Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics...
-
Upload
medicsindex-telepin-slidecase -
Category
Documents
-
view
220 -
download
0
Transcript of Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics...
-
8/14/2019 Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics Index Mem
1/11
Behavior of Radial Fo rearm S kin Flaps Transplanted
into the Oral Cavity
D. BADRAN,1 D.S. SOUTAR,2 A.G. ROBERTSON,3 O. REID,1 E.W. MILNE,1 S.W. MCDONALD,1*
AND R.J. SCOTHORNE1
1Laboratory of Human Anatomy, University of Glasgow, Glasgow, United Kingdom2Department of Plastic and Reconstructive Surgery, Canniesburn Hospital, Glasgow, United Kingdom
3Beatson Oncology Centre, Western Infirmary, Glasgow, United Kingdom
Radial forearm skin flaps transplanted into the oral cavity in patients undergoing treatment forintra-oral tumors frequently acquire a gross appearance resembling that of buccal mucosa. Thisarticle reports studies of biopsies of the flaps in 53 patients, of which 21 showed changes atsome stage in the follow-up period. The project aims to determine whether 1) the change in theepithelium to a mucosal form is genuine or reactive, 2) a creeping replacement of epidermisresults from the surrounding buccal epithelium, 3) alterations in the epidermis could beassociated with changes in the dermis, 4) the change is caused by radiotherapy. Examination ofthe biopsies by resin histology and transmission electron microscopy shows that the changesmay be reversible: it suggests that they are reactive in nature, and related to the degree ofdermal inflammation, rather than to the effect of radiotherapy. The dermis persists as such andis not replaced by buccal lamina propria. Clin. Anat. 11:379389, 1998. 1998 Wiley-Liss, Inc.
Key words: skin fl aps; epidermis; hist ological features; radiotherapy; inflamma-
tion; reactive changes ; reconstructive surgery
INTRODUCTION
The Plastic and Reconstructive Surgery Unit atCanniesburn Hospital is the regional center to whichmost patients with oral tumors in the West of Scotlandare referred. Treatment usually involves excision ofthe tumor and reconstruction using a free radialforearm skin flap (Soutar et al., 1983) combined withradiotherapy (Robertson et al., 1985, 1986), dependingon the tumor stage (UICC, 1987).
During follow-up, it is frequently found that theflap changes in color and texture and, on naked-eyeinspection, resembles the buccal mucosa. The changewas common in patients who had received radiother-apy. The reason for the changed appearance of the flapis unclear. The question is of both biological and clin-ical interest. If the intraoral skin flap were to assumepermanently the characteristics of the oral mucosa, i.e.,of the recipient site, the change would be acceptable,both functionally and cosmetically, to the patient andto the surgeon. There are previous claims of such achange: Lawson (1985), discussing the use of pectoralismajor myocutaneous flaps in oral cavity reconstruction,states that the epithelium changes from keratinizingto non-keratinizing epithelium resulting in a pseudo
mucous membrane consistency with time. Biologi-
cally, however, such a change would be very surprising,in view of the abundant experimental evidence thatthe maintenance of the regional characteristics of anadult epithelium is dependent, in part, on influences ofthe subjacent connective tissue and, in part, on regionalvariations in the competence of the epithelium to re-spond to these influences (Billingham and Silvers, 1968;Mackenzie and Hill, 1984; Hill and Mackenzie, 1984;Sengel, 1986; Coulomb et al., 1989). Since the radial fore-arm flap consists of epidermis and its associated dermisand hypodermis, one would expect the graft to retainsome, at least, of the characteristics of the donor site.
This study aims to answer the following questions:
1) Is the alteration in the appearance of the epithe-lium to a mucosal form a genuine or a reactivechange?
2) Is there a creeping replacement of the epidermisby surrounding (host) buccal epithelium?
*Correspondence to: Dr. S.W. McDonald, Laboratory of HumanAnatomy, University of Glasgow, GLASGOW, G12 8QQ.
Received 30 June 1997; Revised 25 September 1997
Clinical Anatomy 11:379389 (1998)
19 98 Wiley-Liss, Inc.
Member at www.medicsindex.com
-
8/14/2019 Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics Index Mem
2/11
3) Is the native dermis of the graft replaced bybuccal stroma, which might then reinstruct theoverlying epithelium to assume buccal character-istics?
4) Is the change caused by radiotherapy?
MATERIALS AND METHODS
Patients
The patients in this study, which extended for 30months, fell into 2 groups; Group 1: 40 patients alreadybeing treated for intraoral tumors at the start of thestudy, Group 2: 13 patients who presented for treat-ment during the period of the study.
Group 1
Group 1 consisted of 25 males and 15 females,selected because of the suitability of their flaps forbiopsy and their willingness to participate in the study.At the time of surgery, their ages ranged from 2981years. Thirty-eight of the patients had had a squamouscell carcinoma of the oral epithelium; in the other twothe diagnosis was adenocarcinoma and acinic cellcarcinoma. Twenty-five patients had received a courseof postoperative radiotherapy in the the form of 6,000cGy in 30 fractions over 6 weeks. A further three hadreceived a similar course preoperatively and 12 pa-tients were treated by surgery only.
At the start of the study, a biopsy of the flap wascollected from all patients and, in six individuals, a
sample of lining (i.e., non-keratinized) buccal mucosawas also obtained. A second biopsy of the flap wassubsequently taken in six patients.
Group 2
Group 2 consisted of 9 males and 4 females agedbetween 35 and 75 years. All were diagnosed as havingsquamous cell carcinoma of the oral epithelium. Inaddition to surgery, nine patients received radio-therapy as described above. One had previously hadradiotherapy and, like the other three subjects whohad early tumors, received surgery only.
At transplantation, samples of skin were collected
from all flaps. They were immediately fixed in 3%glutaraldehyde in Millonigs buffer (pH 7.4) and pro-cessed into resin. Sections 1 m thick were stainedwith Azur II, resorcin fuchsin or periodic acid-Schiffand hematoxylin.
Biopsy
Biopsies were taken with the informed consent ofthe patient and the approval of the Hospital EthicalCommittee.
Under local anesthesia, a fusiform biopsy was takenfrom the graft. All samples were processed as de-scribed above.
The degree of inflammation in the dermis wasassessed on the following scale:
Grade 0: occasional inflammatory cells,Grade 1: scattered inflammatory cells,Grade 2: small aggregates of inflammatory cells,Grade 3: large aggregates of inflammatory cells,Grade 4: diffuse inflammatory reaction,Grade 5: connective tissue components masked by
inflammatory cells.
Transmission Electron Microscopy
Sections for electron microscopy were obtained on aReichert-Jung Ultracut E microtome using standardtechniques (Weakley, 1981) and examined on a Philips
EM301 transmission electron microscope.In the analysis of the light and electron microscopi-
cal material only qualitative observations were used.
RESULTS
Gross AppearanceGroup 1. The 40 patients in Group 1 had received
treatment up to 8 years before the start of the project.When the study commenced, the flaps in 28 of thesepatients looked like normal skin (Fig. 1), whereas inthe remaining 12 subjects they resembled adjacentbuccal mucosa in whole (Fig. 2) or in part (Fig. 3). In
the 15 patients treated by surgery only, 5 flapswere changed in appearance, whereas in the 25 who
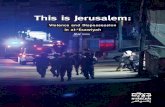
Figs. 14 show the transplanted radial forearm skin flaps of four
different patients.
Fig. 1. Non-irradiated radial forearm flap 1 year after surgery. The
flap has retained the appearance of forearm skin.
3 8 0 Badran e t al.
Member at www.medicsindex.com
-
8/14/2019 Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics Index Mem
3/11
received surgery and radiotherapy, 7 flaps werechanged.
One patients flap developed the appearance ofbuccal mucosa during the 30 months of the study; thisoccurred 8 years after operation. During the study, 5changed flaps (3 irradiated and 2 non-irradiated)showed a partial return to the appearance of normalskin. A further 3 flaps (1 irradiated and 2 non-irradiated) acquired a silver-white color (Fig. 4).
In flaps showing partial change, some of the changedareas were peripherally, others centrally, placed. Thisobservation argues against creeping replacement of
the graft epithelium by buccal epithelium, whichwould have resulted in the changed areas lying at theperiphery of the graft. In flaps which had completely
acquired the appearance of buccal mucosa, a fine scarindicated the margins of the flap. Hairs were seen inmany of the flaps of patients treated by surgery only,but they were absent following radiotherapy.
Group 2
Four of the 13 patients in Group 2 were treated bysurgery only; their flaps retained the appearance ofskin throughout the study. Of the 9 irradiated patients,the flap of one soon recovered from the radiation andhad the appearance of normal skin. The flaps in theother 8 developed, in whole or in part, a silver-white
surface and 2 of these had regained the appearance ofskin by the end of the study.
Table 1 correlates the number of patients in Groups1 and 2, whose flaps did or did not show changes at anytime during the study, with treatment involving radio-therapy. Changed flaps were more common followingradiotherapy but were also seen in patients treated bysurgery only. Chi-squared test showed no significantdifference between the two regimes of treatment(Chi-squared 0.80; df 1).
Light Microsco py
Forearm skin. Biopsies of forearm skin were ob-
tained at the time of initial operation from all 13patients in Group 2. The appearances were typical of
Fig. 2. Non-irradiated flap (arrows) 7 years after surgery showing
a surface similar to buccal mucosa.
Fig. 3. Non-irradiated flap (arrows) 3 years after surgery. This flap
had previously shown more extensive change towards the form of
buccal mucosa. Keratinized areas have become more extensive. Hairs
are present in the areas with the appearance of skin.
Fig. 4. Flap (arrows) which had developed a silver-white surface
6 months after radiotherapy.
TABLE 1. Number of Changed and Unchanged FlapsFollowing Treatment by Surgery Only and in Combinationwith Radiotherapy
Surgery Only Surgery Radiotherapy Total
Unchanged 13 19 32Changed 6 15 21Total 19 34 53
Be havi or of S k i n F laps i n O ral Cavi ty 381
Member at www.medicsindex.com
-
8/14/2019 Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics Index Mem
4/11
thin skin (Fig. 5); the epidermal/dermal interface wasplane; few mitotic figures were visible in the stratumbasale; the stratum spinosum was 35 cells thick andthere was no stainable glycogen; the stratum granulo-sum was 23 cells thick and the stratum corneum
formed a thin layer and showed the typical basketweave pattern. In the dermis, occasional inflammatorycells, mainly lymphocytes, were seen (Grade 0). Hairfollicles, sweat glands, and their ducts were seen in allsamples but sebaceous glands were identified in only 3samples. In the reticular dermis, fiber bundles wereirregular in orientation and closely packed whereas, inthe papillary dermis they were less densely arranged.
Buccal Mucosa
Nineteen biopsies of oral mucosa, of the lining(non-keratinized) variety, were obtained from patientsin Groups 1 and 2 (Fig. 6). The epithelium was 34
times thicker than the epidermis, and the superficialand middle layers were rich in glycogen. The mostsuperficial cells retained pyknotic nuclei (parakerato-sis) but there was no true stratum corneum, nor was a
stratum granulosum seen in any sample. In the lamina
propria, a few inflammatory cells, mainly lymphocytesand neutrophils, were seen (Grade 01). The collagenand elastic fibers were irregularly arranged and lessclosely packed than in the dermis of forearm skin.Some samples showed accessory salivary glands.
Intraoral Radial F orearm Flaps
In total, 77 biopsies were obtained from the flaps ofpatients in Groups 1 and 2. On the basis of their grossappearance, the flaps could easily be classified aschanged or unchanged. The histological appearance ofthe following groups of flaps will be described sepa-rately:
1) postoperative period before radiotherapy,2) unchanged; irradiated and non-irradiated,3) changed; irradiated and non-irradiated,4) partial reversion to appearance of skin, after
mucosal change; irradiated and non-irradiated.
Postoperative Period Before Radiotherapy
Biopsies were taken from four patients 1820 daysafter operation and before radiotherapy. Grossly, the
Figs. 510 are all photomicrographs of vertical resin sections,
stained with Azur II,125.
Fig. 5. Resin section of thin skin of radial forearm flap at time of
surgery. Sweat glands (S) and a hair follicle (F) are indicated.
Fig. 6. Buccal mucosa. The epithelium is thicker than that of flap
skin. There is no stratum corneum.
3 8 2 Badran e t al.
Member at www.medicsindex.com
-
8/14/2019 Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics Index Mem
5/11
flaps had the appearance of skin and absorbablesutures lay at their margins. On histological examina-tion, the epidermis was thickened by about 3 times (cf.Figs. 5 & 7). The stratum basale showed little change,with few mitoses. The stratum spinosum was hypertro-phic, with more cell layers, enlarged cells and nuclei,and widened intercellular spaces, with prominentspines. The cytoplasm was more basophilic and, in themore superficial spinous layers, was rich in glycogen.The stratum granulosum varied between the biopsies:in one, keratohyalin granules and ghosts of nuclei wereseen in the horny layer. The stratum corneum of thefourth biopsy resembled that of thin skin.
The epidermal-dermal interface was undulating inall samples, with deep rete ridges and high dermalpapillae. In all, the papillary dermis showed scatteredinflammatory cells (Grade 1), mainly lymphocytes anda few plasma cells. The deeper part of the reticulardermis showed dilated capillaries surrounded by a fewinflammatory cells. Hair follicles and sweat glandswere seen in all samples but none showed sebaceousglands.
Unchanged Flaps
A total of 36 biopsies was obtained from theunchanged flaps of patients in Groups 1 and 2 (Fig. 8).Eighteen of the biopsies were from irradiated subjects,18 from the 15 non-irradiated patients. There were no
obvious differences in epidermal structure betweenthe irradiated and non-irradiated groups. Most speci-mens showed regression of the hypertrophic changesseen in the postoperative group, but a few still showedthickening of the stratum spinosum, with glycogen inits superficial layers. In all biopsies, the stratumgranulosum was reduced to 35 cell layers, but therewas mild hyperkeratosis in the stratum corneum insome samples.
In four specimens from irradiated patients, theinterface between the epidermis and dermis wasplane. In the dermis of some irradiated flaps, collagenbundles were less closely packed than in healthy
forearm skin and elastic fibers were more numerous,thicker and more tortuous and randomly orientated.Fibroblasts showed characteristic enlargement in irra-diated flaps. All flaps showed mild or no inflammatoryreaction in the dermis (Grade 02). In the reticular
Fig. 7. Postoperative biopsy of flap, 20 days after transplantation.
Compared to thin skin, the epithelium is thicker, particularly in the
stratum spinosum where intercellular spaces are prominent. The
epidermal-dermal interface is undulating.
Fig. 8. Section of unchanged non-irradiated flap, 64 months after
transplantation. The histological appearance resembles thin skin. An
arrector pili muscle (M) is visible.
Be havi or of S k i n F laps i n O ral Cavi ty 383
Member at www.medicsindex.com
-
8/14/2019 Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics Index Mem
6/11
dermis, inflammatory cells, when seen, were mostlylymphocytes and were largely perivascular in position.Blood and lymphatic capillaries were dilated in allsamples and endothelial cell swelling was seen in theblood capillaries of the irradiated material. Hair fol-
licles were seen in biopsies from 7 of the 15 non-irradiated patients but were not found following radio-therapy. Sweat glands and/or ducts were seen in allbiopsies from non-irradiated flaps but in only 12biopsies from the 18 irradiated subjects; because ofdifficulty of access, the biopsies of some of theirradiated flaps may not have been deep enough toshow sweat glands. Sebaceous glands were not seen inany sample.
Changed Flaps
Twenty-one of the 53 patients in the study showedchanges in their flaps (Figs. 2 & 3); 6 had been treated
by surgery only and 15 had received postoperativeradiotherapy.
The epidermis was markedly thicker than in thinskin and in many flaps it had deeper rete ridges and anindistinct stratum corneum (Fig. 9). A few lympho-cytes and neutrophils infiltrated the epithelium.
In the stratum basale, mitotic figures were morenumerous than in forearm epidermis and in theunchanged flaps, numbering 24 per high power field.The basal keratinocytes were widely separated.
The stratum spinosum was markedly increased inthickness in all flaps. Occasional mitotic figures wereseen in the basal parts of this layer. In the deeper parts,
adjacent cells made contact at prominent spines pro-jecting into wide intercellular spaces (spongiosis). Thecells of the more superficial layers of the stratumspinosum were closely packed and the spaces betweenthem almost absent. These cells were enlarged andhad a higher glycogen content than those in the lowerlayers. Vesicles were noted in the upper part of thestratum spinosum in recently irradiated flaps.
The stratum granulosum was variable, absent insome parts and thinner than in forearm skin in others.
Parakeratosis was a common feature of these flaps,both irradiated and non-irradiated, and a few nucle-ated cells sloughed from the surface. Some flapsshowed thin flakes of anucleate cornified cells. Vesicleswere noted in the stratum corneum of irradiated flaps.
The dermal-epidermal interface of some biopsieswas highly undulating, with high connective tissuepapillae. The basement membrane appeared intact insections stained by the PAS technique. In someirradiated flaps, dermal elastic fibers were abundant,thickened, tortuous, and randomly distributed.
Variable grades of inflammatory reaction occurred inthe dermis (Grades 25); in some flaps it was so severe
that it masked the dermal components. The inflamma-tory cells were mainly plasma cells and lymphocytes;many were in perivascular positions. In the deeperdermis, occasional mast cells were seen. In threesamples (2 recently irradiated and 1 non-irradiated)the reticular dermis contained large numbers of extrava-sated erythrocytes. The deep part of the reticulardermis of irradiated flaps was more cellular than innon-irradiated ones. Giant fibroblasts were seen in theirradiated samples. Blood and lymphatic capillariesappeared dilated in all flaps. Hair follicles were ob-served in two of the non-irradiated flaps but in none ofthose subjected to radiotherapy. Sweat glands and/ortheir ducts persisted in all non-irradiated flaps but inonly 9 of the 15 irradiated flaps.
Flaps Showing Partial Reversion
During the routine follow-up of the patients, anumber of flaps which had wholly or partially acquiredthe appearance of oral mucosa subsequently revertedto the appearance of skin. In some the areas resem-
Fig. 9. Section of a flap, 26 months after transplantation, whose
gross appearance resembled buccal mucosa. The epithelium is mark-
edly thickened and the interface between it and the underlying
connective tissue is highly undulating. The connective tissue compo-
nents are masked by the presence of large numbers of inflammatory
cells (Grade 5). This flap had not been irradiated.
3 8 4 Badran e t al.
Member at www.medicsindex.com
-
8/14/2019 Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics Index Mem
7/11
bling oral mucosa were smaller, in others they ap-peared silver-white.
1) Reduction in Siz e of the Changed Area
Biopsies were taken from four flaps which showed
partial reversion from a previous biopsy at the samesite. Three were from irradiated patients and one wasfrom a non-irradiated patient. Biopsy material camefrom reverting areas of these flaps.
The histology resembled that described for thechanged flaps; there were, however, some differences:
1) Although still increased in thickness comparedwith thin skin, the epithelium was thinner thanin the previous biopsies.
2) In the stratum basale, mitotic figures appearedfewer than in the earlier biopsies.
3) In the earlier biopsies of two of these flaps, the
stratum granulosum had been absent but waspresent in the later biopsies.
4) In some of the later biopsies the stratum cor-neum had become well-defined.
5) Dermal inflammation was reduced in the biop-sies of three of the four flaps. Two of theirradiated specimens showed Grade 4 at the firstbiopsy but Grade 3 at the second. The non-irradiated flap had originally shown Grade 5 butthe later biopsy showed Grade 4.
2) Silver-white Appearance
Thirteen biopsies were taken from the flaps which
had acquired a silver-white appearance (Fig. 4): 11were from irradiated flaps and two were from non-irradiated ones. The two non-irradiated and one of theirradiated specimens were collected from Group 1patients. The other 10 irradiated specimens came fromGroup 2 patients, two of whom had repeated biopsies.An earlier biopsy, before the silver-white color devel-oped, had been taken from some of these patientsallowing comparison of the flap histology before andafter the development of the silver-white appearance.The histology of the flap when showing the silver-white appearance (Fig. 10) was generally similar tothat described earlier for the changed flaps. Somedifferences were observed, however:
1) The epithelium was thicker than in thin skin,but for those flaps from which a previous samplewas available, it had become thinner since theearlier biopsy.
2) The stratum corneum remained parakeratotic,but many parakeratotic cells were loosely at-tached to the surface, either as single cells or inclusters. The silver-white appearance was attrib-
uted to these features which resembled thelesions of psoriasis.
3) In the six individuals with previous biopsies,mitotic figures were less frequent in the stratumbasale of the biopsies with the silver-whiteappearance.
4) In the six flaps previously biopsied, the laterbiopsies of five showed reduction of dermalinflammatory reaction.
Electron Microscopy
This part of the study aimed to determine whether,at the ultrastructural level, the flap epithelium re-sembled that of skin or buccal mucosa. In addition tosamples of forearm skin collected at the time ofsurgery, the following biopsies were examined:
1) healthy buccal mucosa: 2 patients2) unchanged flaps: 2 patients1 irradiated; 1
non-irradiated3) changed flaps: 5 patients4 irradiated; 1 non-
irradiated
Fig. 10. Flap showing partial recovery, 36 months after transplan-
tation, with a silver-white appearance on gross examination. The
histology resembles that of changed flaps but, compared to earlier
biopsies, the epithelium is thinner and the dermal inflammatory
reaction reduced. The surface shows parakeratosis.
Be havi or of S k i n F laps i n O ral Cavi ty 385
Member at www.medicsindex.com
-
8/14/2019 Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics Index Mem
8/11
4) recovering flaps: 3 patients2 irradiated; 1 non-irradiated.
Unchanged Flaps
Biopsies of flaps which grossly resembled skinretained the electron microscopical appearances ofthin skin (Fig. 11). In particular, the following wereobserved: superficial electron-dense squames, cellsrich in keratohyalin granules forming a stratum granu-
losum, coarse electron-dense bundles of tonofilamentsin cells of the stratum spinosum.
Changed Flaps
Four of the five changed flaps showed ultrastruc-tural appearances intermediate between those of skinand buccal mucosa. The fifth specimen, which hadbeen irradiated, was similar to buccal mucosa.
Two of the changed flaps resembled buccal mucosain having nucleated surface cells. There were more
Fig. 11. T.E.M. of thin skin (a) and of an irradiated unchanged flap (b). Both show keratinized surface
cells (K), a stratum granulosum (G), and coarse tonofilament bundles in the stratum spinosum (S). Bar
2 m.
3 8 6 Badran e t al.
Member at www.medicsindex.com
-
8/14/2019 Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics Index Mem
9/11
layers of cells in the epithelium than in skin. Thestratum granulosum was absent. In one specimen, thatwhich resembled buccal mucosa in every way, tonofila-ments were inconspicuous (Fig. 12 a,b). In the other,tonofilament bundles were somewhat coarser than in
buccal mucosa, particularly in the deeper cells (Fig. 12c). Microvillous projections on the surfaces of the cellswere less obvious than in buccal mucosa.
The other three changed flaps, which included thenon-irradiated specimen, showed electron-dense super-ficial squames. One showed numerous keratohyalingranules. All showed cytoplasmic tonofilament bundlesintermediate in character between those of buccalmucosa and skin. One specimen, with an epithelialthickness and surface squames similar to skin, showedtonofilament bundles which were somewhat coarserthan in the other changed flaps but still more delicatethan those seen in skin and in unchanged flaps. Again,
in all specimens, the microvillous surface projectionsof the cells were less obvious than in buccal mucosa.
Flaps Showing Partial Recovery of Skin-like
Gross Appearance
The three biopsies taken from recovering flaps, likemost of the changed flaps, showed features intermedi-ate between skin and buccal mucosa. All showedelectron-dense surface squames. Two showed kerato-hyalin granules. Whereas all three showed tonofila-ment bundles finer than those of skin, comparisonwith earlier biopsies showed coarsening of the bundles.
In summary, the electron microscopical study de-
tected two structural alterations in changed flaps:
1) a qualitative reduction of keratohyalin granules,2) cytoplasmic tonofilament bundles finer than
those in skin.
These features varied in degree between individualchanged flaps. No specific differences could be de-tected between irradiated and non-irradiated speci-mens. Unchanged flaps resembled thin skin. Somechanges towards the form of thin skin were visible inthe recovering flaps.
DISCUSSION
While sample sizes are small, the changes whichoccur in skin flaps transplanted to the oral cavity fallinto two categories:
1. Changes in response to transplantation itself.
The epidermis in biopsies taken in the postopera-tive period, before irradiation, showed hypertrophy,and hyper- and parakeratosis, with increased cytoplas-
mic basophilia and accumulation of glycogen in thestratum spinosum. In biopsies taken later, from un-
changed flaps, and from those changed flaps which
had subsequently reverted to the appearance of nor-
mal skin, these epidermal changes had regressed. A
very similar sequence of changes was described inorthotopic human skin autografts by Scothorne and
Scothorne (1953), and it seems likely that in each casethe changes represent the early and later responses to
the process of transplantation.
2. Changes involving other factors: radiation, infec-tion.
Twenty-one of the 53 patients in this study showed
a gross change in the appearance of the flap from themorphology of skin towards that of oral mucosa at
some stage in the period of observation. Although the
change frequently followed radiotherapy, it also oc-curred in non-irradiated patients at any time after sur-gery, and there was no significant difference in the in-
cidence of this changed appearance between irradiated
and non-irradiated patients. In three of these patients,all of whom had received radiotherapy, the changed
appearance reverted to normal after various intervals
and some of the others showed partial reversion.
Histologically, biopsies of the changed flaps dif-fered from normal thin skin in that the epithelium was
thicker and showed parakeratosis, increased glycogen
content, loss of keratohyalin granules, and finer tono-filament bundles. Whereas the changed epithelium, in
several respects, resembled normal buccal epithelium,
the underlying connective tissue retained the struc-
ture of dermis and contained sweat glands, but showedmarked inflammatory changes in many specimens.
These features, together with enlarged intercellular
spaces in the epithelium and the reversible nature ofthe changes, at least in some individuals, indicate a
reactive rather than a genuine change. The histologi-
cal features of the flap epithelium were similar in both
irradiated and non-irradiated patients although somedifferences could be recognized in the dermis.
It is clear that, while radiotherapy may have a role in
initiating the change, other factors must also beimportant. In a few patients, changes in the appear-ance were associated with infection with Candidaalbicans and in one patient the flap reverted to theappearance of normal skin following treatment of theinfection. The relative roles of radiotherapy, infection,and other forms of trauma in the etiology of theobserved changes in the flaps remain unclear. Thegross appearance of the flap, however, is related to thenumber of inflammatory cells infiltrating the dermis.Forearm skin and buccal mucosa showed Grade 0 and
Be havi or of S k i n F laps i n O ral Cavi ty 387
Member at www.medicsindex.com
-
8/14/2019 Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics Index Mem
10/11
Fig. 12. T.E.M. of typical cells in buccal mucosa (a) and in
changed irradiated skin flaps (b & c). Both flaps had living superficial
cells. The fields illustrated were mid-way through their thickness. In
one of the changed flaps (b) tonofilament bundles were inconspicuous
as in buccal mucosa. The other changed flap (c) showed tonofilament
bundles which were coarser than in buccal mucosa but finer than in thin
skin or unchanged flaps (cf. Fig. 11). Bar 2 m.
Member at www.medicsindex.com
-
8/14/2019 Behavior of Radial Forearm Skin Flaps Transplanted Into the Oral Cavity - Dr Darwish Badran - Medics Index Mem
11/11
Grade 01 inflammatory changes respectively. Postop-erative flaps showed Grade 1 inflammation. In un-changed flaps the degree of reaction varied fromGrade 02 while in the changed flaps it was Grades25. Inflammatory changes diminished as flaps re-
gained the appearance of skin.While the connective tissue deep to the epitheliumretained the general features of dermis, recent work hasindicated that adult and fetal fibroblasts differ in func-tions such as their response to cytokines (Ellis et al.,1997). It is possible that transplantation and/or radio-therapy resulted in functional changes in the fibroblastpopulation and consequent alterations in the overlyingepidermis.
It is concluded that the change in the appearance ofthe radial forearm skin flap, to that of buccal mucosa,does not represent a true, permanent change in epithe-lial type. It did not occur consistently at the periphery
of the graft: this argues against the possibility that itwas the result of creeping replacement by surroundingbuccal epithelium. In many cases it was reversible, andits occurrence seemed to be directly related to thedegree of inflammation in the dermis. The presence ofinflammation is not surprising, considering the factorswhich predispose to the development of oral cancer:excessive smoking, drinking, and poor oral hygiene,which continued in at least some of the patients aftertreatment. Of particular interest and importance wasthe fact that the dermis of the flap persisted as suchand was not replaced by lamina propria at the host site.The dermis would therefore be expected to continue
giving its instructive signals to the overlying epithelium,which maintained its essential epidermal characteris-tics.
ACKNOWLEDGMENTS
The authors are grateful to Miss Margaret Hughesfor photography and to the staff of the CombinedClinic.
REFERENCES
Billingham, R.E. and W.K. Silvers 1968 Dermoepidermal inter-
actions and epithelial specificity. In Epithelial-Mesenchy-
mal Interactions. R. Fleischmajer and R.E. Billingham
(eds.). Baltimore: Williams & Wilkins Co., pp. 252266.
Coulomb, B., C. Lebreton and L. Dubertret 1989 Influence ofhuman dermal fibroblasts on epidermalization. J. Invest.
Derm. 92:122125.
Ellis, I., J. Banyard and S.L. Schor 1997 Differential response of
fetal and adult fibroblasts to cytokines: Cell migration and
hyaluronan synthesis. Development 124:15931600.
Hill, M.W. and I.C. Mackenzie 1984 The influence of differing
connective tissue substrates on the maintenance of adult
stratified squamous epithelia. Cell Tis. Res. 237:473478.
Lawson, V.G. 1985 Oral cavity reconstruction using pectoralis
major muscle and amnion. Arch. Otolaryngol. 111:230233.
Mackenzie, I.C. and M.W. Hill 1984 Connective tissue influ-
ences on patterns of epithelial architecture and keratiniza-
tion in skin and oral mucosa of the adult mouse. Cell Tis.
Res. 235:551559.Robertson, A.G., I.A. McGregor, G.E. Flatman, D. Soutar and P.
Boyle 1985 The role of radical surgery and postoperative
radiotherapy in the management of intra-oral carcinoma. Br.
J. Plast. Surg. 38:314320.
Robertson, A.G., I.A. McGregor, D.S. Soutar, M.M. Ferguson,
G.E. Flatman and P. Boyle 1986 Postoperative radiotherapy
in the management of advanced intra-oral cancers. Clin.
Radiol. 37:173178.
Scothorne, R.J. and A.W. Scothorne 1953 Histochemical studies
on human skin autografts. J. Anat. 87:2229.
Sengel, P. 1986 Epidermal-dermal interaction. In Biology of the
Integument, Vol. 2: Vertebrates. J. Bereiter-Hahn, A.G.
Matoltsy and K.S. Richards (eds.). Berlin: Springer-Verlag,
pp. 374408.Soutar, D.S., L.R. Scheker, N.S.B. Tanner and I.A. McGregor
1983 The radial forearm flap: A versatile method for intra-
oral reconstruction. Br. J. Plast. Surg. 36:18.
UICC, International Union Against Cancer 1987 TNM classifi-
cation of malignant tumours. P. Hermanek and L.H. Sobin
(eds.). 4th Ed. Berlin: Springer-Verlag, pp. 1317.
Weakley, B.S. 1981 A Beginners Handbook in Biological
Transmission Electron Microscopy. 2nd Ed. Edinburgh:
Churchill Livingstone.
Be havi or of S k i n F laps i n O ral Cavi ty 389
Member at www.medicsindex.com





![Medics Gone Wild [PIQUE]](https://static.fdocuments.us/doc/165x107/577ce05c1a28ab9e78b327e2/medics-gone-wild-pique.jpg)












![NAME : MOHAMED DARWISH MOHAMED DARWISH TELEPHONE … · 2017-09-11 · [Mohamed Darwish-CV] HIJJA4R2017 Page 5 of 14 Client Relationship • Develop and maintain good working relationship](https://static.fdocuments.us/doc/165x107/5ed8355c0fa3e705ec0e0970/name-mohamed-darwish-mohamed-darwish-telephone-2017-09-11-mohamed-darwish-cv.jpg)