All 12084
-
Upload
ingridbach -
Category
Documents
-
view
229 -
download
0
Transcript of All 12084
-
8/13/2019 All 12084
1/12
P O S I T I O N P A P E R
Unexplained recurrent fever: when is autoinflammation
the explanation?
T. Kallinich1,2
, M. Gattorno3
, C. E. Grattan4
, H. D. de Koning5
, C. Traidl-Hoffmann6,7
, E. Feist1,8
,K. Krause1,9, D. Lipsker10, A. A. Navarini11, M. Maurer1,9, H. J. Lachmann12 & A. Simon13
1Autoinflammation Reference Center Charite (ARC), Charite University Medicine Berlin; 2Department of Pediatric Pneumology and
Immunology, Charite University Medicine Berlin, Berlin, Germany; 3UO Pediatria II, G. Gaslini Institute, Genova, Italy; 4St Johns Institute of
Dermatology, St Thomas Hospital, London, UK; 5Department of Dermatology, Radboud University Nijmegen Medical Centre, Nijmegen,
The Netherlands; 6Department of Dermatology and Allergy Biederstein, Technische Universitat, Munich; 7ZAUM Center for Allergy and
Environment, Technische Universitat Munich/Helmholtz Center, Munich; 8Department of Rheumatology and Clinical Immunology, Charite
University Medicine Berlin, Berlin; 9Department of Dermatology and Allergy, Charite University Medicine Berlin, Berlin, Germany; 10Faculte
de Medecine, Universite de Strasbourg et Clinique Dermatologique, Hopitaux universitaires de Strasbourg, Strasbourg, France;11Department of Dermatology, University Hospital of Zurich, Zurich, Switzerland; 12National Amyloidosis Centre, University College London
Medical School, London, UK; 13Department of General Internal Medicine, Nijmegen Institute for Infection, Inflammation and Immunology
(N4i), Centre for Immunodeficiency and Autoinflammation (NCIA), Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands
To cite this article: Kallinich T, Gattorno M, Grattan CE, de Koning HD, Traidl-Hoffmann C, Feist E, Krause K, Lipsker D, Navarini AA, Maurer M, Lachmann HJ,
Simon A. Unexplained recurrent fever: when is autoinflammation the explanation? Allergy2013; 68: 285296.
Keywords
immunology; paediatrics; urticaria.
Correspondence
Dr. Tilmann Kallinich, Charite University
Medicine Berlin, Pediatric Pneumology and
Immunology, Augustenburger Platz 1,
13353 Berlin, Germany.
Tel.: +49-(0)30-450-566182
Fax: +49-(0)30-450-566931
E-mail: [email protected]
Accepted for publication 21 October 2012
DOI:10.1111/all.12084
Edited by: Thomas Bieber
Abstract
Recurrent fever can be the sole or leading manifestation of a variety of dis-
eases including malignancies, autoimmune diseases and infections. Because the
differential diagnoses are manifold, no formal guidelines for the approach of
patients with recurrent fever exists. The newly recognized group of autoinflam-
matory diseases are often accompanied by repetitive fever attacks. As these
episodes are frequently associated by a variety of divergent presentations, the
differentiation of other causes for febrile illnesses can be difficult. In this arti-cle, we first review disease entities, which frequently present with the symptom
of recurrent fever. In a next step, we summarize their characteristic pattern of
disease presentation. Finally, we analyse key features of autoinflammatory dis-
eases, which are helpful to distinguish this group of diseases from the other
causes of recurrent fever. Recognizing these symptom patterns can provide the
crucial clues and, thus, lead to the initiation of targeted specific diagnostic tests
and therapies.
Abbreviations
CANDLE, chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperature; CAPS, cryopyrin-associated periodic
syndrome; CINCA, chronic infantile neurologic cutaneous and articular syndrome; CRP, C-reactive protein; DIRA, deficiency of the interleukin
receptor antagonist; DITRA, deficiency of Interleukin-36 receptor antagonist; HIDS, hyperimmunoglobulinaemia D with periodic fever
syndrome; FCAS, familial cold autoinflammatory syndrome; FUO, fever of unknown origin; FMF, familial Mediterranean fever; IL-1,
interleukin-1; IL-6, interleukin-6; MWS, MuckleWells syndrome; NOMID, neonatal onset multisystem inflammatory syndrome; PDC,
potentially diagnostical clues; PAPA, pyogenic arthritis, pyoderma gangrenosum and acne; PFAPA, periodic fever, aphthous stomatitis,
pharyngitis and adenitis syndrome; SAA, serum amyloid A; soJIA, systemic onset juvenile idiopathic arthritis; TNF-, tumour necrosis factor-;
TRAPS, TNF receptor-associated periodic syndrome.
Allergy68 (2013) 285296 2013 John Wiley & Sons A/S. Published by Blackwell Publishing Ltd 285
Allergy
-
8/13/2019 All 12084
2/12
The rhythmic recurrence of disease is an age-old problem.
It puzzled ancient physicians who supposed the rhythm to
be controlled by cosmic influences
A number of factors suggest a unity of periodic disor-
ders: The cycles and episodes are of similar duration, theyusually are benign, they often begin in childhood, recur
unchanged for decades and heredity occasionally is evident.
There is an overlapping of symptoms and signs in many of
the disorders often great enough at times to confuse classi-
fication (from Periodic Disease (1))
Recurrent fever is common and can be the most promi-
nent symptom of various diseases. The conditions under-
lying recurrent fever are manifold, which is one of the
reasons why no formal guidelines for an evidence-based
approach to its management are currently available. As
individual episodes of recurrent fever are often of short
duration, many patients are symptom free when they are
reviewed by specialists who may come from a variety of
fields (e.g. paediatrics, immunology, rheumatology, infec-
tious diseases, cardiology, haematology and dermatology).
Thus, the evaluation of the patient is often biased
towards the taken history and evidence of chronic damage
rather than acute signs present only during symptomatic
attacks.
Fever is characterized by a nonphysiological increase
in body temperature due to an increased hypothalamic
set point. It often accompanies infections and other
pathological processes, where cytokines [e.g. interleukin-
1 (IL-1), tumour necrosis factor- (TNF-) and inter-
leukin-6 (IL-6)] mediate an increase in the hypothalamic
set point. To achieve a higher core temperature, the bodychanges its own heat production and heat loss mecha-
nisms (2, 3).
No firm definition of recurrent fever is currently estab-
lished. For reasons of practicability, the suggested definition
by Knockaert, who defined recurrent fever by at least two
episodes of fever separated by an (apparently) symptom-free
interval of at least 2 weeks (4), will be applied in this article.
This definition excludes, amongst others, conditions charac-
terized by intermittent fever with fever episodes occurring
with
-
8/13/2019 All 12084
3/12
per year can occur (10). This is by far the most common
reason for recurrent fever in this age group.
In malignancies, a variety of mechanisms, for example, the
production and release of cytokines by necrotic material and
batch-wise growing tumour cells are proposed to induce
recurrent fever (11). Especially in lymphomas and leukaemias,
which often present with B symptoms, elevated levels of the
endogenous pyrogens IL-1and IL-6 were observed (12).
Noninfectious inflammatory diseases are a diverse group of
disorders, of which the autoimmune diseases are the best rec-
ognized. Autoimmune diseases are classically thought to
induce antigen-specific proinflammatory processes, which
subsequently may result in the development of fever. Inter-
mittent courses, especially at disease onset, are frequently
observed, and thus, these diseases have to be considered in
patients with recurrent fever of unknown sources.
This group also comprises the autoinflammatory diseases,
which are the main subject of this article. Autoinflammatory
diseases are characterized by an often unprovoked cytokine-
driven inflammatory process, mediated by cells of the innate
immune system (see Box 1). Clinical features of these diseases
have recently been reviewed in detail (1315). As recurrence
of fever is one hallmark of a subgroup of autoinflammatorysyndromes, this group was also designated as hereditary fever
syndromes (Table 2). Within these diseases, the fever can dif-
fer in terms of type, duration, frequency, periodicity, first
onset, potential triggers and the associated symptoms
(Table 2). This will be discussed in more detail below.
In addition, there are also three other groups recognized in
FUO. These little three comprise benign hyperthermia, fac-
titious fever and drug fever (4).
In benign hyperthermia, the increase in body temperature
is due to an imbalance of heat production and heat loss
mechanisms with no change in the hypothalamic set point.
Thus, it does not fulfil the definition of fever (2). Given that
this condition can be observed frequently even in young chil-
dren, it is an important differential diagnosis in patients with
recurrent temperature increase (16).
Auto- (Munchausen syndrome) or allo-aggression (Mun-
chausen by proxy) can include factitious fever with recurrent
occurrence and thus must be considered in adults and children,
respectively, with recurrent fever of unknown source (17, 18).
Drug fever is an often-overlooked cause for fever; it occurs
as the sole or most prominent feature in about 35% of
adverse events in hospitalized patients (19). Pathophysiologi-
cal mechanisms of drug-induced fever have previously been
reviewed (20). Although drug fever is usually characterized
by a continuous fever, it can be recurrent, especially in multi-
drug using patients.
How to approach recurrent fever patients
Patients with recurrent fever of unknown source are often
difficult to diagnose. The differential diagnoses are manifold,
and therefore, an algorithm covering all possible causes
appears difficult, if not impossible, to construct.
Prospective studies from the Netherlands have provided
valuable lessons in the diagnostic approach to patients with
(nonrecurrent) FUO (21, 22). These studies demonstrated that
a carefully taken history, repeated physical examinations and
a restricted set of investigations can lead to potential diagnos-
tic clues (PDC). These clues include signs, symptoms and
abnormalities, which potentially point towards the underlying
cause and thus guide more specified tests.
In contrast to patients with FUO, the evaluation of patients
with recurrent fever often necessitates a different approach
since: (i) patients often consult a specialist during an attack-free
period, thus signs of acute inflammation might not be present;
(ii) the patient usually has a long history and many previous
diagnostic (and probably therapeutic) attempts have failed toprovide a conclusive explanation for the presented symptoms;
and, most importantly, (iii) episodes may be characterized by a
specific pattern. Recognition of these characteristic patterns
together with a limited number of obligatory investigations pro-
vides relevant clues for the origin of recurrent fever (see below),
which can then guide the choice of specific diagnostic tests.
Pattern recognition in recurrent fever of unknown
origin
Asking the right questions can identify patterns of recurrent
fever manifestations. The following list of questions will sup-
port a systematic approach to the differential diagnosis.
1 At what age did symptoms first appear?
2 What is the duration of the individual fever episodes?
3 What other symptoms are associated with the fever episodes?
4 What is the time interval between episodes (duration,
variable or fixed intervals)?
5 What can trigger or alleviate a fever episode?
6 How have symptoms developed over time?
7 Which treatments have been used and what was the
response?
8 Is there a family history; does the patient originate from
a certain ethnicity?
Table 1 Disease groups causing recurrent fever
Mechanism
Big three Little three Miscellaneous
Inflammatory,
infectious Inflammatory, noninfectious
Mostly
inflammatory
Mostly noninflammatory,
mostly no fever per definition
Various
mechanisms
Disease(groups)
Infections Autoimmunediseases
Autoinflammatorydisease
Malignancies Munchausen(by proxy)
Drugfever
Benignhyperthermia
E.g. central fever,dehydration
Groups of inflammatory and noninflammatory conditions potentially leading to recurrent fever.
Allergy68 (2013) 285296 2013 John Wiley & Sons A/S. Published by Blackwell Publishing Ltd 287
Kallinich et al. Autoinflammation causes recurrent fever
-
8/13/2019 All 12084
4/12
Table 2 Characteristics of autoinflammatory syndromes with recurrent fever
Disease Gene
Three main
associated findings
Fever
Onset Duration
FMF MEFV Peritonitis
ArthritisPleuritis
First years of life 1272 h
HIDS MVK (mevalonate kinase) Lymphadenopathy
Arthralgias
Abdominal symptoms
First year of life 37 days
CAPS FCAS NLRP3/CIAS1 Cold-induced urticarial rash
Arthralgias
Conjunctivitis
First year of life Median 12 h
MWS Urticarial rash
Sensorineural hearing loss
Amyloidosis
Childhood If present 23 days
NOMID Neonatal onset exanthema
Neurologic symptoms
Arthropathy with exostosis
Neonatal If present varying
duration
TRAPS TNFRSF1A Migrating exanthemas
and myalgias
Periorbital oedema
and conjunctivitis
Peritonitis
First years of life Daysweeks
CANDLE (83, 84) PSMB8 Atypical neutrophilic dermatosis
Lipodystrophy
Delayed physical development
First weeks
to month of life
Daily high frequent
recurrent fever
DITRA (8588) IL36RN Generalized pustular psoriasis
General malaise
Hyperleucocytosis
Variable Variable
NLPR12-
associated
periodic fever
syndrome (89, 90)
NLRP12 Cold-induced episodes
Arthralgias
Urticarial rash
First year of life 210 days
Schnitzlers
syndrome
None Urticarial rash
IgM or IgG paraproteinemia
Bone pain
>50 years Mostly 13, but
varying
PFAPA None Aphthous ulcer
Cervical adenitis
(Sterile) pharyngitis
Median 4th year of life Median 4 days
soJIA None Arthritis
Rash
Serositis, lymphadenopathy,
organomegaly
75% before 10th year
of life
Weeks
AOSD None Arthralgias
Rash
Sore throat, lymphadenopathy,
splenomegaly
75% before 50th year
of life
Weeks
FMF, familial Mediterranean fever; HIDS, hyperimmunoglobulinaemia D with periodic fever syndrome (Mevalonate kinase deficiency); CAPS,
cryopyrin-associated periodic syndrome; FCAS, familial cold autoinflammatory syndrome; MWS, MuckleWells syndrome; NOMID, neonatal
onset multisystem inflammatory syndrome; TRAPS, TNF receptor-associated periodic syndrome; CANDLE, chronic atypical neutrophilic der-
matosis with lipodystrophy and elevated temperature; DITRA, deficiency of interleukin-36 receptor antagonist; PFAPA, periodic fever, apht-
hous stomatitis, pharyngitis and adenitis syndrome; soJIA, systemic onset juvenile idiopathic arthritis; AOSD, adult onset Stills disease;
DIRA, deficiency of the interleukin 1 (IL-1) receptor antagonist; PAPA, pyogenic arthritis, pyoderma gangrenosum and acne.
Only single cases of patients with CANDLE-, DITRA- and NLRP12-associated fever syndrome were described in the literature. These three
diseases are not discussed in detail in the text. Autoinflammatory syndromes not typically associated with recurrent fever (e.g. DIRA, PAPA)
are not mentioned in the table.
FCAS, MWS and NOMID show many phenotypical overlaps and are all caused by mutations in the NLRP3gene (cyropyrin), and thus these
entities are combined as CAPS.
Allergy68 (2013) 285296 2013 John Wiley & Sons A/S. Published by Blackwell Publishing Ltd288
Autoinflammation causes recurrent fever Kallinich et al.
-
8/13/2019 All 12084
5/12
At what age did symptoms first appear?
In the young child, recurrent fever episodes are most likely
caused by the physiological susceptibility to infections. Usu-
ally signs of minor infections accompany these episodes; the
recurrent symptoms resolve during the first year of life with-
out any sequelae (Fig. 1A) (10). Febrile episodes in patients
with an inherited immunodeficiency usually also manifest
first in the (very) young child, but they are frequently
accompanied by severe infections not uncommonly caused
by opportunistic pathogens. Nonetheless, approximately20% of cases of primary immunodeficiency are diagnosed in
adulthood (23). In children, malignant disease, particularly
leukaemias [which are known to induce the synthesis of
pyrogenic interleukins (12)], neuroblastoma, retinoblastoma
and renal tumour, is most prevalent in the under 4-year-old
age group; after the 10th year of life, the prevalence of
malignancy then increases during the whole life span (24,
25). In childhood and early adulthood, systemic lupus
erythematosus is a common autoimmune disease accompa-
nied by fever; in later adulthood different systemic vasculiti-
des, for example, polymyalgia rheumatica also frequently
present with fever.
Most autoinflammatory diseases first manifest during early
childhood. But late onset of symptoms, in adolescence or
later, is seen in some patients (2630).
What is the duration of individual fever episodes?
Although the length of a single febrile episode can vary
between and within individuals, fever duration can be
helpful in pattern recognition. In patients with physio-logical susceptibility to infections, fever episodes are
generally short (35 days) and also depend on the dis-
ease-causing infectious agents. In contrast, fever episodes
in patients with immune deficiencies, autoimmune dis-
eases and malignancies are usually of a longer duration
(Fig. 2A).
Although autoinflammation can produce fever of almost
any duration, individual autoinflammatory disorders are
often associated with inflammatory episodes of characteristic
durations (see next section).
Ca
tegories
Specific
diseases
Physiologic susceptibility
of infections
Immunodeficiency
Malignancy
Autoimmune diseases
Years
Cyclic neutropenia
PFAPA
FMF
HIDS
FCAS
Muckle Wells Syndrome
NOMID/CINCA
TRAPS
Schnitzlers Syndrome
Systemic juvenile idiopathic
arthritis/Adults onset Stills disease
0 1 10 20 30 40 50 60 70 80
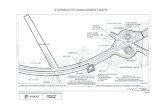
Figure 1 Age of disease onset. Age distribution of disease onset
according to disease groups (A) and specific diseases (B). Red
symbolizes likely, yellow possible and blue unlikely age of disease
manifestation. Systemic lupus erythematosus, dermatomyositis
and polymyositis, mixed connective tissue disease and polymyalgia
rheumatica are summarized as autoimmune diseases. Cyclic neu-
tropenia is included, because it is a rare but important immunodefi-
ciency, which mimics periodic fever syndromes and periodic fever,
aphthous stomatitis, pharyngitis and adenitis syndrome (PFAPA).
Allergy68 (2013) 285296 2013 John Wiley & Sons A/S. Published by Blackwell Publishing Ltd 289
Kallinich et al. Autoinflammation causes recurrent fever
-
8/13/2019 All 12084
6/12
What other symptoms are associated with the fever episodes?
As shown in Fig. 3A, a variety of associated symptoms can be
helpful in classifying different disease groups. Recurrent minor
infections are usually associated with mild symptoms only;
malignancies are often accompanied by the occurrence of B
symptoms (besides fever weight loss, night sweats); and autoim-
mune diseases frequently involve multiple organs. Accompanying
symptoms can also point to certain autoinflammatory disorders.
What is the time interval between episodes (duration,
variable or fixed intervals)?
Usually, febrile episodes occur with varying time intervals
and are rather episodic than strictly periodic. Only rarely the
time interval is fixed, meaning that the symptom-free periods
are always of the same length. This phenomenon is usually
only observed in patients with cyclic neutropenia (31, 32) or
with periodic fever, aphthous stomatitis, pharyngitis and ade-
nitis (PFAPA) syndrome (33, 34).
It is also important to ask whether patients are completely
symptom free between the febrile episodes, or whether some
symptoms persist. Persistent symptoms are more likely in
case of malignancy or autoimmune disease. In many autoin-
flammatory diseases, patients can be completely symptom
free in the intervals, although in some diseases, symptomsmay persist.
What can trigger or alleviate a fever episode?
This question can be helpful in the identification of many dis-
eases and is especially important in patients with recurrent
infections or drug-induced fever.
How have symptoms developed over time?
A general worsening of the symptoms over time with an
increasing number of organ systems affected and generally
reduced well-being are more likely in autoimmune diseases or
malignancies. Although organ damage can eventually develop
over time in autoinflammatory diseases, the symptom com-
plex accompanying the febrile attacks remains usually fairly
constant.
Which treatments have been used and what was the
response?
Here, the response to antibiotics as well as anti-inflammatory
and immunosuppressant therapy is of special interest and
should be meticulously enquired about.
Ca
tegories
Specific
diseases
Physiologic susceptibilityof infections
Immunodeficiency
Malignancy
Autoimmune diseases
Cyclic neutropenia
PFAPA
FMF
HIDS
FCAS
0 1 2 3 4 5 6 7 14 28
Muckle Wells Syndrome
NOMID/CINCA
TRAPS
Schnitzlers Syndrome
Days
Systemic juvenile idiopathic
arthritis/Adults onset Stills disease
Figure 2 Duration of fever attack. Average duration of febrile attacks according to disease groups (A) and specific diseases (B). The colours
symbolize the likelihood as described in Fig. 1.
Allergy68 (2013) 285296 2013 John Wiley & Sons A/S. Published by Blackwell Publishing Ltd290
Autoinflammation causes recurrent fever Kallinich et al.
-
8/13/2019 All 12084
7/12
Is there a family history; does the patient originate from a
certain ethnicity?
Recessive and dominant inheritance is well recognized in immune
deficiencies and autoinflammatory diseases. Autoinflammatory
disease especially segregates in certain ethnicities (see below).
Distinguishing between the different autoinflammatory
diseases using the above questions
The recognition of a pattern can be the first and most impor-
tant step to suspect and, later on, to diagnose an autoinflam-matory disease.
First onset of symptoms is in early childhood
In 90% of patients, symptoms of Familial Mediterranean
fever (FMF) start before the age of 20, in 75%, first symp-
toms are present before the age of 10 (35) (Fig. 1A).
The age of onset in cryopyrin-associated periodic syn-
dromes (CAPS) depends on the phenotype: per definition first
symptoms of neonatal onset multisystem inflammatory
disease (NOMID) also known as chronic infantile neuro-
logic cutaneous and articular syndrome (CINCA) start in
the neonatal period, but recurrent fever episodes may not be
the dominant feature. In 60% of cases, fever in patients with
familial cold autoinflammatory syndrome (FCAS) manifests
during the first days of life, and in nearly all patients, first
symptoms are present during the first half year (36, 37)
Nearly 90% of MuckleWells syndrome (MWS) cases present
in infancy (30, 38). Febrile symptoms of hyperimmunoglobu-
linaemia D with periodic fever syndrome (HIDS) also start
in early childhood, on average around the 6th month of life,
and disease onset during the first weeks of life has beenreported (39). Although first symptoms of TNF receptor-
associated periodic syndrome (TRAPS) occur at a mean age
of 3 years, first manifestations can occur anytime between
the neonatal period and adulthood (29). Periodic fever, apht-
hous stomatitis, pharyngitis and adenitis syndrome syndrome
patients usually exhibit first symptoms before their 5th birth-
day with a wide range of disease onset (1/412 years) (40).
Seventy-five per cent of patients with soJIA have their first
symptoms before the 10th year of age. Adult onset Stills dis-
ease (AOSD) is usually manifests during young adulthood
Categories
Specificdise
ases
Physiologic susceptibility
of infections
Immunodeficiency
Malignancy
Autoimmune diseases
Cyclic neutropenia
PFAPA
FMF
HIDS
FCAS
Muckle Wells Syndrome
NOMID/CINCA
TRAPS
Schnitzler s Syndrome
Systemic juvenile idiopathic
arthritis/Adults onset Stills disease
Figure 3 Associated symptoms according to disease groups (A) and specific diseases (B). The colours symbolize the likelihood as described
in Fig. 1.
Allergy68 (2013) 285296 2013 John Wiley & Sons A/S. Published by Blackwell Publishing Ltd 291
Kallinich et al. Autoinflammation causes recurrent fever
-
8/13/2019 All 12084
8/12
(75% below the 50th year of age). Schnitzlers Syndrome is a
classical example of an autoinflammatory disease character-
ized by recurrent fever, which only manifests in adulthood
(mean age of onset is 50 years) (41).
Duration of fever episode
In FMF, a main diagnostic criterion is the recurrence of
short attacks with a duration of 1272 h (42) (Fig. 2B). Short
episodes are also observed in FCAS with a mean duration of
12 h and a range of 1/272 h (36). In HIDS and PFAPA,
longer episodes of about 37 days are more common (33, 34,
43). In TRAPS, episodes frequently last for up to 3 weeks.
Here, associated fever is only present during the first days
and can be absent, particularly in adult patients (29). In
patients with MWS and NOMID, the length of symptomatic
episodes can vary, and fever is not found consistently. In
Schnitzlers, syndrome, recurrent fever is commonly present
for 13 days, but the pattern is variable (41). In soJIA and
AOSD, fever episodes usually continue to occur for several
weeks.
Accompanying symptoms
Familial Mediterranean fever is generally associated with a
rather limited but specific combination of symptoms caused
by serositis at different sites (peritonitis, pleurisy and arthri-
tis). In other autoinflammatory conditions, specific symptoms
and signs, such as sensorineural hearing loss in CAPS, migra-
tory myalgia in TRAPS, headache, mental retardation and
arthropathy with exostosis in CINCA/NOMID, can be
important diagnostic markers (Fig. 3C and Table 2). In so-
JIA and AOSD fever, the typical transient salmon-pink col-
oured rash can be the crucial diagnostic hint.
Time interval between fever episodes
Cyclic neutropenia (31, 32) or a PFAPA syndrome should be
considered when symptom-free periods are (almost) always
of the same length (33, 34). Whereas young children with
PFAPA often experience attacks every 34 weeks, adults
with persistent symptoms experience fewer attacks (33, 34,
44). A high frequency of attacks, for example every other
week, can be seen in FMF, but patients with symptom-free
intervals of years or even no (febrile) symptoms have also
been described (phenotype II FMF) (35, 45). In patients with
other autoinflammatory diseases, attacks usually occur at
longer time intervals and the frequency may also be influ-
enced by the presence of triggering factors.
Specific triggers are characteristic for certain
autoinflammatory diseases
In general, in all autoinflammatory disorders, inflammatory
episodes can be precipitated by emotional stress, exercise and
(minor) infections, as well as fatigue (29, 39, 43). Female
patients often notice a relationship with their menstrual cycle,
and characteristically, fever episodes in most of the autoin-
flammatory disorders occur less frequently during pregnancy,
but delivery often provokes an attack (46).
Some triggers may be more disease specific. Most impor-
tantly, cold can trigger symptoms in FCAS and MWS
patients (36, 47). Fever episodes triggered by active immuni-
zation are frequently observed in HIDS (39, 43).
Current data derived from comprehensive biochemicalanalyses in PFAPA patients suggest that exposure to envi-
ronmental agents, for example otherwise not pathogenic bac-
teria or viruses or parts of them, induces inappropriate
inflammatory responses leading to recurrent febrile episodes
in PFAPA patients (48).
Development of symptoms over time
The course of the disease should be analysed from two different
perspectives: (i) the characteristics and frequency of individual
attacks and (ii) the development of long-term consequences.
Young children with FMF often present with signs of recur-
rent fever only, and other typical features of the disease such a
relapsing serositis appear as they get older (49). In HIDS, a sig-
nificant decrease in attack frequency with increasing age is
observed, although attack frequency often increases just after
adolescence (39). Fever is a typical symptom in children with
TRAPS but may be absent during attacks in adults (29). Long-
term follow-up of children with PFAPA showed that most
patients improve over time and eventually show complete remis-
sion with a mean duration of disease of 6 years. In patients with
long disease duration, the frequency of febrile episodes
decreased significantly overtime (44). For the group of CAPS,
for example, FCAS, MWS and NOMID, no synoptic data on
age-related characteristics of the single episodes are available,
but in general, acute symptoms seem not to differ over time.
All (untreated) monogenic autoinflammatory fever syn-dromes are associated with the development of AA amyloi-
dosis, although the prevalence varies from very rare [in
FCAS and HIDS (34, 37)], 14% in TRAPS (50), 25% in
FMF (45) to approximately 30% in MWS (51). There are no
reported cases in NOMID, presumably because before mod-
ern treatment few patients lived long enough to develop this
complication. Cryopyrin-associated periodic syndrome-associ-
ated long-term consequences include sensorineural hearing
loss in MWS and NOMID and visual loss and meningitic
headaches as well as arthropathy with exostosis in NOMID
(Table 2). These specific symptoms can be the crucial hint in
making the right diagnosis.
Response to treatment
Inefficacy of antibiotics is often a clear clue for an autoin-
flammatory aetiology. Steroids will have some benefit in
many of the autoinflammatory diseases, although in general
it is only very effective in PFAPA, soJIA and AOSD and to
a lesser extent in HIDS (33, 34). Steroids have no beneficial
effects in classical FMF attacks (45). Response to adequate
colchicine therapy can confirm FMF (52). In many autoin-
flammatory disorders, specific IL-1 inhibitors induce dramatic
and complete resolution of signs and symptoms (5356).
Allergy68 (2013) 285296 2013 John Wiley & Sons A/S. Published by Blackwell Publishing Ltd292
Autoinflammation causes recurrent fever Kallinich et al.
-
8/13/2019 All 12084
9/12
Family history and ethnicity
Familial Mediterranean fever should be especially considered
in patients originating from countries of the eastern Mediter-
ranean basin, for example Israel, Turkey and Armenia (57),
but it also can occur in patients from other ethnicities (58,
59). Hyperimmunoglobulinaemia D with periodic fever syn-
drome is most prevalent in the Netherlands, Italy and
France. The majority of patients from other countries were
European or from European ancestry, but this may be likely
an ascertainment bias, reflecting the availability of diagnostic
testing (39). The other monogenic autoinflammatory diseases
can be found in patients from all over the world.
A family history may reveal the inheritance pattern, which
will point towards the right diagnosis. But a number of
aspects are important: (i) the disease penetrance may vary,
that is, not all mutation carriers are affected, (ii) especially in
NOMID, many patients harbour a de novo-mutation, thus no
other family member is affected (60) and (iii) there may be
variable expressivity, that is, individuals may present with
different symptoms of varying severity at a variable age ofonset, and milder disease presenting later may be missed in a
routinely taken history.
Next diagnostic steps if an autoinflammatory
syndrome is suspected
Acute phase response
In autoinflammatory diseases, inflammatory febrile episodes
are always accompanied by elevated levels of hepatic acute
phase proteins and leucocytosis. Subclinical inflammatory
responses can be detected in the symptom-free intervals in
many instances (6163). Signs of chronic inflammation, for
example organomegaly, growth retardation or chronic anae-mia, can occur. The discrepancy between highly elevated C-
reactive protein (CRP) and low to normal procalcitonin is
characteristic for PFAPA and FMF (64, 65). The phagocyte-
specific danger signals S100A8/9 and S100A12 are sensitive
biomarkers for the detection of (subclinical) inflammation in
patients with FMF, soJIA and CAPS; in certain circum-
stances, they might be superior to classically used markers
(66, 67). Ferritin levels are especially helpful in diagnosing
patients with soJIA and AOSD. Greatly elevated levels may
point to the life-threatening complication of a macrophage
activation syndrome.
Specific biochemistry markers
Slight increases in IgD serum concentrations can be found in
a number of autoinflammatory disorders as well as other
inflammatory diseases. Serum IgD levels in HIDS can be
markedly increased (34, 39, 40, 68). Other biomarkers, for
example, mevalonic acid activity and levels in the urine of
patients with HIDS, the production of IL-1 by cultured
monocytes in CAPS (69) and the serum level of soluble TNF
receptor 1 in TRAPS (70), are not generally available and
are performed mainly for research purposes. In Schnitzlers
syndrome, an IgM paraprotein is typically present (41).
Genetics
Molecular genetic diagnostic testing can confirm autoinflam-
matory disease (Table 2). A diagnostic flow chart for a
rational application of this cost-intensive approach has been
published (71).
Nonetheless, genetic tests must be interpreted in context,and a variety of issues should be considered when using
genetic analyses to diagnose autoinflammatory diseases:
1 Up to 20% of patients with FMF do not exhibit two
mutations within the MEFVgene (72, 73), but their clini-
cal course resembles that of patients with a combined het-
erozygous or homozygous mutations (74). On the other
hand, in certain ethnic groups, most subjects with two
mutations within the MEFVgene do not suffer from clin-
ical FMF (phenotype III FMF) (75, 76).
Another challenge in the interpretation of genetic results
are the occurrences of polymorphisms, especially of the
amino acid exchange at MEFV position 148 (77). Thus,
the diagnosis of FMF is still based on clinical grounds
(42); but the genetic analysis can have a significant value
in the confirmation of the suspected diagnosis and may
allow a prediction on the disease course (78).
2 In patients with CAPS, the frequency of a negative
genetic analysis of the NLRP3 gene varies according to
the subtype: in FCAS up to 10%, in MWS up to 25%
and in NOMID up to 50% of patients do not exhibit
mutations despite a characteristic clinical phenotype (60,
79).
3 TRAPS is defined as a disease caused by mutations
within the TNFRSF1A gene (70). Low-penetrance poly-
morphisms (R92Q or P46L) are usually of no clinical sig-
nificance, although R92Q is sometimes associated with a
milder disease phenotype, which responds to less intensivetreatments (80).
4 A definite diagnosis of mevalonate kinase deficiency or
HIDS can be established when the mevalonate kinase
deficiency is present. This can be determined directly by
biochemical testing (raised mevalonic acid in the urine
during a fever episode) or by genetic testing of the meval-
onate kinase gene (81). The most prevalent mutations are
V377I and I268T.
5 Like in FMF, patients exhibiting (some) clinical charac-
teristics for TRAPS and HIDS but with no mutations in
the relevant gene have been described (47, 82). It is cur-
rently a matter of debate whether these patients should
correctly be classified as autoinflammatory disorder not
otherwise specified.
Conclusions
The underlying causes of recurrent fever are manifold, and
their identification is challenging. Autoinflammatory disor-
ders often present with recurrent febrile attacks and conse-
quently have to be considered when evaluating a patient with
such a history of fever. Recognizing symptom patterns can
provide crucial clues and, thus, lead to the initiation of tar-
geted specific diagnostic tests and therapies.
Allergy68 (2013) 285296 2013 John Wiley & Sons A/S. Published by Blackwell Publishing Ltd 293
Kallinich et al. Autoinflammation causes recurrent fever
-
8/13/2019 All 12084
10/12
Acknowledgment
We thank Nicole Klameth for excellent technical assistance
in generating the figures.
Authors contribution
All authors took part at the EAACI task force meeting on
autoinflammatory disease held January 2011 in Berlin and
were involved in the manuscript preparation.
Conflict of interest
None.
Supporting Information
Additional Supporting Information may be found in the
online version of this article:
Appendix S1. Box 2: Infectious diseases causing recurrent
fever in immunocompetent individuals.
References
1. Reimann HA. Periodic disease.Medicine
(Baltimore)1951;30:219245.
2. Dinarello CA, Gelfand JA. Harrisons Prin-
ciples of Internal Medicine. New York:
McGraw-Hill Publ. Co., 1998; 8490.
3. Kluger MJ, Bartfai T, Dinarello CA. New
York Academy of Sciences & Lovelace
Respiratory Research Institute. Molecular
Mechanisms of Fever. New York Academyof Sciences, 1998.
4. Knockaert DC. Recurrent fevers of
unknown origin. Infect Dis Clin North Am
2007;21:11891211.
5. Kastner DL, Aksentijevich I, Goldbach-
Mansky R. Autoinflammatory disease
reloaded: a clinical perspective. Cell
2010;140:784790.
6. Ryan ME, Ferrigno K, OBoyle T, Long SS.
Periodic fever and skin lesions caused by
disseminated Mycobacterium chelonae infec-
tion in an immunocompetent child. Pediatr
Infect Dis J1996;15:270272.
7. Lekstrom-Himes JA, Dale JK, Kingma DW,
Diaz PS, Jaffe ES, Straus SE. Periodicillness associated with EpsteinBarr virus
infection. Clin Infect Dis 1996;22:2227.
8. Cogswell FB. The hypnozoite and relapse in
primate malaria. Clin Microbiol Rev
1992;5:2635.
9. Notarangelo LD, Fischer A, Geha RS,
Casanova JL, Chapel H, Conley ME et al.
Primary immunodeficiencies: 2009 update.
J Allergy Clin Immunol 2009;124:
11611178.
10. Gruber C, Keil T, Kulig M, Roll S, Wahn
U, Wahn V. History of respiratory infections
in the first 12 yr among children from a
birth cohort. Pediatr Allergy Immunol
2008;19:505512.
11. Johnson M. Neoplastic fever. Palliat Med
1996;10:217224.
12. Kurzrock R. Cytokine deregulation in cancer.
Biomed Pharmacother2001;55:543547.
13. Henderson C, Goldbach-Mansky R. Mono-
genic autoinflammatory diseases: new
insights into clinical aspects and pathogene-
sis. Curr Opin Rheumatol2010;22:567578.
14. Gattorno M, Federici S, Pelagatti MA, Caorsi
R, Brisca G, Malattia C et al. Diagnosis and
management of autoinflammatory diseases in
childhood.J Clin Immunol2008;28(Suppl 1):
S73S83.
15. Masters SL, Simon A, Aksentijevich I,
Kastner DL. Horror autoinflammaticus: the
molecular pathophysiology of autoinflamma-
tory disease (*). Annu Rev Immunol
2009;27:621668.
16. Kallinich T, Keitzer R, Puskas E, Boldt F.
Exercise-induced hyperthermia in childhood:a case report and pilot study. Acta Paediatr
2009;98:12171219.
17. Trejo-Hernandez J, Loredo-Abdala A,
Orozco-Garibay JM. Munchausen syndrome
by proxy in Mexican children: medical,
social, psychological and legal aspects. Rev
Invest Clin 2011;63:253262.
18. Zenone T. Fever of unknown origin in adults:
evaluation of 144 cases in a non-university
hospital.Scand J Infect Dis2006;38:632638.
19. Roush MK, Nelson KM. Understanding
drug-induced febrile reactions. Am Pharm
1993;33:3942.
20. Patel RA, Gallagher JC. Drug fever.Phar-
macotherapy2010;30:5769.21. de Kleijn EM, van Lier HJ, van der Meer
JW. Fever of unknown origin (FUO) II.
Diagnostic procedures in a prospective
multicenter study of 167 patients. The
Netherlands FUO Study Group. Medicine
(Baltimore)1997;76:401414.
22. Bleeker-Rovers CP, Vos FJ, de Kleijn EM,
Mudde AH, Dofferhoff TS, Richter C et al.
A prospective multicenter study on fever of
unknown origin: the yield of a structured
diagnostic protocol. Medicine (Baltimore)
2007;86:2638.
23. Gathmann B, Grimbacher B, Beaute J,
Dudoit Y, Mahlaoui N, Fischer A et al. The
European internet-based patient and
research database for primary immunodefi-
ciencies: results 20062008.Clin Exp Immu-
nol2009;157(Suppl 1):311.
24. Magnani C, Gatta G, Corazziari I, Kramar-
ova E, Pastore G, Viscomi S et al. Childhood
malignancies in the EUROCARE study: the
database and the methods of survival analy-
sis. Eur J Cancer 2001;37:678686.
25. Robert Koch-Institut. Zentrum fur
Krebsregisterdaten, Krebs in Deutschland
2007/2008. http://www.gekid.de/, 2012.
26. Kumpfel T, Hoffmann LA, Rubsamen H,
Pollmann W, Feneberg W, Hohlfeld R et al.
Late-onset tumor necrosis factor receptor-
associated periodic syndrome in multiple
sclerosis patients carrying the TNFRSF1A
R92Q mutation. Arthritis Rheum
2007;56:27742783.
27. Tamir N, Langevitz P, Zemer D, Pras E,
Shinar Y, Padeh S et al. Late-onset familialMediterranean fever (FMF): a subset with
distinct clinical, demographic, and molecular
genetic characteristics. Am J Med Genet
1999;87:3035.
28. Savage T, Loftus BG, Tormey V,
McDermott MF, Moylett E. Tumor necrosis
factor receptor-associated periodic syndrome
(TRAPS) or familial Hibernian fever:
presentation in a four-day-old infant.J Clin
Rheumatol2008;14:342345.
29. Hull KM, Drewe E, Aksentijevich I, Singh
HK, Wong K, McDermott EM et al. The
TNF receptor-associated periodic syndrome
(TRAPS): emerging concepts of an autoin-
flammatory disorder. Medicine (Baltimore)2002;81:349368.
30. Leslie KS, Lachmann HJ, Bruning E,
McGrath JA, Bybee A, Gallimore JR et al.
Phenotype, genotype, and sustained response
to anakinra in 22 patients with autoinflam-
matory disease associated with CIAS-1/
NALP3 mutations. Arch Dermatol
2006;142:15911597.
31. Dale DC, Hammond WPT. Cyclic neutrope-
nia: a clinical review. Blood Rev 1988;2:178
185.
32. Dale DC, Bolyard AA, Aprikyan A. Cyclic
neutropenia. Semin Hematol 2002;39:8994.
33. Thomas KT, Feder HM Jr, Lawton AR,
Edwards KM. Periodic fever syndrome in
children. J Pediatr 1999;135:1521.
34. Padeh S, Brezniak N, Zemer D, Pras E,
Livneh A, Langevitz P et al. Periodic fever,
aphthous stomatitis, pharyngitis, and ade-
nopathy syndrome: clinical characteristics
and outcome. J Pediatr 1999;135:98101.
35. Samuels J, Aksentijevich I, Torosyan Y,
Centola M, Deng Z, Sood R et al. Familial
Mediterranean fever at the millennium
clinical spectrum, ancient mutations, and a
survey of 100 American referrals to the
Allergy68 (2013) 285296 2013 John Wiley & Sons A/S. Published by Blackwell Publishing Ltd294
Autoinflammation causes recurrent fever Kallinich et al.
-
8/13/2019 All 12084
11/12
National Institutes of Health.Medicine
(Baltimore) 1998;77:268297.
36. Hoffman HM, Wanderer AA, Broide DH.
Familial cold autoinflammatory syndrome:
phenotype and genotype of an autosomal
dominant periodic fever. J Allergy Clin
Immunol2001;108:615620.
37. Stych B, Dobrovolny D. Familial cold auto-
inflammatory syndrome (FCAS): character-
ization of symptomatology and impact on
patients lives. Curr Med Res Opin
2008;24:15771582.
38. Muckle TJ, Wells M. Urticaria, deafness,
and amyloidosis: a new heredo-familial
syndrome. Q J Med 1962;31:235248.
39. van der Hilst JC, Bodar EJ, Barron KS,
Frenkel J, Drenth JP, van der Meer JW
et al. Long-term follow-up, clinical features,
and quality of life in a series of 103 patients
with hyperimmunoglobulinemia D
syndrome. Medicine (Baltimore) 2008;87:301
310.
40. Feder HM, Salazar JC. A clinical review
of 105 patients with PFAPA (a periodic
fever syndrome). Acta Paediatr 2010;99:
178184.
41. de Koning HD, Bodar EJ, van der Meer
JW, Simon A. Schnitzler syndrome: beyond
the case reports: review and follow-up of 94
patients with an emphasis on prognosis and
treatment. Semin Arthritis Rheum
2007;37:137148.
42. Livneh A, Langevitz P, Zemer D, Zaks N,
Kees S, Lidar T et al. Criteria for the diag-
nosis of familial Mediterranean fever. Arthri-
tis Rheum 1997;40:18791885.
43. Drenth JP, Haagsma CJ, van der Meer JW.
Hyperimmunoglobulinemia D and periodic
fever syndrome the clinical spectrum in a
series of 50 patients. International Hyper-
IgD Study Group. Medicine (Baltimore)
1994;73:133144.
44. Wurster VM, Carlucci JG, Feder HM Jr,
Edwards KM. Long-term follow-up of chil-
dren with periodic fever, aphthous stomati-
tis, pharyngitis, and cervical adenitis
syndrome. J Pediatr 2011;159:958964.
45. Sohar E, Gafni J, Pras M, Heller H. Famil-
ial Mediterranean fever. A survey of 470
cases and review of the literature. Am J Med
1967;43:227253.
46. Akar S, Soyturk M, Onen F, Tunca M. The
relations between attacks and menstrual peri-
ods and pregnancies of familial Mediterranean
fever patients.Rheumatol Int2006;26:676679.
47. Aganna E, Hammond L, Hawkins PN,
Aldea A, McKee SA, van Amstel HK et al.
Heterogeneity among patients with tumor
necrosis factor receptor-associated periodic
syndrome phenotypes. Arthritis Rheum
2003;48:26322644.
48. Stojanov S, Lapidus S, Chitkara P, Feder H,
Salazar JC, Fleisher TA et al. Periodic fever,
aphthous stomatitis, pharyngitis, and adeni-
tis (PFAPA) is a disorder of innate immu-
nity and Th1 activation responsive to IL-1
blockade. Proc Natl Acad Sci USA
2011;108:71487153.
49. Padeh S, Livneh A, Pras E, Shinar Y, Lidar
M, Feld O et al. Familial Mediterranean
fever in the first two years of life: a unique
phenotype of disease in evolution. J Pediatr
2010;156:985989.
50. Aksentijevich I, Galon J, Soares M, Mans-
field E, Hull K, Oh HH et al. The tumor-
necrosis-factor receptor-associated periodic
syndrome: new mutations in TNFRSF1A,
ancestral origins, genotype-phenotype stud-
ies, and evidence for further genetic hetero-
geneity of periodic fevers. Am J Hum Genet
2001;69:301314.
51. Muckle TJ. The MuckleWells syndrome.
Br J Dermatol 1979;100:8792.
52. Kallinich T, Haffner D, Niehues T, Huss K,
Lainka E, Neudorf U et al. Colchicine use
in children and adolescents with familial
Mediterranean fever: literature review and
consensus statement. Pediatrics 2007;119:
e474e483.
53. Goldbach-Mansky R, Dailey NJ, Canna
SW, Gelabert A, Jones J, Rubin BI et al.
Neonatal-onset multisystem inflammatory
disease responsive to interleukin-1beta inhi-
bition. N Engl J Med2006;355:581592.
54. Bodar EJ, Kuijk LM, Drenth JP, van der
Meer JW, Simon A, Frenkel J. On-demand
anakinra treatment is effective in mevalonate
kinase deficiency. Ann Rheum Dis
2011;70:21552158.
55. Gattorno M, Pelagatti MA, Meini A, Obici
L, Barcellona R, Federici S et al. Persistent
efficacy of anakinra in patients with tumor
necrosis factor receptor-associated periodic
syndrome. Arthritis Rheum 2008;58:1516
1520.
56. Hashkes PJ, Spalding SJ, Giannini EH,
Huang B, Johnson A, Park G et al. Rilona-
cept for colchicine-resistant or -intolerant
familial Mediterranean Fever: a randomized
trial. Ann Internal Med 2012;157:533541.
57. Ben-Chetrit E, Levy M. Familial Mediterra-
nean fever. Lancet 1998;351:659664.
58. Stewart L, Tolmie J, Galea P, Touitou I.
Familial Mediterranean fever in a cold cli-
mate: read The Lancet. Lancet
2000;356:2154.
59. Tchernitchko DO, Gerard-Blanluet M,
Legendre M, Cazeneuve C, Grateau G,
Amselem S. Intrafamilial segregation analy-
sis of the p.E148Q MEFV allele in familial
Mediterranean fever. Ann Rheum Dis
2006;65:11541157.
60. Aksentijevich I, Nowak M, Mallah M, Chae
JJ, Watford WT, Hofmann SR et al. De
novo CIAS1 mutations, cytokine activation,
and evidence for genetic heterogeneity in
patients with neonatal-onset multisystem
inflammatory disease (NOMID): a new
member of the expanding family of pyrin-
associated autoinflammatory diseases. Arthri-
tis Rheum 2002;46:33403348.
61. Lachmann HJ, Sengul B, Yavuzsen TU,
Booth DR, Booth SE, Bybee A et al. Clini-
cal and subclinical inflammation in patients
with familial Mediterranean fever and in het-
erozygous carriers of MEFV mutations.
Rheumatology (Oxford) 2006;45:746750.
62. Korkmaz C, Ozdogan H, Kasapcopur O,
Yazici H. Acute phase response in familial
Mediterranean fever. Ann Rheum Dis
2002;61:7981.
63. Ben-Zvi I, Livneh A. Chronic inflammation
in FMF: markers, risk factors, outcomes
and therapy. Nat Rev Rheumatol2011;7:105
112.
64. Yoshihara T, Imamura T, Yokoi K, Shibata
M, Kano G, Osone S et al. Potential use of
procalcitonin concentrations as a diagnostic
marker of the PFAPA syndrome. Eur J
Pediatr2007;166:621622.
65. Yuksel S, Ekim M, Ozcakar ZB, Yalcnkaya
F, Acar B, Oztuna D et al. The value of
procalcitonin measurements in children with
familial Mediterranean fever. Rheumatol Int
2011; [Epub ahead of print].
66. Wittkowski H, Kuemmerle-Deschner JB,
Austermann J, Holzinger D, Goldbach-
Mansky R, Gramlich K et al. MRP8 and
MRP14, phagocyte-specific danger signals,
are sensitive biomarkers of disease activity in
cryopyrin-associated periodic syndromes.
Ann Rheum Dis 2011;70:20752081.
67. Kallinich T, Wittkowski H, Keitzer R, Roth
J, Foell D. Neutrophil-derived S100A12 as
novel biomarker of inflammation in familial
Mediterranean fever. Ann Rheum Dis
2010;69:677682.
68. Medlej-Hashim M, Petit I, Adib S, Chouery
E, Salem N, Delague V et al. Familial Medi-
terranean fever: association of elevated IgD
plasma levels with specific MEFV mutations.
Eur J Hum Genet 2001;9:849854.
69. Gattorno M, Tassi S, Carta S, Delfino L,
Ferlito F, Pelagatti MA et al. Pattern of
interleukin-1beta secretion in response to
lipopolysaccharide and ATP before and after
interleukin-1 blockade in patients with
CIAS1 mutations. Arthritis Rheum
2007;56:31383148.
70. McDermott MF, Aksentijevich I, Galon J,
McDermott EM, Ogunkolade BW, Centola
M et al. Germline mutations in the extracel-
lular domains of the 55 kDa TNF receptor,
TNFR1, define a family of dominantly
inherited autoinflammatory syndromes. Cell
1999;97:133144.
71. Gattorno M, Sormani MP, DOsualdo A,
Pelagatti MA, Caroli F, Federici S et al. A
diagnostic score for molecular analysis of
Allergy68 (2013) 285296 2013 John Wiley & Sons A/S. Published by Blackwell Publishing Ltd 295
Kallinich et al. Autoinflammation causes recurrent fever
-
8/13/2019 All 12084
12/12
hereditary autoinflammatory syndromes with
periodic fever in children. Arthritis Rheum
2008;58:18231832.
72. Padeh S, Shinar Y, Pras E, Zemer D, Lange-
vitz P, Pras M et al. Clinical and diagnostic
value of genetic testing in 216 Israeli chil-
dren with Familial Mediterranean fever. J
Rheumatol2003;30:185190.
73. Cazeneuve C, Hovannesyan Z, Genevieve D,
Hayrapetyan H, Papin S, Girodon-
Boulandet E et al. Familial Mediterranean
fever among patients from Karabakh and
the diagnostic value of MEFV gene analysis
in all classically affected populations.Arthri-
tis Rheum 2003;48:23242331.
74. Kone-Paut I, Hentgen V, Guillaume-Czi-
trom S, Compeyrot-Lacassagne S, Tran TA,
Touitou I. The clinical spectrum of 94
patients carrying a single mutated MEFV
allele. Rheumatology (Oxford) 2009;48:840
842.
75. Kogan A, Shinar Y, Lidar M, Revivo A,
Langevitz P, Padeh S et al. Common MEFV
mutations among Jewish ethnic groups in
Israel: high frequency of carrier and pheno-
type III states and absence of a perceptible
biological advantage for the carrier state.
Am J Med Genet2001;102:272276.
76. Camus D, Shinar Y, Aamar S, Langevitz P,
Ben-Zvi I, Livneh A et al. Silent carriage of
two familial Mediterranean fever gene muta-
tions in large families with only a single iden-
tified patient.Clin Genet 2011;82:288291.
77. Marek-Yagel D, Bar-Joseph I, Pras E, Berk-
un Y. Is E148Q a benign polymorphism or a
disease-causing mutation? J Rheumatol
2009;36:2372.
78. Cazeneuve C, Sarkisian T, Pecheux C, Der-
vichian M, Nedelec B, Reinert P et al.
MEFV-gene analysis in Armenian patients
with Familial Mediterranean fever: diagnos-
tic value and unfavorable renal prognosis of
the M694V homozygous genotype-genetic
and therapeutic implications. Am J Hum
Genet 1999;65:8897.
79. Aksentijevich I, D Putnam C, Remmers EF,
Mueller JL, Le J, Kolodner RD et al. The
clinical continuum of cryopyrinopathies:
novel CIAS1 mutations in North American
patients and a new cryopyrin model. Arthri-
tis Rheum 2007;56:12731285.
80. Pelagatti MA, Meini A, Caorsi R, Cattalini
M, Federici S et al. Long-term clinical pro-
file of children with the low-penetrance
R92Q mutation of the TNFRSF1A gene.
Arthritis Rheum 2011;63:11411150.
81. Drenth JP, Cuisset L, Grateau G, Vasseur
C, van de Velde-Visser SD, de Jong JG et al.
Mutations in the gene encoding mevalonate
kinase cause hyper-IgD and periodic fever
syndrome International Hyper-IgD Study
Group. Nat Genet 1999;22:178181.
82. Simon A, Cuisset L, Vincent MF, van Der
Velde-Visser SD, Delpech M, van Der Meer
JW et al. Molecular analysis of the mevalo-
nate kinase gene in a cohort of patients with
the hyper-Igd and periodic fever syndrome:
its application as a diagnostic tool. Ann
Intern Med2001;135:338343.
83. Liu Y, Ramot Y, Torrelo A, Paller AS, Si
N, Babay S et al. Mutations in PSMB8
cause CANDLE syndrome with evidence of
genetic and phenotypic heterogeneity.Arthri-
tis Rheum 2011;64:895907.
84. Torrelo A, Patel S, Colmenero I, Gurbindo
D, Lendnez F, Hernandez A et al. Chronic
atypical neutrophilic dermatosis with lip-
odystrophy and elevated temperature (CAN-
DLE) syndrome. J Am Acad Dermatol
2010;62:489495.
85. Marrakchi S, Guigue P, Renshaw BR, Puel
A, Pei XY, Fraitag S et al. Interleukin-
36-receptor antagonist deficiency and gener-
alized pustular psoriasis. N Engl J Med
2011;365:620628.
86. Augey F, Renaudier P, Nicolas JF. General-
ized pustular psoriasis (Zumbusch): a French
epidemiological survey. Eur J Dermatol
2006;16:669673.
87. Zelickson BD, Muller SA. Generalized pus-
tular psoriasis. A review of 63 cases. Arch
Dermatol 1991;127:13391345.
88. Ohkawara A, Yasuda H, Kobayashi H,
Inaba Y, Ogawa H, Hashimoto I et al.
Generalized pustular psoriasis in Japan: two
distinct groups formed by differences in
symptoms and genetic background.Acta
Derm Venereol 1996;76:6871.
89. Borghini S, Tassi S, Chiesa S, Caroli F,
Carta S, Caorsi R et al. Clinical presentation
and pathogenesis of cold-induced autoin-
flammatory disease in a family with recur-
rence of an NLRP12 mutation. Arthritis
Rheum 2011;63:830839.
90. Jeru I, Duquesnoy P, Fernandes-Alnemri T,
Cochet E, Yu JW, Lackmy-Port-Lis M et al.
Mutations in NALP12 cause hereditary
periodic fever syndromes. Proc Natl Acad
Sci USA 2008;105:16141619.
Allergy68 (2013) 285296 2013 John Wiley & Sons A/S. Published by Blackwell Publishing Ltd296
Autoinflammation causes recurrent fever Kallinich et al.