including the assignment of the required Biological Safety
Level (BSL) to the proposed biological research. Biological research includes research involving:
Bacterial, viral, fungal, parasitic, or other potentially infectious agents. Recombinant DNA, including experiments that may be exempt under the NIH Guidelines. Human blood, body fluid, and tissue, including human cell lines. Listed select agents and toxins.
The IBC, in conjunction with EH&S, will review all submitted registration documents; confirm, where applicable, that exempt status is appropriate for certain recombinant DNA work; and
consider approval for those registration documents that are complete and that provide for safe handling of potentially biohazardous materials under the appropriate BSL.
B. Registration and Approval Process
Additional requirements referred to in the registration documents for research involving select agents or toxins, infectious materials, or human blood or tissue (as outlined below) will need to
be fulfilled for final approval to be given.
If the project involves or may involve recombinant DNA; infectious agents (other
than select agents and toxins); human blood, tissue or cell cultures; or other biosafety concerns, the following steps must occur:
1. The Office of Research Integrity and Assurance (ORIA) or the Biosafety Officer distributes
registration forms and the ASU Biosafety Manual to anyone requesting them and to other
researchers who may work with recombinant DNA, infectious agents, human samples, or other biosafety concerns.
2. The Principal Investigator (PI) or researcher reviews the ASU Biosafety Manual and, if
applicable, completes Form 112 for recombinant DNA, infectious agents, human blood, and
tissue or cell culture. The PI may contact ORIA or the Biosafety Officer in EH&S to discuss the project or for guidance in completing the forms. In addition, to assist the PI in
determining the appropriate biosafety level for the proposed research, the PI is directed to the Agent Summary Statements in the BMBL and Appendix B, Classification of Human
Etiologic Agents on the Basis of Hazard in the NIH Guidelines.
3. The PI submits the completed application and necessary attachments to ORIA.
4. ORIA reviews the submitted application for completeness and may contact the PI for
additional information.
5. The Biosafety Officer and members of the Institutional Biosafety Committee review the
completed application to determine whether the project meets federal and university standards.
6. At its monthly meeting, the IBC discusses the proposed project and votes to approve the
research as presented, to approve it with stipulations, or to table it for further information.
7. If the project is approved, the Chair of the IBC signs the application. ORIA retains all
administrative records.

ASU Biosafety Manual 23
8. ORIA, on behalf of the IBC, will notify the PI of the status of the application, including any
stipulations or comments for resolution.
Additional Notes:
A “Continuing Review to Original 112AB Disclosure” Form 112AR is available to facilitate
the annual renewal process.
If the research involves any listed select agents or toxins, the PI must submit Form 112C
as an initial starting point.
Copies of the 112 application forms can be downloaded from the ORIA website at
http://researchintegrity.asu.edu/biosafety/forms or can be obtained the Biosafety Officer
through EH&S.
C. Additional Information and Requirements
1. Select Agents and Toxins
All personnel at Arizona State University are prohibited from possessing, using, receiving, or transferring listed select agents or toxins unless ASU has been granted a certificate of
registration by the HHS Secretary or the USDA Secretary. Additional requirement for
Select Agents and Toxins are found in the appendix titled “Special Considerations for Select Agents and Toxins.”
2. Human Blood and Tissue
In any laboratory where work involves the use of and/or exposure to human blood, body
fluids, or unfixed human tissue, including human cell cultures, there is the danger of
exposure to bloodborne pathogens (disease-causing microorganisms) that may be found in such material. Work with any of these materials in a laboratory setting must follow
ASU procedures as described in the ASU Exposure Control Plan.
In addition, when human blood or tissue donors are involved, the PI must contact ORIA
to determine whether a human subject Institutional Review Board (IRB) application is required. The IRB Coordinator may be contacted in ORIA.
3. Animal Handling
When research involves exposure to and handling of animals, consideration must be
given to the potential allergens, animal pathogens, zoonoses, and physical hazards, e.g.,
bites and scratches that may be encountered by researchers and staff. All research involving the use of animals conducted under the auspices of ASU is reviewed by the
Institutional Animal Care and Use Committee (IACUC), in compliance with federal regulations. Projects involving animal research require that applications be submitted to
the IACUC for protocol approval before research begins.
Principal Investigators and all personnel involved in the care and use of research animals
must obtain certification in the ASU's Humane Practice of Animal Care and Use Training Program. All of these requirements must be fulfilled prior to the acquisition and use of
laboratory animals, including medical review with the Occupational Health Nurse at ASU
Campus Health Services.

ASU Biosafety Manual 24
4. Recombinant DNA Materials
The use of recombinant DNA is regulated by the NIH, as outlined in the NIH Guildelines. At ASU this research must be reviewed by the IBC prior to initiation of the work. Guidelines include registration of the recombinant DNA, understanding the classification
of the use of recombinant DNA, and safe work practices/proper disposal of material
(including whole animals) containing recombinant DNA. The use of more than 10 liters of recombinant material requires special practices.
5. Environmental Samples
Environmental samples, such as water, air, or earth, may contain pathogens (i.e., bacteria, viruses, spores) that could present a health hazard to people, animals, or the
environment. Using appropriate personal protective equipment when collecting environmental samples will reduce exposure to potential pathogens. Use care when
handling environmental samples, especially if the sample will be enhanced in the laboratory by culturing or other growing mechanisms. Techniques used to enhance
and/or culture environmental samples should be conducted at BSL-2 or higher levels in
an appropriate containment device, such as a biological safety cabinet or fume hood. If the environmental sample is sterilized prior to experimentation, then the sample may be
manipulated in a BSL-1 rated laboratory.
Research involving environmental samples must be registered with the ASU Institutional
Biosafety Committee (IBC) for approval. If you require assistance determining whether you need to register this research with the IBC, please contact the Biological Safety
Officer.
6. Protective Clothing Beyond the Laboratory
The improper use or lack of protective clothing and equipment in a laboratory can lead to
chemical burns, biological exposures, or other potential dangers. To help reduce the risk of exposure, personnel in ASU laboratories are required to wear gloves, safety glasses,
lab coats and other personal protective clothing. However, in public areas, such as hallways and lounges, wearing personal protective clothing and equipment is not
recommended. This is because contaminated clothing may present a hazard, and the
perception of contaminated protective clothing and equipment in a public area may project a careless image to both colleagues and visitors.
Wearing gloves outside the laboratory should be minimized, except to move hazardous
materials between laboratories. Chemicals should be transported from place to place on
a cart, in a clean secondary container, or in a bottle carrier with secure handles. When this is not an option, personnel should use a clean, ungloved hand to touch common
surfaces and a gloved hand to carry the items: the one-glove rule. Alternatively, the material should be packaged so the outer container may be transported without the need
for personal protective equipment.
Protective gloves should never come into contact with door handles, elevator buttons,
telephones, lavatory faucets, vending machines, bottled water dispensers, ice-making machines, or other surfaces outside the laboratory. Also, please be aware that strict
federal and state regulations address the transport of hazardous (i.e., biological, chemical, radiological) materials on public roads.
For the sake of safety, appearances, and courtesy, personnel are asked not to wear contaminated, stained, or potentially contaminated lab coats and other research clothing
and equipment in any public area, especially dining areas, lounges, auditoriums, conference rooms, or other non-hazardous areas.

ASU Biosafety Manual 25
7. Food and Beverages in the Laboratory
In order to reduce potential exposures and to ensure compliance with prudent laboratory
operations, regulations, and other best management practices, ASU prohibits the storage and consumption of food and drink in all campus laboratories. The only exception is for
food and beverages used in research and teaching projects. These materials must be
labeled, “Not for Human Consumption.”
In order to prevent potential exposure to hazardous materials:
Do not eat, drink, smoke, chew gum, apply cosmetics, or take medicine in
laboratories where hazardous materials are handled or stored. Do not store food, beverages, cups, or other drinking and eating utensils in areas
where hazardous materials are handled or stored.
Do not use glassware for laboratory operations to prepare or consume food or
beverages.
Do not use laboratory refrigerators, ice chests, cold rooms, and ovens for food
storage or preparation. Do not use laboratory water sources or deionized laboratory water for drinking
water.
Important: Food and beverages must never be stored in any laboratory refrigerator in
which chemicals, biological, and radioactive materials are kept unless they have been
labeled, “Not for Human Consumption.

ASU Biosafety Manual 26
VI. TRAINING FOR WORKING SAFELY WITH BIOHAZARDOUS AGENTS
The PI or laboratory supervisor is responsible for providing or arranging for site-specific training of all
personnel. In addition, each employee must attend Biosafety Training and Laboratory Chemical Safety Training. Contact EH&S or the Biosafety Officer for more information on scheduling training. Training
must be documented. Please refer to the ASU Laboratory-Specific Training Checklist for more
information.

ASU Biosafety Manual 27
VII. LABORATORY PROCEDURES AND EQUIPMENT
A. Exposure Control
The term “containment” is used in describing safe methods for managing biohazardous and
select agents and toxins in the laboratory environment where they are being handled or
maintained. The purpose of containment is to reduce or eliminate exposure of laboratory workers, other people, and the outside environment to potentially hazardous agents. The three
elements of containment include laboratory practices and techniques, safety equipment, and facility design. The risk assessment of the work to be done with a specific agent will determine
the appropriate combination of these elements. Each PI is required to complete a Health Hazard Assessment for each biological agent and toxin stored in his or her laboratory (see Appendix B of
this manual). Copies of the Health Hazard Assessments must be included in the PI’s Lab-Specific
Biosafety Manual.
Laboratory Practice and Technique 1.
The most important element of containment is strict adherence to standard
microbiological practices and techniques. Persons working with infectious agents or infected materials must be aware of potential hazards and must be trained and proficient
in the practices and techniques required for handling such material safely. The PI of each laboratory is responsible for providing or arranging the appropriate training of personnel
and for verifying each person’s competence. In addition, each PI must develop a Lab-Specific Biosafety Manual to address the use, handling, and disposal of biohazardous
material (including select agents and toxins) in the laboratory. The Lab-Specific Biosafety
Manual must identify specific hazards that will or may be encountered and consider procedures needed to minimize or eliminate risks. Personnel should be advised of special
hazards and are expected to follow the required practices and procedures. A template for the Lab-Specific Biosafety Manual may be found in Appendix B of this manual.
Safety Equipment (Primary Barriers) 2.
Safety equipment includes biological safety cabinets (BSC), enclosed biohazardous containers, and other engineering controls designed to eliminate or minimize exposures
to biohazardous agents and toxins. The biological safety cabinet is the principal device
used to provide containment of infectious splashes or aerosols generated by many microbiological procedures. More information on BSCs may be found in the “Biological Safety Cabinet” section of this manual.
Primary safety barriers may also include personal protection equipment (PPE) such as
gloves, lab coats, safety glasses or goggles, face shields and respirators. Personal protective equipment is often used in combination with BSCs and other containment
devices. In some situations in which it is impractical to work in a BSC, personal protective equipment may form the primary barrier between the worker and the infectious
materials. ASU policy requires the use of gloves, lab coat and eye protection at all times when handling biohazardous materials.

ASU Biosafety Manual 28
Facility Design (Secondary Barriers) 3.
The design of a facility is important in providing a barrier to protect those working inside
and outside the laboratory and to protect people or animals in the community from biohazardous agents and toxins which may be accidentally released from the laboratory.
Facilities must be commensurate with the laboratory's function and the recommended
biosafety level for the agent being manipulated.
The secondary barriers required will depend on the risk of transmission of specific agents. For example, in working with agents at Biosafety Level 2, the exposure risks
involve direct contact with the agents or inadvertent contact through contaminated work environments. Recommended secondary barriers in these laboratories include separation
of the laboratory work area from public access, handwashing facilities, and availability of
a decontamination facility such as an autoclave.
When the risk of infection by exposure to an infectious aerosol is present, higher levels of primary containment and multiple secondary barriers may become necessary to prevent
infectious agents from escaping into the environment. Such design features include
specialized ventilation systems to ensure directional airflow, HEPA filtration to remove agents from exhaust air, controlled access zones, airlocks as laboratory entrances, or
separate modules to isolate the laboratory.
B. Biological Safety Cabinets (BSCs)
BSCs are classified as Class I, Class II, or Class III cabinets. When properly maintained and
operated, they effectively contain and capture microbial contaminants and infectious agents using HEPA (High Efficiency Particulate Air) filters (See Figure 1. Source: Biosafety in
Microbiological and Biomedical Laboratories 5th Edition, Appendix A). Biosafety cabinets should
not be confused with clean benches which only protect the material being worked with and are not suitable for work with infectious or toxic material. (Although clean benches, like BSCs, have
HEPA-filtered air, in clean benches the air flows over the experimental material toward the user rather than being drawn away.) BSCs should also not be confused with conventional fume hoods
that do not filter microorganisms.

ASU Biosafety Manual 29
Types of BSCs:
Class I BSCs provide personnel and environmental protection, but not product protection (See Figure 2. Source: Biosafety in Microbiological and Biomedical Laboratories 5th Edition, Appendix A).
Class II BSCs are the most commonly used BSC at ASU for biohazardous agents. These
cabinets provide personnel, environmental, and product protection (See Figure 3. Source: Biosafety in Microbiological and Biomedical Laboratories 5th Edition, Appendix A). Only those
which are hard ducted to the outside and provide a face velocity of 80 to 125 feet per minute should be used when working with volatile chemicals. Additionally, cabinets are not designed to
prevent ignition of volatile flammable chemicals, such as ethanol and isopropanol.

ASU Biosafety Manual 30
Guidelines for Working in a BSC
1. Turn off the ultraviolet lamp if one is in use. Turn on the fluorescent lamp. 2. Inspect the air intake grilles for obstructions and foreign material and remove if necessary.
3. Adjust view screen to proper height.
4. Turn the cabinet on for at least 10 minutes prior to use, if the cabinet is not left running. 5. Prepare a written checklist of materials necessary for the particular activity.
6. Wash hands and arms with mild soap. Put on a rear-fastening, long-sleeved gown with tight-fitting cuffs. Put on safety glasses and a pair (or two pairs) of high quality nitrile gloves.
7. Disinfect work surface with a suitable disinfectant. 8. Place items into the cabinet so that they can be worked with efficiently without unnecessary
disruption of the airflow, working with materials from the clean to the dirty side.
9. Adjust the working height of the stool so that the worker's face is above the front opening. 10. Delay manipulation of materials for approximately one minute after placing hands/arms
inside the cabinet. 11. Minimize the frequency of moving hands in and out of the cabinet.
12. Do not disturb the airflow by covering any portion of the grillwork with materials.
13. Work at a moderate pace to prevent the air flow disruption that occurs with rapid movements.
14. Wipe the bottom and side of the hood surfaces with disinfectant when work is completed.
NOTE: Be very careful when using small pieces of materials such as chemwipes in the hood. These can be blown into the hood and disrupt the motor operations.
Certification of the BSC
Certification is a series of performance tests on the BSC to confirm that it will provide the user and experimental material the protection for which it is designed. The airflow, filters, and cabinet
integrity are checked to ensure that the cabinet meets minimum performance standards.
Certification is arranged through each department and provided by an outside vendor.
BSCs intended for research with biohazardous materials must be certified:
After they are received and installed (before use with infectious materials).
After filter changes.
After being moved (even a few feet).
Annually.
BSC decontamination (using the formaldehyde gas production process) must be provided (e.g.,
by an outside vendor) and needs to be done:
Before any maintenance work requiring disassembly of the air plenum, including filter
replacement.
Prior to cabinet recertification.
Before moving the cabinet to a new laboratory.
Before discarding or salvaging.
The production of formaldehyde gas is a health concern. Many BSCs at ASU are not ducted to the
outside; therefore, extreme caution should be used when having the procedure performed.

ASU Biosafety Manual 31
VIII. GUIDELINES FOR GOOD LABORATORY PRACTICES
A. Guidelines for Good Laboratory Practices at BSL-1
BSL-1 is suitable for work involving well-characterized agents not known to consistently cause
disease in immunocompetent adult humans, and present minimal potential hazard to laboratory personnel and the environment. BSL-1 laboratories are not necessarily separated from the
general traffic patterns in the building. Work is typically conducted on open bench tops using standard microbiological practices. Special containment equipment or facility design is not
required, but may be used as determined by appropriate risk assessment. Laboratory personnel
must have specific training in the procedures conducted in the laboratory and must be supervised by a scientist with training in microbiology or a related science.
The following standard practices, safety equipment, and facility requirements apply to BSL-1:
1. Standard Microbiological Practices
a) The laboratory supervisor must enforce the institutional policies that control
access to the laboratory. b) Persons must wash their hands after working with potentially hazardous
materials and before leaving the laboratory.
c) Eating, drinking, smoking, handling contact lenses, applying cosmetics, and storing food for human consumption must not be permitted in laboratory areas.
Food must be stored outside the laboratory area in cabinets or refrigerators designated and used for this purpose.
d) Mouth pipetting is prohibited; mechanical pipetting devices must be used. e) Policies for the safe handling of sharps, such as needles, scalpels, pipettes, and
broken glassware must be developed and implemented. Whenever practical,
laboratory supervisors should adopt improved engineering and work practice controls that reduce risk of sharps injuries.
Precautions, including those listed below, must always be taken with sharp
items. These include:
i. Careful management of needles and other sharps are of primary
importance. Needles must not be bent, sheared, broken, recapped, removed from disposable syringes, or otherwise manipulated by hand
before disposal. ii. Used disposable needles and syringes must be carefully placed in
conveniently located puncture-resistant containers used for sharps
disposal. iii. Non disposable sharps must be placed in a hard walled container for
transport to a processing area for decontamination, preferably by autoclaving.
iv. Broken glassware must not be handled directly. Instead, it must be
removed using a brush and dustpan, tongs, or forceps. Plasticware should be substituted for glassware whenever possible.
f) Perform all procedures to minimize the creation of splashes and/or aerosols.
g) Decontaminate work surfaces after completion of work and after any spill or
splash of potentially infectious material with appropriate disinfectant. h) Decontaminate all cultures, stocks, and other potentially infectious materials
before disposal using an effective method. Depending on where the decontamination will be performed, the following methods should be used prior
to transport:

ASU Biosafety Manual 32
i. Materials to be decontaminated outside of the immediate laboratory
must be placed in a durable, leak proof container and secured for transport
ii. Materials to be removed from the facility for decontamination must be packed in accordance with applicable local, state, and federal
regulations.
i) A sign incorporating the universal biohazard symbol must be posted at the
entrance to the laboratory when infectious agents are present. The sign may include the name of the agent(s) in use, and the name and phone number of the
laboratory supervisor or other responsible personnel. Agent information should be posted in accordance with the institutional policy.
j)
k) An effective integrated pest management program is required. l) The laboratory supervisor must ensure that laboratory personnel receive
appropriate training regarding their duties, the necessary precautions to prevent exposures, and exposure evaluation procedures. Personnel must receive annual
updates or additional training when procedural or policy changes occur. Personal
health status may impact an individual’s susceptibility to infection, ability to receive immunizations or prophylactic interventions. Therefore, all laboratory
personnel and particularly women of child-bearing age should be provided with information regarding immune competence and conditions that may predispose
them to infection. Individuals having these conditions should be encouraged to self-identify to the institution’s healthcare provider for appropriate counseling
and guidance.
2. Special Practices
None required.
3. Safety Equipment (Primary Barriers and Personal Protective Equipment)
a) Special containment devices or equipment, such as BSCs, are not generally
required. b) Protective laboratory coats, gowns, or uniforms are recommended to prevent
contamination of personal clothing. c) Wear protective eyewear when conducting procedures that have the potential to
create splashes of microorganisms or other hazardous materials. Persons who
wear contact lenses in laboratories should also wear eye protection. d) Gloves must be worn to protect hands from exposure to hazardous materials
Glove selection should be based on an appropriate risk assessment. e) Alternatives to latex gloves should be available. Wash hands prior to leaving the
laboratory. In addition, BSL-1 workers should:
i. Change gloves when contaminated, integrity has been compromised, or
when otherwise necessary. ii. Remove gloves and wash hands when work with hazardous materials
has been completed and before leaving the laboratory.
iii. Do not wash or reuse disposable gloves. Dispose of used gloves with other contaminated laboratory waste. Hand washing protocols must be
rigorously followed.
4. Laboratory Facilities (Secondary Barriers)
a) Laboratories should have doors for access control.
b) Laboratories must have a sink for hand washing.

ASU Biosafety Manual 33
c) The laboratory should be designed so that it can be easily cleaned. Carpets and
rugs in laboratories are not appropriate. d) Laboratory furniture must be capable of supporting anticipated loads and uses
Spaces between benches, cabinets, and equipment should be accessible for cleaning.
i. Bench tops must be impervious to water and resistant to heat, organic solvents, acids, alkalis, and other chemicals.
ii. Chairs used in laboratory work must be covered with a non-porous material that can be easily cleaned and decontaminated with appropriate
disinfectant. iii. Laboratories windows that open to the exterior should be fitted with
screens.
B. Guidelines for Good Laboratory Practices at BSL-2
BSL-2 builds upon BSL-1 practices. BSL-2 is suitable for work involving agents that pose
moderate hazards to personnel and the environment. It differs from BSL-1 in that 1) laboratory
personnel have specific training in handling pathogenic agents and are supervised by scientists competent in handling infectious agents and associated procedures; 2) access to the laboratory is
restricted when work is being conducted; and 3) all procedures in which infectious aerosols or splashes may be created are conducted in BSCs or other physical containment equipment.
The following standard and special practices, safety equipment, and facility requirements apply to
BSL-2:
1. Standard Microbiological Practices
a) The laboratory supervisor must enforce the institutional policies that control
access to the laboratory.
b) Persons must wash their hands after working with potentially hazardous materials and before leaving the laboratory.
c) Eating, drinking, smoking, handling contact lenses, applying cosmetics, and storing food for human consumption must not be permitted in laboratory areas.
Food must be stored outside the laboratory area in cabinets or refrigerators
designated and used for this purpose. d) Mouth pipetting is prohibited; mechanical pipetting devices must be used.
e) Policies for the safe handling of sharps, such as needles, scalpels, pipettes, and broken glassware must be developed and implemented. Whenever practical,
laboratory supervisors should adopt improved engineering and work practice controls that reduce risk of sharps injuries.
Precautions, including those listed below, must always be taken with sharp items. These include:
i. Careful management of needles and other sharps are of primary
importance. Needles must not be bent, sheared, broken, recapped,
removed from disposable syringes, or otherwise manipulated by hand before disposal.
ii. Used disposable needles and syringes must be carefully placed in conveniently located puncture-resistant containers used for sharps
disposal. iii. Non-disposable sharps must be placed in a hard walled container for
transport to a processing area for decontamination, preferably by
autoclaving.

ASU Biosafety Manual 34
iv. Broken glassware must not be handled directly. Instead, it must be
removed using a brush and dustpan, tongs, or forceps. Plasticware should be substituted for glassware whenever possible.
f) Perform all procedures to minimize the creation of splashes and/or aerosols.
g) Decontaminate work surfaces after completion of work and after any spill or
splash of potentially infectious material with appropriate disinfectant. h) Decontaminate all cultures, stocks, and other potentially infectious materials
before disposal using an effective method. Depending on where the decontamination will be performed, the following methods should be used prior
to transport:
i. Materials to be decontaminated outside of the immediate laboratory
must be placed in a durable, leak proof container and secured for transport.
ii. Materials to be removed from the facility for decontamination must be packed in accordance with applicable local, state, and federal
regulations.
i) A sign incorporating the universal biohazard symbol must be posted at the
entrance to the laboratory when infectious agents are present. Posted information must include: the laboratory’s biosafety level, the supervisor’s name
(or other responsible personnel), telephone number, and required procedures for entering and exiting the laboratory. Agent information should be posted in
accordance with the institutional policy.
j) An effective integrated pest management program is required. k) The laboratory supervisor must ensure that laboratory personnel receive
appropriate training regarding their duties, the necessary precautions to prevent exposures, and exposure evaluation procedures. Personnel must receive annual
updates or additional training when procedural or policy changes occur. Personal
health status may impact an individual’s susceptibility to infection, ability to receive immunizations or prophylactic interventions. Therefore, all laboratory
personnel and particularly women of child-bearing age should be provided with information regarding immune competence and conditions that may predispose
them to infection. Individuals having these conditions should be encouraged to
self-identify to the institution’s healthcare provider for appropriate counseling and guidance.
2. Special Practices
a) All persons entering the laboratory must be advised of the potential hazards and meet specific entry/exit requirements.
b) Laboratory personnel must be provided medical surveillance and offered
appropriate immunizations for agents handled or potentially present in the laboratory.
c) Each institution must establish policies and procedures describing the collection and storage of serum samples from at-risk personnel.
d) A Lab-Specific Biosafety Manual must be prepared and adopted as policy. The
biosafety manual must be available and accessible. e) The laboratory supervisor must ensure that laboratory personnel demonstrate
proficiency in standard and special microbiological practices before working with BSL-2 agents.
f) Potentially infectious materials must be placed in a durable, leak proof container during collection, handling, processing, storage, or transport within a facility.
g) Laboratory equipment should be routinely decontaminated, as well as, after
spills, splashes, or other potential contamination.

ASU Biosafety Manual 35
i. Spills involving infectious materials must be contained, decontaminated, and cleaned up by staff properly trained and equipped to work with
infectious material. ii. Equipment must be decontaminated before repair, maintenance, or
removal from the laboratory.
h) Incidents that may result in exposure to infectious materials must be
immediately evaluated and treated according to procedures described in the laboratory biosafety safety manual. All such incidents must be reported to the
laboratory supervisor. Medical evaluation, surveillance, and treatment should be provided and appropriate records maintained.
i) Animals and plants not associated with the work being performed must not be
permitted in the laboratory. j) All procedures involving the manipulation of infectious materials that may
generate an aerosol should be conducted within a BSC or other physical containment devices.
3. Safety Equipment (Primary Barriers and Personal Protective Equipment)
a) Properly maintained BSCs (preferably Class II), other appropriate personal protective equipment, or other physical containment devices must be used
whenever:
i. Procedures with a potential for creating infectious aerosols or splashes
are conducted. These may include pipetting, centrifuging, grinding, blending, shaking, mixing, sonicating, opening containers of infectious
materials, inoculating animals intranasally, and harvesting infected tissues from animals or eggs.
ii. High concentrations or large volumes of infectious agents are used. Such
materials may be centrifuged in the open laboratory using sealed rotor heads or centrifuge safety cups.
b) Protective laboratory coats, gowns, smocks, or uniforms designated for
laboratory use must be worn while working with hazardous materials. Remove
protective clothing before leaving for non-laboratory areas (e.g., cafeteria, library, administrative offices). Dispose of protective clothing appropriately, or
deposit it for laundering by the institution. It is recommended that laboratory clothing not be taken home.
c) Eye and face protection (goggles, mask, face shield or other splatter guard) is used for anticipated splashes or sprays of infectious or other hazardous
materials when the microorganisms must be handled outside the BSC or
containment device. Eye and face protection must be disposed of with other contaminated laboratory waste or decontaminated before reuse. Persons who
wear contact lenses in laboratories should also wear eye protection. d) Gloves must be worn to protect hands from exposure to hazardous materials.
Glove selection should be based on an appropriate risk assessment. Alternatives
to latex gloves should be available. Gloves must not be worn outside the laboratory. In addition, BSL-2 laboratory workers should:
a. Change gloves when contaminated, integrity has been compromised, or
when otherwise necessary. Wear two pairs of gloves when appropriate. b. Remove gloves and wash hands when work with hazardous materials
has been completed and before leaving the laboratory.

ASU Biosafety Manual 36
c. Do not wash or reuse disposable gloves. Dispose of used gloves with
other contaminated laboratory waste. Hand washing protocols must be rigorously followed.
e) Eye, face and respiratory protection should be used in rooms containing
infected animals as determined by the risk assessment.
4. Laboratory Facilities (Secondary Barriers)
a) Laboratory doors should be self-closing and have locks in accordance with the
institutional policies. b) Laboratories must have a sink for hand washing. The sink may be manually,
hands-free, or automatically operated. It should be located near the exit door.]
c) The laboratory should be designed so that it can be easily cleaned and decontaminated. Carpets and rugs in laboratories are not permitted.
d) Laboratory furniture must be capable of supporting anticipated loads and uses. Spaces between benches, cabinets, and equipment should be accessible for
cleaning.
i. Bench tops must be impervious to water and resistant to heat, organic
solvents, acids, alkalis, and other chemicals. ii. Chairs used in laboratory work must be covered with a non-porous
material that can be easily cleaned and decontaminated with appropriate disinfectant.
e) Laboratory windows that open to the exterior are not recommended. However, if a laboratory does have windows that open to the exterior, they must be fitted
with screens. f) BSCs must be installed so that fluctuations of the room air supply and exhaust do
not interfere with proper operations. BSCs should be located away from doors,
windows that can be opened, heavily traveled laboratory areas, and other possible airflow disruptions.
g) Vacuum lines should be protected with High Efficiency Particulate Air (HEPA) filters, or their equivalent. Filters must be replaced as needed. Liquid disinfectant
traps may be required.
h) An eyewash station must be readily available. i) There are no specific requirements on ventilation systems. However, planning of
new facilities should consider mechanical ventilation systems that provide an inward flow of air without recirculation to spaces outside of the laboratory.
j) HEPA filtered exhaust air from a Class II BSC can be safely re-circulated back into the laboratory environment if the cabinet is tested and certified at least
annually and operated according to manufacturer’s recommendations. BSCs can
also be connected to the laboratory exhaust system by either a thimble (canopy) connection or a direct (hard) connection. Provisions to assure proper safety
cabinet performance and air system operation must be verified. k) A method for decontaminating all laboratory wastes should be available in the
facility (e.g., autoclave, chemical disinfection, incineration, or other validated
decontamination method).
C. Guidelines for Good Laboratory Practices at BSL-3
BSL-3 is applicable to clinical, diagnostic, teaching, research, or production facilities where work
is performed with indigenous or exotic agents that may cause serious or potentially lethal disease through inhalation route exposure. Laboratory personnel must receive specific training in
handling pathogenic and potentially lethal agents, and must be supervised by scientists competent in handling infectious agents and associated procedures.

ASU Biosafety Manual 37
All procedures involving the manipulation of infectious materials must be conducted within BSCs, other physical containment devices, or by personnel wearing appropriate personal protective
equipment. A BSL-3 laboratory has special engineering and design features.
The following standard and special safety practices, equipment, and facility requirements apply to
BSL-3:
1. Standard Microbiological Practices
a) The laboratory supervisor must enforce the institutional policies that control access to the laboratory.
b) Persons must wash their hands after working with potentially hazardous
materials and before leaving the laboratory. c) Eating, drinking, smoking, handling contact lenses, applying cosmetics, and
storing food for human consumption must not be permitted in laboratory areas. Food must be stored outside the laboratory area in cabinets or refrigerators
designated and used for this purpose.
d) Mouth pipetting is prohibited; mechanical pipetting devices must be used. e) Policies for the safe handling of sharps, such as needles, scalpels, pipettes, and
broken glassware must be developed and implemented. Whenever practical, laboratory supervisors should adopt improved engineering and work practice
controls that reduce risk of sharps injuries.
Precautions, including those listed below, must always be taken with sharp
items. These include:
i. Careful management of needles and other sharps are of primary importance. Needles must not be bent, sheared, broken, recapped,
removed from disposable syringes, or otherwise manipulated by hand
before disposal. ii. Used disposable needles and syringes must be carefully placed in
conveniently located puncture-resistant containers used for sharps disposal.
iii. Non-disposable sharps must be placed in a hard walled container for
transport to a processing area for decontamination, preferably by autoclaving.
iv. Broken glassware must not be handled directly. Instead, it must be removed using a brush and dustpan, tongs, or forceps. Plasticware
should be substituted for glassware whenever possible.
f) Perform all procedures to minimize the creation of splashes and/or aerosols.
g) Decontaminate work surfaces after completion of work and after any spill or splash of potentially infectious material with appropriate disinfectant.
h) Decontaminate all cultures, stocks, and other potentially infectious materials before disposal using an effective method. A method for decontaminating all
laboratory wastes should be available in the facility, preferably within the
laboratory (e.g., autoclave, chemical disinfection, incineration, or other validated decontamination method). Depending on where the decontamination will be
performed, the following methods should be used prior to transport:
i. Materials to be decontaminated outside of the immediate laboratory must be placed in a durable, leak proof container and secured for
transport.

ASU Biosafety Manual 38
ii. Materials to be removed from the facility for decontamination must be
packed in accordance with applicable local, state, and federal regulations.
i) A sign incorporating the universal biohazard symbol must be posted at the
entrance to the laboratory when infectious agents are present. Posted
information must include the laboratory’s biosafety level, the supervisor’s name (or other responsible personnel), telephone number, and required procedures for
entering and exiting the laboratory. Agent information should be posted in accordance with the institutional policy.
j) An effective integrated pest management program is required. k) The laboratory supervisor must ensure that laboratory personnel receive
appropriate training regarding their duties, the necessary precautions to prevent
exposures, and exposure evaluation procedures. Personnel must receive annual updates or additional training when procedural or policy changes occur. Personal
health status may impact an individual’s susceptibility to infection, ability to receive immunizations or prophylactic interventions. Therefore, all laboratory
personnel and particularly women of child-bearing age should be provided with
information regarding immune competence and conditions that may predispose them to infection. Individuals having these conditions should be encouraged to
self-identify to the institution’s healthcare provider for appropriate counseling and guidance.
2. Special Practices
a) All persons entering the laboratory must be advised of the potential hazards and
meet specific entry/exit requirements.
b) Laboratory personnel must be provided medical surveillance and offered
appropriate immunizations for agents handled or potentially present in the laboratory.
c) Each institution must establish policies and procedures describing the collection and storage of serum samples from at-risk personnel.
d) A Lab-Specific Biosafety Manual must be prepared and adopted as policy. The biosafety manual must be available and accessible.
e) The laboratory supervisor must ensure that laboratory personnel demonstrate
proficiency in standard and special microbiological practices before working with BSL-3 agents.
f) Potentially infectious materials must be placed in a durable, leak proof container during collection, handling, processing, storage, or transport within a facility.
g) Laboratory equipment should be routinely decontaminated, as well as, after
spills, splashes, or other potential contamination.
i. Spills involving infectious materials must be contained, decontaminated, and cleaned up by staff properly trained and equipped to work with
infectious material. ii. Equipment must be decontaminated before repair, maintenance, or
removal from the laboratory.
h) Incidents that may result in exposure to infectious materials must be
immediately evaluated and treated according to procedures described in the laboratory biosafety safety manual. All such incidents must be reported to the
laboratory supervisor. Medical evaluation, surveillance, and treatment should be
provided and appropriate records maintained. i) Animals and plants not associated with the work being performed must not be
permitted in the laboratory.

ASU Biosafety Manual 39
j) All procedures involving the manipulation of infectious materials must be
conducted within a BSC, or other physical containment devices. No work with open vessels is conducted on the bench. When a procedure cannot be performed
within a BSC, a combination of personal protective equipment and other containment devices, such as a centrifuge safety cup or sealed rotor, must be
used.
3. Safety Equipment (Primary Barriers and Personal Protective Equipment)
a) All procedures involving the manipulation of infectious materials must be
conducted within a BSC (preferably Class II or Class III), or other physical containment devices.
b) Protective laboratory clothing with a solid-front such as tie-back or wraparound
gowns, scrub suits, or coveralls is worn by workers when in the laboratory. Protective clothing is not worn outside of the laboratory. Reusable clothing is
decontaminated with appropriate disinfectant before being laundered. Clothing is changed when contaminated.
c) Eye and face protection (goggles, mask, face shield or other splatter guard) is
used for anticipated splashes or sprays of infectious or other hazardous materials. Eye and face protection must be disposed of with other contaminated
laboratory waste or decontaminated before reuse. Persons who wear contact lenses in laboratories must also wear eye protection.
d) Gloves must be worn to protect hands from exposure to hazardous materials. Glove selection should be based on an appropriate risk assessment. Alternatives
to latex gloves should be available. Gloves must not be worn outside the
laboratory. In addition, BSL-3 laboratory workers should:
i. Change gloves when contaminated, integrity has been compromised, or when otherwise necessary. Wear two pairs of gloves when appropriate.
ii. Remove gloves and wash hands when work with hazardous materials
has been completed and before leaving the laboratory. iii. Do not wash or reuse disposable gloves. Dispose of used gloves with
other contaminated laboratory waste. Hand washing protocols must be rigorously followed.
e) Eye, face, and respiratory protection must be used in rooms containing infected animals.
4. Laboratory Facilities (Secondary Barriers)
a) Laboratory doors must be self-closing and have locks in accordance with the
institutional policies. The laboratory must be separated from areas that are open
to unrestricted traffic flow within the building. Access to the laboratory is restricted to entry by a series of two self-closing doors. A clothing change room
(anteroom) may be included in the passageway between the two self-closing doors.
b) Laboratories must have a sink for hand washing. The sink must be hands-free or
automatically operated. It should be located near the exit door. If the laboratory is segregated into different laboratories, a sink must also be available for hand
washing in each zone. Additional sinks may be required as determined by the risk assessment.
c) The laboratory must be designed so that it can be easily cleaned and decontaminated. Carpets and rugs are not permitted. Seams, floors, walls, and
ceiling surfaces should be sealed. Spaces around doors and ventilation openings
should be capable of being sealed to facilitate space decontamination.

ASU Biosafety Manual 40
i. Floors must be slip resistant, impervious to liquids, and resistant to
chemicals. Consideration should be given to the installation of seamless, sealed, resilient or poured floors, with integral cove bases.
ii. Walls should be constructed to produce a sealed smooth finish that can be easily cleaned and decontaminated.
iii. Ceilings should be constructed, sealed, and finished in the same general
manner as walls.
Decontamination of the entire laboratory should be considered when there has been gross contamination of the space, significant changes in laboratory usage,
for major renovations, or maintenance shut downs. Selection of the appropriate materials and methods used to decontaminate the laboratory must be based on
the risk assessment of the biological agents in use.
d) Laboratory furniture must be capable of supporting anticipated loads and uses.
Spaces between benches, cabinets, and equipment must be accessible for cleaning.
i. Bench tops must be impervious to water and resistant to heat, organic solvents, acids, alkalis, and other chemicals.
ii. Chairs used in laboratory work must be covered with a non-porous material that can be easily cleaned and decontaminated with appropriate
disinfectant.
e) All windows in the laboratory must be sealed.
f) BSCs must be installed so that fluctuations of the room air supply and exhaust do not interfere with proper operations. BSCs should be located away from doors,
heavily traveled laboratory areas, and other possible airflow disruptions. g) Vacuum lines must be protected with HEPA filters, or their equivalent. Filters
must be replaced as needed. Liquid disinfectant traps may be required.
h) An eyewash station must be readily available in the laboratory. i) A ducted air ventilation system is required. This system must provide sustained
directional airflow by drawing air into the laboratory from “clean” areas toward “potentially contaminated” areas. The laboratory shall be designed such that
under failure conditions the airflow will not be reversed.
i. Laboratory personnel must be able to verify directional air flow. A visual
monitoring device which confirms directional air flow must be provided at the laboratory entry. Audible alarms should be considered to notify
personnel of air flow disruption. ii. The laboratory exhaust air must not re-circulate to any other area of the
building.
iii. The laboratory building exhaust air should be dispersed away from occupied areas and from building air intake locations or the exhaust air
must be HEPA filtered.
j) HEPA filtered exhaust air from a Class II BSC can be safely re-circulated into the
laboratory environment if the cabinet is tested and certified at least annually and operated according to manufacturer’s recommendations. BSCs can also be
connected to the laboratory exhaust system by either a thimble (canopy) connection or a direct (hard) connection. Provisions to assure proper safety
cabinet performance and air system operation must be verified. BSCs should be certified at least annually to assure correct performance. Class III BSCs must be
directly (hard) connected up through the second exhaust HEPA filter of the
cabinet. Supply air must be provided in such a manner that prevents positive pressurization of the cabinet.

ASU Biosafety Manual 41
k) A method for decontaminating all laboratory wastes should be available in the
facility, preferably within the laboratory (e.g., autoclave, chemical disinfection, incineration, or other validated decontamination method).
l) Equipment that may produce infectious aerosols must be contained in devices that exhaust air through HEPA filtration or other equivalent technology before
being discharged into the laboratory. These HEPA filters should be tested and/or
replaced at least annually. m) Facility design consideration should be given to means of decontaminating large
pieces of equipment before removal from the laboratory. n) Enhanced environmental and personal protection may be required by the agent
summary statement, risk assessment, or applicable local, state, or federal regulations. These laboratory enhancements may include, for example, one or
more of the following; an anteroom for clean storage of equipment and supplies
with dress-in, shower-out capabilities; gas tight dampers to facilitate laboratory isolation; final HEPA filtration of the laboratory exhaust air; laboratory effluent
decontamination; and advanced access control devices such as biometrics. HEPA filter housings should have gas-tight isolation dampers; decontamination ports;
and/or bag-in/bag-out (with appropriate decontamination procedures) capability.
The HEPA filter housing should allow for leak testing of each filter and assembly. The filters and the housing should be certified at least annually.
o) The BSL-3 facility design, operational parameters, and procedures must be verified and documented prior to operation. Facilities must be re-verified and
documented at least annually.

ASU Biosafety Manual 42
IX. EMERGENCY RESPONSE PROCEDURES
ASU has a campus-wide emergency response plan, the ASU Emergency Operations Plan, which is
compliant with 29 CFR 1910.120. Protocols for handing biological emergencies are outlined in the plan. A summary of this plan can be found by reviewing the ASU Emergency Procedures Flipchart or the ASU
Police Department Policies and Procedures Manual.
Principal Investigators must be aware of the provisions for emergency procedures and preparedness.
Emergency procedures and preparedness must be incorporated into the Lab-Specific Biosafety Manual and used in the laboratory. Each laboratory should have a written emergency plan specifying the
appropriate response to potential emergencies. Accidents and spills of infectious materials will be discussed in Emergency Procedures below.
In addition, each PI will submit to EH&S the following:
A completed Responsible Party Information Sheet;
An annual chemical and biological inventory; and
A Health Hazard Assessment for each biological agent and toxin stored or used in the laboratory.
(See Appendix B of this manual.)
A. Decontamination
Decontamination is a process or treatment that renders an instrument or environmental surface
safe to handle. A decontamination procedure can be as simple as clean-up with detergent and water or as thorough as sterilization.
Sterilization is the use of physical or chemical processes to destroy all viable forms of
microbial life, such as bacterial spores.
Disinfection is a chemical or physical treatment that destroys the most resistant
vegetative microbes or viruses, but not the spores, in or on inanimate surfaces.
Effectiveness is influenced by a number of factors, including the type and number of organisms, amount of organic matter, the object being disinfected, the disinfectant being
used, concentration, temperature and exposure time. Antisepsis is the application of a liquid antimicrobial to skin or other living tissue to
inhibit or destroy microorganisms. Examples include handwashing with germicidal
solutions or swabbing skin with alcohol before an injection.
Sterilization, disinfection, and antisepsis are all forms of decontamination.
1. When to Decontaminate
All material and equipment contaminated with or containing potentially biohazardous
agents should be decontaminated:
Upon completion of procedures involving the use of biohazardous material;
In the event of spills of biohazardous materials;
Before being washed, stored, or discarded; and
At least daily.
In most ASU laboratories, it is recommended that decontamination be accomplished by steam heat sterilization in an autoclave or by surface application of or placement in a
chemical disinfectant solution, such as 1:10 bleach solution or its equivalent.

ASU Biosafety Manual 43
2. Autoclave Use
Autoclaving (saturated steam under pressure of approximately 15 pounds per square
inch (psi) to achieve a chamber temperature of at least 250˚F for a designated time) is the preferred and most convenient method to rapidly destroy all forms of microbial life.
However, to do this, the autoclave process must reach proper temperature, pressure,
and time, and also prevent the entrapment of air in the bag or container of treated material.
Material to be sterilized must come into contact with live steam.
Bags or containers should be left open during autoclaving or water (~200 ml)
should be added to sealed bags to generate steam.
Heat indicator tape should be used inside the bag or container with each
autoclave load to indicate that sterilization has been completed. Autoclave sterility monitoring should be conducted on a regular basis using
biological indicators (such as B. stearothermophilus spore strips) placed among
treated materials and at locations throughout the autoclave. The spores, which
are more resistant to heat than most other biological materials, provide validation of general microbial destruction when they are effectively inactivated
by autoclave operation (typically 250˚F for 30 minutes).
3. Chemical Disinfectant Use
The most practical use of chemical disinfectants is for surface decontamination and,
when used in sufficient concentration, as a decontaminant for liquid wastes prior to final disposal. General recommendations are:
Liquid Decontamination
Add liquid chlorine bleach to provide a final 1:10 dilution;
Let stand at least 20 minutes; and
Discard the solution appropriately.
Surface Decontamination
Wipe with 1:10 dilution of chlorine bleach; or
Wipe with iodophor disinfectant (per label concentration).
See Table 1, “Disinfectant Activity” at the end of this manual for further information on
disinfectants.
B. Exposure to Biohazards
In the event of an exposure to a biohazardous agent or material, the following guidelines should be used:
Intact Skin
1. Remove contaminated clothing. Clothing should not be pulled over the face as contact with eyes, nose, and mouth may occur. Shirts should be cut off.
2. Vigorously wash contaminated skin for 1 minute with soap and water.
3. Call 911 or seek medical attention at the ASU Health Services, if necessary. 4. Inform the laboratory’s PI and EH&S.

ASU Biosafety Manual 44
Broken, Cut or Damaged Skin or Puncture Wound
1. Remove contaminated clothing. Clothing should not be pulled over the face as contact
with eyes, nose, and mouth may occur. Shirts should be cut off. 2. Vigorously wash contaminated skin for 5 minutes with soap and water.
3. Call 911 or seek medical attention at the ASU Health Services, if necessary.
4. Inform the laboratory’s PI and EH&S.
Eye
1. Immediately flush eyes for at least 15 minutes with water, using an eyewash. Hold eyelids away from your eyeball and rotate your eyes so that all surfaces may be washed
thoroughly.
2. Remove contaminated clothing. Clothing should not be pulled over the face as contact with eyes, nose, and mouth may occur. Shirts should be cut off.
3. Call 911 or seek medical attention at the ASU Health Services, if necessary. 4. Inform the laboratory’s PI and EH&S.
Ingestion or Inhalation
1. Move to fresh air immediately. 2. Call 911 or seek medical attention at the ASU Health Services, if necessary.
3. Do not induce vomiting unless advised to do so by a health care provider. 4. Inform the laboratory’s PI and EH&S.
C. Spills of Biohazards
ASU does not have a centralized biological spill response team. Therefore, each laboratory working with potentially hazardous biological material must be prepared and trained to handle its
own biological spills. EH&S is available for assistance if necessary. Additional information pertaining to spills which involve recombinant DNA, blood, microorganisms, or any other
bioresearch materials can be found at http://cfo.asu.edu/emergency.
Performing all work on plastic-backed liners to absorb spills can minimize the consequences of a
spill of a biohazardous or select agent. The quantities of these materials should be limited so they can be easily contained, cleaned, or destroyed. If respiratory protection is required, the ASU
Respiratory Protection Program must be followed. A simple spill kit should be on hand including:
Chlorine bleach or some other concentrated disinfectant
A package or roll of paper towels
Autoclave bags
Rubber gloves
Forceps for picking up broken glass.
D. Spills Inside a Biological Safety Cabinet (BSC)
1. Alert the other laboratory employees.
2. Leave the cabinet turned on. 3. While wearing gloves, spray or wipe cabinet walls, work surfaces and equipment with
disinfectant equivalent to 1:10 bleach solution. If necessary, flood the work surface, as well
as drain-pans and catch basins below the work surface, with disinfectant for a contact time of at least 20 minutes.
4. Report the spill to the laboratory’s PI, who will report the spill to the RO if a select agent or toxin is involved.

ASU Biosafety Manual 45
5. Soak up disinfectant and spill with paper towels. Drain catch basin into a container. Lift front
exhaust grill and tray and wipe all surfaces. Ensure that no paper towels or solid debris are blown into the area beneath the grill.
6. Autoclave all clean-up materials before disposal in the biohazard waste container. 7. Wash hands and any exposed surfaces thoroughly after the clean-up procedure.
E. Small Spill of Material Outside of a BSC
1. Alert laboratory employees.
2. Wearing gloves, safety glasses, and a lab coat, cover the spill with paper towels and gently apply disinfectant, proceeding from the outer edge of the spill to its center. Leave in place for
20 minutes. 3. Report the spill to the laboratory’s PI, who will report the spill to the RO if a select agent or
toxin is involved.
4. Pick up the towels and discard into a biohazard container. Pick up any pieces of broken glass with forceps and place in sharps container.
5. Re-wipe the spill area with disinfectant and thoroughly wash hands after glove removal.
F. Large Spill of Biohazardous Material (>500 ml) Outside of a BSC
1. Hold your breath and leave the room immediately.
2. Warn others to stay out of the spill area to prevent spread of contamination. 3. Post a sign stating: “DO NOT ENTER, BIOHAZARD SPILL, contact (name and phone #) for
information.” 4. Remove any contaminated clothing, ensuring that clothing is not pulled over the face, and
put into a biohazard bag for later autoclaving.
5. Wash hands and exposed skin. 6. Notify the Principal Investigator, supervisor, and EH&S.
7. Put on protective clothing (lab coat, gloves and, if indicated, respirator, eye protection, shoe covers) and assemble clean-up materials.
8. Wait 30 minutes before re-entering the contaminated area to allow for dissipation of
aerosols. 9. Cover the spill with paper towels and gently apply disinfectant, proceeding from the outer
edge of the spill to its center. Leave in place for 20 minutes. 10. Collect and autoclave all treated material and discard in a biohazard container. Pick up any
broken glass with forceps and place them into a sharps container. 11. Re-wipe the spill area with disinfectant and wash hands thoroughly at completion of clean-
up.
G. Small Spill (<500 ml) of Recombinant DNA Materials
1. Put on gloves and eye protection if you are not already wearing them.
2. Cover spilled material with an absorbent paper towel or Kimwipe. Once the absorbent
material is in place over the spill, wet the material with a 10% solution of bleach or other appropriate disinfectant.
3. Let stand 15 minutes, wipe up and wash surface with appropriate disinfectant. 4. Wipe down all equipment and surfaces which may have been splashed.
5. Dispose of contaminated paper towels as infectious waste.
H. Large Spill (>500 ml) of Recombinant DNA Materials in a BSC
1. BSC must run during cleanup to contain aerosols and HEPA-filter exhaust air. 2. Don appropriate personal protective gear before initiating cleanup
3. Initiate clean up as soon as possible using a germicidal disinfectant (phenolic or iodophor). Alcohol is not acceptable.

ASU Biosafety Manual 46
4. If the spill is contained on a bench pad, remove the contaminated bench pad discard as
infectious waste. 5. If the spill is on the work area surface, cover spilled material with disinfectant-soaked towels.
Allow 20 minutes contact time then remove the contaminated towels and discard as infectious waste.
6. Wipe down the interior of the cabinet and any splatter on items within the cabinet with a
disinfectant-soaked towel. 7. Wipe down non-autoclavable materials with disinfectant. Allow 20 minutes of contact time
with disinfectant before any items are removed from cabinet. 8. Place items designated as contaminated used sharps in an appropriate infectious waste
sharps container using tongs/forceps. Place other contaminated disposable materials used in the cleanup process in an autoclave bag. Process as infectious waste.
9. Place contaminated re-usable items in biohazard bags, autoclavable pans with lids or wrap
them in newspaper. Sterilize, preferably by autoclaving, and then clean for re-use. 10. If the cabinet has a catch basin beneath the work surface and the spill resulted in liquids
flowing into this area, more extensive decontamination is required.
a. Ensure the drain valve under the cabinet is closed.
b. Pour disinfectant onto the work surface and through the front and rear grilles into the drain pan. Allow 20-30 minutes contact time.
c. Absorb spilled fluid-disinfectant from work surface with paper towels and discard in biohazard bag.
d. Prepare to empty drain pan. Place disinfectant solution in a collection vessel. Attach flexible tubing to the drain valve. The tube should be of sufficient length to allow the
open end to be submerged in the collection vessel to minimize aerosol generation.
e. Open the drain valve and empty the drain pan into the collection vessel containing disinfectant. Flush the drain pan with water and remove the flexible tubing. Manage
contaminated materials as if they are infectious. f. Remove protective clothing used during cleanup and place in a biohazard bag for
autoclaving. Wash hands when gloves are removed.
g. Notify Principal Investigator, supervisor, and EH&S. Consult with EH&S to determine whether formaldehyde decontamination of the cabinet and filters is necessary, especially
if a high-risk agent or a major spill of a moderate-risk agent occurred. h. Run BSC at least 10 minutes after cleanup, before resuming activity in the cabinet.
I. Large Spill (>500 ml) of Recombinant DNA Materials outside of a BSC
1. If a spill of a biohazardous material occurs, outside the BSC, notify other individuals in the laboratory to evacuate.
2. Exit the laboratory to the hallway, closing the door behind you. 3. Remove any contaminated clothing (turn contaminated portion inward) and place it in an
autoclave bag.
4. Wash all exposed skin. 5. Place signs on door(s) to the laboratory warning individuals who may want to enter that a
spill occurred and access is denied. 6. Allow aerosols to settle for 30 minutes before re-entering the laboratory.
7. Notify the Principal Investigator, supervisor, and EH&S prior to proceeding with cleanup.
8. Assemble supplies (e.g., disinfectant, sharps containers, towels, tongs, autoclave bags) before entering the laboratory.
9. Don appropriate personal protective equipment (i.e. disposable gown, protective eyewear, gloves, shoe coverings and respiratory protection [if needed]).
10. Clean up spill with a suitable disinfectant as follows:
a. Surround spill area with disinfectant or diking material that is soaked in disinfectant.
b. Place paper towels soaked in a disinfectant over the entire spill area. c. Allow 20-minute contact time with the disinfectant to ensure adequate germicidal action.

ASU Biosafety Manual 47
d. Wipe down non-autoclavable materials with germicidal disinfectant.
e. Place items designated as contaminated used sharps in an appropriate infectious waste sharps container. Place other disposable materials used in the cleanup process in an
autoclave bag. Process as infectious waste. f. Place contaminated re-usable items in biohazard bags or autoclavable pans with lids.
Sterilize preferably by autoclaving, and then clean for re-use. Remove protective clothing
used during cleanup then place in a biohazard bag for autoclaving. g. Wash hands when gloves are removed.
J. Spill of Recombinant DNA Materials in a Centrifuge
A single centrifuge spill or release can lead to multiple infections in a laboratory. Aerosols are
created when fluid escapes from the rotor or cup while the centrifuge is operating at high speed.
Therefore, whenever opening a centrifuge, it must be performed slowly.
Unsealed Buckets
1. If a centrifuge tube breaks while the centrifuge is running, turn off motor. Allow the machine
to be at rest for 30 minutes before opening. If breakage is discovered after the machine has stopped, re-close the lid immediately and allow the unit to be at rest for 30 minutes.
2. Unplug centrifuge before initiating clean up. 3. Don strong, thick, rubber gloves, and other PPE before proceeding with clean up.
4. Flood centrifuge bowl with a germicidal disinfectant. Place paper towels soaked in a disinfectant over the entire spill area. Allow a 20 minutes contact time.
5. Use mechanical means (e.g., forceps) to remove broken tubes and glass fragments. Place
them in a sharps container for autoclaving and disposal as infectious waste. 6. Remove buckets, trunnions, and rotor and place in disinfectant for 20 minutes or autoclave.
7. Unbroken, capped tubes may be placed in disinfectant and recovered after 20 minutes contact time or autoclaved.
8. Use mechanical means to remove remaining disinfectant soaked materials from centrifuge
bowl and discard as infectious waste. 9. Place paper towels soaked in a disinfectant in the centrifuge bowl and allow it to soak
overnight, wipe down again with disinfectant, wash with water and dry. Discard disinfectant soaked materials as infectious waste.
10. Remove protective clothing used during cleanup and place in a biohazard bag for
autoclaving. Wash hands whenever gloves are removed. 11. Notify Principal Investigator, supervisor, and EH&S.
Sealed Buckets (Safety Cups)
1. If breakage is suspected, remove the sealed bucket to a biological safety cabinet before
opening.
2. If breakage occurred, replace the cap on the safety cup loosely and autoclave. 3. Notify Principal Investigator, supervisor, and EH&S.
K. Reporting Exposures
In the event of an exposure to a biohazardous material:
1. Report to an Occupational Health Nurse or a primary healthcare provider. 2. Complete an Accident-Illness Report Form and submit to EH&S.
3. Work with the Principal Investigator, supervisor, and EH&S to report accident to the NIH
Office of Biotechnology Activities as required by the NIH Guidelines.

ASU Biosafety Manual 48
X. TRANSFERS, PACKAGING, AND SHIPPING OF BIOLOGICAL MATERIALS
A. Transfers
The transferring, packing and shipping of select agents and toxins is HIGHLY regulated. No select
agent or toxin shall be transferred, packed, or shipped without the express approval from the RO. Please see the appendix titled “Special Considerations for Select Agents and Toxins” for additional
information.
For materials that are not Select Agents, each PI must develop procedures for transferring or
shipping from the laboratory. The PI must ensure the following:
Package, label, and transport biohazardous agents in compliance with all applicable local,
federal, and international transportation and shipping regulations, including US Department of Transportation (DOT) regulations. Materials that are transported by airline
carrier should also comply with packaging and shipping regulations set by the
International Air Transport Association (IATA). Personnel who package, handle, and ship these agents (including import and export) are subject to all applicable training. Please
refer to EHS Form 406. The RO must be notified of all select agent transfers; internal or external (see section below for additional information).
Required permits (e.g., granted by the US Public Health Service, USDA, DOT, US
Department of Commerce and IATA) are obtained before biohazardous agents are
prepared for transport. Standard operating procedures should be in place for import and export activities.
Decontaminate contaminated or potentially contaminated materials before they are
removed from the laboratory area. Avoid hand-carrying biohazardous agents when transferring them to other external
facilities. If biohazardous agents are to be hand-carried on common carriers, all
applicable packaging, transport, and training regulations should be followed. Develop and follow a protocol for intra-facility transfer (between laboratories on ASU
campuses) of all biological and biohazardous agents. Contact EHS for assistance.
Packaging and shipping of biological materials must be completed in a way that ensures the contents will not leak and that the package will arrive in good condition.
The definitions below apply to the packaging and shipping instructions that follow:
Etiologic agent means a viable microorganism or its toxin which causes, or may cause,
human disease. Diagnostic specimen means any human or animal material including, but not limited
to, excreta, secreta, blood and its components, tissue and tissue fluids, etc., which is
reasonably believed to contain an etiologic agent and is being shipped for purposes of diagnosis.
Biological product means a biological prepared and manufactured in accordance with
regulations that govern the manufacture of vaccines, reagents, etc. Interstate shipping means shipping across state lines within the continental United
States. Intrastate shipping means shipping within the State of Arizona.
B. Packaging
All biological materials including diagnostic specimens and biological products that may contain an etiologic/biohazardous agent must be packaged to withstand leakage of contents, shocks,
pressure changes and other conditions possible with ordinary handling and transportation (e.g.,
passage through cancellation machines, sorters, conveyors). Contents should not leak to the outside of the shipping container even if leakage of the primary container occurs.

ASU Biosafety Manual 49
Specific packaging requirements apply to materials that are known to contain, or reasonably
believed to contain certain etiologic agents. For such materials the following procedures apply (See Figure 1. Source: Biosafety in Microbiological and Biomedical Laboratories 5th Edition, Appendix C).
Figure 1
Volume not exceeding 50 milliliters (mL):
1. Place material in a securely enclosed, watertight primary container (test tube, vial, etc.). Enclose this primary container in a secondary, durable, watertight container. Several primary
containers may be enclosed in a single secondary container as long as the total volume of material in all the primary containers enclosed does not exceed 50 ml.
2. Place absorbent nonparticulate material (e.g., paper towels, not sawdust or vermiculite, etc.)
in the spaces at the top, bottom, and sides between the primary and secondary containers. Use enough absorbent material to absorb the entire contents of the primary container(s) in
case of breakage or leakage. 3. Enclose each set of primary and secondary containers in an outer shipping container
constructed of corrugated fiberboard, cardboard, wood or other material of equal strength.
Do not use bags, envelops, or similar materials. 4. If you package the material with dry ice, see the section below (Packaging with Dry Ice).

ASU Biosafety Manual 50
Volume greater than 50 ml:
1. Follow requirements for lesser volumes outlined above.
2. Place shock absorbent material at the top, bottom, and sides between the secondary container and the outer shipping container. (This material should at least equal the amount
of absorbent material placed between the primary and secondary containers).
3. Ensure single primary containers contain no more than 1000 ml of material; however, two or more primary containers (combined volumes not exceeding 1000 ml) may be placed in a
single secondary container. The maximum amount of etiologic agent which may be enclosed within a single outer shipping container must not exceed 4000 ml.
C. Packaging with Dry Ice
1. If used, place dry ice between the secondary and outside containers.
2. Place shock absorbent material so as to prevent the secondary container from becoming loose inside the outer container as the dry ice sublimates.
3. Use the DOT dry ice label. Guidelines for shipping with dry ice can be found at EHS MazMat shipping.
D. Labeling
The outer shipping container of all materials containing etiologic/biohazardous agents which are being shipped or transported must bear a special label, as illustrated in Figure 2. These labels are
available from your laboratory supply vendor.
Figure 2 – Example of a Etiological Agent Label
E. Shipping and Transportation Methods and Requirements
Registered Mail or the Equivalent
For a list of etiologic agents that use registered mail or an equivalent system which provides the sender with immediate notification of receipt refer to Appendix A of the CDC Guidelines on
Additional Requirements for Facilities Transferring or Receiving Select Agents and Toxins, 49 CFR
Part 72.
Federal Express or UPS
1. For Federal Express/UPS shipments, internationally or domestically, follow the International
Air Transport Association (IATA) Dangerous Goods Regulations. (Receipt of shipment notice is not required since the shipment is traceable through the specific carrier.)

ASU Biosafety Manual 51
2. Apply appropriate labels to the outer shipping container for packages containing dry ice
and/or biohazardous substances as shown in Figures 3 and 4, respectively. 3. Contact the specific carrier's dangerous goods agent prior to shipment for any additional
packaging and labeling requirements.
Figure 3 Figure 4
Damaged Packages
When evidence of leakage or any other damage to packages bearing an Etiological Agents/Biomedical Material label is discovered, the carrier must promptly isolate the package and
notify the Director, Centers for Disease Control and Prevention (CDC), (404) 633-5313, 1600 Clifton Road NE, Atlanta, Georgia 30333.
Notice of Delivery
In the event that a package sent from ASU is not received by the recipient within 5 days following the anticipated delivery of the package, the sender must notify the Director, Centers for
Disease Control and Prevention, 1600 Clifton Road NE, Atlanta, Georgia 30333 or by telephone (404) 633-5313.
Importation/Exportation of Etiologic Agents
Importation of biohazardous agents, etiologic agents, and vectors that may contain such agents is governed by federal regulation. In general, an importation permit is required for any infectious
agent known to cause disease to humans. This includes, but is not limited to, bacteria, viruses, rickettsia, parasites, yeasts, and molds. In some instances, an agent which is suspected of
causing human disease also requires a permit.
Importation permits are issued by the U.S. Public Health Service (USPHS) only to the importer,
who must be located in the United States. The importation permit, with the proper packaging and labeling, will expedite clearance of the package of infectious materials through the USPHS
Division of Quarantine and release by U.S. Customs.
Instead of an importation permit, a Letter of Authorization may be issued by the Centers for
Disease Control and Prevention after review of an “Application to Import an Etiological Agent.” The letter is issued for materials that are judged to be noninfectious, but which might be
construed to be infectious by U.S. Customs inspection personnel. Letters of Authorization may be
issued for items such as formalin-fixed tissues, sterile cell cultures, clinical materials such as human blood, serum, plasma, urine, cerebrospinal fluid, and other tissues or materials of human

ASU Biosafety Manual 52
origin when there is no evidence or indication that such materials contain an infectious agent.
Letters of Authorization are in effect for two years and do not require a shipping label to be issued by CDC.
Importation permits and Letters of Authorization are issued by the Biosafety Branch, Office of
Health and Safety, CDC, 1600 Clifton Road, Atlanta, Georgia 30333, after review of a completed
application form. Application forms may be obtained by calling CDC at their FAX Information System. Dial 1-888-CDC-FAXX and enter document number 101000. CDC can also be contacted
on the Internet at http://www.cdc.gov/od/eaipp/ . Completed forms may be returned to CDC by mail or FAX at 404-639-2294. Application to CDC for the importation permit should be made 15
working days in advance of the shipment date to allow time for processing, issuance, and delivery of the permit and shipping labels to the permittee.
F. Other Permits
APHIS permits are required for importation or domestic shipping of infectious agents of livestock, poultry, and other animal diseases, and any materials that might contain these agents. Tissue
(cell) culture techniques customarily use bovine material as a stimulant for cell growth. Tissue
culture materials, and suspensions of cell culture-grown viruses or other etiologic agents containing growth stimulants of bovine or other livestock origin are, therefore, controlled by the
USDA due to the potential risk of introduction of exotic animal disease into the U.S. Applications for USDA/APHIS permits may be obtained by calling the USDA/APHIS at (301) 734-3277 or
through the Internet at http://www.aphis.usda.gov/permits/index.shtml.
The importation or domestic transfer of plant pests is also regulated by the USDA. Such a permit
is required for plant pests, plant biological agents, or any material that might contain them. Information may be obtained by calling (301) 734-3277 or through the Internet at
http://www.aphis.usda.gov/plant_health/permits/index.shtml
USDA permits are required for certain live animals and all live bats. Call (800) 358-2104 for
further information.
Export of infectious materials may require license from the Department of Commerce (DoC). Exporters of a wide variety of etiologic agents of human, plant, and animal diseases, including
genetic material and products which might be used for culture of large amounts of agents will
require an export license. Information may be obtained by calling the DoC Bureau of Export Administration at 202-482-4811 or through the Internet at https://bxa.ntis.gov/.

ASU Biosafety Manual 53
XI. SECURITY
Laboratory security is an integral part of an effective safety program. Follow these steps to ensure a
secure working environment in your laboratory:
1. Keep laboratory doors closed and locked when unoccupied.
2. Keep stocks of organisms and hazardous chemicals locked when the laboratory is unoccupied. 3. Keep an accurate record of chemicals, stocks, cultures, project materials, growth media, and those
items that support project activities. 4. Notify ASU police if materials are damaged or missing from laboratories.
5. Inspect all packages arriving into the laboratory. 6. When research is completed for the day, ensure that chemicals and biological materials have been
stored properly and securely.
7. Decontaminate materials and work surfaces after completing work and at least daily. 8. Turn off equipment, flames, steam supply, and electrical appliances after completing work.
9. Ask strangers (someone you do not recognize as a co-worker or support staff person) to exit the room if they are not authorized to be there.
10. Discuss other security-specific requirements with your supervisor and colleagues.
Security procedures for laboratories with select agents and toxins can be found in the appendix titled
“Special Considerations for Select Agents and Toxins.”

ASU Biosafety Manual 54
XII. COMPLIANCE
ASU Environmental Health and Safety (EH&S) will conduct regular inspections, at least annually, of each
laboratory to ensure compliance with the procedures and protocols of this manual. Inspection reports will document violations and be directed to the PI. The results of these inspections will be documented and
kept on file with EH&S. Any significant problems will be reported to the IBC.

ASU Biosafety Manual 55
XIII. RECORDKEEPING
At a minimum, the PI must maintain the following records and be prepared to present these at the
annual laboratory inspection:
An accurate, current list of each biological agent or toxin stored in that room;
A Health Hazard Assessment for each biological agent or toxin stored in that room;
A current Responsible Information Party Sheet;
Training Documentation Forms;
Safety, security, and emergency response plans; and
Safety and security incident reports.

ASU Biosafety Manual 56
XIV. PROGRAM EVALUATION
The review of the elements as noted in the Compliance and Recordkeeping sections of this document will
constitute an evaluation of the ASU Biosafety and Biosecurity Program.

ASU Biosafety Manual 57
Table 1 - Disinfectant Activity
Disinfectants Practical Requirements Inactivates
Type Category Use
Dilution
Contact Time (min) Lipovirus.
Contact Time (min)
Broad Spectrum
Temperature (Co)
Relative Humidity
(%)
Vegetative Bacteria
Lipoviruses Nonlipid Viruses
Mycobacteria Bacterial Spores
Liquid Quat. Ammon.
Cpds 0.1%-2.0%
10 NE + +
Phenolic Cpds 1.0%-5.0%
10 NE + + B
Chlorine Cpds 500 ppm* 10 30 + + + + +
Iodophor 25-1600 ppm*
10 30 + + +
Alcohol, Ethyl 70%-85% 10 30 + + B
Alcohol, Isopropyl 70%-85% 10 30 + + B
Formaldehyde 0.2%-8.0%
10 30 + + + + +
Glutaraldehyde 2% 10 30 + + + + +
Gas Ethylene Oxide 8-23g/ft3 60 60 37 30 + + + + +
Paraformaldehyde 0.3 g/ft3 60 60 >23 60 + + + + +
NE=not effective
B=Variable results dependent on virus *=Available halogen (1:100)

ASU Biosafety Manual 58
Table 2 - Disinfectant Characteristics
Disinfectants Important Characteristics
Type Category Effective Shelf
Life >1 week (A) Corrosive Flammable
Explosion Potential
Residue Inactivated by Organic
Matter
Compatible for Optics
(D)
Skin Irritant
Eye Irritant
Respiratory Irritant
Toxic (E)
Liquid Quat. Ammon.
Cpds + + + + + +
Phenolic Cpds + + + + + +
Chlorine Cpds + + + + + + +
Iodophor + + + + + + +
Alcohol, Ethyl + + + +
Alcohol, Isopropyl + + + +
Formaldehyde + + + + + +
Glutaraldehyde + + + + + + +
Gas Ethylene Oxide N/A +(B) +(B) + + + + +
Paraformaldehyde N/A +(C) +(C) + + + + +
N/A=not applicable (A)=Protected from light and air (B)=Neither flammable nor explosive in 90% CO2 or fluorinated hydrocarbon, the usual form (C)=At concentrations of 7%-73% by volume in air, solid exposure to open flame (D)=Usually compatible, but consider interferences from residues and effects on associated materials such as
mounting (E)=By skin or mouth, or both. Refer to manufacturer's literature and the MSDS.

ASU Biosafety Manual 59
Table 3 - Disinfectant Applications
Disinfectants Important Characteristics
Type Category Work Surface Dirty
Glassware Large Area
Air Handling
Portable Equip. Surface Decon
Port-able Equip.
Penetrating Decon
Fixed Equip. Surface Decon
Fixed Equip.
Penetrating Decon
Optical & Electronic
Inst.
Liquid & Discard
Book, Paper
Liquid Quat. Ammon.
Cpds + + + +
Phenolic Cpds + + + +
Chlorine Cpds + + + + +
Iodophor + + + +
Alcohol, Ethyl + + + +
Alcohol, Isopropyl + + + +
Formaldehyde + + + +
Glutaraldehyde + + + +
Gas Ethylene Oxide + + + +
Paraformaldehyde + + + + + +

Appendix A: Definitions
Biohazardous Agent: Any microorganism (including, but not limited to, bacteria, viruses, fungi, rickettsia,
protozoa or prions) or infectious substance, or any naturally occurring, bioengineered, or synthesized component of any such microorganism or infectious substance, capable of causing:
Death, disease, or other biological malfunction in a human, animal, plant, or another living organism;
Deterioration of food, water, equipment, supplies, or material of any kind; or
Deleterious alteration of the environment.
Recombinant DNA:
Molecules that are constructed outside living cells by joining natural or synthetic DNA segments to DNA
molecules that can replicate in a living cell, or Molecules that result from the replication of those described above, and
Synthetic DNA segments which are likely to yield a potentially harmful polynucleotide or polypeptide.
Centers for Disease Control and Prevention (CDC): The Centers for Disease Control and Prevention of the
United States Department of Health and Human Services
Etiologic Agent: A viable microorganism or its toxin that causes, or may cause, human disease
Overlap agent or toxin: Any microorganism (including, but not limited to, bacteria, viruses, fungi, rickettsia, or
protozoa) or toxin that poses a risk to both human and animal health.
Responsible Official: The individual designated by an institution to act on its behalf. This individual must have the authority and control to ensure compliance with the regulations
Toxin: The toxic material or product of plants, animals, microorganisms (including, but not limited to, bacteria, viruses, fungi, rickettsia, or protozoa), or infectious substances, or a recombinant or synthesized molecule,
whatever their origin and method of production, and includes:
Any poisonous substance or biological product that may be engineered as a result of biotechnology
produced by a living organism; or Any poisonous isomer or biological product, homolog or derivative of such a substance.

61
Appendix B: Lab-Specific Biosafety Manual Template
Arizona State University
Lab-Specific Biosafety Manual
Template
[Your Name]
[Your Title]
[Arizona State University, Department Name]
[Building Name, Room Number]
Tempe, AZ
[Preparation Date]

Instructions to Principal Investigators (PI) for completing this template for Lab-Specific Biosafety
Manual
Before completing this template for the use of select agents and toxins in your laboratory, please review the ASU
Biosafety Manual and its appendices as well as the CDC Guidelines for Working with Toxins of Biological Origin.
In addition, each PI must submit to EH&S the following:
o A completed Responsible Party Information Sheet;
o An annual chemical and biological inventory; and o A Health Hazard Assessment for each biological agent and toxin stored in the laboratory. A copy of this
Health Hazard Assessment should be placed in Appendix B of this document.
Complete all highlighted sections with the laboratory policies and procedures specific to the biohazardous
agent(s) in your laboratory. If you have any questions on completing these procedures, please contact the EH&S, (480) 965-1823, for additional assistance.

63
SIGNATURE and ACKNOWLEDGEMENT PAGE
Authorization [This section is based upon your specific laboratory setup]
All members of the [Principal Investigator’s name] Laboratory who have signed the list below are
approved for entry into Room [XXXX] while work with biohazardous agents is in progress. Anyone (including any workers not in the PI’s Lab) who uses Room [XXXX] lab must sign below.
Acknowledgement
We, the undersigned, understand that [the agents used in Room XXXX] handled in Room [XXXX] of
[Building Name] may be hazardous to humans. Furthermore, we have read and understood this manual
and have attended ASU Laboratory Safety Training, ASU Bloodborne Pathogen Training, and Biosafety Training specific to the agent used in this laboratory prior to handling samples in Room [XXXX].
Name Signature Date Agent Vaccination
(Yes/No/ Declined/NA)
*Agent vaccination in table should be specified, as appropriate to potential exposure in the laboratory: HBV, Vaccinia, Influenza, etc.

64
PURPOSE
This document, in addition to the ASU Biosafety Manual, provides a comprehensive information source for
all matters covering the use of biohazardous agents handled in this laboratory [Room Address of Principal Investigator]. Specifically, it describes the procedures to be used to ensure a safe working environment
while handling biohazardous agents. This manual will be reviewed annually by the Principal Investigator
for changes or corrections to ensure that it is accurate.
[The information in the following two sections is an example of the type of specific description of your operations and activities that you should include in your manual. You should discuss detailed procedures and the actual precautions to be taken by those who actually work with the biohazardous agents found in your laboratory.]
BACKGROUND
Description of work to be performed and biohazardous agents to be used (as shown in the following example):
Biological Hazards under Routine Use [insert a brief summary of the hazards]
Biological Hazards as result of a spill or other accident [insert a brief summary of the hazards]
Procedures involving the use of Biological Hazards [insert a step-by-step procedure for this work]
DESCRIPTION OF LABORATORIES
[Provide a summary of required project equipment and a floor plan showing its location]. Laboratory(s)
is/are located on the [xxx floor] of [Building Name] building within Arizona State University. All biohazardous agents manipulations occur(s) in Room(s) [XXXX].
Floor diagrams are displayed as Appendix A at the end of this manual. Ensure that the location of the sinks, eyewash, safety shower, spill kits, fire extinguishers, exits, MSDSs, and phones are included on the
diagram.
NOTE: PLEASE EDIT THE FOLLOWING POLICES AND PROCEDURES TO FIT YOUR LAB OPERATIONS.
ENSURE THAT ALL ITEMS FROM THE ASU SAFETY BIOSAFETY MANUAL ARE INCORPORATED INTO THIS DOCUMENT.
GENERAL LAB RULES
Work with biohazardous agents will be performed in [Building Name, Room XXXX].
1. Laboratory employees must immediately notify the laboratory supervisor or PI in case of an accident, injury, illness, spill or exposure associated with laboratory activities.
2. Access to this area will be limited to persons meeting the following qualifications:
Have attended all applicable training sessions; and
Have read and signed this manual.
3. No eating, drinking, smoking, handling contact lenses, or applying cosmetics in [Room XXXX or Room YYYY] at any time. Persons who wear contact lenses should also wear goggles or a face shield while
working with biohazardous agents. If laboratory employees elect to wear respirators, all aspects of ASU’s Respiratory Protection Program must be followed. All fit testing and training documentation
should be included in Appendix C.

65
4. Food, medications, or cosmetics should not be brought into the laboratory for storage or later use.
Food is stored outside the work area in cabinets or refrigerators designated specifically for that purpose and labeled accordingly.
5. Mouth pipetting is prohibited; mechanical pipetting devices are to be used at all times.
6. All procedures are performed carefully to minimize the creation of splashes or aerosols.
7. Wash hands: after handling biohazardous materials
after removing gloves, and
before leaving the laboratory.
8. Razor blades, scalpels, and hypodermic needles (“sharps”) should be used only when absolutely needed in [Room XXXX].
9. Work surfaces are decontaminated at least once a day and after any spill of biohazardous agents with [specify the appropriate disinfectant (refer to the ASU Biosafety Manual)].
10. All cultures, stocks, and other regulated biological wastes are decontaminated before disposal by
[specify an approved decontamination method, such as autoclaving].
11. Plastic-ware should be substituted for glassware whenever possible.
12. When biohazards are in use, the room should be posted to indicate “Biohazards in Use - Authorized
Personnel Only.’’ Any special entry requirements should be posted on the entrance(s) to the room. Only personnel whose presence is required should be permitted in the room while biohazards are in
use.
13. All high-risk operations should be conducted with at least two knowledgeable individuals present.
Each must be familiar with the applicable procedures, maintain visual contact with the other, and be ready to assist in the event of an accident.
CONTAINMENT REQUIREMENTS
1. Preparation of biohazardous stock solutions and manipulations of high concentrations or large volumes of biohazard agents should be conducted in a biological safety cabinet or equivalent
containment system approved by a licensed outside contractor.
2. Preparation of primary containers of toxin stock solutions and manipulations of primary containers of
dry forms of toxins should be conducted in a chemical fume hood, a glove box, or a biological safety cabinet or equivalent containment system approved by a licensed outside contractor. HEPA and/or
charcoal filtration of the exhaust air may be required.
3. The user should verify inward airflow of the fume hood or biological safety cabinet before initiating
work.
4. All work should be done within the operationally effective zone of the fume hood or biological safety cabinet.
5. Before containers are removed from the hood, cabinet, or glove box, the exterior of the closed primary container should be decontaminated and placed in a clean secondary container.
Biohazardous agents and toxins should be transported only in leak-proof and spill-proof secondary containers.
6. Contaminated and potentially contaminated protective clothing and equipment should be

66
decontaminated using methods known to be effective against the toxin before removal from the
laboratory for disposal, cleaning or repair. If decontamination is not possible or practical, materials (e.g., used gloves) should be disposed of as biological or toxic waste. Materials contaminated with
infectious agents as well as toxins should also be autoclaved or otherwise rendered non-infectious before leaving the laboratory.
7. The interior of the hood, glove box, or cabinet should be decontaminated periodically (e.g. at the end of a series of related experiments). Until decontaminated, the hood, box, or cabinet should be posted
to indicate that toxins are in use, and access to the equipment and apparatus restricted to necessary, authorized personnel.
8. When vacuum lines are used with systems containing toxins, they should be protected with a HEPA
filter to prevent entry of toxins into the lines. Sink drains should be similarly protected when water
aspirators are used.
PROPER USE OF BIOLOGICAL SAFETY CABINETS
[NOTE: PLEASE REFER TO THE SECTION ON BIOLOGICAL SAFETY CABINETS IN THE ASU BIOSAFEY MANUAL
FOR ADDITIONAL INFORMATION.]
Biological safety cabinets (BSC) must be certified prior to use. A qualified outside contractor must certify
each BSC annually. Check the certification sticker on the front of the unit to verify your C’s condition. The
latest certification can be found in Appendix C.
To assure sterility inside the BSC and establish proper airflow for containment, the blower should be turned on at least ten minutes before infectious materials are put in the BSC.
The BSC airflow (“magnahelic”) gauge should be checked to assure proper operation of the cabinet before placing any materials into it. (Reading is equal to approximately 0.5 inches.) Readings indicate
relative pressure drop across the HEPA filter. Higher readings may, therefore, indicate filter clogging. Zero readings may indicate loss of filter integrity.
After use, wipe inner surfaces (especially the pan) with a solution of [The disinfectant chosen as effective for the agent you are using (refer to Table 1 in the ASU Biosafety Manual) and allow to dry. Always keep
a bottle of the disinfectant in the cabinet for decontaminating or in case of a spill.
NEVER place anything over the front or rear grill of a biosafety cabinet.
Disrupting the airflow into the front grill allows contaminated air from inside the cabinet to blow into the
lab or directly at the person sitting at the cabinet. It also allows non-sterile air from the room to blow into the biosafety cabinet over the experiments.
Materials should be placed in the cabinet so as not to block airflow into the rear grill. Leave a few inches
for air to flow around objects. Any disruption of the air flow in the cabinet decreases its effectiveness.
Remember: “A biosafety cabinet is only as safe as the person using it.”
Before manipulating infectious materials, make sure that you have everything you need in the cabinet.
The fewer times you pull your hands out of the cabinet, the less disruption of the air flow.
Work should be performed in the center of the work surface of the cabinet whenever possible. Work
outward progressing from clean to dirty (contaminated). However, biohazardous agents should not be placed directly adjacent to or directly on the intake grills.

67
After manipulating biohazardous agents, make sure all containers are tightly closed before removing
them. Wipe down the surface of all equipment used in manipulations (mechanical pipettes, etc.) with disinfectant before removing from the cabinet. All waste and disposable items should be left in the
cabinet until properly decontaminated or contained.
After the cabinet has been emptied, wipe exposed surfaces including the front grill and splash area with
disinfectant. Allow the blower to run for a minimum of ten minutes to purge any potentially infectious aerosols from inside the cabinet before shutting off the blower.
NOTE: Class IIA cabinets recirculate about 70% of the air inside themselves and exhaust the remainder
to the lab. Any use of volatile solvents, including ethanol and isopropanol, should be kept to a minimum or done elsewhere. Dangerously high levels of volatile fumes can accumulate inside the cabinet and pose
a threat of fire or explosion.
DECONTAMINATION
[NOTE: PLEASE REFER TO THE SECTION ON EMERGENCY RESPONSE IN THE BIOSAFETY MANUAL FOR
ADDITIONAL INFORMATION.]
The decontaminant of choice is [xxxx. (Please see Table 1 in the ASU Biosafety Manual for disinfectant selections)].
Pans and splash guards (inside and out) should be cleaned after every use.
All material and equipment contaminated with or containing potentially biohazardous agents should be
decontaminated:
Upon completion of procedures involving the use of biohazardous agents;
In the event of spills of such materials;
At least daily; and
Before being washed, stored, or discarded.
Pipettes and other shared small equipment should be wiped with appropriate disinfectant after use and
before removing them from the cabinet.
BIOLOGICAL WASTE DISPOSAL
Wastes associated with biohazardous agents must be disposed of in special ways because they may have
been contaminated with infectious organisms or toxic agents. These potentially infectious items include all sharps, e.g. glass implements, needles, syringes, blades, etc. coming from facilities using infectious
materials; and biologically cultured stocks and plates, human blood or tissues.
For disposal of these wastes, the personnel must:
Sterilize or disinfect waste materials associated with viral, bacterial or other agents infectious to
humans by autoclaving or disinfectant equivalent to 1:10 bleach solution;
Disposed of or destroyed toxins per the Lab-Specific Biosafety Manual;
Place all biohazardous wastes, except for sharps, directly into the red bag-lined medical waste
boxes. The procedures for biohazardous waste handling are described in the ASU Biological Hazardous Waste Management Compliance Guidelines.
PERSONAL PROTECTIVE EQUIPMENT
1. When using an open-fronted fume hood or biological safety cabinet, protective clothing, including gloves and a long-sleeved body covering (gown, laboratory coat, smock, coverall, or similar garment)

68
should be worn so that hands and arms are completely covered.
2. Eye protection should be worn when handling a biohazardous agent or toxin, infectious organism, or
chemicals (e.g. ethanol or other disinfectant).
3. Other protective equipment may be required, depending on the characteristics of the biohazard or
toxin and the containment system. [INSERT ANY ADDITIONAL REQUIRED PPE HERE]
4. When handling dry forms of toxins that are electrostatic:
Do not wear gloves (such as latex) that help to generate static electricity; and
Use glove bag within a hood or biological safety cabinet, a glove box, or a Class III biological
safety cabinet.
5. When handling biohazardous agents that are percutaneous hazards (irritants, necrotic to tissue, or
extremely toxic from dermal exposure), select gloves that are known to be impervious to the biohazard or toxin. GLOVES WORN IN THE LABORATORY WILL BE XXX.
6. Consider the chemical characteristics and potential routes of exposure of biohazardous agents,
diluent, and disinfectant when selecting gloves and other protective clothing.
7. If infectious agents and toxins are used together in an experimental system, consider both when
selecting protective clothing and equipment.
MANAGEMENT OF SPILLS
[NOTE: PLEASE REFER TO THE SECTION ON BIOLOGICAL MATERIAL SPILLS IN THE ASU BIOSAFETY
MANUAL TO COMPLETE THIS SECTION.]
Inside of a containment device such as biosafety cabinet:
Alert the other laboratory employees;
Leave the cabinet turned on;
While wearing gloves, lab coat, and safety glasses, spray or wipe cabinet walls, work surfaces and
equipment with disinfectant equivalent to 1:10 bleach solution. If necessary, flood the work surface, as well as drain pans and catch basins below the work surface, with disinfectant for a contact time of
at least 20 minutes; Soak up disinfectant and spill with paper towels. Drain catch basin into a container. Lift front exhaust
grill and tray and wipe all surfaces. Ensure that no paper towels or solid debris are blown into the
area beneath the grill; Autoclave all clean-up materials before disposal in the biohazard waste container. Wash hands and
any exposed surfaces thoroughly after the clean-up procedure; and
Report the spill to the laboratory’s PI.
Small spills of infectious material outside of a containment device:
All spills must be reported to [the Principal Investigator].
All spills of any nature must be described in your laboratory notebook. The description must
include:
The name of the biohazardous agent and any identifying information (e.g., strain or other
characterization information); An estimate of the quantity released;
The time and duration of the release;

69
The environment into which the release occurred (e.g., in building or outside of building, waste
system);
The location [building, room] from which the release occurred;
The number of individuals potentially exposed at the facility;
Actions taken to respond to the release; and
Hazards posed by the release.
MANAGEMENT OF ACCIDENTAL EXPOSURES
In the event of an exposure to a biohazardous agent:
Intact skin
Remove contaminated clothing;
Vigorously wash contaminated skin for 1 minute with soap and water;
Inform the laboratory’s PI and seek medical attention at the ASU Campus Health Services.
Broken, cut, or damaged skin or puncture wound Remove contaminated clothing;
Vigorously wash contaminated skin for 5 minutes with soap and water; and
Inform the laboratory’s PI and seek medical attention at the ASU Campus Health Services.
Eye Immediately flush eyes for at least 15 minutes with water, using an eyewash;
Hold eyelids away from your eyeball and rotate your eyes so that all surfaces may be washed
thoroughly; and
Inform the laboratory’s PI and seek medical attention at the ASU Campus Health Services.
Ingestion or Inhalation Inform the laboratory’s PI and seek medical attention at the ASU Campus Health Services; and
Do not induce vomiting unless advised to do so by a health care provider.
MEDICAL SURVEILLANCE
Specific biohazards and toxins will be evaluated by [PI’s name] for appropriate medical surveillance
procedures. [Insert any applicable procedures].
TRAINING
[NOTE: PLEASE REFER TO THE SECTION TRAINING IN THE ASU BIOSAFETY MANUAL TO COMPLETE
THIS SECTION.]
Laboratory personnel shall demonstrate the following:
Understand the hazards associated with [the biohazardous agent];
Understand the required practices and procedures for working with [the biohazardous agent];
Know the necessary precautions to prevent exposures; and
Know the safety and security policies and procedures in place for reporting and investigating
unintentional injuries, spills, incidents (e.g., unauthorized personnel in restricted areas, missing
biologic agents or toxins, and unusual or threatening phone calls), or breaches in security measures.
This document will provide the basis of training.
[The PI] will provide information and training at the time of an individual's initial assignment to a work
area where biohazardous agents are present and prior to assignments involving new potential exposure situations. [The PI] will provide refresher training at least annually and when there are any changes in

70
processes or procedures. [Current training records and an outline of the training program can be found in
Appendix C.]
RECEIVING BIOLOGICAL AGENTS
[NOTE: PLEASE REFER TO THE SECTION ON RECEIVING BIOLOGICAL AGENTS IN THE ASU BIOSAFETY
MANUAL TO COMPLETE THIS SECTION.]
Biohazardous agents will be received into the laboratory by [insert procedure here].
EMERGENCY PHONE NUMBERS AND PROCEDURES
Emergency Phone Numbers [insert any additional contacts here]
Fire and Medical Emergencies 911
Police 911
Principal Investigator’s Home Phone xxx-xxxx
Campus Health 965-3346
Hospital Emergency Room xxx-xxxx
ASU Department of Public Safety 965-3456
Department of Environmental Health & Safety 965-1823
Emergency Procedures
[NOTE: PLEASE REFER TO THE SECTION ON EMERGENCY RESPONSE PROCEDURES IN THE ASU BIOSAFETY MANUAL TO COMPLETE THIS SECTION.]
Principal Investigators must be aware of the provisions for emergency procedures and preparedness.
Emergency procedures and preparedness must be incorporated into specific biosafety standard operating
procedures (SOP) for each biohazardous agent used in the laboratory. The Lab-Specific Biosafety Manual must address the following:
The hazards associated with the use of the biohazardous agent;
Personal protective equipment and emergency equipment;
Site security and control;
Emergency recognition and prevention;
Any hazards associated with response actions that could lead to a spread of a biohazardous
agent;
Roles of the laboratory faculty and staff in the event of an emergency;
Decontamination;
Emergency alerting and response procedures;
Emergency medical treatment and first aid;
Safe distances and places of refuge;
Evacuation routes and procedures;
Any additional special procedures needed to address the hazards of the specific agents; and
Reevaluate the ER Plan at least annually. Train employees and conduct exercises of the
emergency response plan at least annually.

71
SPECIMEN TRANSPORT
Biohazardous agents will be transported in the laboratory within a secondary container.

72
VALIDATION AND HISTORY FOR BIOSAFETY MANUAL
Principal Investigator’s Certification
I hereby certify that I have reviewed the contents of this manual and that it reflects my current operating
policy for the laboratories #[XXXX] and [YYYY] located in [Location] research building.
[Principal Investigator’s Name] [Principal Investigator’s Title] Signature Annual Review Date ________
Approvals
Department of Environmental Health & Safety
Signature: Date:
Department Chair
Signature: ______________________ Date: ___________________
Institutional Biosafety Committee Chair
Signature: ______________________ Date: ___________________
History of Manual’s Creation
Date Created:
Author:
Reference Source(s): [Insert P.I. NAME AND ANY APPLICABLE DOCUMENTS]

73
Appendix B-1: Floor Diagram
Include the location of sinks, eyewash, safety shower, spill kits, fire extinguishers, exits, MSDS and phones.

74
Appendix B-2: Health Hazard Assessment Worksheet
Instructions to Principal Investigators (PI) Conducting a Health Hazard Assessment for biological or select agents at ASU Laboratories
Before completing this Health Hazard Assessment (HHA), please review the ASU Biosafety Manual. In addition, it may be helpful to refer to the Public Health Agency of Canada’s MSDS website.
Complete all sections accurately of the attached worksheet. This information must be included in the Lab-Specific
Biosafety Manual. If you have any questions on completing these procedures, please contact Environmental Health & Safety, (480) 965-1823, for additional assistance.
The Principal Investigator (PI) is responsible for initially assessing health hazards in order to set the biosafety level for the work to be done. This must be done in close collaboration with Environmental Health & Safety and
Animal Care (if applicable) to ensure compliance with established guidelines and regulations. The PI should be aware of the following factors prior to conducting the HHA:
1. Biological, chemical, and physical hazards in the laboratory 2. Principles of biological, chemical, and physical safety
3. Method of transmission of various infectious agents o Direct versus Indirect Contact
Direct contact (i.e., between humans, between humans and animals)
Indirect contact through common environmental surfaces (e.g., lab benches, equipment) o Airborne versus Vehicle
Airborne (i.e., inhalation of particles into the respiratory system) Vehicle (i.e., sharps)
o Vectors
Vector-borne (e.g., insects, mites, fleas) 4. Route of Infection
o Ingestion o Inhalation
o Inoculation o Penetration of abraded skin or mucous membrane through skin (e.g., cuts, abrasions)
o Bites (animals or insect) Contact with mucous membranes of eyes, nose, and mouth
5. Biological Agent o Pathogenicity (severity of ability to cause infection). The virulence of microorganisms varies
greatly among types and strains. [Some microbes are highly pathogenic, even in healthy adults, while others are opportunistic and only able to infect hosts with a lowered immunity.]
o Infectious or intoxicating dose (i.e., the number of microorganisms required to initiate an
infection). o Effect of route of exposure (infectious dose and intoxicating dose vary with route of exposure).
o Virulence (primary or secondary communicability) of microorganisms varies greatly among types and strains.
o Host susceptibility or resistance (genetic composition, age, gender, race). Conditions that alter
host defenses at body surfaces or impair the functioning of the immune system my put a worker at increased risk.
o Biological modifiers to resistance (preexisting condition, secondary infection, pregnancy, stress, immunosuppression, vaccination).
o Viability. If the agent is not viable and able to replicate, possibility of infection does not exist. o Sensitization reactions (allergen, acute hypersensitivity).
o Incidence of laboratory infections.
o Treatment (success rate considering various routes of exposure and doses, antibiotic resistance and susceptibility).
o Environmental impact (survival and dissemination in the environment, remediation, public health concerns, impact on humans, flora and fauna).

75
o Unique animal hazards:
Species ectoparasite vectors (fleas, ticks, lice). Species specific in apparent infections (SIV, Monkey B Virus, TB, Hepatitis).
Agent excretion in urine, feces, saliva, blood (offspring) transmission. Escape from facility.
6. Environmental Factors
o Ventilation and laboratory design (directional air, pressure gradients, air breaks, separation of laboratories from offices, interlocking autoclave and airlock doors).
o Laboratory procedures (use of sharps, mouth pipetting, minimization of creating aerosols). o Containment equipment (Class II and III biosafety cabinets, sealed centrifuges cups and rotors).
o Personal protective equipment (gloves, goggles, respirators, aprons, gowns). o Training (handling, containment, destruction and transporting pathogens, emergency evacuation,
spill procedures).
o Laboratory sanitation (decontamination, housekeeping, disinfection, routine cleaning, pest and rodent control).
7. Effects of aerosol-generation in the lab o How aerosols act as modes of transmission for infectious agents and chemical vapors?
o What procedures are likely to cause aerosols?
o What methods can be used to reduce or contain aerosols? 8. Essential safety features necessary to lab operations
o Air handling system. o Safety equipment.
o Adequacy and limitations for decontaminating waste. 9. Type of medical surveillance needed based on each employee's job duties. A medical surveillance
program ensures that safeguards decided upon in fact produce the expected health outcomes. It may
include serum banking, monitoring employee health status, and participating in post-exposure management.
10. How the facility, equipment, personnel, procedures, and hazardous materials must be integrated to create a safe work environment.
11. Local, state, and federal regulations under which the lab operates.
12. Concentration. The number of infectious organisms per unit volume is important to know because an increase in the working volume of high-titered microorganisms increases the risk of infection.
13. Origin. This refers to the geographic location, natural host, or the nature of the source. 14. Availability of data from animal studies.
15. Availability of an effective prophylaxis or therapeutic intervention.
16. Experience and skill level of “at-risk” personnel.
In the United States, the most current classification of biological agents is found in the National Institutes of Health (NIH) Guidelines for Research Involving Recombinant DNA Molecules (NIH Guidelines), May 1999. The
NIH Guidelines classify biological agents (see Table below) known to infect humans as well as select animal
agents that may pose theoretical risk if inoculated into humans. Risk Groups established by the NIH correspond to the Biosafety Levels established by the Centers for Disease Control (CDC).

76
Transmission of Disease
It is important to understand how an infectious disease is transmitted before conducting any work with an agent
of the disease. This should be noted in the PI’s Health Hazard Assessment. The interactions among the biological agent, human, and environment do not always result in disease and/or death. For an infection or illness to occur
in a human, the following conditions must be met:
The biological agent must be capable of causing disease;
There must be a reservoir of sufficient number for the agent to live and reproduce;
The agent must be able to escape the reservoir;
The agent must be able to move through the environment (e.g., airborne, contact, vectors);
There must be a means of transmission into the host (e.g., broken skin, inhalation, blood transfer,
mucous membrane); and
The human must be susceptible to the agent.
Every biosafety control strategy is intended to break one or more of the links in the transmission chain. One of
the basic principles of biosafety is performing a Health Hazard Assessment (described in Administrative Controls),
which involves understanding how an agent is transmitted to humans.
Direct Transmission
Direct transmission from host to host occurs anytime an infected host transmits the disease to a susceptible host
by any number of means. The most frequent portal of entry into the human body occur at sites where mucous membranes meet with the skin, including respiratory (upper and lower airways), gastrointestinal (primarily
mouth), genital, and urinary tracts. Abnormal areas of mucous membranes and skin (e.g., cuts, burns, and other injuries) are also frequent sites of direct transmission.
Indirect Transmission
Indirect host-to-host transmission occurs by either living or inanimate means. Living agents transmitting infection
are called vectors; they are generally arthropods (e.g., insects, mites, fleas) or vertebrates (e.g., dogs, rodents). Arthropods may not actually be hosts for the disease but rather carriers. Indirect transmission by a living agent
may occur from patient to patient on the hands of health care workers.
Inanimate objects such as bedding, toys, books, or surgical instruments may also transmit disease. These
inanimate objects are collectively called fomites. If the inanimate object is food, water, or air, it is referred to as a disease vehicle.

77
Steps for completing the Health Hazard Assessment:
1. Identify the agents to be used;
2. Gather and evaluate existing data on the agents looking at the factors listed above; 3. Evaluate ways the agents can escape containment;
4. Determine the training required of personnel handling the agent;
5. Determine proper lab procedures; 6. Determine personal protective equipment required;
7. Determine safety equipment and containment needs; 8. Assess the capability of each facility to contain the material during normal and emergency situations
9. Determine potential exposure limits;
10. Consider whether the acceptance of risk is voluntary or imposed; 11. Recognize factors that give the illusion of no risk (e.g., unknown history of the agent, lack of toxicity
testing); 12. Fill out the Environmental Health & Safety Health Hazard Assessment Worksheet (attached below); and
13. Include your completed Health Hazard Assessment Worksheet in your Lab-Specific Biosafety Manual.
(There are several systems for classifying human and animal pathogens. All systems are based upon the
pathogenicity of the organism, mode of transmission, host range, availability of effective preventative measures and/or effective treatment.)

78
Please fully complete each section.
1. Agent Identification
Name (genus/species):
Type of Agent (check all that apply)
Bacterium:
Parasite: Fungus:
Rickettsia: Prion:
Toxin derived from living organism: Virus:
Recombinant DNA:
For recombinant DNA, the following questions must be answered:
1) Does the inserted gene encode a known toxin or a relatively uncharacterized toxin?
No: Yes: If yes explain:
2) Does the modification have the potential to alter the host range or cell tropism of the virus?
No: Yes: If yes explain:
3) Does the modification have the potential to increase the replication capacity of the virus?
No: Yes: If yes explain:
4) Does the inserted gene encode a known oncogene?
No: Yes: If yes explain:
5) Does the inserted gene have the potential for altering the cell cycle?
No: Yes: If yes explain:
6) What is the probability of generating replication-competent viruses?
No: Yes: If yes explain:
2. Health Hazards
Disease(s) caused by agent:
Pathogenicity:
Species:
Potential pathogen:
Principal Investigator: Phone No:
Department: Fax No:
Building, Room, Mail
Code: Email:

79
Pathogenic:
Highly pathogenic:
Opportunistic pathogen:
Other:
Epidemiology:
Host Range (check all that apply):
Humans:
Animals: Specify:
Plants: Specify:
Concentration (number of organisms per unit volume):
Infectious Dose:
Known:
Unknown:
Mode of Transmission (check all that apply):
Direct Contact:
Human/human:
Human/animal:
Indirect Contact:
Vector-borne:
Inanimate objects:
Food, water, air:
Airborne:
Vehicle:
Vector:
Route(s) of Entry: (check all that apply)
Ingestion:
Inhalation:

80
Penetration through skin:
Contact with mucous membranes of eyes, nose, and mouth:
Incubation Period:
Dissemination:
Reservoir:
Zoonosis:
No:
Yes: Name:
Vectors:
None:
Yes: Name:
Viability:
Drug Susceptibility:
Drug Resistance:
Disinfectant Susceptibility:
Physical Inactivation:
Survival Outside Host:
Medical:
Surveillance/ known symptoms of infection:
First Aid/Treatment:
Immunization:
Prophylaxis:
Laboratory Hazards:
Laboratory-Acquired Infections (epidemiology of lab-acquired infections):
Sources/Specimens:
Primary Hazards:
Flammable: Reactive: Carcinogenic: Toxic: Corrosive: Oxidizer:

81
Special Hazards:
Recommended Precautions:
Containment Requirements:
Personal Protective Equipment:
Staff Trained and Experienced with Agent:
Other Precautions:
Handling Information:
Spills:
Disposal:
Storage:
Miscellaneous Information:
Congratulations! You now have a material safety data sheet for your biological agent.
Principal Investigator’s Signature
Title: Date:
Updated:
Please forward a copy of this form to Environmental Health & Safety, Mail Code 5412

82
Appendix B-3: IBC Application Documentation
Insert the completed and approved EHS 112 form(s) at this appendix.

83
Appendix B-4: Suggested Format for the Lab-Specific Biosafety Manual
According to federal regulations, all laboratories using biohazardous materials must have a Lab-Specific Biosafety Manual. This manual must be adopted as policy and be accessible to all laboratory personnel. To help the Principal Investigators comply with these regulations, the Biosafety group at ASU has developed documents and
templates that should be incorporated into the Lab-Specific Biosafety Manual. Each laboratory should have a
binder available that includes the following documents in addition to any supplemental materials the Principal Investigator feels will augment the safe and proper handling of biohazardous materials in their laboratory.
1. ASU Biosafety Manual − Every laboratory operating at BSL2 or BSL3 must have a copy of this manual
available.
2. NIH Guidelines Research Involving Recombinant DNA − Laboratories that work with recombinant DNA must have a copy of these guidelines available.
3. Institutional Biosafety Committee (IBC) Disclosures – It is recommended that all approved IBC disclosures be made available to laboratory personnel.
4. Biosafety Inspection Reports − EHS performs annual biosafety inspections and provides a report to the
Principal Investigator. Please make this report available to laboratory personnel. Principal Investigators may also perform their own self-inspection using the Biosafety Inspection Checklist.
5. Lab-Specific Biosafety Training Checklist − All personnel in the lab should fill out this document and keep copies available.
6. Biological Inventory − Each laboratory should maintain a list of all biological organisms that may be present, including known hazards for each organism. Biological material safety data sheets (MSDS) or
fact sheets provided by the manufacturer should also be provided when available.
7. HBV Vaccine Declination Forms − Personnel who work with human blood, human blood products, or any unfixed human tissue must be provided Hepatitis B Virus vaccinations, free of charge. If personnel
decline the vaccination, the HBV Vaccine Declination Form must be signed and maintained. 8. Emergency Contacts − A list of all laboratory personnel and contact information should be recorded and
made available.
9. Standard Operating Procedures (SOPs) − SOPs relevant to the laboratory must be written and made available to lab personnel. Examples include the Biosafety Cabinet SOP and Autoclave Operation SOP.
Other SOPs may be developed for Emergency Spill Clean-up, Biohazardous Waste Disposal, Accident/Incident Reporting, Transporting Biological Materials, Safe Handling of Sharps, Post-exposure
Medical Surveillance, or use of specific equipment in the lab.
Please keep these materials in your laboratory and available to all lab personnel. Annual biosafety inspections will
require the laboratory to produce these documents in accordance with federal regulations. If you have any questions about your Lab-Specific Biosafety Manual, please contact [email protected].

84
Appendix C: Special Considerations for Select Agents and Toxins
SELECT AGENT AND TOXIN REGULATORY INFORMATION
The ASU Biosafety Manual is applicable to all laboratories, research, service and support activities that use or
store select agents or toxins that are regulated by DHHS and/or the USDA. The information presented in this
manual reflects the requirements and guidelines of federal regulations. Each Principal Investigator will supplement this information with written procedures, instruction and guidance regarding specific practices and
procedures unique to the work being done in the laboratory with select agents and toxins.
REGULATORY REQUIREMENTS
Registration Process at ASU
Arizona State University is prohibited from possessing, using, receiving, or transferring select agents or toxins
unless ASU has been granted a certificate of registration by the DHHS Secretary or the USDA Secretary. If a PI from any ASU laboratory would like to apply for a certificate of registration, the PI must contact the Office for
Research Integrity and Assurance (ORIA) and complete the Proposal Routing and Approval Form in addition to
completing the 112C form. These are submitted through a process to the IBC, Animal Care (if required), EH&S, and ORIA. The request to conduct research with a select agent is a lengthy one and involves a requirement for a
compliant facility as well as completion of a site-specific security plan and an agent specific safety plan. These templates and procedures exist, and the EH&S department is ready to assist a PI to navigate this process.
Once approved by the ORIA/IBC, the ASU Responsible Official (RO) will begin the process to obtain a registration
application number from the DHHS or USDA secretary and will submit the application once it has been completed
by the RO in conjunction with the PI. The information requested by DHHS or USDA will be used to determine whether or not ASU will be allowed to conduct activities with the select agent or toxin.
Once the application is approved, the certificate of registration will be valid only for the specific select agents
and/or toxins, and the specified activities and locations that are consistent with the information provided by ASU
upon which the certificate of registration was granted. The RO must promptly notify the DHHS or USDA Secretary, in writing, if a change occurs in any information previously submitted to the DHHS or USDA Secretary.
This includes modifications to the list of individuals approved, changes in area of work, protocols, or objectives of studies.
The certificate of registration will cover activities at only one general physical location (a building or a complex of buildings at a single mailing address). Unless terminated sooner, a certificate of registration will be valid for up to
three years. To obtain a new certificate of registration, ASU must submit a new application.
Security and Emergency Response Requirements
Security and emergency response are very important components of the select agents and toxins regulations and must be an integral part of storing and handling these agents and toxins. Requirements regarding the items in
the following list can be found in the appendix of this manual titled ASU Laboratory Security Guidance for
Laboratories Working with Select Agents:
Physical security;
Data and IT system security;
Security policies for personnel;
Policies for accessing select agent areas;
Specimen accountability;
Receipt of select agents into the laboratory;
Transfer or shipping of select agents from the laboratory (refer to the previous section);
Emergency response plans (refer to the section on emergency response procedures;
Reporting of incidents, injuries, and breaches; and
Recordkeeping

85
Training
The PI, in conjunction with the RO, must provide information and training on safety and security for working with biohazardous and select agents and toxins to each individual approved for access to his/her laboratory and each
unapproved individual working in, or visiting, areas where select agents and toxins are handled or stored. The PI must ensure that all individuals who work in, or visit, the areas understand the hazards of select agents and
toxins present in the area. This training program must be included as part of their Lab-Specific Biosafety Manual and be documented with a signature and date to indicate that each individual was trained. Training records will
kept on file for 3 years.
The PI must provide information and training at the time of an individual's initial assignment to a work area
where select agents or toxins are present and prior to assignments involving new exposure situations. The PI must provide refresher training annually and when there are any changes in processes or procedures.
Audits and Compliance
The Responsible Official, or his or her designee, will conduct regular inspections, at least annually, of each laboratory where select agents or toxins are stored or used to ensure compliance with the procedures and
protocols of this manual. Inspection reports will document violations and be directed to the PI. The results of these inspections with select agents and toxins will be documented and kept on file with the Responsible Official.
Program Evaluation
Program evaluation is conducted annually based upon the effectiveness of this plan. The Select Agent and Toxin Program measurements must be reviewed, performance tested and updated annually. The plan must also be
reviewed and revised as necessary after any incident. Any program evaluation report for laboratories containing select agents and toxins is written by the RO.