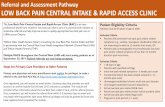
Anatomy of pain pathway
-
Upload
dhritiman-chakrabarti -
Category
Documents
-
view
8.029 -
download
5
description
Transcript of Anatomy of pain pathway

PAIN PATHWAY ANATOMY MODERATOR: DR FAREED AHMED
PRESENTED BY:DR ANURADHA

Sensation of the affected level of unpleasantness
Perception of actual or threatened damage based on past experience, anxiety, cognitive factors
Pain is Subjective
Introductory Ideas

A quality that has complex phenomenological facets (behavioral, sensory, emotional)
Pain perception can be modulated by all kinds of factors, including behavioral states (stress, sex), cognitive states (hypnosis), mental states (“trance”), social norms and drugs.
Pain as a special perceptual quality

Nociceptors are special receptors that respond only to noxious stimuli and generate nerve impulses which the brain interprets as “pain”
Free nerve endings Tissue damage
Nociceptors

Aδ – fast, sensitive to mechanical noxious stimuli. – small, myelinated. High conductance speed
C – slow, sensitive to many noxious stimuli (chemical, etc.) – small, unmyelinated. Slow conductance speed
This distinction has been used to explain the phenomenon of double-pain
Pain receptors

The Nervous System and Pain
SomatosensorySystem
Brain
Somatosensory Cortex
Thalamus
Spinal Cord
Dorsal Horn Ventral Root
PNS
Afferent NeuronEfferent Neuron
A-delta FibersC-Fibers

•Glutamate - Central•Substance P - Central•Brandykinin - Peripheral•Prostaglandins - Peripheral
Pain Initiator
s
•Serotonin•Endorphins•Enkephalins•Dynorphin
Pain Inhibito
rs
The Neurochemicals of Pain

1. gray matter 2. white matter 3. gray commissure 4. central canal Dorsal and ventral nerve roots
Internal Anatomy

Ascending and descending fibers are organized in distinct bundles which occupy particular areas and regions in the white matter
Generally long tracts are located peripherally in the white matter, while shorter tracts are found near the gray matter
White Matter: Pathway Generalizations
• The TRACT is a bundle of nerve fibers (within CNS) having the same origin, course, destination & function
• The name of the tract indicates the origin and destination of its fibers• The axons within each tract are grouped according to the body region
innervated

1. nuclei 2. horns a. dorsal -- sensory b. ventral – motor
c. lateral – autonomicSpinal grey matters divided into 10 layers
Gray Matter

Tracts of the Spinal Cord
Tracts that serve to join brain to the spinal cord Ascending Descending
Fibers that interconnect adjacent or distant segments of the spinal cord Intersegmental (propriospinal)

Three major pathways carry sensory informationPosterior column pathway (gracile & cuneate
fasciculi)Anterolateral pathway (spinothalamic) Spinocerebellar pathway

Monitor conditions both inside the body and in the external environment
Sensation-stimulated receptor passes information to the CNS via afferent (sensory) fibers
Most sensory information is processed in the spinal cord , thalamus, or brain stem. Only 1% reaches the cerebral cortex and our conscious awareness
Processing in the spinal cord can produce a rapid motor response (stretch reflex)
Processing within the brain stem may result in complex motor activities (positional changes in the eye, head, trunk)
Sensory Pathways

THREE neurons from the receptor to the cerebral cortex
First order neuron: Cell body located in the dorsal
root ganglion. The Axon (central process) passes to the spinal cord through the dorsal root of spinal nerve gives many collaterals which take part in spinal cord reflexes runs ipsilaterally and synapses with second-order neurons in the cord and medulla oblongata
Sensory Pathways
1
2
3

Second order neuron:◦Has cell body in the
spinal cord or medulla oblongata
◦Axon decussate &◦Terminate on 3rd order
neuron
Third order neuron:◦Has cell body in
thalamus◦Axon terminates on
cerebral cortex ipsilaterally

DIRECT---- direct conscious appreciation of pain
INDIRECT---affective or arousal impact of pain via
1) Spino-reticular-thalamic –cortical pathway (ARAS)
2) Spino-mesencephelic path (affective impact of pain)
SUBSYSTEM

Pain information travels up the
spinal cord through the
spinothalamic track (2 parts)
ANTERIOR/
VENTRAL
LATERAL
Decussates at the level of spinal
cord
Pain Pathways – Going Up

Descending pain pathway responsible for pain inhibition
“affective sensation”i.e compulsion to act
Pain Pathways – Going Down

Spinothalamic Tracts Located lateral and ventral to
the ventral horn Carry impulses concerned
with pain and thermal sensations (lateral tract) and also non- discriminative touch and pressure (medial tract)
Fibers of the two tracts are intermingled to some extent
In brain stem, constitute the spinal lemniscus
Fibers are highly somato-topically arranged, with those for the lower limb lying most superficially and those for the upper limb lying deeply
Information is sent to the primary sensory cortex on the opposite side of the body

Lateral Spinothalamic Tract
Axons of 1st order neurons terminate in the dorsal horn
Axons of 2nd order neuron (mostly in the nucleus proprius), decussate within one segment of their origin, by passing through the ventral white commissure & terminate on 3rd order neurons in ventral posterior nucleus of the thalamus
Thalamic neurons project to the somatosensory cortex


FIRST ORDER NEURONPseudounipolar cell (dorsal
root ganglion) ,divides into central and
peripheral branch) Head and neck,carried
by 5/6/9/10 via gasserian ganglion,geniculate,superior and inferior
petrosal nerve,jugular ganglion(somatic) and ganglion nodosum (viseral)
Reach brain stem via cranial nerves

Tip of the posterior column near posterior nerve roots
Centrally projecting axons carrying discriminating pain /temperature info regarding location/intensity/quality
Synapse with second order neuron,crosses midline and joins STT
LISSAUER’TRACT

SECOND ORDER NEURONSSUBSTANTIA GELATINOSA: grey horn wid gelatinous
sub which contains neuroglia and nerve cells
Rexed lamina 2 Contains opiod
receptors/ c fibres and a-delta fibres
NUCLEUS PROPRIUS Bulk of dorsal horn Rexed 3/4/5 a/w fine touch and
pressure with nucleus dorsalis

Spinal Cord Internal Structure Spinal Cord Internal Structure
Lamina of Rexed
Lamina I ---------- marginal layer Lamina II ---------- substantia gelatinosa of Rolando Lamina III, IV ----- nucleus proprius Lamina V, VI Lamina VII --------- intermediate gray intermediolateral cell column (ILM) Clarke’s column (Nucleus dorsalis) intermediomedial cell column (IMM) Lamina VIII----------motor horn Lamina IX ---------- anterior horn (motor) cell Lamina X ----------- gray commissure
Lamina of Rexed
Lamina I ---------- marginal layer Lamina II ---------- substantia gelatinosa of Rolando Lamina III, IV ----- nucleus proprius Lamina V, VI Lamina VII --------- intermediate gray intermediolateral cell column (ILM) Clarke’s column (Nucleus dorsalis) intermediomedial cell column (IMM) Lamina VIII----------motor horn Lamina IX ---------- anterior horn (motor) cell Lamina X ----------- gray commissure

ANTERIOR WHITE COMMISURE alba anterior medullae spinalis just anterior to the gray
commissure (Rexed lamina X). A δ fibers and C fibers
ROSTRAL VENTROMEDIAL MEDULLA
midline on the floor of the medulla (myelencephalon
sends descending inhibitory and excitatory fibers to the dorsal horn spinal cord neurons
On-cells, off-cells, and neutral cells.
important in the maintenance of neuropathic pain
RVM contains high levels of both the neurokinin 1 receptor and its endogenous ligand, Substance P (SP).

THALAMUS

Cortical pain processing Sensory aspects of pain seem to be processed in the
Somatosensory cortex. Emotional distress associated with pain seems to be
processed in the Anterior Cingulate Cortex (ACC). Subjects with lesions in ACC could still accurately
judge the intensity of pain. But they were not in the least bothered by it.
• On the other hand, subjects empathy for the pain of others only elicits activity in ACC, not Somatosensory cortex.

CINGULATE CORTEX the medial aspect of the
cortex Part of limbic lobe Receives input from
thalamus and neocortex
PRIMARY SOMATOSENSORY CORTEX
CORTEX

INSULAR CORTEX
deep within the lateral sulcus the fissure separating the temporal and the frontal lobes
linked to emotion
Associated with addiction

gray matter located around the cerebral aqueduct within the tegmentum of the
midbrain. role in the descending modulation of pain
and in defensive behaviour. enkephalin-releasing neurons 5-HT (serotonin) released from the raphe
nuclei descends to the dorsal horn of the spinal cord where it forms excitatory connections with the "inhibitory interneurons" located in Laminae II (aka the substantia gelatinosa).
When activated, these interneurons release either enkephalin or dynorphin which bind to mu opioid receptors
PERIAQUEDUCTAL GREY MATTER

5. “Pain Gate” TheoryMelzack & Wall (1965)
A gate, where pain impulses can be “gated”
The synaptic junctions between the peripheral nociceptor fiber and the dorsal horn cells in the spinal cord are the sites of considerable plasticity.
descending nerve fibers from brain
axons from touch receptors
axons from nociceptors“THE PAIN GATE”
opioid-releasing interneuron
pain pathways

Stimulation of touch fibres for pain relief:◦ TENS (transcutaneous electrical nerve
stimulation)◦ Acupuncture◦ Massage
Release of natural opioids◦ Hypnosis◦ Natural childbirth techniques
Applications of pain gate

MEDIAL SPINOTHALAMIC TRACT:
MEDIAL THALAMUS MEDIATES AUTONOMIC AND UNPLEASANT
PERCEPTION OF PAIN PATHWAY FEW TO PERIAQUEDUCTAL GRAY COLLATERAL FIBRES TO RAS AND
HYPOTHALAMUS-AROUSAL TO PAIN

ran additional route by which dull, aching pain is transmitted to a conscious level
Some 2nd order neurons terminate in the reticular formation of the brain stem, mainly within the medulla
Reticulothalamic fibers ascend to intralaminar nuclei of thalamus, which in turn activate the cerebral cortex
Spino-reticulo-thalamic System

Opiate receptors location Located in
periaqueductal grey matter of the brainstem,amygdala,corpus striatum nd hypothalamus
Spinal cord(substance gelatinosa)
Endorphins inhibit release of excitatory neurotransmitters

Opiate receptors
Mu,kappa and delta Superfamily of G protein
coupled receptors Brain,spinal cord and
peripheral recetors Mimic endogenous ligands l/t hyperpolarisation

38
Visceral Pain
• Pain receptors are the only receptors in viscera whose stimulation produces sensations• Pain receptors respond differently to stimulation• Pain receptors are not well localized• Pain receptors may feel as if coming from some other part of the body• Known as referred pain…

Afferent innervation of the viscera.
Often anatomical separation nociceptive innervation (in sympathetic nerves) from non-nociceptive (predominantly in vagus).
Many visceral afferents are specialized nociceptors, as in other tissues small (Ad and C) fibers involved.
Large numbers of silent/sleeping nociceptors, awakened by inflammation.
Nociceptor sensitization well developed in all visceral nociceptors.

Referred pain Pain originating
from organs perceived as coming from skin
Site of pain may be distant from organ

Convergence theory: This type of referred pain occurs because both visceral and somatic afferents often converge on the same interneurons in the pain pathways.
Excitation of the somatic afferent fibers is the more usual source of afferent discharge,
so we “refer” the location of visceral receptor activation to the somatic source even though in the case of visceral pain.
The perception is incorrect.The convergence of nociceptor input from the viscera and the skin.
Referred pain

42
Regulation of Pain Impulses
• Thalamus • Allows person to be aware of pain
• Cerebral cortex • Judges intensity of pain • Locates source of pain• Produces emotional and motor responses to pain
• Pain inhibiting substances:• Enkephalins• Serotonin• Endorphins

Spinothalamic damage
spinothalamic pathwayLeftspinal cord injury
Loss of sense of:•Touch•Pain•Warmth/coldin right leg
. Anaesthesia will normally begin 1-2 segments below the level of lesion, affecting all caudal body areas.

Hyperalgesia:
The skin, joints, or muscles that have already been damaged are unusually sensitive. A light touch to a damaged area may elicit excruciating pain;
Primary hyperalgesia occurs within the area of damaged tissue;
Secondary hyperalgesia occurs within the tissues surrounding a damaged area.

Melzack (1992) 7 features 1. Phantom limb feels real. Sometimes amputees
try to walk on their phantom limb.2. brain contains neuromatrix of the body image –
neurosignature like a hologram
Phantom limb pain

A well-known case of congenital insensitivity to pain is a girl referred to as 'miss C' who was a student at McGill university in Montreal in the 1950s.
She was normal in every way, except that she could not feel pain. When she was a child she had bitten off the tip of her tongue and had suffered third-degree burns by kneeling on a radiator.
Congenital Analgesia

Aspirin and ibuprofen block formation of prostaglandins that stimulate nociceptors
Novocain blocks conduction of nerve impulses along pain fibers
Morphine lessen the perception of pain in the brain.
Pain Relief

1. Prevents serious damage. If you touch something hot, you are forced to withdraw your hand before it gets seriously burnt.
2.Teaches one what to avoid 3.If pain is in joints, pain limits the activity,
so no permanent damage can occur. but pain can become the problem, and
cause people to want to die.
Purpose of pain