Anatomy and physiology of thyroid and parathyroid gland
-
Upload
lakshminarayan-bhat -
Category
Health & Medicine
-
view
150 -
download
3
Transcript of Anatomy and physiology of thyroid and parathyroid gland
1
Lakshminarayan S BhatPG student, Dept. of Gen. Surgery
29-04-2015
Surgical anatomy and physiology of thyroid and
parathyroid gland
• To know the development and associated anomaly of thyroid and parathyroid gland
• To know the relations, nerve supply, vascular supply, lymphatic drainage of thyroid and parathyroid gland; its surgical importance.
• To know the physiology of thyroid and parathyroid gland.
Aim of the topic
• The thyroid gland appears as an epithelial proliferation in the floor of the pharynx between the tuberculum impar and the copula at a point later indicated by the foramen cecum. The vestigial marking of the thyroglossal duct is the foramen cecum of the tongue.
• Subsequently the thyroid descends in front of the pharyngeal gut as a bilobed diverticulum.
• During this migration,the thyroid remains connected to the tongue by a narrow canal, the thyroglossal duct. This duct later disappears.
• It reaches its final position in front of the trachea in the seventh week. By then it has acquired a small median isthmus and two lateral lobes
• The thyroid begins to function at approximately the end of the third month.
• Follicular cells produce the colloid that serves as a source of thyroxine and triiodothyronine. Parafollicular, or C, cells derived from the ultimobranchial body serve as a source of calcitonin.
Developement
• A thyroglossal cyst: may lie at any point along the migratory pathway of the thyroid gland but is always near or in the midline of the neck. It is a cystic remnant of the thyroglossal duct.
• Approximately 50% of these cysts are close to or just inferior to the body of the hyoid bone,they may also be found at the base of the tongue or close to the thyroid cartilage.
• Thyroglossal fistula: usually arises secondarily after rupture of a cyst but may be present at birth.
• Aberrant thyroid tissue: may be found anywhere along the path of descent of the thyroid gland. It is commonly found in the base of the tongue (Lingual thyroid), just behind the foramen cecum
Developmental abnormalities
• The thyroid gland, brownish-red and highly vascular, is placed anteriorly in the lower neck, level with the sixth cervical to the first thoracic vertebrae
• It is ensheathed by the pretracheal layer of deep cervical fascia and consists of right and left lobes connected by a narrow, median isthmus. Its weight is usually 25g, but this varies.
• The gland is slightly heavier in females, and enlarges during menstruation and pregnancy.
• It is located in the neck, inferior to the larynx and cricoid cartilage.
• The lobes of the thyroid gland are approximately conical. • Their ascending apices diverge laterally to the level of
the oblique lines on the laminae of the thyroid cartilage, and their bases are level with the fourth or fifth tracheal cartilage rings.
• Each lobe is around 5 cm long, its greatest transverse and antero posterior extents being approx.3 cm and 2 cm respectively.
• The posteromedial aspects of the lobes are attached to the side of the cricoid cartilage by a lateral thyroid ligament
• The isthmus connects the lower parts of the two lobes, although occasionally it may be absent
• It measures 1.25 cm transversely and vertically, and is usually anterior to the second and third tracheal cartilages, though often higher or sometimes lower because its site and size vary greatly.
• A conical pyramidal lobe often ascends towards the hyoid bone from the isthmus or the adjacent part of either lobe (more often the left).
• The thyroid gland is surrounded by a fibrous capsule derived from the pretracheal layer of the deep cervical fascia.
• Extensions of this capsule into the body of the thyroid create septae, which divide the gland into lobules.
• This connective tissue firmly connects the thyroid to the larynx and explains why the thyroid moves on swallowing.
• The convex lateral (superficial) surface is covered by sternothyroid, whose attachment to the oblique thyroid line prevents the upper pole of the gland from extending on to thyrohyoid
• More anteriorly lies sternohyoid and the superior belly of omohyoid, overlapped inferiorly by the anterior border of sternocleidomastoid
• The medial surface of the gland is attached to the larynx and trachea, contacting at its superior pole the inferior pharyngeal constrictor and the posterior part of cricothyroid, which separate it from the posterior part of the thyroid lamina and the side of the cricoid cartilage
• The external laryngeal nerve is medial to this part of the gland as it passes to supply cricothyroid. Inferiorly, the trachea and, more posteriorly, the recurrent laryngeal nerve and oesophagus (which is closer on the left) are medial relations.
• The posterolateral surface of the thyroid gland is close to the carotid sheath, and overlaps the common carotid artery
SURFACES AND RELATIONS
• The thin anterior border of the gland, near the anterior branch of the superior thyroid artery, slants down medially.
• The rounded posterior border is related below to the inferior thyroid artery and its anastomosis with the posterior branch of the superior thyroid artery
• The isthmus is covered by sternothyoid, from which it is separated by pretracheal fascia. More superficially it is covered by sternohyoid, the anterior jugular veins, fascia and skin.
• The superior thyroid arteries anastomose along its upper border and the inferior thyroid veins leave the gland at its lower border
Blood supply, nerves • The thyroid is highly vascular, and a bruit (the sound of turbulent blood flow) is sometimes heard in overactive glands• Mainly,It is supplied by two arteries that
anastomose within the gland: the inferior and superior thyroid arteries
• The inferior thyroid artery is a branch of the thyrocervical trunk, which arises from the first part of the subclavian artery and it ascends along the medial edge of the anterior scalene muscle, passes posteriorly to the carotid sheath, and reaches the inferior pole of the lateral lobe of the thyroid gland.
• It divides into inferior branch, which supplies the lower part of the thyroid gland and anastomoses with the posterior branch of the superior thyroid artery; and an ascending branch, which supplies the parathyroid glands.
• The right recurrent laryngeal nerve is intimately related to this artery near the inferior pole of the thyroid gland. During thyroid Surgery it may get damaged if utmost care is not taken.
• Damage to the nerve causes hoarseness of voice
• To minimize the risk, traditional teaching is to ligate artery, far away from the thyroid gland during thyroid surgery
• The superior thyroid artery is the first branch of the external carotid artery.
• It descends, passing along the lateral margin of the thyrohyoid muscle, to reach the superior pole of the lateral lobe of the gland where it divides into anterior and posterior glandular branches:
• the anterior glandular branch passes along the superior border of the thyroid gland and anastomoses with its twin from the opposite side across the isthmus; the posterior glandular branch passes to the posterior side of the gland and may anastomose with the inferior thyroid artery
• The external laryngeal nerve is related to this artery, but it is at less risk than the recurrent laryngeal during thyroid surgery.
• The superior thyroid artery is ligated close to the thyroid gland to reduce this risk
• A third artery, called the thyroidea ima artery, is present in less than 5% of people. It supplies the isthmus and it arises from brachiocephalic trunk or aortic arch.
Venous and lymphatic drainage • The thyroid gland is drained by
three veins: • Superior thyroid vein. • Middle thyroid vein. • Inferior thyroid vein.• The first two veins drain into the
internal jugular, whereas the inferior vein drains into the brachiocephalic veins.
• Thyroid lymphatics drain into four groups of nodes: • Prelaryngeal lymph nodes. • Pretracheal lymph nodes. • Paratracheal lymph nodes. • Deep cervical lymph nodes
Surgical importance of nerves and artery & surgical landmarks in thyroid surgery
Recurrent laryngeal nerve:•The recurrent laryngeal nerves ascend on either side of the trachea and each lies just lateral to ligament of Berry as it enters the larynx.• In about 25% of patients, the recurrent laryngeal nerve is contained within the ligament as it enters the larynx.• Right recurrent laryngeal nerve originates from the vagus nerve as it crosses the subclavian artery; it then passes posterior to the subclavian artery and ascends in a position lateral to the trachea along the tracheoesophageal groove.•Right recurrent laryngeal nerve can usually be found no further than 1 cm lateral to or within the tracheoesophageal groove, at the level of the lower border of the thyroid•At midportion of thyroid the nerve might divide into one, two, or more branches as it enters the first or second ring of the trachea, with the most important branch disappearing beneath the inferior border of the cricothyroid muscle. The nerve can usually be found immediately anterior or posterior to a main arterial trunk of the inferior thyroid artery at this level. •a nonrecurrent right laryngeal nerve can arise directly from the vagus and course medially into the larynx. This nonrecurrent anatomy is found in 0.5% to 1.5% of patients and occurs in the setting of arterial anomalies (arteria lusoria),
• Left side, the recurrent laryngeal nerve separates from the vagus as that nerve traverses the arch of the aorta
• It passes inferiorly and medially to the aorta at the ligamentum arteriosum and begins to ascend toward the larynx, where it enters the tracheoesophageal groove as it ascends to the level of the lower lobe of the thyroid
• A nonrecurrent left laryngeal nerve is associated with more extensive anomalies and it is very rare.
• A small branch of the inferior laryngeal artery crosses the nerve at the level of the ligament of Berry, so bleeding in this area should be addressed with great caution to avoid nerve injury.
Superior Laryngeal Nerve 1. separates from the vagus nerve at the base of the
skull and descends toward the superior pole of the thyroid along the internal carotid artery
2. At the level of the hyoid cornu, it divides into external and internal branches
3. external branch continues to travel along the lateral surface of the inferior pharyngeal constrictor muscle and usually descends anteriorly and medially, along with the superior thyroid artery
4. With in1 cm of the entrance of the superior thyroid artery into the thyroid capsule, the nerve generally takes a medial course and enters the cricothyroid muscle
5. Damage to the external branch can result in severe loss of voice quality or strength.
Cernea’s classificationAccording to this external branch of superior laryngeal nerve is divided into type 1, type 2A and 2B.
Space of reeves• Cricothyroid space of Reeves; performing Medial
Dissection at Superior Pole for Crico-thyroid Space for Ligating the Artery and Vein Individually.
• This is a critical step in order to avoid damage to the external laryngeal nerve
Tubercle of Zuckerkandl • It is the posterior extension of lateral lobes.• It is found in approx. 60-70% of people.
Whenever found the recurrent laryngeal nerve is usually deep to it.
• More common in right side
Physiology of thyroid harmone
• The thyroid gland synthesizes and secretes three hormones:
• Thyroxine (T4). • Tri-iodothyronine (T3). • Calcitonin
Regulation
• Hypothalamic thyrotrophin-releasing hormone (TRH)
stimulates the release of thyroid-stimulating hormone (TSH) from thyrotrophs in the anterior pituitary gland and also causes upregulation of TSH gene transcription.
Thyroxine (T4) andTri-iodothyronine (T3).
• Both of these hormones profoundly increase the metabolic rate of the body.
• Complete lack of thyroid secretion usually causes the basal metabolic rate to fall 40 to 50 per cent below normal, and extreme excesses of thyroid secretion can increase the basal metabolic rate to 60 to 100 per cent above normal.
• Thyroid secretion is controlled primarily by thyroid-stimulating hormone (TSH) secreted by the anterior pituitary gland.
• About 93 per cent of the metabolically active hormones secreted by the thyroid gland is thyroxine, and 7 per cent triiodothyronine.
• However, almost all the thyroxine is eventually converted to triiodothyronine in the tissues, so that both are functionally important.
• The functions of these two hormones are qualitatively the same, but they differ in rapidity and intensity of action.
• Triiodothyronine is about four times as potent as thyroxine, but it is present in the blood in much smaller quantities and persists for a much shorter time than does thyroxine
• The thyroid gland is composed of large numbers of closed follicles (100 to 300 micrometers in diameter) filled with a secretory substance called colloid and lined with cuboidal epithelial cells that secrete into the interior of the follicles.
• The major constituent of colloid is the large glycoprotein thyroglobulin, which contains the thyroid hormones within its molecule.
• The thyroid gland has a blood flow about five times the weight of the gland each minute, which is a blood supply as great as that of any other area of the body
• To form normal quantities of thyroxine, about 50 milligrams of ingested iodine in the form of iodides are required each year. The minimum daily iodine intake that will maintain normal thyroid function is 150ủg in adults
Thyroid harmone synthesis and secretion
• Iodine is an essential raw material for thyroid hormone synthesis. Dietary iodide is absorbed by the intestine and enters the circulation.
• The basolateral membranes of thyrocytes facing the capillaries contain a symporter that transports two Na+ ions and one I– ion into the cell with each cycle, against the electrochemical gradient for I–.
• This Na+/I– symporter (NIS) is capable of producing intracellular I– concentrations that are 20 to 40 times as great as the concentration in plasma.
• the interface between the thyrocyte and the colloid, iodide undergoes a process referred to as organification.
• The oxidation and reaction of iodide with the secreted thyroglobulin is mediated by thyroid peroxidase, a membrane-bound enzyme found in the thyrocyte apical membrane.
• The oxidation and reaction of iodide with the secreted thyroglobulin is mediated by thyroid peroxidase, a membrane-bound enzyme found in the thyrocyte apical membrane.
• When there is a need for thyroid hormone secretion, colloid is internalized by the thyrocytes by endocytosis, and directed toward lysosomal degradation.
• Thyrocytes function can be summed-up in this way: they collect and transport iodine, they synthesize thyroglobulin and secrete it into the colloid, they fix iodine to the thyroglobulin to generate thyroid hormones, and they remove the thyroid hormones from thyroglobulin and secrete them into the circulation
•Thyroid hormone synthesis is a multistep process.•There are two theories of how this coupling reaction occurs. One holds that the coupling occurs with both DIT molecules attached to thyroglobulin (intramolecular coupling)•The other holds that the DIT that forms the outer ring is first detached from thyroglobulin (intermolecular coupling•T3 is formed by condensation of MIT with DIT. A small amount of RT3 is also formed, probably by condensation of DIT with MIT.•In the normal human thyroid, the average distribution of iodinated compounds is 23% MIT, 33% DIT, 35% T4, and 7% T3. Only traces of RT3 and other components are present
Regulation and transportation of thyroid harmone
• The plasma proteins that bind thyroid hormones are albumin, a prealbumin called transthyretin (formerly called thyroxine-binding prealbumin), and a globulin known as thyroxine-binding globulin (TBG). Of the three proteins, albumin has the largest capacity to bind T4.
• However, the affinities of the proteins for T4 (ie, the avidity with which they bind T4 under physiologic conditions) are such that most of the circulating T4 is bound to TBG
Mechanism of action
• Thyroid hormones enter cells and T3 binds to thyroid receptors (TR) in the nuclei. T4 can also bind, but not as avidly.
• The hormone-receptor complex then binds to DNA via zinc fingers and increases (or in some cases, decreases) the expression of a variety of different genes that code for proteins that regulate cell function
Calcitonin
• Calcitonin (also known as thyrocalcitonin) is a 32-amino acid linear polypeptide hormone
• Calcitonin was purified in 1962 by Copp and Cheney.• While it was initially considered a secretion of
the parathyroid glands it was later identified as the secretion of the C-cells of the thyroid gland
• It acts to reduce blood calcium , opposing the effects of PTH - Inhibits Ca2+ absorption by the intestines - Inhibits osteoclast activity in bones - Inhibits renal tubular cell reabsorption of Ca2+ allowing it to be excreted in the urine
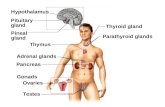
Parathyroid gland• The parathyroid glands are
small, yellowish-brown, ovoid or lentiform structures, usually lying between the posterior lobar borders of the thyroid gland and its capsule
• They are commonly 6 mm long, 3-4 mm across, and 1-2 mm from back to front, each weighing about 50 mg. Usually there are two on each side, superior and inferior.
• The superior parathyroid glands are more constant in location than the inferior and are usually to be found midway along the posterior borders of the thyroid gland, although they may be higher.
• The inferior pair are more variably situated and may be within the fascial thyroid sheath, below the inferior thyroid arteries and near the inferior lobar poles; or outside the sheath, immediately above an inferior thyroid artery; or in the thyroid gland near its inferior pole.
• The superior parathyroids are usually dorsal, the inferior parathyroids ventral, to the recurrent laryngeal nerves.
• The parathyroid glands are very flattened in cross-section and are not normally visible by current imaging methods, including scintigraphy
Development of parathyroid gland
• The third and fourth pouches are characterized at their distal extremity by a dorsal and a ventral wing
• In the fifth week,epithelium of the dorsal wing of the third pouch differentiates into the inferior parathyroidgland, while the ventral wing forms the thymus
• The parathyroid tissue of the third pouch finally comes to rest on the dorsal surface of the thyroid gland and forms the inferior parathyroid gland
• Epithelium of the dorsal wing of the fourth pharyngeal pouch forms the superior parathyroid gland. When the parathyroid gland loses contact with the wall of the pharynx, it attaches itself to the dorsal surface of the caudally migrating thyroid as the superior parathyroid gland
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
• The parathyroid glands have a rich blood supply from the inferior thyroid arteries or from anastomoses between the superior and inferior vessels.
• Approximately one-third of human parathyroid glands have two or more parathyroid arteries.
• Lymph vessels are numerous and associated with those of the thyroid and thymus glands.
INNERVATION
• The nerve supply is sympathetic, either direct from the superior or middle cervical ganglia or via a plexus in the fascia on the posterior lobar aspects.
• Parathyroid activity is controlled by variations in blood calcium level: it is inhibited by a rise and stimulated by a fall.
• The nerves are believed to be vasomotor but not secretomotor
Parathyroid hormones• Parathyroid
hormone (PTH), parathormone or parathyrin, is secreted by the chief cells of the parathyroid glands• It acts to increase the concentration
of calcium (Ca2+) in the blood,• PTH half-life is approximately 4 minutes• tests are used in different clinical situations.• The average PTH level is 10-60 pg/ml.
Synthesis of PTH
• PTH is a linear polypeptide with a molecular weight of 9500 that contains 84 amino acid residues .
• It is synthesized as part of a larger molecule containing 115 amino acid residues (preproPTH).
• On entry of preproPTH into the endoplasmic reticulum, a leader sequence is removed from the amino terminal to form the 90-amino-acid polypeptide proPTH.
• Six additional amino acid residues are removed from the amino terminal of proPTH in the Golgi apparatus, and the 84-amino-acid polypeptide PTH is packaged in secretory granules and released as the main secretory product of the chief cells.
Mechanism of action
• There are at least three different PTH receptors. One binds parathyroid hormone-related protein (PTHrP) and is known as the hPTH/PTHrP receptor.
• A second receptor, PTH2 (hPTH2-R), does not bind PTHrP and is found in the brain, placenta, and pancreas.
• The third receptor, CPTH, which reacts with the carboxyl terminal rather than the amino terminal of PTH.
Regulation of secretion
• Circulating ionized calcium acts directly on the parathyroid glands in a negative feedback fashion to regulate the secretion of PTH.
• The key to this regulation is a cell membrane Ca2+ receptor, CaR.
• Activation of this G-protein coupled receptor leads to inhibition of PTH secretion in parathyroid gland.
• In this way, when the plasma Ca2+ level is high, PTH secretion is inhibited and the Ca2+ is deposited in the bones. When it is low, secretion is increased and Ca2+ is mobilized from the bones
Functions • Parathyroid hormone raises blood Ca by acting on 3 organs: - Bone: main effect- stimulates osteoclasts -> bone breaks down -> Ca released - Intestines: increases uptake of Ca from intestine - Kidney: stimulates reabsorption of Ca from the Ca in kidney tubules • PTH reduces the reabsorption of phosphate from the proximal tubule of the kidney which means more phosphate is excreted through the urine• PTH increases the activity of 1-α-hydroxylase enzyme, which converts 25- hydroxycholecalciferol to 1,25-dihydroxycholecalciferol, the active form of vitamin D.
• Stimulators - Decreased serum Ca2+
- Mild decreases in serum Mg2+
- An increase in serum phosphate • Inhibitors - Increased serum Ca2+
- Severe decreases in serum Mg2+, which also produces symptoms of hypoparathyroidism[
PTHrP
• parathyroid hormone-related protein (PTHrP), is produced by many different tissues in the body.
• It has 140 amino acid residues, compared with 84 in PTH, and is encoded by a gene on human chromosome 12.
• PTHrP and PTH have marked homology at their amino terminal ends and they both bind to the hPTH/ PTHrP receptor, yet their physiologic effects are very different.
• PTHrP has a marked effect on the growth and development of cartilage in utero.
• The hypercalcemia in 80% of the patients with certain malignancy is due to elevated circulating levels of PTHrP (humoral hypercalcemia of malignancy).