Applying Good Laboratory Practices (GLPs) to In Vitro ......Jul 07, 2005 · vitro methods are...
Transcript of Applying Good Laboratory Practices (GLPs) to In Vitro ......Jul 07, 2005 · vitro methods are...

0
50
100
150
200
7-J
ul-04
21-J
ul-04
4-A
ug-0
4
18-A
ug-0
4
1-S
ep-0
4
15-S
ep-0
4
29-S
ep-0
4
13-O
ct-
04
27-O
ct-
04
10-N
ov-0
4
24-N
ov-0
4
8-D
ec-0
4
22-D
ec-0
4
5-J
an-0
5
19-J
an-0
5
2-F
eb-0
5
16-F
eb-0
5
2-M
ar-
05
16-M
ar-
05
30-M
ar-
05
13-A
pr-
05
27-A
pr-
05
11-M
ay-0
5
25-M
ay-0
5
8-J
un-0
5
22-J
un-0
5
Tissue Lot by Receipt Date
ET
(50
)M
inu
tes
ET(50) IIVS
ET(50) MatTek
IIVS Mean
IIVS Upper Limit
IIVS Lower Limit
Quality Assurance Monitoring
· Suppliers of in vitro test systems should be audited prior to accepting their product for use in a GLP study.
· Depending on the test system, suppliers should maintain a set of in-house release criteria for test systems and associated components. Some of this information may not be available at the time of test system receipt, but it should be evaluated and archived appropriately when it does become available. Even if suppliers perform release testing, controls need to be run with the assay at the Test Facility to account for any changes in the test system due to manufacturing changes or shipping damage.
· In-life audits of studies could be performed a number of ways, including a process-based inspection that might not require auditing a phase from each GLP assay. At IIVS, at least one critical phase in each GLP assay is audited.
· Documentation audits include inspections of the protocol and initial study placement paperwork, the workbook or notebook (raw data), and the study report. Elements of documentation critical to in vitro studies such as justification for use of the test system and protocol-defined acceptance criteria should be examined carefully.
The monitoring of in vitro GLP studies requires the auditors to interpret regulations and guidance documents within a new framework. Emphasis in auditing should be placed on those areas of the in vitro laboratory and assay systems that are critical to control when working with in vitro systems.
The supplier's source of materials and cells should be verified. To avoid potential legal problems with proprietary components (e.g. donor cells), it is necessary to assure that the supplier is licensed to use, or is the owner of the materials they are using to provide their product. The supplier should be audited to assure that they are maintaining their facility and equipment to a level of control appropriate for the type of test system they are supplying. Laboratories need to hold suppliers of cells and three-dimensional tissue constructs to a different standard than they would hold a supplier of ex-vivo tissue (e.g. an abattoir).
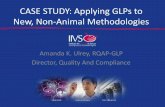
(See Figure 9 for an example of Manufacturing vs. Testing Facility ET response to 0.3% Triton X-100 over time).50
Critical phases are identified prior to performing the study based on the protocol design. Some examples of phases that would be considered "critical" are: test system receipt and handling, test system preparation, application of the test material to the test system, and collection of data. During the in-life audits of the study, auditors should review the documentation (i.e. laboratory notebook or workbook), equipment used, personnel training, and the actual performance of the chosen step. The results of the audit would be circulated to the Study Director and Facility Management.
All elements of documentation combined should provide a full explanation of the conduct of the assay without the need for additional clarification. The final report should accurately reflect the conduct of the assays without any of the data gaps, fabrications, or creative penmanship that led to the establishment of the GLPs in the late 1970s.
TMEpiOcular tissue
Applying Good Laboratory Practices (GLPs) to In Vitro Studies: One Laboratory's Perspective
Amanda K Ulrey, Rodger D Curren, John W Harbell, Greg Mun, and Hans A RaabeInstitute for In Vitro Sciences, Inc., Gaithersburg MD 20878
ABSTRACTThe steady increase in industry use and regulatory acceptance of in vitro test methods has resulted in an increased need to apply Good Laboratory Practice (GLP) regulations to these systems. The original GLP regulations, developed to address the conduct of animal studies, are concerned with many special conditions that apply to animal housing and care, and the relatively long duration of animal studies, that are not present in the shorter in vitro studies. In animal studies, for example, emphasis is placed on the isolation of species and periodic analysis of feed and water; whereas in non-animal studies, there is increased importance on the justification of the test system. Recently, the Organization for Economic Cooperation and Development (OECD) has published advisories (No. 7, The Application of the GLP Principles to Short-term Studies, 1999; No. 14 The Application of the Principles of GLP to in vitro Studies, 2004) to clarify the application of the GLP principles to both short-term and in vitro studies. This poster outlines the approach applied at the Institute for In Vitro Sciences, Inc. (IIVS) to the conduct of in vitro GLP-compliant studies. We describe the translation of the OECD guidance documents into a framework for conducting assays which use ex vivo tissues, monolayer cell cultures, reconstructed skin constructs, and manufactured test kits. We are grateful to auditors from numerous study sponsors and regulatory agencies who have helped us develop what we feel is a best practices approach.
INTRODUCTIONIn the mid 1970s and early 1980s, the US Food and Drug Administration (FDA), and Environmental Protection Agency (EPA) were discovering that the toxicology data submitted to them was not as reliable as they believed. As a result of these revelations, the United States Senate gave power to the agencies to set forth guidelines for laboratories to follow while conducting studies intended for submission. These guidelines, which grew out of industry "best practices", became the Good Laboratory Practices (GLPs) (FDA 21CFR58, EPA TSCA 21CFR792, FIFRA 21CFR160). Many new versions and revisions to the GLPs have been published since the 1970s, so that now, studies conducted in compliance with GLP regulations are recognized throughout the member countries of the OECD and elsewhere as promoting good science and yielding trustworthy data.
The early versions of the GLPs were written with long-term, animal-based toxicology studies in mind. Today, many of these animal-based studies are being replaced by in vitro studies, which are being used by many companies to make safety decisions without accompanying animal data. In order to assure that the data from these validated in vitro methods are universally accepted as being of high quality, the studies must be carried out in compliance with Good Laboratory Practices. Confusion in the interpretation of the regulations arise when the traditional GLPs are applied to short-term, non-animal studies. Differences in test system handling and basic assay design require that the GLPs be supplemented with guidelines that fit the unique structure of these in vitro assays. Workshops were sponsored by such organizations as the European Center for the Validation of Alternative Methods (ECVAM) and IIVS where interested individuals (such as cell culture technologists, toxicologists and quality assurance personnel from industry, academia, and government) were able to discuss the possible design of GLPs for these methods. Following these consensus building workshops, the OECD published "The Application of the GLP Principles to Short Term Studies" (1993, rev. 1999), number 7 in their series on the Principles of GLP and Compliance Monitoring. This document was followed recently (November 2004) by the OECD advisory document titled "The Application of the Principles of GLP to In Vitro Studies" (number 14). These documents supplement the GLPs to effectively assure that there are GLP guidelines to cover all critical aspects of in vitro assay design. Figure 1 shows a time-line of milestones leading to the issuance of the OECD guidance documents for short-term and in vitro studies.
Applying the OECD guidelines in a practical way to day-to-day laboratory work can be challenging. Three areas requiring unique interpretation for in vitro assays are; 1) The use of positive and negative controls and benchmarks; 2) The care and maintenance of test systems; and 3) quality assurance monitoring. At IIVS, we have developed an approach to addressing these areas that has withstood numerous sponsor and several regulatory audits. Although each laboratory will need to apply the Principles of GLP in a way that will complement their facility structure and infrastructure, there are some common concepts that could be applied to in vitro work performed in any laboratory.
Figure 1
Positive and Negative Controls and BenchmarksThe use of benchmarks and positive and negative controls provide valuable information that is highly useful in interpreting results obtained from any study; however, this additional information could not be obtained from in vivo assays without adding additional animals to the study. It is required by Institutional Review Boards (IRB)s and Institutional Animal Care and Use Committees (IACUC)s that measures be taken to reduce the number of animals used for testing as much as possible. In vitro tests allow for the addition of materials to the study without the addition of any moral or ethical concerns.
Positive Control· A positive control sample is run with each assay for the sole purpose of evaluating the performance of the test system. · Positive controls are selected for their ability to detect test system changes in either direction of response · Positive control values from each run of an assay are entered into an historical database (Figure 2 shows the positive control range for the Cytosensor
TM Microphysiometer assay system at IIVS). · At IIVS, the positive control range is updated every three months. · The resulting range is used as a criterion for acceptance of the results of the study.
Negative Control· A negative control sample is run with each assay to measure the response of a dynamic test system over the course of the study. · Negative controls, or blanks, are substances such as sterile, deionized water, saline, or media that are expected to cause little or no change in the test system. · All manipulations specified in the protocol (including removal of the dosing solution) should be carried out on the test system exposed to the negative control.
The use of positive and negative controls should be specified in the study-specific protocol. All control data obtained while running the study are archived along with the study. Spreadsheets maintaining the control ranges are also archived. Since the assay is only accepted when the test system and the controls are performing together within the acceptance ranges, additional characterization and analysis of the controls may not be necessary.
Benchmarks· Although benchmarks (also known as reference materials) are not required by GLP regulations, many sponsors have found it beneficial to run concurrent
benchmarks with studies submitted to agencies.· Benchmarks are materials that are tested alongside the unknown test materials in order to compare and interpret responses. · Benchmarks should be of the same product type as the test materials and be of a defined formulation. For example, a sponsor may submit five new shampoo
formulations to be tested against a shampoo that is already being successfully marketed. · All materials would be run on the same day and the new formulations would be compared against the currently-marketed formulation. · The performance of a benchmark can also be tracked over time to demonstrate consistency in formulation (see Figure 3 as example of many formulations of aerosol
fragrances compared to 2 benchmark materials).
While benchmarks serve to "grade the response of the test system to the test item" (OECD, 2004), they do not necessarily provide enough information to assess the test system's performance (like the positive control).
CYTOSENSOR POSITIVE CONTROL RANGEUpdated 7/7/05
0.0000
0.0200
0.0400
0.0600
0.0800
0.1000
0.1200
0.1400
0.1600
0.1800
Mar.
04
Mar.
04
Mar.
04
Apr.
04
Apr.
04
Apr.
04
Apr.
04
May.
04
May.
04
May.
04
May.
04
May.
04
Jun.04
Jul.
04
Jul.
04
Aug.04
Aug.04
Aug.04
Sep.04
Oct.
04
Oct.
04
Nov.
04
Dec.04
Dec.04
Jan.05
May
05
May
05
May
05
May
05
May
05
Jun.05
Jun.05
Jul.
05
SL
Sco
ncen
trati
on
(mg
/ml)
Figure 2
Figure 3
0
20
40
60
80
100
120
140
1 3 5 7 9
11 13
15
17
19
21
23
25
27
29
31
33
35
37
39
41
43
Formulation #
BC
OP
InV
itro
Sc
ore
(3-m
inu
tee
xp
os
ure
)
Formulation
Ethanol
Reference #1
Reference #2
Test System
· A greater burden is placed on the Study Director to appropriately justify the use of a specific test system.
· As in animal studies, the test system for in vitro studies must be inspected at various times prior to and throughout study conduct.
· The separation of assay types and test systems should be kept in mind when designing the laboratory facility.
· Proper documentation of test system handling is required in both animal studies, as well as in in vitro studies.
· To avoid potential contamination, appropriate separation should be maintained between different test systems.
· The 1997 OECD Principles of GLP state that the test systems "should be acclimatized to the test environment for an adequate period before the first administration/application of the test or reference item." In the case of in vitro test systems, the period of time needed to acclimatize the test system could vary greatly.
· Slight variations between lots of media and reagents have the potential to alter the results obtained from an assay.
A test system is defined as "any biological, chemical, or physical system or a combination thereof, used in a study" (OECD, 1997). In the case of in vitro assays, test systems can range from ex vivo tissues such as the cornea used in the Bovine Corneal Opacity and Permeability Assay (BCOP), to 3T3 cells used in a
TMphototoxicity assay, to the chemical detection media of the CORROSITEX assay for potential dermal corrosivity. While the test systems used in in vitro assays vary greatly, there are a number of common approaches to utilizing them in a GLP study that differ from the handling of animal-based test systems.
Test system selection in animal studies has remained constant for a number of years and is often determined by agency guidelines. A wide number of potentially useful in vitro test systems may be available to address a particular endpoint or need. Study Directors have the ability to choose the proper test system based on the needs of the study. This places great importance on the justification of the test system. This justification should be documented in the protocol and may rely heavily on the prior conduct of successful validation studies using the test system.
Test system inspection helps to show the suitability of the current "batch" of the test system for use in a GLP study. It is important to note the condition of the test system upon receipt. Any in vitro system that does not appear to be suitable for testing, e.g. low cell confluency, contamination, damage, should not be used for a GLP study See Figure 4 for an example of whole globe eyes as they appear upon receipt in the laboratory Test system inspection could involve certain performance checks and/or
a visual inspection. Methods for test system monitoring prior to and during the conduct of the study should be defined in the protocol. If data on test system performance are provided by the supplier, the test facility should verify that the data provided supports the use of the test system for testing. The vendor-supplied quality control data should be retained in the archives.
Ex vivo tissue assays, such as the BCOP assay that are not handled under sterile conditions, should be separated from cell and tissue culture work (See Figure 5 for a photo of the separation of laboratory activities at IIVS). Test materials should be maintained in an isolated area away from the area where most of the assay work is to be performed. While it is not necessary to separate cell cultures by maintaining an incubator for each cell type, test system containers (flasks, culture, plates and dishes) should be properly labeled to avoid confusion. In some dilution-based assays, several dilutions of the test article, along with vehicle controls, may be dosed into consecutive columns on one 96-well plate. If the test material is volatile, contamination between the volatile test material dilutions and adjacent test material or vehicle control dilutions is possible. Separation of the dilutions on a 96-well plate can be achieved by using a plate sealer (See Figure 6 for an example of the difference using a plate sealer can make).
Complete documentation of handling and use is essential to test system traceability through the test facility and use in the assay. Test systems should be tracked from the time they are received in the facility through disposal (including use within an assay if applicable). If the test system needs to leave the facility (as is the case if tissue is sent out for an histological evaluation after test article exposure), it should be accompanied by a Chain of Custody form. An individual should be identified as having responsibility over the test system at all times (usually the Study Director or Principlal Investigator).
Complete labeling of test system containers provides a large amount of protection against mix-ups (See Figures 7 and 8 for examples of proper test system labeling). Work-flow should also be designed with the issue of test system separation in mind.
Cell lines might need to be grown up and split several times prior to beginning the study, which could take several weeks. Three dimensional tissue constructs, on the other hand, only need to be warmed up to a metabolically active state after receipt (which could be as short a time as an hour). As with all other test system specifications, this information should be provided in the study protocol.
The degree to which this variation could potentially occur varies with the type of test system that is being used. If media and reagent variation is a concern (as it would be in cell culture based assays), media and reagent qualification would be beneficial. The positive and negative controls would be run in the assay using the new batch of media or reagent at the same time that another set of controls is run using qualified media or reagents. This approach to media qualification could be adjusted based on the level of risk that the test facility is willing to take. While this approach may be overly cautious for some assay systems, IIVS has found it to be particularly useful in assays such as the Embryonic Stem Cell Assay, which is a labor intensive, multiple day, cell proliferation and differentiation assay system. Media/Reagent qualification can also be useful in the event that the supplier's Quality Control and release testing criteria are not sufficiently stringent to ensure proper functioning in the assay system.
( ).
Cuellar, N., Merrill J.C, Clear, M.L., Mun, G.C., and Herbell, J.W. (2002) The application of benchmarks for the evaluation of the potential ocular irritancy of aerosol fragrances. The Toxicologist 66:243-244
Figure 4
Figure 5 Figure 6
Figure 7 Figure 8
1970s 1980s 1990s 2000s
FDA investigates IBT
FDA launches Toxicology Monitoring
Program
FDA issues GLP
Regulations
EPA Investigates Craven Laboratories
OECD Council adopts Principles of GLPs
EPA Issues GLP Regulations
EC Council Adopts
OECD GLPs
OECD Issues the Application of GLPs
to Short Term Studies
OECD Issues the Application of GLPs
to In Vitro Studies
Useful Resources
EPA Guidance Documents - http://www.epa.gov/compliance EPA Federal Register shortcut - http://www.epa.gov/docs/EPAFR-CONTENTS/
FDA Guidance Documents - http://www.fda.gov/cder/guidance/index.htm FDA Warning Letters - http://www.fda.gov/foi/warning.htm
OECD on-line - http://www.oecd.org Society of Quality Assurance Home Page - http://www.sqa.org
US Code of Federal Regulations - http://www.gpoaccess.gov/cfr/index.html
Figure 9Average and Standard Deviation of
Reference #1 over 44 assays
Average and Standard Deviation of
Reference #2 over 44 assays
Average and Standard Deviation of
Positive Control over 44 assays
Cell Culture Assay Area
Ex Vivo Tissue
Assay Area
NOTE: This graph is constructed to reflect the 240 minute scale of the assay.
IIVS and ECVAM Host “The Principles of Good Laboratory Practice: Application to In Vitro
Toxicology Studies” Workshop
= Positive Control Results Outside of
Range, Therefor the Study Was Repeated
Corneas Rejected Due to Areas of High OpacityCorneas Rejected Due to a Scratch and a Blood Spot
“Acceptable” Cornea
= Positive Control Results Outside of
Range, Therefor the Study Was Repeated
VC = Vehicle ControlDose ID 1= Most concentrated doseDose ID 8 = Least concentrated dose
(With and Without the Use of a Plate Sealer)