Ann Oncol 1998 Ducreux 653 6
Transcript of Ann Oncol 1998 Ducreux 653 6
-
8/13/2019 Ann Oncol 1998 Ducreux 653 6
1/4
nnals of Oncology 9: 653-656, 1998.6 1998 Khmer cademic Publishers. Primed in the Netherlands.
Original article
Effective treatment of advanced biliary tract carcinoma using 5-fluorouracilcontinuous infusion with cisplatin
M. Ducreux, P. Rougier, A. Fandi, M.-C. Clavero-Fabri, A.-L.Villing, F. Fassone, L. Fand i,J. Zarba J.-P. Arman dDepartment of M edicine Institut Gustave Roussy Villejutf France
Summary
ackground The combination of 5-fluorouracil (5-FU) andcisplatin has shown great activity in many different types oftumour with an in vitro synergistic effect between 5-FU andcisplatin. A phase II study of 5-FU plus cisplatin was per-formed in 25 previously untreated patients with inoperablelocally advanced or metastatic biliary tract carcinoma.
Patients and methods: Twenty-five patients, 10 of them menand 15 women with a median age of 58, were entered in tothe study. The chemotherapy regimen consisted of 5-FU:1 g/m /day in continuous intravenous (i.v.) infusion for fiveconsecutive days, and cisplatin: 100 mg/m2/day on day 2 in aone-hour infusion with standard hyperhydration. Twenty-twopatients had metastatic tumours and three had locally ad-vanced disease.
Results: Of the 25 patients entered into the study, 24 wereevaluable for response and 25 for toxicity. Nausea and vomit-ing was the main toxic side effect in 19 patients. Severe, WH Ograde 3-4 thrombocytopenia or neutropenia were observed inthree and seven patients, respectively. There were no toxicdeaths. Of 25 patients, six had partial remissions (overallresponse 24 , 95 confidence interval 7 -41 ). For threepatients, tumour reduction permitted local radiotherapy andone of these patien ts with initially advanced disease is still alivesix years after the beginning of treatm ent.
Conclusions: This study, one of the largest phase II trialsperformed in this disease, shows interesting activity of thecombination of 5-FU and cisplatin in advanced biliary tractcarcinoma.
Key words: biliary tract cancer, chemotherapy
Introduction
Most reports of chemotherapy for cancers of the biliarysystem involve very small num bers of patients. Respon serates appear to be similar to those for advanced carci-nomas of the gallbladder, bile duct and intrahepaticcholangiocarcinoma. For single-agent systemic chemo-therapy , the objective respo nse rates vary from 10 to25 in the series includin g 15 or m ore pat ient s [1, 2].
5-fluorouracil (5-FU) was the most promising agent inthese studies [1]. Multiagent systemic chemotherapy doesnot seem to increase the response rate: the combinationregimens FAM: 5-FU + adriamycin + mitomycin C,and 5-FU plus methyl-CCNU yielded poor results: 29and 10 , respectively [1, 3]. Cis plati n as a single agentchemotherapy is not effective in this tumour [4], butbecause the combination of 5-FU and cisplatin has showngreat activity in many different types of tumour with anin vitro synergistic effect between 5-FU and cisplatin [5],we decided to assess the efficacy of this treatment inbiliary tract cancer.
Patients and methods
From January 1991 to December 1994, 25 consecutive patients wereincluded in this phase II study. Eligibility criteria were the presence ofhistologically proven adenocarcinoma of the biliary tract with evi-dence of metastatic disease or unresectable local recurrence and noprevious chemotherapy. Patients had to have a performance status (PS) 100,000/ml), no signs of renalor hepatic failure (serum creatinine 75 ) and no other malignancy. All patients had to have measurabledisease on computed tomography (CT)-scan. All patients gave theirinformed consent.
Pre-treatment evaluation included a complete physical examina-tion, an abdominal ultrasound, an abdominal CTscan and a thoracicCT scan if they had lung metastases. Renal function tests, hepaticenzymes, serum lactic dehydrogenase (LDH ), carcino-embryonic an ti-gen (CEA) and carbohydrate antigen assays (CA 19-9) were performedbefore each cycle. Complete blood and platelet counts were performedevery week to assess haem atological toxicity.
The chemotherapy regimen was 5-FU: 1 g/m2/day in continuousintravenous (i.v.) infusion for five consecutive days, and cispla tin:100 mg/m2/day on day 2 in a one-hour infusion with standard hyper-hydration. Cycles were repeated every four weeks according to haema-tological, digestive and renal tolerance. Treatment continued until pro-
gression, intolerable toxicity or elective withdrawal from the trial. Allof the patients were given prophylactic antiemetic treatment consistingof 5HT3 antagonists for the first seven patients and a combination of5HT3 antagonists and dexamethasone for the remaining 18. The 5-FUdosage was reduced in instances of stomatitis, diarrhoea, neutropenia
b y g u e s t onA
pr i l 2 8 ,2 0 1 3
h t t p : / / a nn on c . oxf or d j o ur n a l s . or g /
D o wnl o a d e d f r om
http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/ -
8/13/2019 Ann Oncol 1998 Ducreux 653 6
2/4
-
8/13/2019 Ann Oncol 1998 Ducreux 653 6
3/4
655
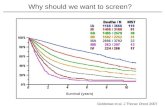
Survival time mont hs)
Figure 1. Overall survival of the 25 patients who were treated bychemotherapy for advanced biliary tract cancer.
Treatment toxicity was manageable and not radicallydifferent from the toxicity observed in other types oftumour with the same schedule [5, 7]. Nausea/vomitingwas the main toxicity, but all patients for whom it wasconsidered effective were able to continue the treatment.
A few studies have tested chemotherapy in biliary tractcarcinoma. Monochemotherapy yielded disappointing re-sults, with objective response rates ranging from 5 to20 . Mitomycin C, which seemed relatively active in thepast, was assessed by the EORTC. The treatment's activ-ity was evaluated using recent and precise rules: of30 patients, three had partial remissions, for an overallresponse rate of 10 [2]. Paclitaxel does not have prom-ising results in biliary tract carcinoma: no complete orpartial responses were noted in 13 patients although twopatients achieved minor responses [8]. Two phase IIstudies compared 5-FU alone to polychemotherapy. Inthe first study, the regimens compared to 5-FU alonewere 5-FU plus streptozotocin and 5-FU plus methyl-CCNU [1]. The comparison did not show an advantagefor the polychemotherapy, which had increased toxiceffects without clear benefit in terms of responses. Thesecond randomised trial gives comparable results dis-proving the hypothesis that 5-FU plus adriamycin plus
mitomycin C are superior to 5-FU alone [9]. In a recentphase II study the combination of 5-FU, epirubicin andmethotrexate yielded no responses [10]. Two recentphase II studies have shown more promising results.The first one combined 5-FU and subcutaneous recombi-nant human interferon-oc-2b in patients with measurablecancer of the biliary tract. The objective response ratewas 34 in this study and the median survival 12 months,closely similar to the results of our study. Grade 3-4toxic effects were frequent: neutropenia 14 , stom atitis:20 , asthenia: 6 . When compared to our schedule, thistreatment seems to have a similar efficacy but a highertoxicity and cost [11]. A second recent phase II studyinvestigated the efficacy of the ECF regimen whichcombined low-dose 5-FU continuous infusion plus epi-rubicin plus cisplatin. Eight of the 20 evaluable patientsresponded; the median duration of response was 10
months and the median survival was 11 months [12]. Theregimen was relatively well tolerated with 16 grade 3-4leukopenia and 19 thrombocytopaen ia, but grade 3alopecia was observed in 31 of the patients. The 5-FUcontinuous infusion does not seem to decrease quality of
life in patients with gastric cancer [13]. However, itmakes the treatment more onerous for the patient andmore expansive than the classical five-day/5-FU cisplatinschedule we chose to test in these patients with short lifeexpectancy.
These recent optimistic data are supported by theresults of the only phase III study performed in thisarea. Glimelius et al. [14] randomised 90 patients withpancreatic or biliary cancer (43 and 37, respectively) toeither chemotherapy in addition to best supportive careor to best supportive care. Chemotherapy was eithersequential 5-FU/leucovorin combined with etoposideor, in elderly and poor-performance-status patients, thesame regimen without etoposide. The overall conclusionwas clear: chemotherapy improves the survival of suchpatients without impairing their quality of life. However,when only the patients with biliary tract cancer wereconsidered the results were no longer statistically signif-icant although they reached the same absolute value.
It must be pointed out that one of our patients had avery extensive local disease recurrence which was notsurgically treatable and difficult to irradiate. This patienthad a very rapid and dramatic response to chemother-apy which rendered him ready for radiotherapy after sixtreatment cycles. With a six-year follow-up she remainsdisease-free.
In conclusion: 5-FU plus cisplatin is an active chemo-therapy in metastatic or inoperable biliary tract carci-noma. This widely used schedule has a manageable tox-icity, and should be considered for further investigation.
References
1. Falkson G, Maclntyre JM, Moertel CG. Eastern CooperativeOncology Group experience with chemotherapy for inoperablegallbladder and bile duct cancer. C ancer 1984; 54: 965-9.
2. Taal BG, Audisio RA , Bleiberg H et al. Phase II trial of mit o-
mycin C (MMC) in advanced gallbladder and biliary tree carci-noma. An EORTC Gastrointestinal Tract Cancer CooperativeGro up study. Ann O ncol 1993; 4: 607-9.
3. Harvey JH, Smith FP, Schein PS. 5-fluorouracil, mitomycin anddoxorubicin (FAM) in carcinoma of the biliary tract. J ClinOncol 1984; 2: 1245 8.
4. Ok ada S, Ishii H, Nose H et al. A phase II study of cisplatin inpatients with biliary tract carcinoma. Oncology 1994; 51: 515-7.
5. Rougier P, Zarba JJ, Ducreux M et al. Phase II study of cisplatinand 120-hour infusion of 5-fluorouracil in patients with advancedpancreatic adenocarc inom a. Ann Oncol 1993: 4: 333-6.
6. Miller AB, Hoogstraten B, Staquet M et al. Reporting results ofcancer treatment. Cancer 1981: 47: 201-14.
7. Rou gier P, Fandi A, Ducre ux M et al. Dem onst rated efficiency of5-fluorouracil continuous infusion and cisplatin in patients with
advanced biliary tract carcinoma. Proc Am Soc Clin Oncol 1995;14: 205 (Abstr).
8. Jones DVJ, Lozano R, Hoque A et al. Phase II study of paclitaxeltherapy for unresectable biliary tree carcinomas. J Clin Oncol1996; 14 (8): 230 6-10.
b y g u e s t onA
pr i l 2 8 ,2 0 1 3
h t t p : / / a nn on c . oxf or d j o ur n a l s . or g /
D o wnl o a d e d f r om
http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/http://annonc.oxfordjournals.org/ -
8/13/2019 Ann Oncol 1998 Ducreux 653 6
4/4