Accessing VA MH Services - University of Texas at...
Transcript of Accessing VA MH Services - University of Texas at...
Accessing VA MH Services:
We’re Not Your Father’s VA Anymore!
Steve Holliday, Ph.D, ABPP-CN
V17 Chief Mental Health Officer
210-694-6223
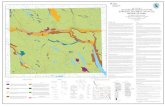
VA in Texas
• VISN 17 - Covers 4 VA Health Care Systems along IH-35 from Dallas to Brownsville
– North Texas HCS (Dallas & Ft. Worth)
– Central Texas HCS (Waco/Temple/Austin)
– South Texas HCS (San Antonio & Kerrville)
– Valley/Costal Bend HCS (Harlingen, Laredo, & CC)
• VISN 16 – Houston & East Texas
• VISN 17 – El Paso & West Texas
Eligibility • OEF/OIF Vets have full eligibility for 5 years
• Served >180 days or Service-connected
• Must have Honorable or General D/C
–Bad D/Cs can be upgraded
• Co-Pays at Higher Incomes Unless SC
• Eligible Vets Receive All VHA Services
• Incarcerated Vets NOT eligible for VA Care
– Except for Outreach Visits by VJOs & RSs
– SC Vets Must Report Incarcerations!
MH Uniform Services Plan
• Based on President’s MH Commission & Recovery Model
• Emphasis on MH/PCC and Suicide Prevention
• Mandates Core MH Services at Each Site
• Standardized MH Care Throughout USA
• Significantly Enhanced MH Staff/Capacity
• Mandates Evidence-Based MH Services
• Site Visits Track Implementation & Access
Rehabilitation/Recovery Model • Recovery is possible for everyone (even SMI)
• It’s the Vet’s Recovery Plan; Not the Doc’s – Uses Understandable, Non-stigmatizing Language
– Based on Vet’s Needs, Strengths & Life Goals
• Use of Certified Peer Counselors
• Include Consumers in MH Planning/Mgmt
• Meaningful Work is the Best Therapy
• Building Support Systems in the Community
• Educating to Reduce Stigma/Facility Recovery Coordinators
VA MH Continuum of Care • ED & Acute Inpatient MH Services • Co-located MH in Primary Care Clinics • Outpatient Mental Health Clinics • Residential Rehabilitation Programs (RRTPs)
– Domiciliary (Doms)… Unique to VA – General, Homeless , PTSD, MST, SUD RRTPs
• Community-based MH Specialty Care – PTSD/MST/SUD Clinics – MHICM Teams for SMI – Homeless Programs (including Justice-involved Vets) – Vocational Programs – Telehealth & Home Health – Suicide Prevention
MH in Primary Care • Co-located Mental Health in Primary Care
– Reduces Stigma for Seeking MH Care
– Rapid Access for MH Screening/Services
– Treatment for Mild MH issues
• Adjustment Issues/Managing Stress
• Uncomplicated Depression & Anxiety D/Os
• Harm Reduction/ME for SUDs
– Referral to MHC/Specialized Tx Programs
• Up to 80% of Cases Managed in PCC
• Healthy Behaviors/Disease Mgmt
Outpatient MH Clinics • BHIP Teams for Extended Outpt. MH Care
• MH Treatment Coordinator for Each Vet
• EB Psychotherapies & Medications for – Depression
– PTSD and MST
– Anxiety Disorders
– Psychotic Disorders
– Couples Therapy
• Refer to Specialty MH Care Programs & Back to Primary Care When Stable
Evidence-Based Treatments • Evidence-Based Psychotropic Medications
– Opiate Safety Initiative, e.g. Benzos + Opiates – Addressing Over/Under Medication with New Metrics
• Evidence-Based Psychotherapies – PE/CPT/ACT for PTSD – CBT for Depression – SUD – ME, 12-SFT, New Medications – Couples/Marital Therapy – SST, PST and MHICM for SMI – DBT and CAMS for Suicide Attempts (VISN 17 only)
• National Training Programs in EBTs – One-week intensive workshop (national experts) – 6-12 Months of weekly case supervision – Train the Trainer Model for future staff
Substance Use Treatment
• Universal Screening Annually (CRs in CPRS)
• Building Motivation/Education in PCC & MHCs
• Inpatient/Outpatient DETOX
• Outpatient SUD Program (1 day/week)
• Intensive Outpatient SUD Program (3-5 days)
• SARRTP (28 Day Residential)
• SUD Tracks in Doms (90-Day Residential)
• Meds for SUD (Bup, Naltrexone, Methadone)
Ending Homelessness! • VA Secretary’s 5-Year Plan – $3.2 Billion
• From 160K to ZERO Homeless Vets!
• Enhanced Existing Homeless Services – HUD-VASH Vouchers
– Enhanced VA SUD and MH Capacity
– Enhanced RRTP/Doms & Contract Beds
– Enhanced Jail/Prison Diversion & Outreach
• New Initiatives/Services – Homeless Hot Line
– Emergency Funding to Prevent Homelessness
Justice-Involved Veterans
• VA Prison Re-Entry Program
– State/Federal Prisons
– Enrolling Eligible Veterans
– Appointments for Care After Release
– Case Management until connected
• Veterans Justice Outreach Program
– County/Local Jails Re-Entry Outreach
– Liaison with local Veterans Courts
– Educate local Law Enforcement/Others
Vocational Rehabilitation
• VBA Educational Benefits (30%+ SC)
• Incentive Therapy (IT)
• Compensated Work Therapy (CWT)
• Supported Community Employment
• Job Search Assistance
• Assistance with VA/SSDI Claims (VSOs)
• Volunteer Positions
Tele Health Services
• Telemental Health Services
– EBTs from the Hospitals to Remote Clinics
– Cross coverage for Smaller MHCs
– “Health Buddies” to Monitor SMI at Home
– Home-based TMH for Highly Rural Vets
– Reduces Barriers of Distance & Stigma
• New Technology
– Anonymous Chat Rooms (Suicide Hot Line)
– Mobile Apps for PTSD and Suicide Prevention
– MyhealthEvet, Secure Email with Providers
Suicide Prevention • National Suicide Hotline 1-800-273-TALK (8255)
– Staffed by Trained MH Providers 24/7
– Over 3000 Rescues in Past Year
– Arrange for Immediate Help
– Live Hand Off to Local VA Facilities for F/U
• Facility Suicide Prevention Coordinators – Suicide Risk Assessments
– Maintains List of High Risk Patients/Chart Flags
– Develops/Implements Suicide Safety Plans
– Investigates Attempts/Completed Suicides
– Educates Staff and Community
24
Warning Signs • Observable signs of serious depression
Unrelenting low mood Pessimism Hopelessness Desperation Anxiety, psychic pain, inner tension Withdrawal Sleep problems
• Increased alcohol and/or other drug use • Recent impulsiveness and taking unnecessary risks • Threatening suicide or expressing strong wish to die • Making a plan
Giving away prized possessions Purchasing a firearm Obtaining other means of killing oneself
You can help. . .
25
• Show you care Take ALL talk of suicide seriously
If you are concerned that someone may take their life, trust your judgment!
Listen Carefully
Reflect what you hear
Use language appropriate for age of person involved Do not worry about doing or saying exactly the
"right" thing. Your genuine interest is what is most important.
You can help. . .
26
• Be Genuine Let the person know you really care. Talk
about your feelings and ask about his or hers. "I'm concerned about you…about how you feel."
"Tell me about your pain."
"You mean a lot to me and I want to help."
"I care about you, about how you're holding up."
"I don't want you to kill yourself."
"I'm on your side…we'll get through this."
You can help. . .
27
Ask about suicide • Don't hesitate to raise the subject.
Talking with people about suicide won't put the idea in their heads. Chances are, if you've observed any of the warning signs, they're already thinking about it. Be direct in a caring, non-confrontational way. Get the conversation started.
You can help. . .
28
You do not need to solve all of the person's problems;
Just engage them
Are you thinking about suicide?
What thoughts or plans do you have?
Are you thinking about harming yourself, ending your life?
How long have you been thinking about suicide?
Have you thought about how you would do it?
Do you have __? (Insert the lethal means they have mentioned.)
Do you really want to die? Or do you want the pain to go away?
You can help. . .
29
Intervention Step Three: •Get help but do NOT leave the
person alone Know referral resources
Reassure the person
Encourage the person to participate in helping process
Outline safety plan
You can help. . .
IT’S YOUR CALL VA Suicide Prevention Outreach Campaign
Presentation to Suicide Prevention Coordinators 03.13.2011
The Best Care Anywhere By Phillip Longman
Ten years ago, veterans hospitals were dangerous, dirty, and scandal-ridden. Today, they're producing the highest quality care in the country. Their turnaround points the way toward solving America's health-care crisis.
Washington Monthly
The Best Medical Care in the U.S.
The VA uses the data gathered in its computers to pinpoint problem areas, such as medication errors. The network also allows it to track how closely the medical staff is following evidence-based treatment and monitor deficiencies. Such tracking pays off. When Rand did an extensive study comparing quality of care at the VA with private-sector hospitals, it found that performance measurement played an important role in helping the VA score higher in every category except acute care, where it came in about even.
Business Week
VA Medical System Earns High Customer Satisfaction Ratings
Good news about government is rare enough. What's outright shocking is when that good news is about how nice government employees are. But that is the bottom line of the recently released American Customer Satisfaction Index report on the Department of Veterans Affairs' medical system.
Not only do veterans rate their VA care much higher
overall than the general population rates its hospital experiences, vets also consistently give VA doctors and nurses high scores for "responsiveness" (83 out of a possible 100), courtesy (90), and "respect and dignity afforded patients" (91).
National Journal
VA: From Worst to First! • Moving from Hospitals to the Community
• CPRS & Performance Measures
– Improved Access to Care
– Improved Quality of Care & Outcomes
– Improved Cost Effectiveness
– Improved Patient Satisfaction
• Holding VA Staff Accountable
– Managers’ Performance Plans
– Providers Performance Plans/Incentive Pay
Electronic Medical Record • Follows Veterans Across Sites/Locations of Care
• Digital X-Rays, Consults, Meds, Lab, etc.
• Flags for High-Risk Conditions
• Clinical Reminders for Better Care • MH/SUD Screening that Requires F/U
• Smoking Cessation
• Obesity/Weight Management
• Diabetes
• Hypertension
• Tracks Quality of Care through PMs
• Integration with DoD Medical Records
Next Steps… • Contact your VISN MH Lead
– VISN 16: [email protected]
– VISN 17: [email protected]
– VISN 18: [email protected]
• Meet your local VJO (see next slide)
• Work with your local MHMR Jail Diversion Committee!
• Work to Establish Veterans’ Courts
• Ask you clients if they are Vets and give us a chance to help!
VJOs in Texas
TEXAS VJO LIST Location VJO NAME Email PHONE
AMARILLO 6010 W Amarillo Blvd, Amarillo, TX 79106 Kathleen Caldwell [email protected] 806-355-9703, Ext. 7543
AUSTIN 1701 Directors Boulevard, Austin, TX 78744 Karen Janda, LCSW [email protected] 512-433-2017
BONHAM 1201 E. 9th St. Bonham, TX 75418 Melissa Stroop [email protected] 903-583-6262
DALLAS/FT WORTH 4500 S Lancaster Rd, Dallas, TX 75216 Latisha Gaten, LMSW [email protected] 214-857-2252
4500 S Lancaster Rd, Dallas, TX 75216 Kathy Finch, LCSW [email protected] 214-857-2260
CORPUS CHRISTI 5283 Old Brownsville Road, Corpus Christi, TX 78405 Edward (Chad) Henderson, Ph.D., LCSW [email protected] 956-490-0440
5283 Old Brownsville Road, Corpus Christi, TX 78405 Yasisca Pujols, Ph.D. [email protected] 956-291-9202
EL PASO 5001 N Piedras St, El Paso, TX 79930 Ellyn Black [email protected] 915-564-6100, Ext. 6159
HOUSTON 2002 Holcombe Blvd, Houston, TX 77030 Loretta Coonan, LCSW [email protected] 832-260-1361
SAN ANTONIO 7400 Merton Minter San Antonio, TX 78229 Treva Neiss, LCSW [email protected] 210-616-9915
7400 Merton Minter San Antonio, TX 78229 Jill A. Koenig, Ph. D. [email protected] 210-617-5300, Ext. 15121
WACO/TEMPLE 4800 Memorial Drive, Waco, TX 76711 Rekita Justice-Logan, LCSW, CCM [email protected] 254-421-7038
Other Resources • www.va.gov/health/
• www.texvet.com – On Line Searchable Database for Vets
– Texas MH, Job, Education, Emergency Services
• 211 Texas – Just Dial 211
– 24/7 Information Line
• Vet Centers – Storefront Locations, Walk-ins
– Veteran and Family Counseling
– GWAT Outreach Staff