BadMedicineWP
Transcript of BadMedicineWP
-
8/9/2019 BadMedicineWP
1/61
-
8/9/2019 BadMedicineWP
2/61
-
8/9/2019 BadMedicineWP
3/61
Copyright 2010 by the Cato Institute.All rights reserved.
Cover design by Jon Meyers.
Printed in the United States of America.
CATO I NSTITUTE1000 Massachusetts Ave., N.W.Washington, D.C. 20001www.cato.org
-
8/9/2019 BadMedicineWP
4/61
For better or worse, President Obamas healthcare reform bill is now law. The Patient Protectionand Affordable Care Act represents the most sig-
nificant transformation of the American healthcare system since Medicare and Medicaid. It willfundamentally change nearly every aspect of health care, from insurance to the final delivery of care.
The length and complexity of the legislation,combined with a debate that often generatedmore heat than light, has led to massive confu-sion about the laws likely impact. But, it is now possible to analyze what is and is not in it, whatit likely will and will not do. In particular, we now know that
While the new law will increase the numberof Americans with insurance coverage, itfalls significantly short of universal cover-age. By 2019, roughly 21 million Americanswill still be uninsured.
The legislation will cost far more than adver-tised, more than $2.7 trillion over 10 years of full implementation, and will add $352 bil-lion to the national debt over that period.
Most American workers and businesses willsee little or no change in their skyrocketinginsurance costs, while millions of others,
including younger and healthier workersand those who buy insurance on their ownthrough the non-group market will actually see their premiums go up faster as a result of this legislation.
The new law will increase taxes by morethan $669 billion between now and 2019,and the burdens it places on business willsignificantly reduce economic growth andemployment.
While the law contains few direct provisionsfor rationing care, it nonetheless sets thestage for government rationing and interfer-ence with how doctors practice medicine.
Millions of Americans who are happy withtheir current health insurance will not beable to keep it.
In short, the more we learn about what is inthis new law, the more it looks like bad news for American taxpayers, businesses, health-careproviders, and patients.
_____________________________________________________________________________________________________
Michael Tanner is a senior fellow with the Cato Institute and co-author of Healthy Competition: WhatsHolding Back Health Care and How to Free It .
Executive Summary
-
8/9/2019 BadMedicineWP
5/61
-
8/9/2019 BadMedicineWP
6/61
Contents
Introduction 1
Part I: The Patient Protection and Affordable Care Act 1
Individual and Employer Mandates 1
Insurance Regulations 5
Subsidies 8
The Exchanges 11
Impact on Consumer-Directed Health Plans 13Medicare Cuts 15
Taxes 19
The CLASS Act 22
Growing the Nanny State 24
Other Provisions 25
Part II: Costs and Consequences 26
Expanded, Not Universal, Coverage 26
Increased Spending, Increased Debt 27
Higher Insurance Premiums 32
Conclusion 33
Appendix I: Timeline 35
Notes 38
-
8/9/2019 BadMedicineWP
7/61
-
8/9/2019 BadMedicineWP
8/61
IntroductionOn March 21, 2010, in an extraordinary
Sunday night session, the House of Represen-
tatives gave final approval to PresidentObamas long-sought health insurance planin a partisan 219212 vote. 1 The bill had earli-er passed the Senate on Christmas Eve 2009.Not a single Republican in either chamber vot-ed for the bill. Four days later, the Senate,using a parliamentary tactic known as recon-ciliation to avoid a Republican filibuster, gavefinal approval to a package of changesdesigned to fix the bill. 2
More than 2,500 pages and 500,000 wordslong,3 the Patient Protection and Affordable
Care Act (PPACA) represents the most signifi-cant transformation of the American healthcare system since Medicare and Medicaid. Itwill fundamentally change nearly every aspectof health care from insurance to the final deliv-ery of care.
The final legislation is, in some ways, animprovement over earlier versions. It is not thesingle-payer system sought by many liberals.Nor did it include the interim step of a so-called public option that would likely haveled to a single-payer system in the long run. 4
The employer mandate is far less onerous thanthe 8 percent payroll tax once championed by the House. 5 And the proposed income tax sur-tax on the wealthy has been dropped. 6 Butthat does not mean that this is, as the presi-dent has claimed, a moderate bill.
It mandates that every American purchasea government-designed insurance package,while fundamentally reordering the insurancemarket and turning insurers into somethingresembling public utilities, privately ownedwhile their operations are substantially regulat-ed and circumscribed by Washington. Insur-ance coverage will be extended to millionsmore Americans as government subsidies areexpanded deep into the middle class. Costs willbe shifted between groups, though ultimately not reduced. And a new entitlement will be cre-ated, with the threat of higher taxes and new debt for future generations. In many ways, it
has rewritten the relationship between the gov-ernment and the people, moving this country closer to European-style social democracy.
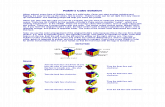
The legislation remains deeply unpopular.Recent polls show substantial majorities sup-
port repealing it. For example, a Rasmussenpoll in late May showed that 63 percent of like-ly voters supported repeal, with 46 percentstrongly supporting repeal. Just 32 percentwanted to keep the law (see Figure 1). 7
It seems likely that repeal or repeal andreplace will be the centerpiece of Republicancampaigns this fall. 8 Numerous court chal-lenges have also been filed, raising questionsabout the constitutionality of various aspectsof the legislation, especially its individualmandate. 9 It seems almost certain, therefore,
that the debate over health care reform will bewith us for some time to come.In the meantime, the legislation has spawn-
ed enormous confusion. Insurance companiesreport people calling and asking, Where dowe get the free Obamacare, and how do I signup for that? 10 But for good or ill, those ex-pecting immediate change are likely to be dis-appointed. Most of the major provisions of the legislation are phased in quite slowly. Themost heavily debated aspects, mandates, sub-sidies, and even most of the insurance reformsdont begin until 2014 or later.
House speaker Nancy Pelosi once famously told us that We have to pass the bill so youcan find out whats in it. 11 With the bill now law, we are indeed discovering what is in it. And what we are finding increasingly lookslike it will leave Americans less healthy, lessprosperous, and less free.
Part I:
The Patient Protection and Affordable Care Act
Individual andEmployer Mandates
Perhaps the single most important pieceof this legislation is its individual mandate, a
1
The individualmandate isunprecedented inU.S. governance
-
8/9/2019 BadMedicineWP
9/61
legal requirement that every American obtainhealth insurance coverage that meets the gov-ernments definition of minimum essentialcoverage. Those who dont receive such cov-erage through government programs, theiremployer, or some other group would berequired to purchase individual coverage ontheir own. 12
This individual mandate is unprecedent-ed in U.S. governance. Back in 1993, whenthe Clinton health care plan was under con-sideration, the Congressional Budget Officenoted A mandate requiring all individuals topurchase health insurance would be anunprecedented federal action. The govern-ment has never required people to buy any good or service as a condition of lawful resi-dence in the United States. 13 Moreover, theindividual mandate raises serious constitu-tional questions. 14 Even the CongressionalResearch Service was not able to conclude itwas constitutional! 15
Under the new law, beginning in 2014,those who fail to obtain insurance so wouldbe subject to a tax penalty. That penalty would be quite mild at first, either $95 or onepercent of annual income in 2014, whicheveris greater. 16 But it ramps up quickly afterthat, the greater of $325 or 2 percent of annu-al income in 2015, and the greater of $695 or2.5 percent of annual income after that. Incalculating the total penalty for an uninsuredfamily, children count as half an adult, whichmeans that in 2016 an uninsured family of four would face a minimum penalty of $2,085 ($695+$695+$347.50+$347.50), andpro-rated based on the number of monthsthat the person was uninsured over thecourse of the year. 17 Individuals will beexempt from the penalties if they earn lessthan an income threshold to be determinedby the secretary of Health and HumanServices (but presumed to be roughly thepoverty level), or if they are unable to obtain
2
Figure 1May 2223 Rasmussen Poll
Source: Rasmussen Reports, poll of 1,000 likely voters, May 22 23, 2010, margin of error +/- 3 percentage points, with a 95% level of confidence.
-
8/9/2019 BadMedicineWP
10/61
insurance that costs less than 8 percent of their gross incomes. 18
According to the CBO, roughly four mil-lion Americans will be hit by penalties in 2016,with the penalties averaging slightly more
than $1,000.19
In fact, the federal governmentexpects to raise $17 billion from penalties by 2019.20
Simply having insurance, however, is notnecessarily enough to satisfy the mandate. Toqualify, insurance would have to meet certaingovernment-defined standards for minimumessential coverage. For example, in order toqualify, plans would be required to cover:ambulatory patient services, emergency ser- vices, hospitalization; maternity and newborncare, mental health and substance abuse treat-
ment; prescription drugs; rehabilitative andhabitative services; laboratory services; preven-tative services; wellness services; chronic dis-ease management; pediatric services, and den-tal and vision care for children. 21 The secretary of HHS is given the authority to define themeaning of those terms and ultimately to setthe minimum benefits package. 22 In addition,plans must meet the new insurance regulatory requirements below.
Unlike in previous versions of the bill,however, individuals who currently have in-surance are grandfathered in, meaning they will not have to change their current insur-ance to meet the new minimum benefit. 23
They will even be able add a spouse or chil-dren to the plan without changing. Whileclearly an improvement over earlier versions,this does not necessarily mean that peoplewill be able to keep their current plan. In par-ticular, making changes to their current planwill end the plans grandfathered status, andwould require that individuals bring theirplan into compliance with the full range of federal mandates and requirements, even if those additional mandates make the new plan more expensive or include benefits thatthe individual does not want. What changesmeet the threshold to end grandfathered sta-tus will be determined by the secretary of HHS. This raises questions of whether some-thing as simple as an increase in co-payments
meets the threshold, or whether it wouldrequire something more substantive, such asa change in carrier. HHS is expected to issuerules later this year. 24
Regardless of what federal regulators
eventually decide, the grandfathering of cur-rent plans may be short-lived. That is be-cause, aside from spouses and children, in-surers will not be able to continue enrollingnew customers in the non-complying plans. As a result, insurers may stop offering theseplans. Over time, the vast majority of non-complying plans will simply fade away.
There has been some dispute over the gov-ernments ability to enforce the mandate.While the law imposes penalties for failure tocomply, and authorizes the IRS to collect
those penalties (indeed, the IRS is expected tohire 16,500 additional agents, auditors, andexaminers for enforcement 25) it does not con-tain any criminal penalties for failing to com-ply, and it forbids the use of liens or levies tocollect the penalties. However, the IRS isnothing if not resourceful. Already, IRSdeputy commissioner Steven Miller has saidthat the IRS may withhold tax refunds toindividuals who fail to comply with the man-date. 26 And, because money is fungible, theIRS could simply apply part of your regulartax payments toward the mandate penalty,and then penalize you for failing to pay thoseregular taxes in full.
Interestingly, the law may have created theworst of both worlds, a mandate that is cost-ly and violates individual liberty, but one thatis still weak enough that it may be cheaperfor many individuals to pay the penalty thanto purchase insurance. As a result it may fallfar short of its proponents goal of bringingyoung and healthy individuals, who today frequently forego insurance, into the insur-ance pool. The Congressional Budget Office,in fact, estimates that the penalties fromindividuals failing to comply with the man-date will generate billions of dollars between2014 and 2019. 27 And according to a RANDCorporation study, those remaining unin-sured after implementation are likely to beyounger and healthier as a group than
3
Simply havinginsurance is notnecessarily enough to satisfythe mandate.
-
8/9/2019 BadMedicineWP
11/61
todays uninsured. 28 Massachusetts experi-ence with an individual mandate yielded justsuch a result. Slightly more than 35 percentof that states remaining uninsured arebetween the ages of 18 and 25, and more
than 60 percent are under the age of 35.29
Before the mandate, those between the agesof 18 and 25 made up roughly 30 percent of the uninsured, suggesting that the young(and presumably healthier) are less likely tocomply with the mandate. 30
Indeed, evidence suggests that Massachu-setts residents are increasingly gaming thesystem: purchasing insurance when they know they are going to use health care ser- vices, then dropping it when they no longerneed it. In 2009 alone, 936 people signed up
for coverage with Blue Cross and Blue Shieldof Massachusetts for three months or less andran up claims of more than $1,000 per monthwhile in the plan. Their medical spendingwhile insured was more than four times theaverage for consumers who buy coverage ontheir own and retain it in a normal fashion. 31
Given that the penalties under the Massa-chusetts mandate are actually stronger thanthose under the Patient Protection and Affordable Care Act, this does not bode wellfor the national plan. 32
The new law also contains an employermandate, although it is watered down fromthe proposal that passed the House last year.The House bill would have required employ-ers with payrolls of more than $250,000 topay 72.5 percent of the premium for individ-ual coverage and 65 percent for family cover-age, or pay a tax equal to 8 percent of theirpayroll. 33 Under the final bill, however, begin-ning in 2014, if a company with 50 or morefull-time employees (or the equivalent 34) doesnot provide health insurance to its workers,and as a result even a single worker qualifiesfor a subsidy to help purchase insurancethrough the exchange (see below), the com-pany must pay a tax penalty of $2,000 forevery person they employ full time (minus 30workers.) Thus a company employing 100workers would be assessed a penalty of $2,000 x 70 workers.35 CBO estimates that
those penalties will cost businesses $52 bil-lion from 2014 to 2019. 36
Even more than the individual mandate,the employer mandate may affect people whoalready have health insurance coverage. In
part, this would be because far more peoplereceive their insurance through work. But, inaddition, HHS has released rules suggestingthat if companies make any significantchanges to their current coverage they will nolonger be grandfathered under the employ-er mandate, meaning that they will have tobring their plan into full compliance with allthe new federal requirements. Among thechanges that would end grandfathered pro-tection would be a change in insurance carri-er and increases in deductibles or co-pay-
ments.37
An internal study by HHS estimatesthat more than two-thirds of companiescould be forced to change their current cover-age. For small businesses, the total couldreach 80 percent. 38
Even offering the correct benefits will notnecessarily exempt companies from penal-ties. Companies that offer coverage, butwhich have employees that still qualify for a subsidy because the employees contributionis deemed unaffordable (that is, it exceeds 8percent of an employees income), will stillhave to pay a penalty of the lesser of $3,000per employee receiving a subsidy or $2,000per worker whether they are receiving a sub-sidy or not for every employee receiving a subsidy or $2,000 for every full-time worker. A survey by the employer benefits firm,Mercer, suggests that as many as one-third of employers could face penalties for failing tomeet the affordable insurance requirement. 39
Such a mandate is simply a disguised taxon employment. As Princeton University pro-fessor Uwe Reinhardt, the dean of health careeconomists, points out, [Just because] thefiscal flows triggered by the mandate wouldnot flow directly through the public budgetsdoes not detract from the measures status of a bona fide tax. 40
And while it might be politically appealingto claim that business will bear the new taxburden, nearly all economists see it quite dif-
4
More thantwo-thirds of
companies couldbe forced tochange their
current coverage.
-
8/9/2019 BadMedicineWP
12/61
ferently. The amount of compensation a worker receives is a function of his or her pro-ductivity. The employer is generally indifferentto the composition of that compensation. Itcan be in the form of wages, benefits, or taxes.
What really matters is the total cost of hiringthat worker. Mandating an increase in the costof hiring a worker by adding a new payroll taxdoes nothing to increase that workers pro-ductivity. Employers will therefore seek waysto offset the added cost by raising prices (theleast likely solution in a competitive market),lowering wages, reducing future wage increas-es, reducing other benefits (such as pensions),cutting back on hiring, laying off currentworkers, shifting workers from full-time topart-time, or outsourcing. 41 In fact, a survey by
Towers Watson shows that employers arepreparing to take exactly those steps. 42
And, as with the individual mandate, thepenalty may be low enough that many busi-nesses may find it less costly to pay than toplay.43 As an internal document preparedfor Verizon explains, Even though the pro-posed assessments [on companies that do notprovide health care] are material, they aremodest when compared to the average cost of health care. 44 In fact, CBO estimates that atleast 10 to 12 million workers could lose theircurrent employer-provided health insur-ance.45 Approximately 8 to 9 million couldend up on Medicaid, with the rest purchasingsubsidized coverage through the exchanges(see below).46 But this may vastly underesti-mate the actual number of workers whocould be dumped from their current coverage.Several large US corporations, have indicatedthat they may drop their current coverage. 47
Insurance Regulations
Since the advent of the McCarran-Ferguson Act in 1945, health insurance hasbeen primarily regulated at the state level. 48
The Patient Protection and Affordable Care Act imposes a host of new federal insuranceregulations that will significantly change theway the health insurance industry does busi-
ness. Some of these regulatory changes arelikely to be among the laws most initially popular provisions. But many are likely tohave unintended consequences.
Perhaps the most frequently discussed
regulatory measure is the ban on insurersdenying coverage because of preexisting con-ditions. Throughout the health care debate,proponents of reform highlighted stories of people with terrible illnesses who wereunable to get insurance coverage. 49
Under the Patient Protection and Afford-able Care Act insurers would be prohibitedfrom making any underwriting decisionsbased on health status, mental or physicalmedical conditions, claims experience, med-ical history, genetic information, disability,
other evidence of insurability, or other factorsto be determined later by the secretary of HHS.50
Specifically, the law would require insurersto accept every employer and individual . . .that applies for such coverage. 51 Insurers arealso forbidden to cancel insurance if a policy-holder becomes sick. 52 Finally, there will belimits on the ability of insurers to vary premi-ums on the basis of an individuals health.That is, insurers must charge the same premi-um for someone who is sick as for someonewho is in perfect health. 53 Insurers may con-sider age in setting premiums, but those pre-miums cannot be more than three times high-er for their oldest than their youngestcustomers. 54 Smokers may also be charged upto 50 percent more than nonsmokers. 55 Theonly other factors that insurers may considerin setting premiums are geographic locationand whether the policy is for an individual ora family.56
It is also worth noting that, while a ban onpreexisting conditions for children starts with-in six months, the rules will not apply toadults until 2014. 57 Until then, adults withpreexisting conditions will be eligible to par-ticipate in federally sponsored high-riskpools. 58 The high-risk pools will contract withprivate, nonprofit insurers for plans that mustcover at least 65 percent of the costs of partic-ipants care. Out-of-pocket costs would be
5
Some of theregulatory changes arelikely to have
unintendedconsequences.
-
8/9/2019 BadMedicineWP
13/61
capped at $5,950 a year for an individual or$11,900 for a family. The risk pools are sup-posed to be in place no later than the end of June 2010.59 The law provides $5 billion toestablish the pools and subsidize coverage, but
many experts worry about future fundingshortfalls. 60 In fact, some analysts suggest thatthe risk pools could ultimately cost up to asmuch as eight times as much. 61
While the ban on medical underwritingmay make health insurance more availableand affordable for those with preexistingconditions and reduce premiums for olderand sicker individuals, it will also increasepremiums for younger and healthier individ-uals. The RAND Corporation recently con-ducted a study for the Associated Press con-
cluding that premiums for the young wouldrise about 17 percent, roughly $500 per year,as a result of the new law. 62 Other studiessuggest the increase could be much higher.For example, a study by the independent
actuarial firm Milliman, Inc., concluded thatpremiums for young men could increase by 10 to as much as 30 percent. 63 The Councilfor Affordable Health Insurance suggeststhat premiums for some individuals could
increase by 75 to 95 percent in states that donot now have guaranteed issue or communi-ty rating requirements (see Figure 2). 64
Moreover, the ban may not be as effectiveas proponents hope in making insuranceavailable to those with preexisting condi-tions. Insurance companies have a variety of mechanisms for evading such restrictions. Asimple example is for insurers to focus theiradvertising on young healthy people; or they can locate their offices on the top floor of a building with no elevator; or provide free
health club memberships while failing toinclude any oncologists in their network.In a similar vein, the law also bans rescis-
sions, or the practice of insurers droppingcoverage for individuals who become sick. 65
6
Figure 2Possible Premium Increases for Young Workers Under PPACA
Source: RAND and Millman studies cited in Carla Johnson, Health Premiums Could Rise 17 Percent for Young Adults, Associated Press, March 29, 2010; and BrianMcManus, Universal Coverage + Guaranteed Issue + Modified Community Rating=95% Rate Increase, Council for Affordable Health Insurance, August 2009.
-
8/9/2019 BadMedicineWP
14/61
Under existing practices, insurers sometimesretroactively review an individuals initialinsurance application and cancel the policy if the application is found to be inaccurate. 66
Because insurers would undertake such a
review only when individuals submitted largeclaims (and were therefore sick) and thegrounds for rescission often appeared to be very minor discrepancies, the practice waswidely condemned by the bills proponents.Under the legislation, insurers could cancelcoverage only in cases of fraud or intentionalmisrepresentation of material fact. Whilelikely to be very popular, this provision may have little practical impact. According to a congressional report, there were actually few-er than 5,000 rescissions per year, and at least
some of those were cases of actual fraudwhere cancellations would still be allowedunder this legislation. 67
A second new insurance regulation wouldprohibit insurers from imposing lifetime lim-its on benefit payouts. 68 Although popular,this provision is also likely to have less impactthan most people believe. Roughly 40 percentof insured Americans already had policies withno lifetime caps. For those policies that didhave a cap on lifetime benefits, that cap wasusually somewhere between $2.5 million and$5 million, with many running as high as $8million, amounts that very few people everreached.69 Still, some individuals with chronicor catastrophic conditions will undoubtedly benefit from this provision, although there areno solid estimates on how many. Removinglifetime caps will most likely increase the costof re-insuring policies, leading ultimately tohigher premiums, but most insurers predictthe increase will be modest. 70
This regulation, however, may have a much bigger impact on more than one mil-lion part-time, seasonal, and low-wage work-ers who currently take advantage of low-cost,limited benefit plans. Those plans, known inthe industry as mini-med plans, have inex-pensive premiums because they can, amongother things, restrict the number of covereddoctor visits or impose a maximum on insur-ance payouts in a year. They are particularly
popular with low-wage workers in the restau-rant and retail industries. The prohibition onlifetime caps could all but eliminate theseplans, meaning that as many as a millionworkers could lose the coverage they have
now. Some could be forced into Medicaid,while others would be forced to purchasemuch more expensive insurance than they have today. 71
The law also places limits on deductibles.Employer plans may not have an annualdeductible higher than $2,000. Family poli-cies are limited to deductibles of $4,000 orless.72 There is an exception, however, for indi- viduals under the age of 30, who will beallowed to purchase a catastrophic policy with a deductible of $4,000 for an individual,
$8,000 for a family plan.73
In addition, the law requires insurers tomaintain a medical loss-ratio (that is the ratioof benefits paid to premiums collected) of atleast 85 percent for large groups and 80 per-cent for small groups and individuals. 74
Insurance companies who pay out benefitsless than the required proportion of premi-ums, must rebate the difference to policy hold-ers on an annual basis beginning in 2011. Thisrequirement is intended to force insurers tobecome more efficient by reducing theamount of premiums that can be used foradministrative expenses (and insurer prof-its).75 However, while there is undoubtedly waste in insurance overhead, such a rigid capmay create a number of unintended conse-quences. Insurance overhead includes many useful services and programs. These includeefforts to monitor patient care to ensure thosewith chronic medical conditions are gettingappropriate care, exactly the type of programthat President Obama says he wants toencourage, and efforts to combat fraud andabuse. Those programs can actually reduceoverall costs and result in lower insurance pre-miums. Forcing insurers to abandon thoseefforts could have the perverse effect of increasing costs to consumers. 76
Finally, the legislation would also allow parents to keep their dependent children ontheir policies until the child reaches age 26.
7
Such a rigid capmay create anumber of unintendedconsequences.
-
8/9/2019 BadMedicineWP
15/61
This too is generally considered a popularaspect of the new law, but it does come witha price tag. HHS estimates that every depen-dent added to a policy will increase premi-ums by $3,380 per year. 77 Although this pro-
vision would not go into full effect until nextyear, most large insurers have indicated thatthey would be willing to begin coveringdependent children sooner, perhaps as early as this summer. Employers, however, haveindicated that they will be reluctant to adddependent children to the coverage they pro- vide, even if insurers offer it, until they arerequired to in January 2011. 78
Overall, most of the laws insurancereforms are likely to be among the more polit-ically popular aspects of the new law, though
they are likely to have only a minor impact andmay, indeed, have a number of unintendedconsequences.
SubsidiesThe number one reason that people give
for not purchasing insurance is that they can-not afford it. 79 Therefore, the legislationsprincipal mechanism for expanding coverage(aside from the individual and employer man-dates) is to pay for it, either through govern-ment-run programs such as Medicaid and theState Childrens Health Insurance Program(SCHIP) or through subsidizing the purchaseof private health insurance.
Starting in 2011, states are required toexpand their Medicaid programs to cover allU.S. citizens with incomes below 133 percentof the poverty level ($14,404 for an individual;$29,327 for a family of four; higher in Alaska,Hawaii, and the District of Columbia). 80
Previously, only pregnant women and chil-dren under age six were covered to 133 percentof the poverty level. Children 618 wererequired to be covered up to 100 percent of thepoverty level, though 18 states covered chil-dren from families with higher incomes. Infact a few states covered pregnant women andchildren under age 1 up to 185 percent of thepoverty level.81 Most other low-income chil-
dren were covered through SCHIP (up to 250percent of poverty).
Thus, the primary result of the lawsMedicaid expansion would be to extend cover-age to the parents in low-income families and
to childless adults. In particular, single, child-less men will now be eligible for Medicaid.This raises potentially serious concerns. Low-income, childless, adult men in particular are a high-risk, high-cost health care population.That means costs may run higher than expect-ed, a problem that may be exacerbated by adverse selection within that population.
Tennessees experience with Tenncare pro- vides a cautionary tale. In 1994, Tennesseeexpanded Medicaid eligibility to uninsured cit-izens who werent able to get health insurance
through their employers or existing govern-ment programs and to citizens who were unin-surable because of preexisting conditions. Overthe next 10 years, Medicaid costs in the other49 states rose by 71 percent. In Tennessee they increased by an overwhelming 149 percent. 82
Despite this massive increase in spending,health outcomes did not improve. Even thestates Democratic governor Phil Bredesencalled the program a disaster. 83 Similar prob-lems with the Patient Protection and Afford-able Care Acts Medicaid expansion could dra-matically drive up costs for both the federaland state governments.
Initially, the federal government will pay 100 percent of the cost for new enrollees.However, beginning in 2017, states will berequired to pick up a portion of the cost: 5percent of the cost in 2017, gradually increas-ing to 10 percent by 2020. States will alsoreceive a slight (0.15 percent) increase in thefederal match toward coverage of existingMedicaid recipients.
The impact on state budgets would vary dramatically (see Table 1). The biggest losersin terms of total dollars would be California,whose Medicaid costs would increase by nearly $5 billion between 2014 and 2019, andTexas, whose costs would rise by nearly $4.5billion. Taken as a percentage of a statesGeneral Funds, the hardest hit states wouldbe Texas (1.8 percent), Mississippi (1.7 per-
8
Tennesseesexperience with
Tenncareprovides a
cautionary tale.
-
8/9/2019 BadMedicineWP
16/61
9
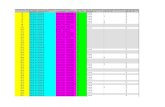
Table 1Medicaid on State Budgets
State Unfunded Medicaid Liability Percent of State General Funds
Texas $746.2 1.88%
Mississippi $87.6 1.70% Nevada $55.8 1.62%Arizona $155.0 1.54%
Arkansas $64.4 1.48%Florida $401.2 1.45%
Colorado $106.2 1.43%Oklahoma $88.6 1.37%
Michigan $131.8 1.33%Louisiana $110.2 1.14%
South Carolina $79.7 1.11%
Missouri $88.5 1.10%Oregon $73.5 1.05%
Alabama $90.3 1.05%Georgia $200.1 1.03%
Montana $20.9 1.01%Tennessee $104.6 0.95%
North Carolina $181.5 0.88%South Dakota $10.3 0.87%
New Mexico $51.8 0.86%West Virginia $32.2 0.86%
Kentucky $81.0 0.86%Illinois $225.0 0.83%Idaho $22.9 0.82%
California $833.0 0.81% New Hampshire $12.3 0.80%
Nebraska $23.7 0.73% North Dakota $8.6 0.72%
Kansas $43.5 0.71%Indiana $88.3 0.69%
Utah $39.5 0.68%Virginia $109.6 0.63%
New York $309.0 0.58%Ohio $150.9 0.57%
Iowa $33.5 0.57%
Maryland $81.2 0.56%Washington $78.6 0.54%
Pennsylvania $139.8 0.52%
Continued next page
-
8/9/2019 BadMedicineWP
17/61
cent), Nevada (1.6 percent), Florida (1.5 per-cent), and Arizona (1.5 percent).
SCHIP would be continued until Septem-ber 30, 2019. Between 2014 and 2019, the fed-eral government will increase its contributionto the program, raising the federal match rateby 23 percentage points (subject to a 100 per-cent cap). 84 States must maintain their cur-rent income eligibility levels for the pro-gram. 85 Individuals with incomes too high toqualify for Medicaid but below 400 percent of the poverty level ($88,000 per year) will be eli-gible for subsidies to assist their purchase of private health insurance. These subsidies,which will be provided in the form of refund-able tax credits, are expected to total morethan $449 billion between 2014, when indi- viduals are first eligible for the payments, and2020.86
There are actually two separate creditsdesigned to work more or less in conjunctionwith one another. The first is a premium taxcredit.87 The credit is calculated on a slidingscale according to income in such a way as tolimit the total proportion of income that anindividual would have to pay for insurance. 88
Thus, individuals with incomes between 133and 200 percent of the poverty level willreceive a credit covering the cost of premiumsup to four percent of their income, whilethose earning 300400 percent of the poverty level will receive a credit for costs in excess of9.5 percent of their income.
The second credit, a cost-sharing creditprovides a subsidy for a proportion of out-of-pocket costs, such as deductibles and co-pay-ments. Those subsidies are also provided on a sliding income-based scale, so that thosewith incomes below 150 percent of the pover-ty level receive a credit that effectively reducestheir maximum out-of-pocket costs to 6 per-cent of a plans actuarial value, while thosewith incomes between 250 and 400 percentof the poverty level would, after receiving thecredit, have maximum out-of-pocket costs of no more than 30 percent of a plans actuarial value.
The net result of this rather complex for-mula is that a family of four with an annualincome of $30,000 per year, purchasing aninsurance policy that cost $9,435, wouldreceive a federal subsidy of $8,481, and have to
10
The phase-out of these benefitscreates a highmarginal tax
penalty.
Table 1 Continued Medicaid on State Budgets
State Unfunded Medicaid Liability Percent of State General Funds
Wisconsin $58.9 0.44%
New Jersey $137.2 0.41%Wyoming $7.2 0.40%Maine $11.3 0.36%
Rhose Island $10.4 0.31%
Delaware $10.2 0.30%Minnesota $50.2 0.30%
Connecticut $36.6 0.22%Alaska $10.6 0.19%
Hawaii $10.1 0.19%Massachusetts $52.9 0.16%
Vermont -$6.0 -0.50%
Source: Authors calculations based on Heritage Foundations State Costs for ObamaCare Medicaid Expansion anddata from the National Association of State Budget Officers, 2008 State Expenditure Report.
-
8/9/2019 BadMedicineWP
18/61
pay $954 themselves. If the same family hadan income of $65,000 per year, they wouldreceive a subsidy of $3,358 and pay $6,077themselves. 89
As with many tax credits, the phase-out of
these benefits creates a high marginal taxpenalty as wages increase. In some cases,workers who increase their wages could actu-ally see their after-tax income decline as thesubsidies are reduced. This creates a perverseset of incentives that can act as a poverty trap for low-wage workers. 90
In addition to the individual subsidies,there will also be new government subsidiesfor some small businesses. Beginning nextyear, businesses with fewer than 25 employeesand average wages below $50,000 will be eligi-
ble for a tax credit to help offset the cost of providing insurance to their workers. 91 To beeligible, employers must provide insurance toall full-time workers and pay at least 50 per-cent of the cost of that coverage. The actualamount of the credit depends on the size of the employer and the average worker salary.Between 2011 and 2014, when the exchangesbegin operation (see below), employers with10 or fewer workers and an average wagebelow $25,000 per year would be eligible for a credit equal to 35 percent of the employerscontribution. For a typical family policy, thecredit would be around $2,000. The creditgradually phases out as the size of the compa-ny and average wages increase.
Once the exchanges are operational after2014, businesses with 10 or fewer employeesand average wages below $25,000 that pur-chase their insurance through the exchangewill be eligible for a credit of up to 50 percentof the employers contribution toward a work-ers insurance. Again, the credit is phased outas the size of the company and average wagesincrease. The credit can only be claimed fortwo years.
In addition, the legislation establishes a $5billion temporary reinsurance program foremployers who provide health insurance cov-erage for retirees over age 55 who are not yeteligible for Medicare. 92 The program will reim-burse insurers for 80 percent of retiree claims
between $15,000 and $90,000. 93 Insurers arerequired to pass those savings on to employersthrough lower premiums, though how thatwill be enforced remains a question. 94 The pro-gram is supposed to begin by June 23 of this
year and expire on January 1, 2014.95
The law also increases funding for commu-nity health centers by $11 billion. 96 Approxi-mately $1.5 billion would be used for the con-struction of new health centers in inner-city orrural low-income neighborhoods, with theremainder designed to subsidize operations forexisting centers. Community health centers areexpected to treat nearly 40 million patients by 2015, nearly double todays utilization. 97
All together, this law represents a massiveincrease in the welfare state, adding millions
of Americans to the roll of those dependent, atleast to some extent, on government largess. Yet for all the new spending, the PatientProtection and Affordable Care Act falls shortof its goal of achieving universal coverage (seebelow).
The Exchanges
Perhaps the most fundamental reorderingof the current insurance market is the cre-ation of exchanges in each state. Ezra Klein,one of the bills most prominent liberal sup-porters, maintains that that the exchangesare the most important element in theplan. 98 The exchanges would function as a clearinghouse, a sort of wholesaler or mid-dleman, matching customers with providersand products.
Exchanges would also allow individualsand workers in small companies to takeadvantage of the economies of scale, both interms of administration and risk pooling,which are currently enjoyed by large employ-ers. The larger risk pools should theoretically reduce premiums, as would the exchangesability to use market share to bargain downthe prices of services.99
However, one should be skeptical of claimsthat the exchange will reduce premiums. InMassachusetts, supporters of the connector
11
All together thelaw represents amassive increasein the welfare
state.
-
8/9/2019 BadMedicineWP
19/61
claimed that it would reduce premiums forindividual insurance policies by 25 to 40 per-cent.100 Instead, premiums for policies soldthrough the connector have been rising, up 11percent for the lowest cost plans since the pro-
gram began.101
Beginning in 2014, one or more ex-changes would be set up by each state andlargely operated according to rules developedby that state. States would also have theoption of joining with other states and creat-ing regional exchanges. If a state refuses tocreate an exchange, the federal government isempowered to set one up within that state. 102
States are given considerable discretion overhow the exchanges would operate, but someof the federal requirements are significant.
Exchanges may be either a governmentalagency or a private nonprofit entity. 103 Andstates would have the option of either main-taining separate insurance pools for the indi- vidual and small-group markets or of combin-ing them into a single pool. 104 The poolswould also include individual or small-grouppolicies sold outside the exchange. 105 Existingplans could not be included in those pools,however.106
Initially, only businesses with fewer than50 employees, or uninsured individuals, orthe self-employed may purchase insurancethrough the exchange. Members of Congressand senior congressional staff are also re-quired to purchase their insurance throughthe exchange. 107 However, beginning in 2017,states have the option of opening the ex-change to large employers. 108
Insurance plans offered for sale within theexchanges would be grouped into four cate-gories based on actuarial value: bronze, thelowest cost plans, providing 60 percent of theactuarial value of a standard plan as defined by the secretary of HHS; silver, providing 70 per-cent of the actuarial value; gold, providing 80percent of the actuarial value; and platinum,providing 90 percent of the actuarial value. 109
In addition, exchanges may offer a special cata-strophic plan to individuals who are under age30 or who have incomes low enough to exemptthem from the individual mandate. 110
For all categories of plans, out-of-pocketexpenses would be limited according to theincome of the purchaser. For individuals andfamilies with incomes above 400 percent of the poverty level, out-of-pocket expenses
would be limited to $5,950 for individuals and$11,900 for families, approximately the cur-rent limits for a Health Savings Account.Those limits would also apply to those whopurchase the catastrophic plan. Individualswith incomes between 300 and 400 percent of the poverty level would have out-of-pocketexpenses limited to two-thirds of the HSA lim-its ($3,987/individual and $7,973/family); 200to 300 percent of poverty would have out-of-pocket expenses limited to one-half of theHSA limits ($2,975/individual and $5,950/
family); and those with incomes below 200percent of poverty would have out-of-pocketexpenses limited to one-third of the HSA lim-its ($1,983 per individual and $3,967 per fam-ily). The reductions in out-of-pocket expenseswould occur within the plan in such a way asnot to change their overall actuarial value.
CBO estimates that premiums for bronzeplans would probably average between $4,500and $5,000 for an individual and between$12,000 and $12,500 for family policies. 111
The more inclusive policies would have corre-spondingly higher premiums.
Plans offered through the exchange mustmeet the federal requirements for minimumbenefits. State mandated benefits are notpreempted, meaning that states may contin-ue to impose additional mandates.
In addition to the state insurance plans, thelegislation authorizes the federal Office of Personnel Management to contract with pri- vate insurers to ensure that each state ex-change offers at least two multi-state insur-ance plans. These multi-state plans aresupposed to resemble those available in theFederal Employee Health Benefit Program,but will operate separately from the FEHBPand will have a separate risk pool. 112 The mul-ti-state plans must meet the licensing and reg-ulatory requirements of each state in whichthey are offered. 113 At least one plan must notinclude abortion coverage, and one must be
12
Plans offeredthrough the
exchange mustmeet the federal
requirements forminimum
benefits.
-
8/9/2019 BadMedicineWP
20/61
offered by a nonprofit insurer. The legislationalso provides start-up funds for states to estab-lish health insurance cooperatives which may participate in the states exchange. 114
Exactly how significant the exchanges will
prove to be remains to be seen. At the very leastexchanges will change the way individuals andsmall businesses purchase health insurance.However, if expanded to include large busi-nesses or their employees, exchanges representa potential framework for a far more extensivegovernment intervention in the insurancemarket.
Impact on Consumer-Directed Health Plans
The health care bill reverses much of theprogress in recent years toward more con-sumer-directed health care.
Consumer-directed health care is a broadterm used to describe a variety of insurance
arrangements, including health savingsaccounts (HSAs), flexible spending accounts(FSAs), and health reimbursement accounts(HRAs), based on the concept that patients(consumers) should have more control
over the utilization of their healthcare dol-lars.115 The goal is to simultaneously controlcosts and improve quality by creating incen-tives for consumers to make judgmentsbased on price and value; in short to pur-chase health care the way we buy other goodsand services.116 More than 46 million workerscurrently participate in consumer-directedhealth plans (see Figure 3).
President Obama has always been hostileto consumer-directed health care. In his book,The Audacity of Hope, for example, he dismisses
health savings accounts as being based on theidea that people have an irrational desire topurchase more than they need. 117 That hos-tility is reflected in the final legislative lan-guage. Notably, the legislation puts substan-tial new restrictions on such consumer-
13
President Obamahas alwaysbeen hostile toconsumer-
directed healthcare.
Source: Source for HRAs: Employer Benefit Research Institute, What Do We Know About Enrollment in Consumer-Driven Health Plans? vol. 30, no. 12, December 2009.
Figure 3Workers with Consumer-Directed Health Plans
-
8/9/2019 BadMedicineWP
21/61
oriented innovations as Health Savings Ac-counts and Flexible Spending Accounts.
Roughly 10 million Americans currently have health savings accounts. 118 Nothing inthe legislation directly prohibits them. How-
ever, the law does add several new restrictions.For example, the tax penalty for HSA with-drawals that are not used for qualified med-ical expenses will be doubled from the current10 percent to 20 percent, starting in 2011. 119
In addition, the definition of qualified med-ical expense has been made more restrictive. Among other things, over-the-counter med-ications will no longer be considered a quali-fied medical expense. 120
Of greater concern is the potential impactof the law on high-deductible insurance plans.
Current law requires than an HSA be accom-panied by such a policy. However, many of theinsurance regulations discussed above raisequestions about whether or not high-de-ductible plans will remain viable.
For example, the lowest permissible actu-arial value for an insurance plan (the bronzeplan) would be 60 percent. 121 It is unclearwhether a plans actuarial value wouldinclude employer or individual contributionsmade to the individuals HSA. That decisionis left to the discretion of the secretary of HHS.122 Whether or not HSA contributionsare included can make as much as a 1020percent difference in a plans actuarial value. As a result, if the contributions are notincluded, many, if not most, high-deductibleplans will not qualify. The fate of HSAs istherefore dependent on a regulatory rulingby the secretary of HHS in an administrationavowedly hostile to HSAs.
The 80 percent minimum medical lossratio required of insurance plans could alsoprove problematic for HSAs. Again, how thisprovision will work in practice will dependon rules to be developed by the secretary of HHS. But, the legislation makes no distinc-tion between traditional and high-deductibleinsurance plans. Few if any current high-deductible policies meet this requirement.
In addition, there is reason to wonderwhether high-deductible insurance plans will
likely be able to meet the laws requirementthat insurance plans provide first-dollar cover-age for all preventive services.123 Currently,most high-deductible plans do cover preven-tive services as defined by the IRS. However, as
discussed above, under the Patient Protectionand Affordable Care Act, preventive serviceswill be defined by the U.S. PreventativeServices Task Force and, once again, the secre-tary of HHS. 124 If the new definition of pre- ventive services is more expansive than the IRSdefinition, as seems likely, most current highdeductible plans will once again be out of compliance.
Finally, insurers must make certain thattheir high-deductible plans are designed so asto comply with the laws limits on out-of-
pocket expenses.In theory, a high deductible plan designedto work with health savings accounts couldmeet all the new requirements. But industry sources warn that a plan designed to thosespecifications would offer few if any advan-tages over traditional insurance and would notbe competitive in todays markets. As a result,insurers may stop offering high deductiblepolicies.125 And since the rules for HSAs requirethat they be accompanied by a high deductibleplan, the result would be to end HSAs.
The law also includes new limits on FSAs,which are currently used by as many as 30million Americans. 126 Starting in taxable year2013, the maximum tax-exempt contributionto an FSA will be cut in half, from the current$5,000 annually to just $2,500. 127 The newdefinition of qualified medical expense willalso be applied to FSAs, meaning that as withHSAs, FSAs could not be used to pay for over-the-counter medications. 128
The impact of these provisions extendswell beyond their impact on workers whocurrently take advantage of such innovativeproducts as HSAs and FSAs. More signifi-cantly, the assault on these products repre-sents a fundamental philosophical shift inthe health care debate. Through this legisla-tion, the president and Democrats in Con-gress reject consumer-oriented health carereform in clear favor of government control.
14
The fate of HSAsis therefore
dependent on aregulatory rulingby the Secretary
of HHS.
-
8/9/2019 BadMedicineWP
22/61
Medicare CutsDespite denials from the Obama adminis-
tration and Democrats in Congress, the legis-
lation does cut Medicareand it should!Medicare is facing unfunded liabilities of $50trillion to $100 trillion depending on theaccounting measure used, making futurebenefit cuts both inevitable and desirable. 129
Of course it would have been better, if the sav-ings from any cuts had been used to reducethe programs future obligations rather thanto fund a brand new entitlement program. And, clearly, not all Medicare cuts are createdequal.130 Still, that should not obscure thenecessity for dealing with Medicares looming
financial crisis (see Figure 4.)The legislation anticipates a net reductionin Medicare spending of $416.5 billion over
10 years.131 Total cuts would actually amountto slightly more than $459 billion, but sincethe bill would also increase spending underthe Medicare Part D prescription drug pro-gram by $42.6 billion, the actual savings
would be somewhat less.132
The key word here is anticipates, be-cause several of those cuts are speculative atbest. For example, the bill anticipates a 23percent reduction in Medicare fee-for-servicereimbursement payments to providers, yield-ing $196 billion in savings. 133 But Medicarehas been supposed to make similar reduc-tions since 2003, yet, each year, Congress has voted to defer the cuts. There is no reason tobelieve that Congress is now more likely tofollow through on such cuts. In fact, in a per-
fect exercise in cynicism, the House hasalready passed separate legislation to repealthem.
15
Figure 4Medicare Cash Flow
Source: 2009 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds,Figure II.E2.
-
8/9/2019 BadMedicineWP
23/61
More likely, but still problematic, are $136billion in cuts to the Medicare Advantage pro-gram. Currently, some 10.2 million seniors, 22percent of all Medicare recipients, are enrolledin the Medicare Advantage program, which
allows Medicare recipients to receive their cov-erage through private insurance plans. 134 Thebill would change the way payments are calcu-lated for Medicare Advantage. Currently Medicare Advantage programs receive pay-ments that average 14 percent more than tra-ditional fee-for-service Medicare, 135 somethingthat Democrats have derided as wasteful. 136
However, the program also offers benefits notincluded in traditional Medicare, includingpreventive-care services, coordinated care forchronic conditions, routine physical examina-
tions, additional hospitalization, skilled nurs-ing facility stays, routine eye and hearingexaminations, glasses and hearing aids, andmore extensive prescription drug coveragethan offered under Medicare Part D. 137
The law imposes a new competitive bid-ding model on the Medicare Advantage pro-gram that will effectively end the 14 percentoverpayment. 138 The change will be phased-inover three years beginning in 2012. Inresponse, many insurers are expected to stopparticipating in the program, while others willincrease the premiums they charge seniors. Analysis of similar proposals in the past, havesuggested that 1.5 to 3 million seniors couldbe forced out of their current insurance planand back into traditional Medicare. 139 TheCongressional Budget Office predicts thesecuts could lead many plans to limit the bene-fits they offer, raise their premiums, or with-draw from the program.
Particularly hard hit would be minoritiesand seniors living in underserved areas. Forexample, nearly 40 percent of African- American and 54 percent of Latino seniorsparticipate in Medicare Advantage, in partbecause lower-income seniors see it as a low-cost alternative to Medigap insurance forbenefits not included under traditionalMedicare. 140 Interestingly, the law exemptsthree counties in south Florida from theMedicare Advantage cuts.
In addition, a new productivity adjust-ment would be applied to reimbursements tohospitals, ambulatory service centers, skillednursing facilities, hospice centers, clinical lab-oratories, and other providers, resulting in an
estimated savings of $156.6 billion over 10years.141 There would also be $3 billion in cut-backs in reimbursement for services that thegovernment believes are over used, such asdiagnostic screening and imaging services. And, beginning next year, the utilizationassumption used to determine Medicarereimbursement rates for high-cost imagingequipment will be increased from 50 to 75 per-cent, effectively reducing reimbursement formany services.142 This change is expected toreduce total imaging expenditures by as much
as $2.3 billion over 10 years.143
Other Medicarecuts include freezing reimbursement rates forhome health care and inpatient rehabilitativeservices and $1 billion in cuts to physician-owned hospitals. 144
And, for the first time, the secretary of HHS would be permitted to use comparativeeffectiveness research in making reimburse-ment decisions. The use of comparative effec-tiveness research has been extremely contro- versial throughout this debate. On the onehand, many health care experts believe thatmuch of U.S. health care spending is wastefulor unnecessary. 145 Medicare spending varieswildly from region to region, without any evi-dence that the variation is reflected in thehealth of patients or procedural outcomes. 146
A case could certainly be made that taxpayersshould not have to subsidize health care thathas not proven effective, nor can Medicareand Medicaid pay for every possible treat-ment regardless of cost-effectiveness.
On the other hand, the use of suchresearch in determining what procedureswould be reimbursed could fundamentally alter the way medicine is practiced and couldinterpose government bureaucracies in deter-mining how patients should be treated.Moreover, there are significant questionsabout whether comparative effectiveness canprovide a truly effective basis for determiningreimbursement policy. 147 In fact, it could be
16
The legislationdoes cut
Medicareand it should!
-
8/9/2019 BadMedicineWP
24/61
argued that Medicare is particularly unsuitedfor such a policy. 148
Many others worry that the use of compar-ative effectiveness research for governmentprograms such as Medicare sets the stage for
its extension to private medical practice. Thereis no doubt that national health care systemsin other countries use comparative effective-ness research as the basis for rationing. 149
Some of President Obamas health care advis-ers, such as former Sen. Tom Daschle, haverecommended that it be extended to privateinsurance plans. 150 And the president hasnamed as the new director of the Center forMedicare and Medicaid Services, Dr. DonaldBerwick, who is an outspoken admirer of theBritish National Health Service, and particu-
larly its National Institute for ClinicalEffectiveness, which makes such cost-effective-ness decisions. 151
While some of the cuts described aboveare problematic, many other proposed cutsin this bill are actually steps in the right direc-tion. For example, the law reduces MedicarePart D subsidies by $10.7 billion for high-income recipients. This means that individu-als with incomes over $85,000 and coupleswith incomes over $170,000 will no longerhave their prescription drug purchases subsi-dized by taxpayers.
In addition, the law will eliminate part of a Bush-era subsidy for businesses that includeprescription drug coverage in retiree healthplans. 152 Since 2006, as part of the Medicareprescription drug program, companies havereceived a federal subsidy for 28 percent (up toa cap of $1,330 per retiree) of the cost of pro- viding prescription drugs to retired workers. 153
The subsidy was justified on the grounds thatcompanies would otherwise dump workersinto Medicare, raising the cost of the Part D,prescription drug plan. However, not only didbusinesses receive the subsidy, they were alsoallowed to deduct the subsidy from their tax-es, receiving what was in effect a second sub-sidy. In fact, University of CaliforniaBerkeley economist Brad DeLong estimates that by making the original subsidy tax free, the feder-al government actually ends up subsidizing 63
percent of the cost of retiree drug benefits forsome companies. 154 The health care legislationretains the subsidy but eliminates the taxbreak beginning in 2013. 155
This change received a great deal of press
attention when it forced several companies,such as Caterpillar, Lockheed Martin, and AT&T, to take charges against earnings ontheir SEC filings. Altogether those chargescould total more than $4.5 billion, reflectingfuture tax costs to those companies. 156
Democrats reacted to the accountingchanges with outrage and threatened hearingson the issue. However, the charges appear to berequired under SEC rules, and Democrats laterbacked down. 157 On the other side, Republi-cans attempted to score points by warning that
the change could reduce economic growth andreduce employment. They have a point in thatthe money that the companies will now have topay in taxes is money that cannot be used toexpand operations or pay workers. However,not all tax breaks are created equal. This one, inparticular, appears to be a highly questionableform of corporate welfare.
Finally, the new law establishes a new Independent Payment Advisory Board (IPAB)which would have the power to recommendchanges to the procedures that Medicare willcover, and the criteria to determine whenthose services would be covered, provided itsrecommendations improve the quality of care or improve the efficiency of the Medi-care programs operation. 158 Starting in2013, if Medicare spending is projected togrow faster than the combined average rate of general inflation and medical inflation (aver-aged over five years), IPAB must submit rec-ommendations bringing spending back inline with that target. Beginning in 2018, theannual spending target becomes the rate of GDP growth plus 1 percent. Once IPABmakes its recommendations, Congress wouldhave 30 days to vote to overrule them. If Congress does not act, the secretary of HHSwould have the authority to implement thoserecommendations unilaterally.
Given Congresss proven inability torestrain the growth in Medicare spending, an
17
Many otherproposed cutsare actually stepin the right
direction.
-
8/9/2019 BadMedicineWP
25/61
independent commission, and a requirementthat Congress vote on the issue, could provebeneficial. Unfortunately, IPAB is prohibitedfrom making any recommendation thatwould ration care, increase revenues, or
change benefits, eligibility, or Medicare benefi-ciary cost-sharing (including Medicare premi-ums). 159 That leaves IPAB with few optionsbeyond reductions in provider payments.Hospitals and hospices would be exempt fromany cuts until 2020. 160 Thus, most of the cutswould fall on physicians. With Medicarealready under-reimbursing providers, furthersuch cuts would have severe consequences,including driving physicians from the pro-gram and increased cost-shifting to privateinsurance. More likely, therefore, IPAB will
end up as neutered as previous attempts toimpose fiscal discipline on government healthcare programs. 161
On the other side of the ledger, the legisla-tion increases subsidies under the MedicarePart D prescription drug program. A Medi-care recipient enrolled in the standard versionof the prescription drug plan currently pays a deductible of $250. Thereafter, Medicare pays75 percent of costs between $250 and $2,250in drug spending. The patient will pay the re-maining 25 percent of these costs. The patientthen encounters the notorious doughnuthole. For drug costs above $2,250 but below $3,600 in out-of-pocket spending, the patientmust pay 100 percent of the costs. After that,the prescription drug plan kicks in again andpays 95 percent of costs above $3,600. 162
The Patient Protection and AffordableCare Act ever so slowly closes this donut hole.In June, seniors enrolled in the program whohave drug costs in excess of $2,700 beganreceiving a $250 check as a partial rebate of their drug costs. 163 Starting in 2011, a slow reduction in the amount that seniors have topay out-of-pocket within the donut holebegins, eventually reducing that amountfrom the current 100 percent to 25 percent by 2020. Part of the cost of filling the donut holewill be borne by pharmaceutical companies,who will be required to provide a 50 percentdiscount on the price of brand-name drugs.
This provisions cost to drug companies hasbeen estimated at approximately $42.6 bil-lion.164 The remaining 25 percent reductionin out-of-pocket costs will come from federalsubsidies. For generic drugs, the entire out-of-
pocket cost reduction is through subsidies.In considering any of the cuts discussedabove, there are three things to keep in mind.First, cuts in Medicare are both necessary andinevitable. However, there will almost cer-tainly be an impact on the quality and avail-ability of care. For example, according toMedicares chief actuary, if the cuts were tooccur as projected, as many as 15 percent of U.S. hospitals could close. 165
Second, savings from the cuts will not beused to deal with Medicares looming budget
shortfalls, but rather to finance the new enti-tlements under the legislation. Democratshave pointed out that changes under the legis-lation, combined with new Medicare tax rev-enue, would extend the life of the MedicareTrust Fund by as much as 12 years. Whiletechnically true, this represents a very mislead-ing double counting of the savings and rev-enue.
The new funds would indeed be routedthrough the Medicare Trust Fund, where gov-ernment trust fund accounting methodology would count them as extending the trustfunds solvency. However, as has been pointedout with regard to the Social Security TrustFund, the government is structurally inca-pable of actually saving the money. In fact, thefunds would be used to purchase special issuetreasury bonds. When the bonds are pur-chased, the funds used to purchase them be-come general revenue, and are spent on thegovernments annual general operating ex-penses. What remains behind in the trust fundare the bonds, plus an interest payment attrib-uted to the bonds (also paid in bonds, ratherthan cash). Government bonds are, in essence,a form of IOU. They are a promise againstfuture tax revenue. When the bonds becomedue, the government will have to repay themout of general revenue. 166 In the meantime,however, the government counts on that new general revenue to pay for the cost of the new
18
Savings from thecuts will not be
used to dealwith Medicareslooming budget
shortfalls.
-
8/9/2019 BadMedicineWP
26/61
health legislation. Thus, the governmentspends the money now, while pretending it isavailable in the future to pay for futureMedicare benefits.
As Medicares chief actuary points out, In
practice, the improved [Medicare] financingcannot be simultaneously used to financeother Federal outlays (such as the coverageexpansions) and to extend the trust fund,despite the appearance of this result from therespective accounting conventions. 167
And third, there is ample reason to be skep-tical about whether the cuts will ever actually occur. Medicares actuary warns that the pro-posed cuts may be unrealistic. 168 The CBOitself cautions that It is unclear whether sucha reduction in the growth rate of spending
could be achieved, and if so, whether it wouldbe accomplished through greater efficienciesin the delivery of health care or through reduc-tions in access to care or the quality of care. 169
Congresss record in this regard is decid-edly mixed. As the bills proponents pointout, it is untrue to say that Congress has nev-er cut Medicare spending. At least 11 timessince 1980, Congress has passed Medicarecuts that actually did take place. 170 Most weremodest reductions in payments to certaintypes of providers, reductions in dispropor-tionate share (DSH) payments to hospitals,or small increases in cost-sharing by seniors,or in Medicare premiums. At least in limitedcircumstances, Congress has been able totrim Medicare. 171
However, Medicare is still facing a $50 tril-lion$100 trillion funding gap, and Congresshas proven itself unable to take the steps nec-essary to deal with this long-term gap. Some of the most significant cuts that have been pro-posed have later been reduced or repealed. Forinstance, in 1997, as part of the BalancedBudget Act, Congress established the sustain-able growth rate (SGR), designed to holdannual increases in Medicare reimbursementsto a manageable growth rate. But in 2002,2003, 2005, 2007, 2008, and this year (reach-ing back to 2009), Congress has overturnedprovider payment cuts that would have beenrequired by the SGR. A bill before Congress
the infamous doc fix (see below)wouldpermanently eliminate future SGR mandatedcuts. 172
In some ways the legislation is a victim of Medicare itself. Because the legislation does
nothing to reform the programs unsustain-able structure, Congress is caught betweentwo unpalatable choices. If it makes the cutscalled for under the legislation, it risks,according to the CBO reductions in accessto care or the quality of care. 173 But if it failsto make those cuts, then the legislation willadd a huge new cost to an already explodingdebt.
That is a recipe for legislative paralysis.
TaxesThe Patient Protection and Affordable
Care Act imposes more than $669 billion innew or increased taxes over the first 10years.174 These include
Tax on Cadillac Insurance Plans.One of the most heavily debated new tax-es in the health care bill was the tax onhigh-cost insurance plans. Beginning in2018, a 40 percent excise tax will beimposed on employer-provided insur-ance plans with an actuarial value inexcess of $10,200 for an individual or$27,500 for families. (The threshold isincreased to $11,850 for individuals and$30,950 for families whose head of household is over the age of 55 or en-gaged in high-risk professions such aspolice, firefighters, or miners.) The taxfalls on the value of the plan over thethreshold and is paid by the insurer, orthe employer if self-insured. 175 The bene-fit value of employer-sponsored coveragewould include the value of contributionsto employees FSAs, HRAs, and HSAs. It isestimated that 12 percent of workers willinitially have policies that are subject tothe tax. 176 However, the tax is indexed toinflation rather than the faster-risingmedical inflation, which drives insurance
19
The legislationdoes nothingto reform theprogramsunsustainablestructure.
-
8/9/2019 BadMedicineWP
27/61
premiums. As a result, more and moreworkers will eventually find their insur-ance plans falling subject to the tax. Infact, a study for the benefits consultingfirm Towers Watson concludes, Assum-ing even reasonable annual plan costincreases to project 2018 costs, many of todays average plans will easily exceed thecost ceilings directed at todays gold-plat-ed plans.177
Payroll Tax Hike. The Medicare payrolltax will be increased from 2.9 percenttoday to 3.8 percent for individuals withincomes over $200,000 for a single indi- vidual or $250,000 for a couple. 178 Thepayroll tax hike would mean that ineight states, workers would face margin-al tax rates in excess of 50 percent (seeFigure 5).179
Tax on Investment Income. Starting in2013, the 3.8 percent Medicare tax will
be applied to capital gains and interestand dividend income if an individualstotal gross income exceeds $200,000 or a couples income exceeds $250,000. 180
The tax would only apply to the amountof income in excess of those limits, butwould be based on total income. Thus, if a couple had $200,000 in wage incomeand $100,000 in capital gains, $50,000would be taxed. Moreover, the definitionof capital gains includes capital gainsfrom the sale of real estate, meaning thatan individual who sold his or her homefor a profit of $200,000 or more wouldbe subject to the tax. Given the currentweakness in the housing market, thiswould seem to create a particularly per-nicious outcome.
It is also worth noting that theObama administration has also pro-posed allowing the Bush tax cuts on cap-
20
Figure 5States with Marginal Tax Rates over 50% after PPACA
Source: Tax Foundation, Private Report.
-
8/9/2019 BadMedicineWP
28/61
ital gains to expire. Combining thatincrease with the one contained in thehealth care legislation would raise thetax rate on capital gains from 15 percenttoday to nearly 24 percent. 181 Similarly,
the top tax rate for interest on taxablebonds could rise to 43.4 percent. 182
Numerous studies have shown that highcapital gains taxes discourage invest-ment, resulting in lower economicgrowth, fewer jobs, and reduced wages.
Limit on Itemized Deductions. Begin-ning in 2013, the threshold at which tax-payers can deduct medical expenses willbe raised from the current 7.5 percent of adjusted gross income to a new floor of 10 percent. 183 The increased threshold
would be postponed until 2016 for tax-payers age 65 or older. 184 Tax on Prescription Drugs. The legisla-
tion would levy a new tax on brand nameprescription drugs designed to raise a spe-cific amount of money annually. Ratherthan imposing a specific tax amount, thelegislation identifies a specific amount of revenue to be raised, ranging from $2.5billion in 2011 to $4.2 billion in 2018,before leveling off at $2.8 billion there-after, and assigns a proportion of thatamount to pharmaceutical manufactur-ers according to a formula based on thecompanys aggregate revenue frombranded prescription drugs. 185 The struc-ture of this tax almost guarantees that itwill be passed along to consumersthrough higher prices.
Tax on Medical Devices. A 2.9 percentfederal sales tax is imposed on medicaldevices, which includes everything fromCT scanners to surgical scissors. 186 Thesecretary of HHS has the authority towaive this tax for items that are sold atretail for use by the general public. 187
However, almost everything used by doctors, hospitals, or clinics would betaxed. The tax would also fall on labora-tory tests. The governments chief actu-ary has concluded that this tax, as withthose on pharmaceutical manufacturers
and insurers would generally be passedthrough to health consumers. 188 Infact, a study by the Republican staff of the Joint Economic Committee esti-mates that the pass-through could cost
the typical family of four with job-basedcoverage an additional $1,000 a year inhigher premiums. 189
Additional Taxes on Insurers. Similarto the tax on pharmaceutical companies,the legislation imposes a tax on healthinsurers based on their market share. 190
The total assessment will begin at $8 bil-lion and rise to $14.3 billion by 2018.Thereafter the total assessment willincrease by the same percentage as premi-um growth for the previous year. 191 The
tax will be allocated according to a for-mula based on both the total premiumscollected by an insurer and the insurersadministrative costs. 192 However, someinsurers in Michigan and Nebraska received a special exemption. 193 This tax isalso expected to be passed through toconsumers through higher premiums.
Tax on Tanning Beds. The legislationimposes a 10 percent tax on tanningsalons. 194 While tanning may be seen asa luxury or frivolous expenditure, it isactually a recommended treatment forpsoriasis and certain other medical con-ditions. The law makes no distinctionbetween tanning for medical or cosmet-ic reasons. This tax goes into effectimmediately.
The combination of taxes and subsidies inthis law results in a substantial redistributionof income. The new law will cost familiesearning more than $348,000 per year, (top 1percent of incomes) an additional $52,000per year on average in new taxes and reducedbenefits. 195 In contrast, those earning$18,00055,000 per year will see a net incomeincrease of roughly $2,000 per family. 196
The new law also contains other tax-relatedprovisions that will add significantly to busi-ness costs. For example, the legislation requiresthat businesses provide a 1099 form to every
21
The combinationof taxes andsubsidies in thislaw results in a
substantialredistributionof income.
-
8/9/2019 BadMedicineWP
29/61
vendor with whom they do more than $600worth of business over the course of a year. 197
Of course businesses already have to file 1099sfor outlays on items like consultants. But thenew rule will mean that even the smallest of
businesses will have to issue a formand filewith the IRSfor virtually every purchase orpayment. The burden falls on the other partnerin the transaction, too. The business providingthe goods and services would have to collect1099s from all its customers and integratethem with the rest of its tax records. Thiswould be a significant burden even for busi-nesses with computerized record keeping. Forthe millions of small businesses that still dobookkeeping by hand, the cost in both timeand money will be devastating. Furthermore,
businesses will be required to collect all the req-uisite information from everyone they do busi-ness with, including their taxpayer ID, to filethe required form. This, in turn, poses a wholenew set of threats to privacy.
For both individual Americans and busi-nesses large and small, the Patient Protectionand Affordable Care Act is a tax and regula-tory nightmare.
The CLASS ActThe health care legislation establishes a
new national long-term care program, calledthe Community Living Assistance and Sup-port Act (CLASS Act), designed to help seniorsand the disabled pay for such services as an in-home caretaker or adult day services. 198
The CLASS Act is theoretically designed tobe self-financed. Workers would be automati-cally enrolled in the program, but would havethe right to opt out. Those that participate willpay a monthly premium that has not yet beendetermined. 199 However, the CBO estimatesthat will be roughly $123 per month for theaverage worker. 200 Other estimates suggestthat the premiums could be much higher, per-haps $180240 per month. 201 Workers mustcontribute to the program for at least fiveyears before they become eligible for bene-fits.202 (Individuals age 55 or over at the time
the program is fully implemented must notonly contribute for five years, but must beemployed for at least three years following theprograms implementation date.) 203 There isno health underwriting of participation or
premiums.The actual benefits to be provided underthe program are among the many details thatremain to be determined but will not be lessthan an average of $50 daily adjusted for infla-tion.204 Some estimates suggest that benefitswill average roughly $75 per day, or slightly more than $27,000 per year. 205 Benefits will bepaid directly to the individual, not to the ser- vice provider, based on the degree of an indi- viduals impairment, and can be used to pur-chase home care and other community-based
long-term care assistance, as well as certainnonmedical services. 206 Benefits may be paiddaily, weekly, monthly, or deferred and rolledover from month to month at the beneficia-rys discretion. 207 There is no lifetime limit tobenefits.
Theoretically, the program will begin tocollect premiums in 2011, although so many aspects of the program remain to be deter-mined that many experts predict implemen-tation could be delayed until as late as2013.208 As mentioned, there is a five-year vesting period for benefits, so there will be nopayouts until at least five years after the startof premium collections.
Eligibility for benefits will be based on thesame criteria currently used to qualify forfederal tax-qualified long-term care insur-ance benefits. That is, a person must beunable to perform at least two activities of daily living from a list of six such activities,or need substantial supervision due to cogni-tive impairment. 209 The secretary of HHSmay also develop different or additional eligi-bility requirements. 210
During the laws first five years it will col-lect premiums, but not pay benefits. As a result, over the first 10 years, the period con- veniently included in the budget scoring win-dow, the CLASS Act will run a surplus, col-lecting more in premiums than it pays out inbenefits (see Figure 6).
22
The PatientProtection and
Affordable CareAct is a tax and
regulatory nightmare.
-
8/9/2019 BadMedicineWP
30/61
Those premiums will accrue in a CLASS Act Trust Fund, similar to the Social Security and Medicare trust funds. Using trust fundaccounting measures, the premium pay-ments will reduce the federal deficit over thatperiod by roughly $70.2 billion. 211 However,thereafter, the CLASS Act will begin to pay out benefits faster than it brings in revenue. Although this time period falls outside theformal 10-year scoring window, CBO warns,In the decade following 2029, the CLASSprogram would begin to increase budgetdeficits . . . by amounts on the order of tens of billions of dollars for each 10-year period. 212CBO goes on to warn, We have grave con-cerns that the real effect of [the CLASS Act]would be to create a new federal entitlementprogram with large, long-term spendingincreases that far exceed revenues.
Trust fund accounting, of course, is littlemore than budgetary sleight of hand. Because
the government is structurally incapable of saving such surpluses, they become simply a source of current revenue for the governmentto use for whatever purpose seems most press-ing at the time. It does not provide resourceswith which to pay the future obligations thathave been created. 213 Even Senate Budget com-mittee chairman Kent Conrad (D-ND), whoeventually voted for the bill, called it a Ponzischeme of the first order, the kind of thingthat Bernie Madoff would have been proudof.214
In addition, the structure of the programcreates a huge adverse selection risk thatcould add to the programs financial instabil-ity. As the actuarial firm Milliman Associatespoints out: The voluntary aspect of the pro-gram allows low-risk individuals to never signup for the program while the guaranteedissue enables some of the highest-risk individ-uals to join the program. This is a formula
23
Figure 6Effect of CLASS Act on Federal Budget
Source: Letter from Douglas Elmendorf, Director, Congressional Budget Office, to House speaker Nancy Pelosi, March 20, 2010, and Letter from DouglasElmendorf, Director, Congressional Budget Office, to Sen. Tom Harkin, November 25, 2009.
-
8/9/2019 BadMedicineWP
31/61
that is virtually certain to create financialinstability in any insurance program unlessthere are other important provisions to con-trol risk. 215
The law tries to ameliorate the adverse
selection problem by requiring individualswho opt out of the program to pay a higherpremiumup to 250 percent higherif they later decide to opt back in. 216 But experts sug-gest that these provisions will be insufficientto prevent gaming the system. And, other pro- visions actually make adverse selection morelikely. For example, the law limits marketingcosts to no more than 3 percent of premiums.The resulting lack of marketing will likely result in a low participation rate by the publicat large, while those with health problems are
most likely to seek out the benefits. The American Academy of Actuaries estimatesthat only about 6 percent of the U.S. popula-tion will participate in the program. 217 And,Richard Foster suggests that just 2 percent of workers will participate after three years. 218
Given such low participation levels, the cov-ered population will almost certainly be farsicker than the general insurance pool. Fosterwarns that there is a very serious risk that theproblem of adverse selection will make theCLASS program unsustainable. 219
Making matters worse, the legislation capspremiums for low-income workers and under-graduate students and prohibits future premi-um hikes for some groups of retirees. 220
Therefore, if the program is to remain self-sus-taining, other workers will have to bear a dis-proportionate share of future premium hikes.That in turn increases the risk that programpremiums will exceed those for products avail-able in the private market. Healthier individu-als, in particular, would have an incentive toflee the program for less expensive privatealternatives, leaving only the sickest and mostexpensive participants in the government plan.The adverse selection death spiral would be infull force, which could tempt the governmentto solve the problem by making participationmandatory, forcing Americans into a programthey may not want and to which there are supe-rior private alternatives. 221 The only other alter-
native will be a taxpayer bailout.The CLASS Act, therefore, while little
debated, may represent one of the health carelegislations biggest fiscal time bombs.
Growing the Nanny State A little-discussed provision of the health
care legislation requires restaurant chains withat least 20 locations or franchises to post calo-rie counts next to prices on menus, menuboards, and drive-through menus. In addition,restaurateurs would be required to post a brief statement regarding daily caloric intake andadvise guests that additional nutrition infor-mation is available. Other nutrition data,
which must be available on request, wouldinclude calories from fat, total fat, saturatedfat, cholesterol, sodium, carbohydrates, sug-ars, dietary fiber and protein. 222 More than200,000 establishments will be affected by thechange. 223 The law also requires nutritioninformation to be posted on food and bever-age vending machines. 224
There is no doubt that the United Stateshas a serious obesity problem. 225 However,posting calories is unlikely to have a signifi-cant impact. Studies show that only about 56percent of chain restaurant customers saidthey even notice posted calorie information,while even fewer, just 15 percent, take thecalorie information into account when mak-ing their choices. 226
But, while they are unlikely to significant-ly reduce obesity, the new regulations willimpose a cost on restaurants and consumers.Estimates suggest that the cost of analyzingcalories runs as high as $1,000 per menuitem. 227 In addition there will be the cost of changing all those menus and signs. And, thecost of posting the information on vendingmachines has been estimated to be at least$56.4 million for the first year. 228
While the financial cost of this provisionis not substantial, especially in the context of other taxes and regulatory costs imposed by this law, it does represent yet another blow against individual responsibility.
24
The CLASS Actmay represent
one of the healthcare legislations
biggest fiscal timebombs.
-
8/9/2019 BadMedicineWP
32/61
Other ProvisionsThe legislation includes a number of pilot
programs designed to increase quality of
health care or control costs. Most are wellintentioned but unlikely to have significantimpact, especially in the short term. Thesewould include programs such as bundled pay-ments, global payments, accountable-careorganizations and medical homes throughmultiple payers and settings. 229 It would alsocreate a new Center for Innovation within theCenters for Medicare and Medicaid Services(CMS) to evaluate innovative models of care,and would require CMS to develop a NationalQuality Strategy to improve care delivery,
health outcomes and population health.230
The federal government would also pro- vide grants to states for incentives for Medic-aid beneficiaries to participate in healthy-lifestyle programs. A state option would enrollMedicaid beneficiaries with chronic illnessesinto health homes that offer comprehensive,team-based care, and a new optional Medicaidbenefit would allow people with disabilities toreceive community-based services and sup-ports. 231 Other grants would provide incen-tives for states to shift Medicaid beneficiariesaway from nursing homes and toward care inthe home or community. 232
The law would also reward hospitals forproviding value-based care, and penalize hos-pitals that perform poorly on quality mea-sures such as preventable