ANNEXURE 3 MASTER CHART52.172.27.147:8080/jspui/bitstream/123456789/9478/1/gaurav.pdf · BREAST...
Transcript of ANNEXURE 3 MASTER CHART52.172.27.147:8080/jspui/bitstream/123456789/9478/1/gaurav.pdf · BREAST...
-
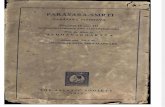
“SENTINEL LYMPH NODE BIOPSY IN EARLY
BREAST CANCER USING METHYLENE BLUE”
BY
Dr. GAURAV PARASHAR M.B.B.S.
Dissertation submitted to the
Rajiv Gandhi University of Health Sciences, Bangalore, Karnataka
In Partial fulfillment
of the requirements for the degree of
MASTER OF SURGERY
IN
GENERAL SURGERY
Under the guidance of
Dr. DINESH M. GUNASAGAR M.S.
Professor
DEPARTMENT OF GENERAL SURGERY
J.J.M. MEDICAL COLLEGE
DAVANGERE 577004
2014
-
i
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES
-
ii
-
iii
-
iv
© Rajiv Gandhi University of Health Sciences, Karnataka
-
v
ACKNOWLEDGEMENT
Dissertation writing is that point of time in our career as a PG, which puts us all
through trying times. The unaccustomed task of sorting out references, collecting
data, writing discussions, to fathom statistics, does leave one fuzzy and apprehensive.
But this daunting assignment saw an easy execution thanks to the guidance and
support of my teachers, family and colleagues.
First and foremost I would like to extend my sincere thanks and appreciation
towards all our patients for their willingness to cooperate with this study.
I express my heartfelt gratitude to my guide Dr. Dinesh MG, Professor,
Department of Surgery, JJM Medical College, Davangere, an embodiment of
patience and compassion who with his vast experience helped me through my
dissertation work and without whose support this dissertation would not have seen
the light of this day.
My inexpressible gratitude to Dr R.L.Chandersekhar, Professor & Head,
Department of Surgery, JJM Medical College, Davangere, without whose support
and constant encouragement, my dissertation and post graduate course wouldn’t have
been such a hurdle free experience.
With great respect, I express my gratitude to Dr. Patil Virupaxa
Gouda, Professor, Department of Surgery, JJM Medical College, Davangere, a
fastidious disciplinarian for his encouragement and cooperation at every juncture.
My sincere thanks to my Professors Dr. R.M. SHEKHAR, Dr. M.
SHIVAKUMAR, Dr. G.C. RAJENDRA, Dr. G. MANJUNATH GOWDA, Dr.
J.T. BASAVARAJ, Dr. S.N. SOMASEKHAR, Dr. DEEPAK UDAPUDI,
-
vi
-
vii
LIST OF ABBREVIATIONS USED
(in alphabetical order)
1. AJCC American Joint Committee on Cancer
2. ALND Axillary Lymph Node Dissection
3. FN False Negative
4. FP False Positive
5. H&E Hematoxylon & Eosin
6. IM Internal Mammary
7. IMC Internal Mammary Chain
8. IMN Internal Mammary Noade
9. IMSN Internal Mammary Sentinel Node
10. ITC Isolated Tumor Cells
11. LNMM Lymph Node Micro Metastasis
12. mm millimeter
13. MRM Modified Radical Mastectomy
14. NPV Negative Predictive Value
15. PPV Positive Predictive Value
16. RT Radiotherapy
17. SLN Sentinel Lymph Node
18. SLNB Sentinel Lymph Node Biopsy
19. TN True Negative
20. TP True Positive
21. UICC Union for International Cancer Control
-
viii
ABSTRACT
Background: SLNB in early breast cancer performed by intra-parenchymal and/or
intra-dermal injections of blue dye and/or radioactive colloid remains a highly
acceptable method of identifying sentinel nodes, largely because of its high success
rate. The purpose of this study is to assess the efficacy of dye-only SLNB by using
the sub-areolar injection of methylene blue dye in our set up.
Study Design: In the 2 years between June 2011 and May 2013, 58 women with
early breast cancer in stages T1/T2 N0M0 underwent sentinel node biopsy
performed solely by subareolar injections of methylene blue dye, followed by
MRM. The technique involved the injection of methylene blue dye into the
subareolar plexus. The ability of subareolar dye injections to identify sentinel nodes
and accurately predict the pathologic status of the axilla was determined.
Results: The identification rate of sentinel nodes was 86% (in 50 of 58 patients).
Axillary basins harbouring positive lymph nodes were found in 32 (64%) of these
50 patients. In 18 cases no axillary node metastasis was found. All 8 cases in which
sentinel lymph node was not identified had axillary node metastasis. Sentinel nodes
correctly predicted the status of these positive axillary basins in 27(84.38%) of 32
patients. SLN correctly predicted the negative status of axillary lymph nodes in 18
cases. There were 5 cases of false-negative sentinel node biopsies, indicating a
false-negative rate of 15.63%. The overall accuracy, sensitivity and specificity were
-
ix
90%, 84.38% and 100% respectively. The positive & negative predictive value of
SLNB in our study was 100% & 78.26% respectively.
Conclusions: The present study of sub areolar methylene blue dye injection shows
comparable results with other series of dye only SLNB in identifying SLN. Our
study, however has slightly higher (15.63%) false negative rate in comparison to
these studies. On the basis of these findings, we propose routine application of this
procedure along with completion ALND in our set up, in selected patients, to
provide an opportunity for both surgeon and pathologist to gain expertise and reduce
the false negative rate to an acceptable minimum.
Keywords: Sentinel Lymph Node; Sentinel Lymph Node Biopsy; Methylene
Blue; Breast Cancer; Subareolar Injection; Axillary Lymph Node,
Axiilary Lymph Node Dissection
-
x
TABLE OF CONTENTS
PAGE No.
1. INTRODUCTION 01
2. OBJECTIVES 04
3. REVIEW OF LITERATURE 06
4. METHODOLOGY 49
5. RESULTS 53
6. DISCUSSION 62
7. CONCLUSION 68
8. SUMMARY 70
9. BIBLIOGRAPHY 72
10. ANNEXURES 85
ANNEXURE 1: PROFORMA 86
ANNEXURE 2: CONSENT FORM 93
ANNEXURE 3: MASTER CHART 96
-
xi
LIST OF TABLES
Table
No
Tables Pg No.
1 Tumor characteristics of patients in whom SLN identified 55
2 Tumor characteristics of patients in whom SLN not
identified
57
3 Salient features of SLN 59
4 Statistics (Diagnostic Validation Tests) 61
5 Summary of the literature on injection technique for SLNB 65
6 Summary of the literature on dye only injection technique
for SLNB
67
-
xii
LIST OF FIGURES
Fig. No. FIGURES Pg No.
1 Quadrants of Breast 17
2 Vasculature of Breast 20
3 Lymphatic Draining of breast parenchyma into axillary
lymph node & further spread
26
4 Lymphatic drainage of breast 27
5 Subareolar Injection of Methylene Blue Dye 36
6 Subareolar Injection of Methylene Blue Dye 36
7 Stained Lymphatics after Subareolar Injection of Methylene
Blue
37
8 Methylene Blue stained Lymph Node In Situ
(Sentinel Lymph Node)
37
-
1
Introduction
-
2
INTRODUCTION
In recent years breast cancer treatment has gradually shifted from aggressive
surgical treatment to minimally invasive surgical procedures. The introduction of
mass screening programs resulted in the earlier detection of breast cancers, which
has brought about a change in stage distribution. These smaller breast lesions made
room for less aggressive treatment options. Besides this rearrangement in stage
distribution, the addition of neo-adjuvant and adjuvant chemotherapy, radiotherapy
made less invasive treatment possible1. An excellent example of this shift in
treatment is the sentinel node technique as an alternative for ALND for staging in
breast cancer.
In the early 1900's Halsted proposed the hypothesis of stepwise dissemination
in breast cancer2.He devised a theory that metastases would initially remain
localized in the lower axilla and would then go higher up the chain towards the
subclavicular and supraclavicular basins. In accordance with Halsted's concept,
breast cancer was treated with radical mastectomy, in which the breast, axillary
lymph nodes and the pectoral muscle were dissected. This was followed by the
supra-radical mastectomy, whereby, in addition to the axillary lymph nodes, the
internal mammary nodes were removed. In 1948 Patey introduced the modified
radical mastectomy in which the pectoral muscle was spared. In 1981 breast
conserving treatment was advocated by Veronesi. All along, axillary lymph node
dissection remained an essential part of the treatment: for staging, local regional
control and an indicator of the need for adjuvant therapy. In 30% to 40% of patients
with curable breast cancer metastases in the axilla are found. Axillary clearance in
this group provides regional tumour control. However, the morbidity of ALND is
considerable: high percentages of chronic lymphedema (6-56%), pain (16-55%),
-
3
sensibility disorders (58-81%) and dysfunction of the shoulder and arm (14-32%)
are reported3. In patients with a tumour negative axilla, who make up 60-70% of all
patients, lymph node dissection has no additional value. With SLNB it is now
possible to offer this group of patients an accurate staging without the morbidity of
axillary clearance.
SLNB is based on the theory of stepwise dissemination. A node that receives
lymph fluid directly from a tumour is most likely also the node that will be the first
to contain metastatic disease if lymphatic dissemination occurs. This particular
(first) node can be visualized with the aid of a radioactive tracer and blue dye and
can then be harvested. Dependent on the tumor-status of the sentinel node, axillary
lymph node dissection is performed. The sentinel node procedure thus serves two
purposes. Firstly, to identify patients who do not have metastases in the axilla and
can be spared axillary clearance. Secondly, to improve the accuracy of staging .Not
only nodes in the axilla are evaluated, but also nodes that are located in the internal
mammary chain or elsewhere. These nodes can be harvested and appropriate
treatment instituted if they are shown to be involved. Furthermore, a more thorough
evaluation of the lymph nodes is possible without spending more time as only one
or a few nodes are removed with sentinel node biopsy.
The pathologist used to receive a complete lymph node dissection specimen
from each breast cancer patient that usually contained ten or more lymph nodes.
Each of these nodes had to be evaluated and a relatively crude work-up of the
specimen was performed. With the current meticulous pathological evaluation of
sentinel lymph nodes, even smaller metastases (micro metastasis) are identified
although their clinical relevance is subject of debate.
-
4
Objectives
-
5
OBJECTIVES OF THE STUDY
To assess the efficacy of sentinel lymph node biopsy in detecting axillary metastasis
in cases of node negative early breast cancer
-
6
Review of Literature
-
7
REVIEW OF LITERATURE
HISTORICAL ASPECTS
Bartholin first described the existence of a ‘lymphatic’ in 1653. Virchow, in the
nineteenth century, formulated the theory that lymph nodes filter particulate matter
from lymph. This important assumption led to the awareness that cancer could be
cured at an early stage with adequate surgery. The next step in the evolution of
Virchow’s theory was the introduction of the radical mastectomy by Halsted at the
end of the nineteenth century2.
To determine the barrier function of lymph nodes, several investigators injected
inanimate particles or tumour cells into certain afferent lymphatics in animal
models. Studying mesenteries of dogs and rabbits, Gilchrist saw no passage of
carbon suspensions through any node after injections with varying pressures 4.
Zeidman and Buss injected stained V2 carcinoma cells into the afferent lymphatics
of popliteal nodes in rabbits 5. They found that tumour cell emboli are immediately
trapped in the subcapsular sinus and do not spread to the next node for at least 3
weeks. However Fisher and Fisher found that less than 40% of 51Cr-labelled V2
carcinoma cells were retained in a rabbit’s popliteal node6. Subsequently nodal
involvement was suggested not to be an orderly contiguous extension, but rather a
marker of distant disease7.
The spectrum hypothesis was found to be most consistent with clinical
observations. Hellman thought breast cancer as a spectrum of disease with increased
inclination towards metastasis as a function of tumour growth and progression7. A
lymph node metastasis may either be the only site of dissemination, especially in
small tumours, or can be a marker of distant disease. The observation that many
cancer patients are cured after adequate loco regional treatment made the spectrum
-
8
theory attractive. The introduction of the sentinel node concept was an attempt to
clarify the controversy caused by the spectrum hypotheses. The sentinel node
concept is actually based on the Halsted theory that stressed the importance of loco
regional cancer treatment because of the step-wise spread. The spectrum and
systemic hypotheses, however, suggest that lymph node involvement can be an
indicator of distant disease and therefore sentinel node biopsy is also a staging tool
to select patients for adjuvant systemic treatment.
The concept of sentinel node biopsy is based on two basic principles: the
existence of an orderly and predictable pattern of lymphatic drainage to a regional
lymph node basin, and the functioning of a first lymph node as an effective filter for
tumour cells. With the widespread use of sentinel node biopsy, sufficient data was
provided to prove that sequential lymphatic dissemination and entrapment of tumour
cells in first draining lymph nodes occur8,9
. The description of "sentinel node" first
appeared in the literature in 1960. A normal-appearing node at the junction of the
anterior and posterior facial vein was sent for frozen section investigation during a
total parotidectomy in 1951. In the description of Gould, the pathology report was
‘lymph node with metastatic tumour’10
. Intraoperative examination of this lymph
node in its typical anatomical location guided the decision to perform a radical neck
dissection during the following parotidectomies.
Two decades later, Cabañas observed the existence of a sentinel node in the
lymphatic drainage of the penis11
. Lymphangiographic studies elucidated the precise
location of such sentinel nodes. Direct drainage from the penis to the lymph nodes
associated with the superficial epigastric vein was observed. He reported that the
lymphatic system of the penis drains to one lymph node (or a group of nodes), ‘the
sentinel lymph node’, which is the dominant site of tumour spread from penile
-
9
carcinoma. Patients with a tumour-positive sentinel lymph node underwent
subsequent inguinal lymph node dissection.
Studying lymphatic drainage of testicular cancer also revealed the existence of
a sentinel node. Chiappa et al postulated primary testicular lymph centres using
lymphangiographic studies12
. Weissbach and Boedefeld examined the feasibility of
a limited retroperitoneal lymph node dissection, based on their observations of areas
in which solitary metastases occur. Lymph nodes in these areas were called
sentinels13
. Weissbach and Boedefeld stated that ‘a more limited approach strictly
for the purpose of pathological staging, which aims at the prevention of long-term
damage without compromising diagnostic accuracy, must be based on the
knowledge of the pathways of lymphatic dissemination and, particularly, on the first
sites of nodal involvement’
Kett et al administered contrast medium in breast lymphatics that were
visualised with the aid of areolar blue dye injection14
. They observed flow to an
isolated lymph node, called the ‘Sorgius’ node, and subsequent drainage through
many lymphatic vessels and lymph nodes to the collecting system around the
axillary vein. Using breast lymphoscintigraphy in 1980, Christensen et al observed
‘primary draining nodes’15
. Haagensen studied the route of metastases through the
axillary lymph node filter and stated that the nodes of the central group are not only
most often involved, but also most often exclusively involved16
. An interesting
finding is that he used the term sentinel node for specific lymph nodes of the inferior
deep cervical group because of their close relationship to the jugular–subclavian
venous confluence.
Morton transferred this concept of sentinel lymph node to melanoma patients
for staging in 199217
.He localised sentinel lymph node by visualisation of lymphatic
-
10
duct leading to the sentinel lymph node with blue dye (isosulfan blue) at the
operating theatre. Patent blue dye was injected intradermally around the biopsy site
of a primary melanoma and 10-20 min later, a skin incision was made in the
regional lymph drainage region. Blue stained lymphatic vessels and blue stained
nodes could be traced during this operation.
In 1993, Alex and Krag introduced the use of a radioactive tracer 99m
Technetium sulphur colloid, injected intradermally around a primary melanoma site,
followed by imaging and subsequent intraoperative use of a gamma probe to
localize and extirpate the sentinel lymph node. In addition, they compared gamma-
probe-guided localization to vital blue dye mapping in an animal model18
.
In same year Krag described the sentinel node biopsy technique in breast
cancer19
. He injected a radioactive tracer around the tumour. The sentinel lymph
node was localized during surgery by measuring the radioactivity with a gamma
probe.
Based on the intradermal injection technique used by Morton for melanomas,
Giuliano et al introduced a peritumoural injection technique with blue dye17,20,21,22
and concluded that intra operative lymphatic mapping can accurately identify the
sentinel node in some patients and multiple sectioning with immune-histochemical
staining of sentinel nodes can increase the accuracy of axillary staging in breast
cancer and can identify significantly more patients with lymph nodes metastases,
especially micrometastases, than can ALND with routine histopathologic processing
of lymph nodes.
Intra-operative lymphatic mapping using a combination of a vital blue dye and
filtered technetium-labelled sulphur colloid was done by Albertini et al 21
. The SLN
-
11
was identified and removed, followed by a definitive cancer operation, including a
complete axillary node dissection. They confirmed that lymphatic mapping was
technically possible in the patient with breast cancer and that the histologic
characteristics of the SLN probably reflected the histologic characteristics of the rest
of the axillary lymph nodes.
Borgstein et al postulated that both the mammary gland and overlying skin
share a common lympathic pathway to the same axillary sentinel node. They tested
this with intradermal injection of blue dye and comparing it with intramammary
injection of radioactive colloid in patients with clinical stage T1-T2, N0 invasive
breast cancer. They confirmed that the lymphatics of the overlying skin drain to the
same axillary sentinel node as the underlying glandular breast tissue23
. This
simplified the sentinel lymph node technique by showing that the intracutaneous
blue dye injection identified the same axillary lymph nodes as the peritumoral
radioactive tracer injection. Later, they concluded that periareolar blue dye injection
could be ideally suited to identify the principal (axillary) metastasis route in early
breast cancer and that intradermal injection improves the efficacy of blue dye,
because transport by skin lymphatics is more rapid and reliable than in the breast
parenchyma24.
Sentinel node biopsy has evolved rapidly as an alternative to extensive axillary
clearance for staging breast cancer. Many centres across world have stopped
performing axillary clearance if sentinel node is found to be negative. In initial
sentinel node procedures in 34 breast cancer patients, Giuliano reported that tumour
was found in 39 of 63 sentinel nodes (62%) compared with 93 of 688 non-sentinel
nodes (14%). He stated that ‘this suggests that a primary breast carcinoma spreads
to the axilla along a specific pathway of lymph nodes that cannot be identified by
-
12
random axillary sampling’25
. But whether absence of tumour cells in the sentinel
node indicated absence of tumour cells in the other lymph nodes of the regional
basin, i.e. false negative rate, remained a major concern. Morton et al found, in the
first 194 lymphadenectomy specimens that had an identifiable sentinel node, non-
sentinel nodes were the sole site of melanoma metastasis in only two patients17
. The
sentinel node was involved with tumour in 38 patients, resulting in a false negative
rate of 5% (2/40). This result showed a high degree of accuracy in identifying early-
stage melanoma patients with clinically occult lymph node metastases and
suggested that the concept is valid. With extensive pathological examination of
sentinel nodes and non-sentinel nodes in breast cancer, Turner et al described that, if
the sentinel node is tumour free, the probability of involvement of a non-sentinel
node is 1 in 1087 26
.
Numerous studies in melanoma and breast cancer patients have confirmed that
the sentinel node is the first node reached by metastasising cells as they enter the
regional lymphatic basin in the vast majority of patients. A review of sentinel node
biopsy in breast cancer reported an accuracy of more than 95% in all studies27
. A
wide range of false negative rates among different centres does, however, exist.
Unacceptable failure rates can occur because of technique, physician and patient
related factors. The first observational study of sentinel node biopsy not followed by
routine axillary lymph node dissection in 133 breast cancer patients showed no
axillary recurrences after a median follow-up of 39 months28
.
Numerous studies were done to standardize the technique of sentinel lymph
node biopsy including site of injection and to determine efficacy of dye alone
method over inclusion of radiocolloid for the purpose of sentinel node identification.
Different methods of SLN biopsy reported in the literature included the use of
-
13
various forms of radioisotopes, blue dye, both blue dye and radioisotopes, and
injection of the material either into the breast parenchyma, subdermally, or
intradermally. Problems have been reported with each of these various methods. The
dye injection technique has been reported to have a steep learning curve as
demonstrated by Giuliano’s original reports of identification rates of only 66%
increasing to 93% in 3 years and later to 100% 21,22,25
. A meta analysis of SLN
biopsy in breast cancer encompassing 11 different studies showed a false-negative
rate of 7% and an identification rate of only 74% for the blue dye method alone 29
.
Better results seem to have been obtained when both blue dye and radioactive
tracers were used 29,30
.
“It is drainage of the breast not the location of the tumor that is of primary
importance in lymphatic metastases.” Based on this hypothesis, along with the
anatomic work completed by other investigators during the 1950s and 1960s
demonstrating the importance of a subareolar lymphatic plexus in the lymphatic
drainage of the breast; studies using vital blue dye staining and radiographic
techniques showing communication of subareolar plexus with the other
parenchymal lymphatics of the breast before terminating in the regional lymph
nodes, Smith et al31
conducted a study to test the hypothesis that subareolar
injection of Tc is as accurate as peritumoral injection in localizing the SLN
determined by completion ALND. Their results after injecting tracing material into
the subareolar tissue showed subareolar injection to be as accurate if not more, than
most other studies evaluating peritumoral injection of either blue dye or radioactive
colloid. Even when performed with both filtered and unfiltered Tc by several
different injectors they found this technique to be easy and reliable. Subareolar
injection also avoided the problem of shine through in lesions close to either the
-
14
axilla or mediastinal nodal basins. With subareolar injection as performed by them,
an internal mammary lymph node could be removed if this was found to be the hot
node. Their study and those conducted by Klimberg et al32
and Kern33
showed great
efficiency and accuracy for subareolar injection. Also, no image-guidance for the
injection in non palpable lesions is required since the site is always subareolar. This
may help to improve efficiency and decrease costs, especially with the increasing
diagnosis of occult cancers. Subareolar injection may prove to have particular
application in nonpalpable lesions, upper outer quadrant lesions, multifocality, and
internal mammary sentinel lymph nodes.
SLNB with blue dye for evaluation of the axilla has been found to be a rapid
and accurate technique that provides increased efficacy in the detection of lymphatic
metastasis when careful pathologic evaluation with serial sectioning is performed.
The risk-benefit analysis of lymphatic mapping with blue dye provides
improvement in staging, with reduced morbidity and hospital stay.
ANATOMICAL ASPECTS
The breasts consist of mammary glands and associated skin and connective
tissues. The mammary glands are modified sweat glands in the superficial fascia
anterior to the pectoral muscles and the anterior thoracic wall. The base, or attached
surface, of each breast extends vertically from ribs II to VI, and transversely from
the lateral border of sternum to as far laterally as the mid-axillary line. The upper
lateral region of the breast can project around the lateral margin of the pectoralis
major muscle and into the axilla. This axillary process (axillary tail) may perforate
deep fascia and extend as far superiorly as the apex of the axilla.
-
15
The mammary glands consist of a series of ducts and associated secretory
lobules. These converge to form 15 to 20 lactiferous ducts, which open
independently onto the nipple. Each duct has a dilated portion, the lactiferous sinus,
in which a small droplet of milk accumulates or remains in the nursing mother. The
nipple is surrounded by a circular pigmented area of skin termed the areola. The
areola contains numerous sebaceous glands, which enlarge during pregnancy and
secrete an oily substance that provides a protective lubricant for the areola and
nipple. The nipples are conical or cylindrical prominences in the centre of the
areola. The nipples have no fat, hair, or sweat glands. The tips of the nipples are
fissured with the lactiferous ducts opening into them. The nipples are composed
mostly of circularly arranged smooth muscle fibres that compress the lactiferous
ducts during lactation and erect the nipples in response to stimulation, as when a
baby begins to suckle.
A well-developed, connective tissue stroma surrounds the ducts and lobules of the
mammary gland. In certain regions, this condenses to form well-defined ligaments, the
suspensory ligaments of breast, which are continuous with the dermis of the skin and
support the breast. The breast lies on deep fascia related to the pectoralis major, serratus
anterior and the aponeurosis of external oblique muscle. The deep pectoral fascia
envelops the pectoralis major muscle and is continuous with the deep abdominal fascia
below. It attaches to the sternum medially and to the clavicle and axillary fascia above
and laterally. Along the lateral border of the pectoralis major muscle, the anterior lamina
of the deep pectoral fascia unites with the fascia of the pectoralis minor muscle and,
more inferiorly, with the fascia of the serratus anterior. A posterior extension of this
fascia is continuous with the fascia of the latissimus dorsi and forms the suspensory
ligament of the axilla. A layer of loose connective tissue (the retromammary space)
-
16
separates the breast from the deep fascia and provides some degree of movement over
underlying structures. For the anatomical location and description of tumors and cysts,
the surface of the breast is divided into four quadrants (fig. 1). The upper outer quadrant
of the breast contains a greater volume of tissue than do the other quadrants.
-
17
Fig. 1 Quadrants of breast
-
18
BLOOD SUPPLY
The breast receives its principal arterial blood supply from -
(a) perforating branches of the internal thoracic (or internal mammary) artery, a
branch of the subclavian artery; it courses parallel with the lateral border of the
sternum behind the transversus thoracis muscles. From the internal thoracic artery,
perforating branches pass through the intercostal muscles of the first six interspaces
and the pectoralis major muscle to supply the medial half of the breast and
surrounding skin. Typically these arteries descend laterally toward the nipple-
areolar complex so that most of the arterial supply arises above the level of the
nipple. Therefore, radial incisions in the upper half of the breast are less likely to
injure the major arterial supply than transverse incisions. The inferior parts of the
breast below the level of the nipple are almost free of major vessels.
(b) lateral branches of the posterior intercostal arteries; and
(c) branches from the axillary artery, including the highest thoracic, lateral thoracic,
pectoral branches of the thoracoacromial artery and unnamed mammary branches.
The lateral thoracic artery is the most important of these vessels.
The second, third, and fourth anterior intercostal perforators and branches of the
internal mammary artery arborize in the breast as the medial mammary arteries.
The veins of the breast and chest wall follow the course of the arteries, with
venous drainage being toward the axilla. The three principal groups of veins are -
-
19
(a) perforating branches of the internal thoracic vein - The perforating tributaries
from the medial half of the breast carry the greater part of the venous drainage. They
enter the internal thoracic vein, which joins the brachiocephalic vein.
(b) perforating branches of the posterior intercostal veins, and
(c) tributaries of the axillary vein.
Batson's vertebral venous plexus, which invests the vertebrae and extends from
the base of the skull to the sacrum, may provide a route for breast cancer metastases
to the vertebrae, skull, pelvic bones, and central nervous system.
NERVE SUPPLY
Lateral cutaneous branches of the third through sixth intercostal nerves provide
sensory innervation of the breast (lateral mammary branches) and of the
anterolateral chest wall. Cutaneous branches that arise from the cervical plexus,
specifically the anterior branches of the supraclavicular nerve, supply a limited area
of skin over the upper portion of the breast. The intercostobrachial nerve is the
lateral cutaneous branch of the second intercostal nerve and may be visualized
during surgical dissection of the axilla. Resection of the intercostobrachial nerve
causes loss of sensation over the medial aspect of the upper arm.
-
20
Figure 2. Vasculature of breast. A. The mammary gland is supplied
from its medial aspect mainly by perforating branches of the
internal thoracic artery and by several branches of the axillary
artery (principally the lateral thoracic artery) superiorly and
laterally. B. The breast is supplied deeply by branches arising from
the intercostal arteries. C. Venous drainage is to the axillary
(mainly) and internal thoracic veins.
-
21
LYMPHATIC DRAINAGE
The lymphatic flow of the breast is of great clinical significance because
metastatic dissemination occurs principally by the lymphatic routes. The dominant
lymphatic drainage of the breast is derived from the dermal network. The breast
lymphatics branch extensively and do not contain valves: lymphatic blockage
through tumour occlusion may therefore result in reverse blood flow through the
lymphatic channels.
The direction of lymphatic flow within the breast parallels the major venous
tributaries and enters the regional lymph nodes via the extensive periductal and
perilobular network of lymphatic channels. Lymph passes from the nipple, areola,
and lobules of the gland to the subareolar lymphatic plexus. From this plexus most
lymph (> 75%), especially from the lateral breast quadrants, drains to the axillary
lymph nodes, initially to the anterior or pectoral nodes for the most part. However,
some lymph may drain directly to other axillary nodes or even to interpectoral,
deltopectoral, supraclavicular, or inferior deep cervical nodes.
Axillary nodes are 20–40 nodes, grouped artificially as pectoral (anterior),
subscapular (posterior), central and apical. Surgically, the nodes are described in
relation to pectoralis minor. Those lying below pectoralis minor are the low nodes
(level 1), those behind the muscle are the middle group (level 2), while the nodes
between the upper border of pectoralis minor and the lower border of the clavicle
are the upper or apical nodes (level 3).There are six axillary lymph node groups
recognized by surgeons (a) the axillary vein group (lateral), which consists of four
-
22
to six lymph nodes that lie medial or posterior to the vein and receive most of the
lymph drainage from the upper extremity; (b) the external mammary group (anterior
or pectoral group), which consists of five or six lymph nodes that lie along the lower
border of the pectoralis minor muscle contiguous with the lateral thoracic vessels
and receive most of the lymph drainage from the lateral aspect of the breast; (c) the
scapular group (posterior or subscapular), which consists of five to seven lymph
nodes that lie along the posterior wall of the axilla at the lateral border of the
scapula contiguous with the subscapular vessels and receive lymph drainage
principally from the lower posterior neck, the posterior trunk, and the posterior
shoulder; (d) the central group, which consists of three or four sets of lymph nodes
that are embedded in the fat of the axilla lying immediately posterior to the
pectoralis minor muscle and receive lymph drainage both from the axillary vein,
external mammary, and scapular groups of lymph nodes, and directly from the
breast; (e) the subclavicular group (apical), which consists of six to twelve sets of
lymph nodes that lie posterior and superior to the upper border of the pectoralis
minor muscle and receive lymph drainage from all of the other groups of axillary
lymph nodes; and (f) the interpectoral group (Rotter's nodes), which consists of one
to four lymph nodes that are interposed between the pectoralis major and pectoralis
minor muscles and receive lymph drainage directly from the breast. The lymph fluid
that passes through the interpectoral group of lymph nodes passes directly into the
central and subclavicular groups.
Lymph from the axillary nodes drains into clavicular (infraclavicular and
supraclavicular) lymph nodes and from them into the subclavian lymphatic trunk,
which also drains lymph from the upper limb. Efferent vessels directly from the
-
23
breast pass round the anterior axillary border through the axillary fascia to the
pectoral lymph nodes; some may pass directly to the subscapular nodes. A few
vessels pass from the superior part of the breast to the apical axillary nodes,
sometimes interrupted by the infraclavicular nodes or by small, inconstant,
interpectoral nodes. Lymphatic vessels occasionally follow lateral cutaneous
branches of the posterior intercostal arteries to the intercostal nodes.
Lymph from the skin of the breast, except the nipple and areola, drains into the
ipsilateral axillary, inferior deep cervical, and infraclavicular lymph nodes and also
into the parasternal lymph nodes of both sides. Dermal lymphatics penetrate
pectoralis major to join channels that drain the deeper parenchymal tissues, and then
follow the vascular channels to terminate in the subclavicular lymph nodes. Part of
the medial side of the breast drains towards the internal thoracic group of lymph
nodes whereas lymph from the inferior quadrants may pass deeply to abdominal
lymph nodes (subdiaphragmatic inferior phrenic lymph nodes). The internal thoracic
chain may drain inferiorly via the superior and inferior epigastric lymphatic routes
to the groin. Connecting lymphatics across the midline may provide access of
lymphatic flow to the opposite axilla. Lymph from the parasternal nodes enters the
bronchomediastinal lymphatic trunk, which also drains lymph from the thoracic
viscera. The termination of these lymphatic trunks varies; traditionally, these trunks
are described as merging with each other and with the jugular lymphatic trunk,
draining the head and neck to form a short right lymphatic duct on the right side or
entering the termination at the thoracic duct on the left side. However, in many
cases, the trunks open independently into the junction of the internal jugular and
subclavian vein, the venous angle, to form the brachiocephalic veins. In some cases,
-
24
they open into both of these veins. [34,35,36]
The mammary gland is embryologically derived from the ectoderm and eventually
develops entirely within the superficial fascia of the skin. The circumareolar
lymphatic plexus on the external surface of the gland anastomoses with the
superficial cutaneous lymph network of the overlying skin.
The breast functions as a single biologic unit, and the preferential lymph
drainage pathway from all quadrants is essentially toward the same axillary
(sentinel) lymph nodes. Parenchymal lymph vessels accompany the lactiferous ducts
centripetally to empty into the dense subareolar plexus of Sappey, where pooling of
lymph from all parts of the breast occurs. Generally, two enormous lymph trunks
(vasa lymphatica mammaria magna) leave the areolar region to course superficially
toward the lower axillary lymph nodes.
Contrary to the widely accepted opinions the subareolar plexus does hold a key
position in conveying lymph produced by the whole mammary gland toward the
first lymph node filter of the axilla. This unique arrangement of the breast lymphatic
system, provides an adequate transport system capable of accommodating the
dramatic surges of lymph flow occurring during lactation to preserve the
physiologic balance. Logically, this will also be the preferential initial route for
disseminating cancer cells, originating from any site in the breast, because these
tumor emboli are passively carried along the direction of the prevailing lymph flow.
Studies have repeatedly shown that the breast cannot be divided into functionally
separate segments. This explains why previous excision biopsy may merely reduce
the detection rate, but will not necessarily affect the accuracy of SN biopsy—that is,
-
25
unless prior (upper outer quadrant) excision has severed both main lymph trunks.
The most important of all the accessory routes is the internal mammary pathway.
However, it is rare to find internal mammary node metastases in the absence of
axillary involvement. In the past, much emphasis has been placed on a variety of
alternative lymphatic pathways, but these accessory pathways however, assume
clinical importance once the main axillary drainage route has become obstructed.24
-
26
Fig 3. Lymphatic Draining of breast parenchyma into axillary
lymph node & further spread
-
27
Fig.4 Lymphatic drainage of breast- A. The lymph nodes in the region are
shown. B. The red arrows indicate lymph flow from the right breast. Most
lymph, especially that from the superior lateral quadrant and center of the
breast, drains to the axillary lymph nodes, which, in turn, are drained by the
subclavian lymphatic trunk and then into the venous system via the right
lymphatic duct. C. Most lymph from the left breast returns to the venous
system via the thoracic duct, which enters the left venous angle.
-
28
EARLY BREAST CANCER & SENTINEL LYMPH NODE BIOPSY
Early-stage tumors comprise those that are neither fixed to the chest wall nor
inflammatory. Stage I breast cancer includes primary malignancies that are 2 cm in
greatest dimension and do not involve the lymph nodes and micro invasive tumors
that are 0.1 cm in greatest dimension. Stage II breast cancer encompasses primary
tumors of 2 to 5 cm that can involve ipsilateral axillary lymph nodes and tumors >5
cm without lymph node involvement37
.
Determination of axillary nodal involvement is an integral part of management
for patients with early stage breast cancer because axillary nodal status is the most
important prognostic factor in this patient cohort. Complete ALND has been
accepted as the gold standard for axillary staging38
. This is because of the axillary
staging accuracy associated with ALND: a less than 2% false-negative rate 39-41
. But
the ability to achieve this level of accuracy is at the expense of considerable
morbidity with this procedure; there is an acute complication rate of 20% to 30%
and a chronic lymphedema rate as high as 6% to 56% 3.
Because only about one third of patients with a clinically negative axilla have
nodal metastases on histopathologic examination of the ALND specimen, routine
ALND places a substantial number of patients at risk for operative morbidity
without any known benefit from the operative procedure. There is a need for a less
morbid and equally accurate method of assessing axillary nodal status. Untill
recently, assessment of axillary status using less invasive techniques has not
achieved adequate clinical applicability. Assessment of axillary involvement with
various radiographic methods (eg, mammography, computed tomography, and
positron emission tomography) is also associated with an equally unacceptable
-
29
false-negative rate 42-44
. Limiting the extent of axillary dissection, thereby decreasing
the complication rate, is not a comparable surgical alternative to ALND; there is a
40% false negative rate with random axillary nodal sampling and a 10% to 15%
false-negative rate with excision of level I nodes alone 45
.
The introduction of SLNB in breast cancer patients provides a less invasive but
equally accurate alternative of axillary assessment to ALND. Over the years SLNB
for breast cancer has become an accepted standard of care in many centers due to its
accurate prediction of axillary lymph node status that may safely avoid extensive
dissection of the regional lymph node basin 46,47,48.
TECHNIQUE AND PATIENT SELECTION
The materials used and the technique of SLNB have rapidly evolved over the
last decade. Some centers rely on injection of blue dye alone, some use radioisotope
alone, while most claim better success with a combination of both. Site of injection
has also been an area of extensive research, with variable success rates reported with
peritumoral, intra-dermal, subcutaneous, and sub-areolar or central injections.
Currently the gold standard and most widely published lymphatic mapping
technique is dual peritumoral injection 46
.
Although SLN dissection as a stand-alone procedure for axillary staging for
breast cancer is becoming more common, there are still differences of opinion
regarding the correct method for mapping and the number of sentinel nodes to
remove for accurate staging of axilla. Risks of dissecting so many SLNs as to equal
that of a complete axillary lymph node dissection against the risk of missing a
pathologically positive node has to be weighed for adequate SLNB.
Among various aspects of SLNB, technique-dye alone, radioactive tracer or
both; site of injection-with peritumoral, intra-dermal, subcutaneous, and sub-areolar
-
30
or central; patient selection and finally method for pathological examination of SLN
along with number of nodes to determine adequacy of SLNB assume main
importance for successful use of this technique in routine.
For those wishing to start a SLNB program, there are several guiding
principles. First, SLN biopsy requires close collaboration among the disciplines of
nuclear medicine, surgery, and pathology. Second, SLNB should be done according
to a well-defined and consistently applied protocol. Early on, SLNB should be
validated by a backup ALND to allow an audit of both the success rate (which
should exceed 90%) and the false-negative rate (which should not exceed 5% to
10%). There is a learning curve for SLNB, but it remains unclear how many backup
ALNDs are required before one can perform SLNB on one’s own. Convincing data
from the Axillary Lymphatic Mapping Against Nodal Axillary Clearance
(ALMANAC) trial show that for experienced surgeons working within a well-
defined protocol, most failed and/or false-negative procedures occur within a
surgeon’s first few cases 49
.
SLNs have been identified using blue dye, radio-isotopes or a combination of
both. Cox et al reported a SLN identification rate of 80% with blue dye, 89% with
radio-isotope and 96% using a combination of both. Cody et al reported a similar
identification rate – 81% with blue dye, 87% with radio-isotope and 95% with
combined technique. Similar results were published in a multicentre study
conducted by Japanese Breast Cancer Society, identifying SLN in 94% cases using
combination technique in comparison to a low of 74% using blue dye alone.
However in a RCT conducted by Morrow et al, no significant difference in two
techniques (88% with dye alone, 86% with combined technique) was reported50
.
Even though their reported rate of SLN identification with combined technique was
-
31
lower than that reported by Cox or Cody they concluded that there was no
advantage in using dye plus radio-isotope.
Currently, however blue dye and radio-isotope technique are considered
complimentary and a higher SLN identification rate is seen when two techniques are
used together. Various sites for injection of dye or radio-isotope for SLN
identification have been described in the literature. These are either superficial
(intra-dermal, sub-dermal and sub-areolar) or deep (intra-tumoral and peri-
tumoral).There is, however no worldwide consensus on either the choice of the dye
used, the plane or site of the injection.
Since the goal of SLNB is to identify the node draining directly from tumor it
is logical to inject the tracer material into the tumor, however there is a potential risk
of seeding the needle tract with tumor cells. SLNB has also been performed by
injecting the tracer into the parenchyma of breast around the tumor. However, this is
associated with technical problem of inconsistent pre-operative or intra-operative
SLN identification because of ‘shine effect’ especially in the upper outer quadrant
tumor.
To optimize SLN identification, sub-dermal or intra-dermal approach was
proposed. This was based on the assumption that skin overlying the breast
parenchyma has the same embryological origin as the underlying tissue and so it
will have the same lymphatic pattern. This was confirmed in various studies23,50,51
.
The sub-areolar approach is based on studies indicating that this area provides a
central access route to peripheral lymphatic pathways32,33
. These studies indicated
that there are clear advantages to subareolar injection for SLN localization like
avoidance of need for image guided injection in non palpable lesions, no
-
32
overlapping of diffusion zone in upper outer quadrant lesions with that of SLN in
axilla and in medial lesions with internal mammary lymph nodes.
A combined use of sub-dermal injection over the primary tumor and sub-
areolar injection are becoming increasingly popular technique. However, it is
important to realize that intra-dermal and subdermal injections can help visualize the
superficial lymphatics running towards axilla but they do not trace the deep
lymphatics running to internal mammary, inter-pectoral or intra-mammary nodes.
For a more accurate SLN identification a combination of peri-tumoral and sub-
dermal / intra-dermal / sub-areolar injection may be used. If internal mammary,
inter-pectoral or intra-mammary nodes are to be targeted a peri-tumoral injection of
radio-isotope along with intra-dermal para-areolar blue dye injection may be used
whereas if these nodes are not targeted peri-tumoral blue dye injection with either
sub-dermal or sub-areolar injection of radio-isotope may suffice 50
.
Selection of appropriate patients is the first step to successful and rational
application of SLNB in breast cancer management. Ideal SLNB patients are those
with low probability of harbouring axillary metastases, but in whom the presence of
axillary nodal involvement would change adjuvant systemic therapy, i.e. patients
with small primary tumors. At present the selection of patients for sentinel node
biopsy is commonly based on size or grade of the primary tumour. The size of
primary tumour, grade of primary tumour, age of the patient, quadrant of the breast
and lympho-vascular invasion are all independent predictors of lymph node
involvement.
For T1a lesion node positivity rate is 15% compared to 67% in T2 lesions over
3 cm in size; T2 lesions the incidence of lymph node positivity is 41%, which
increases to 75% in T3 lesions. Grade I breast cancer is likely to have positive nodes
-
33
in 10% of patients, while 39% of patients with grade III tumours are likely to have
positive nodes 52
.
Other factors associated with lymph node positivity are quadrant of the breast
in which the tumour is situated and whether it is palpable. Thirty-three percent of
tumours situated in the upper outer quadrant of breast are node positive compared
with 21% for upper inner quadrant tumours 52
. Axillary nodal metastasis occurs less
frequently in impalpable tumours. This may be due to the fact that the deep tumours
are more likely to be impalpable and drain to the lymphatics on the surface of the
pectoral fascia leading to internal mammary nodes.
Breast cancers showing lymphovascular invasion on microscopy have a 57%
chance of being node positive compared with 23% for tumours without
lymphovascular invasion52
. Younger age is associated with increased incidence of
axillary nodal metastases. In women under 35 years of age or younger, even in T1
lesions 28% of patients have nodal metastases and overall node positivity in women
under 35 years of age is 59%. For T1a tumour node positivity rate in women under
50 years of age is 43% compared with 4% in women between 51 and 70 years of
age. Women under 50 years of age carry a 40% risk of developing node positive
breast cancer compared with 31% in women 51-70 years of age. Breast cancer
patients over 70 years of age have a 23% risk of node positivity52
.
Currently patients are often offered minimally invasive axillary surgery based
on size and possibly grade of tumour. Adding patient and tumour based factors can
refine the criterion for selection of patients for axillary surgery. Selection of patients
based on clinic-pathological variables may reliably predict patients with likelihood
of (sentinel and non-sentinel) lymph node positivity like patients with large tumors
(>5 cm) are not good candidates for SLNB because lymphatic drainage may be to
-
34
multiple nodes ,patients with previous axillary surgery may have distorted lymphatic
drainage from the primary tumor such that SLNB may not be successful, patients
with large biopsy cavities (>6 cm) may not have an accurate SNB result because
lymphatic drainage from the surrounding breast tissue may not be the same as that
from the primary tumor. This practise can assist patients to make informed decision
regarding the relative benefits of sentinel node biopsy or axillary clearance thus
minimising the need for a second operation and avoiding delay for oncological
treatment.
SLNB was designed as a minimally invasive technique that can accurately
stage the axilla while sparing the morbidity of a complete ALND. However, the
achievement of this objective rests on the ability to reliably assess the axilla with the
removal of a limited number of lymph nodes. The removal of more lymph nodes (as
in an ALND) does not improve survival and is associated with significantly greater
morbidity than the removal of few SLNs. Although this technique involves
removing the most radioactive nodes, the blue nodes, the nodes at the end of a blue
lymphatic channel, any nodes with radioactive counts greater than 10% of the
hottest node, and any palpably suspicious nodes, in general, an average of 2 SLNs
are removed. In some cases, however, significantly more SLNs are removed,
resulting in nearly a complete ALND.
In general, ALND involves the removal of 10 or more nodes. Some studies
have also suggested that the removal of fewer than 4 SLNs can accurately stage the
axilla, and, therefore, the removal of additional SLNs adds the morbidity of
removing more axillary lymph nodes without concomitant benefit. The removal of
more SLNs involves greater operative time; increased pathology cost; and although
it is imperative that all SLNs identified are removed.
-
35
Numerous studies have elucidated factors which may be affecting the number
of SLNs identified in breast cancer patients. Three factors (tumor palpability,
surgeon experience, and SLN biopsy technique) influence the ability to identify a
SLN. On average, palpable tumors are associated with having more SLNs identified
than non-palpable ones and surgeons with more experience with SLN biopsy (>10
cases) remove fewer SLNs than those with less experience. Non-palpable tumors
tend to be associated with the greatest failure rate in identifying a SLN, and, in these
patients, using a dual-injection technique (with blue dye and radiocolloid) is
recommended 53
.
Regarding optimal number of SLNs published data show that 97-98% of
positive SLNs are discovered in one of the first three nodes examined, and that it is
rare to find a positive SLN after identifying the first three nodes as negative 54-60
.
-
36
Fig. 5 Subareolar Injection Of Methylene Blue Dye
Fig. 6 Subareolar Injection Of Methylene Blue Dye
-
37
Fig. 7 Stained Lymphatics after Subareolar Injection of Methylene Blue
Fig. 8 Methylene Blue stained Lymph Node In Situ (Sentinel Lymph Node)
-
38
PATHOLOGICAL ASPECTS
Axillary SLNB produces an average of 1-3 nodes per axilla examined. Full
ALND usually produces 15-20 lymph nodes. With the smaller number of SLNs
requiring examination, the aim is to examine these more closely. The rationale of
this is to avoid under-staging the axilla and leaving metastatic disease in other,
higher echelon lymph nodes.
Intra-operative assessment- There are two main techniques, frozen section and
imprint cytology.
1) Frozen section: The frozen section technique has an advantage in that the
node is examined in a format familiar to most histo-pathologists. The false-negative
rate is 6–24% 51,61-63
.In Veronesi’s original series, the false-negative rate was 24%,
despite serial sectioning of the SLNs. The false negative rate is higher in nodes with
small-volume metastatic disease and in patients with small primary tumours. It can
be reduced by sectioning the node grossly at smaller intervals (1–1.5 mm) rather
than simply bisecting it, by cutting serial step sections and by using rapid
immunocytochemistry, which may reduce the false-negative rate61
.
Frozen section examination of the SLN also has disadvantages. Much tissue
can be lost in the cutting of serial sections, and if the diagnosis is found to be
lymphoma or infection (e.g. tuberculosis), vital diagnostic material may be lost. The
technique is extremely time consuming and requires special expertise. Operating
times are also increased, especially when multiple serial sections are used.
2) Imprint cytology is an alternative to frozen section or may be used in
conjunction with it. It has the advantages of potentially greater rapidity of reporting
and less tissue destruction, but is often seen as more demanding in its interpretation.
The false-negative rate varies widely between series at 5–66%, with a pooled false-
-
39
negative rate of 37% on meta-analysis 64,65
. Causes of false-negative findings are
low-volume nodal metastatic disease and invasive lobular carcinoma. Rapid
immunocytochemistry can improve the sensitivity.
False-positive findings are rare, but appear to be a greater problem for imprint
cytology than for frozen section. This results in unnecessary ALND.
Other methods: An alternative, or adjunct, to intraoperative assessment is
preoperative axillary imaging by ultrasonography in combination with fine-needle
aspiration cytology or core biopsy. Another possibility is removal of the SLN as a
primary procedure followed (at a later date) by surgery on the primary tumour, with
or without further axillary surgery as guided by the definitive SLN pathology report.
Postoperative assessment
According to UICC 66
disease within the axilla is defined as macro-
metastatic if more than 2mm in diameter, micro-metastatic if more than 0.2mm but
no more than 2mm in diameter, and ITCs if 0.2mm or less in greatest dimension .
ITCs are classified as node negative. It is evident that the more intensively the SLN
is examined, the more likely it is that small-volume metastatic disease will be found.
However, there is as yet no consensus on the best method of pathological
assessment of the SLN in breast cancer.
Different pathology protocols, ranging from examination of one H&E level
of each face of the SLN, to molecular analysis, multiple deeper levels and
immunocytochemistry with various cytokeratin antibodies are in practise. At the
most basic level, a single H&E section is examined. A mathematical model
analysing this approach suggests that, as long as levels are separated by no more
than 1 mm, all macro-metastases (i.e. >2 mm) will be identified and correctly
categorized in terms of metastasis size according to TNM 67
. If the SLN is sectioned
-
40
grossly at intervals of less than 2mm and all sections are embedded such that all
non-opposing faces are examined, a single, full-face H&E will identify all macro-
metastases (assuming that metastatic deposits are roughly spherical). If the
metastasis is less than 2mm in size (on initial H&E assessment), deeper levels
should be cut into this block, and adjacent blocks if appropriate, until the maximum
extent of the metastatic disease is accurately identified. Accurate identification of
most (but not all) micro-metastases would require sectioning of the entire SLN at
intervals of 200–250 mm 67
.
Use of immunocytochemistry can further increase the number of cases in
which metastatic disease is identified; such techniques lead to upstaging in 9–47%
of cases 68
. This results in a process of stage migration. Immunocytochemistry is
usually of little benefit in the detection of macro-metastases, but can identify more
cases of micro-metastasis and ITCs. In one retrospective study, all of the
‘undetected’ micro-metastatic disease in SLNs was visible on the original H&E
slides; only ITCs were revealed by immunocytochemistry 69
.The role of
immunocytochemistry is of limited value in the routine assessment of SLNs,
because the prognostic significance of ITCs is doubtful. The reporting of low-
volume metastatic disease in the SLN is subject to wide inter-observer variability.
Reverse transcriptase polymerase chain reaction analysis of genes expressed
by breast epithelial cells is potentially a highly sensitive method for identifying SLN
metastases70
. However, it does not permit quantification of metastatic disease, which
is of prognostic significance. In addition, it may give a positive result in patients
with benign nodal inclusions or in whom breast epithelial/tumour tissue has been
dislodged into the lymphatics by sampling procedures or tumour massage (so-called
-
41
‘benign mechanical transport’)71
. The significance of polymerase chain reaction-
positive nodes in the absence of a morphological correlate is unclear.
A further problem with the finding of ever smaller amounts of metastatic
disease within the axilla is the issue of stage migration. This involves the up-staging
of disease that would previously have been regarded as stage 1 (node negative) to
stage 2 (node positive). Stage migration results in an apparently better prognosis for
more advanced-stage disease, but in fact simply reflects a change in stage in a
patient who would previously have been treated for node-negative (stage 1) disease.
This leads to an apparent improvement in the outcome of patients with apparently
more advanced breast cancer, but may also result in over-treatment of patients with
low-volume metastatic disease. In summary, there are as yet no widely accepted
consensus guidelines on the best method of postoperative pathological SLN
assessment.
Recommendations for the pathological assessment of SLNB-
Macrometastatic disease must be identified by processing each SLN in its entirety. It
should be sectioned macroscopically into slices less than 2mm thick (preferably,
approximately 1 mm). All slices should be embedded, ensuring that all non-
opposing faces are examined completely. A single H&E slide should be prepared
from each block and examined. This technique ensures that all metastases greater
than 2mm in diameter are identified. If metastatic disease is present at a sub macro-
metastatic (
-
42
SLN and then proceed to a full ALND have shown that, if macro-metastatic disease
is identified in the SLN, there is a 50% risk of additional non-SLN involvement.
With SLN micro-metastatic disease, the risk declines to 20%, and for
metastases detectable only by immunocytochemistry the risk is approximately 9%
(this group inevitably contains a mixture of micrometastatic and ITC cases) 72-74
.
Immunocytochemistry may be particularly useful in lobular carcinoma, in which
tumour cells may be difficult to differentiate from lymphocytes or macrophages
morphologically.
SLNB - CLINICAL IMPLICATIONS AND CONTROVERSIES
SLNB has been one of the most exciting developments in the surgical
management of breast cancer since the advent of breast conserving surgery. A tumor
negative SLN virtually excludes lymphatic involvement of the entire regional
lymphatic basin, rendering ALND unnecessary in patients with node negative breast
cancer. It results in fewer ALND related complications, shorter hospital stay, cost
reduction, and a more accurate indication for treatment with adjuvant therapy.
With the spreading awareness regarding breast cancer and options available in
treatment modalities for early breast cancer SLNB has evolved rapidly and is being
used in routine at various cancer treatment centres. However, there are some issues
which still demand attention. These include-
1) clinical significance of micro-metastasis,
2) false negative SLNB;
3) relevance of internal mammary SLNB.
-
43
Clinical significance of micro-metastasis
AJCC defines micro-metastasis as metastatic foci less than 2 mm in diameter;
however, the arbitrary cut off point varies between 0.2 and 2 mm in various studies.
The detection rate of micro-metastases in axillary lymph nodes has been reported to
range from 9 to 46% 75,76.
Studies have used serial sectioning with or without immune-histo-chemical
stains for the detection of micro-metastatic foci and these methods do have a
definite impact on detection rates. Despite all this, the clinical significance of micro-
metastasis is yet to be determined.
Nodal micro-metastases appear to have a small but significant adverse effect
on distant recurrence and survival in some studies77
. It is imperative that the
prognostic significance of nodal micro-metastases be determined, as there are
important implications for systemic adjuvant chemotherapy and hormonal therapy.
The International (Ludwig) Breast Cancer Study78
, one of the largest micro-
metastases studies, showed that both disease free interval and overall survival were
significantly affected by the presence of micro-metastatic disease at 5 and 6 years of
follow up. The overall survival was 80% in the node negative group and 70% in the
node positive group76
. Rosen et al found that patients had poorer disease free
interval and overall survival at 10 years with nodal metastasis smaller than 2 mm.
However, this described a group with T1 tumours, whereas no survival disadvantage
as such was found in T2 cancer79
.
Present-day data of sentinel lymph node micro-metastases do not possess
sufficient follow-up to observe any survival effects as some retrospective studies
have shown, and therefore the prognostic significance of such occult metastasis at
this time is unknown. However, in 7th edition of the AJCC Staging Manual staging
-
44
of LNMM traditionally grouped with macro-metastasis (stage II and above), has
been down-staged to stage IB for small tumors, in order to ‘‘indicate the better
prognosis for the subset of breast cancer patients and to facilitate further
investigation.”
FALSE NEGATIVE SLNB
The false-negative rate is defined as the number of negative SLNs identified
within an axilla that is found to be positive on subsequent full examination of all the
axillary nodes, divided by the total number of positive axillae. In other words, false-
negative rate is the counterpart of the sensitivity, which is defined as the proportion
of node-positive patients (sentinel node–positive patients and patients with recurring
disease) that is identified by sentinel node biopsy.
Early experiences in SLNB showed false-negative rates ranging from 16% to
38%80
. Even in the interim analysis of the Multicenter Selective Lymphadenectomy
Trial I, the false-negative rate is 17.6% 81
.
The cause for such high false-negative rates are multiple and a reason for
concern. Testori et al. mention the nuclear medicine physician, the surgeon, and the
pathologist as sources of failure. Also the concept of sequential dissemination may
not always apply. We are dealing with a biological system with associated
variability. It is possible that tumor cells may pass through a sentinel node and lodge
in the next lymph node. Another cause may be that the lymphoscintigraphy is not
100% accurate in pointing out the sentinel node. The new and sensitive single-
photon emission computed tomography/computed tomography method has
demonstrated that there are more sentinel nodes than can be found via conventional
lymphoscintigraphy 82
.
-
45
Lymph flow is known to be variable. It is possible that the sentinel node
contains tumor that blocks the lymphatic channel. Scintigraphy and blue dye will
then be diverted to a ‘‘neo’’ sentinel node that may not yet be involved. Lymph
fluid travels swiftly through a lymph vessel, but little is known about the kinetics of
tumor cells in lymphatics. Thus, another reason for a false-negative result may be
that tumor cells are still in transit at the time of the sentinel node biopsy.
Most studies have demonstrated a learning curve for surgeons, during which
the detection rate of SLNs increases to approximately 98% and the false-negative
rate declines 80,81
. The false-negative rate does not fall below 5%, and this seems to
be accepted by the medical breast cancer community.
Relevance of Internal Mammary SLNB
The two main nodal regions of the breast are the axillary and the parasternal or
internal mammary (IM) chain. Although a purely mechanical approach would
suggest that medial tumours drain towards the IMNs and lateral tumours towards the
axilla, this is not truly the case, although the location of the tumour may influence
the frequency of IMN metastasis.
Radical surgery was once considered the main treatment option for breast
cancer. One such surgical approach was extended radical mastectomy that dissected
not only the axilla, but the IMNs as well. Reports on this treatment option form the
main source of information on the extent of nodal involvement in the IM region At
the end of seventies, on the basis of prospective randomized clinical trials 83
, it was
shown that the dissection of internal mammary chain associated to Halsted
mastectomy was unable to achieve better results than Halsted mastectomy itself.
Survival rates after the two surgical procedures were similar, the recurrence rate to
-
46
internal mammary chain was very low in patients submitted to radical mastectomy,
and the frequency of metastatic spread to endo-thoracic organs was not modified by
IMC dissection. Hence, the role of enlarged mastectomy was also denied as a
staging procedure because of the limited number of patients with negative axillary
nodes and positive internal mammary nodes84-86
. Also some reports suggested that
there may be an improvement in survival in patients treated with extended radical
mastectomy, though this effect may be minor and not worth the risks and morbidity
of IMN dissection.
The SLN procedure has become the standard of care for staging clinically
node-negative patients with breast cancer. However, controversy exists about the
management of extra-axillary nodes, especially those located in the IM chain.
Depending on the technique of injecting the tracer and the site of the tumor, extra
axillary lymph drainage to the IMC is found in up to 30 % of breast cancer patients.
Several studies reported that prognosis of patients with medially located tumors is
inferior to that of patients with laterally located tumors, probably, a result of under
staging of IMC lymph node metastases with the consequence of omitting adjuvant
treatment in this patient group. However, in randomised trial by Romestaing et al 87
,
of patients with RT versus no RT of the IMC after surgery no significant difference
was found in 10 year overall survival.
Studies also show that IM lymph node metastases are mostly found
concomitantly with axillary metastases and are more common in larger tumours. In
the multivariable analysis 88
, a positive axillary lymph node status, medial tumour
location and increasing age were independent predictors for a positive IMSN.
Although the IM chain nodes are rarely explored, the pTNM classification of
breast carcinomas includes any IMN metastasis in the pN3 category, which leads to
-
47
the disease being classified as advanced stage breast cancer. With axillary nodal
involvement, the incidence of IMN metastasis increases. A larger axillary metastatic
load may represent a higher risk of IMN metastasis. Functioning lymphatic shunts
between the axillary and IM region can sometimes be visualised by lymphography,
but under pathological conditions, such as obstruction and a rise in pressure due to
metastatic obliteration, the communication between the two regions becomes more
obvious, and this is reflected by a 2- to 8-fold rise in positivity of the IMNs. In case
of IM hotspots on lymphoscintigraphy, the risk of these nodes harbouring
metastases is substantial 88
.
Isolated IMN involvement is rare, ranging between 2 and 9% 89
. Currently,
IMN positivity is recognised as a feature predicting a poor outcome, and is
considered to forecast a worse prognosis than that for axillary nodal metastases.
The TNM system of the UICC is the basis of the AJCC staging system, where
any metastatic load to the IMNs (independently of the presence or absence of
axillary nodal metastases) would result in a diagnosis of advanced stage breast
cancer (stage IIIB, if distant metastases are absent). Patients with isolated IMN
involvement may be over staged within this system. Determination of the IMN
status is therefore of prognostic importance, and its role may lie in the indication or
selection of adjuvant systemic treatment.
SLNB in the axilla is an ideal procedure for axillary staging, and this may be
the case with IM SLNB too. As the incidence of IM drainage is in the range 6–20%
in most studies, the 23% overall and 5% isolated IMN involvement of patients
undergoing IM SLNB means that IMN involvement is rare (1.4–4.6%) in patients
selected for lymphatic mapping 89
. The rate of identification of SLNs in the IM
-
48
region is lower than in the case of axillary SLNB. Although more challenging than
axillary SLNB, IM SLNB is feasible and causes complications only rarely; its
morbidity is far less than that of complete dissection of these nodes. Since the
dissection of IMNs probably has at most a negligible effect on survival, IM SLNB
may be a good alternative with which to complement the staging of breast cancer. It
may allow the selection of a few axillary node-negative patients for adjuvant
therapy who would otherwise not receive this option of treatment on the basis of the
tumour characteristics. However, the number of these patients seems very small
(about 1% with isolated IMN metastasis) 89
.
Another role of nodal positivity detected by IM SLNB may be the indication
of more aggressive systemic treatment in axillary node-positive patients. Although
radiation therapy of the parasternal region does not seem to improve the
survival88,89
, the value of this treatment in IMN-positive patients detected by SLNB
should also be assessed in future studies. As an important complement to the
benefits of IM SLNB (staging and prognostic value), its costs (extra time required
and morbidity) should additionally be assessed before this tool is implemented in
the staging of breast cancer.
Current knowledge is insufficient to allow this procedure to be recommended
for routine use, but its potential for improving the staging and influencing the
treatment of breast cancer should be assessed in centres that have experience with
SLNB.
-
49
METHODOLOGY
-
50
Methodology
Study Design:
This is a prospective study conducted on 58 patients.
Settings:
Department of General Surgery at J.J.M Medical College, Davangere,
Karnataka, India.
Source of Data:
58 female patients with primary diagnosis of early breast cancer, clinical stage
T1/T2 N0M0, admitted in Chigateri general hospital and Bapuji hospital attached to
J.J.M Medical College, Davangere from June 2011 to May 2013 (2 years), were
selected for this study.
Method of Collection of data:
A pretested proforma was used to collect relevant information (patient data,
detailed history, clinical examination, FNAC/Trucut biopsy, USG breast and axilla,
USG abdomen, mammography and chest x-ray, lab investigations, etc.) from all
selected patient and patients were assessed.
With all the required preoperative investigations, informed consent from all
participating patients and after ensuring fitness for surgery, these patients were
taken for SLNB along with modified radical mastectomy.
Methylene blue dye (5 cc of 1% dye) was injected in subareolar region 20
minutes prior to surgery. The breast was then massaged for 5 minutes.
Intraoperatively, sentinel lymph node were searched after raising superior flap.
Dissection of axillary tissue to identify stained lymph node was done. All blue
-
51
nodes and any node receiving a blue lymphatic channel were considered as sentinel
nodes. After excising the stained lymph nodes, complete axillary clearance and
removal of breast tissue was done.
Lymph nodes were divided into two groups: the dye stained lymph node as
Sentinel Node and the rest of the lymph nodes removed by axillary clearance. These
along with the breast specimen were subjected to histopathological examination and
pathological data including histopathological type, size of the tumor, ER/PR status,
HeR2Neu status, lymph node status in sentinel and non sentinel lymph nodes was
collected.
Inclusion Criteria
Patients with pathologically (FNAC/Trucut biopsy) proved early breast cancer
without clinically palpable nodes, clinical stage T1/T2 N0 M0.
Exclusion Criteria
1) Pregnant/lactating patients.
2) Patients with clinically palpable nodes.
3) Patients with primary breast lesions clinically larger than 5cm.
4) Patients with multicentric and multifocal tumor.
5) Patients with systemic metastasis.
6) Patients with previous breast surgery.
7) Patients with previous radiotherapy and/or chemotherapy.
8) Patients who were allergic to methylene blue dye.
-
52
METHOD OF STATISTICAL ANALYSIS:
Diagnostic Validity Tests calculating sensitivity, specificity, false negative,
positive predictive value, negative predictive value and accuracy of the sentinel
lymph node biopsy were done after final histopathology report was available in
comparison with rest of the axillary lymph nodal status to assess the efficacy of
sentinel lymph node biopsy in detecting axillary metastasis using following
formulae-
-
53
RESULTS
-
54
RESULTS
“SENTINEL LYMPH NODE BIOPSY IN EARLY BREAST CANCER
USING METHYLENE BLUE”, a prospective study was conducted in a total
of 58 female patients from June 2011 to May 2013 (2 years). Sentinel lymph
node was identified in 50 cases (identification rate 86%), in 08 cases sentinel
lymph node could not be identified. The efficacy was analysed using diagnostic
validation tests in terms of sensitivity, specificity, false negative rate, positive
predictive & negative predictive value and accuracy in determining axillary
metastasis.
None of the patient’s had local irritation of the skin or any hypersensitivity
reaction to methylene blue dye.
Between June 2011 and May 2013, 58 patients underwent SLNB using
methylene blue dye followed by MRM in same operative setting.
Average age of the patients was 44 yrs (range 25–70 years).
-
55
Table 1 Tumor characteristics of patients in whom SLN identified
Breast Carcinoma No. of Cases
SIDE
RIGHT sided tumor 27 (54%)
LEFT sided tumor 23 (46%)
QUADRANT
OUTER quadrant 39 (78%)
INNER quadrant 08(16%)
CENTRAL 03 (06%)
T stage
T 1 tumors 12 (24%)
T 2 tumors 38 (76%)
TUMOR HISTOLOGY
Invasive ductal carcinoma 43 (86%)
Invasive lobular carcinoma 05 (10%)
Mucinous carcinoma 01 (02%)
Tubular carcinoma 01 (02%)
Hormone Receptor
ER/PR Positive 42 (84%)
Negative 08 (16%)
Her2neu Positive 05 (10%)
Negative 45 (90%)
-
56
Among 50 cases in which SLN was identified, 27 cases (54%) had right
sided tumor while 23 cases (46%) had tumor on left side. In 39 cases (78%)
tumors were located in outer quadrant of involved breast, in 8 cases (20%) in
the inner quadrant and in 3 cases (6%) tumor occupied central/subareolar
position.
On clinically staging, 38 cases (76%) had tumors in T2 stage and 12 cases
(24%) were classified as T1 stage tumors. In none of the cases axillary
lymph nodes were clinically palpable and no evidence of distant metastasis
was seen.
On histopathological examination of excised tumor, infiltrating ductal
carcinoma was found in 43 cases (86%), 5 cases (10%) were lobular
carcinoma and 1 case (2%) each of mucinous & tubular carcinoma was
found.
Hormone Receptor ER/PR was positive in 42 cases (84%) while Her2neu
was positive in 5 (10%) cases. In 4 cases (8%) tumors were positive for both
ER/PR and Her2neu while in 1 case (2%) tumor was positive only for
Her2neu receptor. 7 cases (14%) were negative for both ER/PR and
Her2neu receptors.