ARareCauseofThromboticThrombocytopeniaPurpura- (TTP ...
Transcript of ARareCauseofThromboticThrombocytopeniaPurpura- (TTP ...

Case ReportA Rare Cause of Thrombotic Thrombocytopenia Purpura-(TTP-) Like Syndrome, Vitamin B12 Deficiency: Interpretation ofSignificant Pathological Findings
Morgan Bailey ,1 Travis Maestas,1 Robert Betancourt,1 Dalia Mikhael,2
and Hani M. Babiker 3
1Department of Internal Medicine, University of Arizona, Tucson, AZ, USA2Department of Internal Medicine, Banner University Medical Center-Tucson, Tucson, AZ, USA3Department of Hematology-Oncology, University of Arizona Cancer Center, Tucson, AZ, USA
Correspondence should be addressed to Morgan Bailey; [email protected]
Received 7 December 2018; Accepted 27 February 2019; Published 18 March 2019
Academic Editor: Giuseppe Murdaca
Copyright © 2019Morgan Bailey et al.*is is an open access article distributed under the Creative Commons Attribution License,which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
*rombotic thrombocytopenia purpura (TTP) is a hematological emergency that requires rapid assessment followed by promptinitiation of therapy due to high mortality associated with delayed treatment. TTP has many causes including heritable syn-dromes, ADAMTS13 deficiency, and drugs-related etiologies. Profound vitamin B12 deficiency can, in rare cases, mimic TTP inpresentation, and since plasmapheresis can be of limited benefit, prompt diagnosis is necessary for accurate treatment with B12.*erefore, careful analysis of all clinical signs, symptoms, and labs must be assessed. We report a patient who presented with adiagnosis of TTP, and repeat assessment confirmed a diagnosis of sever vitamin B12 (B12) deficiency with pancytopenia who wasappropriately treated with B12.
1. Introduction
TTP is characterized by a microangiopathic hemolyticanemia (MAHA), thrombocytopenia, and end-organ dys-function which requires accurate diagnosis and plasma-pheresis [1]. With an incidence of 4 cases in 100000, TTP canhave multiple complications including rapid progression toend-organ dysfunction and death [1, 2]. However, it is notuncommon for other conditions, such as vitamin B12 de-ficiency, to present in a similar fashion, with thrombocy-topenia and microangiopathy. Hence, it is important to keepin mind this rare syndrome in addition to other differentialdiagnoses including disseminated intravascular coagulation(DIC), hemolytic-uremic syndrome (HUS), and autoim-mune hemolysis as they can often bemistaken for TTP [2, 3].Because the results of ADAMTS13 are not readily availableat time of presentation, plasmapheresis is often initiated ifthere is a suspicion for TTP. *e case below illustrates suchan example in which the patient presented with
pancytopenia and microangiopathy concerning for TTP.Emergent plasmapheresis was initiated, and upon furtherworkup, the patient symptoms were attributable to a severevitamin B12 deficiency.
2. Case Presentation
A 70-year-old Caucasian woman with no past medicalhistory presented to her local care facility after sustaining amechanical fall the day prior to presentation. She endorsedprogressive fatigue, weakness, and dyspnea on exertion inaddition to symmetric, bilateral lower extremity numbnessfor two months. Per her husband, she had become pro-gressively more confused over the past week in addition toendorsing new onset jaundice and scleral icterus.
On initial presentation, she was confused and dyspneic.Lab work was significant for a severe anemia with a he-moglobin of 5.7 g/dL (12–16 g/dL). She received four unitsof pRBCs and was subsequently transferred to our care
HindawiCase Reports in HematologyVolume 2019, Article ID 1529306, 5 pageshttps://doi.org/10.1155/2019/1529306

facility for further evaluation. On presentation, tempera-ture was 36.3°C, pulse 70 bpm, blood pressure 105/57mmHg, respirations 18, and oxygen saturation of 100%on room air. Physical exam findings were significant formild scleral icterus and palpable splenomegaly. *e patientwas initially oriented to person only; however, the re-mainder of the physical exam, including the neurologicalexam, was unremarkable without motor or sensory deficitson initial presentation. Initial laboratory studies weresignificant for pancytopenia with WBC of 1.8 K/mm3
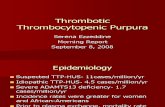
(4.0–11.0 K/mm3), hemoglobin of 8.3 g/dL (12–16 g/dL),MCV of 103 fL (78–100 fL), RDW 24.7% (11.0–15.0%),haptoglobin of <10mg/dL (43–212mg/dL), and platelets of44 K/mm3 (130–450 K/mm3) (Table 1). Direct antiglobulintest was negative. Her chemistry profile was significant fora total bilirubin of 3.7mg/dL (0.2–1.3mg/dL) with a directbilirubin of 1.3mg/dL (0.1–0.5mg/dL), and a lactate de-hydrogenase of 1908 IU/L. Liver chemistries and serumcreatinine were normal. Examination of a repeat peripheralblood smear was significant for hypersegmented neutro-phils and moderate ovalocytes (Figure 1). In addition, therewas concern for schistocytes on the initial smearprompting concern for TTP. At the time of presentation,ADAMTS13 activity was pending. Initially, the patientunderwent plasmapheresis starting on admission, for atotal of three days in addition to prednisone. Repeat smearwas significant for hypersegmented neutrophils and amacrocytic normochromic anemia without evidence of anincrease in schistocytes or microspherocytes to suggest ahemolytic process. Serum B12 level drawn on admissionwas <150 pg/mL (200–650 pg/L). Serum folate level wasnormal, and serum methylmalonic acid level was orderedto confirm the diagnosis of B12 deficiency and was sig-nificantly elevated at 36090 nmol/L (87–318 nmol/L). Anti-intrinsic factor antibodies were positive. In addition, thepatient was found to be hypothyroid with TSH of13.53mIU/L (0.4–4.0mIU/L) and free T4 of 0.58 ng/dLand was started on synthroid at 100 μg daily. *eADAMTS13 result eventually returned within normallimits. *erapy with intramuscular B12 was begun with1000 μg daily, initiated on the same day as plasmapheresis,for one week followed by 1000 μg weekly for four weeks andthen monthly thereafter for life. *e patient continued toclinically improve with treatment. Repeat vitamin B12levels one month after therapy were >2000 pg/mL. CBCvalues also normalized after therapy (Table 2 and Figure 2).Two months after initial therapy, the patient’s confusionhad resolved; however, her bilateral lower extremityneuropathy continued to persist until the initiation ofgabapentin outpatient.
3. Discussion
TTP is an emergent diagnosis and necessitates rapid initiationof plasmapheresis if there is suspicion on initial presentation.Due to the high mortality associated with TTP, plasmaphe-resis is still performed despite ADAMTS13 results not beingimmediately available. *e list of differential diagnoses forhemolytic anemia is broad and can include thrombotic
microangiopathies (TMA), autoimmune hemolytic anemia,drug-induced hemolysis (cephalosporins, dapsone, andlevodopa), paroxysmal nocturnal hemoglobinuria (PNH),and other hereditary syndromes [13]. Vitamin B12 deficiencyis not often associated with hemolytic anemia; however, uponliterature review, there have been multiple cases with similarpresentations [14] (Table 2). Vitamin B12 deficiency can causehemolytic anemia most commonly via intramedullary he-molysis of immature reticulocytes; however, thromboticmicroangiopathy is rarely seen [15]. Reticulocytopenia incobalamin deficiency commonly reflects ineffective erythro-poiesis in the setting of bone marrow involvement andintramedullary destruction as opposed to peripheral hemo-lysis as seen with TTP [15, 16]. *is mechanism is initiated bypremature death via hemolysis of the developing erythrocyteprecursors in the bone marrow and is associated with thelaboratory findings of hemolysis including elevated LDH,bilirubin, and decreased haptoglobin [16, 17]. However, veryfew cases of vitamin B12 deficiency have been linked withMAHA, and previous studies indicate that this may arise fromacute hyperhomocystinemia which can lead to micro-angiopathic hemolytic anemia termed pseudothromboticangiopathy [18]. *erefore, initial laboratory and pathologicfindings can often mimic TTP in severe cases of cobalamindeficiency and in rare cases, such as ours, it can present withmicroangiopathic hemolysis.
4. Conclusion
TTP is a life-threatening microangiopathic hemolytic ane-mia that can lead to death without timely diagnosis and
Table 1: Lab values before and after therapy.
Lab values On presentation *ree weeks aftertherapy
Hemoglobin 5.7 g/dL 11.5 g/dLMCV 103 fL 96 fLPlatelet count 44K/mm3 223K/mm3
White blood cell count 1.8 K/mm3 8.4 K/mm3
Haptoglobin <10mg/dL N/ATotal bilirubin/directbilirubin
3.7mg/dL/1.3mg/dL 1.0mg/dL/NA
LDH 1908 IU/L 279 IU/L HSerum B12 level <150 pg/mL >2000 pg/mL
Figure 1: Hypersegmented neutrophils and hypochromic eryth-rocytes characteristic of a megaloblastic anemia. H&E stain.Magnification: 400x.
2 Case Reports in Hematology

Tabl
e2:
Caserepo
rtsof
severe
vitamin
B12presentin
gwith
finding
ssim
ilarto
TTP.
Cases
areorganizedby
ageof
patient,clin
ical
symptom
sat
timeof
presentatio
n,treatm
ent,and
outcom
es.
Manuscript
Age
Presentatio
nTreatm
ent
Outcome
Rodrigueset
al.[4]
10-m
onth-
oldF
Twoweeks
ofinterm
ittentv
omiting
,poo
rfeeding,anddecrease
inweigh
tpercentile
from
50%
to5%
.Markedpallo
r,sligh
tlyjaun
diced
appearance,and
mild
dehydration
Redbloo
dcells
transfusion,
cyanocob
alam
in(50μg
subcutaneously,fi
vedo
ses;100μg,o
ral,
perd
ayfor1
mon
th),folic
acid
(5mg/day),and
food
diversificatio
n
Biochemical
andhematologic
remiss
ionafter
1weekand1mon
th,respectively.
Infant
developm
entno
rmalized
at24
mon
ths
Tadakamalla
etal.
[5]
31yo
FOne
mon
thof
generalized
fatig
ueandbilateral
paresthesia
sof
thefeet
foron
eweek
Plasmapheresis
for4days
follo
wed
byIM
vitamin
B12
B12def2
/2pernicious
anem
ia.C
omplete
biochemical
respon
seandresolutio
nof
symptom
sat
4mon
ths
RouthandKoenig
[6]
43yo
MTw
o-weekhistoryof
confusion,
fever,dyspnea,
dizziness,andfatig
ueassociated
with
diarrhea
andhematochezia
3un
itsFF
P,plasmapheresis
IMB1
2Not
repo
rted
Podd
eret
al.[7]
46yo
MOne
dayhistoryof
hematuria
andhemop
tysis
Plasmapheresis
24un
itsFF
PRe
solutio
nofbiochemicalparameters.Acquired
TTPin
thesetting
ofpernicious
anem
ia
Chh
abra
etal.[8]
52yo
MFatig
ue,loo
sestoo
ls,andweigh
tloss
forsix
mon
ths
Interm
uscularvitamin
B12
Hem
atological
resolutio
nof
anem
ia
Walteret
at.[9]
77yo
FAlteredmentalstatus,renalinsuffi
ciency,and
thrombo
cytopenia
Plasmapheresis
IMvitamin
B12
forlife
Resolutio
nof
clinical
symptom
sandanem
ia3weeks
afterdischarge
MerinoandCid
[10]
36yo
M3-4weeks
ofastheniain
additio
nto
fatig
ueand
conjun
ctival
pallo
rIM
vitamin
B12forlife
Resolutio
nof
clinical
andbiochemical
parameters
Trub
inet
al.[11]
41yo
FTw
omon
thsof
fatig
ueIM
vitamin
B12for10
days
Resolutio
nof
symptom
sandcorrectio
nof
anem
ia
Chapu
iset
al.[12]
52yo
M14
days
ofshortnesso
fbreath,generalw
eakn
ess,
weigh
tloss,and
asore
tong
ue2un
itspR
BCsIM
vitamin
B12forlife
Resolutio
nof
biochemical
parameters9days
aftertherapy.R
esolutionof
symptom
s6mon
ths
aftertherapy
Case Reports in Hematology 3

treatment with plasmapheresis. Due to the high mortalityassociated with TTP, plasmapheresis should be initiateddespite pending ADAMTS13 results. As discussed above,TTP can often mimic other common hemolytic anemias;however, there are few cases where severe vitamin B12de�ciency can result in a hemolytic anemia (Table 2). Inaddition, pathologic �ndings of severe B12 de�ciency canoften mimic hemolysis both biochemically and on initialpathology [4, 18, 19]. In the presentation above, the initialworking diagnosis was TTP, and thus plasmapheresis wasinitiated. After further workup and con�rmation withnormal ADAMTS13 results, the patient was found to beseverely de�cient in vitamin B12. As discussed, studies haveshown that severe vitamin B12 de�ciency can presentsimilarly as a hemolytic anemia [1, 4–12] with similarbiochemical pro�les, thus leading to the initiation of plas-mapheresis. �is case is important in recognizing this ratherunusual presentation of severe vitamin B12 de�ciency.Health providers should always act urgently if TTP is sus-pected, but as this case points out, it is also important to keepother rare causes of hemolytic anemia, such as severe vi-tamin B12 de�ciency.
Conflicts of Interest
�e authors declare that they have no con�icts of interest.
References
[1] D. W. Abbot, K. D. Friedman, and M. S. Kara�n, “Di�er-entiation of pernicious anemia from thrombotic
thrombocytopenic purpura: the clinical value of subtlepathologic �ndings,” Transfusion and Apheresis Science,vol. 55, no. 3, pp. 318–322, 2016.
[2] F. Yousaf, B. Spinowitz, C. Charytan, and M. Galler, “Per-nicious anemia associated cobalamin de�ciency and throm-botic microangiopathy: case report and review of theliterature,” Case Reports in Medicine, vol. 2017, Article ID9410727, 8 pages, 2017.
[3] L. Garderet, E. Maury, M. Lagrange, A. Najman, G. O�enstadt,and B. Guidet, “Schizocytosis in pernicious anemia mimickingthrombotic thrombocytopenic purpura,”�eAmerican Journalof Medicine, vol. 114, no. 5, pp. 423–425, 2003.
[4] V. Rodrigues, A. Dias, M. J. Brito, I. Galvao, andG. C. Ferreira, “Severe megaloblastic anemia in an infant,”BMJ Case Reports, vol. 2011, Article bcr0220113835, 2011.
[5] A. K. Tadakamalla, S. K. Talluri, and S. Besur, “Pseudo-thrombotic thrombocytopenic purpura: a rare presentationof pernicious anemia,” North American Journal of MedicalSciences, vol. 3, no. 10, pp. 472–474, 2011.
[6] J. K. Routh and S. C. Koenig, “Severe vitamin B12 de�ciencymimicking thrombotic thrombocytopenic purpura,” Blood,vol. 124, no. 11, p. 1844, 2014.
[7] S. Podder, J. Cervates, and B. R. Dey, “Association of acquiredthrombotic thrombocytopaenic purpura in a patient withpernicious anaemia,” BMJ Case Reports, vol. 2015, Article IDbcr2015211989, 2015.
[8] N. Chhabra, S. Lee, and E. G. Sakalis, “Cobalamin de�ciencycausing severe hemolytic anemia: a pernicious presentation,”American Journal of Medicine, vol. 128, no. 10, pp. e5–e6,2015.
[9] K.Walter, J. Vaughn, and D.Martin, “�erapeutic dilemma inthe management of a patient with the clinical picture of TTPand severe B 12 de�ciency,” BMC Hematology, vol. 15, no. 1,p. 16, 2015.
[10] A. Merino and J. Cid, “Very unusual presentation of perni-cious anemia with schistocytes in peripheral blood,” Blood,vol. 122, no. 24, p. 3862, 2013.
[11] P. Trubin, J. Edward, and M. Hand, “Pseudo-thromboticthrombocytopenic purpura due to severe vitamin B12 de-�ciency,” Journal of the Louisiana State Medical Society: Of-�cial Organ of the Louisiana State Medical Society, vol. 168,no. 6, pp. 196–200, 2016.
[12] T. M. Chapuis, B. Favrat, and P. Bodenmann, “Cobalaminde�ciency resulting in a rare haematological disorder: a casereport,” Journal of Medical Case Reports, vol. 3, no. 1, p. 80,2009.
[13] S. P. Stabler, “Vitamin B12 de�ciency,” New England Journalof Medicine, vol. 368, no. 2, pp. 149–160, 2013.
[14] N. Noel, G. Maigne, G. Tertian et al., “Hemolysis andschistocytosis in the emergency department: consider pseu-dothrombotic microangiopathy related to vitamin B12 de-�ciency,” QJM, vol. 106, no. 11, pp. 1017–1022, 2013.
[15] E. Andres, S. A�enberger, J. Zimmer et al., “Current hema-tological �ndings in cobalamin de�ciency. A study of 201consecutive patients with documented cobalamin de�ciency,”Clinical and Laboratory Haematology, vol. 28, no. 1, pp. 50–56,2006.
[16] P. N. Tran and M.-H. Tran, “Cobalamin de�ciency presentingwith thrombotic microangiopathy (TMA) features: a sys-tematic review,” Transfusion and Apheresis Science, vol. 57,no. 1, pp. 102–106, 2018.
[17] B. S. Joly, P. Coppo, and A. Veyradier, “�romboticthrombocytopenic purpura,” Blood, vol. 129, no. 21,pp. 2836–2846, 2017.
0
50
100
150
200
250
300
35011
-29-
17
11-3
0-17
12-1
-17
12-2
-17
12-3
-17
12-4
-17
12-5
-17
12-1
8-17
1-15
-18
2-19
-18
WBCHemoglobinMCVPlatelets
Total bilirubinDirect bilirubinHaptoglobin
Dates of hospital course
Figure 2: Signi�cant lab values throughout hospital course andthree months after initial therapy. Red arrows indicate the dates inwhich the patient underwent plasmapheresis. �e blue arrow in-dicates the date in which B12 replacement was initiated.
4 Case Reports in Hematology

[18] T. Panchabhai, P. Patil, E. Riley, and C. Mitchell, “When thepicture is fragmented: vitamin B12deficiency masquerading asthrombotic thrombocytopenic purpura,” International Jour-nal of Critical Illness and Injury Science, vol. 6, no. 2,pp. 89–92, 2016.
[19] S. Dalia, C. Milani, J. Castillo, A. Mega, and F. J. Schiffman,“Fooled by the fragments: masquerading microangiopathy,”Medicine and Health, Rhode Island, vol. 93, no. 1, pp. 25-26,2010.
Case Reports in Hematology 5

Stem Cells International
Hindawiwww.hindawi.com Volume 2018
Hindawiwww.hindawi.com Volume 2018
MEDIATORSINFLAMMATION
of
EndocrinologyInternational Journal of
Hindawiwww.hindawi.com Volume 2018
Hindawiwww.hindawi.com Volume 2018
Disease Markers
Hindawiwww.hindawi.com Volume 2018
BioMed Research International
OncologyJournal of
Hindawiwww.hindawi.com Volume 2013
Hindawiwww.hindawi.com Volume 2018
Oxidative Medicine and Cellular Longevity
Hindawiwww.hindawi.com Volume 2018
PPAR Research
Hindawi Publishing Corporation http://www.hindawi.com Volume 2013Hindawiwww.hindawi.com
The Scientific World Journal
Volume 2018
Immunology ResearchHindawiwww.hindawi.com Volume 2018
Journal of
ObesityJournal of
Hindawiwww.hindawi.com Volume 2018
Hindawiwww.hindawi.com Volume 2018
Computational and Mathematical Methods in Medicine
Hindawiwww.hindawi.com Volume 2018
Behavioural Neurology
OphthalmologyJournal of
Hindawiwww.hindawi.com Volume 2018
Diabetes ResearchJournal of
Hindawiwww.hindawi.com Volume 2018
Hindawiwww.hindawi.com Volume 2018
Research and TreatmentAIDS
Hindawiwww.hindawi.com Volume 2018
Gastroenterology Research and Practice
Hindawiwww.hindawi.com Volume 2018
Parkinson’s Disease
Evidence-Based Complementary andAlternative Medicine
Volume 2018Hindawiwww.hindawi.com
Submit your manuscripts atwww.hindawi.com