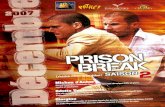
ADR News Dec2007 Vol9 No3
-
Upload
william-chandra -
Category
Documents
-
view
7 -
download
0
description
Transcript of ADR News Dec2007 Vol9 No3

Published by the Centre for Drug Administration, HSA and the Pharmacovigilance Advisory Committee
Adverse Drug Reactionn e w s
CONTENTS
ISSN: 0219 – 2152 December 2007
Vol.9 No.3
1 Advisory on the use of cough and cold medicines in children
3 Gadolinium-based contrast agents – Important safety information
2 Association of salbutamol and myocardial ischaemia in premature labour
4 Risk of torsade de pointes and QT prolongation with haloperidol
5 Reports of adverse reactions to Beauty Express®Miracle Pigmentation Scar Cream
n view of concerns raised on the recent recall in the United States of over-the-counter cough and cold products
marketed for infants and toddlers, and the ensuing recommendations from the public advisory committee meeting convened by the US Food & Drug Administration (FDA) on the safe use of these medicines in young children, HSA has provided an interim advisory to healthcare professionals on the appropriate use of these products while we continue to review the scientific data. These recommendations were included in the Dear Healthcare Professional Letter issued on 30 October 2007 and posted at the MOH Health Professional portal at http://www.hpp.moh.gov.sg.
Background
The recent recall in the US in October 2007 involved 14 brands of cough and cold preparations (containing antihistamines and decongestants) targeted for infants and very young children. They were voluntarily recalled by drug companies due to the danger of overdosage and misuse in this group of patients. Examples of such products are Concentrated Infants' Tylenol Drops Plus Cold & Cough, Dimetapp Decongestant Plus Cough Infant Drops, and Decongestant Infant Drops. HSA confirms that these products are not licensed for sale or use in Singapore.
The US FDA also convened an expert advisory committee in October to deliberate on the efficacy and safety of cough and cold products when used in children under six years of age. In view of the lack of efficacy data in young children balanced against the occurrences of rare but serious adverse drug reactions (ADRs) associated with the use of these products, the expert panel recommended stronger cautionary labels on these products and not to use them in children under six years old. FDA will deliberate on the panel’s recommendations before coming to a conclusion on this issue.
Advisory on the use of cough and cold medicines in children
Active ingredients discussed during the meeting between US FDA and its expert panel for which adverse event reports were analysed:
Table 1: Interim recommendations on use of cough and cold medicines in various age groups of children
1 Brompheniramine,chlorpheniramine,diphenhydramine2 Codeine, dextromethorphan, diphenhydramine3 Ephedrine, guaifenesin, phenylephrine, pseudoephedrine
Promethazine
Category /
Drug
Under
6 months
6 months to
2 years
2 years &
above
ContraindicatedNot
recommendedUse with caution
Antihistamines1
Cough
suppressants 2
Cold and flu
products 3
Notrecommended
Notrecommended
Notrecommended
Use only when benefits
have been assessed to
outweigh risks
Use only when benefits
have been assessed to
outweigh risks
Use only when benefits
have been assessed to
outweigh risks
Use with caution
Use with caution
Use with caution
continued on Page 2
7 Package insert amendments reflecting safety issues
6 Package insert amendments reflecting safety issues
8 Voluntary suspension of sales of aprotinin (Trasylol®)
7 Voluntary withdrawal of clobutinol (Silomat®) cough syrup
5 Summary of advisories issued by HSA and companies

laxoSmithKline (GSK) has issued a Dear Healthcare Professional Letter to alert our healthcare professionals
on reports of myocardial ischaemia associated with the use of salbutamol (Ventolin®) as a tocolytic agent. GSK also advised healthcare professionals to exercise caution when using salbutamol for premature labour, to carefully monitor patient’s cardiovascular function including ECG, and to discontinue the drug if signs of myocardial ischaemia develop.
BackgroundSalbutamol, a selective beta2-adrenoreceptor agonist, is available in several dosage forms with varied uses. Parenteral preparations of salbutamol are registered for the management of uncomplicated premature labour in the last trimester of pregnancy though it is known that salbutamol tablets may sometimes be used for this purpose.
The advice by GSK follows a company-initiated review of the available data from published literature, clinical trials and spontaneous reports of myocardial ischaemia in association with salbutamol. The review found eight spontaneously reported cases in the company database and nine reports in published literature, suggestive of a causal association with myocardial ischaemia when salbutamol was given for the treatment of premature labour.
Summary of spontaneous reports and literatureThe reported events included myocardial ischaemia, myocardial infarction, chest pain and ECG abnormalities indicative of myocardial ischaemia. All the events were reported with the use of intravenous salbutamol except one which was reported with the use of salbutamol tablets. Five cases required hospitalisation and one was considered life-threatening.
The time to onset ranged between 1.5 hours to 4 days with most of the cases occurring within the same day as treatment initiation. No significant pre-disposing factors could be
identified for the development of ischaemic events besides preterm labour. In four of the cases, it was specifically stated that the patients had no known risk factors. One patient had a paternal history of cardiovascular disease while another had a possible pre-existing coronary vascular occlusion.
About half of the cases reported a positive dechallenge on salbutamol discontinuation. One case documented ST depression on the re-introduction of salbutamol one year after the first incident of myocardial ischaemia. However, most of the cases did not provide information on rechallenge. Where specified in the reports, actions taken after the occurrence of the adverse event include the discontinuation of salbutamol and treatment with nifedipine, heparin, aspirin, nitroglycerin and verapamil.
Conclusions and recommendationsAlthough the effects of sympathomimetics may be exaggerated in preterm labour due to high background sympathetic drive, hyperventilation, dehydration and haemodilution through the use of intravenous fluids, the association between myocardial ischaemia with salbutamol use in preterm labour cannot be ruled out as the reported cases were well-documented and contained no significant pre-disposing factors for the development of ischaemic events other than preterm labour.
To date, HSA has not received any spontaneous local ADR report of myocardial ischaemia associated with the use of salbutamol in preterm labour. Nevertheless, healthcare professionals are advised to be cautious when using salbutamol for this purpose, and to report any serious adverse reactions suspected to be due to its use in pregnancy to the Pharmacovigilance Unit of HSA. The local package inserts of parenteral and oral Ventolin® products has been updated to include this new safety information.
References
1. Aust N Z J Obstet Gynaecol 1981; 21:1-4. 2. Eur J Obstet Gynecol Reprod Biol 2001; 98:177-185. 3. Singapore J Obstet Gynaecol 1986; 17:54-58. 4. Arch Mal Coeur 1997; 90:1651-1654.5. Acta Obstet Gynecol Scand 1987; 66:417-420. 6. Am J Obstet Gynecol 1989; 161:318-321.7. Circulation 2006; 113: 1564-1571.
Adverse Drug Reaction News • December 2007 • Vol.9 No.3
Review of data by US FDA
A review of the adverse reports from the US FDA associated with the antihistamines (diphenhydramine, brompheniramine and chlorpheniramine), and the decongestants (pseudoephedrine, phenylephrine, and ephedrine) over 1969–2006 revealed that most of the ADRs occurred in children under two years old and overdosage and drug toxicities were the common causes. A further analysis of the adverse events associated with pseudoephedrine, chlorpheniramine, diphenhydramine and dextromethorphan from 2002–2007 showed that serious events and deaths related to the nervous system (e.g. seizures), cardiac and respiratory system were associated with both overdoses as well as labeled doses of cough and cold medicines. There is also a potential risk of overdose when using multiple cough and cold products.
Local situtation
HSA has not received any local reports of fatal adverse drug reactions associated with cough and cold medicines. However, taking into consideration the findings by US FDA and the lack of efficacy data of cough and cold medicines used in children, HSA has provided healthcare professionals with an interim advisory on the use of cough and cold medicines in young children. This advisory takes into consideration guidelines developed by other regulatory agencies, and the previous review conducted by HSA and its Pharmacovigilance Advisory Committee in 2005 on the use of promethazine in children under two years of age.
continued on Page 1 - Advisory on the use of cough and cold medicines in children
Association of salbutamol and
myocardial ischaemia in premature labour

Adverse Drug Reaction News • December 2007 • Vol.9 No.3
rising from the emerging concerns associated
with gadolinium-based contrast agents (GBCAs)
and the protential increased risk of nephrogenic fibrosing
dermopathy (NFD) and nephrogenic systemic
fibrosis (NSF), the Health Sciences Authority (HSA)
and its Pharmacovigilance Advisory Committee have
reviewed the safety profile and use of these products,
particularly in patients with renal dysfunction.
Brief overview
Gadolinium-based contrast agents (GBCAs) are approved by
HSA for use in magnetic resonance imaging (MRI).
Seven GBCAs are registered in Singapore: gadodiamide
(Omniscan®, GE Healthcare), gadopentetate dimeglumine
(Magnevist®, Bayer Schering Phama), gadoterate
meg lumine (Dotarem®, Guerbe t ) , gadobut ro l
(Gadovist®, Bayer Schering Phama), gadobenate dimeglumine
(Multihance®, IDS Pharmaceutical Division), gadoversetamide
(Optimark®, Tyco Healthcare) and gadoxetic acid
(Primovist®, Bayer Schering Phama).
HSA has been closely monitoring the association of NFD/NSF
with these contrast agents since May 2006, following the
first alert by GE Healthcare on NFD/NSF reported with the use
of Omniscan® in patients with severe renal impairment. An
article was published in July 2006 issue of the Adverse Drug
Reaction News Bulletin to alert healthcare professionals
of these adverse reactions.
Following the first alert on Omniscan®, more global reports
of NFD/NSF were subsequently received for Omniscan®
(more than 150 cases), as well as Magnevist® (78 cases)
and Optimark® (11 cases). More recently, isolated cases
associated with other GBCAs were also reported. All these
reports occurred only in patients with renal dysfunction and
is associated with swelling and tightening of the skin
in the extremities which may develop over a period of days
to several weeks. The mechanism by which a GBCA can
cause NFD/NSF has not been elucidated but the current
understanding is that GBCAs are associated with different
levels of NFD/NSF risk based on their physicochemical
and pharmacokinetic properties.
HSA has issued a Dear Healthcare Professional Letter (DHCPL)
in December 2007 to all registered physicians to alert
them to the above safety information, as well as advise on
appropriate use of these drugs. For details of the DHCPL,
please log on to the MOH Health Professionals Portal at
http://www.hpp.moh.gov.sg.
Summary of recommendations
• Use of Omniscan® or Magnevist® is contraindicated in
patients with severe renal failure (GFR < 30mL/min/1.72m2).
• The risk for the development of NFD/NSF in patients with
moderate renal impairment is unknown, therefore
Omniscan® and Magnevist® should be used with
caution in patients with moderate renal impairment
(GFR 30–59mL/min/1.73m2), especially if any gadolinium-
based contrast media have been previously administered.
• Omniscan® and Magnevist® should be used in neonates
and infants only if the benefits outweigh the risks as
these patients have immature kidney functions.
• The other GBCAs should be used in patients with severe
renal impairment (GFR < 30mL/min) only when absolutely
necessary where the benefits outweigh their risks. Any
possible alternative imaging tests that do not require GBCA,
the clinical need for GBCA use, the relative risk for the
patient, the type of agent to be used and any history of prior
GBCA exposure should be considered when using the other
GBCAs in severe renal impaired patients.
• There is no robust evidence to show that haemodialysis
can prevent or treat the development of NFD/NSF, but
haemodialysis shortly after GBCAs administration in
patients currently receiving haemodialysis may be useful
in removing the agent from the body, and there is some
preliminary evidence that suggests NFD/NSF is less likely
to develop in patients receiving early and adequate
haemodialysis. If it is to be performed, the US and European
authorities have recommended that at least two episodes
of haemodialysis, the first commencing within 24 hours
of administration of GBCA, performed in patients
at risk who receive any of the GBCAs.
Gadolinium-based contrast agents – Important safety information
Omniscan® and Magnevist® contraindicated in patients with severe renal failure

Adverse Drug Reaction News • December 2007 • Vol.9 No.3
aloperidol is a butyrophenone antipsychotic agent andits indications include the management of psychoses,
schizophrenia and manic states and management of aggressive and agitated behavior. Haloperidol injection has been registered in Singapore since 1994 and is licensed only for intramuscular administration.
Recent safety alert issued by the US FDA
The US Food and Drug Administration (FDA) has recently
issued a safety alert which highlights the potential increased
risk of QT prolongation and torsade de pointes (TdP) with the
use of intravenous (IV) administration of haloperidol.
Although injectable haloperidol is approved by the FDA only
to be used as an intramuscular injection, there is considerable
evidence from the medical literature that IV haloperidol is a
relatively common ‘off-label’ clinical practice, primarily to
treat cases of severe agitation in intensive care units.
There are at least 28 case reports of QT prolongation and TdP
in the medical literature, some with fatal outcome in the
context of off-label IV administration of haloperidol.
Additionally, case control studies performed have
demonstrated a dose-response relationship between
intravenous haloperidol dosing and subsequent TdP.
Johnson & Johnson (sponsor of the proprietary brand of
haloperidol, Haldol® in the US) recently conducted two
post-marketing studies analysing QT prolongation and
TdP with the administration of haloperidol (both oral and
injectable). In the first study, Johnson & Johnson performed
a search of their Benefit Risk Management worldwide safety database. The results revealed 73 cases of TdP,
of which 11 of these cases led to fatalities. Eight of these fatalities involved the IV administration of haloperidol.
The second study involved a post-marketing investigation that examined reports of cardiac events that involved
haloperidol received by the company as of 30 July 2005. Thirteen of these haloperidol related cardiac events reported
involved the occurrence of TdP, QT prolongation, ventricular
arrhythmia and/or sudden death.
Label amendments in the US
Based on these recent findings, the labelling of Haldol®
products in the US were revised to include the following warnings:
• Higher doses and IV administration of haloperidol
appear to be associated with a higher risk of QT prolongation and TdP.
• Although cases of sudden death, TdP and QT prolongation
have been reported even in the absence of predisposing factors, particular caution is advised in treating patients
using any formulation of haloperidol who:
• have other QT prolonging conditions, including
electrolyte imbalance (particularly hypokalaemia and
hypomagnesemia),
• have underlying cardiac abnormalities, hypothyroidism,or familial long QT syndrome, or
• are taking drugs known to prolong the QT interval.
• Because of this risk of TdP and QT prolongation, ECG monitoring is recommended if haloperidol is given intravenously.
Additionally, Johnson & Johnson’s recent amendments to
Haldol®’s labelling now include that Haldol® is not approved for intravenous administration.
Conclusion
HSA has not received any local reports of prolonged QTc
or TdP involving the use of haloperidol, and will continue to monitor the situation. The FDA, in its safety update, stated
that based on case reports alone, it was unable to estimate the frequency with which QT prolongation or TdP occur
following administration of haloperidol and will continue to monitor post-marketing reports for such adverse events and
further regulatory actions and communications will be effected as additional information becomes available.
It advised that healthcare professionals should take into consideration the above new safety information when making
individual treatment decisions for their patients.
References
1. FDA information for healthcare professionals, 17 September 2007. http://www.fda.gov/Cder/drug/InfoSheets/HCP/haloperidol.htm
2. Reuters. FDA warns of heart risks with schizophrenia drug. http://www.reuters.com/article/governmentFilingsNews/idUSWBT00759220070917
Risk of torsade de pointes and QT prolongation with haloperidol

he Pharmacovigilance Unit, HSA has received local reports of adverse reactions resulting from use of
adulterated cosmetic products. The cases below relate to the experience of some patients.
Local case reports
The cosmetic product, Beauty Express® Miracle Pigmentation Scar Cream was tested by HSA to contain betamethasone dipropionate 0.023%, a potent steroid, following reports of adverse drug reactions to the product. A few female patients who
purchased the product from a retail shop in Singapore as skin whitener for skin pigmentation developed rashes, redness and skin sensitivity on their face after using the creams for several years. These patients became very dependent on the cream and suffered flares of skin redness and soreness whenever they stopped application of the creams. Clinically, the rashes on their face were very suggestive of “steroid
facies” as the skin on their face were red and atrophied with surface telangiectasia. The reporting physician suspected steroid facies and symptoms of steroid withdrawal syndrome when they stopped using the cream. Steroid facies is caused by prolonged use of fluorinated topical steroids on the face. Other side effects of topical fluorinated steroids on the face include perioral and periorbital dermatitis (which manifest as acneiform eruptions around the mouth and eyes).
Betamethasone dipropionate is a very potent corticosteroid as compared to other topical corticosteroids such as hydrocortisone and betamethasone valerate. It can result in Cushing's syndrome, skin atropy and hyperglycaemia. Prolonged and widespread use may also result in reversible hypothalamic-pituitary-adrenal (HPA) axis suppression.
The local company marketing Beauty Express® Miracle Pigmentation Scar Cream was prosecuted by HSA for adulterating the product with betamethasone dipropionate.
When diagnosing an adverse reaction in patients, healthcare professionals are encouraged to take a detailed medical history which may take into consideration the patient’s use of cosmetic products.
Reports of adverse reactions to Beauty
Express® Miracle Pigmentation Scar Cream
Summary of Dear Healthcare Professional Letters issued by HSA and/or pharmaceutical companies from January 2006 to November 2007.For details, please log on to http://www.hpp.moh.gov.sg using your professional board register number or Singpass.
Summary of advisories issued by HSA and companies
9 Jan 2006 – Rosiglitazone (Avandia® or Avandamet®): Rare reports of macular oedema
14 Feb 2006 – Aprotinin (Trasylol®): Literature reports on the possible risk of serious renal and cardiovascular toxicity following Trasylol® administration to patients undergoing coronary artery bypass grafting surgery (CABG)
22 Feb 2006 – Gatifloxacin (Tequin®): Safety update and product labelling changes of serious cases of hypoglycaemia and hyperglycaemia
23 Jun 2006 – Lamotrigine (Lamictal®): Risk of oral clefts
21 Jun 2006 – Infliximab (Remicade®): Risk of hepatosplenic T-cell lymphoma
8 Feb 2007 – Ranibizumab (Lucentis®): Risk of stroke
21 Feb 2007 – Entecavir (Baraclude®): Risk of developing HIV resistance cannot be excluded with entecavir therapy in HIV/HBV co-infected patients not receiving HAART
12 Mar 2007 – Rosiglitazone (Avandia®): Clinical trial observation of an increased incidence of fractures in female patients receiving long-term treatment with rosiglitazone for type 2 diabetes mellitus
3 Apr 2007 – Tegaserod (Zelmac®): Temporary withdrawal of sales
9 May 2007 – Bevacizumab (Avastin®): Risk of tracheo-esophageal fistula
24 May 2007 – Zolendronic acid (Zometa®): Reports of atrial fibrillation observed in clinical study
11 Jun 2007 – Nimesulide: Suspension of sales following signals of liver toxicities
14 Jun 2007 – Deferasirox (Exjade®): Risk of acute renal failure and blood cytopenias
5 Jul 2007 – Tegaserod (Zelmac®)/ Restrictions on the supply of tegaserod and special access for patients who have no therapeutic alternatives
21 Aug 2007 – Rosiglitazone (Avandia®)/ Rosiglitazone and metformin (Avandamet®): Advisory for patients with congestive heart failure
23 Aug 2007 – Lopinavir and ritonavir (Kaletra®): Accidental overdose in children
04 Sep 2007 – Clobutinol (Silomat®): Withdrawal of sales
07 Sep 2007 – Salbutamol: Risk of myocardial ischaemia when used during premature labour in pregnant women
30 Oct 2007 – Advisory on the use of cough and cold medicines in children
7 Nov 2007 – Aprotinin (Trasylol®): Temporary suspension of sales
9 Nov 2007 – Mycophenolate mofetil (Cellcept®): Increased risk of congenital malformations observed following use in pregnancy
Adverse Drug Reaction News • December 2007 • Vol.9 No.3

Adverse Drug Reaction News • December 2007 • Vol.9 No.3
continued on Page 7
HSA has approved the following package insert changes due to safety updates from June 2007 to October 2007. Please note that due to space constraints, the list published is not exhaustive and you are encouraged to refer to the following website for the complete listing with details: www.hsa.gov.sg/safetyinfo_and_recalls. Please also note that there might be a time lag in the availability of the package insert which reflects the latest change(s).
Package insert amendments reflecting safety issues
1. Adefovir (Hepsera®, GSK) Caution: Elderly. Warning: Lactic acidosis (in the absence of hypoxemia), sometimes fatal, usually associated with severe hepatomegaly & hepatic steatosis may occur, hence treatment with nucleoside analogues should be discontinued when rapidly elevating aminotransferase levels, progressive hepatomegaly or metabolic lactic acidosis of unknown etiology occur & caution should be exercised when prescribing nucleoside analogues to any patient (particularly obese women) with hepatomegaly, or other known risk factors for liver disease. New ADRs: Vomiting, mild to moderate increases in serum creatinine levels, hypophosphatemia & a decrease in carnitine concentrations.
2. Alendronate (Fosamax®, MSD) Cautions: Discontinuation should be considered in patients with osteonecrosis of jaw (ONJ) based on individual benefit / risk assessment, especially for patients requiring invasive dental surgery. Dental surgery may exacerbate ONJ. Known risk factors for ONJ include co-morbid disorders like periodontal disease.
3. Anagrelide (Agrylin®, IDS) Elderly patients had twice the incidence of serious adverse events, mainly cardiac-related events. Contraindication: Moderate/severe hepatic impairment or moderate/severe renal impairment (ClCr <50ml/min). Potential risks & benefits of anagrelide therapy in patients with mild hepatic impairment should be assessed before treatment is started. Warning: Cardiomegaly & congestive heart failure reported. Cautions: Patients with known or suspected heart disease. Pre-treatment cardiovascular examination (echocardiography, electrocardiogram) & continued monitoring of CV function is recommended. Not recommended in patients with elevated transaminases (>5 times ULN). Concomitant use with other PDE III inhibitors such as milrinone, amrinone, enoximone, olprinone & cilostazol is not recommended. Potential risks & benefits of concomitant use of anagrelide with acetylsalicylic acid in patients with a platelet count >1500 x 109/L &/or a history of haemorrhage should be assessed before starting treatment. Patients with rare hereditary problems of galactose intolerance, Lapp lactase deficiency or glucose-galactose malabsorption should not be given with anagrelide.
4. Baclofen (Lioresal®, Novartis) Signs & symptoms of overdosage have been reported with doses >5mg/day in patients undergoing chronic haemodialysis as baclofen concentrations in plasma are elevated. Cautions: i) Patients suffering from depressive, manic disorders or Parkinson's disease; ii) Discontinuation or cases of overdosage as lowering of convulsion threshold may occur & seizures have occasionally been reported; iii) Abrupt withdrawal as dyskinesia & hyperthermia have been reported.
Clinical characteristics of withdrawal of intrathecal Lioresal® may resemble autonomic dysreflexia, infection (sepsis), malignant hyperthermia, neuroleptic malignant syndrome, or other conditions associated with a hypermetabolic state or widespread rhabdomyolysis.
Drug interactions: Synthetic opiates, alcohol, morphine & levodopa. Careful monitoring of respiratory & cardiovascular functions is essential, especially cardiopulmonary disease & respiratory muscle weakness. ADRs: Hypothermia, pollakiuria & erectile dysfunction.
5. Cabergoline (Dostinex®, Pfizer) Warnings: Chest x-ray is recommended when new clinical symptoms of respiratory disorders are presented. Discontinue therapy in the case of x-ray signs of pleural effusion/pulmonary fibrosis or in the diagnosis of valvulopathy. Pathological gambling, increased libido & hypersexuality (reversible upon reduction of dose or treatment discontinuation) reported. ADRs: Alopecia, aggression & psychotic disorder.
6. Carbamazepine (Tegretol®, Novartis) Warning: Toxic epidermal necrolysis & SJS have been rarely reported with Tegretol®. Drug interactions: Paroxetine & levetiracetam. ADR: Hypogammaglobulinaemia.
7. Ceftibuten (Cedax®, Schering-Plough) Ceftibuten can rarely lead to prolonged prothrombin time (PT), especially in patients previously stabilised on oral anticoagulant therapy. PT or INR should be monitored in patients at risk & treated as required. ADRs: Bronchospasm, dyspnoea, rash, urticaria, photosensitivity reaction, pruritus, angioneurotic oedema & pseudomembranous colitis.
8. Cholestyramine (PMS-Cholestyramine®, Apotheca) Caution: May cause steatorrhea or accentuate pre-existing steatorrhea & this may require reduction & adjustment of dosage.
Drug interactions: Digitalis & estrogens that undergo enterohepatic recirculation. Cholestyramine has been shown to reduce the bioavailability of HMG-CoA reductase inhibitors; the clinical cholesterol-lowering effects of an HMG-CoA reductase inhibitor & cholestyramine have been shown to be additive. ADRs: Dental bleeding, diuresis, weight loss/gain, increased libido, swollen glands, edema & dental caries.
9. Ciclosporin (Sandimmun Neoral®, Novartis) Warnings: Avoid excess UV light exposure; monitor renal function in elderly. There is only limited experience with the use in children with endogenous uveitis.
Drug interactions: Oxcarbazepine, bosentan, voriconazole & colchicine. Methotrexate exhibits nephrotoxic synergy with ciclosporin. Following concomitant administration of ciclosporin & lercanidipine, AUC of lercanidipine was increased 3 times & AUC of ciclosporin was increased 21%. Concomitant use of potassium sparing drugs e.g. potassium sparing diuretics, ACE inhibitors, angiotensin I I receptor antagonists or potassium containing drugs may lead to significant increases in serum potassium.
10. Clobetasol (Univate®, Apex Pharmacy) Contraindication: Treatment of dermatoses, peri-anal & genital pruritus in children <1yr, including dermatitis& nappy eruption. Severe ADRs are likely to happen if application of more than 50g/week is used.
11. Diclofenac (Cataflam®, Novartis) Caution: Breastfeeding. Drug interactions: Concomitant use of topical diclofenac & topical steroids in patients with significant pre-existing corneal inflammation may increase risk of developing corneal complications. ADRs: Conjunctival hyperaemia, allergic conjunctivitis, eyelid erythema, urticaria, rash, eczema, erythema, pruritus, hypersensitivity, cough & rhinitis.
12. Diphtheria, haemophilius influenzae, pertussis, polio & tetanus (Infanrix-IPV+Hib®, GSK) Warning: For children with progressive neurological disorders like infantile spasms, uncontrolled epilepsy or progressive encephalopathy, to defer pertussis immunization until condition is corrected. ADRs: Local or diffuse swelling at injection site, sometimes involving adjacent joint. Large swelling reactions more likely when children primed with acellular pertussis vaccines vs whole cell vaccine; local swelling & diffuse swelling may be more frequent when booster dose is administered between 4 & 6 years, resolving over an average of 4 days. Swelling of the entire injected limb has been reported.
13. Eletriptan (Relpax®, Pfizer) Caution: Co-administering with other drugs having serotonergic activity, such as SNRIs & SSRIs due to possible development of serotonin syndrome. Thus, careful observation of the patient is warranted particularly during treatment initiation or dose increase of either eletriptan or SSRIs/SNRIs. Concomitant use with potent CYP3A4 inhibitors e.g. ketoconazole, itraconazole, erythromycin, clarithromycin & protease inhibitors is not recommended.
14. Epoetin alfa (Eprex®, Johnson & Johnson) Warnings: Monitor haemoglobin (Hb) levels closely due to a potential increased risk of thromboembolic events & fatal outcomes when patients are treated at Hb levels above the target for the indication of use. In patients with chronic renal failure, maintenance Hb concentration should not exceed the upper limit of the target Hb concentration. Hb levels >12g/dL may be associated with a higher risk of cardiovascular events, including death. ADRs: Increase in blood pressure, aggravation of existing hypertension, myalgia, hypertensive crisis with encephalopathy & seizures, shunt thromboses, & porphyria.
15. Estramustine (Estracyt®, Pfizer) Warnings: Patients with prostate cancer & osteoblastic metastases are at risk for hypocalcemia. Monitor calcium levels.
16. Etoricoxib (Arcoxia®, MSD) Warnings: Long-term administration of NSAIDs has resulted in renal papillary necrosis & other renal injury. Perforations, ulcers or bleeds can occur at any time during use & without warning symptoms though the results of the MEDAL Program demonstrate that risk of GI toxicity in patients treated with Arcoxia® 60mg or 90mg once daily is significantly less than with diclofenac 150mg daily. ADR: Shock. Serious skin reactions, some of them fatal, may occur.
17. Gadoxetic acid (Primovist®, Zuellig) Warnings: Occurrence of nephrogenic systemic fibrosis (NSF) / nephrogenic fibrosing dermopathy (NFD) in patients with severe renal impairment (GFR <30ml/min/1.73m2) were reported. No robust evidence that haemodialysis can prevent or treat the development of NSF but haemodialysis shortly after Primovist® administration in patients currently recently receiving haemodialysis may be useful at removing Primovist® from the body. No evidence to support the initiation of haemodialysis for prevention or treatment of NSF in patients not already undergoing haemodialysis.
18. Ibandronic acid (Bonviva®, Roche) Osteonecrosis of the jaw, associated with tooth extraction &/or local infection has been reported in cancer patients receiving mainly IV bisphosphonates & in patients with osteoporosis receiving oral bisphosphonates. Consider dental examination with appropriate preventive dentistry in those with concomitant risk factors e.g. cancer, chemotherapy, radiotherapy, corticosteroids, & poor oral hygiene. Avoid in patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose-galactose malabsorption.
19. Isradipine (Dynacirc SRO®, Novartis) Warnings: Angina pectoris may occur, predominantly in patients with pre-existing coronary artery disease. In patients with pre-existing angina pectoris, frequency, duration & severity of anginal attacks may be increased by rapid dosage increments or at the start of treatment. Food interaction: Grapefruit juice may increase bioavailability of isradipine. ADRs: Polyuria, malaise, weight increased, stroke, syncope, transient ischaemic attack, lethargy, dry mouth, constipation, diarrhoea, insomnia, & chest pain.
20. Lansoprazole (Prevacid®, Luen Wah Medical) Contraindication: Patients on atazanavir therapy. Drug interactions: Theophylline & atazanavir. ADRs: Anaphylactic reactions, dyspnea, shock, toxic epidermal necrolysis (Lyell syndrome), oculomucocutaneous syndrome, Stevens Johnson syndrome, severe hepatic dysfunction with jaundice, hepatitis, agranulocytosis, pancytopenia, haemolytic anaemia, nausea, vomiting, anorexia, abdominal pain, candidiasis, stomatitis, glossitis, taste abnormality, interstitial nephritis, acute renal failure, interstitial pneumonia, gynaecomastia, blurred vision, oedema, weakness, malaise, numbness of tongue or lips, numbness of limbs, arthralgia, muscle pain, & alopecia.

Discontinue lansoprazole in the following cases: i) Diarrhoea persists. ii) Abdominal pain & frequent diarrhoea occurring in H.pylori eradication. iii) Abnormalities in renal function test values e.g. increases in BUN, creatinine, etc. iv) Fever, coughing, dyspnoea, abnormal lung sound (crepitation) etc.When such symptoms arise, chest X-ray should be performed immediately & patient treated with corticosteroid.
21. Lopinavir & ritonavir (Kaletra®, Abbott) Precautions: Coadministration of ritonavir & digoxin may result in significantly increased digoxin levels, therefore monitoring of serum digoxin levels is recommended. Drug interactions: Rifampin, fluticasone & tipranavir. ADRs: Myocardial infarct, hepatomegaly, liver fatty deposit, liver tenderness, joint disorder, myasthenia, extrapyramidal syndrome, increased cough, neoplasm, skin striae, & impotence.
22. Naftidrofuryl (Praxilene®, Merck) Contraindication: History of hyperoxaluria. Warnings: Taking Praxilene® without liquid before going to bed may cause local oesophagitis. Recommended to drink large volumes of liquid during the whole treatment period to maintain an adequate level of diuresis and to reduce the formation of calcium oxalate kidney stones. ADRs: Nausea & hepatitis.
23. Nifedipine (Adalat LA®, Bayer) Warnings: Bezoars can occur rarely & may require surgical intervention. ADRs: Anaphylactoid reaction, anxiety reactions, migraine, par-/dysaesthesia, visual disturbances, palpitations, nosebleed, nasal congestion, GI & abdominal pain, erythema, joint swelling, & erectile dysfunction.
24. Octreotide (Sandostatin LAR® & Sandostatin multidose®, Novartis) Warnings: Uncommon cases of bradycardia have been reported hence dose adjustments of drugs like beta blockers, calcium channel blockers, or agents to control fluid & electrolyte balance may be necessary. Octreotide may alter absorption of dietary fats in some patients. Depressed vitamin B12 levels & abnormal Schilling's tests observed in some patients on octreotide hence to monitor vitamin B12 levels in patients on Sandostatin LAR® & who have a history of vitamin B12 deficiency. ADRs: Anaphylaxis, tachycardia, dyspnoea, cholecystitis, thyroid dysfunction, dyspepsic signs, symptoms & episodes of arrhythmia, ECG changes e.g. QT prolongation.
25. Oxybutynin (Lyrinel®, J&J) Warnings: Monitor patients for signs of anticholinergic CNS effects, particularly in the first few months after beginning treatment or increasing the dose. ADRs: Psychotic disorder & agitation.
26. Paricalcitol (Zemplar®, Abbott) Chronic renal failure subjects showed a decreased clearance & increased half-life of paricalcitol. ADRs: Facial & oral oedema.
27. Pimecrolimus (Elidel®, Novartis) Use of Elidel® cream in patients <2 yrs old is not recommended until further data becomes available. ADRs: Anaphylactic reactions, alcohol intolerance (flushing, rash, burning, itching or swelling), allergic reactions & skin discoloration (e.g. hypopigmentation, hyperpigmentation).
28. Pneumococcal 7-valent conjugate (Prevenar®, Wyeth) When Prevenar® is co-administered with hexavalent vaccines (DTaP-Hib-IPV-HepB), the rate of febrile reactions was higher compared to that occurring following administration of hexavalent vaccines alone. Reactions were mostly moderate (≤39oC) & transient. ADR: Urticaria-like rash.
29. Procaterol (Meptin®, Luen Wah Medical) Precautions: Pregnancy. Use only as additional therapy for patients whose symptoms are not adequately controlled
& not as a substitute for inhaled corticosteroids & other anti-inflammatory agents. Use short-acting inhaled beta2 stimulants in episodes of acute asthma.
30. Raloxifene (Evista®, Eli Lilly) Caution: Postmenopausal women with a history of stroke or other significant stroke factors such as transient ischaemic attack or atrial fibrillation. ADRs: Thrombocytopenia, peripheral oedema, venous & arterial thromboembolic reaction.
31. Ropinirole (Requip®, GSK) Warnings: Compulsive behaviours such as pathological gambling & hypersexuality have been reported in Parkinson's disease patients treated with ropinirole, especially at high doses & were generally reversible upon dose reduction or treatment discontinuation. In some cases, other factors like a history of compulsive behaviours or concurrent dopaminergic treatment were present. ADRs: Constipation, peripheral oedema & hypersexuality.
32. Sulfasalazine (PMS-Sulfasalazine®, IDS) Contraindications: Intestinal & urinary obstructions. Not to be used in patients in whom acute asthmatic attacks, urticaria, rhinitis or other allergic manifestations are precipitated by ASA or other NSAIDs as fatal anaphylactic reactions have occurred in such individuals. Cautions: Patients with hepatic or renal damage, blood dyscrasias, severe allergy or bronchial asthma. Pancreatitis has been observed in some susceptible individuals. Deaths associated with the use of sulfasalazine have been reported from hypersensitivity reactions, agranulocytosis, aplastic anemia, other blood dyscrasias, renal & liver damage, irreversible neuromuscular & CNS changes & fibrosing alveolitis. Presence of clinical signs like sore throat, fever, pallor, purpura or jaundice may be indications of serious blood disorders. Bone marrow depression has been reported usually within the first 3 months of starting treatment & is usually reversible on stopping sulfasalazine. A full blood count, including differential white blood cell count, should be carried out before starting therapy & monitored closelyduring the first few months of treatment, thereafter patients should be screened if their condition changes or if they have symptoms of infection. Oligospermia with infertility have been observed in men treated with sulfasalazine. Adequate fluid intake must be maintained in order to prevent crystalluria & stone formation.
33. Ziprasidone (Zeldox®, Pfizer) Cautions: Patients with severe hepatic insufficiency; concomitant use with other centrally acting agents & drugs acting on thedopaminergic & serotonergic systems. Warnings: Rare post-marketing reports of torsade de pointes in patients with multiple confounding risk factors taking ziprasidone reported. Discontinue drug if signs of neuroleptic malignant syndrome occurred. Zeldox® is not approved for elderly patients with dementia-related psychosis. Women of childbearing potential receiving ziprasidone should use an appropriate contraceptive.
ADRs: Seizures, body weight gain & loss, transient elevation of prolactin, mania/hypomania, serotonin syndrome, syncope, torsade de pointes, angioedema, galactorrhea, & priapism.
34. Zoledronic acid (Zometa®, Novartis) Warnings: Renal deterioration, progression to renal failure & dialysis have been reported in patients after the initial dose or a single dose of Zometa®. ADRs: Atrial fibrillation, somnolence & bronchoconstriction.
HSA has approved the following package insert changes due to safety updates from June 2007 to October 2007. Please note that due to space constraints, the list published is not exhaustive and you are encouraged to refer to the following website for the complete listing with details: www.hsa.gov.sg/safetyinfo_and_recalls. Please also note that there might be a time lag in the availability of the package insert which reflects the latest change(s).
Package insert amendments reflecting safety issues
Adverse Drug Reaction News • December 2007 • Vol.9 No.3
Voluntary withdrawal of clobutinol (Silomat®) cough syrup
lobutinol (Silomat®, Boehringer Ingelheim) was licenced in Singapore in 1999. It is an orally active non-opioid
antitussive agent, and is indicated for the treatment of irritable, non-productive cough and inflammatory disorders of the airways.
In September 2007, Boehringer Ingelheim voluntarily withdrew Silomat® from the Singapore market as a precautionary measure due to concerns of a potential increased risk of cardiac arrhythmias that could be associated with the active ingredient.
Published experimental data have indicated the potential of clobutinol affecting the hERG (human ether-a-go-go related
gene) potassium channels. Preliminary findings from a recent clinical trial with clobutinol in adult healthy volunteers have shown a prolongation of the QTc interval in the ECG. As clobutinol is indicated for a non-serious disease condition and in view of the potentially life-threatening adverse effects, HSA agreed with the actions of Boehringer Ingelheim to withdraw clobutinol from the worldwide market. A Dear Healthcare Professional Letter (DHCPL) was issued by the company to alert healthcare professionals to the findings and the decision to recall and suspend the sales of Silomat®. For details of the DHCPL, please log on to the Health Professionals Portal at http://www.hpp.moh.gov.sg.

protinin (Trasylol®, Bayer HealthCare) is an
antifibrinolytic agent used to reduce blood loss and
the need for blood transfusion in adult patients at risk of blood
loss who are undergoing cardiopulmonary bypass in the
course of coronary artery bypass graft surgery. It has been
registered in Singapore since 1994.
Recent safety findings
Recent findings have raised concerns regarding the safety
issues associated with the use of aprotinin in cardiac surgery.
Earlier observational studies have suggested that aprotinin
may increase the risk of mortality when compared against
other antifibrinolytic agents. The latest Canadian study,
BART (Blood conservation using antifibrinolytics: A randomized
trial in high risk cardiac surgery patients), a trial comparing
the safety and efficacy of aprotinin (2 million units bolus + 2
million units in pump prime + 2 million units via infusion over
4 hours) against epsilon-aminocaproic acid (10g bolus + 250
mL NaCl in pump prime + 2g/hr infusion) or tranexamic acid
(30mg/kg bolus + 2mg/kg/hr in pump prime + 16mg/kg/hr
infusion) suggested an increase in all-cause mortality among
patients in the aprotinin arm of the study compared to the
other two drugs: the 30 days mortality of aprotinin compared
to the two drugs were relative risks of 1.5 at p=0.06 and p=0.08.
Although statistical significance was not reached, a trend
towards an increase in mortality in the aprotinin-treated group
was present throughout most of the trial.
International measures
As a result of the findings of the BART study, and in consultation
with the German Federal Institute for Drugs and Medical
Devices (BfArM), the US Food and Drug Administration (FDA),
Health Canada and other regulatory authorities, Bayer
HealthCare® decided to temporarily suspend the worldwide
sales of Trasylol® until the final data from the study can be
compiled and evaluated.
HSA’s action and advisory
In consultation with the Health Sciences Authority (HSA), the
sales of Trasylol® was temporarily suspended in Singapore
on 6 November 2007 pending further evaluation of information
from the BART study. A final regulatory decision on Trasylol®
will be made in due course and healthcare professionals
will be informed accordingly.
As an interim measure, HSA has worked with Bayer to allow
supply of Trasylol® through restricted access under certain
conditions, to a small group of patients who have been
assessed by their physicians to have no other therapeutic
options, and where the benefits of the drug may outweigh its
risks. Physicians are required to discuss the risks associated
with using Trasylol® and obtain written consent from either
the patient or the next of kin should the patient be incapable
or incompetent in doing so before prescribing Trasylol®.
References
1. FDA early communication about an ongoing safety review aprotinin injection,
25 October 2007. http://www.fda.gov/cder/drug/early_comm/aprotinin.htm
2. N Engl J Med Jan 2006; 354(4):353-65.
3. Transfusion Mar 2006; 46(3):327-338.
Enquiries, comments and suggestions to:
Pharmacovigilance UnitCentre for Drug AdministrationHealth Products Regulation GroupHealth Sciences Authority11 Biopolis Way, #11-03, Helios, Singapore 138667
Tel: (65) 6866 3538 Fax: (65) 6478 9069
Website: http://www.hsa.gov.sgEmail: [email protected]
Editor-in-Chief
Ms Chan Cheng Leng, BSc (Pharm) Hons
Executive Editor
Ms Ang Pei San, BSc (Pharm)
Staff Editors
Mr Choong Chih Tzer, BPharm
Dr Yvonne Koh, BSc (Pharm) Hons, PhD
Ms Adena Lim, BSc (Pharm) Hons, MPharm (Clin Pharm)
Ms Belinda Tan, BSc (Pharm)
Editorial Board
Clinical Prof. Goh Chee Leok
Prof. Edmund Lee Joo Deoon
Clinical A/Prof. Chng Hiok Hee
Clinical A/Prof. Gilbert Lau Kwang Fatt
Dr Lee Kheng Hock
The contents are not to be reproduced in part or in whole, without prior written approval from the editor. Whilst every effort is made in compiling the content of this publication,the publishers, editors and authors accept no liability whatsoever for the consequences of any inaccurate or misleading data, opinions or statements. The mention of any product by the authors does not imply any official endorsement of the product by the Health Sciences Authority.
Copyright© 2007 Health Sciences Authority of Singapore. All Rights Reserved.
Adverse Drug Reaction News • December 2007 • Vol.9 No.3
Voluntary suspension
of sales of
aprotinin (Trasylol®)