Antimicrobial Resistance - Australian Medical Students ... · areas for future improvement in...
Transcript of Antimicrobial Resistance - Australian Medical Students ... · areas for future improvement in...

Policy Document
Antimicrobial Resistance
Background
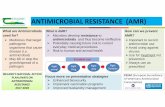
The Australian Medical Students’ Association (AMSA) is the peak representative body of all Australian medical students. AMSA believes that all communities have the right to the best attainable health. Accordingly, AMSA advocates on issues which impact health outcomes of communities in Australia and globally. The World Health Organisation (WHO) defines antimicrobial resistance (AMR) as when “microorganisms such as bacteria, viruses, fungi and parasites change in ways that render the medications used to cure the infections they cause ineffective”.[1] AMR is a serious global health problem, claiming the lives of an estimated 700,000 people worldwide every year.[2] If the current trends in AMR continue, this number is predicted to increase to at least 10 million deaths per year (see Appendix 3).[2] In addition to increased morbidity and mortality, AMR increases the length of hospital stays, the length of time on mechanical ventilation, a need for intensive care and invasive devices as well as excess surgeries performed.[3] Furthermore, AMR burdens hospitals through the need for additional care, support services, diagnostic tests and imaging, use of isolation rooms, and the use of consumables such as gloves.[3] Antibiotic resistance is the highest priority AMR worldwide and in Australia, due to the importance of antibiotic use in many routine therapies including surgery, cancer management and organ transplantation. The most serious resistances include Vancomycin-resistant enterococci (VRE), a community-based strain of methicillin-resistant Staphylococcus aureus (MRSA), resistant Neisseria gonorrhoea, and resistant Enterobacteriaceae.[4-8] Globally, in particular the Asia-Pacific region, multidrug-resistant tuberculosis (MDR-TB) is a significant health issue causing an estimated 170,000 deaths in 2012.[4,5] Antiviral and antimalarial resistance are also a concern in the Asia-Pacific region, with a rise in influenza resistance and the presence of drug-resistant malaria along the Thailand-Cambodian border.[4,9] Antifungal-resistance is associated with deaths attributed to resistant Candida albicans.[4] Recently, alcohol-based handrub resistant Enterococcus faecium has been identified in Australian hospitals, which may lead to a reduction in the efficacy of hand hygiene for controlling spread of bacteria.[10] Factors Contributing to the Rise of Antimicrobial Resistance Multiple factors are contributing to the rise of AMR both within Australia and globally. Antimicrobial agents are used in a variety of settings including human healthcare, veterinary medicine, and in agriculture. Within the human health care setting, factors responsible for the rise of AMR can be broadly separated into healthcare-associated factors and patient-associated factors. A variety of healthcare-associated factors are associated with an increase in AMR. Inappropriate prescription of antimicrobials by doctors contribute to the rise of AMR; Australia has the 8th-highest antimicrobial prescribing rate among OECD countries, and almost a quarter of antibiotic prescribing in hospitals was found to not comply with guidelines.[6] An increase in AMR is associated with excessive use of antimicrobials, failure to narrow antimicrobial therapy when a causative organism is identified, using sub-inhibitory concentrations of antimicrobials and prolonged

prophylactic therapy.[6,11-21] Antibiotic prescribing patterns and attitudes towards antibiotic resistance have been shown to be instilled early on in medical student education.[22,23] This highlights the importance of medical education in combating AMR. Finally, underuse of infection prevention measures such as hand hygiene by staff has shown to be associated with the spread of healthcare-associated resistant microorganisms.[24] Patients also contribute to the rise of AMR by missing doses and stopping use inappropriately.[25] Additionally, patient attitudes, misconceptions and a demand for antibiotics has culminated in 40% of General Practitioners (GPs) admitting to prescribing antibiotics to meet patient expectations.[26] Up to 65% of Australian workers believe they will recover faster from a common cold with antibiotics.[5] Furthermore, despite most Australians being aware of AMR,[3] studies have found that AMR awareness may not equate to understanding.[6] This may manifest as not completing the course of antibiotics, demanding antibiotics for viral infection, sharing antibiotics, and self-medication.[27] Non-human antimicrobial use also has a significant impact on AMR globally.[8] Australia has strict regulations on the use of antibiotics in the agricultural and veterinary industries. Currently there are bans of 3 major antibiotic classes reserved for human use only. These are fluoroquinolones, colistin and fourth generation cephalosporins.[8,28] This has ensured that some resistant strains that are a serious problem elsewhere in the world are of less concern in Australia.[29] Future Directions in Tackling Antimicrobial Resistance In order to shift public attitudes, Australia may consider interventions implemented overseas. France targeted young families through the use of mass media, and involves re-educating high-prescribing practitioners on AMR.[30] Their annual ‘Antibiotics Are Not Automatic’ campaign is associated with a 26.5% reduction of winter antibiotic prescriptions.[30] Evidence from large-scale campaigns in Canada and Belgium suggest that television is the most cost-effective method of increasing awareness of the public on this issue.[31] Furthermore, the UK’s “Do Bugs Need Drugs” campaign demonstrates that interactive education and instruction on behavioural changes such as increased handwashing can improve the public’s understanding of AMR and of its contributing factors.[31] Key messages across successful campaigns are outlined in Appendix 2. Worldwide, governing bodies are calling for both national and international efforts to slow the development of AMR. In 2015, the WHO adopted a global action plan on AMR and outlined five key objectives to achieve this.[32] Alongside the action plan, the WHO launched the ‘Global Antimicrobial Surveillance System’ (GLASS), a global collaborative effort to standardise AMR surveillance.[33] In the first publication, 42 countries had enrolled. Australia is not currently enrolled, and is considering the feasibility of contributing to GLASS.[33] WHO have also developed the ‘One Health’ strategy, a world-wide initiative to bring human and animal health experts together to tackle global health issues such as climate-related disease outbreaks, AMR and zoonotic infections.[34] Establishing the foundations of ‘One Health’ surveillance for AMR as well as increasing surveillance in animal populations and the food industry are important steps outlined in the most recent report “Responding to the threat of Antimicrobial Resistance” by the Department of Health and Department of Agriculture.[5] In line with the WHO, Australia released its first ‘National Antimicrobial Resistance Strategy’ for 2015-2019[5] with the goal of minimising the development and spread of AMR and to ensure the continued availability of effective antimicrobials through seven objectives (Appendix 4). An implementation plan to support this national strategy was released in 2016,[35] and a progress report on the strategy was released in late 2017.[36]

The Australian Government has several other initiatives to combat the spread of AMR. The NIH AMR Challenge receives $20 million in funding to incentivise the development of rapid point-of-care diagnostic tests to prevent spread of AMR.[37] There is an urgent need for further investment in research and development of new antibiotics with the WHO identifying 12 classes of pathogens of high priority in developing AMR.[38] This list includes Neisseria gonorrhoea and Pseudomonas aeruginosa, both of which are Gram negative bacteria for which no new classes of antibiotics have been developed in over 40 years.[39] Currently 33 antimicrobials are in development against these 12 pathogens.[40] However, only 9 of these compounds qualify as innovative antibiotics with a new target, chemical class or mechanism of action.[40] This suggests an urgent need to fund AMR research and to discover novel antimicrobials and biologicals before the resistance crisis becomes a pandemic, with some institutes calling for a public health emergency response from WHO.[41] Many pharmaceutical companies do not view AMR as an economically worthwhile investment due to their relatively short courses, making them less profitable than drugs that manage chronic conditions. Most newly developed antibiotics cost between $1,000 and $3,000 per course.[11] In comparison, chemotherapy costs tens of thousands of dollars.[11] Of the eighteen largest pharmaceutical companies, fifteen have abandoned research in the antibiotic field.[11] In this era of AMR, research can no longer rely on the development of novel antimicrobial compounds, but instead on promising new technologies that may prevent AMR or treat infection in an entirely new way. Novel methods that are being investigated include bacteriophage technology, iChip technology, faecal microbiota transplantation, antimicrobial adjuvants and the CRISPR-Cas9 system.[42-48] See further explanation of novel therapies in Table 2 of the appendices. The National Health and Medical Research Council (NHMRC) has listed AMR as a research priority and has correspondingly increased the funding devoted to this issue in recent years (see figure in Appendix 4). However, AMR research currently receives only $25 million AUD out of the $1 billion AUD total NHMRC funding, despite the imminent global impact of increasing AMR (Appendix 4). Additionally, Australia lacks a national AMR research agenda that identifies specific research and development priorities, and current gaps where the greatest impact of investment could be achieved. Furthermore, Australia still lacks a national mechanism for improved collaboration and data sharing to maximise efficiency of resources. These are all areas for future improvement in tackling the spread of AMR.
Position Statement
AMSA’s position on Antimicrobial Resistance is that:
• AMR is an immediate global threat, requiring an international and collaborative multi-disciplinary and multi-targeted approach.
• Australia should be an international leader in tackling AMR, working internationally to addressing AMR through funding, surveillance and education.
• Australian medical students and medical professionals must take it upon themselves to enact antimicrobial stewardship and minimise inappropriate use of antimicrobials.
Policy AMSA calls upon:
1. The Australian Government to
a. Renew and update the National Antimicrobial Resistance Strategy

when it expires in 2019
b. Facilitate the appropriate and evidence-based antibiotic use across all
sectors through
i. Infection control measures including but not limited to,
vaccination, effective sanitation, hygiene and infection
prevention measures
ii. Public education campaigns about infection control and the
appropriate/inappropriate use of antibiotics
iii. Continual development of appropriate antimicrobial use policies
to combat AMR in the veterinary, agricultural, aquacultural and
food production industries in accordance with the One Health
framework
iv. Develop, provide and implement tailored, evidence-based
resources and approaches to antimicrobial stewardship across
all sectors
c. Actively contribute to surveillance and to the monitoring of AMR
through
i. Contribution to worldwide surveillance of AMR by enrolling in
WHO’s GLASS initiative and to encourage bilateral
participation.
ii. Setting up a government-funded national surveillance system
for AMR in non-human sectors including the agricultural,
aquacultural, and veterinary industries in accordance with the
One Health framework
iii. Regularly reporting on progress AMR through AURA
d. Increase funding into AMR research.
i. Maintain AMR as a research priority and increase investment in
research and development of new antibiotics, alternative
antimicrobial therapies, and vaccinations, with appropriate
funding directed towards priority organisms (table 1.)
ii. Research alternative ways to minimise the spread of AMR such
as effective public education, hygiene processes, and
prescribing guidelines (refer to appendix)
2. Australian Universities to
a. Provide adequate training for medical students in appropriate
antimicrobial use involving a longitudinal and integrative approach to
AMR teaching, including:
i. Training on current prescription guidelines
ii. Interactive and realistic mock-clinical scenarios for students to
practice refusing to prescribe unnecessary antibiotics to
patients requesting them, and educating these patients on why
an antibiotic prescription is inappropriate for their condition.
iii. Emphasising that AMR encompasses antiviral, antiprotozoan
and antifungal resistance as well as antibiotic resistance, and
communicating the importance of these issues in terms of local
and global health.
3. Australian Medical Students to
a. Consider how they will contribute to antibiotic stewardship in the future
including challenging situations where they may feel pressured to
prescribe antibiotics inappropriately.

b. Recognise that AMR encompasses antibacterial, antiviral,
antiprotozoan and antifungal resistance, and raise awareness of this
among colleagues
4. Australian Medical Professionals to
a. Make antimicrobial stewardship an integral part of their practice
through
i. Considering all antimicrobial use, abiding by stewardship
guidelines whether prescribing for patients or when taking
antibiotics themselves
ii. Promoting appropriate, evidence-based antimicrobial
prescription practices
iii. Educating patients about how antibiotics are ineffective against
viruses, and refuse to prescribe them for this reason
iv. Planning and preparing for AMR through the promotion of
preventative methods such as vaccination and methods to
control spread of infection
b. Engage with public health policies regarding AMR
5. Australian Medical Regulatory Bodies and Colleges
a. Sufficient support and encouragement to doctors and hospitals leading
AMR stewardship
b. To develop and maintain guidelines on AMR
References
1. World Health Organization. What is antimicrobial resistance [Internet]. World Health Organization; 2017 July [Cited 2017 August 18]. Available from: http://www.who.int/features/qa/75/en/
2. Review on Antimicrobial Resistance. Antimicrobial Resistance: tackling a crisis for the
future health and wealth of nations. London: Review on Antimicrobial Resistance; 2014 Dec 11. 20 p. Report no.: 1. Available from: https://amr-review.org/Publications.html
3. Cosgrove SE, Carmeli Y. The impact of antimicrobial resistance on health and
economic outcomes. Clin Infect Dis. 2003;36(11):1433-7
4. World Health Organization (CH). Antimicrobial resistance: global report on surveillance. World Health Organization; Apr. 2014. 257 p. Available from: http://www.who.int/drugresistance/documents/surveillancereport/en/
5. Commonwealth of Australia. National antimicrobial resistance strategy 2015-2019. Canberra: Australian Government: Department of Health, Department of Agriculture; 2015 Jun 30. 48 p. Available from: https://www.amr.gov.au/resources/national-amr-strategy
6. Australian Commission on Safety and Quality in Health Care. AURA 2017: second Australian report on antimicrobial use and resistance in human health. Sydney: Australian Commission on Safety and Quality in Health Care; 2017 Aug 2. 238 p. Available from: https://www.safetyandquality.gov.au/publications/second-australian-report-on-antimicrobial-use-and-resistance-in-human-health/
7. Commonwealth of Australia. AMR and human health in Australia. Canberra: Australian Government: Department of Health, Department of Agriculture and Water Resources; 2017 Oct 31. Available from: https://www.amr.gov.au/about-amr/what-current-amr-situation/amr-internationally
8. Australian Pesticides and Veterinary Medicines Authority (APVMA). Antibiotic resistance in animals: a report for the APVMA. Canberra (AU): APVMA; 2017 Aug. 48

p. Available from: https://apvma.gov.au/node/27316
9. World Health Organization. Antimicrobial resistance [Internet]. World Health Organization; 2018 Feb 15 [cited 2018 Jul 29]. Available from: http://www.who.int/en/news-room/fact-sheets/detail/antimicrobial-resistance
10. Pidot S, Gao W, Buultjens AH, Monk IR, Guerillot R, Carter GP et al. Increasing tolerance of hospital Enterococcus faecium to handwash alcohols. Sci Transl Med. [Internet]. 2018 Aug 01 [cited 2018 Aug 15];10(452).
11. Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T.
2015;40(4):277-83.
12. "Duration of antibiotic therapy and resistance". NPS Medicinewise. National Prescribing Service Limited trading, Australia. 13 June 2013. Retrieved 22 July 2015.
13. Laxminarayan R, Duse A, Wattal C, Zaidi AK, Wertheim HF, Sumpradit N, et al.
Antibiotic resistance-the need for global solutions. Lancet Infect Dis. 2013;13(12):1057-98.
14. Pechère JC (September 2001). "Patients' interviews and misuse of antibiotics". Clinical Infectious Diseases. 33 Suppl 3: S170–3. CiteSeerX 10.1.1.560.8090 Freely accessible. doi:10.1086/321844.
15. Arnold SR, Straus SE (October 2005). Arnold SR, ed. "Interventions to improve antibiotic prescribing practices in ambulatory care". The Cochrane Database of Systematic Reviews (4): CD003539.PMID 11524715.
16. Tacconelli E, De Angelis G, Cataldo MA, Pozzi E, Cauda R (January 2008). "Does antibiotic exposure increase the risk of methicillin-resistant Staphylococcus aureus (MRSA) isolation? A systematic review and meta-analysis". The Journal of Antimicrobial Chemotherapy. 61 (1): 26–38.
17. Muto CA, Jernigan JA, Ostrowsky BE, Richet HM, Jarvis WR, Boyce JM, Farr BM (May 2003). "SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus". Infection Control and Hospital Epidemiology. 24 (5): 362–86.
18. Vonberg R. "Clostridium difficile: a challenge for hospitals". European Center for
Disease Prevention and Control. Institute for Medical Microbiology and Hospital Epidemiology: IHE. Archived from the original on 11 June 2009. Retrieved 27 July 2009
19. Kuijper EJ, van Dissel JT, Wilcox MH (August 2007). "Clostridium difficile: changing epidemiology and new treatment options". Current Opinion in Infectious Diseases. 20 (4): 376–83.
20. Leekha S, Terrell CL, Edson RS. General Principles of Antimicrobial Therapy. Mayo Clin Proc. 2011; 86(2): 156–167.
21. Michael CA, Dominey-Howes D, Labbate M. The antimicrobial resistance crisis: causes, consequences and management. Frontiers in Public Health. 2014;2.
22. Australian Commission on Safety and Quality in Health Care. Antimicrobial
Stewardship in Australian Health Care 2018. Sydney: ACSQHC; 2018
23. Ibia E, Sheridan M, Schwartz R. Knowledge of the principles of judicious antibiotic use for upper respiratory infections: a survey of senior medical students. Southern Medical Journal. 2005;98(9).
24. Girou E, Legrand P, Soing-Altrach S, Lemire A, Poulain C, Allaire A, Tkoub-Scheirlinck L, Chai SH, Dupeyron C, Loche CM (October 2006). "Association between hand hygiene compliance and methicillin-resistant Staphylococcus aureus prevalence

in a French rehabilitation hospital". Infection Control and Hospital Epidemiology. 27 (10): 1128–30.
25. Pechère JC (September 2001). "Patients' interviews and misuse of antibiotics".
Clinical Infectious Diseases. 33 Suppl 3: S170–3.
26. Hardy-Holbrook R, Aristidi S, Chandnani V, DeWindt D, Dinh K. Antibiotic resistance and prescribing in Australia: current attitudes and practice of GPs. Healthcare Infection. 2013;18(4):147-51.
27. McNulty CA, Boyle P, Nichols T, Clappison P, Davey P. Don’t wear me out – the
public’s knowledge of and attitudes to antibiotic use. Journal of Antimicrobial Chemotherapy. 2007;59:727-738.
28. Chang Q, Wang W, Regev-Yochay G, Lipsitch M, Hanage WP. Antibiotics in
agriculture and the risk to human health: how worried should we be? Evol Appl. 2015;8(3):240-7.
29. The department (2007). Pilot Surveillance Program for Antimicrobial Resistance in Bacteria of Animal Origin. Australian Government Department of Agriculture Canberra
30. Huttner B, Harbarth S. “Antibiotics are not automatic anymore” – The French national
campaign to cut antibiotic overuse. PLoS Medicine. 2009;6(6).
31. Finch RG, Metlay JP, Davey PG, Baker LJ. Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquium, 2002. The Lancet: Infectious Diseases. 2002;4.
32. World Health Organization. Global Action Plan on Antimicrobial Resistance. Geneva, Switzerland: WHO Press; 2015. ISBN: 978 92 4 150976 3 Contract No.: 19 August 2018.
33. World Health Organization. Global antimicrobial resistance surveillance system (GLASS) report: early implementation 2016-2017. Geneva: WHO Press; 2017. Report No.: 978-92-4-151344-9 Contract No.: 19 August.
34. World Health Organization. One Health 2017 [updated September 2017; cited 2018
19 August]. Available from: http://www.who.int/features/qa/one-health/en/
35. Department of Health. Canberra: Australian Government; 2016 [updated 30 November 2016; cited 2018 19 August]. Available from: https://www.amr.gov.au/resources/national-amr-implementation-plan.
36. Department of Health Department of Agriculture and Water Resources. Australia’s First National Antimicrobial Resistance Strategy 2015‐2019, Progress Report. Australian Government; 2017 1 November 2017. Contract No.: 19 August.
37. Division of Program Coordination, Planning, and Strategic Initiatives. Antimicrobial Resistance Diagnostic Challenge Maryland: National Institutes of Health; 2017 [updated 05 May 2017; cited 2018 19 August]. Available from: https://dpcpsi.nih.gov/AMRChallenge.
38. E. Tacconelli NM. GLOBAL PRIORITY LIST OF ANTIBIOTIC-RESISTANT BACTERIA TO GUIDE RESEARCH, DISCOVERY, AND DEVELOPMENT OF NEW ANTIBIOTICS. Geneva: World Health Organization,; 2017 17 February 2017. Contract No.: 19 August.
39. Buckland, D. (2017), Antimicrobial resistance and the race to find new antibiotics. Prescriber, 28: 12-15. doi:10.1002/psb.1528
40. World Health Organisation, September 2017 Antibacterial agents in clinical development. An analysis of the antibacterial clinical development pipeline, including tuberculosis. WHO/EMP/IAU/2017.11

41. Arie Sophie. Researchers and WHO clash over global threat of drug resistant malaria
BMJ 2017; 359 :j5127
42. Ling LL, Schneider T, Peoples AJ, Spoering AL, Engels I, Conlon BP, et al. A new antibiotic kills pathogens without detectable resistance. Nature. 2015;517(7535):455-9
43. Kaur I. Novel Strategies to Combat Antimicrobial Resistance. Journal Infectious Diseases & Therapy. 2016;4(4):6.
44. Lin DM, Koskella B, Lin HC. Phage therapy: An alternative to antibiotics in the age of multidrug resistance. World J Gastrointest Pharmacol Ther. 2017;8(3):162-73.
45. Millan B, Park H, Hotte N, Mathieu O, Burguiere P, Tompkins TA, et al. Fecal Microbial Transplants Reduce Antibiotic-resistant Genes in Patients With Recurrent Clostridium difficile Infection. Clin Infect Dis. 2016;62(12):1479-86
46. Kim JS, Cho DH, Park M, Chung WJ, Shin D, Ko KS, et al. CRISPR/Cas9-Mediated Re-Sensitization of Antibiotic-Resistant Escherichia coli Harboring Extended-Spectrum beta-Lactamases. J Microbiol Biotechnol. 2016;26(2):394-401
47. Sherpa RT, Reese CJ, Montazeri Aliabadi H. Application of iChip to Grow "Uncultivable" Microorganisms and its Impact on Antibiotic Discovery. J Pharm Pharm Sci. 2015;18(3):303-15
48. Wright GD. Antibiotic Adjuvants: Rescuing Antibiotics from Resistance: (Trends in Microbiology 24, 862-871; October 17, 2016). Trends Microbiol. 2016;24(11):928
49. Leekha S, Terrell CL, Edson RS. General Principles of Antimicrobial Therapy. Mayo Clin Proc. 2011; 86(2): 156–167.
50. Mahy M, Stover J, Stanecki K, Stoneburner R, Tassie JM. Estimating the impact of antiretroviral therapy: regional and global estimates of life-years gained among adults. Sex Transm Infect. 2010;86 Suppl 2:ii67-71
51. Yang WL, Kouyos RD, Boni J, Yerly S, Klimkait T, Aubert V, et al. Persistence of transmitted HIV-1 drug resistance mutations associated with fitness costs and viral genetic backgrounds. PLoS Pathog. 2015;11(3):e1004722
52. Centres for Disease Control and Prevention. Antifungal Resistance 2014 [updated 05 June 2018; cited 2018 17 August]. Available from: https://www.cdc.gov/fungal/antifungal-resistance.html
53. Wiederhold NP. Antifungal resistance: current trends and future strategies to combat. Infect Drug Resist. 2017;10:249-59
54. Salmond G, Fineran P “A Century of the Phage: Past, Present and Future”. 2015, Nature Rev Micro 13, 777-786. Available here: https://www.nature.com/articles/nrmicro3564#main
55. Oechslin F., Piccardi P., Mancini S., Gabard J., Moreillon P., Entenza J.M., Resch G., Que Y-A. "Synergistic interaction between phage therapy and antibiotics clears Pseudomonas aeruginosa infection in endocarditis and reduces virulence" in J Infect Dis. 2016 December; jiw632 Available here: https://academic.oup.com/jid/article/215/5/703/2733318
56. Srisuknimit V J, “Fighting Fire with Fire: Killing bacteria with virus” Feb 1, 2018 Blog: Harvard Science In The News. Available here: http://sitn.hms.harvard.edu/flash/2018/bacteriophage-solution-antibiotics-problem/
57. Kelso, A. ‘Solutions for Drug-Resistant Infections, 4 April 2017 Opportunities for
funding research on antimicrobial resistance through the National Health and Medical Research Council’ 2017. Available here: https://www.nhmrc.gov.au/_files_nhmrc/file/kelso_sdri_4_april_2017.pdf
Policy Details

Name: Antimicrobial Resistance
Category: G – Global Health
History: Adopted, Council 3, 2014 Reviewed, Council 3, 2018
Milla Mclean, Erica Keller, Isobel Dunbabin, Damien Wu, Jessie Zhang, Jonathan Wirth, Rewena Mahesh
Appendix
Definitions Antimicrobial: An agent that kills or stops the growth of microorganisms including bacteria, viruses and fungi. Such agents include antibiotics, antivirals, antiprotozoans, antifungals and disinfectants. Antibiotics: Drugs used in the treatment of or prevention of bacterial infections of an human or animal host. Antivirals: Drugs used in the treatment of viral infections of an human or animal host. Antifungals: Drugs used in the treatment of fungal infections of an human or animal host. Appropriate Antimicrobial Therapy: Appropriate antimicrobial therapy requires several important considerations including: obtaining an accurate diagnosis of the infection, understanding the difference between empiric and definitive treatment, using narrow-spectrum agents when possible, reducing treatment duration where possible, understanding pharmacological characteristics of the drug prescribed and efficacy at the site of infection, and recognising opportunities to ‘watch and wait’.[49] Disinfectant: An agent that kills or inhibits the growth of a range of microorganisms on non-living surfaces.
Abbreviations
ACT - artemisinin combination therapy (used against malaria) AMR - antimicrobial resistance ART - antiretroviral treatment (used to manage HIV/AIDS) ARV - antiretroviral (drug used to manage HIV/AIDS) MDR - multidrug resistant MRSA - Methicillin-resistant Staphylococcus aureus
OECD - Organization for Economic Co-operation and Development VRE - Vancomycin-resistant enterococci WHO - World Health Organization
Appendix 1. Current Statistics Australia Antibiotic resistance:
- In Australia, MRSA has attained a 19% prevalence rate.[5] - In Australia and in other countries, gonorrhoea has shown resistance to its last-resort
treatment.[9] - Australia has higher rates of VRE than any European country with comparable
surveillance systems.[7] - 48% of all critical antimicrobial resistances reported in Australia in 2015 were for
carbapenemase-resistant Enterobacteriaceae (resistant to their antibiotic of last resort).[5]
- MDR Salmonella, E.coli and Campylobacter strains have been found in animals.[8] - Resistance to fluoroquinolone has been found in animals. As the non-human use of
this antibiotic is banned in Australia, this shows that resistance can develop through alternative means that direct exposure to an antimicrobial.[8]

- MDR MRSA has been found in dogs, cats, pigs and horses.[8] - Antibiotic resistance is common in the aquaculture industry, despite minor use permits
for antibiotics only being issued occasionally.[8] Disinfectant resistance:
- Bacteria collected from two major Australian hospitals over a period of nineteen years showed that Enterococcus faecium bacteria displayed increasing tolerance to alcohol such as that used in alcohol-based handrubs.[10]
Antibiotic use: - A 2014 poll of Australian workers showed that 65% of respondents thought that
antibiotics would help them recover from a cold or flu faster.[5] - 20% of Australians expect antibiotics for viral infections.[5] - Almost 60% of surveyed GPs said that they would prescribe antibiotics if a patient
demanded or expected them.[5] - In 2014, 44.7% (10.7 million) Australians received at least one antimicrobial dispensed
under PBS/RPBS.[6] - In 2015, 93% of the antibacterials used in Australian hospitals were one of 20
types.[6] - In Australian hospitals, 23.3% of antibiotic prescribing doesn’t comply with
guidelines.[6] - Antibiotic prescribing rates in the community increased from 2010-2015.[6]
Global Statistics
- Antibiotic use globally rose almost 40% between 2000-2010.[2] - As of 2014, an estimated 700 000 people worldwide each year die due directly to
AMR.[2] - AMR currently costs US health system $21-34 billion USD a year.[4]
Antibiotic resistance:
- Resistance to last resort treatment (carbapenem antibiotics) in Klebsiella pneumoniae exists in all regions of world – in some places, treatment fails in more than half of patients treated.[9]
- Some life-threatening Enterobacteriaceae infections are now untreatable.[9] - The fatality rates for patients with MRSA are up to 64% higher than patients with a
non-resistant Staph. aureus infection.[9] - There were an estimated 450,000 new cases of MDR-TB worldwide in 2012, and
170,000 deaths from this type of the disease.[4] - 3.6% of new TB cases and 20.2% of those previously treated are estimated to be
multi-drug resistant.[4] - Treatment failed for half of all MDR-TB patients in 2014.[9]
ART resistance:
- ART has, between 1995 and 2009, led to an estimated 14.4 million life-years globally in HIV infected patients. [50]
- ART-resistant HIV strains have arisen and transmitting in most countries using ART. Thus, patients infected with these strains will have a higher chance of failing to respond to ART [51]
- 10-17% patients in Europe, US, Australia and Japan who have not previously started ART for HIV have resistance to at least one ARV drug.[4]
- Some countries reported resistance to first-line treatments of more than 15% in those starting ART, and of almost 40% in those restarting it.[9]
- The nature of HIV means that some level of ARV-resistance develops even with optimum treatment and adherence.[4]
- Resistance to ARV drugs is increasing slowly with the increased use of ART;[4] and in 2015, the WHO recommended ART for everyone living with HIV.[9]
- Second-line ARV treatments are three times more expensive than first-line treatments, and third-line treatments are eighteen times more expensive.[9]
Antimalarial resistance: ACT resistance for P. falciparum now in Cambodia, Myanmar, Thailand, Viet Nam & Lao People’s Democratic Republic.[9]
- makes global malaria control more expensive and less effective – also in indirect social costs.[4]

- The estimated costs to contain artemisinin resistance in areas where this exists are
US$10-20 a year per person at risk.[4] Other antiviral resistance:
- The global use of antiviral drugs in treating pandemic and epidemic influenza has increased over the last 10 years.[4]
- Widespread resistance to adamantanes, one of the two classes of antivirals effective in treating influenza exists - therefore these are not commonly used.[4]
- The remaining class, neuraminidase inhibitors, are often stockpiled in preparation for pandemics; but resistance to one of these (oseltamivir) has already emerged, indicating that resistance to all antivirals used against influenza is a real possibility.[4]
Antifungal resistance: - Resistance to antifungals, including fluconazole, exists; this is especially a problem in
systemic candidiasis and in countries where fluconazole is the standard or only available antifungal treatment.[4]
- Resistance to echinocandins is an emerging problem in developed countries where these are recommended therapy.[4]
- Candida infections currently cost the US health system $8 billion USD each year,[4] and high mortality and morbidity rates are associated with invasive Candida infections.[4]
- The number of resistant Candida glabrata strains to echinocandins, the mainstay treatment of Candida glabrata, doubled between 2008 and 2014. [52]
- There are currently few available antifungal agents, some of which have potential drug-drug interactions and adverse effects limiting their usage. [53]
Appendix 2. Key Messages in Successful Campaigns involving AMR The common key messages across successful campaigns involved a combination of 1) antibiotics are only for bacterial infections 2) colds and most coughs are caused by viruses 3) do not miss or leave unfinished doses 4) empowering the public to wash their hands and enquire about narrow spectrum antibiotics. These campaigns highlight the necessity for sustained and multifaceted campaigns that target both the public and primary care providers. References [32] and [33].
Appendix 3. Future predictions
1. If current trends continue, some estimate that AMR will claim the lives of 10 million people a year by 2050, with 22,000 deaths a year in Australia. [2] This can be compared to the 8.2 million deaths that will be caused by cancer. [2]
2. There will be a 2-3.5% reduction in global GDP, amounting to $100 trillion USD. [2] 3. If effective antimicrobials become unavailable, infection rates following hip
replacements could rise to 40-50% with a fatality rate of up to 30%. [6]
Table 1. Priority pathogens identified by WHO and their resistance
Pathogen Current resistance
Mycobacterium tuberculosis Multidrug resistance, including to isoniazid and rifampicin. Extensively drug resistant strains also resistant to fluoroquinolones and injectable second-line anti-TB medications.
Acinetobacter baumannii Carbapenem resistance
Pseudomonas aeruginosa Carbapenem resistance
Enterobacteriaceae Carbapenem resistance 3rd generation cephalosporin resistance

Staphylococcus aureus Vancomycin resistance Methicillin resistance
Enterococcus faecium Vancomycin resistance
Helicobacter pylori Clarithromycin resistance
Salmonella species Fluoroquinolone resistance
Campylobacter species Fluoroquinolone resistance
Neisseria gonorrhoea 3rd generation cephalosporin resistance fluoroquinolone resistance
Streptococcus pneumoniae Penicillin resistance
Haemophilus influenzae Ampicillin resistance
Shigella species Fluoroquinolone resistance
WHO Antibacterial Agents in Clinical Development 2017 [40]
Table 2. Novel Techniques with research papers
Technique Summary References
Bacteriophage technology
Currently there are trials looking at bacteriophage viruses to infect and lyse bacteria. [44] One promising trial, PhagoBurn has shown results in clearing Pseudomonas aeruginosa infection [54,55]. Phage therapy however is far from a manufacturing stage due to issues relating to purification. [56]
Lin, 2017 [44] Salmond 2015 [54] Oechslin, 2016 [55] Srisuknimit, 2018 [56]
Faecal microbiota transplantation
faecal microbiota transplantation which has shown a reduction of AMR genes in Clostridium difficile-infected patients [45]
Millan 2016, [45]
CRISPR-Cas9 CRISPR-Cas9 system which shows promise against E. coli [46]
Kim et al. 2016, [46]
iChip A novel iChip technique has been developed to explore a greater diversity of soil-residing organisms with potential antimicrobial properties. iChip has discovered Teixobactin against Gram-positive bacteria in 2015 [42]
Ling 2015, [42]
Appendix 4. Australian strategies against AMR and NHMRC funding into AMR
Australia’s first national antimicrobial resistance strategy 2015-2019 Objectives:
1. Increase awareness and understanding of antimicrobial resistance, its implications, and actions to combat it through effective communication, education and training
2. Implement effective antimicrobial stewardship practices across human health and animal care settings to ensure the appropriate and judicious prescribing, dispensing and administering of antimicrobials
3. Develop nationally coordinated One Health surveillance of antimicrobial resistance and antimicrobial usage

4. Improve infection prevention and control measures across human health and animal
care settings to help prevent infections and the spread of antimicrobial resistance 5. Agree a national research agenda and promote investment in the discovery and
development of new products and approaches to prevent, detect and contain antimicrobial resistance.
6. Strengthen international partnerships and collaboration on regional and global efforts to respond to antimicrobial resistance.
7. Establish and support clear governance arrangements at the local, jurisdictional, national and international levels to ensure leadership, engagement and accountability for actions to combat antimicrobial resistance.
NHMRC funding for AMR research, and alignment with AMR strategy. [57]