Arsha kc001 hyd
-
Upload
ayurmitra-ksrprasad -
Category
Documents
-
view
4.048 -
download
31
description
Transcript of Arsha kc001 hyd
A STUDY OF THE EFFECT OF
HARITAKYADI LEHYAM IN ARSHOROGA
DISSERTATION SUBMITTED IN PARTIAL FULFILMENT FOR THE DEGREE OF
DOCTOR OF AYURVEDIC MEDICINE – M.D. (AYURVEDA)
BY
DR.Ch.SADANANDAM
GUIDE
Dr.V.VIJAYA BABU M.D. (Ay.)
READER, KAYACHIKITSA, P.G. UNIT
DEPARTMENT OF KAYACHIKITSA, P.G. UNIT
DR.B.R.K.R.GOVERNMENT AYURVEDIC COLLEGE / HOSPITAL
HYDERABAD
AFFILIATED TO Dr. N.T.R. UNIVERSITY OF HEALTH SCIENCES,
VIJAYAWADA
2007
NTR UNIVERSITY OF HEALTH SCIENCES VIJAYAWADA, A.P.
DEPT. OF KAYA CHIKITSA
POST GRADUATE UNIT
Dr.B.R.K.R. GOVT. AYURVEDIC COLLEGE / HOSPITAL ERRAGADDA, HYDERABAD, A.P. ; INDIA
Date: 14.05.2007
Place: Hyderabad
C E R T I F I C A T E
This is to certify that Dr.Ch.Sadanandam, student of Dept. of
Kayachiktsa M.D. (Ayurveda) has worked for the dissertation on the topic
“A Study of the effect of HARITAKYADI LEHYAM in ARSHOROGA”
as per the requirements of the ordinances laid down by the University of
Health Sciences, Vijayawada, for the purpose. The topic is duly approved by
the Academic council of the University.
I am fully satisfied with his work and hereby forward this
dissertation for evaluation of the adjudicators.
Dr. Prakash Chander M.D.(Kayachikitsa)
Prof. & Head of the Dept. of Kayachikitsa, Post-Graduate Unit
Dr.B.R.K.R.Govt. Ayurvedic College Erragadda, Hyderabad
NTR UNIVERSITY OF HEALTH SCIENCES VIJAYAWADA, A.P.
DEPT. OF KAYA CHIKITSA
POST GRADUATE UNIT
Dr.B.R.K.R. GOVT. AYURVEDIC COLLEGE / HOSPITAL ERRAGADDA, HYDERABAD, A.P. ; INDIA
Date: 14.05.2007
Place: Hyderabad
C E R T I F I C A T E
This is to certify that Dr.Ch.Sadanandam, student of Dept. of
Kayachiktsa M.D. (Ayurveda) has worked for the dissertation on the topic
“A Study of the effect of HARITAKYADI LEHYAM in ARSHOROGA”
as per the requirements of the ordinances laid down by the University of
Health Sciences, Vijayawada, for the purpose. The topic is duly approved by
the Academic council of the University.
I am fully satisfied with his work and hereby forward this
dissertation for evaluation of the adjudicators.
Dr.V.Vijaya Babu M.D.(Kayachikitsa)
Reader, Dept. of K.C., P.G.Unit Dr.B.R.K.R.Govt. Ayurvedic College
Erragadda, Hyderabad
ACKNOWLEDGEMENTS
At the outset, I would like to express my thankfulness to Dr.Prakash
Chander, Profesor and Head of the Department of Kaya chikitsa,
P.G.Unit, for his guidance and co-operation.
The satisfaction and euphoria that accompany the successful
completion of any work would be incomplete without mentioning those
people who made it possible with their constant guidance and
encouragement crowned my efforts with success. I would like to express my
gratitude to my Guide Dr.V.Vijaya Babu, Reader, Department of
Kayachikitsa, P.G. Unit, for his valuable guidance and co-operation
extended during the clinical study, without which it is impossible to
complete this dissertation work.
I would like to thank Dr.V.A.S.Chary I/c Professor and H.O.D.
Dept of Shalya, for his co-operation, and I am especially thankful to
Dr.S.Sarangapani, Asst. Professor for his guidance and timely suggestions
in M.O.T. I am also thankful to B.Satyanarayana, Technical Assistant for
his help.
Words carry no meaning when it comes to acknowledge the help and
support I got from my teachers Dr.M.Srinivassulu, Professor,
Dr.M.L.Naidu, Reader, Dr.S.Jayaprakash, Professor, Dr.Bhaswanta
Rao, Dr.B.Venktaiah, Reader, Dept.of Shalakya, Dr.Philip Anand
kumar, Reader, Dept.of Dravyaguna, Dr.V.R.K.Murthy, Asst.Professor,
Dr.K.Ravinder, Asst.Professor, Dr.E.Anilkumar, Asst.Professor,
Dr.Ramalingeshwar Rao, Technical Assistant and Dr.P.Raghupathi
goud they were there to help me out from many intricacies that used to prop
up in my mind during this dissertation work
My grateful acknowledgements to our Principal Dr.M.Sadasiva Rao
and Hospital Superintendent Dr.L.R.K.Murthy, for providing excellent
working atmosphere.
I am thankful to all my friends & colleagues who supported and
encouraged in every way to get away from some bitter experience and
boosted my confidence. Special thanks to Dr.N.Sridhar Sarma,
Dr.M.Surya Prakash, Dr.Ch.Ravi Kumar, Dr.D.Rama Gopal and
Dr.Binod Kumar Singh.
I avail this opportunity to express my deepest love to my family
members, my wife Sunitha and my children Sujith Chakra, Shilpa Chakra
and Shirish Chakra. They have always been my pillar to my strength and
support.
I am also very much thankful to the librarians of college and research
libraries for their cooperation.
And last but not the least are my patients without whom the work will
not be completed, for which I am very much indebted to all of them.
Dr.Ch.Sadanandam
INDEX
Name of the chapter Page No
SECTION I DISEASE PROFILE
1. Introduction 1
2. Review of Sareeram 7
3. Classification 25
4. Nidanam 30
5. Poorva Roopam 38
6. Roopam 40
7. Samprapti 55
8. Rugvinischayam 57
9. Sadhya-Asadhyata 60
10. Upadravas 61
11. Chikitsa 62
12. Pathya-Apathyas 72
SECTION II DRUG REVIEW
13. Haritakyadi Lehyam 73
SECTION III CLINICAL STUDY
14. Material and Methods 90
15. Observation and Results 92
16. Discussion and Conclusion 98
17. Summary 103
18. Special Case sheet
19. Bibliography
1
INTRODUCTION
Ayurveda is the “Science of Life” that is which helps in achieving a
longer life span by preventing the occurrence of diseases as well as curing it
to the possible extent if occurred. Thus it is established that maintenance of
‘Swasthya’ or health is the aim of Ayurveda.
The condition other than ‘swasthya’ is ‘vyadhi’ i.e. disease (dis-ease).
Susrutha1 mentioned ‘Ashtamaha Vyadhis’ viz. vata vyadhi, prameha,
kushta, arshas, bhagandaram, asmari, mudhagarbha and udara. Vagbhata2
also mentions Ashtamaha gadas, differeing from Susrutha, that he mentions
Grahani instead of Mudhagarbha. The reason for these being considered as a
special category is the intensity of suffering caused by them and the
difficulty in treating them, hence the term ‘Mahagadas’.
The paryayas of vyadhi are all attributable to these Ashta mahagadas
i.e. vyadhi = it causes vividha dukhas; amaya = generally caused due to ama;
gada = which is caused due to aneka karanas; atanka = krichra jeevana due
to dukha i.e. sorrowful, miserable life; yakshma = roga samuha; jwara =
causes tapa of both deha and manas; vikara = a state in which pancha
gnanendriyas, pancha karmendriyas and manas are all diverted from their
natural activities; roga = ruja yuktata i.e. painfulness; papma = papa
samudbhavam; dukham = upatapakatwam, i.e. uneasiness; abadham = peeda
of kaya and manas.3,4
It is not only that the above mentioned vyadhis are themselves painful
but they are also causative factors to many other vyadhis as well as
complications or upadarvas.
2
Arshas is one of these and the incidence of the disease is on the rise
due to Specific life style and aetiological factors like – heredity, work
timings, irregular food habits, spicy foods, controlling urges (vega dharana),
excess sexual indulgence, etc.
Therefore this disease is selected for special study.
Susrutha samhitha advocates the management of Arshas under four
headings – Oushadha, Kshara, Agni and Shastra Chikitsas. Of these four the
first and foremost is the Oushadha chikitsa and the remaining are to be
considered when it is out of range of medicines. It is also true that a case
selected for surgery will also be advised medical regimen to avoid
recurrence of the disease.
Charaka specially mentions that Oushadha chikitsa is being described
because there is chance of relapse of arshas treated in other three ways,
‘Punarviruho rudhanam’ is the term he uses.
Susrutha samhitha also mentions that ‘oushadha can be tried even in a
case where surgery is advised, but surgery should not be the option when
the vyadhi is oushadha sadhya’. This sutra holds good for all the times.
The yogam ‘Haritakyadi Lehyam’ is selected for the study. It is
taken from the texts ‘Bhava Prakasha’5 and ‘Bhaishajya Ratnavali’6.
Ayurveda mentions ‘aptopadesha’ as the first step of gaining
knowledge and Bhava Prakasha and Bhaishajya Ratnavali are famous
Ayurvedic text full of excellent ‘Gem’ like yogas.
3
Haritakyadi Lehyam - The yoga contains simple dravyas – Haritaki
– 7parts, Sunthi – 6parts, Nimba beeja – 5parts, Karanja beeja – 4 parts,
Indrayava – 3 parts, Chitramula – 2parts, Saindhava lavana – 1part and
Gudam – 8parts, which possess the dravya gunas said in chikitsa pada
chatushtayam, i.e. they are abundantly available, have many gunas, can be
made into various forms and are also cost effective. They are non-toxic
hence do not need any sodhana procedures; they are not drastic (teekshna)
too. The yogam is in ‘lehyam’ form which is palatable, hence can be given
to all age groups, and in the required ‘matra’ it is accepted from the patient’s
side. The ‘Oushadha guna kala avadhi’ i.e. shelf life for lehyas is said to be
one year. Therefore it can be prepared in bulk at once, preserved and used
throughout the year.
Paryayas and Niruktis
Arshas, Gudamkura, Gudakeela, Durnama (Rajanighantu),
Durnamakam (Amarakosam).
Arshas –
(1) “Arivat pranan srunoti hinasti iti arshas” i.e. the disease which
tortures like enemy. The word arshas is derived from the ‘SRU - himsayam”
dhatu.7
(2) “Arivat praninam syati tanu karoti it arshas” i.e. it makes the
patient shrink as if a person in the hands of an enemy.7
(3) “Rupamiyarti udgachati iti arshas” i.e. that which makes the
patient appear ugly (because of the complications of impaired agni).7
(4) “Arivat pranino mamsa kilaka visasanti yat,
Arshamsi tasmaduchyante guda marga nirodhatah” i.e. arshas are
protrusions of mamsa which obstruct guda marga and torture the peson like
enemy.8
4
Gudankura – “ankyate lakshyate iti ankurah” i.e. that which is seen or
observed, having its own entity, like a sprout.9
Gudakeela – “Keela is a synonym of agni; keela bandhane, gati
nirodhane” i.e. this indicates the importance of vitiation of agni in this
vyadhi, as well as the symptom mala badhata caused by it.10
Durnama – “Paparogatvena prasiddhataya dushtam nama asya iti
durnamakam” i.e. it is considered as a dushta or neecha vyadhi because papa
is thought be the causative factor, therefore rogi cannot reveal its existence.11
Arsho Adhishthanam
Mainly the Arsho roga is originating in the valis of guda10. But other
than gudavalis arshas is formed in nasa, sira, shishna, karna, netra, gala,
yoni, mukha, talu, vartma and over the twak12. The arshas over twak is
called charma keela or adhimamsa. Arshas on shishna, yoni, garbhasaya are
called as lingarshas.
According to Vagbhata arshas is originating from the gudavali and
obstructs the pureeshavaha srotas giving disturbance in guda like enemy and
also arshas is formed at guda due to vitiated vatadi tridoshas along with the
vitiation of twak, mamsa and medas13.
Doshas in arshas
Panchatma Marutah, Pittam and Kapham – that all the panchavidha
vatas, panchavidha pittas and Panchavidha kaphas are involved in the
causation of the Mahavyadhi Arshas14.
5
Dushyas of arshas
Charaka as well as Madhava Nidana mentioned that the dushyas of
arshas are twak, mamsa and medas.15
Historical aspect
History starts from the vedic literature. In Rigveda there are
references about the manifestation and treatments for the disease originated
in guda. Reference of agnikarma in durnamaroga is also available in
Rigveda. Arshas is mentioned in Krishnayajurveda, which is related with
Vyshampayana descriptions about the diseases like arshas, sleepada,
hrudroga, kushta, sodha are mentioned in Krishnayajurveda. Reference
about ano-rectal disease and their management is specially described in
Atharvanaveda. The Garuda purana possesses knowledge about the systemic
disorders, in which arshas is also described. In the period of Lord Buddha,
kings have promoted ayurveda as a social science. Ayurvedic literature is
categorized as Samhita kalika, Sangrahakalika and recent one.16
The Brihattrayi: Charaka samhita, Susruta samhita and Astanga
Hrudaya are the good resources from the samhita kala.
As per the knowledge available, the earliest description about arshas
was given by Agnivesa in his Agnivesa tantra. Years later Charaka reset the
Agnivesa tantra into a detailed treatise in which he gave much importance
for oushadha chikitsa.
Between 600 and 1000BC Susrutha, The father of Surgery elaborated
fourfold chikista of arshas as oushadha, kshara, agni and shastra karmas.
6
Vagbhata, in his Astanga hrudaya made a compilation work from
Susruta samhita and Charaka samhita, which comprises more practical
aspects of the both.
The Laghu trayee: Madhava nidana, Sarangadhara samhita and Bhava
prakasa are the Laghutrayee followed the Brihatrayee, possessing literature
about arshas.
References about arshas are available in other texts such as Bhava
Prakasha, Bhaishajya ratnavali, Chakradatta, Rasaratna samuchhaya,
Gadanigraha, Yogaratnakra and Basava Rajeeyam.
According to Vagbhata arshas is originating from the gudavali and
obstructs the pureeshavaha srotas giving disturbance in guda like enemy and
also arshas is formed at guda due to vitiated vatadi tridoshas along with the
vitiation of twak, mamsa and medas.
7
REVIEW OF SAREERAM
The summary of the Ayurvedic descriptions regarding sareera aspect
of guda, is as follows –
Utpathi (origin) – Charaka says that Guda is a Mridu and Matruja
avayava and is formed from the uthama sara bhaga of rakta and kapha,
digested by the pitta and vayu, giving it a hollow or tubular structure.17
Sthana (location) - Charaka mentions Uttara guda and Adhara guda as
parts of the fifteen Koshtangas. Chakrapani’s vyakhya on this says that
Uttaraguda is where pureesha is stored and Adharaguda through which
pureesha passes out i.e. excreted.18
Charaka in the context of Uttara Vasti, describes the location of Vasti
– Vasti is located between Mushkas, Sthula guda, Sevani and Sukra and
Mutra vaha Nadis.19
Vagbhata says that Guda is Sthulantra pratibaddha, through which
vata and pureesha move out and abhighata to it causes sadyomaranam.20
According to Susrutha – Guda, Vasti, Vasti shiras, Vrushans and
Pourusha granthi are Eka sambandhi and are related to Gudasthi vivara21;
there are Dwa trimsat22 (32) siras in Sroni supplying Guda and Medhra;
Guda is Sthulantra pratibaddha (joined proximally with Sthulantra), Ardha
panchangulam (four and half angulas in length), Adhi ardha angula trivalaya
sambhuta (formed with three valis, each one and half angula in length) and
namely Pravahini, Visarjini and Samvarani.23
8
Guda is Chaturangula ayata (four angulas in diameter), and has three
valis, all of which are tiryak, ekangula, ucchrita (lie horizontally, one above
the other, in one angula distance). They are like Sankha avartas (the spiral
grooves of a Conch), and are Gajatalunibha (like the palate of an Elephant in
colour). When seen externally, taking the romas (hair) located at guda
pradesha as criteria, from the ending line of romas, one ‘yava’ inside is
located the ‘Gudaoushtha’. From this Gudaoushtha one angula inside is the
first Vali, i.e Samvarani.24
Ashtanga Hridaya says Valis are three in number; the first is
Pravahani, in between is the Visarjini and externally lays the Samvarani,
from where Gudaoushtha is one angula externally.25
Susruta and Vagbhata mentioned the length of the guda as four and
half anguli. The anguli has been standardised in BHU and it is fixed at about
2Cms. approximately. Thus the length of the guda includes the whole of the
anal canal and lowers 6Cm of the rectum, which extends upto the inferior
Houston’s valve roughly. The total length of the anorectal canal from the
anal margin to the recto sigmoid junction is known to be about 16.5Cm. Out
of which 3Cm. is the anal canal itself. Thus guda includes anal canal and a
part of rectum.
Susruta’s opinion about these three valis is anatomical as well as
physiological. Middle Houston’s valve, internal and external sphincters also
take important part in the complete act of defaecation.
Commentators on Susruta samhita come out through different ideas
about the valis. Dr.Ambikadatta Sastri has supposed Samvarani vali and
Visarjini vali as sphincter ani internal and sphincter ani external
9
respectively. According to vaidya Ranjeet Rai Desai, the piles are to occur ½
inch above the gudostha even though all the three valis are affected. He
found that vali thrayee are rather above to the folds described in modern
anatomy.26
The earlier work of Dr.V.S.Patil who enlightened on marma at BHU
has come out with a clear explanation that instead of Houston’s valves, the
lower part of the ampulla of rectum with internal and external sphincters
may be taken as three valis respectively, based on physiological importance
rather than structural importance.
According to B.G.Ghanekar the two peshis which are round in shape
and meant for closing of guda are called as samvarani vali and situated
externally.
Pravahani: This is the first vali and is situated in the proximal part of
gudanalika and is about 1½ inch above the Visarjinivali. Since it initiates the
vega of pureesha pravartana (sensation of expulsion) and pushes (pravahana)
the pureesha downwards, it is called Pravahani.
‘Pravahanyastu pravahanam’ – Dalhana27
This is the middle one third of the rectum or the upper half of the
ampullary part of the rectum. The beginning or the proximal end is indicated
by the presence of the second Houston’s valve. The distance from the second
to the third houston’s valves is about 3 to 4cm. which is similar to the
Ayurvedic decription. The mucous membrane of this part of the rectum is
pale pink in colour, which is semi-transparent and branching radicles of the
superior rectal vessels are seen through it. The mucosa normally presents a
smooth velvetty appearance due to the myriads of tiny opening in to the
10
crypts of Leiberkuhn. In empty condition of the rectum the mucous
membrane presents a number of longitudinal folds, which are obliterated
when the rectum is distended and are the reason for the maximum diameter
of the ampullary part of the rectum, than any other part of the colon. The
blood supply is derived primarily from the superior rectal artery, which is
the continuation of the inferior mesenteric artery. Some supply is also
received from the middle rectal and median sacral arteries. The venous
drainage is through the superior rectal (Haemorrhoidal) veins, which drain
into the portal system via the inferior mesenteric vein. The superior, middle
and inferior rectal veins converge to form the internal rectal venous plexus
or haemorrhoidal plexus in the submucosa of the columns of Morgagni and
dilatation of this plexus gives rise to internal haemorrhoids.
The middle Houston’s valve which lies at the upper end of the rectal
ampulla and is the largest and the most constant one. Hence Ayurvedic
Acharyas had given it great importance and considered as a landmark.
The faecal matter is stored in the Sigmoid colon and at the time of
evacuation by mass peristaltic movements it enters the ampulla of the rectum
and the person feels the urge for defaecation and ‘Prvahanam’ or the effort
to defaecate occurs. Hence the name ‘Pravahani’.
Visarjini: This is the second vali situated between pravahini and samvarani
and is about 1½ inch and is in the middle portion of guda. It helps in moving
the fecal matter forward by its expansion and aids in its expulsion.
“Tasam antaramadhya Visarjini” (Vagbhata)28
“Visrujateeti Visarjini” (Dalhana)29
11
This is the last one third of the rectum or the lower half of the ampulla
of the rectum. Its beginning or proximal end is indicated by the third
Houston’s valve and the distal end by the ano-rectal ring, and its length is
about 3 to 4cm. and lies anterior to the tip of the coccyx bone and above the
pelvic diaphragm. This part is in continuation with Pravahani above and
Samvarani below. The mucous membrane of this part is pink in colour and
the tributaries of the superior and middle rectal vessels are seen through it.
The mucous membrane of this part contains longitudinal folds similar to
Pavahani. The blood supply and venous drainage are same as the Pravahani.
This is related – the base of the urinary bladder, terminal parts of the
ureters, seminal vesicles, vasa deferentia and prostate and in females with
vagina. This description correlates well with the Charaka’s and Susruta’s
description of Guda and its relations.
Samvarani: This is the third vali situated below visarjini and 1 inch above
the gudaousshtha and is the last vali. Its function is to open when faecal
matter comes from above and to close the guda after its expulsion.
“Samvaranateeti samvarani” (Dalhana)30
This part is the anal canal with internal and external anal sphincters. It
is in continuation with the rectum above and is marked by the Ano-rectal
ring. Anal canal is the terminal portion of the large intestine. It begins at the
ano-rectal ring and terminates at the anal verge. The length of the anal canal
is approximately 3cm and the diameter is also 3cm laterally it is surrounded
by ischio-rectal fossa around the sphincters and over its whole length it is
surrounded by sphincter ani muscles. The upper half of anal canal is lined by
mucous membrane and is in ‘Plum’ colour owing to the blood in the
subjacent internal venous plexus. The blood supply is from superior and
12
inferior rectal arteries of which the superior rectal arteries supply the anal
canal and the inferior rectal arteries supply the sphincter muscles and the
ischio-retcal fossae. The venous drainage is into Internal and External rectal
venous plexuses which communicate with each other and inturn drain into
superior and inferior rectal veins. Veins in the three anal columns, situated at
3, 7 and 11 o’clock positions as seen in the lithotomy position, are large and
constitute the potential sites for primary internal piles. Anal veins are
arranged radially around the anal margin. They communicate with the
internal rectal plexus and the inferior rectal veins. Excessive straining during
defaecation may rupture on of these veins, forming the subcutaneous
perianal haematoma known as ‘External piles’.
The internal anal sphincter is involuntary and the external anal
sphincter is under voluntary control. Both of these open for defaecation and
close after passing out of the faecal matter, hence the name ‘Samvarani’.
MODERN ASPECT
Anatomy of rectum and anal canal
The embryonic proctoderm provides the lining of the anal canal. This
lining being ectodermal in origin is described to form anal skin. The rectum
is derived from the hindgut. Hence the mucosal lining of the rectum is
endodermal in origin.
Rectum: The rectum constitutes the terminal segment of the colon. It’s
length varies from 12 to 15 cm and possesses a larger lumen than any other
portion of the colon. It begins at the level of the third sacral vertebra and
ending at the anal canal i.e. from the recto-sigmoid junction above to the
dentate line below. The rectum is having total three convex curves; two of
13
the curves to the right side and one convex curve at the left. The rectum
from its origin comes down following the concavity of the sacrum and
coccyx forming an antero-posterior curve which is called as sacral flexure of
the rectum. First it passes downwards and backwards then downwards and
lastly forwards to become in continuation with anal canal by passing through
the pelvic diaphragm. Above it’s junction with the anal canal it passes
through the pelvic floor, which is formed by levator ani muscle. In addition
to the antero posterior curve the rectum deviates from the midline at three
lateral curves. The upper one is convex to right, the middle one is more
convex to left and the lower one is again convex to right.
The diameter of the upper part of the rectum in empty state is 4 cm. as
at the sigmoid colon but its lower part is distended to the widest portion
known as ampulla of rectum. Peritoneum is related with rectum only to the
upper two thirds of it. The upper one third is covered is by peritoneum
anteriorly and laterally, the middle one third is covered anteriorly only. In
males the peritoneum reflects on the bladder and forms recto-vesical pouch
where as in females it reflects upon vagina and uterus which is recto-uterine
pouch or the “pouch of Douglas”.
The lower portion of the rectum is devoid of peritoneum and is
covered by fibrous sheath, which is derived from the true pelvic fascia. In
empty condition of the rectum the mucous membrane of its lower part
presents a number of longitudinal folds which affect the distension of the
rectum.
Houston’s valves: These are nothing but three spiral foldings of the mucosal
and submucosal layers which are found with in the rectum. The lowest valve
is seen in the left, the middle one in the right and the upper most one on the
14
left. Each valve arises gradually at one end for the rectal valve extending
into lumen of the gut. It then recedes at its other end into the rectal valve.
The Houston valves can be seen through the sigmoidoscopy.
The rectal mucosa normally presents a smooth velvetty appearance
due to the myriads of tiny opening in to the crypts of Leiberkuhn. The
mucous membrane of the lower part of the rectum is pale pink in colour,
which is semi-transparent and branching radicles of the superior rectal
vessels are seen through it.
Ano-rectal junction: The junction of anal canal and rectum is about two to
three cm. in front of and slightly below the tip of the coccyx. In males at this
level opposite to this there is the apex of the prostrate gland. At the ano-
rectal junction the folding back of the gut is known as the perineal flexure.
Anal canal: Anal canal is the terminal portion of the large intestine. It begins
at the ano-rectal ring and terminates at the anal verge. The length of the anal
canal is approximately 4 cm. and the diameter is 3 cm. The junction is
indicated by the pectinate line (anal valves). It provides voluntary and
involuntary sphincters at the outlet of the rectum. The external opening of
the anus is situated in the midline, posterior to the perineal body. The empty
lumen is puckered into longitudinal folds, the columns of Morgagni and they
are 5-10 or 8-12 in number. Posteriorly it contacts with a mass of fibrous and
muscular tissue known as ano-coccygeal ligament, which separates the anal
canal from the tip of the coccyx. Anteriorly, it is separated from the perineal
body, by the membranous part of the urethra and the bulb of penis in the
male and lower end of the vagina in the female. Laterally it is surrounded by
ischio-rectal fossa around the sphincters over its whole length it is
surrounded by sphincter muscles.
15
The upper half of anal canal is lined by mucous membrane and its
colour is plum owing to the blood in the subjacent internal venous plexus.
The epithelium in the region is variable in character. The mucous membrane
in this part has 6-10 vertical folds, the anal columns. Each column contains a
terminal radicle in these three sites constitute primary internal haemorrhoids.
The line along with the anal valves are situated is termed as pectinate line.
Sometimes small epithelial projections (anal papilli) are present on the edges
of the anal valves. The succeeding part of the anal canal extends for about 15
mm below the anal valves and is known as “transitional zone of pecten”.
This zone ends narrow and wavy known as White line or Hilton’s line.
Below the Hilton’s line the lower 8 mm or so of the anal canal are lined by
true skin which contains sweat glands and sebaceous glands.
Musculature of anal canal:
External anal sphincter: It is under voluntary nerve control, made up of
striated muscle and supplied by inferior rectal and perineal branch of fourth
sacral nerves. It surrounds the whole length of the anal canal and has three
parts - subcutaneous, superficial and deep. The subcutaneous part lies below
the level of internal sphincter and surrounds the lower part of anal canal as a
flat band about 15mm broad. It has no bony attachment. The superficial part
is elliptical in shape and arises from posterior surface of the terminal
segment of coccyx as the ano-coccygeal ligament.
Internal anal sphincter: It is involuntary in nature, formed by the thickened,
circular muscle coat of the gut and surrounds the upper ¾ (3cm) of the anal
canal, lies above the subcutaneous part and deep to the superficial and deep
parts of the external sphincter, and ends below at the Hilton’s white line.
16
Conjoint longitudinal coat: It is formed by the fusion of puborectalis with
the longitudinal muscle coat of rectum at the ano-rectal junction, between
the external and internal sphincters. Soon it becomes fibro elastic and at the
level of the white line it breaks up into a number of fibro elastic septa which
spread out fan wise, pierce the subcutaneous part of external sphincter and
are attached to the skin around the anus. The most lateral septum forms the
perianal fascia and the most medial are the anal inter muscular septum that is
attached to the white line. In addition, some strands pierce obliquely the
internal sphincter and end in the sub mucosa below the anal valves.
Ano-rectal ring: It is a muscular ring of the ano-rectal junction, formed by
the fusion of the pubo-rectals, deep external sphincter and the internal
sphincter. It is easily felt by a finger in the anal canal. Surgical division of
this ring results in rectal incontinence. The ring is less marked anteriorly
where the fibers of puborectalis are absent.
Surgical spaces: The tissue spaces are filled with cutaneous tissue and
important from the surgical point of view because they are the possible sites
of infection. The surgical spaces are as follows.
1. Ischio-rectal space: It is a pyramidal space and comprises of the upper
2/3 of ischiorectal fossa. This space is crossed by the inferior
haemorrhoidal vessels and nerves. Morgagni has showed that the
ischiorectal space is liable to become filled with pus in high anal fistula
and ischiorectal abcesses. Countrey described that this space connects
with the opposite ischiorectal space through the subsphincteric space and
is an important avenue of existence of infection.
17
2. Peri-anal space: It surrounds the anal canal below the white line. It
contains the subcutaneous external sphincter, the external rectal venous
plexuses, and the terminal branches of the vessels and nerves.
3. Sub-mucous space: Sub-mucousa of the anal canal lies above the white
line between the mucous membrane and the internal sphincter. It contains
the internal rectal venous plexus and lymphatics.
4. Peri-rectal space: This space is a potential space which lies between the
pelvic peritoneal floor and levator ani muscle.
5. Intermuscular space: Its medial boundary is internal anal sphincter and
external anal sphincter. This space was described by Eisen Hammer.
6. Ischio rectal fossa: It lies between the sidewall of the pelvic and the anal
canal and the lower part of the rectum. The apex is above and base is
below formed by the perianal skin. Milliganetal described the ischiorectal
fossa as being divided into two spaces by a horizontal fascia i.e., perianal
space and ischiorectal space.
Anal Orifice or Anus: The anus is the lower aperture of the anal canal and is
situated about 4cms below and in front of the tip of the coccyx in the cleft
between the buttocks.
Surgical anal canal lining: The surgical anal canal is lined above by mucosa
and below by anoderm which is modified skin. The anal crypts are in the
upper part of the anoderm.
A line at the level of the crypts is the pectinate line or dentate line.
Above this line there are number of vertical mucosal folds, the columns of
Morgagni, which overline the internal haemorrhoidal plexus. Intermediately
18
above the dentate line or dentate line is an important landmark for surgeons.
At the lower part of the anal canal, this line is wavy, whitish, which is
known as Hilton’s line named by its founder.
Anal sphincter: The anal sphincter has three distinct “U” shaped loops which
have specific mechanism.
1st Loop: In this top loop the deep portion of the external sphincter and the
puborectalis are fixed into one muscle. This attaches to the lower part of the
symphysis pubis and loops around the upper part of the anal canal with the
downward inclination.
2nd Loop: This intermediate loop is the superficial external sphincter which
arises from the tip of the coccyx as a tendon and gives rise to strong muscle
bundles passing forward to encircle the anal canal below the top loop.
3rd Loop: The third or base loop is the subcutaneous external sphincter. It
attaches anteriorly to the perianal skin in the mid line and passes backward
with an upward inclination to loop around the lower part of the anal canal.
Anal Glands: Anal Glands are vestegial structures lined by stratified mucus
secreting columnar epithelium and squamous epithelium. Normally there are
six to ten glands in the circumference of the anus. Each gland has a duct and
discharges into the anal crypt at the dentate line.
19
Arterial Supply of the Rectum and Anal Canal
1. The superior rectal or Haemorrhoidal artery: It is the continuation of the
inferior mesenteric artery and descends posteriorly to the rectum, where
it bifurcates to supply the rectum and upper portion of the anal canal.
2. The middle rectal or haemorrhoidal arteries: These arise from the internal
iliac artery on each side and enter the lower portion of the rectum antero
laterally at the level of levator ani muscle. They do not enter lateral stalks
as previously believed. The arteries anastomose with the branches of the
superior rectal artery.
3. The inferior rectal or haemorrhoidal arteries: These arise on each side
from the internal pudendal artery, a branch of the internal iliac artery and
traverse the ischio-rectal fossa on each side to supply the anal sphincter
muscles. There is no evidence of anastomosis between the superior and
inferior rectal arteries.
4. The middle sacral artery: It provides an insignificant amount of blood
supply to the rectum. It arises posteriorly just above the bifurcation of
aorta, descends over the lumber vertebrae, sacrum and coccyx, and gives
only small branches to the posterior wall of the lower portion of the
rectum.
Venous Drainage of Rectum and Anal canal
Return of the blood from the rectum and anal canal is via two systems
– Portal and Systemic. The superior rectal (Haemorrhoidal) veins drain the
rectum and the upper part of the anal canal into the portal system via the
inferior mesenteric vein. Primarily the middle rectal veins drain the lower
part of the rectum and the upper part of the anal canal. They accompany the
middle rectal artery and terminate in internal iliac veins. The inferior retcal
20
veins, following the corresponding arteries drain the lower part of the anal
canal via the internal pudendal veins, which empty into the internal iliac
veins. Dilatation of the inferior rectal veins leads to external haemorrhoids.
The superior, middle and inferior rectal veins converge to form the
internal rectal (haemorrhoidal) plexus in the submucosa of the columns of
Morgangi. Dilatation of this plexus gives rise to internal haemorrhoids.
Venous Plexuses
1) Internal rectal venous plexus:
It lies in the submucosa of the anal canal. It drains mainly into
superior rectal vein but communicates freely with the external plexus and
thus with the middle and inferior rectal veins. The plexus therefore is an
important site of communication between the portal and systemic veins. This
is a series of dilated pouches connected by transverse branches around the
anal canal.
2) External rectal venous plexus:
It lies outside the muscular coat of the rectum and the anal canal and
communicates freely with the internal plexus and is drained by the inferior
rectal vein into the internal pudendal vein; the middle part by the middle
rectal vein, into the internal iliac vein, and the upper part of the superior
rectal vein which continues as the inferior rectal vein which further
continues as the inferior mesenteric vein.
3) Anal veins:
These are arranged radially around the anal margin. They
communicate with the internal rectal plexus and the inferior rectal veins.
21
Excessive straining during defaecation may rupture one of these veins,
forming subcutaneous perianal haematoma, known as external piles.
Lymphatic Drainage of Rectum and Anal canal
Mainly there are three sets of lymphatic channels –
1. Superior rectal lymph nodes:
These run with the Superior rectal vessels. A special group lies just
above the Levator ani and close to the rectal wall in the region of ampulla.
They are the para rectal nodes of the aorta. These are larger nodes at the
bifurcation of the Superior rectal artery.
2. Middle rectal lymph nodes:
These lie along the lateral ligament of rectum close to the middle
rectal vessels. From here they pass to the lymph nodes around the internal
iliac artery.
3. Inguinal lymph nodes:
The lower portion of the anal canal and the anus are drained by
lymphatics, which pass to the inguinal nodes.
Above the pectinate line the lymphatics drain with those of the rectum
into the internal iliac nodes. Below the pectinate line the lymphatics drain
into the medial group of the superficial inguinal nodes.
Nerve Supply of Rectum and Anal canal
Sympathetic innervation:
Rectum and the upper half of the anal canal derive their sympathetic
supply from the lumbar part of the trunk and the superior hypogastric plexus
by means of the plexus on the branches of the inferior mesenteric artery. The
sympathetic nerves to the rectum and upper part of the anal canal pass
22
mainly along the inferior mesenteric and the superior rectal arteries and
partly via the superior and inferior hypogastric plexuses. The latter
supplying the lower part of the rectum and internal sphincter.
Para sympathetic innervation:
This is derived from pelvic splanchnic nerves; for these the fibres pass
as long strands from sacral nerves to join the inferior hypogastric plexuses
which enter on the sides of rectum, being motor to the musculature of the
rectum and inhibitory to internal sphincter. The external sphincter is
supplied by the inferior rectal branch of the pudendal nerve (S2, S3) and the
perineal branch of the fourth sacral nerve. Afferent impulses underlying
sensations of physiological distension are conveyed by the para sympathetic
nerves, while pain impulses are conducted by both sympathetic as well as
para sympathetic nerves supplying the rectum and upper part of the anal
canal.
Importance of Guda
Charaka includes Guda in Dasa Pranayatanas31 and Susrutha in
Marmas; Guda is a Mamsa and Sadyo pranahara marma.32
Vata is controller of all the sareerika kriyas, which is divided into five
types depending upon the site it occupies. Thus ‘Apana vata’ is the one
which occupies below the nabhi in general and pakwashaya in vishesha.
Apana vayu prakopa produces diseases at guda and vasti pradesha, like
Arshas, Ashmari, Bhagandara, etc.33
23
According to Charaka, Pakwashaya and Sthula guda are the moolas
for Pureesha vaha srotas.34 Thus it is understood that the function of the
Guda is Pureesha dharana and Visarjana.
Seated in the pakwashaya the apana vata does the function of ‘adho
nayana’ or bringing downwards of vata, mutra, pureesha, artava, retas and
garbha in time.35
“Ahara sambhavam vastu deho hi ahara sambhavah” says Charaka.
The body is made from ahara and is also maintained by it. This ahara is
subjected jatharagni and its pachana takes place after which sara kitta
vibhajana occurs. The sara bhaga is absorbed and the kitta bhaga or
‘pureesha’ is pushed forward to the end part of pakwasaya i.e. guda (uttara
guda) where it is stored until its elimination. Therefore it is said that
pakwashaya (uttara guda) and guda (adho guda) are the sthanas of pureesha
vaha srotas. When the pureesha accumulates in sufficient quantity (the
pramana of pureesha is seven anjalis), the desire for defaecation occurs.
When the desire for defaecation is being felt by an individual, there
occurs propulsion of faecal column beyond the Pravahini. At this stage
Visarjini relaxes and accommodates the advancing faecal column, which
progresses onwards by induction of pressure of Pravahini, by the individual.
The column of the fecal material thus passes through the relaxed internal
sphincter (ano-rectal ring) and the external sphincter to the outside.
Samvarani comes into action when sufficient column has advanced beyond
the external opening and by contraction cuts the fecal column and releases it
to be dropped out. Hence physiologically these three levels are very
important during the act of defaecation.
24
The important function of guda is defaecation. Dalhana comments on
Susrutha regarding the function of the Valis, by which they get their name
i.e. Pravahana, Visarjana and Samvarana are the functions or actions of
Pravahani, Visarjini and Smavarani respectively. These are the different
actions exhibited by the Guda for pureesha visarjana.
Mechanism of Defaecation
Defaecation means process of passing faeces from the anus. It is a
reflex mechanism, which is under voluntary control in the normal condition
of the life. Usually the rectum remains empty and faeces are stored in pelvic
colon. The urge for defaecation occurs when the faecal matter enters the
rectum on increase of the intraluminal pressure of the rectum from 20 to 25
mm of water. Faecal matter does not collect elsewhere if defaecation is
regular, however, if defaecation is long deferred; the descending colon
becomes filled when pelvic colon can hold no more. As a result of mass
movement, some faeces enters the rectum when the desire to defaecate
occurs while the usual stimulations are – taking food, a glass of warm water,
a cup of coffee or tea or smoking may have the same effects. The desire to
defaecate may be induced by straining effort, which may raise the abdominal
pressure to as much as 200mm. of mercury and forces faecal matter into the
rectum.
The process of defaecation includes the action of voluntary and
involuntary muscles, which are highly susceptible to emotional stimuli. The
reflex centres for defaecation have been located in the hypothalamus, in
lower lumbar and upper sacral segments of the spinal cord and ganglionic
plexuses of the gut.
25
CLASSIFICATION OF ARSHAS
Ayurvedic classification
Arshas can be broadly classified in to five types –
1. Utpathi bhedena
2. Dosha bhedena
3. Anubandha bhedena
4. Adhishthana bhedena
5. Sadhyasadhya bhedena
Utpathi bhedena
According to Utpathi arshas are classified into Sahajanma and
Utharothana or Jatasyottara kalaja.36
Dosha bhedena
According to Charaka it is of six types37 – Sahaja, Vataja, Pittaja,
Kaphaja, Dwandwaja and Sannipataja.
According Susrutha38 and Madhavakara39 it is of six varieties –
Vataja, Pittaja, Kaphaja, Raktaja, Sannipataja and Sahaja. Vagbhata while
describing the lakshanas mentions ‘Dwandwaja arshas’. Though they
mentioned Raktaja type separately, in the description they says that, it has
Pitta lakshanas.
Anubandha bhedena
Charaka in the context of chikitsa mentioned Vatanubandha and
Kaphanubandha Raktarsho lakshanas40 are also mentioned.
Vagbhata mentions that Raktaja arshas may have Vata or
Kaphanubandha.41
26
Charaka again mentioned two types of arshas according to chikitsa –
Sushka and Ardra arshas42. The arshas in which vata (or) kapha (or)
vatakapha dushti is more, is called as ‘Sushka’ arshas and those in which
rakta (or) pitta (or) raktapitta dushti is more, they were termed as ‘Ardra or
Sravi’ arshas. Again Charaka described the Sravi43 arshas to be of two types
according to anubandha, i.e. Vata and Kapha anubandha.
Adhishthana bhedena
According Adhishthana Bheda arshas is of 13 types, i.e. it can be
occur at 13 sthanas, viz. guda valis, siras, nasa, netra, karna, nabhi, gala,
talu, oshtha, kantha, mukha, vartma and twak44, 45.
Sadhyasadhya bhedena
These are mainly of two types:- 1.Sadhya arshas and 2.Asadhya
arshas. Sadhya arshas is again subdivided into Kruchra sadhya and Sukha
sadhya arshas. Asadhya arshas are of two varieties. They are Yapya and
Pratyakhyeya arshas.45
Regarding arshas, Vagbhata classified based on Susruta’s and
Charaka’s concepts. In Arsha nidana he describes the types of arshas as
1. Sahaja
2. Janmottarothana and Sushka arshas and Sravi arshas.
But while describing the samprapti and lakshanas he narrated six
varieties of arshas. Madhava Nidana also has the same classification which
is based on the Charaka and Susruta.
Ambikadatta Sastry explained that Sushka arshas are Vata or Kapha
or Vatakapha predominant. If there is vata or kapha or vatakapha there will
be no bleeding or secretion and it is dry and painful. They are called as
27
‘Bahya Arshas’. Ardra arshas are predominant of rakta or pitta or both rakta
and pitta which are always bleeds are called as ‘Sravi arshas’ or Rakta
arshas.
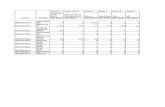
Table showing Arsho bhedas according to Different Achayras
Arsho bheda
Charaka
Susruta
Vagbhata
Madhava nidana
Sahaja + + + +
Janmothara +
Vataja + + + +
Pittaja + + + +
Kaphaja + + + +
Sannipataja + + + +
Raktaja Sravi + + +
- Vatanubandha + +
- Kaphanubandha + +
Dwandwaja + + +
Sushka + +
Ardra (Sravi) + +
MODERN CLASSIFICATION
The modern science classifies Anal protrusions47 as follows -
1. Internal haemorrhoids – First, Second and Third Degree
2. External haemorrhoids
3. Interno external haemorrhoids
4. Symptomatic piles
5. Secondary or accessory piles
28
Internal Haemorrhoids
These are exaggerated vascular cushions involving the superior
haemorrhoidal veins, normally located above the dentate line and are
covered by mucous membrane of the rectum or anal canal. These are
classified into three varieties depending on their prolapse, viz. First, Second
and Third Degree haemorrhoids.
– Haemorrhoids that bleed but do not prolapse out side the anal canal
are called first degree haemorrhoids.
– Haemorrhoids that prolapse on defaecation but return or need to be
replaced manually and then stay reduced are called second degree
haemorrhoids.
– Haemorrhoids that are permanently prolapsed are called third
degree haemorrhoids.
External Haemorrhoids
External piles are located below the dentate line and are covered by
squamous epithelium (skin). These are mainly the dilated venules of inferior
haemorrhoidal plexus.
These are classified into two groups:
a) True external haemorrhoids
These are rare and nothing but small skin tags. These are generally
associated with internal haemorrhoids and anal fissures. The skin tag is an
area of fibrous connective tissue covered by skin.
b) Perianal haematoma
It is nothing but small haematoma arising from rupture of the external
haemorrhoidal plexus. A thrombosed haemorrhoid is that in which blood has
clotted both intra-vascularly and to some degree extra-vascularly.
29
Interno-external Haemorrhoids
This is a combination of internal and external haemorrhoids.
Symptomatic Haemorrhoids
Symptomatic piles may appear in condition where the problem or
disease is specific and the piles are secondary viz. carcinoma of rectum,
pregnancy, straining at micturition and from chronic constipation.
Secondary or Accessory Haemorrhoids
Superior rectal vein has three main branches out of these two of them
situated in the cushions of upper anal canal at right anterior, right posterior
and the third at left lateral position. The new structures between or nearer to
these segments are called accessory or secondary piles.
30
NIDANA
The word ‘Nidana’ is described as follows –
‘Nischitya deeyate pratipadyate vyadhiraneneti nidanam’ – Jejjata48
‘Nirdisyate vyadhiraneneti nidanam’ – Gadadhara49
‘Vyadhi nischaya karanam nidanam’ – Vararuchi50
‘Hetulakshana nirdesat nidanani’ – Susruta51
The meaning of the above quotations is – ‘nidana is the karana or the
factor which indicates as well as confirms the disease’. Here it is used in a
broader sense and should be understood as ‘Pancha lakshana nidana’ or
‘Nidana panchaka’ which comprises of Nidana, Poorva roopa, Roopa,
Upasaya and Samprapti, because each of these individually and also unitedly
give the knowledge of the disease. But, in general usage the word Nidana is
used in specific sense and it means only the first one of the Pancha lakshana
nidana, which is described as follows – ‘Nidanam karanam ityuktam agre’ – Charaka52
‘Nidanam rogotpadako hetuh’ – Madava nidana53
‘Seti kartavyatako rogotpadaka heturnidanam’ – 54
i.e. the causative factors which aid in the production of the disease
are said as Nidanam. ‘Sankshepatah kriya yogo nidana parivarjanam’55 Susruta mentioned the importance of this nidanam and said that
‘avoiding the causative factors it is chikitsa in brief’. This is supported by
the Madhukosa commentary which says – ‘if nidana is not known then how
its avoidance is possible?’ Hence it is necessary to study the nidana
individually.
31
Nidana according to Ayurveda
Charaka has dealt with the Nidanas in an elaborated manner. Firstly
he described nidana of Sahaja arshas, then Samanya nidana of arshas, then
the individual nidanas of Vataja, Pittaja and Kaphaja arshas and finally
Dwandwaja and Sannipataja arshas in a line. He did not mention Raktaja
arsho nidanam. Susrutha mentioned them very briefly and Madhavakara has
taken the nidanas for Vata, Pitta, Kapha, Dwandwa and Sannipataja arshas,
from Charaka. Eventhough both Susrutha and Madhavakara have mentioned
Raktaja arshas as one of the types of arshas and described its lakshanas, they
did not mention individual nidana for it, which supports the Charaka’s
opinion of considering Raktaja arshas as a part Pittaja arshas. The nidanas
are as follows:
Nidana of Sahaja arshas
According to Charaka ‘Guda vali beeja upataptam’56 is the nidana for
Sahaja arshas. This again occurs by two ways, one is ‘Matru pitru krita
apachara’ and the second is the ‘purva karma’. This Nidana has to be
attributed to all Sahaja vikaras says Charaka.
Susrutha in the Nidana sthana mentioned that – Sahaja arshas are due
to ‘Dushta sonita sukra nimittani’.57
Modern science also accepts this concept of congenital weakness of
the vessels of the anal region in persons whose parents have similar history
and are more and easily prone to piles.
‘The condition is so frequently seen in members of the same family
that there must be a predisposing factor, such as a congenital weakness of
the vein walls or an abnormally large arterial supply to the rectal plexus’ –
Bailey & Love – Short Practice of Surgery.58
32
Samanya nidana
The Samanya nidanas mentioned by Charaka can be classified into
Ahara, Vihara, Vyadhi and Pancha karma vyapat.59
Ahara karanas – Guru, Madhura, Seeta, Abhishyandi, Vidahi,
Viruddha aharas; Ajeerna, Pramitasana (alpa matra), Asatmya bhojana;
Gavya – Matsya – Varaha - Mahisha – Aja – Avika – Pishita Bhakshana;
Krusha, Sushka, Puti mamsa, Pyshtika, Paramanna, Ksheera modaka,
Dhadhi, Tila, Guda vikruti sevana; Masha, Yusha, Ikshurasa, Pinyaka,
Pindaluka, Sushka saka, Sukta, lasuna, Kilata, Pindaka, Bisa, Mrinala,
Saluka, Krounchadana, Kaseruka, Srungataka, Taruna, Virudha,
Navadhanya, Ama mulaka upayogat; Guru Phala, Saka, Raga, Haritaka,
Mardaka, Vasa, Siraspada, Paryushita-Puti-Sankeerna anna Abhyavaharanat;
Mandaka, Atikranta Madyapana, Vyapanna – Guru Salila pana.
Vihara karanas – Ati vyavaya, Avyavayat, Diva swapnat, Sukha
sayana asana upasevanat, Ratha, Utkatuka – Vishama – kathina Asana
sevanat, Udbhranta yanat, Ushtra yana, Vata – Mutra – Pureesha vega
udeeranat, Samudeerna vega vinigrahat, Abhikshnam Seetambu
samsparshat, Chela – Loshta – Trina adi gharshanat, Streenam ama garbha
bhramsat, Garbha utpeedanat, Bahu and Vishama Prasutis.
Pancha karma vyapat karanas - Ati snehanat, Ati Samsodhanat,
Vastikarma vibhramat, Vasti netra asamyak pranidhanat, Guda kshananat
Vyadhi karanas – Arshas, Grahani dosha and Atisara – these three can
be nidanas for one another says Charaka.
33
Susrutha briefly mentioned that – the karanas attributed for dosha
prakopa, and Viruddhasana, Adhyasana, Stree prasanga, Utkatuka aasana,
Prishta yana and Vega vidharana to be the nidana for arsho vhadhi and says
that the Parivruddhi of ‘Guda Kandas’ occurs due to Trina, Kashtha, Upala,
Loshtha, Vastra, etc.60
Vagbhata mentioned same as Susrutha and Madhavakara did not
mention any Samanya nidana.
After this Charaka has mentioned the Vishesha nidanas or individual
nidanas which are as follows –
Vataja arsho nidanam61, 62
Ahara karanas – Kashaya, Katu, Ruksha, Sheeta and Laghu, Pramita
Alpashana and Teekshna madyam
Vihara karanas – Langhanam, Maithunam, Vyayamam, Seeta Desha
and Seeta Kala sevana, Shoka, Vata and Atapa sevana.
Pittaja arsho nidanam63, 64
Ahara karanas – Katu, Amla, Lavana, Ushna, Teekshna, Vidahi,
Ksharam, Madyam
Oushadha karanas – Vidahi, Teekshna and Ushna Oushadhas
Vihara karanas – Krodha, Shishira Desha and Shishira Kalaeeta
Kaphaja arsho nidanam65, 66
Ahara karanas – Madhura, Snigdha, Seeta, Guru, Teekshna, Lavana,
Amla aharas.
Vihara karanas – Avyayama, Diwaswapna, Shayana sukha, Asana
sukha, Pragvata sevana, Seeta Desha and Seeta Kala sevana and achintana.
34
Dwandwaja arsho nidanam67, 68
The nidanas which cause prakopa of two dosahs, if join together cause
Dwandwa or Samsargaja arshas.
Sannipataja arsho nidanam69, 70
The nidana which cause sarva dosha prakopa i.e. prakopa of all the
three doshas leads to Sannipataja arshas.
NIDANA ACCORDING TO MODERN SCIENCE71
The causative factors can be classified as follows –
1. Hereditary
2. Morphological
3. Anatomical and
4. Exciting causes
5. Other conditions or Symptomatic
Hereditary
The condition is so frequently seen in the members of the same family
that there must be a predisposing factor, such as a congenital weakness of
the vein walls or an abnormally large arterial supply to the rectal plexus.
Varicose veins of the legs and haemorrhoids often occur concurrently.
Morphological
In quadrupeds, gravity aids, or any rate does not retard, return of
venous blood from the rectum. Consequently venous valves are not required.
In man the weight of the column of blood unassisted by valves produces a
high venous pressure in the lower rectum, unparalleled in the body. Except
in a few fat old dogs, haemorrhoids are exceedingly rare in animals.
35
Anatomical
(1) The collecting radicles of the superior haemorrhoidal vein lie
unsupported in the very loose submucous connective of the
anorectum.
(2) These veins pass through muscular tissue and are liable to be
constricted by its contraction during defaecation.
(3) The superior rectal veins, being tributaries of the portal vein, have
no valves.
Exciting causes
Straining accompanying constipation or that induced by over
purgation is considered to be a potent cause of haemorrhoids. Less often the
diarrhoea of enteritis, colitis, or the dysenteries aggravates latent
haemorrhoids. In instances, descent and swelling of the anal cushions is a
prominent feature.
Symptomatic haemorrhoids
Haemorrhoids may be symptomatic of some other condition in the
body like –
a) In carcinoma of rectum – this by compressing or causing thrombosis
of the superior rectal veins, gives rise to haemorrhoids sufficiently
often to warrant examination of the rectum and the rectosigmoid
junction for a neoplasm in every case of haemorrhoids.
b) During pregnancy – pregnancy piles are due to compression of the
superior rectal veins by the pregnant uterus and relaxing effect of the
progesterone, F.S.H, prolactin and glucocorticoids on smooth muscles
in the walls of veins.
36
c) Straining at micturition due to enlarged prostate or stricture of the
urethra.
d) Large ovarian or uterine masses.
e) Cirrhosis of the liver leads to portal obstruction and portal
hypertension and cardiac weakness leads to tension within the
haemorrhoidal plexus.
f) Anal infection is also an important cause of piles. The infectious
material (stool) is trapped into anal crypts and directed into anal
glands at the time of defaecation leading to inflammation and vascular
tension in the rectal plexuses, which leads to haemorrhoids and their
protrusion.
g) Lack of indigestible part in food like fiber and cellulose causes
constipation, which leads into the piles.
Table showing the Vataja arsho nidanas
Nidana
Charaka
Susruta
Madhava Nidana
Kashaya + - Same as Charaka Katu + - ” Tikta + - ” Ruksha + - ” Seeta + - ” Laghu + - ” Pramita Alpasana
+ - ”
Teekshna Madyam
+ - ”
Maithuna + - ” Langhanam + - ” Seeta Desha + - ” Seeya Kala + - ” Vyayama + - ” Soka + - ” Vata sparsha + - ” Atapa sparsha + - ”
37
Table showing the Pittaja arsho nidanas
Nidana
Charaka
Susrutha
Madhava Nidana
Katu + - Same as Charaka Amla + - ” Lavana + - ” Kshara + - ” Vyayama + - ” Agni + - ” Atapa + - ” Sisira Desha + - ” Sisira Kala + - ” Krodha + - ” Madyam
+ - ”
Asuya + - ” Vidahi + - ” Teekshna + - ” Ushna + - ”
Table showing the Kaphaja arsho nidanas
Nidana
Charaka
Susrutha
Madhava Nidana
Madhura + - Same as Charaka Snigdha + - ” Seeta + - ” Lavana + - ” Amla + - ” Guru + - ” Avyayama + - ” Divasvapna + - ” Sayya sukha + - ” Asana sukha + - ” Pragvata seva + - ” Seeta Desha + - ” Seeta Kala + - ” Avachintana + - ”
38
POORVA ROOPAM
When Dosha dooshya sammurchana takes place in sthana samsraya
kala the Poorva roopa takes place. The lakshanas of the disease will be
alpabala and swalpa lakshanas and invisible. Sometimes the lakshanas of the
disease are strong.
Regarding Poorva roopa some of Acharyas said the prakupitha doshas
when takes stana samsraya then the vyadhi bodhaka lakshanas clearly
visible.
These lakshanas are vyadhi bodhakas that’s way Acharyas said as
Poorva roopa lakshanas.
The Poorva roopa is two types72 –
1. Samanya poorva roopa and
2. Vishesha poorva roopa
According to Charaka –
Anna vistamba (Avipakam), Atopa, Karshya, Daurbhalya, Mandagni,
Udgara bhavulyata, Alpamala pravruthi and Grahani dosha, Pandu roga
shanka can be seen in Arsho poorva roopa stage73.
According to Sushrutha –
Anna asraddha, Kruchra pachanam, Amlika, Paridaha, Vishtambha,
Pipasa, Saktisadana, Atopa, Karshyam, Udgara bahulyam, Swayathu of
Akshi, Antra koojanam, Gudaparikartanam, Paridaha, Amlika, Bhrama,
Tandra, Nidra and Ashanka of Pandu roga, Grahani dosha or Sosha, Kasa,
Swasa, Balahani and Indriya dourbalyam.74
39
Vagbhata followed Susruta while Madhavakara mentioned the same
poorva roopas which were mentioned by Charaka.75
Table showing the Poorva Roopas of Arshas
Poorva roopa
Charaka
Sushruta
As.Hrudayam
Madhava Nidana
Anna vistamba + + + + Atopa + + + + Karshya + + + + Daurbhalya + + Mandagni + + Udgara bahulyata + + + + Alpamala pravruthi + + Grahani dosha shanka + + + + Pandu roga shanka + + + + Anna asraddha + + Kruchra pachanam + + Amlika + + Paridaha + + Saktisadana + + Pipasa + + Akshi swayathu + + Antra koojanam + + Guda parikartanam + + Bhrama + + Tandra + + Nidra + + Ashanka of Pandu roga
+ +
Ashanka of Gahani dosha
+ +
Ashanka of Sosha + + Kasa + + Swasa + + Balahani + + + Indriya dourbalyam + +
40
ROOPAM
This is the stage in which the lakshanas of a vyadhi have become
prominenent and present according to the doshas. Again Charaka gives a
detailed description of the lakshanas of Sahaja arshas, samanya lakshanas of
arshas, then vataja, pittaja and kaphaja arsho lakshanas, and finally
Dwandwaja and Sannipataja arsho lakshanas but did not mention Raktaja
arsho lakshanas. Susrutha and Madhavakara dealt with Sahaja arsho
lakshanas in a line and also mentioned Raktaja arsho lakshanas along with
doshaja lakshanas.
Sahaja arsho lakshnas
According to Charaka they are as follows –
Arsho swaroopam76 – Anu, Mahan, Deergha, Hraswa, Vrutta, Vishama,
Visruta, Antah kutila, Bahih kutila, Jatila, Antarmukha and varna according
to dosha.
Rogi lakshans77 – Janma prabhruti ati krusha, Vivarnah, Kshama, Deena,
Prachura vibaddha vata mutra pureesha, Sarkara peedita, Asmari peedita,
Mala – aniyata, vibaddha, mukta, pakwa, ama, sushka, bhinna; Antarantara –
Sweta, Pandu, Harita, Peeta, Rakta, Aruna, Tanu, Sandra, Picchila, Kunapa
gandha, Ama pureesha; Prachura parikartika in Nabhi, Vasthi and Vankshna;
Guda sula, Pravahika, Pariharsha (roma harsha), Prameha, Vishtambha,
Antrakujana, Udavarta, Hrydaya indriya upalepa, Prachura vibaddha tikta
amla udgara, Sudurbala, Sudurbalagni, Alpa sukra, Krodhano,
Dukhopachara seela, Kasa, Swasa, tamaka, Trushna, Hrillasa, Chardi,
Arochaka, Avipaka, Peenasa, Kshavathu, Timira, Sirassula, Swara –
Kshama, Bhinna, Sakta, Jarjara; Karna rogi, Sula of Pani, Pada, Vadana,
Akshikuta; Jwara, Angamarda, Sarva parva asthi soola, Antarantara graha of
41
Parswa, Kukshi, Vasthi, Hrudaya,Prishtha, Trika graha; Pradhyanapara,
Parama alasa.
Susrutha78 mentions that the lakshanas of Gudankuras in Sahaja arshas
are according to the dosha but still vishesha lakshanas are like –
Durdarshanani, Parusha, Pandu varna, Daruna, Antarmukha; and the rogi is
Krusha and Alpabhukta; suffers with Upadravas like – Aruchi, Alpagni, Sira
santata gatra, Ksheena reta, Alpa praja, Kshama swara, Krodha, Nasa-siro-
netra-shrotra rogas, Satata antrakujana, Atopa, Hridaya pralepa, etc.
Madhavakara says Sahaja and Sannipataja arsho lakshanas are alike.79
Samanya roopa
Samanya Swaroopa of Vata, Pitta and Kaphaja arshas according to
Charaka80 – Sarshapa, Masoora, Masha, Mudga, Makushtaka, Yava, Kalaya,
Pindi, Tintikera, Kharjura, Karkanthu, Kakanantika, Bimbi, Badara, Kareera,
Udumbara, Jambava, Gostana, Angushtha, Kaseruka, Srungataka; and
appearance like Tunda – Jihwa – Mukula – Karnika of Srungi, Daksha,
Sikhi, Sukatunda.
Vagbhata81 mentioned the Samanya lakshanas of arshas as follows –
Agnimandya, Krusatha, Hatoutsaha, Deenata, Durbala, Ati nishprabha,
Saraheena Guda vedana, Kasa, Trishna, Mukha vyrasya, Swasa, Peenasa,
Klama, Angabhanga, Vamana, Kshavadhu, Sotha, Jwara, Kleebatha,
Arochaka, Vedana in Parswasthi, Hrudaya, Nabhi, Payu and Vankshana;
Pulakodaka sadrusa guda srava, and Pureesha is sushka or ardra, ama or
pakwa, whose varna is pandu, haridra, harita or rakta.
42
Vishesha roopa
Charaka, Susrutha and Vagbhata mentioned Vishesha roopa as
doshaja lakshanas. Madhavakara followed the description of Vagbhata. They
are as follows –
Vataja arshas
According to Charaka82 – Gudankuras are Sushka, Mlana, Kathina,
Parusha, Rooksha, Syava, Teekshna agra, Vakra, Sphutita mukha, Vishama,
and Visturta; vedana casused by gudankuras – Sula, Akshepa, Toda,
Sphurana, Chimichima, Samharshana, Upasaya with Snigdha, Ushna aharas;
Pravahika, Adhmana, Sisna, Vrushana, Vasthi, Vankshna, Hridgraha,
Angamarda, Hridaya drava, Pratata vibaddha Vata, Mutra and Varcha,
Kathina Varcha; Sula of Uru, Kati, Prishta, Trika, Parswa, Kukshi and
Vasthi; Siro Abhitapa, Kshavathu, Udgara, Pratisyaya, Kasa, Udavarta,
Ayasa, Sosha, Sotha, Murcha, Arochaka, Mukha vairasya, Timira, kandu,
Sula of Nasa, karna and Sankha,Swaropaghata; Nakha – Nnayana-
VadanaTwak- Mutra- Pureesha are Syava, Aruna and Parusha.
According to Susrutha83 the Gudankuras are – Parisushka, Aruna,
Vivarna, Vishama Madhya, and their akruti like - Kadamba pushpa,
Tundikeri, Nadi, Mukula and Suchimukha; Sasula Samhata mala tyaga,
Vedana of Kati, Prishta, Parswa, Medhra, Guda and Nabhi; Arshas leading
to Gulma, Ashtheela, Pleeha and Udara; Krishnata of Twak, nakha, nayana,
Vadana, Mutra, Pureesha.
According to Madhavakara84 the Gudankuras are – Bahu, Sushka,
Chimachimanvita, Mlana, Syava varna, Aruna varna, Stabdha, Vishada,
Parusha, Khara, Visadrusha (akruti different from each other), Vakra,
Teekshna, Visphutita anana; and in akrutis like Bimbi phala, Kharjura phala,
43
Karkanthu phala, Karpasa phala, Kadamba pushpa abha, Siddharthaka
upama; causing vyatha of Shira, Parswa, Kati, Uru, Vankshna; having
Kshavathu, Udgara, Vishtambha, Hirdgraha, Arochaka, Kasa, Swasa, Agni
Vaishamya, Karnanada, Bhrama; and passes mala – Grathita, Stoka,
Sashabda, Sapravahika, Ruk, Phena, Pichhanugata, and Vibaddha; Krishnata
of Twak, Nakha, Vit, Mutra, Netra and Vaktra; Gulma, Pleeha, Udara and
Ashtheela may be caused by Vatarshas.
Pittaja arshas
According to Charaka85 – the Gudankuras are – Mridu, Sithila,
Sukumara, Sparsha asaha, Rakta, Peeta, Neela, Krishna, Sweda Upakleda
bahulani, Visra gandha, Srava is Tanu, Peeta, Rakta; Daha, Kandu, Soola,
Nistoda, paka, Upasaya with Sisira ahara viharas, Sambhinna Peeta harita
Varchas, peeta visragandha Pachura Vit Mutra, Pipasa, Jwara, Tamaka,
Sammoha, Bhojana dwesha, Peeta – Nakha Nayana, Twak, Mutra Pureesha.
According to Susrutha86 the Gudankuras are – Neela agra, Tanu, Visarpa
guna, petra avabhasa, yakrut prakasa, Suka jihwa samsthana, Yava Madhya,
Jalouka vaktra sadrusha, Praklinna, rogi is Sadaha – rudhira atisara,
upadravas like Jwara daha pipasa murcha; Peeta - Twak Nakha Nayana
Dashana Vadana Mutra Pureesha.
According to Madhavakara87 the Gudankuras are – Neela mukha;
Rakta-Peeta-Asita prabha, Tanu (alpa sankhya), Mridu, Shlatha (hanging);
Sparsha asaha; Srava is Asra, Tanu and Visra gandha; Akruthi like Suka
jihwa, Yakrit khanda, Jalouka vaktra; Mala is Ushma yukta, Drava, Neela,
Ushna, Peeta, Rakta, Amayukta; causing lakshanas like Daha, Paka, Jwara,
Sweda, Trishna, Murcha, Aruchi, Moha; Twak, Nakha, Vit, Mutra, Netra
and Vaktra are in Harita, Peeta and Haridra varnas.
44
Sleshmaja arshas
According to Charaka88 the Gudankuras are – Adhika Pramana,
Upachita, Slakshna, Sparsha Saha, Sweta, Pandu, Picchila, Stabdha, Gurru,
Stimita, Suptasupta, Sthira, Swayathu – kandu bahula, Pratata Pinjara Sweta
Rakta Piccha srava; Mutra and Pureesha are Guru, Picchila and Sweta;
Upasaya with Ruksah Ushna ajhara viharas, Pravahika, Atimatra vankshna
anaha, Parikartika, Hrillasa, kapha nishtheeva, kasa, Arochaka, Pratisyaya,
Gourava, Chardi, Mutra kricchra, Sosha, Sotha, pandu, Seeta jwara, Asmari,
Sarkara, Upalepa of Hridaya and Indriyas, Asya Maturya, prameha, Deergha
kala anupasayani, Atimatra – agnimardava, klaibya kara; Amavikara
prabala, Guru; Sukla – Nakha, Nayana, Vadana, Twak, Mutra, Pureesha.
According to Susrutha89 – the Gudankuras are – Sweta, mahamula,
Sthira, Vrutha, Snigdha, Pandu; Akara like kareera, Panasa astjhi, Gostana;
Na bhidyate, Na sravanthi, kandu bahula; Sleshma yukta - analpa -
mamsadhavana prakasa atisara, Sopha, Seeta jwara, Arochaka, Avipaka,
Siro gourava, Sukla – Twak, Vnakha, Nayana, Dashana, Vadana, Mutra,
Puresha.
According to Madhavakara90 the Gudankuras are – Maha mula,
Ghana, Mandaruja, Seeta, Utsanna, Upachita, Snigdha, Stabdha, Vrutha,
Guru, Sthira, Picchila, Stimitha, Slakshna, Kandu adhya and Sparshana
priya; Na sravanthi, Na bhidyante; their akruthi – Kareera, Panasa asthi
abha, gostana sannibha; Pureesha is Vasaabha, Kapha yukta, and Pureesha
pravruthi is Sapravahika; causing lakshanas like Vankshna anaha, Payu-
Vasthi- Nabhi vikarshana; Swasa, Kasa, Hrillasa, Praseka, Aruchi, Peenasa,
Meha kricchra, Shiroruja, Sishira jwara, Klaibya, Agni mardava, Chardi, and
Ama praya vikaras; Twak, Nakha, Vit, Mutra, Netra and Vaktra are Pandu
and Snigdha.
45
Raktaja arshas
According to Susrutha91 they are – Nyagrodha praroha, Vidruma,
kakanantika phala sadrusha; Pitta lakshanayukta, at the time of Avagadha
mala tyaga, sahasa, atyartha, dushta, analpa asruk srava, atipravruthi of rakta
causes Sonita atiyoga upadravas.
According to Madhavakara92 the ankuras are - Pittakruti samanvita,
Vata praroha sadrusha; Gunja Vidruma sannibha; Sravanthi sahasa raktam;
Rogi is – Dushta, Ushna and Gadha vitka prapeeditah; Bhekabha, Heena
varna bala utsaha, Hatouja, Kalushendriyas, Sonita kshaya sambhava dukha
Peedita, and has Pitta lakshanas.
The upadravas of sonita atipravruthi are – Siro abhitapam, Andhyam,
Adhimantham, Timira, Dhatu kshaya, Akshepaka, Pakshaghata, Ekanga
vikaram, Trishna, Daha, Hikka, kasa, Swasa, Panduroga, Maranam – Sonita
varnaneeya adhyaya.93
Vata anubandha Raktarshas
According to Charaka94 - Mala is in Syava varna, Kathina and
Ruksha; Adhovayu na vartate; Asruk from arshas is Tanu, Aruna varna and
Phenila; Rogi is seen with Kati–Uru–Guda Sula and Adhika dourbalya; and
if the Hetu is Rukshanam – then it should be understood as Vatanubandha
Raktarshas.
Madhavakara95 also expressed the same opinion.
Kaphanubandha Raktarshas
According to Charaka96 – Mala is Sithila, Swetha and Peetha in varna;
Asruk from Arshas is Snigdha, Guru, Seethala, Ghana, Tantumat, Pandu and
Picchilam; Guda sthana is Sapiccham and Sthimitam; and if the Karanas are
46
Guru and Snigdha gunas, then it should be understood as Kaphanubandha
Raktarshas.
Same is the description of Madhavakara.97
Dwandwaja Arshas
In these the lakshanas of dwandwa ulbana doshas are seen.98
Sannipataja arshas
According to Charaka99, Susruta100, Vagbhata101 and Madhavakara102
Tridosha Lakshanas are seen in Sannipataja and Sahaja Arshas.
THE SIGNS AND SYMPTOMS OF HAEMORRHOIDS
INTERNAL HAEMORROIDS
The primary haemorrhoids are generally arranged at three places i.e.
at 3, 7 and 11 o’clock with the patient in the lithotomy position. In between
these three primary haemorrhoids there may be smaller secondary
haemorrhoids.
Each principal haemorrhoid can be divided into three parts:
a) The Pedicle – This is situated at the anorectal ring. As seen through a
proctoscope it is covered with pale pink mucosa and occasionally a
pulsating artery can be felt in this situation.
b) The Internal haemorrhoid, which commences just below the anorectal
ring. It is bright red or purple and covered by mucous membrane and
the size is variable.
c) An external associated haemorrhoid lies between the dentate line and
the anal margin. It is covered by skin, through which blue veins can
seen, unless fibrosis has occurred. This associated haemorrhoid is
present only in well-established cases.
47
Entering the pedicle of an internal haemorrhoid may be a branch of
the superior rectal artery. Very occasionally there is a haemangiomatous
condition of this artery – an ‘arterial pile’ – which leads to ferocious
bleeding at operation.
Clinical features
Bleeding – As the name haemorrhoid implies, bleeding is the principal and
the earliest symptom. At first the bleeding is slight; it is bright red and
occurs during defaecation (a ‘splash in the pan’), and it may continue
intermittently thus for months or years. Haemorrhoids that bleed but do not
prolapse out side the anal canal are called first degree haemorrhoids.
Prolapse – This is a much later symptom. In the beginning the protrusion is
slight and occurs at stool, and reduction is spontaneous. As time goes on the
haemorrhoids do not reduce themselves, but have to be replaced digitally by
the patient. Haemorrhoids that prolapse on defaecation but return or need to
be replaced manually and then stay reduced are called second degree
haemorrhoids. Still later, prolapse occurs during the day, apart from
defaecation, often when the patient is tired or exerts himself. Haemorrhoids
that are permanently prolapsed are called third degree haemorrhoids. By
now the haemorrhoids have become as a source of great discomfort and
cause a feeling of heaviness in the rectum but are not usually acutely painful.
Discharge – A mucoid discharge is a frequent accompaniment of prolapsed
haemorrhoids. It is composed of mucus from the engorged mucous
membrane, sometimes augmented by leakage of ingested liquid paraffin.
Pruritus will almost certainly follow this discharge.
48
Pain – is absent unless complications supervene. For this reason any patient
complaining of ‘painful piles’ must be suspected of having another condition
(Possibly serious) and examined accordingly.
Anaemia – can be caused very rarely by persistent profuse bleeding from
the haemorrhoids.
On inspection – there may be no evidence of internal haemorrhoids. In
more advanced cases, redundant folds or tags of skin can be seen in the
position of one or more of the three primary haemorrhoids. When the patient
strains, internal piles may come into view transiently, or if they are of the
third degree they remain prolapsed.
By Digital examination, internal haemorrhoids cannot be felt unless they
are thrombosed.
By Proctoscopy – they can be seen bulging into the lumen of the
proctoscope, just below the anorectal ring.
Complications
Profuse haemorrahge – is not rare. Most often it occurs in the early stage
of the second degree. The bleeding occurs mainly externally, but it may
continue internally after the bleeding haemorrhoid has retracted or has been
returned. In these circumstances, the rectum is found to contain blood.
Strangulation – one or more of the internal haemorrhoids prolapse and
become gripped by the external sphincter. Further congestion follows
because the venous return is impeded. Second degree haemorrhoids are most
often complicated in this way. Strangulation is accompanied by considerable
49
pain, and is often spoken of by the patient as an ‘acute attack of the piles’.
Unless the internal haemorrhoids can be reduced with in an hour or two,
strangulation is followed by thrombosis.
Thrombosis – the affected haemorrhoid or haemorrhoids become dark
purple or black and feel solid. Considerable oedema of the anal margin
accompanies thrombosis. Once the thrombosis has occurred, the pain of the
strangulation largely passes off, but tenderness persists.
Ulceration – superficial ulceration of the exposed mucous membrane often
accompanies strangulation with thrombosis.
Gangrene – occurs when strangulation is sufficiently tight to constrict the
arterial supply of the haemorrhoid. The resulting sloughing is usually
superficial and localized. Occasionally, a whole haemorrhoid sloughs off,
leaving an ulcer which heals gradually. Very occasionally massive gangrene
extends to the mucous membrane within the anal canal and rectum and can
be the cause of spreading anaerobic infection and portal pyemia.
Fibrosis – after thrombosis, internal haemorrhoids sometimes become
converted into fibrous tissue. The fibrosed haemorrhoid is at first sessile, but
by repeated traction during prolapse at defaecation, it becomes pedunculated
and constitutes a fibrous polypus that is readily distinguished by its white
colour from an adenoma, which is bright red. Fibrosis following transient
strangulation commonly occurs in the subcutaneous part of a primary
haemorrhoid. Fibrosis in an external haemorrhoid favours prolapse of an
associated internal haemorrhoid.
50
Suppuration – is uncommon. It occurs as a result of infection of a
thrombosed haemorrhoid. Throbbing pain is followed by perianal swelling,
and a perianal or submucous abscess results.
Pylephlebitis (Portal pyaemia) – theoretically, infected haemorrhoids should
be a potent cause of portal pyaemia and liver abscesses. Although cases do
occur from time to time, this complication is surprisingly infrequent. It can
occur when patients with strangulated haemorrhoids are subjected to ill-
advised surgery, and have even been reported to follow banding.
EXTERNAL HAEMORRHOIDS
Unlike internal haemorrhoids, external haemorrhoids comprise of a
conglomerate group of distinct clinical entities.
a) A thrombosed external haemorrhoid – this is commonly termed a
perianal haematoma. It is a small clot occurring in the perianal
subcutaneous connective tissue, usually superficial to the corrugator cutis
ani muscle. The condition is due to backpressure on a venule consequent
upon straining at stool, coughing, or lifting a heavy weight.
The condition appears suddenly and is very painful, and on
examination a tense, tender swelling which resembles a semi-ripe
blackcurrant is seen. The haematoma is usually situated in a lateral region of
the anal margin. Untreated it may resolve, suppurate, fibrose, and give rise
to a cutaneous tag, or burst and extrude the clot, or continue bleeding.
In the majority of cases resolution or fibrosis occurs. Indeed, this
condition is called ‘a 5-day, painful, self-curing lesion’.
51
Provided it is seen within 36 hours of the onset, a perianal haematoma
is best treated as an emergency. Under local anaesthesia the haemorrhoid is
bisected and the two halves are excised together with 1.25cm of adjacent
skin. This leaves a pear-shaped wound, which is allowed to granulate. The
relief of pain is immediate and a permanent cure is certain. On the rare
occasions in which a perianal haematoma is situated anteriorly or
posteriorly, it should be treated conservatively because of the liability of a
skin wound in this region is said to be an anal fissure.
b) Dilatation of the veins of the external anal verge - This becomes
evident only if the patient strains, when a bluish, cushion-like ring appears.
This variety of external haemorrhoids is almost a perquisite of those who
lead a sedentary life. The only treatment required is an adjustment of the
patient.
c) Sentinel Pile – A thickening of the mucous membrane at the lower end of
a fissure of the anus.
52
Table showing the Vataja Arsho Lakshanas
Charaka Susrutha As.Hru. Ma. Ni.Sushka Parisushka + Same
as Mlana + As.Hru.Kathina Parusha + Ruksha Syava + Teekshna agra + Vakra + Sphutita mukha + Vishama Vistruta Sula Akshepa Toda Sphurana Chimichima + Samharshana Snigdha Ushna Upasaya
Visadrusa
Aruna Aruna Vivarna Stabdha Vishama Madhya Visada Kadamba pushpa + Tundikeri Bimbi Nadi Kharjura Mukula Karkanthu Suchi mukha Karpasi phala Khara Siddharthaka
upama
53
Table showing the Pittaja Arsho Lakshanas Roopam Charaka Susrutha Vagbhata Madhava
Nidana Mrudu + Neela agra + Sithila + Tanu Sukumara + Visarpa Sparsha asaha + Peeta avabhasa Rakta + Yakrut prakasa + Peeta + Suka jihva
sadrusa +
Neela + Yava Madhya + Krishna + Jalouka vaktra
sadrusa Asita
Sveda bahulya + Praklinna Upakleda bahulya
+
Visra gandha + + Tanu peeta rakta srava
+ +
Daha + Kandu + Soola + Nistoda + Paka + Sisira upasaya + + Slatha + Sukajihwa Jalouka
vaktra
Yava Madhya
54
Table showing the Kaphaja Arsho Lakshanas Roopam Charaka Susrutha Vagbhata Madhava
Nidana Pramana + Sveta Ghana Upachita + Maha
moola Mahamoola
Slakshna + Sthira Mandaruja Sparsha saha + Vrutta Utsanna Sveta + Snigdha Upachita Pandu + Pandu Snigdha Picchila + Kareera Stabdha Stabdha + Panasa
asthi Vrutta
Guru + Gostana Guru Stimita + Na
bhidyante Sthira
Supta sputa + Na sravanti Picchila Sthira + Stimita Svayathu + Slakshna Kandu bahula + + Kandu adhya Pinjara, Sveta, Rakta, Piccha Srava
+ Sparshana priya
Ruksha, Ushna Upasaya
+ Karira
+ Panasa asthi + Gostana + Na sravanti + Na bhidyanti Table showing the Raktaja Arsho Lakshanas
Charaka Susrutha Vagbhata Madhava Nidana Nyagrodha praroha Vata praroha Vidruma Gunja Kakanantika phala Vidruma Pitta lakshanani Rakta srava Pitta laksjhnanai
55
SAMPRAPTI (PATHOGENESIS)
According to Charaka Samprapti103 of Arshas (1) by intake of various
specific nidanas (aggravating causes) agnimandya takes place and leads
excessive accumulation of mala (faeces) (2) due to specific aggravating
causes the apanavata accumulated in guda valis leads to arshas.
Vagbhata104 explained the samprapti in brief. The aggravated dosha
vitiates twak, mamsa, medas of guda region and forms mamsa ankura of
various types, and they are called as arshas.
Madhavakara105 had the same opinion.
As per Sushruta106 doshas by their aggravating factors splits from their
normal seat alone or together including Rakta, which reaches the guda
marga through pradhana dhamanis and causes the vitiation of valis of guda
which results into production or formation of mamsa ankuras specifically in
mandagni person an irritation of guda by trina, kastha, upala (stone), lostha
(soil lump), vastra and shitodaka sparsha. These mamsankuras further
aggravate to result into arshas.
Dalhana in his commentary on Sushruta explained pradhana dhamani
as purisha vaha dhamani. Dr.Ghanekar’s commentary on Sushruta also gives
the idea about the pradhana dhamani is one of the adhogami dhamani which
goes downwards from the ridaya and arshas are described as the ‘Vikruti of
malashaya siras’ since dhamanis and siras are synonyms. Sushruta’s school
of thought seems to be correct. His opinion is absolutely relevant and which
has considered even by the scientific thinkers, because varicosity of the
rectal veins is called Haemorrhoids.
56
Modern aspect
The anal canal receives a rich blood supply from the superior, middle
and inferior rectal arteries, whose branches reach the anal submucosa and
forms the venous plexuses, being surrounded by smooth muscle under the
anal submucosa. Straining during defaecation and the passage of hard and
small volume stools results in the engorgement of anal cushions. This may
cause injury to the mucous membrane resulting in bright red bleeding from
the capillaries of the lamina propria. With repeated straining, the anal
cushions are damaged so that the normal supports are stretched and tendency
to prolapse outside the anal canal develops. Early in the evolution of the
disease, the normal rectal mucosa above the anal cushions eventually is
dragged with the prolapsing anal cushions, so that it adds to the bulge.
Prolapse of anal cushion and its supporting frame work by the straining at
stools and constricting pecten bands produces piles, obstructing stool
passage causing the venous congestion.
Anal infection is also a cause of piles; the infectious material (stool) is
trapped into anal crypts and directed into anal glands at the time of
defaecation. There the infection takes place and causes inflammation and
vascular tension is developed in rectal plexuses which leads to haemorrhoids
and their protrusion.
57
RUGVINISCHAYAM
Arshas has to be diagnosed based on the Darshana pariksha with the
help of Arsho darshana nadi yantram or a Proctoscope and Sparshana
pariksha i.e. digital examination. Raktaja arshas has to be differentiated from
Raktatisara and Raktapitta. They are described as follows:
Rectal Examination
Position of the patient: Lithotomy position, left lateral (Sim’s) position and
knee-elbow position are advised, where as the lithotomy position is more
convenient for the examination.
Digital examination – In lithotomy position stretching the buttocks aside
and inspecting the anal region, it is to be noted that whether any eruption,
external piles, etc. are present. Fit a finger stall to the right forefinger and
smear it with a lubricant. Massage the anus for a moment with the finger and
then press gently with the pulp of the finger till it enters the anus directing it
straightly forwards. Once the anal canal is passed, direct the finger slightly
downwards directly towards umbilicus. Feel the mucous membrane for pile
masses, polyps, ulcers and malignant neoplasm. Haemorrhoids are not
palpable unless thrombosed. On withdrawing the finger, examine the finger
for the presence of mucous, blood, etc.
Proctoscopy – The patient should be in left lateral or ‘knee-elbow’ position.
The proctoscope should be made warm and lubricated and should be gently
inserted into the rectum. The instrument should be introduced at first in the
direction of the axis of the anal canal i.e. upwards and forwards towards the
patient’s umbilicus until the anal canal is passed. The instrument is then
directed posteriorly to enter into the rectum properly. Now the obturator is
58
withdrawn and the interior of the rectum and anal canal is seen with the help
of a light. The internal piles, fissures, ulcer and growth can be seen if
present. The piles will prolapse into the proctoscope as the instrument is
being withdrawn. Note the position of the piles. They are generally
positioned according to the main branches of the superior haemorrhoidal
vein. The main three branches are situated in the left lateral, right anterior
and right posterior positions. When then patient is in the lithotomy position
these positions will correspond to 3, 7 and 11 o’clock positions respectively,
if a watch is imagined to be held against the anus. These are called ‘primary
piles’. A few secondary piles (4-5) may frequently develop in between the
primary ones. Chronic fissure is often situated on the midline posteriorly. By
proctoscope one can also find inner opening of fistula and biopsy can also be
taken from a growth or an ulcer through a proctoscope.
Table showing the differences between Raktarshas and Rakta pitta
Raktarshas
Rakta pitta
History of arshas present History absent Bleeding is only per rectum Bleeding can occur from other sites also, like
nose, mouth, genitals, etc. Digital examination reveals masses
Digital examination does not reveal any masses
Bleeding is before or after defaecation
Bleeding can occur irrespective of defaecation
Pain during defaeceation present
Pain is absent
Generally constipation is seen
Constipation not necessary
Dog or crow will take blood mixed food
They do not accept the blood mixed food
Vastra ranjana absent Vastra ranjana present Blood quantity is comparatively less
Bleeding is more
59
Differences between Raktarshas and Rakta atisaram
Raktarshas
Rakta atisaram
History of arshas present History of arshas absent
Digital examination reveals of masses No masses
Bleeding is before or after defaecation, as
abrasion occurs during defeacation
Blood mixed with stool
Stool mass is hard and solid Normal or loose stools
60
SADHYA-ASADHYATA
Arshas is said as a ‘Maha vyadhi’ and by prakruti itself it is
Duschikitsyam i.e. difficult to treat.107 According to Charaka108 - Arshas
involves pancha vidha vatas, pancha vidha pittas, pancha vidha kaphas and
Guda vali trayam; hence they are said to be dukhaani, bahu vyadhikaraani,
sarva dehopataapini and prayah krichhratamani. But still depending on the
vali in which they have originated and the kala avadhi they are classified as
Sukhasadhya, Krichrasadhya and Asadhya.
Sukhasadhya arsho lakshanas
According to Charaka109 and Madhavakara110 Bahya valijata, Eka
dosholbana and na chirotpatitani are said to be Sukhasadhya.
Kricchrasadhya arsho lakshanas
According to Charaka111 and Madhavakara 112 Dwidoshajas, Dwitiya
vali janita and Eka samvatsara purana are said to be Krichhrasadhyas.
Asadhya arsho lakshanas
According to Charaka113 and Madhavakara114 Sahaja, Tridoshaja,
Abhyantara valijanita arshas are said as Asadhyas.
Yapya arsho lakshanas
A rogi with Asadhya Arshas having Ayush sesha, Deepta kayagni and
Chatushpadopapathi, can be considered as Yapya and a rogi not possessing
these turns to be Pratyakhyeya.115, 116
According to Susruta117 – Arshas occurring on Bahya and Madhyama
valis are sadhyas and those occurring on antara vali are asadhays.
61
UPADRAVAS
Some Upadravas are also mentioned for Arshovyadhi, the presence of
which in a rogi indicates Pratyakhyeyatva. They are – Sotha of hasta, pada,
mukha, guda and Vrushanas; Hrit parswa sula, Sammoha, Chardi, Angaruk,
Jwara, Trishna, Gudapaka, Arochaka, Ati prasruta sonita and Atisara. It is
said that arshas with these upadravas will definitely kill the rogi.
62
ARSHO CHIKITSA
Charaka and Susrutha, both have described the chikitsa of arshas in a
detailed manner, but differing in orientation, i.e. Oushadha pradhana and
Shastrakarma pradhana. Even then Susrutha has mentioned Oushadha at
first, which shows the importance of Oushadha chikitsa.
Charaka describes oushadha chikitsa in detail but still mentions very
briefly regarding Kshara, Agni and Shastra karmas saying that ‘some people
say that arshas are to be treated with Kshara, some say Shastra, and some
say Agnikarma. For performing these, the Vaidya should have wide
knowledge and should have seen many times, these chikitsas being done by
expert surgeons, because these treatments if improperly done, may lead to
complications like Pumstva upaghata, Swayathu of Guda, Vega vinigraha,
Adhmanam, Daruna Soola, Vyatha, Rakta ati pravruthi, Guda kleda, Guda
bhramsa, Punarviroha of rudhas (recurrence of the gudankuras, which
have subsided) or even Marana120. Therefore a treatment which is Sukha,
Adaruna and Alpa bhramsam will be described for the Samula nivruthi of
arsho vyadhi.’121 This shows the importance given to Oushadha chikitsa,
compared to others.
Susruthokta Arsho Chikitsa
Susrutha says ‘Sankshepatah Kriya yogo nidana parivarjanam’, i.e.
nidana parivarjana itself is the treatment, in brief. So it has to be followed
first, without which all the treatments will remain unfruitful.
The chikitsa of arshas is said to be of four types122, the names and the
conditions in which they are indicated are as follows –
63
• Oushadha sadhyas - Achira kala jatani, Alpa dosha, Alpa linga, Alpa
upadrava yukta, and Adrushya arshas.
• Kshara sadhyas – Mridu, Prasruta, Avagadha and Ucchrita.
• Agni sadhyas – Karkasha, Asthira, Prithu and Kathina.
• Shastra sadhyas – Tanu moola, Ucchritani and Kledayukta.
According to dosha of arshas also these chikitsas are indicated123 –
• Agni and Kshara karmas in Vataja and Sleshmaja arshas
• Mridu Kshara in Pittaja and Raktaja arshas
Susrutha cautions that these Kshara, Agni and Shastra chikitsas are to
be done with utmost care, as Vibhrama of these chikitsas leads to Shandyam,
Sopha, Daha, Mada, Murcha, Atopa, Anaha, Atisara, Pravahana or even
Marana124.
Mandagni is the cause for arshas and all the chikitsas are aimed at
Agni vruddhi and Agni Samrakshana.125
The general outlines of Oushadha chikitsa126 – in Vataja arshas –
Sneha, Sweda, Vamana, Virechana, Asthapana and Anuvasana; in Pittaja
arshas – Virechanam; in Raktaja arshas – Samshamanam; in Kaphaja arshas
– Anulomana, Vibandha hara oushadhas and in Sarva doshaja arshas Sarva
dosha hara oushadha like oushadha sidha payah.
Bhallataka prayoga127 is specially mentioned along with some other
yogas. Two single drugs, Vrukshaka (Kutaja) and Arushkara (Bhallataka)128
have been highlighted, saying that they can cure all types of arshas,
comparing them with two other single drugs Khadira and Beejaka
64
(Vijayasara) in the cure of Kushthas. Similarly Kshara and Agni129 prayogas
have been emphasized to cure all types all types of arshas, comparing with
Haridra prayoga, which can cure sixteen types of pramehas.
Finally emphasizes Nidana parivarjana, Agni samrakshana, and
Anuloma oushadha sevana.130
Charakokta Arsho Chiktsa
Before starting chikitsa Charaka mentions Sadhya asadhya lakshanas,
the intention is to look for them and handle the case accordingly.
Importance of early treatment - Arshas should be treated as early as
possible, because it may cause obstruction to Guda, which may lead Baddha
gudodaram.131
Charaka’s opinion regarding Ksharadi chikitsas is already mentioned.
It is said that there may be recurrence with these chikitsas, hence Oushadha
chikitsa is stated to be uttama.
Arshas has been categorized into Sushka and Prasravi or Ardra
varieties, which are Vata Sleshma and Pitta Rakta adhikya janyas
respectively.
Chikitsa for Sushka arshas with Bhinna Shakrut
For Stabdha arshas, Abhyanga should be done with Chitraka kshara or
Bilwa taila or with any taila or sarpi and then Swedana should be done with
oushadha siddha pottali or pinda. Avagaha and Sechana is done with
Kashayas, Gomutra, Souvira or Tushodaka Madyas, Takra, Dadhi manda,
Amla kanjika, etc. which are sukhoshna. This is followed by Dhoopana,
65
which is done with Vasas of different animals, human hairs, Skins or
Arkamoola, Tumburu, etc. Lepas are advised for rogi with soola, sotha and
hridroga.
The aim of these bahya chikitsas is to reduce the Stabdhata,
Swayathu, Kandu and Vedana and the Dushta rakta accumulated in them
drains out and give relief.
Rakta mokshana132 – when rakta dushti is present, seetha, ushna,
snigdha or rooksha chikitsas will not give relief. Then Rakta mokshana
should be done again and again with Jaluka, Shastra or Suchi, to let out
dushta rakta.
After these bahya chikitsas abhyantara oushadha prayoga is done.
“yad vayoranulomyaya yad agni bala vruddhaye,
anna pana oushadha dravyam tat sevyam nityam arshasaih”133
Mandagni has been considered as the important nidana for arsho roga.
Hence Arsho rogi is advised to take always, Anna, Pana and Oushadha
dravyas, which causes Vatanulomana and Agni bala vruddhi. Hence all the
treatments are aimed at these two.
Tryushana, Patha, Hingu, Chitraka, Saindhava lavana, etc. are given
with Manda, Madya or Ushnodaka, which will relieve from Guda swayathu,
Soola and Mandagni.
Abhaya with Guda is advised to be taken as Pourva bhakta i.e. before
bhojana, which causes arsho sankshayam.
66
Taktra134 has been highlighted to be one of the best arshohara dravya.
It is of three types – Ruksham i.e. navaneeta fully removed, Ardha
uddhrutam i.e. navaneeta half removed and Sneham i.e. navaneeta not
removed. These are given according to agni bala of rogi i.e. alpabala,
madhyama bala and uttama bala accordingly. Takra can be taken alone or
prepared with other oushadha dravyas, mixed with oushadha dravyas or
annam. Sushka Arshas cured by Takra prayoga will not relapse just like the
Truna which is dagdha with takra poured on ground. Takra causes Sroto
suddhi, with which pushti, bala, varna and praharsha are gained. Hundred
varieties of vata kapha vaydhis are curable with Takra and nothing is better
than Takra for kapha vata vyadhi samana. ‘Takrarishta’135 is a special
preparation which is very effective in arshas.
Varieties of Peya, Khada and Yushas are mentioned. Rakta Shali,
Maha Shali, Kalama, Jangala, Sarada and Shashthika are varieties of
dhanyas which can be used as Pathya by an arsho rogi.
Chikitsa for Sushka arshas with Gadha Shakrut
Madira, Seethu, Souvirakam, Prasanna and other yogas prepared with
various oushadhas, with Ghrita and Lavana are mentioned which cause Vata
anulomana and Varcho anulomana, which should be taken as Pourva
bhaktika i.e. before food.
Ghrita yogas prepared with pippali, nagara, kshara, dhanyaka, jeeraka,
phanita, phalamla, pippalimoola, chitramoola, chavya, dadima, patha,
tumburu, yamani, lavana, bilwa, abhaya, swadanshtra, changeri, dadhi, etc.
in different combinations are mentioned which are Vatanulomana, Vibandha
hara, Kapha vata hara, and also useful in pravahika, guda bhramsa, mutra
67
kricchram, parisravam, guda soola, vankshna soola, grahani dosha, etc.
Pippalyadi ghrita is a special yoga mentioned in this context.
Haritaki (ghrita bharjita) and taken with guda and pippali or trivrut
and danti is advised which is Varcho Vata Kapha Pitta anulomaka and
causes Arsho prasamana and Agnideepana.136
Mamsa rasas prepared with different birds and animals are mentioned
which are useful in Pureesha bandha and as Vata shamaka.
Shakas advised as Pathyas – Trivrut, Danti, Palasha, Changeri,
Chitraka, Upodika, Tanduleeyaka, Veera, Vastuka, Suvarchala, Salonika,
Yava, Avalguja, Kakamachi, Ruha patram, Maha patram, Amlika, Jeevanthi,
Sathi, Grinjana are advised to be taken prepared with Dadhi, Dadima,
Yamaka sneha, Dhanya, Nagara, etc.137
Anupanam – Madira, Shaarkara, Seethu, Takram, Tushodakam
Arishtam, Dadhimandam, Sruta seeta jala or jala sruta with Kantakari, or
Nagara and Dhanyaka should be given as anupanas for a arsho rogi with
Vatadhikyata, Rukshata and Deeptagni for causing Vatanulomana and
Varcho anulomana.138
Vasti karma - Anuvasana vasti – snehas prepared with different vata
hara oushadhas are advised for Anuvasana vasti for ati virukshita arsho rogi
suffering with Kandu yukta and Stabdha arshas and also in Udavarta,
Viloma vata, Kati soola, Guda soola, Guda sopha, anaha, Dourbalyam,
Pavahika, Mutra kricchram, etc. Niruha vasti can be given with Ksheera
prepared with Dasamoola, Mutra, Sneha, Lavana and Phala kalkas.
68
Shoucha karma is advised to be done with Ushnodaka and Kashayas
prepared with different patras.
Chikitsa for Sravi (Rakta sravi) arshas
In Vatanubandha, Kaphanubandha, Pitta Kaphadhika and Dushta
rakta srava yukta arshas, Snigdha – Seeta, Ruksha – Seeta, Sodhana and
Upeksha or Langhana chikitsas respectively are advised.139
If the Dushta rakta srava from arshas is stopped, it causes Rakta pitta,
Jwara, Trishna, Agni nashana, Arochakam, Kamala, Swayathu, Guda and
Vankshna Soola, Kandu, Kotha, Pidaka, Kushtha, Pandu, Vata mutra
pureesha vibandha, Sirassula, Staimityam, Guru gatrata, and other Raktaja
gadas. Therefore Rakta sangrahana should be done after complete dushta
rakta srava.140 Vaidya having knowledge of Hetu, Lakshana, Kala, Bala,
Sonita varna, etc. should wait till the dushta rakta srava is complete. Tikta
dravyas are advised for Agni deepana, Rakta sangrahana and Dosha
pachana. If Rakta srava is there in rogi with dosha kshaya and vatolbana, to
him Sneha should be given as Pana, Abhyanga and Anuvasana. Rakta srava
occurring in Ushna kala, which is Pittolbana and without Vata
kaphanubandha, should be stopped immediately. Preparations with Kutaja
twak, Dadima twak, Nagara, Chandana, Kirata tikta, Darvi twak, Useera,
Nimba, Ativisha, Kutaja beeja, and Rasanjana are advised as Rakta
sangrahakas. Kutajadi Rasakriya, Nilotpala prayoga, some ghritas and peyas
are mentioned in this context.
Shakas useful in raktarshas – Kasmari, Amalaki, karbdara, Dadima,
Grunjana, Salmali niryasa, Chukrika, Nyagrodha sunga and Kovidara
pushpa given with dadhi sara (Creamy layer on Dadhi).141
69
Palandu, navaneeta, Ghrita, Chaga mamsa, Shashtika dhanya, Shali
dhanya, Taruna Sura and Taruna Sura manda are very useful as Rakta
sangrahakas. Seetala upacharas like, Parisheka, Avagaha, Udaka dhara, and
Pratisarana are also advised.
Picchavasti is a vishesha yoga mentioned in this context.142
Abhayarishta, Dantyarishta, Phalarishta, Sharkarasava, Kanakarishta
Pippalyadi Ghritam, Hriberadi Ghritam and Changeri Ghritam are the
vishesha yogas mentioned in the context of arshas.
Since Mandagni is the nidana for arshas, agni bala vruddhi causes
ksheena of vyadhi and agni bala ksheena causes vruddhi of vyadhi; hence
Agni bala samrakshana is emphasized at all the times and by all means.
70
MODERN METHODS OF MANAGEMENT OF HAEMORRHOIDS143
Non-operative or Conservative treatment
Small asymptotic first degree piles, which are found incidentally, may
be left alone. If the patients have constipation and difficulty with
defaecation, they require advice about fluid intake and high-residue diet or
the use of laxatives to ensure a regular, easy bowel movement without
excessive straining. Symptomatic piles are to be treated accordingly, along
with laxatives, external lubricant ointments and suppositories and if
necessary by surgery or injection.
Injection therapy
First-degree internal piles with bleeding are advised to have injection
therapy. A Gabriel syringe is filled with sclerosant (5% phenol in almond
oil) and using a proctoscope, 3-5 ml is injected into the pedicle of each pile
at or just above the ano-rectal ring. This produces submucosal fibrosis in the
upper anal canal and lower rectum, constricting vascular spaces within the
pile and decreasing mucosal mobility.
Banding treatment
This is advised in cases with second-degree piles, which are too large
and cannot be handled by injections. The principle of elastic band ligation is
to apply a tight elastic band above the internal haemorrhoid and the mucosa
above it. Not only does this some of the redundant mucosa but also fixes it at
the site of banding to the underlying muscle by scar tissue, thereby
preventing the haemorrhoid from sliding down the anal canal. Banding is not
applicable to piles covered with skin or associated skin tags.
71
Third degree piles, failure of non-operative treatments of second-
degree piles, fibrosed piles and interno-external piles are not suitable
injection or banding treatmetns.
Cryosurgery
The application of liquid nitrogen (–196oC), the extreme cold of
which causes coagulation necrosis of the piles which subsequently separate
and drop off. The procedure is painless and can be done in the Outpatient
department. The technique tends to cause troublesome mucus discharge,
which is the limiting factor for its use. This technique is suitable for internal
haemorrhoids.
Photocoagulation
The application of infra-red coagulation by a specially designed
instrument is advocated for piles that do not prolapse. This is an effective
and painless method.
Manual Anal Dilatation
Manual anal dilation is used to disrupt the tight unyielding sphincter
and reduce the activity of the internal anal sphincter. This can be done as an
O.P. case and postoperative regime of a regular bulk laxative and the
passage of an anal dilator are recommended.
Haemorrhoidectomy
Third degree piles, failure of non-operative treatments of second-
degree piles, fibrosed piles and interno-external piles are not suitable
injection or banding treatments. These are indications for
haemorrhoidectomy.
72
PATHYA-APATYHAS
‘If pathya is followed what is the necessity of chikitsa and
if pathya is not followed what is the use of chikitsa’
– This is what a vaidyakeeya subhashitam says, which indicates that
Pathyapathyas play an important role in the chikitsa of any vyadhi.
Dhanyas: Rakta Shali, Maha Shali, Kalama, Jangala, Sarada and Shashthika
varieties of dhanyas.
Shakas: Trivrut, Danti, Palasha, Changeri, Chitraka, Upodika,
Tanduleeyaka, Veera, Vastuka, Suvarchala, Salonika, Yava, Avalguja,
Kakamachi, Ruha patram, Maha patram, Amlika, Jeevanthi, Sathi, Grinjana,
Chukrika, Nagara, Kovidara pushpa, Nyagrodha sunga. Palandu is specially
mentioned as Rakta sangrhaka.
Phalas: Kasmari, Amalaki, Karbudara, Dadima.
Mamsas: Chaga, Barhi, Tittira, Lava, Daksha.
Dairy products: Ksheera (for vasti), Dadhi, Dadhi sara, Takram, Navaneetam
and Ghritam. Navaneetam and Takram specially mentioned.
Madyas: Madira, Shaarkara, Seethu, Tushodakam, Arishtakam, Taruna Sura
and Taruna Sura manda.
Anupanam – Madira, Shaarkara, Seethu, Takram, Tushodakam Arishtam,
Dadhimandam, Sruta seeta jala should be given as anupanas for causing
Deepana, Pachana, Vatanulomana, Varcho anulomana, Anahahara,
Soolahara, Laghavakara.
TYPES OF ARSHAS
UTPATHI DOSHA ANUBANDHA ADHISHTHANA SADHYASADHYA Sahajanma 1. Vataja 1.Siras 7.Gala 2. Pittaja 2.Nasa 8.Oshtha Uttarothana 3. Kaphaja Sushka Ardra 3.Netra 9.Kantha Sadhya Asadhya 4. Raktaja 4.Karna 10.Mukha 5. Sannipataja 5.Nabhi 11.Vartma 6. Sahaja 6.Talu 12.Twak Sukha Sadhya Kichra sadhya Yapya Pratyakhyeya
CLASSIFICATION OF HAEMORRHOIDS
Internal haemorrhoids External Interno-external Symptomatic Secondary or Accessory Haemorrhoids Haemorrhoids Piles Piles First degree Second degree Third degree
Table showing Lakshnas of Arshas according to Dosha
Dosha
Vata
Pitta
Kapha
Rakta
Vata Rakta
Kapha Rakta
Sannipataja
Varna (colour)
Syava varna Neelamukha, Rakta, Peeta, Asita, prabha
Sita Vata praroha
Aruna varna
Panduni
Akruti (shape)
Bimbi, Kharjura, Karkanthu,
Karpasi
Sukajihwa, Yakrut khanda, Jalouka
vaktra
Karira, Panasa asthi, Gostana
Gunja, Vidruma
Antarmukhani
Parimana (size)
Kadamba puhpa, Siddharthaka
upama
Sukshma Mahamula, Utsanna, Upachita
Irregular
Srava (discharge)
Anila, Sushka, Mlana
Tanu srava, durgandha
Arik Tanu,
Phenila
Asrik Ghana, Tantumat,
Pandu, Picchila
Sparsha (nature)
Stabdha, Vishada, Khara,
Mitho Visadrusa, Vakra,
Teekshna, Visphutita
Mrudu, Slatha, Paka
Snigdha, Stabdha, Vrutta,
Guru, Sthira, Picchila, Sthimita, Slakshna,
Sparshana priya
Daruna, Parusha,
Durdarshana
Mala (stool)
Frothy mucous discharge
Bloody stool Mucous pus discharge
Gadha Sweta, Peeta, Snigdha
Irregular
Vedana (pain)
Adhika vedana (irregular)
Dahayukta vedana Mild pain with itching
Nabhi, Vasti, Vankshna
73
DRUG REVIEW
The oushadha yoga selected for the present study is Hareethakyadi
Lehyam, selected from Bhava Prakasha and Bhaishajya Ratnavali. The
ingredients of the yoga and their proportions are as follows –
1. Haritaki - 7 parts (2100gms)
2. Shunti - 6 parts (1800gms)
3. Nimba beeja - 5 parts (1500gms)
4. Karanja beeja - 4 parts (1200gms)
5. Indrayava - 3 parts (900gms)
6. Chitramulam - 2 parts (600gms)
7. Saindhava lavanam - 1 part (300gms)
8. Gudam - 8 parts (2400gms)
Lehya preparation: Take the drugs from 2 to 7 and make them into a fine
powder and mix them well and keep aside. Take Guda and Saindhava lavana
in wide mouthed vessel and heat slowly till they melt and then they are
mixed well. Now the mixture of the fine powders of the above mentioned
drugs is slowly added to the molten Guda and Saindhava lavana, mixing it
with a darvi. When it reaches the lehya paka stage, the vessel is taken down
from the stove and when moderately hot Ghrita and Madhu are added to it
and allowed to cool to room temperature and preserved in an airtight
container.
Matra : 5gm – twice daily
Anupana : Jalam
74
Hareetaki
Botanical name : Terminalia chebula
Family : Combretaceae
Synonyms
Sanskrit : Abhaya, Pathya, Amrutha, Kayastha, Haimavathi, Siva,
Cetaki, Sreyasi, Vayastha, Vijaya, Jivanti, Rohini,
Putana
Telugu : Karakkaya
English : Chebulic myrobalan
Hindi : Hara, Harara, Harad
Assam : Shilikha
Bengal : Haritaki
Gujarati : Hirdo, Himaja, Pulo – harda.
Kannada : Alalekai
Kashmiri : Halela
Malayalam : Kathikka
Marathi : Hirda, Haritaki, Harda, Hireda
Orissa : Harida
Punjabi : Halela, Harar
Urdu : Halela
Ganas:
• Jwaraghna, Arshoghna, Kasaghna, Kushtaghna,Prajasthapana (Charaka)
• Amalakyadi, Parushakadi, Triphala (Susruta)
• Triphala, Hareetakyadi varga (Bh.Pr.)
Brief description of the plant: It grows wildly and is seen throughout India,
especially in the Sub-Himilayan regions from Ravi River to West Bengal
75
and Assam. It grows to a height of 50 to 80ft. The flowering occurs in the
months of April and May and the fruits are seen during winter. The fruit is
yellowish brown, ovoid, wrinkled and ribbed longitudinally. The useful part
is the phala twak or pericarp, which is fibrous, non-adherent to the seed.
Bhava Prakasha mentions seven varieties of Hareethaki viz. Vijaya,
Rohini, Putana,Amrutha, Abhaya, Jeevanthi and Chetaki. This classification
might be based on the desha and guna karmas. In general usage it is said to
of three varieties Bala Hareetaki, Peeta Hareetaki and Hareethaki i.e. purna
pakwa phala. These are nothing but the fruits collected during different
stages.
The pericarp contains Tannins of which the important are Chebulagic
acid, Chebulinic acid and Corilagin. It also contains Chebulic acid,
Gallotanic acid, Gallic acid, Sorbitol, anthraquinones and polyphenolic
compounds.
Prayojyangas: Phala
Matra: 3-6gm
Gunas:
Rasa : Kashaya pradhana (pancharasa alavana)
Guna : Laghu, Ruksha
Veerya : Ushna
Vipaka : Madhura
Prabhava : Tridoshahara, Rasayanam
76
Karmas:
Tridoshahara, Rasayana, Yogavahi, Deepana, Pachana, Medhya,
Cakshushya, Brimhana, Anulomana, Lekhana, Hridya, Lekhana, Vrushya,
Smrutikara, Buddhida, Vayasthapana, Buddhi Indriya Bala prasadanam,
Vedanahara, Mootrala, Rakta shodhaka, Sroto vibandha. Useful in Hikka,
Swasa, Kasa, Prameha, Arshas, Kushta, Sopha, Udara, Krimi, Visarpa,
Grahani roga, Vibandha, Vishama jwara, Gulma, Vrana, Kantha –
Hridamaya, Kamala, Yakrut – Pleehodbhava soola, Asmari, Mootra
kricchra, Mutra ghata, Jwara, Atisara, Asyapaka, Hanti Santarpana krita
rogan.
Vijaya and Jeevanthi are Sarvarogahara.
77
Sunthi
Botanical Name : Zinziber officinale
Family : Zinziberaceae
Synonyms
Sanskrsit : Ardraka, Ardrika,Visva, Visvam, Visvausadham, Visva
bhesajam, Mahaushadham, Nagaram, Katu bhadram,
Sringaveram, Usanam, Katugranthi, Katushanam,
Souparnam
Telugu : Sonthi
English : Dried Ginger
Hindi : Sunth
Tamil : Chukku
Malayalam : Chukku
Bengali : Shunta, Shunti
Gujarati : Shunthya, Sunta, Soontha.
Kannada : Shunti, Shonthi, Onsuthi, Venam Shutti.
Marathi : Suntha
Punjabi : Sunda
Urdu : Sonth, Zanjabeel
Ganas:
• Triptighna, Arshoghna, Dipaniya, Shula prasamana, Trishna nigrahana
(Ch)
• Pippalyadi, Trikatu (Susruta)
• Panchakola, Shadushan, Hareethakyadi varga (Bhav Prakasha)
Brief description of the plant: A slender perennial rhizomatous herb. The
rhizomes are white to yellowish brown in colour, irregularly branched. The
surface is smooth and if broken a few fibrous elements of the vascular
78
bundles project out from the cut ends. It grows wildly in hot and humid
climates; found extensively in Western Ghats and is also cultivated through
India.
Indian Ginger contains the active principles Gingerin and Shogaol,
some starch, and an aromatic volatile oil containing Camphene, Phelladren,
Zinziberine, Oleo-resins; proteins, calcium, phosphorous, iron and vitamins
A, B, and C and some fat and fiber.
Parts used: Kanda (Rhizome)
Matra: Ardraka swarasa – 5 to 10ml; Sunthi churna – 1to2gm
Gunas:
Rasa : Katu
Guna : Ardraka – Guru, Ruksha, Teekshna
Sunthi – Laghu, Snigdha
Veerya : Ushna
Vipaka : Ardraka – Katu; Sunthi – Madhura
Karma : Kapha Vatahara, Deepana, Pachana, Rechana, Balya, Vrishya
Grahi, Swaryam, Vatanulomana, Truptighna, Sheeta prashamana,
Vedanasthapana, Nadiuthejhaka, Hridyathejak, Raktha shodhaka, Mala
Sangrahi; useful in – Udara, Sleepada, Pandu, Amavata, Katisula, Siroruja,
Vibandha, Anaha, Sotha, Arshas, Chardi, Sula, Kasa, Swasa, Jwara, etc.
79
Nimba (Beeja)
Botanical Name : Azadirachta indica A.Juss (Melia azadirachta. Linn)
Family : Meliaceae
Synonyms
Sanskrit : Tiktaka, Paribhadra, Pichumarda, Hinguniryasa,
Arishta, Sarvatobhadra.
Telugu : Vepa, Konda vepa
English : Neem tree, Margosa tree, Indian lilac
Hindi : Nim, Nimba
Bengali : Nim
Marathi : Kadu nimb
Gujarathi : Leemdo
Tamil : Vembu, Vempu
Punjabi : Nimb
Malayalam : Vempu
Ganas:
• Kandughna, Tiktaskandha (Charaka)
• Aragwadhadi, Guduchyadi, Lakshadi (Susruta)
• Guduchyadi varga (Bh.Pra.)
Brief description of the plant: This grows from about 25 –50 ft. high. Found
extensively throughout India. Flowering occurs from February to March and
fruits are seen from April onwards.
The parts used are Twak, Moola twak, Patram, Pushpam, Phalam,
Beejam, Tailam and Niryasam. There are many active principles of which
important ones are Nimbin, Nimbidin, Nimbinin, Nimboesterol, Margosine,
80
etc. All the parts of the plant and active principles and extracts possessed a
lot of significant pharmacological properties and uses as – antiseptic,
analgesic, antibacterial, antiprotozoal, antiviral, antihelminthic, in skin
diseases, gastric ulcers, snake bite, scorpion sting, etc. Sulphur is present in
considerable amounts, which is the reason for many of the effects.
Neem oil, Nimbin and Nimbidin were found to possess anti-
inflammatory property. Nimbin was to found to possess analgesic and
antipyretic effect. Nimbin and Nimbidin have significant effect on gastric
and peptic ulcers in experimental models; produced antiulcer activity against
various types of gastro duodenal lesions in animals; exhibited healing effect
on peptic ulcer without any side effects. Alcoholic extracts possessed
potentiality on scabies, ringworm, acute eczema and also very effective in
helminthiasis. An unsaponifiable matter from oil of seeds exhibited
antibacterial property against S. aureus, Proteus Sp., E.coli and B.subtilis in
particular. It cured ringworm infection in 4-8 days applied in the form of
lotion. Dramatic action exhibited in 2 days of application. Lotion of neem
leaves applied externally twice a day for 3 consecutive days found highly
effective on scabies. It also exhibited cure for eczema (weeping, acute and
chronic).
Prayojyangas : Twak, Moola twak, Patram, Pushpam, Phalam, Beejam,
Tailam and Niryasam
Matra : Twak churna – 2 to 4gm; Patra swarasa – 10 to 20ml;
Tailam – 5 to 10 drops; Beeja churnam – 1 to 2gm
81
Gunas:
Rasa : Tikta, Kashaya
Guna : Laghu, Ruksha
Veerya : Seeta
Vipaka : Katu
Karmas:
Twak - Kapha Pitta hara, Ahrudya, Grahi, Vedanahara, Varnya,
Twakrogahara, Vrana shodhana and Vrana ropana, Yakruduttejaka;
useful in Srama, Trishna, Kasa, Jwara, Aruchi, Krimi, Vrana, Chardi,
Hrillasa, Kushta, Meha, Sotha;
Patra – Netryam; Raktapitta, Kapha, Krimi, and Visha hara, Vatalam,
katupakam, Arochaka and Kushta hara; Salaka (Rachis of the leaf) is
Kasa swasahara, Sreshta Krimihara, Kushtha jwarahara
Phalam – Tikta rasa, katu paka, Laghu guna, Bhedanam, Aruksham,
Ushnam, Gulma, Krimi, Meha hara
Pakwa phalam – Madhura tikta rasa, Snigdham, Guru, Picchilam; useful
in Sonita pitta, kapha, Nayanamayas, Kshtaksheena
Niryasa – Guru, Picchila, Bhedana, Krimi, Kushta, Sothaharas
Pushpam – Chakshushyam, Krimi, Pitta, Vishahara
Tailam – Laghu, Teekshna, Sara; Katu Rasa; Katu Vipaka;Ushna Veerya;
Vata Kaphahara; useful in Krimi, Kushta, Siro roga
82
Karanja (Beeja)
Botanical Name : Pongamia pinnata
Family : Leguminosae
Synonyms
Sanskrit : Karanja, Naktamala, Guchha pushpaka, Ghritapua,
Snigdha patra, Prakeerya, Pushpa manjari
Telugu : Kanuga, Kalukranuga, Ganuga
English : Indian beech
Hindi : Dithouri
Marathi : Karanja
Gujarathi : Karanja, Kanajhi
Bengali : Dahar Karanja
Tamil : Pongum
Malayalam : Ponnam
Kannada : Honge
Ganas:
• Kandughna, Virechana, Katuka skandha, Tikta skandha (Charaka)
• Aragvadhadi, Varunadi, Arkadi, Syamadi, Sirovirechana, Kapha
samsamana (Susrutha)
• Guduchyadi varga (Bhava prakasa)
Brief description of the plant: This is a mid sized tree growing about 25 – 50
ft. high. It is found throughout India especially in South India and coastal
regions. Flowering occurs from May to June and fruits in December and
January. The parts used are Twak, Patra and Beeja. The oil extracted from
the seeds called Pongamia oil, is bitter and dark couloured active principle
83
called Karanjin which is very good antibacterial. Root bark contains
alkaloids like Kanugin, Demethoxy kanugin, etc.
Prayojyangas: Twak, Patra and Beeja, Tailam
Matra: Swarasa of twak/patra – 10 to 20 ml;
Beeja churna – 1 to 3 gm.
Gunas:
Rasa : Tikta, Katu, Kashaya
Guna : Laghu, Tikshna
Vipaka : Katu
Veerya : Ushna
Karmas:
Twak: Vata Kaphahara, Pitta vardhaka, Bhedana, Kriminasaka, Vrana
ropana, Vedanasthapana, Rakta doshahara; useful in Krimi, Sotha,
Kustha, Meha, Udara, Arshas, Yoni dosha, Gulma, Udavarta, Pleeham
Patra – Kapha vatahara, Pittalam, Deepana, Pachana, Bhedana, Sopha,
Visha, Arsha, Krimi, Kushtha
Phalam (Beeja) – Kapha vatathara, Meha, Arsha, Krimi, Kushtha, Jantujit
84
Indrayava (Kutaja beeja)
Botaical Name : Holerrhina antidysenterica
Family : Apocyanaceae
Synonyms
Sanskrit : Girimallika, Vatsaka, Vrukshaka, Kalinga, Indravruksha
Telugu : Kodisapala, Palakodisa, Kutaja
English : Kurchi
Hindi : Kutaj, Kuda
Bengali : Kurchi
Marathi : Kuda
Gujarathi : Kudo
Tamil : Veppalai
Kannada : Korchi
Urdu : Kherda
Punjabi : Kenar
Ganas:
• Arshoghna, Kandooghna, Stanya sodhana, Asthapanopaga,
Vamanaopaga (Charaka)
• Aragvadhadi, Pippalyadi, Lakshadi, Haridradi, Urdhwabhagahara
(Susrutha)
• Hareetakyadi varga (Bh.Pra.)
Brief description of the plant: This is a medium sized plant growing upto 30
ft. high. Distributed wildly throughout the country. Charaka has mentioned
two varieties namely – Stree and Pum Kutaja. Ayurvedic physicians of the
later period found two varieties – namely Swetha and Krishna. These are
correlated as – Swetha to be Pum Kutaja i.e. Holerrhina antidysenterica and
85
Krishna to be Stree Kutaja i.e. Wrightia tinctoria. The parts used are Twak
and Beeja. The bark and seeds contain many alkaloids like Kurchicine,
Conessin, Holerrhine, Kurchin, etc. of which ‘Conessin’ is the important
one. It is a well known remedy for diarrhoea and dysentery and has specific
action on E. histolytica.
Prayojyangas: Twak and Beeja
Matra: Twak Churna – 10 to 30 gm. (taken as Kashaya);
Beeja Churna – 3 to 6 gm.
Gunas:
Rasa : Tikta, Kashya
Guna : Laghu, Ruksha
Veerya : Seeta
Vipaka : Katu
Karmas:
Twak – Kapha Pitta hara, Trishnahara, Amahara, Sulahara, Deepana,
Grahi, Upashoshaka and useful in, Arshas, Krimi, Kushta, Atisara,
Raktapitta, Hridroga, Vatarakta and Visarpa.
Beeja – Tridoshaghna, and other gunas same as twak.
86
Chitraka
Botanical Name : Plumibago Zeylanica Linn.
Family : Plumbaginaceae
Synonyms
Sanskrit : Agni, Vahni, Jvalanakya, Dhana
Telugu : Chitramulam
English : Leadwort
Hindi : Cheetah, Chira, Chitra
Marathi : Chitraka
Bengali : Chita
Gujarati : Chitro
Tamil : Chittira
Urdu : Sheetras
Ganas:
• Deepaneeya, Truptighna, Shoola Prashamana, Bhedaneeya, Arshoghna,
Lekhaneya, Katukaskandha (Cha)
• Pippalyadi, Mustadi, Amalakyadi, Mushkakadi, Varunadi, Argwadhadi
(Su)
• Panchakola, Shadooshana, Hareetakyadi varga (Bha. Pra)
Brief description of the plant: It is a perennial shrub found throughout India,
distributed wildly and is also cultivated. Three varieties of Chitraka are
mentioned in the texts i.e Swetha (P. zeylanica), Rakta (P. indica) and Neela
(P. auriculata). Of these Swetha is the variety abundantly available and
generally used. The part used is root and it contains an alkaloid which is
yellow coloured, bitter in taste forming needle shaped crystals known as
Plumbagin.
87
Prayojyangas : Moola Twak
Matra : 1 – 2 gr. Of powder
Gunas:
Rasa : Katu
Guna : Laghu, Rusha, Ushna, Teeksha
Veerya : Ushna
Vipaka : Katu
Karmas:
Vata kapha haram, Pitta vardhanam, Deepanam, Pachanam, Grahi,
Rasayanam. Useful in Shoola, Grahani, Kustha, Shotha, Arshas, Krumi,
Kasa, Udara and Pandu.
Vishakta lakshanas (toxic symptoms): Excessive dosage produces –
• Kshobhaka and madak visha lakshanas- it produces burning sensation in
throat, stomach & whole body, vomiting and diarrhoea
• Mutrakruchram
• Pulse – low and irregular
• Coldness of skin
• Abortifacient
The condition should be treated with Pitta shamaka, snigdha-sheetala
dravya Prayogam.
88
Saindhava Lavanam
Latin name : Sodii chloridum
Synonyms
Sanskrit : Saindhava, Sheetashiva, Lavanottama, Sindhu lavana,
Pathya, Shivatmaja, Manibandha
Telugu : Saindhava lavanam
English : Sodium chloride
Hindi : Saidhavon
Bangali : Saidhavalanam
Gujarati : Sindhalun
Ganas : Lavana Panchakam, Hareetakyadi varga (Bh.Pra.)
Gunas:
Rasa : Lavana, Madhura
Guna : Laghu, Snigdha, Seeta, Sookshma
Veerya : Anushna
Vipaka : Madhura
Karmas:
Uttama Tridoshagnam, Deepanam, Pachanam, Ruchyam, Himam,
Vrushyam, Netryam, Hrudyam, Avidahi, Lavanothamam.
89
Gudam (Ikshurasa vikara)
Botanical name : Saccharum officinarum Linn.
Family : Graminae
Synonyms
Sanskrit : Ikshu, Dirghacchada, Bhurirasa, Asipatra, Madhutruna,
Gudamula
Telugu : Bellamu, Cheruku
English : Jaggery
Hindi : Gud
Ganas:
• Trina panchamoola (Su)
• Ikshu varga (Bh.Pra.)
Brief Description: Guda or Jaggery is prepared from Ikshurasa by the
‘Rasakriya’ process. It is a rich source of sugar and also contains Iron in
high quantities.
Prayojyanga: Moola, Rasa (made into Sarkara or Guda)
Gunas:
Rasa : Madhura
Guna : Guru, Snigdha
Veerya : Seeta
Vipaka : Madhura
Karmas: Vataghnam, Nati Pittakaram, Vrushya, Mutra sodhaka, Balyam,
Medovardhakam, Kaphavardhakam, Raktapittahara, Trishna prasamana,
Krimikara.
Table showing the Gunas of ingredients of Haritakyadi Lehyam.
Dravya
Rasa
Guna
Veerya
Vipaka Action on Doshas
Other actions
Harithaki Pancharasa, Alavana, Kashaya pradhana
Laghu, Ruksha Ushna Madhura Tridoshahara,
Rasayanam, Deepana, Pachana, Anulomana
Sunthi Katu Laghu, Snigdha Ushna Madhura Kapha Vatahara Deepana, Pachana, Rechana, Balya, Vrushya Vibandha Anaha
Nimba beeja Tikta, Kashaya Laghu, Ruksha Seeta Katu Kapha Vata hara Bhedana, Gulma, Krimi, Kushtha
Karanja beeja Tikta, Katu, Kashaya
Laghu, Teekshna Ushna Katu Kapha Vata hara Meha, Krimi
Indrayava Tikta, Kashaya Laghu, Ruksha Seeta Katu Tridoshaghna Deepana, Grahi, Arshohara
Chitramulam Katu Laghu, Ruksha, Ushna, Teekshna
Ushna Katu Vata Kaphahara Pitta vardhaka
Rasayanam, Deepana, Pachana
Saindhava Lavanam
Lavana, Madhura
Laghu, Snigdha, Seeta
Anushna Madhura Tridoshaghna Deepana, Pachana, Vrushya, Hrudya
Gudam Madhura Guru, Snigdha Seeta Madhura Vataghna, Nati Pittala Kaphakara
Vrushya Balya Rakta pittahara
90
MATERIAL AND METHODS
The present clinical study namely “A Study of the Effect of
Haritakyadi Lehyam in Arshoroga” is carried out at the O.P. wing of the
P.G. Unit of Kayachikitsa, Govt. Ayurvedic Hospital, Erragadda,
Hyderabad, spread over a period of Eighteen months during the years 2006 –
2007.
The cases were selected exclusively from the O.P. wing of the P.G.
Unit of Kayachikitsa. Patients of both the sexes and of all age groups were
taken. The cases were selected randomly and thoroughly examined. Patients
with carcinoma of the rectum were not taken for the study. Patients with
hypertension and diabetes were also taken for study. Finally 30 cases were
taken for the study.
All these patients were examined thoroughly as per the parameters
mentioned in Ayurveda as well as Modern medicine. All the details were
recorded in a special case sheet designed for this purpose. Then the trial drug
‘Haritakyadi Lehyam’ was given for a period of 40 days. Dietary regulations
mentioned for arsho rogi were explained and the patients were asked to
follow them to the possible extent.
The criteria taken into consideration for the assessment of results were
– Sex, Diet, Age group and Economic status, Dosha, Chronicity, Heredity,
Smoking and Alcoholism.
The parameters taken for assessment of result are Vedana, Daha,
Kandu, Sotha, Sravam, Rakta srava, Kharatva, Mala baddhata, Parimana and
Pandu, which were recorded from time to time.
91
Routine investigations like BP, Weight, Hb%, CBP, ESR, RBS, CUE
and special diagnostic procedure i.e. Proctoscopy were done in each and
every case. The necessary investigations were repeated at regular intervals
and the data was recorded carefully in a special case sheet.
Material: The trial drug is Haritakyadi Lehyam which is in the form of
Lehyam, whose ingredients are Haritaki, Sunthi, Nimba beeja, Karanja
beeja, Indrayava, Chitramulam, Saindhava Lavanam, and Gudam.
Matra : The dose of the drug is fixed to be 5gm, twice daily.
Kala : Morning and Night
Anupanam : Jalam
Assessment of Result: In the present clinical study the results were assessed
comparing the subjective and objective parameters, before starting the
treatment and after completion of course of treatment. Based on the
percentage of progress the results are categorized in to three groups –
Result Percentage of Progress
Good above 70%
Moderate 50% - 70%
Poor 30% - 50%
92
OBSERVATION AND RESULTS
The patients were classified according to Sex, Age and Diet,
Economic status, Heredity, Smoking, Habit of Alcohol, Chronicity and
Doshic predominance of Arshas.
Observation
1.Sex: The patients were classified on the basis of sex and the study
reveals that the affected males and females are 19 (63.3%) and 11 (36.7%)
respectively, i.e. the incidence in males is almost double than that in
females, which might be due to the fact that males are subjected more to the
nidanas than females.
Table showing the incidence of Arshas in Male and Female.
Sex No. of patients
Male 19
Female 11
Total 30
2. Age: The patients were classified according to their age and the
present study reveals that the incidence is highest among the age groups of
20-40 years age group i.e. including both 20-30 years age group and 30-40
years age group, whose number is 22 (73.3%), the number of patients in 40-
50 years age group is 6 (20%) and those in 50-60 years age group is 2
(6.7%). As the persons in the above mentioned age groups will be in the
93
stages of final education or early working and earning categories, hence it
can be said that the disease will have a considerable effect on the education
part or the earning part of the life which may affect their lively hood, hence
the necessity for a better treatment.
Table showing the incidence of Arsahs in different age groups.
Age group No. of patients .
21-30 11
31-40 11
41-50 6
51-60 2
Total 30
3. Diet: The patients were classified according to their dietary habit,
whether Vegetarian or Mixed diet. It is observed that the patients taking
mixed diet are more affected 25 patients (83.3%) compared to pure
vegetarian 5 patients (16.7%).
Table showing incidence of Arshas in Vegetarian and Mixed diet
patients.
Dietary habit No. of patients .
Vegetarian 5
Mixed 25
Total 30
94
4.Economic status: The patients were classified according to their
economic status (income), and the observation reveals that the incidence of
Arshas among higher, middle and lower income groups is 10% (3 patients),
56.7% (17 patients) and 33.3% (10 patients) respectively. The reason for the
number being least in higher income group may be the living conditions and
the timely and proper medication, which the people of other two groups are
deprived of.
Table showing the incidence of Arshas in different income groups.
Economic status No. of patients .
Higher income group 3
Middle income group 17
Lower income group 10
Total 30
5. Heredity: The present study reveals that the affected patients
having hereditary history are only 6 (20%) against the number of patients
having no hereditary history, whose number is 24 (80%). This indicates that
though heredity is an important factor, arshas occurring with out hereditary
history due to the severity of the nidanas is also more.
Table showing the incidence of Hereditary factor in arshas patients.
Hereditary history No. of patients .
Present 6
Absent 24
Total 30
95
6. Smoking: The patients are classified based on the habit of
smoking, whose number is 8 (26.7%) and the remaining 22 (73.3%) are non-
smoking. It is observed that in non-smoking category of patients, the relief is
observed early compared to smoking category.
Table showing the number of patients according to habit of Smoking.
Habit of smoking No. of patients .
Yes 8
No 22
Total 30
7. Habit of Alcohol: The patients were classified based on the habit
of consuming alcohol and 7 patients (23.3%) were found to be having the
habit and the remaining 23 (76.6%) were considered to be non-alcoholics. It
is observed that in non-alcoholic category of patients, the relief is observed
early compared to alcoholic category.
Table showing the number of patients according to habit of Alcohol.
Habit of Alcohol No. of patients .
Yes 7
No 23
Total 30
96
8. Chronicity: The patients were classified according to the
chronicity of the arshas. As mentioned in the nidana, history of arshas more
than one year is considered to be chronic and within a year is considered to
be non-chronic. 8 patients (26.7%) were chronic and 22 patients (73.3%)
were non-chronic. It was observed that in chronic cases relief is obtained
after longer duration compared to the other group and relief is also less and
in some cases relief was observed only while using the medicine and after
stopping the medicine the symptoms relapsed.
Table showing the number of patients according to Chronicity.
Chronicity No. of patients .
Chronic 8
Non-chronic 22
Total 30
9. Doshic predominance: The patients were classified according to the
predominance of Dosha and their numbers were found to be 23 (76.7%) in
Vata predominant category and 7 (23.3%) in Kapha predominant category.
Table showing the doshic predominance in arshas patients.
Doshic predominance No. of patients .
Vata 23
Kapha 7
Total 30
97
RESULT:
The result of the study is tabulated as follows:
Table showing the Result of the treatment
No. of patients Result of the treatment . Male Female Total
Good 9 7 16
Moderate 5 3 8
Poor 5 1 6
Total 19 11 30
‘Good’ result was observed in 16 patients (53.3%), most of them
responded in the first 10 days of treatment. Rakta srava, Malabaddhata and
Vedana were completely disappeared and the patients were able to do their
routine work without any disturbance.
‘Moderate’ result was observed in 8 patients (26.7%).
‘Poor’ result was observed in 6 patients (20%).
The results are presented in the form of a ‘Master Table’ and also
depicted in the form of ‘Graphs’.
98
DISCUSSION AND CONCLUSION
Though the modern medical and surgical wings developed vastly, still
there are many diseases, which are not amenable to the present day
management. In these conditions the attention of the patients as well as the
modern medicine is turning to alternate systems of medicine for a better
and permanent solution. The patients suffering with Arshas also belong to
the same category. They feel as if they do not have any cure for the
diseases and they develop some sort of desperate tendency.
Since Arshas occurs due to various nidanas and has many sites,
though treated by surgical way still there are chances of recurrence of the old
ones, as well as new ones may also develop as long as the nidanas are not
taken care of, hence the emphasis on Oushadha chikitsa by Charaka and
Susrutha.
In classics there are many number of medicines prescribed for the
treatment of Arshas. Each and every medicine has its own role of action and
specification. It is needed to evolve a simple and effective medicine among
them, which suits Arshas of all types. This work is a trial for evaluation of
one such medicine at random in the cases of Arshas.
The analysis of the data obtained from the present study gives very
valuable information about the disease which is as follows.
The affected number of males with Arshas is more than that of
females. This can be explained as due to the hard working i.e. laborious jobs,
food habits, habits like smoking and alcohol, altered bowel habits, etc.
99
People in the Age groups of 21 to 30 and 31 to 40 years are more
affected, because it is the prime phase of working hard and earning or to say
the ‘productive period of an individual’, and the people in these age groups
are more exposed to the said causative factors of Arshas and hence the
incidence.
Diet plays an important role as a nidana of Arshas. The people with
mixed dietary habit are more affected than pure vegetarians. This is due to
the less quantity of fiber available in fleshy food stuffs as well as the spicy
nature of them without which people don’t relish them and hence is a must.
The Mamsa ahara and the spicy nature of the food come under the category
of Rajoguna vardhaka ahara, which is considered as Dosha prakopaka and
the nature of the persons taking such ahara are also Rajoguna pradhana. It is
not that the people with other Gunas (Satwa and Tamo) do not take such
food but they may follow the ‘Matra, Kala and Anupana, which are the key
factors behind the menace.
The data about the economic status suggests that the number of
patients in the higher income group is less when compared to the other two
groups. This is because of the working conditions they have, the quality of
the food they can get, the flexibility of time to have timely food and last but
not the least is the proper place to take food. It has been observed in many
cases that people hesitate to carry their own/home made food because they
don’t get proper place to have it and have to resort to the food available
outside. Some people, who are in jobs like marketing, do not have a fixed
schedule, and even take back their lunch boxes because of some or other
reason. Thus ‘proper place to have food’ also stands to be an important
factor. The number of patients in the lower economic group is comparatively
100
less because of their unawareness about Ayurvedic medicine and the false
beliefs about Pathya-apathyas.
Hereditary factor stands to be of moderate concern because the
number of patients with hereditary history is only one fifth of the total
number and the result of the treatment was better in this group because of
the strict adherence to the other regimen advised to them. Hence it can be
said that though Heredity is an important factor, Mithya ahara viharas are of
much more importance both in causation as well as in the treatment aspect.
Smoking and Alcoholism are also important factors as Nidana and
also as Apathya. It was observed that relief was obtained earlier in the
nonsmoking and non-alcoholic category of patients compared to those with
smoking and/or alcohol habit.
Chronicity has its effect on the result of the treatment, perhaps a case
turns to be chronic only if proper attention is not paid and proper care is not
taken of in the aspect of both treatment and Pathya-apathyas. Therefore it is
clearly mentioned in the sadhya-asadhyata aspect that these cases belong to
the ‘Yapya’ category.
Doshic predominance has got its own impact as a nidana factor. If
Arshas itself was considered as a Pitta pradhana vyadhi, Vata is observed to
be anubandha dosha having predominance compared to Kapha. This is
expressed as the lakshanas, of which Rukshata is important one. Therefore
stress was laid on the vatanulomana and snigdha aharas in the chikitsa
aspect.
101
Action of the drug:
The action of the drug can be explained on the basis of its Rasa, Guna,
Veerya, Vipaka and Prabhava and those of HARITHAKYADI LEHYAM
are tabulated below.
Rasa: Madhura rasa is Pitta, Vata samaka, Rakta sangrahaka, Gouravakara
and Anulomana. Lavana rasa is Vata samaka, Ama pachaka, Deepana,
Anulomana and Kledakara. Katu rasa is Vata Kapha samaka, Deepana,
Pachana, Kledakara, Anulomana and Rechana. Tikta rasa is Kapha Pitta
samaka, Ama pachaka, Rakta sangrahaka. Kashaya rasa is Pitta Kapha
samaka, Gouravakara, Rakta sangrahaka, Anulomana. By all these gunas the
drug acts as Tridosha samaka, Deepana, Pachana, Rakta sangrahaka,
Kledakara, Anulomana and Mridu Rechana.
Guna: Laghu and Ruksha gunas are Kapha samaka, Deepana, Pachana,
Rakta sangrahaka. Guru guna is Vata samaka, Kapha vardhaka,
Gouravakara, Anulomana. Snigdha guna is Vata samaka, Mardavakara
Gouravakara, Anulomana. Ushna and Teekshna gunas are Vata Kapha
samaka, Deepana, Pachana, Anulomana, Rechana, etc. Thus by the above
gunas the drug acts as Vata Kapha samaka predominantly, Deepana,
Pachana, Anulomana, Rakta sangrahaka, Rechaka, etc.
Veerya: Seetha veerya acts as Pitta Kapha samaka, Rakta sangrahaka,
Anulomana, etc. Ushna veerya acts as Vata samaka, Deepana, Pachana,
Kledakara, Anulomana, Rechana, etc. Thus the drug acts as Vata Kapha
samaka predominantly, and also Deepana, Pachana, Kledakara, Anulomana,
and Rechana.
Vipaka: Madhura Vipaka is Pitta Vata samaka and Kapha vardhaka. Katu
vipaka is Vata Kapha samaka and Pitta vardhaka. The drug is
102
predominanltly Vata Kapha samaka, Deepana, Pachana, Anulomana and
Rechana.
Prabhava: Rasayana prabhava is possessed by Harithaki, Saindhava lavana
and Chitramula.
By all the above mentioned properties of the individual drugs the
compound drug ‘Harithakyadi Lehyam’ exhibits the actions of Vata Kapha
samana, Deepana, Pachana, Rakta sangrahana, Mardavakara, Kledana,
Anulomana, Mridu rechana, etc. and improvement was seen in all types of
Arshas cases. Pandu condition was also improved by virtue of Gudam. Thus
it can be said that the drug is very effective in all the types of Arshas.
CONCLUSION: The results of the present study are encouraging. Good result was
obtained in 16 cases (53.3%) and Moderate result was seen in 8 cases
(26.7%) and Poor result was obtained in 6 cases (20%). Patients suffering
with severity of the symptoms were also relieved with in first ten days of
treatment. In chronic or Yapya category of cases also relief was observed as
long as the medicine was taken in the dosage and timing as prescribed. All
these facts prove the drug to be very effective in all types of Arshas.
103
SUMMARY
Disease profile
• General introduction of the disease, drug and their selection criteria are
discussed.
• Synonyms, derivations and definitions of the word Arshas are discussed.
• Classification of the Arshas is discussed in detail.
• Anatomical aspect of Guda, Valis with their correlation in modern aspect
is discussed.
• Importance of Guda and process of mala visarjana is discussed.
• Nidana aspect is discussed in detail considering all the types of Arshas.
• Poorva Roopa and Roopa aspects are discussed in detail considering all
the types of Arshas and the Roopa (lakshanas) is given in a tabular form
which serves as a ready reckoner of the lakshanas of all the types of
Arshas.
• Vyadhi vyavachedaka nidanam or differential diagnosis is described.
• Sadhya-asadhayta is discussed.
• Chikitsa part is discussed in detail including principles of treatment,
general line of treatment, and the important drugs, single and compound,
were mentioned.
• Pathya-apathyas are described accordingly.
Drug Review
• In the Drug review part the composition and preparation of the lehyam,
its dosage and description of the individual drugs in detail are mentioned.
104
Clinical Study
• The Methods and Material, Parameters taken for the diagnosis and
assessment of progress in the patients are described.
• In the Observation and Results part, the data obtained in the study is
tabulated and also presented in the form of graphs for easy
understanding.
• In the Discussion and Conclusion part discussion regarding the data
obtained and the derivations done based on the data as well as the
explanation on the mode of action of the drug are given in detail and the
Conclusion is made.
• Finally summary is given.
BIBLIOGRAPHY
A Text Book Of pathology – William Boyd
Amara Kosamu – Jayalakshmi Publications
Ashtanga Hridayam – Chowkhamba publication
Ashtanga Sangraha – Baidyanath publication
Ayurveda Kriya Sareera – Vaidya Ranjit Roy Desai
Bailey and Love – A short text book of Surgery
Bhaishajya Ratnavali - Chowkhamba Publication
Bhava Prakasa – Chowkhamba Publication
Chamberlain’s Symptoms and Signs in Clinical Medicine
Charaka Samhita with commentaries of Chakrapani and Jajjata – Edited by
Sri Hari Datta Sastry, Chowkhamba publiacation
Charaka Samhita, Telugu – Sripada Krishnamurthy Sastry
Clinical Methods of Ayurveda – Prof. K.R. Srikantha Murthy
Differential Diagnosis – Dr.Gupta and Gupta
Dravya Guna Vignan – Acharya Priya Vrat Sharma
Human Anatomy – B.D.Chaurasia
Human Physiology – C.C.Chatterjee
Hutchison’s Clinical Methods
Indian Materia Medica – Dr.K.M.Nadkarni
Indian Medicinal Plants – Orient Longman
Introduction to Kayachikitsa – Dr.C.Dwarakanath
Madhava Nidanam – Deevi Gopalacharyulu
Madhava Nidanam with Madhukosa Vyakhya– Chokhamba publication
Parishadyam Sabdartha Saareeram – Baidyanath
Principles in Surgery – K.Das & S..Das……..
Principles of Anatomy and Physiology - Gerard J. Tortora
Raja Nighantu – Krishna Das Academy, Chowkhamba Publication
Rasa Ratna Samucchayam – Chivukula Satyanarana Sastry
Sareera Kriya Vignanamu – A.P. Ayurvedic Lit. Improvement Trust
Susrutha Samhita – Ambika Datta Sastry - Chowkhamba Publication
Tridosha Theory – V.V.Subrahmanya Sastry
Vedon me Ayurved – Ram Gopal Sastry
REFERENCES
1. Su.Su.33/45 2. As.Hru.Ni. 8/30 3. Ch.Ni. 1/1-5 4. As.Hru.Ni. 1/1 5. 5th - Arsho adhikara 6. 9th – Arsho adhyaya 7. Amarakosa, 2/6/54 8. As.Hru.Ni.7 9. Amarakosa, 2/4/4 10. Amarakosa 1/1/56 11. Amarakosa 2/6/54 12. Ch.Chi.14/6 13. Ch.Chi.14/6 14. A.Hru.Ni. 15. Ch.Chi.1/25 16. Vedon me Ayurved,
Ramgopal Sastry 17. Ch.Sa.3/6 18. Ch.Sa.7/13 19. Ch.Si.9/3 20. As.San.Sa.7/18 21. Su.Ni.3/19 22. Su.Sa.7/23 23. Su.Ni.2/5 24. Su.Ni.2/6-8 25. As.Hru.Ni.7 26. A.D.Sastry on Su.Ni.2/6 27. Dalhana on Su.Ni.2/5 28. As.Hru.Ni.7 29. Dalhana on Su.Ni.2/5 30. Dalhana on Su.Ni.2/5 31. Ch.Su.29/3 32. Su.Sa.6/9 33. Ch.Su.12/8 34. Ch.Vi.5/4 35. Ch. 36. Ch.Chi.14/5 37. Ch.Chi.14/5 38. Su.Ni.2/3 39. Ma.Ni.5/1 40. Ch.Chi.14/171-174
41. As.Hru.Ni.7 42. Ch.Chi.14/38 43. Ch.Chi.14/170 44. Ch.Chi.14/6 45. Ma.Ni.5/43 46. Ch.Chi.14/26-31 47. Bailey and Love, 48. Ma.Ni.5 49. Ma.Ni.5 50. Ma.Ni.5 51. Su.Su.3 52. Ch.Ni.1/7 53. Ma.Ni.1 54. Madhukosa on Ma.Ni.1 55. Su.Ni.1 56. Ch.Chi.14/4-5 57. Su.Ni.2/16 58. Bailey and Love 59. Ch.Chi.14/9-10 60. Su.Ni.2/4 61. Ch.Chi.14/14 62. Ma.Ni.5/3-4 63. Ch.Chi.14/17 64. Ma.Ni.5/5-6 65. Ch.Chi.14/19 66. Ma.Ni.5/7-8 67. Ch.Chi.14/20 68. Ma.Ni.5/9 69. Ch.Chi.14/20 70. Ma.Ni.5/9 71. Bailey and Love 72. Ma.Ni.1.Madhukosa 73. Ch.Chi.14/22 74. Su.Ni. 2/9 75. Ma.Ni.5/31-32 76. Ch.Chi.14/7 77. Ch.Chi.14/8 78. Su.Ni.2/16 79. Ma.Ni.5/9 80. Ch.Chi.14/11 81. As.Hru.Ni.7 82. Ch.Chi.14/12 83. Su.Ni.2/11
84. Ma.Ni.5/10-15 85. Ch.Chi.14/15 86. Su.Ni.2/12 87. Ma.Ni.5/16-18 88. Ch.Chi.14/18 89. Su.Ni.2/13 90. Ma.Ni.5/19-23 91. Su.Ni.2/14 92. Ma.Ni.24-26 93. Comm. on Su.Ni.2/14 94. Ch.Chi.14/171-172 95. Ma.Ni.5/27-28 96. Ch.Chi.14/173-174 97. Ma.Ni.5/29-30 98. Ch.Chi.14/20 99. Ch.Chi.14/20 100. Su.Ni.2/15 101.As.Hru.Ni.7 102.Ma.Ni.5/24 103.Ch.Chi.14/10 104.As.Hru.Ni.7 105.Ma.Ni.5/2 106.Su.Ni.2/4 107.Su.Su.33/4-5 108.Ch.Chi.14/25 109.Ch.Chi.14/31 110.Ma.Ni.5/35 111.Ch.Chi.14/30 112.Ma.Ni.5/36 113.Ch.Chi.14/26-28 114.Ma.Ni.5/37 115.Ch.Chi.14/29 116.Ma.Ni.5/38 117.Su.Ni.2/17 118.Ch.Chi.14/26-28 119.Su.Su.23 120.Ch.Chi.14/36 121.Ch.Chi.14/37 122.Su.Chi.6/3 123.Su.Chi.6/5 124.Su.Chi.6/10 125.Su.Chi.6/13 126.Su.Chi.6/16
127.Su.Chi.6/17 128.Su.Chi.6/19 129.Su.Chi.6/20 130.Su.Chi.6/22 131.Ch.Chi.14/32 132.Ch.Chi.14/60-61 133.Ch.Chi.14/247-248 134.Ch.Chi.14/84-88 135.Ch.Chi.14/72-75 136.Ch.Chi.14/120 137.Ch.Chi.14/125 138.Ch.Chi.14/128 139.Ch.Chi.14/176 140.Ch.Chi.14/181 141.Ch.Chi.14/203 142.Ch.Chi.14/225-228 143.Bailey and Love
MASTER CHART
Sl. No.
Name
Age In
Yrs
Sex
Occupation
Diet
Smoking
Alcohol
Economic
Status
Hereditary
History
Anubandha
Dosha
Chroni
-city
Result
1 Narahari 53 M Carpenter M Yes Yes MIG No Kapha + Poor 2 A.Srinivas 25 M Student M No No MIG No Vata --- Good 3 A.Balaji 40 M Software M Yes Yes MIG Yes Vata + Moderate 4 S.Mahitha 26 F Student M No No MIG No Vata --- Good 5 Y.Hari babu 26 M Student M No No MIG No Vata --- Good 6 B.Venkatesh 27 M Security Guard M Yes Yes LIG No Kapha --- Moderate 7 Smitha 45 F Housewife V No No HIG Yes Vata + Moderate 8 Venkatesh 35 M Employee M No No MIG No Kapha --- Good 9 D.Jyothi 23 F Housewife M No No MIG No Vata --- Good
10 K.Hanumantha Rao 25 M Taxi driver M Yes Yes LIG No Vata --- Good 11 H.Raju 22 M Auto driver M Yes Yes LIG No Vata --- Poor 12 Lakshmi 28 F Research scholar M No No MIG No Kapha --- Good 13 R.Shivaji 27 M Employee M No No LIG No Vata --- Moderate 14 K.Narsing Rao 45 M Employee V No No HIG Yes Vata + Poor 15 Rajesh 35 M Business M No No MIG No Vata --- Good 16 Balamma 40 F Green grocery M No No LIG No Vata --- Moderate 17 Kalavathi 45 F Housewife M No No MIG No Vata --- Good 18 Mangala 35 F Housewife V No No HIG No Vata --- Good 19 Govind 35 M Office boy M Yes Yes LIG No Kapha --- Good 20 Buchaiah 50 M Business M No No MIG Yes Vata + Moderate 21 Nagaiah 50 M Employee M No No MIG No Vata --- Poor 22 Bharathi 45 F Housewife M No No LIG No Vata --- Good 23 Suguna 45 F Employee M No No MIG Yes Vata + Moderate 24 Santhosh 40 M Attender M No No LIG No Vata --- Good 25 Khajauddin 55 M Auto driver M Yes No LIG Yes Kapha + Poor 26 Balabhaskar 42 M Employee M No No MIG No Vata --- Good 27 R.Srinivasa rao 28 M Teacher V No No MIG No Vata --- Good 28 Archana Joshi 32 F Employee V No No MIG No Vata --- Good 29 Ameeruddin 27 M Hamali M Yes Yes LIG No Kapha + Moderate 30 Sumathi 33 F Housewife M No No MIG No Vata --- Poor
ABBREVATIONS:
Diet: V-Vegetarian; M-Mixed
Economic status: LIG – Low Income Group; MIG – Middle Income Group; HIG – Higher Income Group
Chronicity: ‘+’ More than a year; ‘–’ Less than a year