Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
Transcript of Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
-
7/29/2019 Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
1/11
-
7/29/2019 Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
2/11
Best practice
Arch Dis Child Educ Pract Ed2012;97:122131. doi:10.1136/edpract-2011-300593 123
differentiation and convolution occurs to form theprimitive fore, mid and hind brain. By the time we areborn the brain is over 10% of our total body weight(~400 gm), further synaptic connection, supportiveglial cell formation and myelination lead to increasedrapid growth and development. By age 3, the averagebrain weighs 1.2 kg, close on adult size.
The most rapid phase of central nervous system
growth occurs from inutero, until about 5 months afterwe are born. During this stage, the brain is susceptibleto malformation, infection, damage and disruption ofits emerging blood supply, which, in turn, starts devel-oping in the rst trimester of pregnancy on the frontand back surface of the brain and migrates centrallyand downwards to the deeper structures.
Therefore, in the immature brain, the area most sus-ceptible to damage from disruption to the blood owis the central watershed, periventricular zone of themotor cortex the area furthest from the large bloodvessels. However, by full term, the blood supply tothe brain is much more robust and if hypoxic damage
occurs at this stage it is initially in the cells that havethe highest metabolic need the basal ganglia.
Beyond infancy, these basal ganglia are the locomo-tor driving system of our motor control, where reexpatterns of movement are unconsciously co-ordinated.
Fluid motor patterns are initiated by desire and antici-pation of function and are modied by the inputssuch as the peripheral sensory interaction, and visionand balance the equilibrium and adaptive systems.At this point, intracerebral reex loops organise thedescending upper motor control of the peripherallower motor neurons via, among others, the corticos-pinal tracts.
It is obviously a lot more complicated, not leastbecause of the tremendous amount of potential tractreorganisation that can occur with damage neu-roplasticity. There has been considerable researcharound the basic science of the projection and organisa-tion of motor tracts during early neurological develop-ment; outlining the process of functional cortico-spinalinnervation from all ipsi and contralateral areas of thebrain and the subsequent pathway regression.3
Yet, to put it simply, when this complex motor sys-tem is impaired, the uidity of control breaks down,leading to the non-progressive movement disorder.
In summary, anything that can cause non-progres-
sive lesions of the central nervous system can lead to amovement disorder. Developmental structural abnor-malities and in particular disruption in blood ow, pre,peri and postterm lead to different physical impair-ments and thus different clinical patterns.
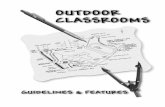
Figu 1 The gross motor unctional classifcation system (GMFCS).
group.bmj.comon September 10, 2012 - Published byep.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://ep.bmj.com/http://ep.bmj.com/http://group.bmj.com/http://ep.bmj.com/ -
7/29/2019 Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
3/11
Best practice
Arch Dis Child Educ Pract Ed2012;97:122131. doi:10.1136/edpract-2011-300593124
With such a myriad of potential causes, CP, as adescriptive umbrella, is by far the commonest physi-cal neurodisability during childhood and as such has amassive socio-economic impact.4 Overall prevalence inEurope, America and Australasia is fairly stable at 23per 1000 live births, though in susceptible prematureinfants it rises to up to 100 per 1000 in those bornbefore 28 weeks gestational age.1
Severity, motor pattern and distribution o CP
There is a massive variance in clinical presentation andrange of disability observed in individuals with CP.The impact of the lesion depends on its site and sever-ity and our management differs with the level of back-ground functional ability.
Subdivision of the movement disorder is dependent onthe distribution, severity and motor pattern observed;as well as by the accompanying comorbidity.
Distribution
Classication systems focus on the pattern of trunk, limband bulbar involvement. There seems to be increasingagreement on using the terms unilateral or bilateral, asoutlined in the SCPE; with less emphasis on hemiple-gia (unilateral), diplegia (leg involvement>arms) andquadriplegia (all four limbs), though these terms arestill frequently used.
Severity of the motor difculty is assessed asfollows:- The gross motor functional classication system
(GMFCS gure 1) is used clinically to delineateindividuals with CP into ve groups dependent ontheir level of mobility; level one being completely
independent and ve totally dependent.5
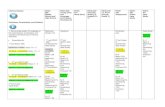
The Manual Ability Classication System (MACS gure 2) does the same for arm and handfunction.6
As yet the oro-motor system and swallowing has notbeen looked at in such detail, but its dysfunctionaleffect on activity and quality of life can be justas marked as the other more obvious motor
difculties.The motor pattern of secondary abnormal muscletone observed is almost universally associated withthe site of the underlying primary pathophysiology,though, as all clinical problems are individual, totalreliance of neuroimaging for diagnosis is not entirelyreliable. Spasticity velocity dependent increase in tonic
stretch reexes causing hypertonia, which isassociated with the positive side of the uppermotor syndrome. Simplistically, the descendingcortico-spinal tracts normally stimulate release ofthe inhibitory neurotransmitter -amino butyric
acid (GABA) at the spinal level. Lesions lead todysinhibition of the spinal reex arc and muscleover activation. Treatment policies focus on musclerigidity/hypertonia rather than the spasticity itself.While we focus on the corticospinal tracts, thereis considerable neuro-physiology research on theinterplay with other pathways of descending motorcontrol.3 7
Functionally, the negative symptoms of the uppermotor syndrome reduced motor activity leadingto weakness and poor selective motor control are
Figu 2 The Manual Ability Classifcation System (MACS).
group.bmj.comon September 10, 2012 - Published byep.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://ep.bmj.com/http://ep.bmj.com/http://group.bmj.com/http://ep.bmj.com/ -
7/29/2019 Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
4/11
Best practice
Arch Dis Child Educ Pract Ed2012;97:122131. doi:10.1136/edpract-2011-300593 125
far more disabling for the individual and moredifcult for us to treat.
Dystonia On the other hand, damage primarilyto the basal ganglia leads to patterns of sustaineddisturbed muscle contraction causing abnormalpostures that are frequently associated withinvoluntary movements especially with sensoryoverload such as anxiety, noise or discomfort
dystonic CP. These strange, non-sustainedmovements can of course be further subdivided, forexample, chorea and athetosis, but the overridingterm of dystonia, helps focus treatment. The termdoes not include rare ataxic forms of CP, whichgenerally arise from impairment of the cerebellum.The term dyskinesia is often used in a similarcontext dys+kinesis=abnormal+movement, souctuating movement pattern.
It is of course more common to see a combinationof dystonic and spastic elements rather than truedystonia within an individuals movement disorder.
Looking at the prevalence of different motor pat-
terns, all have remained remarkably static over the last20 years, though the complexity may have increasedwith neonatal survival.1
1.21.5 per 1000 bilateral spastic CP; 0.60.8 per 1000 unilateral or hemiplegic CP
and 0.150.25 per 1000 bilateral dystonic CP.
Dierential diagnosis
When the clinical team assesses any child with a move-ment disorder, the rst question should be what is thecause? Once again, it is important to stress that CP isnot a diagnostic but a descriptive term. It is vital to
ensure that a progressive or rarely treatable form of amovement disorder is not missed. Clear early obstetricand neonatal history and neurological examination areof greatest aetiological importance. However, even ifan ante, peri or postnatal cause is given, if the pat-tern of on-going development does not continue asexpected, or if other body systems are involved, fur-ther investigation may be necessary to look for a poten-
tial cause, including neuro-imaging and appropriateassays. Indeed the recommendations of the AmericanAcademy of Neurology and SCPE are that all childrenwith suspected CP of uncertain origin should have cer-ebral imaging.1 8
Differential diagnoses include genetic, metabolic,mitochondrial and progressive neurological andneuro-muscular conditions. There are numerousrare differentials but consideration of a dopamineor partial dopamine responsive disorder is particu-larly important in dystonia, when a short therapeutictrial ofl-dihydroxyphenylalanine (DOPA)can makea phenomenal functional difference. If there is any
question of aetiology, referral to a specialist regionalcentre is appropriate. However, routine screeningmetabolic tests alone are unlikely to provide furtherinformation.9
InterventionsPresentation is generally either during neonatalfollow-up with an at risk history or from primarycare screening for neurodevelopmental delay. Often,abnormal muscle tone is obvious from an early stage orelse comorbidities such as epilepsy, gastro-oesophagealreux and feeding difculty are clinically overwhelm-ing. If present, dystonia develops only when the neuralpathways are sufciently mature around 18 months
Figu 3 Medical movement therapy options.
group.bmj.comon September 10, 2012 - Published byep.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://ep.bmj.com/http://ep.bmj.com/http://group.bmj.com/http://ep.bmj.com/ -
7/29/2019 Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
5/11
-
7/29/2019 Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
6/11
Best practice
Arch Dis Child Educ Pract Ed2012;97:122131. doi:10.1136/edpract-2011-300593 127
medical emergency. There is no overriding consen-sus, but generally intravenous clonidine or high-dose benzodiazepines are used followed by articialinitiation of sleep, as this abolishes all dystonicmovements.15
Invasive options
Botulinum toxin A injections
Botulinum toxin A (BTX-A) was rst used to reducefocal spasticity in CP in the mid-1990s. It is licensedonly for use in children over the age of 2 for dynamic
equinus foot deformity caused by spasticity in ambu-lant paediatric CP. However, there has been consid-erable publication on its use in other muscles andglands that cause focal, functional difculty, includingmultilevel lower and upper limb, hip (for pain relief),neck and paraspinal muscles as well as salivary glandinjections. There is good level 1 evidence for its use atcalf, hip adductor, hamstring and upper limb levels.The American Academy of Neurology has stated thatit should be universally offered as a treatment optionduring childhood.12 16
Table 1 Some of the more commonly used oral medicines
Mul laxa bakgoud ad ff sid ff Do
Bacloen The commonest drug or adult and childhoodhypertonia, used since the 1970s
It has diculty crossing the bloodbrainbarrier and thereore high-peripheral doses ooral medicine are necessary or eect
Start5 mg, three times a day, halved invery small children
It works on the pre and postsynaptic GABAB
receptors o the spine to reduce excitation othe spinal refex arc
As such, it has a narrow therapeutic windowbeore signicant side eects o truncalhypotonia, sedation and increased seizurepropensity are seen
Max0.3 mg/kg/day. Increased slowlyto eect or side eect with upperlimits up to 5 mg/kg/day
Tizanidine Used increasingly requently in the adultpopulation
There is limited experience o its use inchildren
Uncertain start1 mg twice daily 10 years
This central 2-noradrenergic agonist is gener-ally better tolerated than bacloen in adults
Sedation, hypotension, agitation, depressionand gastrointestinal problems are the mainside eects
Max0.05 mg/kg/day2 mg three times a day >12 years
Diazepam Other benzodiazepines work at the spinalGABA level by increasing presynaptic inhibi-tion. They are extremely eective, especially inshort-term use i emergency muscle relaxationis needed or sleep disturbed
Highly sedating and tolerance is easilydeveloped
Start0.25 mg/kg twice daily
Benzodiazepine withdrawal syndrome is a sig-nicant concern with long-term use, especiallyin the very young
MaxInant 2.5 mg twice dailyChild 5 mg twice daily>12 years 10 mg twice daily
Dantrolene Works at the muscle level by inhibi ting calciumrelease rom the sarcoplasmic reticulum
It causes global weakness and rarely, thoughcatastrophically, liver ailure in around 1% o
patients
Start0.5 mg/kg twice daily or 4 days,
increase to three times a day thenour times a day
Max3 mg/kg our times a day or 100mg our times a day
Antidystonic medicineInitiation and supervision o such treatment should be in specialist units
LaevoDopa plusCocareldopa
I there is any possible doubt about diagnosisrom history and/or neuroimaging then atrial o LaevoDopa should be given. Rarely aDOPA responsive dystonia can mimic CP withextraordinary benets or the individual itreated early
It is given with a peripheral inhibitor CoCareldopa (Sinemet, Madopar) to minimiseside eects o nausea, insomnia and increasedchorea
Start12 mg/kg/day LDopa in our six doses
Laevo:Cocarel 4:1 ration at low dose, 10:1ratio at high dose
MaxIncrease every 23 days to max10 mg/kg/dayCheck liver unction 6 monthly
Trihexyphenidyl Probably the antidystonic medicine with thegreatest therapeutic benet
Side eects come rom its mode o actionand include disorientation, gastrointestinaldisturbances (especially constipation), urinaryretention and xerostomia (excessively drymouth)
Start0.5, 1 or 2 mg twice daily,increase weekly to twice daily,then three times a day, then 0.5mg 2 mg/week
This anticholinergic agent works at the level othe basal ganglia
Max1 mg/kg/day Exceptionally highdoses are oten necessary, up to1.6 mg/kg/day
Tetrabenazine Dopamine depletors, prevent neurotransmitterdegradation
Akathesia, depression and other mooddisorders, agitation
Start12.5 mg increase slowly to max
Max100 mg/day
CP, cerebral palsy; DOPA, dihydroxyphenylalanine; GABA, -amino butyric acid.
group.bmj.comon September 10, 2012 - Published byep.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://ep.bmj.com/http://ep.bmj.com/http://group.bmj.com/http://ep.bmj.com/ -
7/29/2019 Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
7/11
Best practice
Arch Dis Child Educ Pract Ed2012;97:122131. doi:10.1136/edpract-2011-300593128
Evidence-based guidelines are regularly updated withthe most recent being the 2009 European and 2010International consensus statements.17 These focus onmedicolegal and medicoeconomic factors, commonindications and integration with other therapy modali-ties; appropriate assessment, accepted off license use,dosage, safety, administration, re-evaluation, continua-tion and discontinuation.
Three products are commercially available: Botox
(Allergan, Irvine, California), Dysport (Ipsen, Paris,France) and Xeomin (Merz, Frankfurt, Germany).Their dose ranges are not interchangeable, with indi-vidual different pharmacokinetic and pharmacody-namic responses.
This potent neurotoxin is taken up in neuromus-cular junction end plates due to its high afnity forthe synaptic vesicle protein 2 which is upregulated inactive neurons. The cleaved short chain then targetsthe SNAP-25 protein of the acetylcholine release com-plex, thereby irreversibly blocking the motor end platepotential. Synaptic regression then occurs and a newbud resprouts from the end of the axonal sheath. This
is why the effect of focal muscle relaxation lasts foraround 3 to 4 months. Clinical benet often lasts fora longer period of time due to the prolonged musclerelaxation and stretch. Weakness is exacerbated andthere are increasing concerns about long-term effectsif used too frequently.18
Multidisciplinary assessment of muscle function anddysfunction and correct administration to targetedareas is vital. The use of electromyography (EMG),
muscle stimulators or direct ultrasound guidance forplacement is increasingly accepted as the best practice.It is not a treatment to be used without consideration ofpostinjection guidelines, such as those provided by theAssociation of Paediatric Chartered Physiotherapists.19
Intrathecal baclofen pumps (ITB)
These have been used in paediatrics for over two dec-ades. The aim is to maximise antispasticity benetsof baclofen at the spinal GABA-ergic level and mini-mise the cerebral side effects, by using an implantablepump. Oral baclofen does not cross the bloodbrainbarrier easily as it is poorly fat soluble.
Table 2 Alternative treatments used internationally for the management of CP
complmay hapy Pai ad vid a
Acupuncture A reduction o muscle hypertonicity by the use o both acupuncture and acupressure has beenobserved in children with spastic CP. The degree o benet is very individual but the evidence romcase series are encouraging.
Amino-acid therapy Extremely high doses o oral amino acids are linked with patterning physiotherapy. The latter providesshort-term benet. The ormer is at best physiologically questionable.
Aromatherapy The use o volatile essential plant oils and aromatic compounds to relax overactive muscle contrac-tion.
Alexander technique A method o physical and mental re-education where the ocus is on inducing core stability withsel-improvement techniques.
Bowen technique Specialist osteopathic massage o muscles and ascia to improve movement and posture.
Chinese herbal medicines Modulation o muscle tone by traditional herbal approaches.
Chiropractic therapy Skilled practitioner manipulation, especially o the spine, improves the unction o joints and sur-rounding sot tissues.
Cranial osteopathy The treatment o musculoskeletal problems by inducing sel-recuperation rom somatic dysunction.A multicentre trial has recently been completed on its use in children aged 512 years with cerebralpalsy showing no improvement in health or quality o lie. A number o case series do show consis-tent improvement in posture, range o movement and comort, especially in inants.
Hippotherapy Adaptation to horses movement, working on posture and co-ordination, reducing muscle spasm.There are encouraging case series looking at improvement in core stability.
Homeopathy Homeopathic medicine, including specic G therapy o tissue salts and herb extracts, can be used or
a variety o neurodevelopmental disorders including cerebral palsy. There is no medical evidence inpeer-reviewed journals.
Hyperbaric oxygen therapy The theory is to heal damaged tissue in central nervous system by removing ree radicals by usinghigh oxygen concentrations in pressure chambers. No peer reviewed evidence base.
Scotson technique Focuses on diaphragmatic strengthening, the theory is to improve oxygen fow to the damaged brainby gentle manual delivery o breath and pulse like pressures.
Suit/adeli/thera/spider therapy Repetit ive patterning exercises in a tight-tting suit provide resistance to movement. It is connectedby hooks, rings and elastic bungee cords to provide adjustable pressure and support at dierent jointlevels. It is said to improve motor development and decrease bone demineralisation but evidence islimited.
Refexology Pressure application to the eet and hands, the premise is to restore equilibrium.
Yoga and pilates Various dierent types o physical and breathing exercises, sometimes linked to meditation, to aidrelaxation, strengthen and improve balance and reduce stiness.
CP, cerebral palsy; G therapy, specic Ayurvedic homeopathic strategy or CP.
group.bmj.comon September 10, 2012 - Published byep.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://ep.bmj.com/http://ep.bmj.com/http://group.bmj.com/http://ep.bmj.com/ -
7/29/2019 Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
8/11
Best practice
Arch Dis Child Educ Pract Ed2012;97:122131. doi:10.1136/edpract-2011-300593 129
A recent 2010 European Consensus on the appropri-ate use of ITB therapy in paediatric spasticity has beenpublished.20 This focuses on its use as an antispasticitymeasure, though it is also of benet when both musclehypertonia and dystonia are present.
The evidence is strong for use in young people witha severe motor disability GMFCS levels 4 and 5,though there is less published work on its use in chil-
dren who are independent or therapeutic communitywalkers GMFCS levels 1, 2 and 3, the populationgroup increasingly targeted. An appropriately usedITB can improve care, activities of daily living andquality of life.
A trial of oral medication is initially given to deducethe balance of effect and side effect. As always, carefulassessment and clear understanding of the procedureand the possible outcomes, by all the members of thefamily is necessary.
A screening trial of 50 mcg is given intrathecally, as abolus, to observe any functional improvement. If suc-cessful, the neurosurgical teams insert the pump and
catheter. Standard rates vary individually but are usu-ally in the range of 0.051.25 mg per day. Rellingneeds to occur every few months, through an internalportal; syringe and needle, doses can be regulated atthat time.
Overdose tends to lead to hypotonia, sleepinessand respiratory depression. Clinical signs of with-drawal include increased muscle tone, agitation, hal-lucinations, itching, hyperthermia, seizures and unlessrecognised in time multi organ failure and musclerhabdomyolysis.
Selective dorsal rhizotomySurgical resection of nerve rootlets in the dorsal spi-nal root can reduce the stimulation of the spinal reexarc, a procedure rst carried out in the early 1900s.Exceptionally careful physical, functional and elec-trophysiological assessment is necessary, to minimiserisk and optimise potential, as any such interventionis irreversible.
A minimal laminectomy is performed, the motorand sensory nerves are separated and then the sensorybres are blunt dissected into a series of rootlets. Ontable EMG stimulation elicits peripheral motor effect.
A proportion of rootlets are then cut between 25 and50% of L2 to S2.Recent National Institute for Health and Clinical
Excellence guidelines for the use of SDR in paediatricspasticity have been collated.21 Published effects arevariable and though short-term benets can be marked,long-term functional difference is less reproducible.22Evidence of benet is seen primarily in reducing mod-erate to severe lower limb spasticity GMFCS levels4 and 5. It is also increasingly being used in the inde-pendent walking population GMFCS levels 2 and 3.Great care must be taken not to critically weaken themuscles at the expense of reducing rigidity. In published
series, up to 30% of individuals have irreversible sideeffects such as back pain, increased scoliosis, sensoryloss, weakness, neuropathic bowel and bladder.
The skill of the whole team is therefore vital foroutcome, with a prolonged period of focused reha-bilitation absolutely necessary. Although assessmentand intervention is offered in several regional centres,there is a current trend with children accepted onto
expensive intervention programmes from units outsidethe UK. With long distance and limited appraisal, thereare potential dangers to the child, raised expectationsfor the families and the burden of unplanned expen-sive rehabilitation for NHS services.
In comparative papers, the invasive options ofBTX-A, ITB, SDR and multilevel orthopaedic surgeryseem to have equal mid- to long-term outcomes.2325
Deep brain stimulation
In young people with severe dystonic quadriplegic CP,implanting quadripolar electrodes within the basalganglia of the brain can deliver a continuous electrical
signal to the target nuclei. The globus pallidus internais usually targeted and by doing this aberrant signalsfrom the damaged locomotor driving system are felt tobe made more organised.26
The insertion of this brain pace maker has led tothe improvement in dystonia rating scales between5% and 40%, as well as the general quality of life. Anintact corticospinal tract is necessary for benet so anyextensive damage of this is a contraindication. In thiscase, insertion of an intrathecal baclofen pump wouldbe considered instead.
Obviously assessment, implantation and on-going
management should only occur in specialist centres.Side effects are not uncommon and generally it is onlyconsidered if all other avenues of treatment have nothelped provide a comfortable quality of life. There isat present little published work looking at the long-term benet in children with secondary movementdisorders such as CP but short-term improvement inquality of life is also signicant.
Orthopaedic surgery
Orthopaedic screening in bilateral CP is vital. Earlyhip screening and intervention programmes can make
a dramatic effect on comfort, care and quality of lifeby reducing subluxation and dislocation.27 Later, spi-nal curvature needs regular assessment. Soft tissue andbony surgical management is often core to the holisticwell-being of the child. Timing of any intervention isvital, obviously a child should be better off in the longterm having had surgery than they would have beenwithout it.
Generally surgical options are to lengthen shortened muscletendon complexes, move awkward muscles, bio-mechanically improve lever arms or provide a stable base for standing and/or walking.
group.bmj.comon September 10, 2012 - Published byep.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://ep.bmj.com/http://ep.bmj.com/http://group.bmj.com/http://ep.bmj.com/ -
7/29/2019 Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
9/11
-
7/29/2019 Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
10/11
Best practice
Arch Dis Child Educ Pract Ed2012;97:122131. doi:10.1136/edpract-2011-300593 131
best. Randomised control trials with a baseline of nointervention are difcult to countenance in a situationwhere to do nothing puts the child at risk of develop-ing secondary deformity. However, over the next fewyears both in the UK and in Europe the aim of special-ist working parties will be to provide clinicians withcareful guidance of what motor management policy isappropriate, at what age and developmental level.
compig i None.
Pova ad p viw Commissioned; externally peer reviewed.
reFerences
1. Surveillance of Cerebral Palsy in Europe (SCPE). Surveillance
of cerebral palsy in Europe: a collaboration of cerebral palsy
surveys and registers.Dev Med Child Neurol 2000;42:81624.
2. BaxM, Goldstein M, Rosenbaum P, et al. Proposed denition
and classication of cerebral palsy, April 2005.Dev Med Child
Neurol 2005;47:5716.
3. EyreJA. Corticospinal tract development and its plasticity after
perinatal injury.Neurosci Biobehav Rev 2007;31:113649.
4. SawyerMG, Bittman M, LA Greca AM, et al. Time demands
of caring for children with cerebral palsy: what are theimplications for maternal mental health?Dev Med Child Neurol
2011;53:33843.
5. PalisanoR, Rosenbaum P, Walter S, et al. Development
and reliability of a system to classify gross motor function
in children with cerebral palsy.Dev Med Child Neurol
1997;39:21423.
6. EliassonAC, Krumlinde-Sundholm L, Rsblad B, et al. The
Manual Ability Classication System (MACS) for children with
cerebral palsy: scale development and evidence of validity and
reliability.Dev Med Child Neurol 2006;48:54954.
7. JohnstonMV. Plasticity in the developing brain: implications
for rehabilitation.Dev Disabil Res Rev 2009;15:94101.
8. KorzeniewskiSJ, Birbeck G, DeLano MC, et al. A systematic
review of neuroimaging for cerebral palsy.J Child Neurol
2008;23:21627.
9. LeonardJM, Cozens AL, Reid SM, et al. Should children with
cerebral palsy and normal imaging undergo testing for inherited
metabolic disorders?Dev Med Child Neurol 2011;53:22632.
10. DamianoDL. Rehabilitative therapies in cerebral palsy:
the good, the not as good, and the possible.J Child Neurol
2009;24:12004.
11. AnttilaH, Suoranta J, Malmivaara A, et al. Effectiveness of
physiotherapy and conductive education interventions in
children with cerebral palsy: a focused review.Am J Phys Med
Rehabil 2008;87:478501.
12. DelgadoMR, Hirtz D, Aisen M, et al. Practice parameter:
pharmacologic treatment of spasticity in children andadolescents with cerebral palsy (an evidence-based review):
report of the Quality Standards Subcommittee of the American
Academy of Neurology and the Practice Committee of the
Child Neurology Society.Neurology 2010;74:33643.
13. CloudLJ, Jinnah HA. Treatment strategies for dystonia.Expert
Opin Pharmacother2010;11:515.
14. Carranza-del RioJ, Clegg NJ, Moore A, et al. Use of
trihexyphenidyl in children with cerebral palsy.Pediatr Neurol
2011;44:2026.
15. MariottiP, Fasano A, Contarino MF, et al. Management of
status dystonicus: our experience and review of the literature.
Mov Disord2007;22:9638.
16. SimpsonDM, Gracies JM, Graham HK, et al. Assessment:
Botulinum neurotoxin for the treatment of spasticity (an
evidence-based review): report of the Therapeutics and
Technology Assessment Subcommittee of the American
Academy of Neurology.Neurology 2008;70:16918.
17. HeinenF, Desloovere K, Schroeder AS, et al. The updated
European Consensus 2009 on the use of Botulinum toxin
for children with cerebral palsy.Eur J Paediatr Neurol
2010;14:4566.
18. GoughM, Fairhurst C, Shortland AP. Botulinum toxin andcerebral palsy: time for reection?Dev Med Child Neurol
2005;47:70912.
19. Katchburian L, Cawker S, Coombe et al. Evidence based
guidance for physiotherapists 2008. Association of Paediatric
Chartered Physiotherapists 2008.
20. DanB, Motta F, Vles JS, et al. Consensus on the appropriate
use of intrathecal baclofen (ITB) therapy in paediatric spasticity.
Eur J Paediatr Neurol 2010;14:1928.
21. National Institute for Health and Clinical Excellence
Interventional Procedures Programme. Interventional
Procedure Overview of Selective Dorsal Rhizotomy for
Spasticity in Cerebral Palsy, 2009. IP 3182.
22. GruntS, Becher JG, Vermeulen RJ. Long-term outcome and
adverse effects of selective dorsal rhizotomy in children with
cerebral palsy: a systematic review.Dev Med Child Neurol
2011;53:4908.
23. KanP, Gooch J, Amini A, et al. Surgical treatment of spasticity
in children: comparison of selective dorsal rhizotomy and
intrathecal baclofen pump implantation. Childs Nerv Syst
2008;24:23943.
24. BuckonCE, Thomas SS, Piatt JH Jr, et al. Selective dorsal
rhizotomy versus orthopedic surgery: a multidimensional
assessment of outcome efcacy.Arch Phys Med Rehabil
2004;85:45765.
25. WongAM, Pei YC, Lui TN, et al. Comparison between
botulinum toxin type A injection and selective posterior
rhizotomy in improving gait performance in children withcerebral palsy.J Neurosurg2005;102:3859.
26. VidailhetM, Yelnik J, Lagrange C, et al. Bilateral pallidal deep
brain stimulation for the treatment of patients with dystonia-
choreoathetosis cerebral palsy: a prospective pilot study.
Lancet Neurol 2009;8:70917.
27. HgglundG, Andersson S, Dppe H, et al. Prevention of
dislocation of the hip in children with cerebral palsy.
The rst ten years of a population-based prevention
programme.J Bone Joint Surg Br2005;87:95101.
28. Robb JE, Brunner R. Orthopaedic Management Of Cerebral
Palsy, In Childrens Orthopaedics And Fractures. London, UK:
Springer Verlag, London Ltd 2010:30725.
29. RegenbergAC, Hutchinson LA, Schanker B, et al. Medicine on
the fringe: stem cell-based interventions in advance of evidence.
Stem Cells 2009;27:231219.
30. LiptakGS. Complementary and alternative therapies for cerebral
palsy.Ment Retard Dev Disabil Res Rev 2005;11:15663.
31. WyattK, Edwards V, Franck L, et al. Cranial osteopathy for
children with cerebral palsy: a randomised controlled trial.
Arch Dis Child2011;96:50512.
32. Mackeith Press. The adult with cerebral palsy.Dev Med Child
Neurol 2009;51(suppl 4):1184.
group.bmj.comon September 10, 2012 - Published byep.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://ep.bmj.com/http://ep.bmj.com/http://group.bmj.com/http://ep.bmj.com/ -
7/29/2019 Arch Dis Child Educ Pract Ed-2012-Fairhurst-122-31
11/11
doi: 10.1136/edpract-2011-3005932012 97: 122-131Arch Dis Child Educ Pract Ed
Charlie FairhurstCerebral palsy: the whys and hows
http://ep.bmj.com/content/97/4/122.full.htmlUpdated information and services can be found at:
These include:
Referenceshttp://ep.bmj.com/content/97/4/122.full.html#ref-list-1
This article cites 28 articles, 5 of which can be accessed free at:
service
Email alerting
the box at the top right corner of the online article.
Receive free email alerts when new articles cite this article. Sign up in
CollectionsTopic
(186 articles)Child health(14 articles)Poisoning
(10 articles)Oesophagus(11 articles)Occupational and environmental medicine
(12 articles)Neuromuscular disease(10 articles)Foodborne infections
(42 articles)Drugs: CNS (not psychiatric)(5 articles)Complementary medicine
(17 articles)Epilepsy and seizures(8 articles)Cerebral palsy(11 articles)Editor's choice
Articles on similar topics can be found in the following collections
Notes
http://group.bmj.com/group/rights-licensing/permissionsTo request permissions go to:
http://journals.bmj.com/cgi/reprintformTo order reprints go to:
http://group.bmj.com/subscribe/To subscribe to BMJ go to:
group.bmj.comon September 10, 2012 - Published byep.bmj.comDownloaded from
http://ep.bmj.com/content/97/4/122.full.htmlhttp://ep.bmj.com/content/97/4/122.full.html#ref-list-1http://ep.bmj.com/content/97/4/122.full.html#ref-list-1http://ep.bmj.com/cgi/collection/child_healthhttp://ep.bmj.com/cgi/collection/child_healthhttp://ep.bmj.com/cgi/collection/child_healthhttp://ep.bmj.com/cgi/collection/child_healthhttp://ep.bmj.com/cgi/collection/child_healthhttp://ep.bmj.com/cgi/collection/poisoninghttp://ep.bmj.com/cgi/collection/oesophagushttp://ep.bmj.com/cgi/collection/poisoninghttp://ep.bmj.com/cgi/collection/oesophagushttp://ep.bmj.com/cgi/collection/occupational_and_environmental_medicinehttp://ep.bmj.com/cgi/collection/oesophagushttp://ep.bmj.com/cgi/collection/occupational_and_environmental_medicinehttp://ep.bmj.com/cgi/collection/occupational_and_environmental_medicinehttp://ep.bmj.com/cgi/collection/occupational_and_environmental_medicinehttp://ep.bmj.com/cgi/collection/neuromuscular_diseasehttp://ep.bmj.com/cgi/collection/neuromuscular_diseasehttp://ep.bmj.com/cgi/collection/neuromuscular_diseasehttp://ep.bmj.com/cgi/collection/foodborne_infectionshttp://ep.bmj.com/cgi/collection/drugs_cns_not_psychiatrichttp://ep.bmj.com/cgi/collection/foodborne_infectionshttp://ep.bmj.com/cgi/collection/drugs_cns_not_psychiatrichttp://ep.bmj.com/cgi/collection/drugs_cns_not_psychiatrichttp://ep.bmj.com/cgi/collection/drugs_cns_not_psychiatrichttp://ep.bmj.com/cgi/collection/complementary_medicinehttp://ep.bmj.com/cgi/collection/complementary_medicinehttp://ep.bmj.com/cgi/collection/complementary_medicinehttp://ep.bmj.com/cgi/collection/epilepsy_and_seizureshttp://ep.bmj.com/cgi/collection/epilepsy_and_seizureshttp://ep.bmj.com/cgi/collection/epilepsy_and_seizureshttp://ep.bmj.com/cgi/collection/cerebral_palsyhttp://ep.bmj.com/cgi/collection/cerebral_palsyhttp://group.bmj.com/group/rights-licensing/permissionshttp://group.bmj.com/group/rights-licensing/permissionshttp://journals.bmj.com/cgi/reprintformhttp://journals.bmj.com/cgi/reprintformhttp://group.bmj.com/subscribe/http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://ep.bmj.com/http://ep.bmj.com/http://group.bmj.com/http://ep.bmj.com/http://group.bmj.com/subscribe/http://journals.bmj.com/cgi/reprintformhttp://group.bmj.com/group/rights-licensing/permissionshttp://ep.bmj.com/cgi/collection/child_healthhttp://ep.bmj.com/cgi/collection/poisoninghttp://ep.bmj.com/cgi/collection/oesophagushttp://ep.bmj.com/cgi/collection/occupational_and_environmental_medicinehttp://ep.bmj.com/cgi/collection/neuromuscular_diseasehttp://ep.bmj.com/cgi/collection/foodborne_infectionshttp://ep.bmj.com/cgi/collection/drugs_cns_not_psychiatrichttp://ep.bmj.com/cgi/collection/complementary_medicinehttp://ep.bmj.com/cgi/collection/epilepsy_and_seizureshttp://ep.bmj.com/cgi/collection/cerebral_palsyhttp://ep.bmj.com/cgi/collection/editors_choicehttp://ep.bmj.com/content/97/4/122.full.html#ref-list-1http://ep.bmj.com/content/97/4/122.full.html