Sentinel Lymph Node Biopsy Versus Axillary Clearance in Operable
Axillary lymph node status in carcinoma of the breast
-
Upload
vanessa-lewis -
Category
Documents
-
view
212 -
download
0
Transcript of Axillary lymph node status in carcinoma of the breast

JOURNAL OF PATHOLOGY, VOL. 155: 221-224 (1988)
AXILLARY LYMPH NODE STATUS IN CARCINOMA OF THE BREAST
VANESSA LEWIS AND PAUL RICE
Department of Pathology and Surgery, Southampton University General Hospital, Southampton SO9 4XY, U.K.
Received 20 November 1987 Accepted 12 January 1988
SUMMARY In this prospective study, axillary clearance specimens from consecutive routine mastectomies and wide excisions for
carcinoma were divided into three segments by sutures in the theatre: apical (furthest from the tumour), mid and basal (nearest to the tumour) segments. Each specimen was then randomized to either formalin or Carnoy's fixation. Following fixation, lymph nodes were dissected from each of the three segments, sectioned once through the hilum, and examined microscopically.
There was a significant (P<0.05) difference in the total number and number of reactiire lymph nodes harvested from Carnoy's compared with formalin-fixed material. The number of nodes containing metastatic carcinoma was not significantly different (P= 0.64).
In several cases, involved apical segment lymph nodes were found with no involvement of the proximal groups; this observation may have serious implications for the procedure of proximal lymph node sampling in the surgical manage- ment of breast cancer. It is suggested that clearing of axillary contents with Carnoy's fixative does not provide any additional information of clinical significance, although it may allow the pathologist to identify lymph nodes rapidly.
KEY WORDS-Breast carcinoma, lymph nodes, fo rmah fixation, Carnoy's fixation.
INTRODUCTION
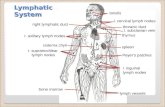
Metastatic involvement of the axillary lymph nodes remains the most powerful prognostic factor in breast cancer,'-5 although many other estab- lished determinants of prognosis, such as tumour size,5 local skin inv~lvement,~.~ and tumour growth rate,7 are recognized. Up to 1968, prog- nosis was related only to the presence or absence of axillary lymph node involvement, but the first clini- cal trial of the National Surgical Adjuvant Breast and Bowel Project (NSABP) reported that greater numbers of involved axillary lymph nodes were associated with a less favourable outcome. The trial grouped patients into those having 1-3 nodes or greater than or equal to four nodes, involved by metastatic tumour. In 1983, an NSABP update trial concluded that further subdivision of those with
Addressee for correspondence: Dr Paul Rice, Department of Pathology, Medical Division, Chemical Defence Establishment, Porton Down, Salisbury, Wiltshire SP4 OJQ, U.K.
0022-341 7/88/07022 1 4 4 $05.00 0 1988 by John Wiley & Sons, Ltd.
greater than or equal to four positive nodes was required for increased prognostic precision, and subdivided patients with greater than or equal to 13 positive nodes.'
There still remains dispute as to what constitutes an adequate pathological study of the axillary clear- ance specimen. Hand dissection with visual and tactile inspection of the fresh or formalin-fixed specimen is the usual method of identifying nodes in such specimen^.^ This is, however, a difficult and tedious procedure due to the presence of fatty tissue and the generally small size of the lymph nodes present. The number of nodes dissected is clearly related to the skill and enthusiasm of the path- ologist. It is possible to use clearing agents, which render fat translucent and facilitate lymph node dissection."
Although there have been previous studies on the use of various clearing agent^,^"' the benefits of clearing the axillary specimen with Carnoy's fixative have not been previously investigated, to the authors' knowledge. The aim of this study was to investigate whether clearing the axillary fat with

222 V. LEWIS AND P. RICE
Table I-Carnoy’s versus formalin fixation
Fixative Mean number of lymph nodes dissected
Reactive Malignant Total
Carnoy’s fixative (n = 28) 12.9 2.3 15.2 Formalin fixation (n = 28) 9.9 2.9 12.8 Two sample t-test P valueI7 0.01 NS 0.05
Carnoy’s solution as compared with routine fix- ation in formalin leads to a more accurate assess- ment of axillary lymph node status.
MATERIALS AND METHODS
This was a prospective study of consecutive patients admitted to the Professorial Surgical Unit for either wide excision or simple mastectomy, with full axillary clearance, for breast carcinoma (stages I and 11). A standard axillary clearance was per- formed on every patient. The operating surgeon marked the apical (furthest from the tumour), mid, and basal (nearest to the tumour) portions of the resected axillary specimen with black sutures for orientation in the pathology laboratory. The speci- men was placed in either Carnoy’s (a mixture of 60 per cent ethyl alcohol, 30 per cent chloroform, and 10 per cent glacial acetic acid by volume) or forma- lin fixative; random selection of the fixative was implemented by the sealed envelope technique.
The axillary specimens were allowed to fix for 24-48 h at room temperature and were then divided into apical, mid, and basal segments by making in- cisions across the specimen equidistant to the three tied sutures. All detectable lymph nodes were harvested from each portion, sectioned once through their hilar regions, and placed in three separate, labelled cassettes according to their site of origin in the original specimen. Care was taken to avoid duplication of nodes by incomplete or partial removal and, within reasonable limits, the same dis- section time was allotted to each case ( 1 5-20 min).
All lymph nodes were embedded in paraffin wax, cut to 4pm sections, and stained routinely with haematoxylin and eosin. The numbers of reactive and/or lymph nodes containing metastatic tumour harvested from each segment of the axilla were recorded following histological examination by both authors.
RESULTS
General group data The study consisted initially of 60 patients but the
number of specimens examined totalled 56, four specimens being excluded as these were dissected, in error, by pathologists other than the authors. There was equal randomization between Carnoy’s and formalin fixatives.
The median age of the patients was 60.5 years; range 32-78 years. Thirty-five (58 per cent) patients had carcinoma of the left and 24 (40 per cent) of the right breast. A single patient was found to have bi- lateral disease. Twenty-two (39 per cent) of patients were found to have metastatic involvement of the axillary lymph nodes on histological examination. No correlation was found between the site of the primary tumour and the presence or number of lymph nodes containing metastases.
Carnoy ’s versus formalinjixation The mean numbers of total, reactive, and meta-
static deposit containing lymph nodes for each of the two fixatives are summarized in Table 1 . There was a significant difference in mean total number (P<O.O5) and the mean number of reactive (P< 0.01) lymph nodes harvested from Carnoy’s as compared with formalin-fixed material. The mean number of nodes containing metastases was not significantly different (P= 0.64).
Distribution of lymph nodes containing metastases A total of 56 specimens were dissected, and 22 (39
per cent) contained lymph nodes with deposits of metastatic tumour. The distribution of these lymph nodes is summarized in Table 11.
DISCUSSION
Comparison o f j i xa t ives Clearing of axillary fat has been shown to yield a
greater number of dissected lymph nodes than

AXILLARY LYMPH NODES AND BREAST CARCINOMA 223
Table 11-Distribution of lymph nodes containing metastases
No. of Percentage of Zone containing metastases* patients patients with metastases
1,2, and 3 2 and 3 3 only 1 and2 2 only, ‘skip lesions’ 1 only
27.3 22.7 4.5
22.7 18.3 4.5
22 100.0
*Zone 1, apical. Zone 2, mid. Zone 3, basal.
routine formalin fixation;“”’ however, the prog- nostic and therapeutic importance of the additional data is ~ n c e r t a i n . ~ , ’ ~ - ’ ~ Carnoy’s fixative is a clear- ing agent whose value in the fixation, and subsequent dissection, of axillary specimens is previously unassessed.
The study results show that Carnoy’s fixation yields a significantly greater number of lymph nodes as compared with formalin fixation (P< 0.05). However, while a significantly greater number of reactive nodes were dissected from Carnoy’s- fixed material ( P < 0.0 l), no significant difference was found in the number of lymph nodes contain- ing metastatic tumour (P= 0.64). Hence, the extra lymph nodes dissected were reactive rather than involved and, therefore, of no prognostic significance.
Carnoy’s solution was found to be advantageous compared with formalin in that it allowed easier and more rapid identification of lymph nodes. There are, however, several practical disadvantages encoun- tered with Carnoy’s solution. The content of chloro- form renders the solution highly flammable, necessitating care in handling and storage. The solution is corrosive and must be stored and used in glass rather than the usual, cheaper plastic con- tainers. Tissue penetration, compared with forma- lin, is poor. Finally, Carnoy’s solution, on the basis of current laboratory prices, is approximately 18 times more expensive per given volume than formalin.
Distribution of axillary lymph node metustuses
Lymph nodes containing metastatic tumour deposits were found in 22 (39 per cent) patients. In
ten of these patients (45.4 per cent), the involved lymph nodes were situated in the axillary zones 1 and 2 , thereby giving rise to ‘skip lesions’, where proximal lymph nodes are not involved. It would seem from current lymph node sampling procedures undertaken at surgery in some centres that zones 2 and 3 described in this study would be sampled, and that zone 1 would be completely unsampled. Only one of our patients showed metastatic deposits which skipped zones 2 and 3 completely (Table 11). However, in nine patients, nodal metastases were found in zones 1 and 2 only. It is not possible to ascertain the proportion of these that would be missed if lymph node sampling, rather than full axillary clearance, had been carried out. Our figures compare favourably with those reported previously by Forrest et aZ.’* if we assume that his zonal description is similar to that employed in this study (Table 111).
Table 111-Incidence of axillary ‘skip lesions’
Study Site of metastases
Zones 1 and 2 Zone 1 only
Present study 9/56 (16%) 1/56 (2%) Forrest et a1.18 5/43 (12%) 1/43 (2%)
The order of incidence of ‘skip lesions’ may be low enough to make axillary lymph node sampling an acceptable operative policy. However, for the advocates of adjuvant therapy and teaching centres

224 V. LEWIS AND P. RICE
conducting long-term research programmes regard- ing the treatment of breast cancer, axillary clearance must remain the definitive procedure, providing the most accurate nodal assessment in these patients.
In conclusion, we suggest that although Carnoy’s fixation allows for rapid identification of axillary lymph nodes, since it fails to reveal additional prog- nostic information, penetrates tissue poorly, is diffi- cult to handle, and is significantly more expensive than formalin, its use in the routine fixation and dissection of axillary clearance specimens cannot be justified at the Dresent time.
I .
2.
3.
4.
5.
6.
7.
REFERENCES Rosen PP, Saigo PE, Braun DW, Weathers E, Kinne DW. Prognosis of stage 11, (Tl, N1, MO), breast cancer. Ann Surg 1981; 194 576-584. Adair F, Berg J, Jourbert L, Robbins GF. Long- term follow-up of breast cancer patients. The 30 year report. Cancer 1974; 33 1145-1 150. Urban JA. Changing patterns of breast cancer. Cancer 1976; 37: 11 1-1 17. Valegussa P, Bonadonna G, Veronesi V. Pattern of relapse and survival following radical mastectomy. Cancer 1978; 41: 1170-1178. Fisher B, Raudin RG, Ausman RK, et al. Surgical adjuvant chemotherapy in cancer of the breast: results of a decade of co-operative investigation. Ann Surg 1968; 168: 337-356. Haagensen CD. Diseases of the Breast. 2nd ed. Philadelphia: W. B. Saunders, 1971. Kusama S, Spratt JS, Donegan WL, Watson FR, Cunningham C. The gross rates of growth of human mammary carcinoma. Cancer 1972; 30: 594-599.
8. Fisher B, Bauer M, Wickerham DL, Redmond CK, Fisher ER. Relation of number of positive axillary lymph nodes to the prognosis of patients with primary breast cancer. Cancer 1983; 52: 1551-1557.
9. Durkin K, Haagensen CD. An improved technique for the study of lymph nodes in surgical specimens. Ann Surg 1980; 191: 419-429.
10. Bancroft JD, Stevens A (eds). Theory and Practice of Histological Techniques. Edinburgh: Churchill Livingstone, 1977.
11. Monroe CW. Lymphatic spread of carcinoma of the breast. Arch Surg 1948; 57: 479-486.
12. Davis HH, Neis DD. Distribution of axillary lymph node metastases in carcinoma of the breast. Ann Surg
13. Symmers WStC. Unpublished observations 1953- 1955. In: Payling Wright G, Symmers WStC, eds. Systemic Pathology, Vol. 1. London: Longmans Green, 1009-1 010.
14. Morrow M, Evans J, Rosen PP, Kinne DW. Does clearing the axillary lymph nodes contribute to accur- ate staging of breast carcinoma? Cancer 1984; 53:
15. Hartveit F, Samonsen G, Tangen M, Halvorsen JF. Routine histological investigation of the axillary lymph nodes in breast cancer. Clin Oncol 1982; 8:
16. Kingsley WB, Peters GN, Cheek JH. What consti- tutes adequate study of the axillary nodes in breast cancer? Ann Surg 1985; 201: 31 1-314.
17. Snedecor GW, Cochran WG. Statistical Methods. 6th ed. Ames: Iowa State University Press, 1967.
18. Forrest APM, Stewart HJ, Roberts MM, Steele RJC. Simple mastectomy and lymph node sampling (pec- toral node biopsy) in the management of primary breast cancer. Ann Surg 1982; 196 371-377.
1952; 136 604-609.
1329-1 332.
121-126.